Abstract
Background
Xanthelasma palpebrarum is the most common of the xanthomas with asymptomatic, symmetrical, bilateral, soft, yellow, polygonal papules around the eyelids. Though it is a benign lesion causing no functional disturbance, it is esthetically annoying. The surgical laser offers an extremely elegant and powerful solution to this problem.
Objective
To evaluate the effectiveness of erbium:YAG and argon lasers in the treatment of xanthelasma lesions.
Patients and methods
Forty patients were included in the study. Twenty patients (15 patients were bilateral with 30 eyes either in the upper or lower lid and 5 patients were unilateral) were treated with erbium:YAG laser. Another 20 patients (10 patients were bilateral with 20 eyes and 10 patients were unilateral) were treated with argon laser.
Results
In the majority of treated patients (either treated with erbium:YAG or argon laser), xanthelasma lesions were completely disappeared or significantly decreased in size. Two patients showed pigmentary changes in the form of hypopigmentation with erbium:YAG laser (one case), another case showed hyperpigmentation. No intraoperative complication was observed. No significant scar or recurrence was observed.
Conclusion
Argon laser in xanthelasma is an easy, effective, and safe method of treatment for small lesions and YAG laser is more better for large lesions than argon laser.
Keywords: Xanthelasma, Argon laser, Erbium:YAG laser
Introduction
Xanthelasma is a disfiguring lesion. It appears as yellowish, flat, and soft plaques located most commonly on the medial portion of the eye lid. They may also be present as semisolid or calcareous masses.1 Hyperlipidemia, thyroid dysfunction, and diabetes mellitus are possible pathogenic triggers.2 Xanthelasma has been reported following erythroderma, inflammatory skin disorders, and allergic contact dermatitis in spite of normal lipid profiles.3
The mechanism that initiates macrophages accumulation, cholesterol uptake, and foam-cell formation in a normolipemic patient following an inflammatory skin disorder is not clearly understood. It has been suggested that increased plasma lipid peroxidation (derived from oxidized low-density lipoprotein) may lead to accumulation of cholesterol in macrophages and formation of foam cells.3
Histologically, well defined deposits of doubly refractile cholesterol and other lipids are found in macrophages which develop into foam cells (Touton giant cells). These changes initially are found in the connective tissue around the perivascular spaces in the upper dermis of the eye lids.4
Several different methods can be used to treat xanthelasma palpebrarum, including simple surgical excision which bears a considerable risk of side effects especially an ectropion and scarring,5 cryotherapy,6 chemical peeling with trichloroacetic acid, with risk of irritation and pain,7 and laser treatment. Different types of laser were tried using carbon dioxide laser,8 argon laser,9 KTP laser,2 erbium:YAG laser,10 and pulsed dye laser.11
This study aims to evaluate the effectiveness of argon laser and erbium:YAG laser in the treatment of patients with xanthelasma palpebrarum.
Patients and methods
Forty patients were enrolled from the outpatient clinic of Mansoura Ophthalmic Center from June 2010 to August 2011. The patients were randomly treated. The determination of group for the individual was randomized (dependent on last digit of hospital ID number. If it was an even number the patient was treated with argon laser, if it was an odd number, the patient was treated with YAG laser). Patients were thoroughly informed about technique, postoperative results and possible complications and written consents were taken from all patients. All patients were carried out in accordance with the tenets of the Declaration of Helsinki (1989) of the world medical association. The study was approved by Mansoura University Hospital trust ethics committee.
Patients preparations
Before laser application, margin of the skin lesion was outlined with a black pen and local infiltration anesthesia by lidocaine HCl 2% was injected under the lesion.
Settings of laser
Argon laser
Slit lamp mounted argon laser was used with the following parameters, spot size 1000 μm, pulse duration 0.8–0.9 s, and energy varied from 600 to 800 mw. Patient instructed to close his eyes during laser application. Argon laser was used in continuous mode.
Coagulation of the lesion margin is started first, then toward the center. During laser application, subcutaneous tissues start to shrink. At the end of treatment, xanthelasma lesion looks smaller.
Erbium:YAG laser
Twenty patients (30 eyes) were treated with erbium:YAG laser. For smaller lesions, spots were used with diameter of 1.6 mm, energy of 300 mJ, frequency 1 Hz and number varying in relation to the extent of the pathology. When the area to be treated was more extensive, the frequency increased to 5 Hz while the diameter and energy remained the same. After having bordered off the xanthelasma with a row of spots, application was continued in a centripetal direction until the lesion was covered throughout.
