Abstract
The aim of this study is to report clinical and imaging findings, and treatment outcomes of a patient with nodular posterior scleritis. A 41-year-old woman was diagnosed as nodular posterior scleritis in the light of clinical and imaging findings. At first admission best corrected visual acuity was 20/50 in her right eye. Fundus examination revealed an amelanotic subretinal mass under the superior temporal arcade associated with subretinal fluid surrounding it. B-scan ultrasonography, optical coherence tomography, fluorescein angiography, and indocyanine green angiography findings confirmed the diagnosis. As treatment, nepafenac eye drops 3 times a day, and flurbiprofen tablet 100 mg twice a day were prescribed. After 4 weeks of treatment, the ocular pain was relieved, BCVA improved to 20/20, and subretinal mass totally regressed. Although the diagnosis of nodular posterior scleritis may be confusing, it has to be kept in mind in patients with a subretinal/choroidal mass. Multimodal fundus imaging may be helpful in differential diagnosis. The condition is usually curable with non-steroidal anti-inflammatory drugs and/or systemic steroids.
Keywords: Scleritis, Choroidal mass, Subretinal fluid
Introduction
Posterior scleritis is a rare and potentially blinding condition which is usually misdiagnosed due to its varied presentation and low incidence.1,2 The inflammation may affect the whole sclera (diffuse posterior scleritis) or only a part of it (nodular posterior scleritis).1–4 Nodular posterior scleritis is more complex than the diffuse form, because it usually simulates a choroidal mass which may lead the physician to misdiagnosis and unwarranted surgeries.3–6 In this case report we aimed to present a patient with nodular posterior scleritis mimicking a choroidal mass, and who was treated successfully with topical and systemic non-steroidal anti-inflammatory drugs.
Case report
A 41-year-old woman admitted with a complaint of visual loss associated with ocular pain since 3 days in the right eye. Systemic evaluation was not notable. Her family history was not significant. On ocular examination, best corrected visual acuity (BCVA) was 20/50 in the right eye and 20/20 in the left eye. Slit lamp examination of the anterior segment did not show any abnormality. Intraocular pressure was within normal limits in both eyes. Fundus examination revealed an amelanotic subretinal mass under the superior temporal arcade associated with subretinal fluid surrounding it in the right eye (Fig. 1a). B-scan ultrasonography showed a hyperechoic dome-shaped mass (Fig. 2). Optical coherence tomography (OCT) revealed elevated retina with a normal choroidal tissue beneath it. There was subretinal fluid surrounding the retinal elevation (Fig. 3a). Although OCT did not show choroidal mass, fluorescein angiography (FA) was performed to rule out dual circulation which is a classical finding of choroidal melanomas. FA did not show dual circulation; however it revealed pooling type hyperfluorescence around the lesion (Fig. 4a). Indocyanine green angiography, showed an intense hypofluorescence surrounded by a mild hypofluorescence (Fig. 4b). The central intense hypofluorescence was thought to be due to retinal edema, the surrounding mild hypofluorescence was due to subretinal fluid. Based on ocular findings and history, the patient was diagnosed as nodular posterior scleritis. However, the patient had a history of breast cyst. Therefore, she was referred to an internal medicine specialist to rule out a systemic malignancy. The laboratory evaluation, tumor markers, and systemic imaging were within normal limits, and the breast cyst was diagnosed as a benign breast cyst.
Figure 1.
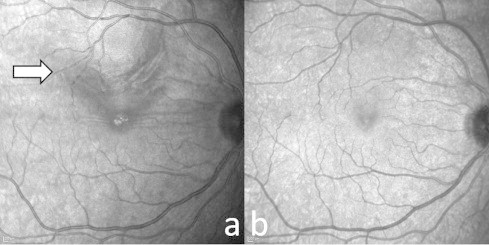
(a) Infrared imaging of the subretinal mass (white arrow) under the superior vascular arcade. (b) Infrared imaging after 4 weeks of treatment shows complete regression of the subretinal mass.
