Abstract
Medicinal lasers are a standard source of light to produce retinal tissue photocoagulation to treat retinovascular disease. The Diabetic Retinopathy Study and the Early Treatment Diabetic Retinopathy Study were large randomized clinical trials that have shown beneficial effect of retinal laser photocoagulation in diabetic retinopathy and have dictated the standard of care for decades. However, current treatment protocols undergo modifications. Types of lasers used in treatment of retinal diseases include argon, diode, dye and multicolor lasers, micropulse lasers and lasers for photodynamic therapy. Delivery systems include contact lens slit-lamp laser delivery, indirect ophthalmocope based laser photocoagulation and camera based navigated retinal photocoagulation with retinal eye-tracking. Selective targeted photocoagulation could be a future alternative to panretinal photocoagulation.
Keywords: Retinal Laser, Photocoagulation, Therapy, Pattern laser, Micropulse laser, Navigated laser
A brief history of retinal photocoagulation
Past laser photocoagulation concepts
Photocoagulation uses light to coagulate tissue. Medicinal lasers have become a source of light to produce tissue coagulation. The effect of laser interaction with retinal tissue had been studied earlier but it was not until Meyer-Schwickerath’s report in 1954 that beneficial therapeutic effects of laser photic burns were recognized.1 With Hans Littmann of Zeiss Laboratories they assembled the first xenon-arc photocoagulator in 1956.2 The system was effective but it was difficult to focus beam to a small spot, treatments required long exposures and were often painful. Theodore Maiman, PhD, designed the first ophthalmic laser in 1960 at the Hughes Research Laboratories emitting monochromatic energy. Systems using ruby laser (694-nm wavelength) were among the first to be studied in ophthalmology.3,4 They offered some variability in pulse durations and more precisely targeted treatments. They could be successfully applied therapeutically but intense chorioretinal destruction and frequent hemorrhaging soon showed to be an issue. The advent of argon laser marked a new milestone in retinal photocoagulation.5,6
Argon laser can use the blue (488-nm wavelength) and green (514-nm wavelength) light emission absorbed by both hemoglobin and melanin. The Diabetic Retinopathy Study7 and the Early Treatment Diabetic Retinopathy Study8 were large randomized clinical trials that have shown beneficial effect of retinal laser photocoagulation in diabetic retinopathy and have dictated the standard of care for decades. In DRS, argon laser had equal efficacy to xenon arc laser but in general produced less adverse effects. Later on water-cooled argon lasers have been replaced by air-cooled Nd:YAG frequency doubled lasers (532-nm wavelength). Other conditions, including age-related macular degeneration and retinal vein occlusion, were found to benefit from laser retinal photocoagulation, widening treatment indications.9
Introduction of dye lasers represented a further development. The design of a dye laser is similar to a pulsed solid-state laser with the laser crystal replaced by a dye cell.10,11 Dye lasers can usually be used for a much wider range of wavelengths. The introduction of solid state lasers has offered an advantage of being less expensive and portable.
