Abstract
Background
Dialysis patients have an excessive risk of cardiovascular death after myocardial infarction (MI). Underutilization of cardiac therapies may partially explain this risk, but whether patients on maintenance dialysis have differential rates of coronary angiography or revascularization during admission for MI compared with patients not on dialysis and whether these differences are explained by the presence of comorbid illness were uncertain.
Methods
We analyzed 154692 patients with a primary diagnosis of MI in the 2001 National Inpatient Sample, and we compared procedure use in patients on long-term dialysis, patients with non–dialysis-dependent chronic kidney disease (CKD), or normal renal function.
Results
Dialysis patients and patients with dialysis-independent CKD were significantly less likely to undergo coronary angiography than patients with normal renal function (39% and 34% vs 56%). They were also less likely to undergo coronary revascularization (19% and 23% vs 41%) or to have a coronary intervention after diagnostic angiography (46% and 62% vs 70%). After adjustment, these differences remained, with a lower likelihood of angiography (42% and 45% vs 56%), revascularization (22% and 31% vs 41%), or coronary intervention after diagnostic angiography (52% and 66% vs 70%).
Conclusions
Despite a high mortality rate after MI, patients on dialysis are markedly less likely than patients with dialysis-independent CKD or normal renal function to undergo diagnostic angiography or coronary revascularization after admission for MI. Additional studies to determine how these disparities are related to mortality are warranted.
The US long-term dialysis population is plagued by a high incidence of fatal and nonfatal myocardial infarction (MI) and will grow to more than 600000 patients by 2010.1 Approximately 30% of new dialysis patients will experience an MI2 within 5 years, and their 30-day mortality rate will be much higher than in general population or in other high risk populations.3,4 Within the first year after MI, 59.3% of dialysis patients will die, and by 5 years, 89% will die.5
This high mortality rate may be due to underutilization of life-saving medical and revascularization therapies.6,7 Although initiation of aspirin therapy, β-receptor blockade, and angiotensin-converting enzyme inhibition have been shown to extend survival in the general population,8–10 patients on dialysis are far less likely than others to be treated with these medications after MI.7 Coronary revascularization also reduces mortality after MI in the general population,11–13 but the rate of coronary angiography and coronary revascularization after MI in dialysis patients has not been well contrasted with rates in the general population. We evaluated whether rates of coronary angiography and revascularization in maintenance dialysis patients differ from rates in patients not on dialysis, and we adjusted these findings for relevant comorbidities that might account for observed differences.
Methods
Patient population
The 2001 National Inpatient Sample (NIS) is a nationally representative sample of inpatient records collected by the Healthcare Cost and Utilization Project. In 2001, administrative data from more than 7.4 million admissions to 1000 hospitals in 33 states were collected. Demographics, diagnoses, procedures, length of stay, costs, and hospital characteristics are recorded from the day of admission through the day of discharge. Our analyses were conducted within the subset of patients with a primary diagnosis of MI.
Selection criteria
Diagnoses and procedures were identified from International Classification of Diseases, Ninth Edition, Clinical Modification (ICD-9-CM) diagnostic and procedure codes. Patients with a principal diagnosis of acute MI were identified by the codes 410.0-9.
Our aim was to analyze the differential use of invasive cardiac procedures after MI in patients with chronic, dialysis-dependent, end-stage renal disease compared with patients not requiring dialysis at the time of admission. The study population was therefore divided into 3 groups: (1) long-term dialysis, (2) dialysis-independent chronic kidney disease (CKD), and (3) normal renal function or no significant CKD. Long-term dialysis patients were identified from their use of peritoneal dialysis or hemodialysis (54.98 and 39.95) in the absence of acute renal failure (584) during the hospitalization. Patients with CKD were identified using a validated algorithm based on the presence of codes for renal insufficiency (582, 583, 585-587), diabetic nephropathy (250.4, 250.41-43), or hypertensive nephropathy (403.xx).14 Individuals not meeting criteria for long-term dialysis or CKD status were assigned to the third group.
Procedural definitions
Coronary angiography (37.22-37.23 and 88.53-88.57), percutaneous coronary intervention (PCI, 36.01-36.06), thrombolysis (99.10), and coronary artery bypass grafting (CABG, 36.10-36.19) were identified from procedure codes. Diagnostic cardiac catheterization included both angiography and percutaneous intervention. Revascularization included both PCI and CABG.
Definition of comorbid conditions
Baseline comorbidities (Table I) were identified with minor modifications of the methods described by Elixhauser et al,15 which was developed and validated within a subset of the NIS and was predictive of mortality and resource use after MI in this database.16 A condition was considered a baseline comorbidity if ICD-9 codes for that individual condition were present and diagnosis related group (DRG) codes were absent. Cardiac comorbidities were not distinguished from cardiac complications of the index MI, and we identified valvular heart disease, congestive heart failure, and arrhythmia from the presence of the corresponding ICD-9 codes alone.15 Pneumonia (480-486) and sepsis (041, 038) were prespecified as conditions that might delay invasive coronary procedures until a subsequent admission.