Post treatment
Post treatment therapy was antibiotic-steroid ophthalmic ointment twice daily for 2 weeks. During this period, the crust which had formed falled within 7–14 days and newly formed layer of skin is seen.
Photographic documentation of the lesion before laser treatment and immediately afterward and at each of the successive checkup visits was carried out. Follow up period was 6 months. According to size and density of the lesion, one or more laser sessions were required. The results rating from good to excellent (excellent means the skin of the lesion returned normal as the rest of the surrounding skin, very good means the skin of the lesion returned nearly normal as the rest of the surrounding skin, good means the skin of the lesion had acceptable color.
Results
The study included 40 patients (65 eyes): 25 patients were bilateral with 50 eyes either in the upper or lower lid and 15 patients were unilateral, so, a total of 65 eyes. Twenty patients (35 eyes) were treated with argon laser (group 1) and 20 patients (30 eyes) were treated with Erbium:YAG laser (group 2). The sex, age, and lesion characteristic were included in Tables 1 and 2.
Table 1.
Demographic features among groups.
| Age | Group 1 |
Group 2 |
||||||
|---|---|---|---|---|---|---|---|---|
| Female |
Male |
Female |
Male |
|||||
| No | % | No | % | No | % | No | % | |
| 30–40 | 2 | 10 | – | – | 2 | 10 | – | – |
| 41–50 | 5 | 25 | 4 | 20 | 6 | 30 | 4 | 20 |
| 51–60 | 4 | 20 | 5 | 25 | 4 | 20 | 4 | 20 |
| Total | 11 | 55 | 9 | 45 | 12 | 60 | 8 | 40 |
Table 2.
Xanthelasma characters among groups.
| Lesion character tics |
Group 1 | Group 2 | |
|---|---|---|---|
| Size | Texture | Number | Number |
| <lcm2 | & soft, flat | 15 | 12 |
| <lcm2 | & elevated, semisolid | 6 | 7 |
| >lcm | & soft, flat | 15 | 6 |
| >lcm | & elevated, semisolid | 4 | 5 |
| Total | 40 | 30 lesion | |
| in 35 eyes | in 30 eyes | ||
| in 20 patients | In 20 patients | ||
During xanthelasma ablation either with argon or YAG laser, there was no pain or bleeding in all patients and laser treatment was well tolerated.
All lesions respond to laser, by formation of crust in xanthelasma followed by disappearance of xanthelasma or decrease in size. During this period, no complaint was noticed. No signs of inflammatory reaction or infection was noticed in all cases. The newly formed layer, originally was more pink in color and assumed a coloring homogenous with the surrounding tissue within 4–5 weeks.
Most of the patients got satisfactory cosmetic appearance with the results rating from good to excellent (Figs. 1-5 and Table 3).
Figure 1.
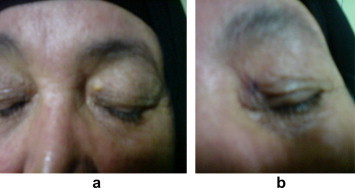
Effect of Argon laser treatment. a: Xanthelasma of left eye before treatment, b: after 1 week of argon laser therapy (with transient hyperpigmentation).
Figure 2.
Effect of Argon laser treatment. a: Xanthelasma of left eye before treatment, b: (moderate clearance after 2nd session).
Figure 3.

Effect of Argon laser treatment. a: Xanthelasma of the right lower eyelid before treatment. b: One month after argon laser therapy with excellent clearance of the lesion.
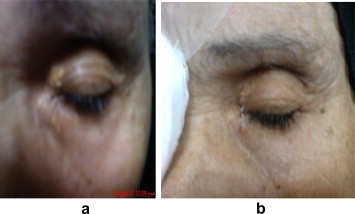
Figure 4.

Shows effect of YAG laser treatment. a: Xanthelasma of left eye before treatment. b: Transient hypopigmentation after one week of erbium:YAG laser.
Figure 5.

Erbium:YAG laser. a: Xanthelasma of left eye before treatment. b: After one month of one session of treatment with erbium:YAG laser (with excellent clearance).
Table 3.