Past laser delivery systems
Mode of delivery is an important aspect of laser photocoagulation. While the ruby laser was attached to a monocular direct ophthalmoscope, subsequent generations of lasers could be attached to indirect ophthalmoscope, operating microscope or slit lamp. Endolaser photocoagulation (applied via a fiberoptic probe placed inside the eye) has shortened treatment times and improved results of vitreoretinal surgery. Coupling lasers with slit lamp improved laser delivery to the retina, especially for posterior pole application in the clinic.12
Modern laser technology developments and applications
Current laser photocoagulation concepts and techniques
The above-mentioned clinical trials and subsequent clinical experience by physicians established retinal photocoagulation as the standard treatment of choice for complications of diabetic retinopathy for over 40 years. Although clinically effective, retinal laser photocoagulation leads to collateral damage and side effects including reduced night vision, macular and peripheral scotomata with decrease in central and peripheral vision, exacerbation of macular edema and disruption of the retinal anatomy through scarring.13–16
In search for ways to spare retinal tissue yet achieving desired therapeutic benefit, the first attempts were aimed at titration of laser power to reduce tissue damage. Diode lasers (810-nm wavelength) were used to produce “classically” subthreshold (ophthalmoscopically less visible) burns in diabetic macular edema (DME)17 and age-related macular degeneration (AMD).18,19
In 1990 Pankratov developed the micropulsed diode laser. Producing a train of millisecond laser pulses separated by variable quiet intervals, micropulsing allowed selective treatment of the retinal pigment epithelium (RPE) and sparing of the neurosensory retina.20,21 Early use of micropulsed lasers reduced but did not eliminate thermal retinal damage due to use of high treatment powers and / or micropulse duty cycles, as well as the continuing belief in the need to produce at least some laser-induced thermal retinal injury to achieve a therapeutic effect. This long-held maxim was called into question by the later finding that use of particular micropulsed laser parameters (high-density/low-intensity “true” Subthreshold Diode Micropulse laser, or “SDM”) is clinically effective without any laser-induced retina injury detectable by any currently available retinal imaging modality, or known adverse treatment effects. Non-destructive and thus non-inflammatory, SDM has been reported effective for a number of disorders and uniquely allows safe transfoveal treatment in eyes with good visual acuity.19,22,23 SDM has also been uniquely shown to increase, rather than decrease, retinal sensitivity by microperimetry at the locus of laser application.24
In 1992 Reginald Birngruber and colleagues introduced application of even shorter microsecond continuous-wave laser pulses. These microsecond laser pulses also selectively target the retinal pigment epithelium (RPE) sparing the photoreceptors and other intraretinal cells.25,26 Such short-pulse continuous wave laser cause explosive vaporization of melanosomes and formation of cavitation bubbles resulting in cell death and subsequent proliferation and migration of RPE cells to restore the integrity of the defective RPE layer.25 The clinical term adopted for this approach has been “Selective Retina Therapy” or SRT.26
Another concept to use laser therapy with minimal collateral damage is transpupillary thermotherapy (TTT) using near-infrared (810-nm wavelength) laser, low irradiance and long exposure (1 min), and large retinal treatment spots. TTT continues to be used in the treatment of small choroidal melanomas, nowadays in combination with other modalities such as brachytherapy.27,28 However, former use for neovascular AMD and other macular disorders has been abandoned due to higher efficacy of intravitreal anti-angiogenic therapy and the risk of inadvertent macular photocoagulation and visual loss.29
Also in the 1990s, a new concept of targeting choroidal vessels in the neovascular membrane emerged using a photosensitizer activated by red/near-infrared laser and became known as photodynamic therapy (PDT). The original photosensitizer phthalocyanine was replaced by the liposomal benzoporphyrin derivative complex with affinity to endothelium of newly formed blood vessels.30–32 The latter is commercially known as verteporfin which was the first pharmacologic treatment for AMD.33 The PDT treatment causes intraluminal vascular occlusion with subsequent regression of choroidal neovascular membrane.34 With time, its use in AMD has been replaced by more effective and less destructive intravitreal anti-angiogenic therapy. It still remains a treatment option or supplemental therapy in some pathologic choroidal conditions.
Current laser delivery systems
Developments in laser technology lagged behind developments in other areas of retinal field such as imaging, pharmacology and genetics. Most innovations in laser therapy in previous decades have focused on laser adjustments such as spot size and pulse duration. However, two major developments took place in recent years.
In 2006, OptiMedica Corp. (Santa Clara, CA) introduced PASCAL pattern scan laser photocoagulator with a 532-nm laser used for standard photocoagulation procedures that can apply a uniform pattern of many laser spots at one time.35 Due to short pulse duration, the heat is decreased resulting in less thermal damage. The pattern laser technology allows equidistant spacing of individual spots and fairly consistent retina burns. The PASCAL laser allows ophthalmologists to perform macular grid treatments effectively and panretinal photocoagulation more rapidly with less pain than conventional lasers.36,37 At present, it is one of the most common laser delivery systems.