Table I.
Baseline covariates (N = 154692)
| Characteristic | Dialysis (N = 2369) | CKD (N = 8957) | Normal renal function (N = 143367) |
|---|---|---|---|
| Age (SE) (y) | 67.45 (0.32) | 73.34 (0.20) | 68.33 (0.16) |
| Male | 1292 (54.5) | 5171 (57.7) | 84742 (59.1) |
| Black race | 465 (24.9) | 765 (11.2) | 7490 (7.1) |
| Medicare | 1866 (78.7) | 6880 (76.8) | 82249 (57.4) |
| Admitted to teaching hospital | 1126 (49.5) | 3492 (40.8) | 59006 (42.9) |
| Diabetes | 1348 (57.0) | 4662 (52.2) | 37070 (25.9) |
| Congestive heart failure | 1342 (56.5) | 5483 (5.8) | 41605 (29.0) |
| Arrhythmia | 649 (27.2) | 2586 (28.9) | 31743 (22.1) |
| Valvular heart disease | 369 (15.5) | 1453 (16.2) | 16150 (11.2) |
| Pulmonary circulatory disease | 71 (2.98) | 251 (2.8) | 2427 (1.7) |
| Neurologic disorders | 102 (4.3) | 328 (3.7) | 4452 (3.1) |
| Chronic pulmonary disease | 399 (16.8) | 1996 (22.2) | 25428 (17.7) |
| Cancer | 162 (6.85) | 604 (6.7) | 10008 (7.0) |
| Coagulopathy | 133 (5.61) | 346 (3.9) | 3214 (2.2) |
| Peripheral vascular disease | 391 (16.6) | 1163 (13.0) | 9410 (6.6) |
| Sepsis | 212 (8.92) | 669 (7.5) | 4963 (3.5) |
| Pneumonia | 205 (2.31) | 924 (10.3) | 7718 (5.4) |
The data are expressed as number (%), unless otherwise noted.
Statistics and sensitivity analysis
Univariable analyses were performed using Student t tests or χ2 tests, as appropriate. Relative risks were calculated against the normal renal function group. Statistical significance was defined as P < .05. All analyses were performed using SAS-callable SUDAAN (RTI, Durham, NC) to account for the complex clustered sampling structure of the NIS.
Multivariable logistic regression was used to adjust for confounding. Factors in Table I as well as AIDS, liver disease, peptic ulcer disease, obesity, alcohol or drug abuse, and psychiatric disorders were included in an initial logistic regression model. Age, sex, race, and renal function were forced into the model, and backward stepwise logistic regression was used to generate the final model. Terms whose removal did not alter the effect estimate for dialysis status by ≥10% were removed in order of significance. Because racial data are not collected by several states, a term indicating missing race was generated to prevent data from these states from being discarded by our software in the regression models. Exclusion of admissions with missing values had minimal effect on the results of these analyses (data not shown).
Dialysis patients are typically dialyzed 3 times per week, whereas development and recovery from dialysis-dependent acute renal failure are unlikely to occur in less than 7 days. We repeated our main regression models in data sets restricted to subjects with lengths of stay >2 days or ≤1 week to investigate the sensitivity of our analyses to misclassification of short-term and long-term dialysis status. The sensitivity of our results to the adjustment scheme was examined using quintiles of the Charlson comorbidity score to adjust for comorbidity.
Results
Study population
Of the entire NIS sample, 154692 (2.1%) patients were admitted with a principal diagnosis of acute MI. Two thousand three hundred sixty-nine (1.5%) were on long-term dialysis and 8957 (5.8%) had CKD. Dialysis patients were younger and were more likely to be black, to be admitted to a teaching hospital, and to have Medicare as their primary insurance. Compared with subjects with CKD or subjects without renal disease, dialysis patients had a higher incidence of diabetes, congestive heart failure, peripheral vascular disease, and coagulopathy. They were less likely to be diagnosed with an anterior MI (7.7%, 11.0%, and 16.4%, respectively, P < .0001) or pneumonia (2.3% vs 10.3% and 5.4%, P < .0001) (Table I). Finally, dialysis patients had longer (8.3 vs 8.1 and 5.2 days, P < .0001) and more expensive hospitalizations ($40147 vs $37697, and $30297, P < .00001) than patients with CKD or without renal disease.
