Abstract
AIM: To clarify clinical features of the NSAID-induced small bowel lesions using a new method of endoscopy.
METHODS: This is a retrospective study and we analyzed seven patients with small bowel lesions while taking NSAIDs among 61 patients who had undergone double-balloon endoscopy because of gastro-intestinal bleeding or anemia between September 2000 and March 2004, at Jichi Medical School Hospital in Japan. Neither conventional EGD nor colonoscopy revealed any lesions of potential bleeding sources including ulcerations. Double-balloon endoscopy was carried out from oral approach in three patients, from anal approach in three patients, and from both approaches in one patient.
RESULTS: Ulcers or erosions were observed in the ileum in six patients and in the jejunum in one patient, respectively. The ulcers were multiple in all the patients with different features from tiny punched out ulcers to deep ulcerations with oozing hemorrhage or scar. All the patients recovered uneventfully and had full resolution of symptoms after suspension of the drug.
CONCLUSION: NSAIDs can induce injuries in the small bowel even in patients without any lesions in both the stomach and colon.
Keywords: Double-balloon endoscopy, NSAIDS-induced small bowel injuries
INTRODUCTION
Adverse effects of non-steroidal anti-inflammatory drugs (NSAIDs) in the upper and lower gastro-intestinal tract are well known[1]. In addition, NSAIDs can induce and exacerbate damage in the small bowel[2,3]. There is a study showing that 8.4% of patients taking NSAIDs developed small bowel ulcerations[4]. Evidence that those lesions may also cause perforation, strictures or hemorrhage stems from a case-control study and several case reports[5-14]. Despite the necessity, endoscopic observation of the small intestine was technically difficult because of its long length and multiple complex looped configurations. Recently, a video capsule endoscopy, which enables observation of the entire small bowel, was developed and this novel technology provided an outstanding progress for the diagnosis of small bowel diseases[15-19]. In addition, we have developed a new method of endoscopy using a double-balloon technique (Fujinon EN-450P5/20, Fujinon Corp., Saitama, Japan), which also allows observations of small bowel under controlled movement even from a retrograde approach[20-23]. The aim of this study was to delineate clinical features of the NSAID-induced small bowel mucosal injuries using the double-balloon endoscopy.
MATERIALS AND METHODS
The records of all the patients who underwent double-balloon endoscopy at Jichi Medical School Hospital, Japan between September 2000 and March 2004 were reviewed. Patients were identified from endoscopy case logs and cross-referenced with pathology database. Charts were also reviewed for NSAID prescription in those patients. Necessary telephone interview was also carried out. Patients with pre-existing or concomitant risk factors for possible small bowel complications, including Crohn’s disease and mesenteric vascular disease, were excluded and all the patients with evidence of other small bowel pathology were also excluded. Reasons for exclusion on review of pathology included inflammatory bowel disease, small bowel lymphoma, primary or metastatic carcinoma, small bowel gastro-intestinal stromal tumor, small bowel granuloma, small bowel diverticulum, angiodysplasia, and post-operative lesions. Two patients who have been on NSAIDs, were excluded and seven patients, in whom small bowel injuries were found while still on NSAIDs, were selected among 61 patients with obscure gastro-intestinal bleeding. These seven patients, two men and five women, with ages ranging 65-89 years (73.7 years on an average), were enrolled and subjected to the analysis.
RESULTS
Of these seven patients, six had melena and one had undetermined anemia with positive fecal occult blood tests during NSAID medications. Underlining disease of these patients included knee joint pain, back pain, headache, and rheumatoid arthritis. Neither conventional EGD nor colonoscopy revealed any lesions of possible cause of bleeding including ulcerations except for one patient (patient 1) in whom gastric ulcer scar was observed. Drug usage by these patients consisted of diclofenac in four patients (57%), and either ampiroxicam, aspirin, or loxoprofen in each of the remaining three patients, respectively (Table 1). Duration of the medication was different for patients, ranging from 7 d to 10 years. More than five units of packed red blood cell was required on an average for blood transfusion before diagnosis.
Table 1.