The second major development was introduction of new laser platform called NAVILAS (OD-OS, Inc. Germany) which uses retinal navigation and fundus camera based delivery. This 532-nm pattern-type eye-tracking laser integrates live color fundus imaging, red-free and infra-red imaging, fluorescein angiography with photocoagulator system.38–40 After image acquisition and making customized treatment plans by physicians including marking areas which will be coagulated the treatment plan is superimposed onto the live digital retina image during treatment. The physician controls laser application and the systems assist with prepositioning the laser beam. This platform allows for digital documentation of treatment for future reference. For the first time physicians are able to deliver fast and painless laser through camera system and monitor treatment progress on wide screen.41,42 Retinal navigation has resulted in significant increase in treatment accuracy in comparison to conventional slit-lamp lasers.39,43
Current posterior pole laser treatment techniques
Conventional laser photocoagulation techniques
Argon laser photocoagulation (488 and 514.5-nm) has been the most common standard treatment for diabetic maculopathy with DME and continues to be a treatment option even in the era of intravitreal pharmacotherapy. The ETDRS showed that laser treatment reduced the incidence of moderate vision loss by 50%.44 The effects of therapy are controlled by exposure time, power, spot size with a short and intense exposure time increasing risk of tissue (Bruch’s membrane) rupture and retinal hemorrhages. Long and less intense exposure times as used in treatment of some vascular malformations increase in size afterwards. A consideration of different magnification factors for contact lens is also important (Mainster focal grid (1.05), Volk area centralis (1.0) and the Goldmann 3-mirror contact glass (1.08) induce no significant magnification. However, Quadraspheric (1.92), SuperQuad 160 (2.0) and Ultrafield (1.89) need laser beam reduction by half). The retinal target should be properly focused and aligned perpendicular to the axis of the slit-lamp beam, giving a sharp laser spot on the retinal surface.
Early treatment with focal macular photocoagulation before chronic macular edema ensues is recommended for maintaining good vision. Focal laser refers to a direct treatment of leaking aneurysms in the edematous retina within 3000 μm of the center of the macula. For conventional treatment, each microaneurysm is treated by a 50- to 100-μm spot and an exposure of 0.1 s, leading to spots of small chorioretinal scars. Parameters can be modified if we wish to apply subthreshold treatments.
Grid pattern laser photocoagulation has been believed to increase the migration and proliferation of retinal pigment epithelium cells and endothelial cells, thus decreasing fluid exudation. Grid laser is mainly used in areas of diffuse leakage with no defined focal leakage. The grid technique is composed of burns 50–200 μm in diameter, producing a pattern of equally spaced burns and spots. Grid laser in diffuse DME has questionable long-term efficacy.45 Grid laser photocoagulation has been an evidence-based treatment of choice for macular edema due to branch retinal vein occlusion46 but may now be complimented or replaced by antiangiogenic drug therapy as the first line of treatment.
Pattern scanning laser photocoagulation techniques
Pattern scanning laser (PASCAL) photocoagulator delivers multiple burns in a rapid predetermined sequence in the form of a pattern array produced by a scanner. The pulse duration is reduced to 10–30 ms. The aim is to optimize therapeutic effect with minimal damage to the retina tissue. In initial studies the treatment of macular edema seemed safe, comfortable and of the same efficacy as conventional laser.47,48 For macular grid laser photocoagulation, however, the single spot technique seems to be safer due to danger of eye movement during the treatment.49 Clinical efficacy of short pulse pattern photocoagulation has been shown in macular edema associated with branch retinal vein occlusion.50 Immediate tissue remodeling has been found using spectral-domain51 and polarization-sensitive OCT.52 While tissue damage is minimized, healing occurs by migration and filling-in of adjacent surviving tissue rather than regeneration with inherent loss of retinal function and re-treatment limitation. However, no loss of photoreceptors in humans has been observed using adaptive optics imaging.53
Subthreshold diode micropulse technique
As described above, SDM employs a unique treatment paradigm: low-intensity micropulsed laser spots are applied which, while absorbed selectively by the RPE, do not damage the RPE in any currently detectable way.54,55 Thus, focal treatment of retinal microaneurysms is not a strategy of SDM. The low-intensity treatment effect is then amplified and maximized by placement of many confluent and contiguous laser spots (high-density treatment) over the entire area of retinal pathology. In the absence of tissue damage and subsequent inflammation and healing, SDM appears to work by normalizing RPE function, likely manifest by altered cytokine expression.19 SDM has no known adverse treatment effects and, in the treatment of DME, has been found to be more effective than conventional photocoagulation in a randomized clinical trial.56 In the absence of retinal damage the potential for retreatment with SDM is unlimited. SDM can be used alone or in combination with drug therapy to achieve retina-sparing disease management.55 Despite the absence of retinal damage or adverse treatment effects, SDM has been reported effective in the treatment of DME, proliferative diabetic retinopathy, retinal vein occlusion, central serous chorioretinopathy, and other disorders (Fig. 1).19
Figure 1.