Details of the results in the study.
| Results | Group 1 |
Group 2 |
||
|---|---|---|---|---|
| Number of eyes | % | Number of eyes | % | |
| Excellent (normal) | 25 | 71.4 | 20 | 66.7 |
| Very good (nearly normal) | 7 | 20 | 5 | 16.7 |
| Good (acceptable) | 2 | 5.7 | 1 | 3.3 |
| Satisfactory (hardly seen scar) | 1 | 2.8 | 2 | 6.6 |
| Pigmentation | – | 2 | 6.6 | |
| Recurrence | – | – | ||
| Disfiguring scar | – | – | ||
| Total | 35 | 30 | ||
Discussion
Treatment of xanthelasma is usually regarded as a cosmetic procedure. Methods for xanthelasma removal should have only minimal side effects. Surgical excision is often followed by slight scarring, no matter if wound closure is achieved through primary closure, full thickness skin grafting,12,13 or granulation.5
Postoperative healing may be further complicated by infections and poor wound healing as well as ectropion. Extensive xanthelasmas that inflict the whole periorbital space are not treatable surgically. Alternative to this treatment is cauterization with trichloracetic acid, liquid nitrogen or organic and non organic acids.14
However, all of these methods with risks of side effects including persistent erythema, infection, depigmentation and scarring. The therapeutic effect of chemical measures is often unsatisfactory. The depth of tissue penetration by the chemicals is hardly controllable and risk of ocular damage.15
Xanthelasmas are an ideal target for laser therapy because of its superficial location. It is presumed that the caloric energy that originates from coagulation of the vessels within the upper corium leads to damage of perivascular foam cells in the lesion. The coagulation of the pathologically hyperpermeable vessels would lead to block of the leakage of lipids into the tissue and thereby prevents recurrence. The precise photoablation and coagulation of the skin strata allow a gentle and bloodless ablation of the lesions.16
There are different types of laser that can be used for treatment of xanthelasma. Raulin and his co-workers reported series of 52 periorbital xanthelasma treated with ultra-pulsed carbon dioxide laser, all lesions were removed completely with a single laser treatment. As regard for side effects, only transient pigment changes (4% hyperpigmentation, and 13% hypopigmentation) with no visible scarring was observed. Three patients (13%) developed a recurrence of xanthelasma.17
Also, Saif MYS treated 25 patients with carbon dioxide with promising results. Most of patients got satisfactory cosmetic appearance. In 5 lids some pigmentary (5.7%) changes and 8 (9.1%) lids had recurrence.18
Berger and Kopera employed KTP laser (532 nm) for first time with 85.7% of cases showed respectable reduction in xanthelasma after 1–3 KTP laser sessions without side effects, also 70% of their patients tolerated treatment without any analgesia 2. The use of dye laser (585 nm) was described by Gosepath and Mann who divided treatment in 4–5 successive sessions, high patient acceptance with absence of complication was reported.19
Another type of laser for treating skin lesions is erbium:YAG. Despite it is being of the pulsed type, studies have shown that it causes continuous ablation that starts with a slight delay in relation to the pulsation and lasts until the latter ends. The first studies on its ablation effect on the skin showed a linear increase in the rate of ablation with a radiation exposure threshold of 1 J/cm2 and slop efficiency of 6.7 Mm/J/cm2.20
Erbium:YAG laser which was used in this study, is an instrument that allows surface ablation of skin with minimum heat effect, only operative inside the skin without involving the melanocytes and blood vessels. It is characterized by a wave length 2.94 μm that corresponds to maximum absorption of water. Since approximately 77% of skin consists of water, this absorption was the optimal condition for the ablation effect. When the energy administered reaches the ablation threshold, the water vaporizes at ultrasonic speed, removing the tissue with the sound phenomenon of a sharp bang.10
Borelli and Kaudewitz treated 33 xanthelasma lesions with erbium:YAG laser with promising results as all lesions were removed without hyperpigmentation or scarring.10 Also, Mannino and colleagues reported good esthetic results in 30 female patients, 70 xanthelasmas treated with erbium:YAG laser without leaving scars and/or dyschromia.21
Kaufman and Hibst treated 9 xanthelasmas in 4 patients with erbium:YAG laser using spots with a diameter 2 mm and energy of 315 mJ. Only in 2 particularly extensive patients, atrophic scars remained after 4 months.22
Drnovsek-Olup and Vedlin reported that in 32 xanthelasmas of 8 patients treated with erbium:YAG laser and with average follow up of 3 months, an optimum results was achieved in 100% of patients. For all the lesions, one single session of treatment was sufficient.23
In our study, 30 xanthelasma lesions in 30 eyes in 20 patients were treated with erbium:YAG laser. Only 2 patients developed hypopigmentation. All patients were needed only one session. The treatment is well tolerated by patients. The procedure was done in sitting or lying position.