Figure 2.
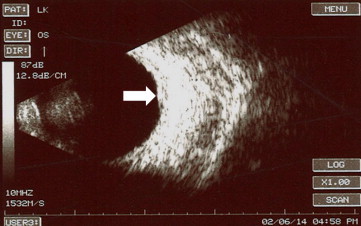
B-scan ultrasonography image shows a hyperechoic dome-shaped mass (white arrow) in the posterior wall of the eye.
Figure 3.
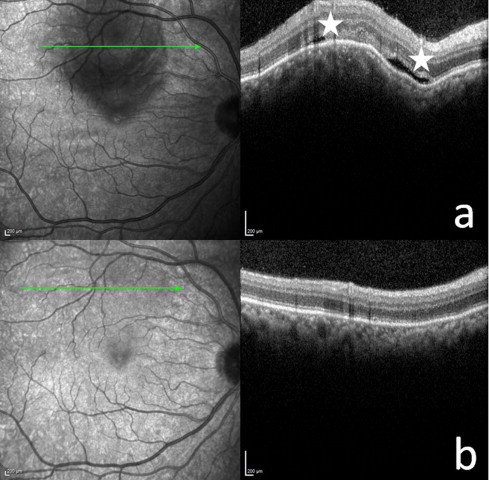
(a)Optical coherence tomography scan demonstrates an elevated retina with normal retinal layers, subretinal fluid (white stars), and normal choroidal tissue. (b) Optical coherence tomography after 4 weeks of treatment shows complete regression of retinal elevating, and resolution of subretinal fluid.
Figure 4.
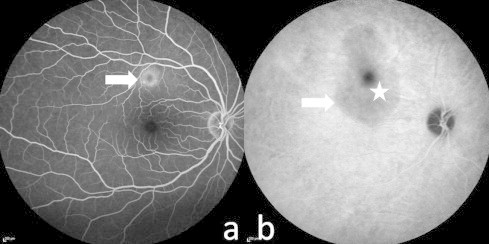
(a) Fluorescein angiography shows pooling type hyperfluorescence (white arrow). (b) Indocyanine green angiography shows an intense hypofluorescence (white star) surrounded by a mild hypofluorescence (white arrow).
As treatment, nepafenac eye drops 3 times a day, and flurbiprofen tablet 100 mg twice a day was prescribed. After 4 weeks of treatment, the ocular pain was relieved; BCVA improved to 20/20, subretinal mass totally regressed (Fig. 1b) and subretinal fluid was decreased in the right eye (Fig. 3b).
Discussion
Nodular posterior scleritis is a very rare disease. In the literature, it has been reported only as case reports.3–6
Clinically, ocular pain is the main symptom that may alert the physician for the diagnosis of an inflammatory disease. Hage et al., Perez-Campagne et al., Shukla and Kim also reported the association of ocular pain with nodular posterior scleritis.7
Ocular examination of posterior nodular scleritis may reveal conjunctival injection, anterior uveitis, anterior scleritis, subretinal mass, subretinal fluid, choroidal/retinal folds, and exudative retinal detachment.4–7 However, fundus examination alone is not capable of ruling out an inflammatory lesion from a malign lesion. Various imaging methods are required for differential diagnosis. B-scan ultrasonography is defined as the key diagnosis by Hage et al.6 They mentioned that, B-scan ultrasonography may show nodular thickening of the sclera associated and diffuse hyperechogenicity without orbital shadowing, unlike choroidal tumors or metastasis which is characterized by a moderate hyperechogenicity or a hypoechogenicity.6 In our case B-scan ultrasonography also showed similar findings. Fluorescein angiography is also an important method, and presence of dual circulation is a classical finding for choroidal melanomas.5 In previous reports, optical coherence tomography findings were described by several authors.5,6 Optical coherence tomography may show subretinal mass, subretinal fluid, and retinal/choroidal folds in patients with posterior scleritis. In our opinion OCT is also a very important diagnostic tool for nodular posterior scleritis, especially when the subretinal mass is not very large. In our case, OCT scans showed that choroidal tissue was normal and the vascular network of choroid was in normal configuration. Therefore, we easily ruled out a choroidal mass. Indocyanine green angiography (ICGA), computerized tomography (CT), and magnetic resonance imaging (MRI) findings of posterior scleritis were also described in previous reports.5–7 Arevalo et al., reported that ICGA only revealed choroidal folds which did not aid the diagnosis. CT and especially MRI may show scleral thickening and rule out choroidal masses.8
Our patient was successfully treated with topical and systemic non-steroidal anti-inflammatory drugs. In the literature, the use of non-steroidal drugs, oral or intravenous systemic steroids were reported as successful treatment options.