(Case 1). Eye with diffuse center-involving diabetic macular edema: Fundus autofluorescence photograph (FAF) before (A) and after (B) transfoveal low-intensity high-density subthreshold diode micropulse laser (SDM). Note reduction in cystoid macular edema and severity of posterior retinopathy without evidence of laser-induced retinal damage. Fundus fluorescein angiogram before (C) and after (D) treatment. Note absence of laser-induced retinal damage. (E) Spectral-domain optical coherence tomogram before (above) and after (below) transfoveal SDM. Note reduction in DME without evidence of laser-induced retinal damage. (Images by Dr. J. Luttrull).
Navigated laser photocoagulation technique
Both focal and grid laser treatments of the posterior pole can now be performed using retinal eye-tracking assisted photocoagulation. Navigated laser photocoagulation is a safe technique that significantly increases accuracy of laser delivery to the retina.39 This is especially useful in focal photocoagulation technique where the exact location and targeting of diabetic microaneurysms, for instance, is of crucial importance (Figs. 2–5). In accuracy of laser delivery, it significantly outperformed conventional laser photocoagulation with 96% of laser applications being delivered within 100 μm from the target spot.41 This is believed to contribute to its clinical efficacy in focal retinovascular disease.57,58 Because of different imaging principles, the photocoagulation does not require the use of contact lens and can be monitored on computer screen.
Figure 2.
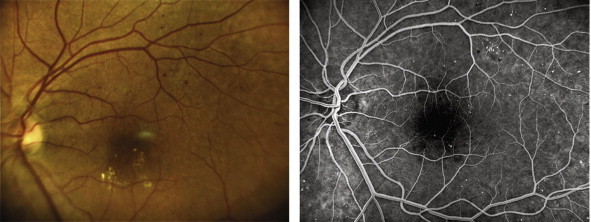
(Case 2). LEFT PANEL: Color fundus image of an eye with non-proliferative diabetic retinopathy and maculopathy showing dot blot hemorrhages and hard exudates in the macular area. RIGHT PANEL: Late phase fluorescein angiography showing multiple microaneurysms throughout the posterior pole.
Figure 3.

(Case 2). LEFT PANEL: Optical coherence tomography thickness map of the same eye showing increased foveal thickness. RIGHT PANEL: Color fundus photograph of the same eye immediately after navigated focal laser photocoagulation showing a laser burn (white arrow) to the macular microaneurysm (please compare with pre-treatment color fundus photo from Fig. 2).
Figure 4.

(Case 2). UPPER PANEL: Pre-treatment optical coherence tomography macular B-scan of the same eye showing intraretinal edema. LOWER PANEL: Post-treatment optical coherence tomography macular B-scan of the same eye showing resolution of the macular edema with residual intraretinal hard exudates.
Figure 5.

(Case 2). Post-treatment optical coherence tomography retinal thickness map of the same eye showing resolution of the macular edema with laser spots (left side) and follow-up scan of the same retinal section showing the amount of thickness decrease (right side) (Image series by Dr. I. Kozak).