By using slit lamp mounted argon laser, Hintschich reported that in 32 xanthelasma lesions treated with green argon, good and very good cosmetic results was achieved in 80% of cases. There were no intra or postoperative complication or functional scars. Recurrence occurred in 14 out of 25 lids after 12–16 month of follow up.16
Ruban and colleagues treated 25 patients with 101 xanthelasma by slit lamp blue-green argon laser. Cosmetic results was good in 83% of cases without either scarring or dyschromia and in 13.3% of patients, there was minimal scarring/slight dyschromia while in 3.3% of patients there was visible scarring/marked dyschromia.24
Basar and co-workers reported 85% good, 10% fair and 5% poor cosmetic results in 40 eyes with xanthelasma treated with argon laser.25
In this study, 40 xanthelasma lesions, 35 eyes in 20 patients were treated with argon laser. 71.4% had excellent results, 20% very good, 5.7% good, 2.8% had satisfactory results. Small lesion <1 cm2 had excellent results in all cases regardless of its firmness. Large lesions needed more than one session with 2 weeks apart.
Hintschich showed that effectiveness of argon laser in xanthelasma is due to its thermal effect when laser energy absorbed with skin chromospheres, it is converted into heat and by using sublesional probe to measure the temperature it was elevated to 50–60° which alter the foam cells in xanthelasma and coagulated blood vessel.26 Sampath et al. showed that histological changes of xanthelasma after argon laser are consistent with a superficial photocoagulation of the upper skin levels to a depth of 1 mm dermis preserving dermal appendages and aiding in the rapid healing of the wound without scar.27
Major disadvantage of argon laser photocoagulation as reported in literature was significant recurrence rate. One study has reported that 14 recurrences out of 32 treated lesions were within the first 12–16 months after argon laser.26 Baser and coworkers were also reported that 6 out of 40 treated with argon laser were recurred after one year of treatment.25
Most of recurrences were found to be developed from the margin of xanthelasma, so margin of xanthelasma should be treated well. In this study, there was no recurrence which may be due to relatively short follow up period (6 months).
In summary, laser represents a valid alternative to the more traditional methods of treating xanthelasma because of the simplicity and speed of performance, minimal postoperative treatment and the positive functional and esthetic results.
Conflict of interest
The authors declared that there is no conflict of interest.
Appendix A. Supplementary data
References
- 1.Howard G.R. Xanthelasma. In: Roy F.H., editor. Master Techniques in Ophthalmic Surgery. Williams and Wilkins; Baltimore: 1995. p. 520. [Google Scholar]
- 2.Berger C., Kopera D. KTP laser coagulation for xanthelasma palpebrarum. J Dtsch Dermatol Ges. 2005;3:775–779. doi: 10.1111/j.1610-0387.2005.05746.x. [DOI] [PubMed] [Google Scholar]
- 3.Akhyani M., Daneshpazhooh M., Jafari A.K., Naraghi Z.S., Farahami F. Koebner phenomenon in xanthelasma after treatment with trichloroacetic acid. Dermatol Line J. 2006;12(2):12. [PubMed] [Google Scholar]
- 4.Braun-falco O., Plewig G., Wolff H.H., Burgdorf W.H.C. 2nd ed. Springer-Verlag; Berlin Heidelberg New York: 2000. Dermatology. pp. 1245–49. [Google Scholar]
- 5.Eedy D.J. Treatment of xanthelasma by excision with secondary intention healing. Clin Exp Dermatol. 1996;21:273–275. doi: 10.1111/j.1365-2230.1996.tb00092.x. [DOI] [PubMed] [Google Scholar]
- 6.Dowber R., Clover G., Jackaneous A. Martin Dunitz Ltd; London: 1992. Benign Lesions. Cutaneous Cryo Surgery. Principles and Clinical Practice. p. 53. [Google Scholar]