Rates of cardiac procedures
Maintenance dialysis patients were less likely than non–dialysis-dependent patients to undergo invasive coronary procedures (Figure 1, Table II). The incidence of either surgical or percutaneous revascularization was 19.2% in dialysis patients, 23.0% in patients with CKD, and 41.4% in patients in the normal renal function group (RR vs normal renal function, 0.46 [95% CI 0.42–0.52] and 0.56 [95% CI 0.53–0.59] for dialysis and patients with CKD, respectively). Rates of diagnostic angiography were also substantially lower in dialysis patients (38.6%, RR 0.68, 95% CI 0.64–0.73) and in patients with CKD (34.9%, RR 0.62, 95% CI 0.59–0.64) than in patients with normal renal function (56.6%). Thrombolysis was uncommon but was used significantly less often in dialysis patients (1.2%, RR 0.31, 95% CI 0.21–0.44) and patients with CKD (1.3%, RR 0.33, 95% CI 0.28–0.40) than in patients with normal renal function (4.0%).
Figure 1.
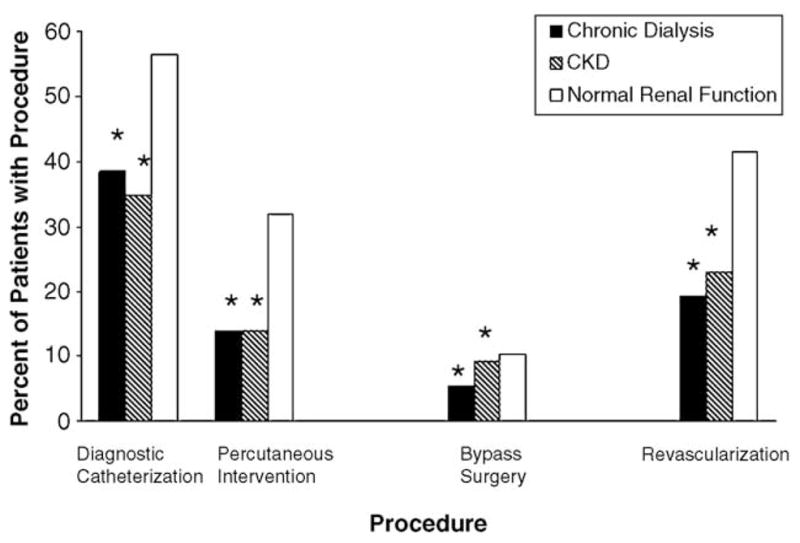
Rates of revascularization. *P < .001 for comparison with normal renal function.
Table II.
Unadjusted procedure rates
| Outcome | No. with outcome (%) | Relative risk* (95% CI) | P |
|---|---|---|---|
| Diagnostic angiography | |||
| Normal renal function | 80822 (56.6) | – | – |
| CKD | 3100 (34.9) | 0.62 (0.59–0.64) | <.0001 |
| Dialysis | 906 (38.6) | 0.68 (0.64–0.73) | <.0001 |
| Revascularization | |||
| Normal renal function | 58886 (41.4) | – | – |
| CKD | 2029 (23.0) | 0.56 (0.53–0.59) | <.0001 |
| Dialysis | 448 (19.2) | 0.46 (0.42–0.52) | <.0001 |
| PCI | |||
| Normal renal function | 45101 (31.7) | – | – |
| CKD | 1230 (13.9) | 0.44 (0.41–0.47) | <.0001 |
| Dialysis | 322 (13.9) | 0.44 (0.38–0.50) | <.0001 |
| CABG | |||
| Normal renal function | 14797 (10.4) | – | – |
| CKD | 822 (9.3) | 0.89 (0.83–0.97) | <.0001 |
| Dialysis | 130 (5.5) | 0.53 (0.44–0.65) | <.0001 |
Relative risk versus normal renal function.
Rates of coronary revascularization after diagnostic angiography
Among patients undergoing in–hospital diagnostic angiography, differences in the use of coronary intervention persisted but were less marked than in the overall population. The rate of either surgical or percutaneous revascularization after angiography was 46.4% (RR 0.66, 95% CI 0.61–0.72) in dialysis patients, 61.6% (RR 0.88, 95% CI 0.86–0.90) in patients with CKD, and 70.1% in patients with normal renal function. Maintenance dialysis patients were significantly less likely than patients with normal renal function to undergo bypass surgery (10.9% vs 15.4%, RR 0.71, 95% CI 0.57–0.88). Conversely, patients with CKD were more likely than patients with normal renal function to undergo bypass surgery after a diagnostic angiography (22.4% vs 15.4%, RR 1.46, 95% CI 1.37–1.55) (Table III).
Table III.
Unadjusted procedure rates after diagnostic angiography
| Outcome | No. with outcome (%) | Relative risk* (95% CI) | P |
|---|---|---|---|
| Revascularization | |||
| Normal renal function | 56482 (70.1) | – | – |
| CKD | 1899 (61.6) | 0.88 (0.86–0.90) | <.0001 |
| Dialysis | 417 (46.4) | 0.66 (0.61–0.72) | <.0001 |
| PCI | |||
| Normal renal function | 45101(56.0) | – | – |
| CKD | 1230 (39.9) | 0.71 (0.68–0.75) | <.0001 |
| Dialysis | 322 (36.0) | 0.64 (0.58–0.72) | <.0001 |
| CABG | |||
| Normal renal function | 12393 (15.4) | – | – |
| CKD | 692 (22.4) | 1.46 (1.37–1.55) | <.0001 |
| Dialysis | 99 (10.9) | 0.71 (0.57–0.88) | .002 |
Relative risk versus normal renal function.