Current panretinal photocoagulation (PRP)
Conventional single-spot laser PRP
The Diabetic Retinopathy Study and Early Treatment Diabetic Retinopathy Study are landmark studies that for long have impacted clinical practice patterns.7,8 Until today, the panretinal photocoagulation is the first treatment of choice for high risk proliferative diabetic retinopathy and its complications such as rubeosis iridis. Panretinal photocoagulation, as recommended by those original randomized clinical trials, uses visible end point (whitening of the retina) achieved by recommended parameters of 500 microns spot size, one-half to one spot diameter spacing and 100–200 ms duration.8 The whitening is caused by thermal damage in which the temperature rises 20–30 °C above baseline body temperature. A typical PRP pattern of 1200 to 1500 burns is applied in order to reduce the number of metabolically active photoreceptors as well as total oxygen consumption of the outer retina. Significant regression of retinopathy risk factors has been reported after PRP.59,60 Some modifications in argon laser technique such as light PRP (LPRP) were adopted to reduce adverse effects of heavy PRP.61 Other types of lasers have been used for PRP such as orange dye (600-nm) laser,62 red (630-nm) and yellow (580-nm) dye lasers,63 krypton laser,64 diode laser,65 and double-frequency Nd:YAG laser.66
Pattern scanning laser photocoagulation PRP
Panretinal photocoagulation with conventional laser systems can cause a variety of side effects including peripheral field loss and decrease in central and peripheral vision due to retinal tissue destruction.15,16 The procedure can be painful for patients and is usually divided into several sessions. The short-pulse semiautomated PRP is now possible with the PASCAL photocoagulator which is capable of producing a variety of short-pulse pattern arrays (Fig. 6). Pattern PRP has significantly shortened treatment times and has been shown to produce less pain during the procedure compared to conventional lasers.37,47 Single session treatment has been reported to be of equal clinical efficacy in controlling proliferative diabetic eye disease as multiple sessions.67 Favorable regression rates in proliferative diabetic retinopathy have been described68 as well as some concerns that reduction of treatment parameters may cause failure to control proliferative disease calling for adjusting the parameters.69
Figure 6.
(Case 3). Wide-field late phase fluorescein angiogram of an eye with aggressive proliferative diabetic retinopathy showing areas of retinal non-perfusion and active neovascularization in spite of prior pattern short-pulse panretinal photocoagulation (Image by Dr. I. Kozak).
Subthreshold diode micropulse PRP
The subthreshold diode micropulse laser approach has been used in panretinal photocoagulation after its efficacy has been shown in DME (Fig. 7). The rationale is that the patholophysiology of diabetic retinopathy is the same in all parts of the retina. In the macula, it is manifested by diabetic macular edema and, less often, macular ischemia. In the rest of the retina it is manifested by ischemia leading to ocular neovascularization. Thus treatments effective against DME are hypothesized to be effective against proliferative diabetic retinopathy. Thus, it is not surprising that SDM, which is effective in the treatment of DME, has also been reported to be effective as panretinal laser treatment for PDR.70 In this study, the clinical response to SDM PRP appeared to be more benign than following conventional PRP, but similar to anti-VEGF therapy. This was attributed to the lack of retinal damage and subsequent inflammation. Progression of severe non-proliferative diabetic retinopathy to proliferative retinopathy also appeared reduced. There were no treatment complications or adverse effects, and no laser-induced retinal damage by FFA. However, it has since become clear that all therapeutically effective treatment modes for diabetic retinopathy, including retinal photocoagulation and intravitreal drug therapy, also slow, stop, or reverse the rate of disease progression.71 The unique safety profile of SDM suggests that it, or a similarly safe process, may become the first practical preventive treatment for diabetic retinopathy.
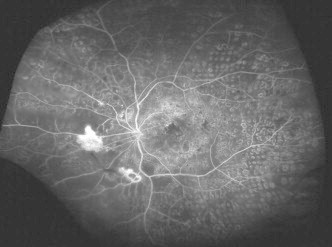
Figure 7.

(Case 4). Intravenous fundus fluorescein angiogram before (A) and after (B) subthreshold diode micropulse (SDM) laser panretinal photocoagulation for severe non-proliferative diabetic retinopathy. Note reversal of retinopathy severity, reduction in micro- and macrovascular leakage, resolution of local retinal capillary non-perfusion, and absence of laser-induced retinal damage. Preoperative visual acuity 20/20; postoperative 20/15 (Images by Dr. J. Luttrull).
Navigated laser PRP
Panretinal photocoagulation is now possible to be performed with retinal eye-tracking (Fig. 8). Unlike treating the posterior pole of the retina with eye-tracking where we do not need the contact lens, in PRP we use a wide-field contact lens. In navigated PRP, the laser system provides a pattern positioning on the retina, independent from the imaging by using galvanometer scanners controlled by the operator via elements on the system base joystick or by placing treatment patterns on the touch screen. Unlike pattern laser systems which can use only short pulse arrays, the navigated PRP arrays can be performed with 100 ms pulse durations thereby following the original criteria from randomized clinical trials.7,8 It has been observed that PRP laser scars are more uniform in navigated PRP compared to pattern laser system probably due to different optical systems used by both systems.72
Figure 8.