Clinical Features of the patients with nonsteroidal anti-inflammatory drug-induced small bowel lesions
| Patient | Age/sex | Approach | Partial /total | Findings | Location | Dose (mg/d) | NSAIDs | Duration | Serum albumin (g/dL) | Blood transfusion (unit1) |
| 12 | 89/M | Oral | Partial, -middle ileum | Ulcers and erosions | Ileum | 27 | Ampiroxicam | 10 yr | 2.1 | 10 |
| 2 | 69/F | Oral | Total | Ulcers | Ileum | 25 | Diclofenac | 7 yr | 3.1 | 12 |
| 3 | 65/M | Anal | Partial, -upper jejunum | Ulcers and erosions | Ileum | 75 | Diclofenac | 1 wk | 3.9 | 0 |
| 4 | 76/F | Anal | Partial, -middle ileum | Ulcers | Ileum | 25 | Diclofenac | 8 yr | 2.7 | 7 |
| 5 | 74/F | Anal | Partial, -upper ileum | Erosions | Ileum | 100 | Aspirin | 4 yr | 3.5 | 0 |
| 6 | 76/F | Oral | Partial, -upper ileum | Ulcers | Jejunum | 120 | Loxoprofen | 4 yr | 1.9 | 8 |
| 7 | 67/F | Oral+anal | Total | Ulcers | Ileum | 75 | Diclofenac | 1 yr | 3 | 0 |
11 unit = Packed blood cells separated from 450 mL of whole blood. 2Gastric ulcer scar was observed in this patient.
Double-balloon endoscopy was carried out from oral approach alone in three patients and from anal approach alone in three patients. The approach route was chosen, based on the clinical information including color of the stool. The depth of insertion estimated from the number of pleating procedures and the fluoroscopic images of the small intestine and endoscope in these patients was difficult but approximately 1/2-2/3 of the entire length of the small intestine with rough estimation, although we have succeeded in examining the entire small intestine from oral approach alone in one patient. In addition, another patient underwent total enteroscopy by both approaches. Patient’s demographics are delineated in Table 1. Whether the lesions were located in the jejunum or ileum was determined radiographically based on a distance from either pylorus ring or ileocecal valve in each case. Ulcers or erosions were observed in the ileum in six patients (86%) and in the jejunum in one patient (14%). The ulcers were multiple in all the patients with different features from tiny punched out ulcers (Figure 1) to deep ulcerations with oozing hemorrhage (Figure 2A) or scar. Edematous villi around the ulcers were prominent features by the endoscopic observation. Oozing hemorrhage from the ulcer, observed in one patient, was treated endoscopically using coagulator (ERBE, German, Figure 2B). Of interest, both circular ulcers (Figure 3A) and circular scars (Figure 3B) were observed in a different part of the small bowel in the same patient. Biopsies, taken from the edge of the ulcer in two patients, revealed non-specific inflammation. All the patients recovered uneventfully and had full resolution of the symptoms in accordance with their hemoglobin levels after suspension of the drug.
Figure 1.
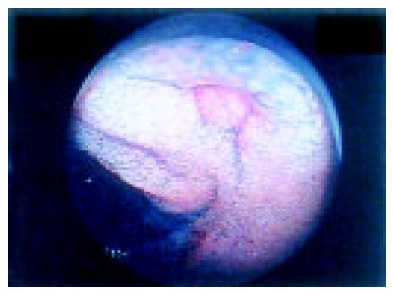
Endoscopic view of the punched-out ulcer in the ileum in a 65-year-old woman (patient 3). Edematous villi were observed around the ulcer.
Figure 2.
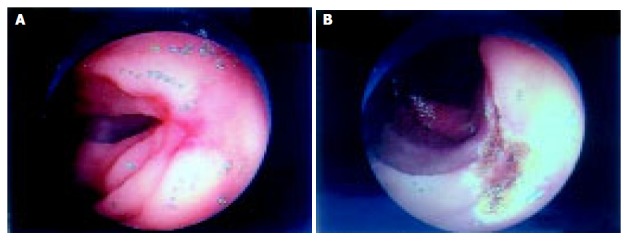
Endoscopic view of the ulcer with oozing hemorrhage in the ileum in a 74-year-old woman (patient 4). A: Before coagulation therapy; B: After coagulation therapy.
Figure 3.
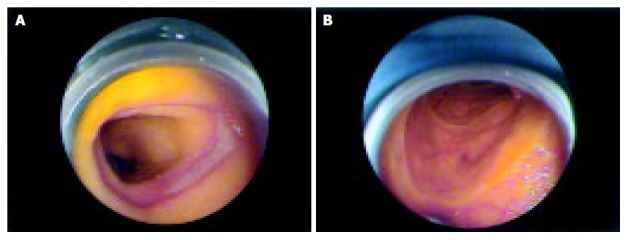
Endoscopic view of the (A) circular ulcer and (B) circular ulcer scar in the ileum in a 67-year-old woman (patient 7).