Mortality
Patients on dialysis (13.2%, RR 1.78, 95% CI 1.59–1.98) or CKD (17.7%, RR 2.37, 95% CI 2.26–2.49) were more likely to die during hospitalization for acute MI than subjects with normal renal function (7.4%). Coronary angiography and PCI were associated with decreased risks of inhospital death in all 3 groups. Patients undergoing CABG had a lower incidence of death than patients not treated surgically in both the CKD group (12.0 vs 18.3%) and in the group with normal renal function (4.9 vs 7.7%), but among dialysis patients, there was a nonsignificant increase in the incidence of inhospital death (17.9% vs 12.9%, RR 1.39, 95% CI 0.90–2.13) (Table IV).
Table IV.
Mortality rates stratified by procedure use
| Procedure | No. with inhospital death (%) | Relative risk* (95% CI) | P |
|---|---|---|---|
| Dialysis | |||
| Medical therapy | 269 (14.0) | 1.40 (1.02–1.91) | .023 |
| Revascularization | 45 (10.0) | Reference | – |
| Catheterization | 71 (7.8) | 0.47 (0.36–0.61) | <.0001 |
| No catheterization | 243 (16.6) | Reference | – |
| PCI | 22 (6.7) | 0.47 (0.31–0.71) | <.0001 |
| No PCI | 292 (14.3) | Reference | – |
| CABG | 23 (17.9) | 1.39 (0.90–2.13) | .199 |
| No CABG | 291 (12.9) | Reference | – |
| CKD | |||
| Medical therapy | 1365 (19.7) | 1.83 (1.58–2.12) | <.0001 |
| Revascularization | 216 (10.8) | Reference | – |
| Catheterization | 309 (10.1) | 0.46 (0.41–0.52) | <.0001 |
| No catheterization | 1272 (21.7) | Reference | – |
| PCI | 123 (10.1) | 0.54 (0.45–0.64) | <.0001 |
| No PCI | 1458 (18.9) | Reference | – |
| CABG | 98 (12.0) | 0.66 (0.53–0.82) | .0001 |
| No CABG | 1483 (18.3) | Reference | – |
| Normal renal function | |||
| Medical therapy | 8690 (10.3) | 3.03 (2.81–3.26) | <.0001 |
| Revascularization | 1999 (3.4) | Reference | – |
| Catheterization | 2844 (3.5) | 0.28 (0.26–0.30) | <.0001 |
| No catheterization | 7845 (12.5) | Reference | – |
| PCI | 1346 (3.0) | 0.31 (0.29–0.34) | <.0001 |
| No PCI | 9343 (9.5) | Reference | – |
| CABG | 728 (4.9) | 0.64 (0.59–0.71) | <.0001 |
| No CABG | 9961 (7.7) | Reference | – |
Relative risk versus normal renal function.
Adjusted analysis
Adjustment for demographic conditions and comorbidities slightly increased the rate of angiography in dialysis patients (from 38.6% to 42%, OR vs normal renal function: 0.49, 95% CI 0.43–0.55) and increased it more markedly in patients with CKD (38.6%–45%, OR 0.57, 0.53–0.61). However, the rates in both groups remained significantly lower than in patients with normal renal function (56%) (Tables V–VII). Dialysis patients were markedly less likely than patients with normal renal function to undergo revascularization after diagnostic angiography 52% versus 56% (OR 0.46, 95% CI 0.39–0.54). Differences in the rate of revascularization after angiography were less impressive but remained lower in patients with CKD versus those with normal renal function (66 vs 70%, OR 0.65, 95% CI 0.61–0.68).
Table V.
Adjusted odds of diagnostic angiography
| Covariate | χ2 | OR (95% CI) | P |
|---|---|---|---|
| Renal function | 404.9 | ||
| Dialysis dependent | – | 0.49 (0.43–0.55) | <.0001 |
| CKD | – | 0.57 (0.53–0.61) | <.0001 |
| Normal renal function | – | Reference | – |
| Congestive heart failure | 628.8 | 0.56 (0.53–0.58) | <.0001 |
| Female | 186.6 | 0.81 (0.79–0.84) | .0001 |
| Black race | 18.8 | 0.69 (0.58–0.82) | <.0001 |
| Diabetes | 136.5 | 0.82 (0.80–0.85) | |
| Age | 2029.2 | <.0001 | |
| ≤20 years old | – | 0.53 (0.28–1.00) | .049 |
| 21–40 years old | – | 1.00 (0.93–1.09) | .933 |
| 41–60 years old | – | Reference | |
| 61–80 years old | – | 0.65 (0.62–0.68) | <.0001 |
| ≥80 years old | – | 0.19 (0.18–0.21) | <.0001 |
| Neurologic disorders | 473.2 | 0.41 (0.38–0.44 | <.0001 |
| Pneumonia | 333.0 | 0.55 (0.51–0.59) | <.0001 |
| Diabetes | 136.5 | 0.83 (0.80–0.86) | <.0001 |
Table VII.