(Case 5). Wide-field fundus photo of an eye with proliferative diabetic retinopathy during navigated panretinal photocoagulation (A) with 100 ms pulse duration pattern as shown in final report (B) (Images by Dr. I. Kozak).
Targeted retinal photocoagulation (TRP)
Targeted or selective therapy in general is any therapy aimed to block a specific target. Examples of targeted retinal therapy can be feeder vessel photocoagulation in choroidal neovascularization or focal laser photocoagulation in the treatment of DME. These are not new concepts and, therefore, here we would like to focus on selective retina laser therapy to areas of non-perfusion.
The idea behind targeted retinal photocoagulation (TRP) is to selectively treat ischemic retinal areas and adjacent intermediate areas showing angiographic leakage while minimizing some of the risks and complications of conventional PRP.73,74 Wide-angle fluorescein angiography has been instrumental in identification of peripheral areas of non-perfusion and has opened the door for clinical application of TRP.75–77 It has served as a guide for TRP in recent studies. In reports by Muqit et al. TRP for proliferative diabetic retinopathy using 20-ms PASCAL did not produce increased macular thickness and paradoxically improved central retinal thickness and visual field sensitivity with reasonable neovascularization regression rate.78,79 TRP may be less effective in central retinal vein occlusion which has a different ischemic load compared to diabetic retinopathy. Spaide in a recent prospective study reported no clinical benefit using laser photocoagulation to peripheral areas of non-perfusion visualized by wide-field angiography.80 It is obvious that more prospective randomized trials are needed to assess the real benefit of TRP.
Conflict of interest
The authors declared that there is no conflict of interest.
References
- 1.Meyer-Schwickerath G. Light Coagulation: a method for treatment and prevention of the retinal detachment. Albert Von Graefes Arch Ophthalmol. 1954;156(1):2–34. [PubMed] [Google Scholar]
- 2.Meyer-Schwickerath G. Prophylactic treatment of retinal detachment by light coagulation. Trans Ophthalmol Soc UK. 1956;76:739–750. [PubMed] [Google Scholar]
- 3.Kapany N.S., Peppers N.A., Zweng H.C., Flocks M. Retinal photocoagulation by lasers. Nature. 1963;199:146–149. doi: 10.1038/199146a0. [DOI] [PubMed] [Google Scholar]
- 4.Noyori K.S., Campbell C.J., Rittler M.C., Koester C. Ocular thermal effects produced by photocoagulation. Arch Ophthalmol. 1963;70:817–822. doi: 10.1001/archopht.1963.00960050819017. [DOI] [PubMed] [Google Scholar]
- 5.Bridges W.B. Laser oscillation in singly ionized argon in visible spectrum. Appl Phys Lett. 1964;4:128. [Google Scholar]
- 6.L’Esperance F.A., Jr. An ophthalmic argon laser photocoagulation system: design, construction, and laboratory investigations. Trans Am Ophthalmol Soc. 1968;66:827–904. [PMC free article] [PubMed] [Google Scholar]
- 7.The Diabetic Retinopathy Study Research Group Photocoagulation treatment of proliferative diabetic retinopathy: clinical application of Diabetic Retinopathy Study (DRS) findings, DRS Report Number 8. Ophthalmology. 1981;88(7):583–600. [PubMed] [Google Scholar]
- 8.Early Treatment Diabetic Retinopathy Study Research Group Techniques for scatter and local photocoagulation treatment of diabetic retinopathy. Early Treatment Diabetic Retinopathy Study Report Number 3. Int Ophthalmol Clin. 1987;27(4):254–264. doi: 10.1097/00004397-198702740-00005. [DOI] [PubMed] [Google Scholar]