DISCUSSION
This is a report to delineate NSAID-induced small bowel injuries using double-balloon endoscopy. NSAID-induced injuries were identified in seven out of 61 patients with obscure gastro-intestinal bleeding (11.5%). Despite limitation of this study due to the lack of observation of the entire small bowel in most patients, NSAID-induced ulcers were observed more frequently in the ileum than in the jejunum in consistent with a previous report by Kessler et al[13]. Further prospective study intended for evaluation of the entire small bowel, if substantiated, will clarify the exact distribution of NSAIDs-induced lesions. NSAIDs-induced lesions, identified by endoscopy, were multiple with different features from tiny ulcers to hemorrhagic ulcers or circular ulcers. These different features of ulcers, even observed in different parts of the small intestine in the same patient, may represent different stages of ulcers. The ulcers may be healing, because NSAIDs were suspended on the day of admission in all patients. Alternatively, either the dose of NSAIDs or the length that NSAIDs that was given, could attribute to the difference in size and shape of the ulcers, although such tendency was not observed in our study. Of interest, we could observe circular ulcers and even circular scars in the same patients. This observation may reinforce the association between ulcers and severe strictures in the small bowel after NSAID therapy. Further study describing the feature of circular ulcers is warranted for better understanding of these relationships.
In conclusion, NSAID-induced injuries in the small bowel were endoscopically observed and described using double-balloon endoscopy. NSAIDs-induced ulcers were found in the small bowel even in patients without any ulcers and erosions in the stomach as well as colon. Although this was a preliminary study, double-balloon endoscopy was useful for the direct observation and description of each lesion in detail by anterograde as well as retrograde approach.
Footnotes
Science Editor Guo SY Language Editor Elsevier HK
References
- 1.Bjarnason I, Hayllar J, MacPherson AJ, Russell AS. Side effects of nonsteroidal anti-inflammatory drugs on the small and large intestine in humans. Gastroenterology. 1993;104:1832–1847. doi: 10.1016/0016-5085(93)90667-2. [DOI] [PubMed] [Google Scholar]
- 2.Davies NM, Saleh JY, Skjodt NM. Detection and prevention of NSAID-induced enteropathy. J Pharm Pharm Sci. 2000;3:137–155. [PubMed] [Google Scholar]
- 3.de Sanctis S, Qureshi T, Stebbing JF. Clinical and pathological overlap in nonsteroidal anti-inflammatory drug-related small bowel diaphragm disease and the neuromuscular and vascular hamartoma of the small bowel. Am J Surg Pathol. 2001;25:539–541. doi: 10.1097/00000478-200104000-00017. [DOI] [PubMed] [Google Scholar]
- 4.Allison MC, Howatson AG, Torrance CJ, Lee FD, Russell RI. Gastrointestinal damage associated with the use of nonsteroidal antiinflammatory drugs. N Engl J Med. 1992;327:749–754. doi: 10.1056/NEJM199209103271101. [DOI] [PubMed] [Google Scholar]
- 5.Madhok R, MacKenzie JA, Lee FD, Bruckner FE, Terry TR, Sturrock RD. Small bowel ulceration in patients receiving non-steroidal anti-inflammatory drugs for rheumatoid arthritis. Q J Med. 1986;58:53–58. [PubMed] [Google Scholar]
- 6.Langman MJ, Morgan L, Worrall A. Use of anti-inflammatory drugs by patients admitted with small or large bowel perforations and haemorrhage. Br Med J (Clin Res Ed) 1985;290:347–349. doi: 10.1136/bmj.290.6465.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bjarnason I, Zanelli G, Prouse P, Smethurst P, Smith T, Levi S, Gumpel MJ, Levi AJ. Blood and protein loss via small-intestinal inflammation induced by non-steroidal anti-inflammatory drugs. Lancet. 1987;2:711–714. doi: 10.1016/s0140-6736(87)91075-0. [DOI] [PubMed] [Google Scholar]