Adjusted odds of revascularization after diagnostic angiography
| Covariate | χ2 | OR (95% CI) | P |
|---|---|---|---|
| Renal function | |||
| Dialysis dependent | 108.4 | 0.45 (0.38–0.53) | <.0001 |
| CKD | – | 0.83 (0.78–0.90) | <.0001 |
| Normal renal function | – | Reference | – |
| Congestive heart failure | 241.6 | 0.52 (0.50–0.55) | <.0001 |
| Female | 240.9 | 0.71 (0.69–0.74) | <.0001 |
| Black race | 13.3 | 0.61 (0.51–0.74) | <.0003 |
| Age | 252.1 | 0.85 (0.82–0.88) | <.0001 |
| ≤20 years old | – | 0.01 (0.00–0.08) | <.0001 |
| 21–40 years old | – | 0.66 (0.60–0.72) | <.0001 |
| 41–60 years old | – | Reference | – |
| 61–80 years old | – | 0.81 (0.78–0.85) | <.0001 |
| ≥80 years old | – | 0.66 (0.61–0.70) | <.0001 |
Sensitivity analysis
Results in subjects with lengths of stays >48 hours or ≤7 days were not significantly different than in the overall population. Use of the Charlson index to adjust for comorbidity yielded results qualitatively similar to those in the main analysis (Table VIII).
Table VIII.
Odds ratio of procedure use: sensitivity analysis
| Alternative analysis | Diagnostic angiography, OR (95% CI) | Revascularization, OR (95% CI) | Revascularization after diagnostic angiography, OR (95% CI) |
|---|---|---|---|
| Length of stay >2 d | |||
| Dialysis | 0.45 (0.40–0.51) | 0.30 (0.26–0.35) | 0.36 (0.28–0.48) |
| CKD | 0.57 (0.53–0.62) | 0.59 (0.55–0.63) | 0.69 (0.61–0.78) |
| Length of stay ≤1 wk | |||
| Dialysis | 0.55 (0.48–0.64) | 0.34 (0.28–0.41) | 0.41 (0.34–0.49) |
| CKD | 0.45 (0.42–0.49) | 0.44 (0.41–0.48) | 0.82 (0.75–0.88) |
| Adjusted for Charlson score, sex, and Race | |||
| Dialysis | 0.49 (0.44–0.55) | 0.35 (0.30–0.40) | 0.40 (0.34–0.47) |
| CKD | 0.41 (0.38–0.44) | 0.42 (0.39–0.45) | 0.70 (0.65–0.75) |
Discussion
In this sample of 154692 admissions for acute MI, we found that patients on maintenance dialysis were markedly less likely than patients with dialysis-independent CKD or patients with normal renal function to undergo diagnostic coronary angiography or coronary revascularization, and that these disparities persisted after adjustment for baseline comorbidities and other factors. The low rates of use in patients with dialysis-independent CKD may be appropriately motivated by concerns that exposure to intravenous contrast or bypass surgery will negatively impact residual renal function in these individuals, but no such motivation exists in patients already on maintenance dialysis. Given their nearly 60% first-year mortality rate after acute MI, the even lower rate of application of potentially life-saving coronary interventions in dialysis patients is surprising and merits further study to improve understanding of the underlying causes and prognostic implications of this practice.
Revascularization rates after diagnostic angiography were also markedly lower in dialysis patients than in patients with normal renal function or CKD. Early invasive therapy after MI is associated with substantial reductions in mortality,11–13 and coronary artery bypass surgery markedly reduces mortality, especially in high-risk patients with 3-vessel or left-main disease.17 Dialysis patients referred for angiography after MI represent a highly selected group that would be expected to have a high incidence of significant coronary disease, and studies of dialysis patients suggest that coronary revascularization after MI is associated with markedly improved survival compared with medical therapy alone.18 That the use of diagnostic angiography is low and that CABG and PCI nevertheless take place only 52% of the time after diagnostic angiography suggest that dialysis patients have coronary anatomy that is ill-suited for coronary revascularization, or that physicians prefer to treat post-MI dialysis patients conservatively even when intervention is technically feasible. Studies with comparative angiographic analyses are needed to distinguish between these possibilities.