- 9.Macula Photocoagulation Study Group Argon laser photocoagulation for senile macular degeneration: results of a randomized clinical trial. Arch Ophthalmol. 1982;100(6):912–918. doi: 10.1001/archopht.1982.01030030920003. [DOI] [PubMed] [Google Scholar]
- 10.Holzrichter J.F., Schawlow A.L. Design and analysis of flashlamp systems for pumping organic dye lasers. Ann N Y Acad Sci. 1969;168(3):703–714. doi: 10.1111/j.1749-6632.1969.tb43155.x. [DOI] [PubMed] [Google Scholar]
- 11.Manson N., Marshall J., Mellerio J., Smart D. Comments on histological studies of gas laser lesions in humans and possible non-linear optical phenomena, together with experiments using a tuneable dye laser. Mod Probl Ophthalmol. 1972;10:114–128. [PubMed] [Google Scholar]
- 12.Little H.L., Zweng H.C., Peabody R.R. Argon laser slit-lamp retinal photocoagulation. Trans Am Acad Ophthalmol Otolaryngol. 1970;74(1):85–97. [PubMed] [Google Scholar]
- 13.Morgan C.M., Schatz H. Atrophic creep of the retinal pigment epithelium after focal macular photocoagulation. Ophthalmology. 1989;96(1):96–103. doi: 10.1016/s0161-6420(89)32924-1. [DOI] [PubMed] [Google Scholar]
- 14.McDonald H.R., Schatz H. Macular edema following panretinal photocoagulation. Retina. 1985;5(1):5–10. doi: 10.1097/00006982-198500510-00002. [DOI] [PubMed] [Google Scholar]
- 15.Frank R.N. Visual fields and electroretinography following extensive photocoagulation. Arch Ophthalmol. 1975;93(8):591–598. doi: 10.1001/archopht.1975.01010020575004. [DOI] [PubMed] [Google Scholar]
- 16.McDonald H.R., Schatz H. Visual loss following panretinal photocoagulation for proliferative diabetic retinopathy. Ophthalmology. 1985;92(3):388–393. doi: 10.1016/s0161-6420(85)34016-2. [DOI] [PubMed] [Google Scholar]
- 17.Akduman L., Olk R.J. Subthreshold (invisible) modified grid diode laser photocoagulation in diffuse diabetic macular edema (DDME) Ophthalmic Surg Lasers. 1999;30(9):706–714. [PubMed] [Google Scholar]
- 18.Olk R.J., Friberg T.R., Stickney K.L., Akduman L., Wong K.L., Chen M.C. Ophthalmology. 1999;106(11):2082–2090. doi: 10.1016/S0161-6420(99)90487-6. [DOI] [PubMed] [Google Scholar]
- 19.Luttrull J.K., Dorin G. Subthreshold diode micropulse photocoagulation as invisible retinal phototherapy for diabetic macular edema. A review. Curr Diab Rev. 2012;8:274–284. doi: 10.2174/157339912800840523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roider J., Hillenkamp F., Flotte T.J., Birngruber R. Microphotocoagulation: selective effects of repetitive short laser pulses. Proc Natl Acad Sci USA. 1993;90(11):2037–2038. doi: 10.1073/pnas.90.18.8643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pankratov M.M. Pulsed delivery of laser energy in experimental thermal retinal photocoagulation. Proc Soc Photo Opt Instrum Eng. 1990;1202:205–213. [Google Scholar]
- 22.Dorin G. Subthreshold and micropulse photocoagulation. Semin Ophthalmol. 2003;18:147–153. doi: 10.1076/soph.18.3.147.29812. [DOI] [PubMed] [Google Scholar]
- 23.Roider J., Michaud N.A., Flotte T.J., Birngruber R. Response of the retinal pigment epithelium to selective photocoagulation. Arch Ophthalmol. 1992;110(12):1786–1792. doi: 10.1001/archopht.1992.01080240126045. [DOI] [PubMed] [Google Scholar]
- 24.Vujosevic S., Bottega E., Casciano M., Pilotto E., Convento E., Midena E. Microperimetry and fundus autofluorescence in diabetic macular edema. Subthreshold micropulse diode laser versus modified Early Treatment Diabetic Retinopathy Study Laser photocoagulation. Retina. 2010;30:908–916. doi: 10.1097/IAE.0b013e3181c96986. [DOI] [PubMed] [Google Scholar]