- 8.Bjarnason I, Price AB, Zanelli G, Smethurst P, Burke M, Gumpel JM, Levi AJ. Clinicopathological features of nonsteroidal antiinflammatory drug-induced small intestinal strictures. Gastroenterology. 1988;94:1070–1074. doi: 10.1016/0016-5085(88)90568-9. [DOI] [PubMed] [Google Scholar]
- 9.Lang J, Price AB, Levi AJ, Burke M, Gumpel JM, Bjarnason I. Diaphragm disease: pathology of disease of the small intestine induced by non-steroidal anti-inflammatory drugs. J Clin Pathol. 1988;41:516–526. doi: 10.1136/jcp.41.5.516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Matsuhashi N, Yamada A, Hiraishi M, Konishi T, Minota S, Saito T, Sugano K, Yazaki Y, Mori M, Shiga J. Multiple strictures of the small intestine after long-term nonsteroidal anti-inflammatory drug therapy. Am J Gastroenterol. 1992;87:1183–1186. [PubMed] [Google Scholar]
- 11.Speed CA, Bramble MG, Corbett WA, Haslock I. Non-steroidal anti-inflammatory induced diaphragm disease of the small intestine: complexities of diagnosis and management. Br J Rheumatol. 1994;33:778–780. doi: 10.1093/rheumatology/33.8.778. [DOI] [PubMed] [Google Scholar]
- 12.Davies NM, Jamali F, Skeith KJ. Nonsteroidal antiinflammatory drug-induced enteropathy and severe chronic anemia in a patient with rheumatoid arthritis. Arthritis Rheum. 1996;39:321–324. doi: 10.1002/art.1780390222. [DOI] [PubMed] [Google Scholar]
- 13.Kessler WF, Shires GT, Fahey TJ. Surgical complications of nonsteroidal antiinflammatory drug-induced small bowel ulceration. J Am Coll Surg. 1997;185:250–254. doi: 10.1016/s1072-7515(97)00067-7. [DOI] [PubMed] [Google Scholar]
- 14.Zalev AH, Gardiner GW, Warren RE. NSAID injury to the small intestine. Abdom Imaging. 1998;23:40–44. doi: 10.1007/s002619900282. [DOI] [PubMed] [Google Scholar]
- 15.Iddan G, Meron G, Glukhovsky A, Swain P. Wireless capsule endoscopy. Nature. 2000;405:417. doi: 10.1038/35013140. [DOI] [PubMed] [Google Scholar]
- 16.Appleyard M, Fireman Z, Glukhovsky A, Jacob H, Shreiver R, Kadirkamanathan S, Lavy A, Lewkowicz S, Scapa E, Shofti R, et al. A randomized trial comparing wireless capsule endoscopy with push enteroscopy for the detection of small-bowel lesions. Gastroenterology. 2000;119:1431–1438. doi: 10.1053/gast.2000.20844. [DOI] [PubMed] [Google Scholar]
- 17.Costamagna G, Shah SK, Riccioni ME, Foschia F, Mutignani M, Perri V, Vecchioli A, Brizi MG, Picciocchi A, Marano P. A prospective trial comparing small bowel radiographs and video capsule endoscopy for suspected small bowel disease. Gastroenterology. 2002;123:999–1005. doi: 10.1053/gast.2002.35988. [DOI] [PubMed] [Google Scholar]
- 18.Lewis BS, Swain P. Capsule endoscopy in the evaluation of patients with suspected small intestinal bleeding: Results of a pilot study. Gastrointest Endosc. 2002;56:349–353. doi: 10.1016/s0016-5107(02)70037-0. [DOI] [PubMed] [Google Scholar]
- 19.Van Gossum A. Capsule endoscopy in patients with obscure GI bleeding. Gastrointest Endosc. 2003;57:629; author reply 629–630. doi: 10.1067/mge.2003.172. [DOI] [PubMed] [Google Scholar]
- 20.Yamamoto H, Sekine Y, Sato Y, Higashizawa T, Miyata T, Iino S, Ido K, Sugano K. Total enteroscopy with a nonsurgical steerable double-balloon method. Gastrointest Endosc. 2001;53:216–220. doi: 10.1067/mge.2001.112181. [DOI] [PubMed] [Google Scholar]
- 21.Yamamoto H, Sugano K. A new method of enteroscopy--the double-balloon method. Can J Gastroenterol. 2003;17:273–274. doi: 10.1155/2003/309532. [DOI] [PubMed] [Google Scholar]
- 22.Hashimoto A, Yamamoto H, Yano T, Hashimoto N, Kita H, Kawakami S, Miyata T, Sunada K, Ohnishi N, Iwamoto M, et al. A case of malignant lymphoma of the small intestine with successful endoscopic hemostasis using double-balloon enteroscopy. Progress Dig Endoscopy. 2003;62:104–105. [Google Scholar]
- 23.Yamamoto H, Kita H, Sunada K, Hayashi Y, Sato H, Yano T, Iwamoto M, Sekine Y, Miyata T, Kuno A, et al. Clinical outcomes of double-balloon endoscopy for the diagnosis and treatment of small-intestinal diseases. Clin Gastroenterol Hepatol. 2004;2:1010–1016. doi: 10.1016/s1542-3565(04)00453-7. [DOI] [PubMed] [Google Scholar]