Dialysis patients and patients with CKD might be less likely to undergo invasive cardiac procedures because of patient or physician concerns that the risks of invasive procedures are excessive, and the likelihood of benefits is low when kidney function is impaired. Alternatively, differences in the type (ST vs non-ST) or severity of MI between patients with normal renal function, CKD, or dialysis dependence might affect the propensity to use medical therapy and invasive diagnostic and therapeutic procedures. ICD-9 diagnostic codes do not distinguish between ST and non-ST MI, and the NIS lacks the data needed to assess for differences in clinical presentation or recognition of MI in long-term dialysis patients. We thus cannot rule out the possibility that an altered clinical presentation of MI in dialysis patients explains the low use of invasive procedures. This issue merits further study, but it should be recognized that diagnostic coronary angiography has been advocated for both ST and non–ST-elevation MI, and even for unstable angina,11–13 and our results demonstrate that guidelines on the treatment of MI are not being applied in the care of dialysis patients.19
In a study that included only dialysis of 44 patients, Wright et al20 found that dialysis patients have lower rates of revascularization than others, and others have found that as few as 12% of dialysis patients are revascularized during or after admission for MI.6,18 Our study extends these observations by demonstrating in a large, contemporary, national sample that dialysis patients are markedly less likely than patients not requiring maintenance dialysis to undergo coronary angiography or revascularization after an MI, and that neither demographic differences nor comorbid disease in the dialysis population completely explains these findings. Because dialysis patients are also 22% to 60% less likely to be prescribed aspirin, β-blockers, or angiotensin-converting enzyme inhibitors during an admission for MI,7 our findings highlight the fact that potentially life-saving therapies are routinely not used in a group of patients at extremely high risk of death after MI. Our results thus raise the possibility that the low use of invasive coronary procedures in dialysis patients may be related to their high rate of death after MI.
Despite the potential benefit from a wider use of early invasive therapy in dialysis patients, it remains uncertain whether the more conservative approaches we found are inappropriate because dialysis patients have been excluded from most randomized trials of peri-MI intervention, and a few retrospective studies have suggested that the benefits of revascularization are attenuated in dialysis patients.21,22 However, other retrospective analyses suggest that CABG and PCI reduce mortality in dialysis patients with MI,18,20,23,24 and in our analysis, medically treated patients had 40% higher risk of in–hospital death than revascularized dialysis patients. Thus, prejudice against the use of early invasive therapy in dialysis patients and the underutilization of these procedures could partly explain the high rates of cardiovascular mortality seen in the dialysis population.
The primary limitation of our analysis is the administrative nature of our source data, which could be susceptible to misclassification of events or diagnoses. Misclassification of MI is an unlikely source of error in our analyses because ICD-9 codes accurately identify subjects with MI,25 and any error introduced by misclassification should apply equally to the dialysis and nondialysis groups. Some patients with acute renal failure may have been misclassified as long-term dialysis patients, but our results were similar when we restricted our analysis to subjects with lengths of stay less than 1 week—which should exclude most of the patients developing dialysis-dependent acute renal failure. Furthermore, we identified 1866 dialysis-dependent admissions in which Medicare was listed as the primary insurance. Under the sampling scheme of the NIS, this is equivalent to approximately 9000 admissions during 2001, a number within 1% of the United States Renal Data System estimate for this period.2,e
Residual confounding could result from underreporting of comorbid conditions.26 We assessed and adjusted for comorbidity using a method designed for use in the NIS15 and validated for the analysis of MI,16 and results were similar when the Charlson comorbidity score was used to adjust for confounding. With up to 15 recorded diagnoses for each admission, the NIS may also be less susceptible to underreporting than other data sets.
Finally, the lack of longitudinal data prevents us from ruling out a higher frequency of post–discharge angiography in dialysis patients. Given dialysis patients’ low rates of diagnostic testing after an MI,6,18 increased testing after discharge is unlikely to attenuate the observed differences Thus, although residual confounding is possible, we believe that this is unlikely to fully explain our findings.
In conclusion, the use of both diagnostic angiography and revascularization after MI is significantly lower in patients on dialysis than in patients not on dialysis, and this difference is not driven by their high rate of comorbid conditions. Cardiovascular disease is the leading cause of death in dialysis patients, and this underutilization of cardiac procedures may partly explain the high mortality rates in this population. Further study of this phenomenon and prospective studies of coronary revascularization in this growing population are sorely needed. In the interim, education on the potential importance of these procedures and removal of barriers to their use should be considered.
Table VI.