- 7.Fine F.D., Brooke P., Moschella S.L. Diseases of nutrition & metabolism. In: Orkin M., Maibach H.I., editors. Dahi MV. Appleton & Lange; Dermatology East Norwalk: 1991. pp. 374–392. [Google Scholar]
- 8.Ullmann Y., Har-Shai Y., Peled I.J. The use of CO2 laser for the treatment of xanthelasma palpebrarum. Ann Plast Surg. 1993;31:504–527. doi: 10.1097/00000637-199312000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Drosner M., Vogt H.J. Xanthelasma palpebrarum: argon laser therapy. Z Hautkr. 1992;67:144–147. [Google Scholar]
- 10.Borelli C., Kaudewitz P. Xanthelasma palpebrarum treatment with the erbium–YAG laser. Laser Surg Med. 2001;29:260. doi: 10.1002/lsm.1117. [DOI] [PubMed] [Google Scholar]
- 11.Schoenermark M.P., Raulin C. Treatment of xanthelasma palpebrarum with the pulsed dye laser. Lasers Surg Med. 1996;19:336–339. doi: 10.1002/(SICI)1096-9101(1996)19:3<336::AID-LSM9>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- 12.Parkes M.L., Waller T.S. Xanthelasma palpebrarum ectropion. Laryngoscope. 1994;1984:1238–1240. doi: 10.1288/00005537-198409000-00019. [DOI] [PubMed] [Google Scholar]
- 13.Rose E.H., Vistnes L.M. Unilateral invasive xanthelasma palpebrarum. Ophthal Plast Reconstr Surg. 1987;3:91–94. doi: 10.1097/00002341-198703020-00007. [DOI] [PubMed] [Google Scholar]
- 14.Stegman S.J., Tromovitch T.A. Cosmetic dermatologic Surgery. Arch Dermatol. 1982;118:1013–1016. [PubMed] [Google Scholar]
- 15.Ronnen M., Suster S., Huszar M., Gilad E. Treatment of xanthelasma with Solcoderm. J Am Acad Dermatol. 1989;21:807–809. doi: 10.1016/s0190-9622(89)80280-4. [DOI] [PubMed] [Google Scholar]
- 16.Hintschich C. Argon laser coagulation of xanthelasmas. Opthalmologe. 1995;92:885–891. [PubMed] [Google Scholar]
- 17.Raulin C., Schoenermark M.P., Werner S. Xanthelasma palpebrarum treatment with ultrapulsed CO2 laser. Lasers Surg Med. 1994;24:122–127. doi: 10.1002/(sici)1096-9101(1999)24:2<122::aid-lsm7>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 18.Saif M.Y.S. Xanthelasma palpebrarum treatment by CO2 laser. Bull Ophthalmol Soc Egypt. 2007;100:791–794. [Google Scholar]
- 19.Gosepath K., Mann W. Der gepulste farbstoff laser zur behind lung gutartiger oberflachnnahr gefa BmiBbildurger. Laryngo-Rhino-Otol. 1995;74:500–503. doi: 10.1055/s-2007-997788. [DOI] [PubMed] [Google Scholar]
- 20.Chernoff G., Slatkine M., Zair E. Silk touch: a new technology for skin resurfacing in anesthetic surgery. Lasers Surg Ned. 1995;13:97–100. doi: 10.1089/clm.1995.13.97. [DOI] [PubMed] [Google Scholar]
- 21.Mannino G., Papale A., De Bella F., Mollo R. Use of Erbium:YAG laser in the treatment of palpepral xanthelasmas. Opthalmic Surg Lasers. 2001;32:129–133. [PubMed] [Google Scholar]
- 22.Kaufmann R., Hibst R. Pulsed Erbium.YAG laser ablation in cutaneous surgery. Lasers Surg Med. 1996;19:324–330. doi: 10.1002/(SICI)1096-9101(1996)19:3<324::AID-LSM7>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 23.Drnovsek-Olup B., Vedlin B. Use of Erbium:YAG laser for benign skin disorders. Lasers Surg Ned. 1997;21:13–19. doi: 10.1002/(sici)1096-9101(1997)21:1<13::aid-lsm3>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 24.Ruban J.M., Vasselon J., Burillon C. Treatment des xanthelasma par le laser argon. Ophthalmologie. 1996;10:442–446. [Google Scholar]
- 25.Basar E., Oguz H., Ozdemir H. Treatment of xanthelasma palpebrarum with argon laser photocoagulation. Int Ophthalmol. 2004;25:9–11. doi: 10.1023/b:inte.0000018523.55861.6c. [DOI] [PubMed] [Google Scholar]
- 26.Hintschich C. Treatment of xanthelasma palpebrarum by argon laser coagulation. Orbit. 1995;14:123–129. [Google Scholar]
- 27.Sampath R., Parmar D., Cree I.A., Collin J.R. Histology of xanthelasma lesion treated by argon laser photocoagulation. Eye. 1998;12:479–480. doi: 10.1038/eye.1998.110. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