Conclusion
The diagnosis of nodular posterior scleritis has to be kept in mind in patients with a subretinal/choroidal mass. Multimodal fundus imaging may be helpful in differential diagnosis. The condition is usually curable with non-steroidal anti-inflammatory drugs and/or systemic steroids.
Conflict of interest
The authors declared that there is no conflict of interest.
Footnotes
Peer review under responsibility of Saudi Ophthalmological Society, King Saud University.
Contributor Information
Abdullah Ozkaya, Email: abdozkaya@gmail.com.
Cengiz Alagoz, Email: alagozcengiz@gmail.com.
Alperen Koc, Email: dr.alperen.koc@gmail.com.
Hande Mefkure Ozkaya, Email: hndebektas@gmail.com.
Ahmet Taylan Yazıcı, Email: ahmettaylan19@gmail.com.
References
- 1.Benson W.E. Posterior scleritis. Surv Ophthalmol. 1988;32:297–316. doi: 10.1016/0039-6257(88)90093-8. [DOI] [PubMed] [Google Scholar]
- 2.McCluskey P.J., Watson P.G., Lightman S., Haybittle J., Restori M., Branley M. Posterior scleritis: clinical features, systemic associations, and outcome in a large series of patients. Ophthalmology. 1999;106:2380–2386. doi: 10.1016/S0161-6420(99)90543-2. [DOI] [PubMed] [Google Scholar]
- 3.Finger P.T., Perry H.D., Packer S., Erdey R.A., Weisman G.D., Sibony P.A. Posterior scleritis as an intraocular tumour. Br J Ophthalmol. 1990;74:121–122. doi: 10.1136/bjo.74.2.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Demirci H., Shields C.L., Honavar S.G., Shields J.A., Bardenstein D.S. Long-term follow-up of giant nodular posterior scleritis simulating choroidal melanoma. Arch Ophthalmol. 2000;118:1290–1292. doi: 10.1001/archopht.118.9.1290. [DOI] [PubMed] [Google Scholar]
- 5.Pérez-Campagne E., Guex-Crosier Y., Schalenbourg A., Uffer S., Zografos L. Giant nodular posterior scleritis compatible with ocular sarcoidosis simulating choroidal melanoma. Arch Soc Esp Oftalmol. 2007;82:563–566. doi: 10.4321/s0365-66912007000900010. [Article in Spanish] [DOI] [PubMed] [Google Scholar]
- 6.Hage R., Jean-Charles A., Guyomarch J., Rahimian O., Donnio A., Merle H. Nodular posterior scleritis mimicking choroidal metastasis: a report of two cases. Clin Ophthalmol. 2011;5:877–880. doi: 10.2147/OPTH.S21255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shukla D., Kim R. Giant nodular posterior scleritis simulating choroidal melanoma. Indian J Ophthalmol. 2006;54:120–122. doi: 10.4103/0301-4738.25835. [DOI] [PubMed] [Google Scholar]
- 8.Arevalo J.F., Shields C.L., Shields J.A. Giant nodular posterior scleritis simulating choroidal melanoma and birdshot retinochoroidopathy. Ophthal Surg Las Imag. 2003;34:403–405. [PubMed] [Google Scholar]