Adjusted odds of coronary revascularization
| Covariate | χ2 | OR (95% CI) | P |
|---|---|---|---|
| Renal function | |||
| Dialysis dependent | 468.6 | 0.35 (0.31–0.41) | <.0001 |
| CKD | – | 0.59 (0.56–0.63) | <.0001 |
| Normal renal function | – | Reference | – |
| Congestive heart failure | 598.4 | 0.52 (0.50–0.55) | <.0001 |
| Female | 469.2 | 0.71 (0.69–0.74) | <.0001 |
| Black race | 25.4 | 0.61 (0.51–0.74) | <.0001 |
| Diabetes | 83.2 | 0.85 (0.82–0.88) | <.0001 |
| Age | 2097.0 | ||
| ≤20 years old | – | .01 (0.0–0.1) | <.0001 |
| 21–40 years old | – | 0.77 (0.71–0.83 | <.0001 |
| 41–60 years old | – | Reference | – |
| 61–80 years old | – | 0.70 (0.67–0.73) | <.0001 |
| ≥80 years old | – | 0.24 (0.22–0.25) | <.0001 |
| Neurologic disorders | 265.9 | 0.48 (0.44–0.53) | – |
| Pneumonia | 154.3 | 0.62 (0.57–0.67) | <.0001 |
| Coagulopathy | 90.4 | 1.73 (1.55–1.94) | <.0001 |
| Cancer | 83.2 | 0.76 (0.72–0.81) | <.0001 |
| Drug abuse | 102.9 | 0.45 (0.38–0.52) | <.0001 |
| Admission to teaching hospital | 94.1 | 3.13 (2.44–3.85) | <.0001 |
Acknowledgments
This work was supported by NIH grant T32-DK07199-25 and was presented at the American Society of Nephrology, St. Louis, MO, in October 2004.
We thank Ellen McCarthy, Sidney Atwood, and Shimon Shaykevitch for their assistance.
Footnotes
The data reported here have been supplied by the United States Renal Data System. The interpretation and reporting of these data are the responsibility of the authors and in no way should be seen as an official policy or the interpretation of the US government.
References
- 1.Gilbertson DT, Craig AS, Jay LX, et al. Projecting the U.S. ESRD Population to 2030. J Am Soc Nephrol. 2003;14:F-PO881. [Google Scholar]
- 2.United States Renal Data System. USRDS 2003 Annual data report: atlas of end-stage renal disease in the United States. Bethesda, MD: National Institute of Health; 2003. [Google Scholar]
- 3.Iseki K, Fukiyama K. Long-term prognosis and incidence of acute myocardial infarction in patients on chronic hemodialysis. The Okinawa Dialysis Study Group. Am J Kidney Dis. 2000;36:820–5. doi: 10.1053/ajkd.2000.17676. [DOI] [PubMed] [Google Scholar]
- 4.Sprafka JM, Burke GL, Folsom AR, et al. Trends in prevalence of diabetes mellitus in patients with myocardial infarction and effect of diabetes on survival. The Minnesota Heart Survey. Diabetes Care. 1991;14:537–43. doi: 10.2337/diacare.14.7.537. [DOI] [PubMed] [Google Scholar]
- 5.Herzog CA, Ma JZ, Collins AJ. Poor long-term survival after acute myocardial infarction among patients on long-term dialysis. N Engl J Med. 1998;339:799–805. doi: 10.1056/NEJM199809173391203. [DOI] [PubMed] [Google Scholar]
- 6.United States Renal Data System. USRDS 2001 Annual data report: atlas of end-stage renal disease in the United States. Bethesda MD: National Institute of Health; 2001. [Google Scholar]
- 7.Berger AK, Duval S, Krumholz HM. Aspirin, beta-blocker, and angiotensin-converting enzyme inhibitor therapy in patients with end-stage renal disease and an acute myocardial infarction. J Am Coll Cardiol. 2003;42:201–8. doi: 10.1016/s0735-1097(03)00572-2. [DOI] [PubMed] [Google Scholar]
- 8.Collaboration AT. Collaborative overview of randomised trials of antiplatelet therapy—I: prevention of death, myocardial infarction, and stroke by prolonged antiplatelet therapy in various categories of patients. Antiplatelet Trialists’ Collaboration. BMJ. 1994;308:81–106. [PMC free article] [PubMed] [Google Scholar]
- 9.A randomized trial of propranolol in patients with acute myocardial infarction. I. Mortality results. JAMA. 1982;247:1707–14. doi: 10.1001/jama.1982.03320370021023. [DOI] [PubMed] [Google Scholar]
- 10.Pfeffer MA, Braunwald E, Moye LA, et al. Effect of captopril on mortality and morbidity in patients with left ventricular dysfunction after myocardial infarction. Results of the survival and ventricular enlargement trial. The SAVE Investigators. N Engl J Med. 1992;327:669–77. doi: 10.1056/NEJM199209033271001. [DOI] [PubMed] [Google Scholar]
- 11.Fox KA, Poole-Wilson PA, Henderson RA, et al. Interventional versus conservative treatment for patients with unstable angina or non–ST-elevation myocardial infarction: the British Heart Foundation RITA 3 randomised trial. Randomized Intervention Trial of unstable Angina. Lancet. 2002;360:743–51. doi: 10.1016/s0140-6736(02)09894-x. [DOI] [PubMed] [Google Scholar]
- 12.Wallentin L, Lagerqvist B, Husted S, et al. Outcome at 1 year after an invasive compared with a non-invasive strategy in unstable coronary-artery disease: the FRISC II invasive randomised trial. FRISC II Investigators. Fast revascularisation during instability in coronary artery disease. Lancet. 2000;356:9–16. doi: 10.1016/s0140-6736(00)02427-2. [DOI] [PubMed] [Google Scholar]
- 13.Cannon CP, Weintraub WS, Demopoulos LA, et al. Comparison of early invasive and conservative strategies in patients with unstable coronary syndromes treated with the glycoprotein IIb/IIIa inhibitor tirofiban. N Engl J Med. 2001;344:1879–87. doi: 10.1056/NEJM200106213442501. [DOI] [PubMed] [Google Scholar]
- 14.Winkelmayer WC, Schneeweiss S, Mogun H, et al. Identification of individuals with CKD from Medicare claims data: a validation study. Am J Kidney Dis. 2005;46:225–32. doi: 10.1053/j.ajkd.2005.04.029. [DOI] [PubMed] [Google Scholar]
- 15.Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Southern DA, Quan H, Ghali WA. Comparison of the Elixhauser and Charlson/Deyo methods of comorbidity measurement in administrative data. Med Care. 2004;42:355–60. doi: 10.1097/01.mlr.0000118861.56848.ee. [DOI] [PubMed] [Google Scholar]
- 17.Yusuf S, Zucker D, Peduzzi P, et al. Effect of coronary artery bypass graft surgery on survival: overview of 10-year results from randomised trials by the Coronary Artery Bypass Graft Surgery Trialists Collaboration. Lancet. 1994;344:563–70. doi: 10.1016/s0140-6736(94)91963-1. [DOI] [PubMed] [Google Scholar]
- 18.Chertow GM, Normand SL, Silva LR, et al. Survival after acute myocardial infarction in patients with end-stage renal disease: results from the cooperative cardiovascular project. Am J Kidney Dis. 2000;35:1044–51. doi: 10.1016/s0272-6386(00)70038-2. [DOI] [PubMed] [Google Scholar]
- 19.Braunwald E, Antman EM, Beasley JW, et al. ACC/AHA guidelines for the management of patients with unstable angina and non–ST-segment elevation myocardial infarction. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on the Management of Patients With Unstable Angina) J Am Coll Cardiol. 2000;36:970–1062. doi: 10.1016/s0735-1097(00)00889-5. [DOI] [PubMed] [Google Scholar]
- 20.Wright RS, Reeder GS, Herzog CA, et al. Acute myocardial infarction and renal dysfunction: a high-risk combination. Ann Intern Med. 2002;137:563–70. doi: 10.7326/0003-4819-137-7-200210010-00007. [DOI] [PubMed] [Google Scholar]
- 21.Azar RR, Prpic R, Ho KK, et al. Impact of end-stage renal disease on clinical and angiographic outcomes after coronary stenting. Am J Cardiol. 2000;86:485–9. doi: 10.1016/s0002-9149(00)00998-x. [DOI] [PubMed] [Google Scholar]
- 22.Herzog CA, Ma JZ, Collins AJ. Long-term outcome of dialysis patients in the United States with coronary revascularization procedures. Kidney Int. 1999;56:324–32. doi: 10.1046/j.1523-1755.1999.00540.x. [DOI] [PubMed] [Google Scholar]
- 23.Szczech LA, Reddan DN, Owen WF, et al. Differential survival after coronary revascularization procedures among patients with renal insufficiency. Kidney Int. 2001;60:292–9. doi: 10.1046/j.1523-1755.2001.00799.x. [DOI] [PubMed] [Google Scholar]
- 24.Herzog CA, Ma JZ, Collins AJ. Comparative survival of dialysis patients in the United States after coronary angioplasty, coronary artery stenting, and coronary artery bypass surgery and impact of diabetes. Circulation. 2002;106:2207–11. doi: 10.1161/01.cir.0000035248.71165.eb. [DOI] [PubMed] [Google Scholar]
- 25.Kiyota Y, Schneeweiss S, Glynn RJ, et al. Accuracy of Medicare claims-based diagnosis of acute myocardial infarction: estimating positive predictive value on the basis of review of hospital records. Am Heart J. 2004;148:99–104. doi: 10.1016/j.ahj.2004.02.013. [DOI] [PubMed] [Google Scholar]
- 26.Powell H, Lim LL, Heller RF. Accuracy of administrative data to assess comorbidity in patients with heart disease. An Australian perspective. J Clin Epidemiol. 2001;54:687–93. doi: 10.1016/s0895-4356(00)00364-4. [DOI] [PubMed] [Google Scholar]