- 25.Roider J., Brinkmann R., Wirbelauer C., Laqua H., Birngruber R. Subthreshold (retinal pigment epithelium) photocoagulation in macular diseases: a pilot study. Br J Ophthalmol. 2000;84(1):40–47. doi: 10.1136/bjo.84.1.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brinkmann R., Roider J., Birngruber R. Selective retina therapy (SRT): a review on methods, techniques, preclinical and first clinical results. Bull Soc Belge Ophthalmol. 2006;302:51–69. [PubMed] [Google Scholar]
- 27.Journee-de Korver JG J.G., Oosterhius J.A., Kakebeeke-Kemme H.M., de Wolff-Rouendaal D. Transpupillary thermotherapy (TTT) by infrared irradiation of choroidal melanoma. Doc Ophthalmol. 1992;82(3):185–191. doi: 10.1007/BF00160764. [DOI] [PubMed] [Google Scholar]
- 28.Kwon H.J., Ko J.S., Kim M., Lee C.S., Lee S.C. Prognosis of choroidal melanoma and the result of ruthenium brachytherapy combined with transpupillary thermotherapy in Korean patients. Br J Ophthalmol. 2013;97(5):653–658. doi: 10.1136/bjophthalmol-2012-302584. [DOI] [PubMed] [Google Scholar]
- 29.Squirrell D.M., Stewart A.W., Joondeph B.C. Large-spot subthreshold infrared laser to treat diabetic macular edema. Retina. 2008;28(4):615–621. doi: 10.1097/IAE.0b013e31815ee567. [DOI] [PubMed] [Google Scholar]
- 30.Kliman G.H., Puliafito C.A., Stern D., Borirakchanyavat S., Gregory W.A. Phthalocyanine photodynamic therapy: new strategy for closure of choroidal neovascularization. Lasers Surg Med. 1994;15(1):2–10. doi: 10.1002/lsm.1900150103. [DOI] [PubMed] [Google Scholar]
- 31.Schmidt-Erfurth U., Hasan T., Gragoudas E., Birngruber R. Selective occlusion of subretinal neovascularization with photodynamic therapy. Ophthalmologe. 1994;91(6):789–795. [PubMed] [Google Scholar]
- 32.Miller J.W., Walsh A.W., Kramer M., Hasan T., Michaud N., Flotte T.J. Photodynamic therapy of experimental choroidal neovascularization using lipoprotein-delivered benzoporphyrin. Arch Ophthalmol. 1995;113(6):810–818. doi: 10.1001/archopht.1995.01100060136048. [DOI] [PubMed] [Google Scholar]
- 33.Bressler N.M. Treatment of age-related macular degeneration with photodynamic therapy (TAP) Study group. Arch Ophthalmol. 2001;119(2):198–202. [PubMed] [Google Scholar]
- 34.Luttrull J.K., Spink C.J. Prolonged choroidal hypofluorescence following verteporfin photodynamic therapy combined with intravitreal triamcinolone acetonide injection. Retina. 2007;27(6):688–692. doi: 10.1097/IAE.0b013e318030e999. [DOI] [PubMed] [Google Scholar]
- 35.Blumenkranz M.S., Yellachich D., Andersen D.E., Wiltberger M.W., Mordaunt D., Marcellino G.R. Semiautomated patterned scanning laser for retinal photocoagulation. Retina. 2006;26(3):370–376. doi: 10.1097/00006982-200603000-00024. [DOI] [PubMed] [Google Scholar]
- 36.Muqit M.M., Marcellino G.R., Gray J.C., McLauchlan R., Henson D.B., Young L.B. Pain responses of Pascal 20 ms multi-spot and 100 ms single-spot panretinal photocoagulation: Manchester Pascal Study, MAPASS report 2. Br J Ophthalmol. 2010;94(11):1493–1498. doi: 10.1136/bjo.2009.176677. [DOI] [PubMed] [Google Scholar]
- 37.Nagpal M., Marlecha S., Nagpal K. Comparison of laser photocoagulation for diabetic retinopathy using 532-nm standard laser versus multisport pattern scan laser. Retina. 2010;30(3):452–458. doi: 10.1097/IAE.0b013e3181c70127. [DOI] [PubMed] [Google Scholar]
- 38.Liesfeld B., Amthor K.U., Dowell D., Weber U., Teiwes W. Navigating comfortably across the retina. IFMBE Proc. 2009;25(11):243–246. [Google Scholar]
- 39.Kozak I., Oster S.F., Cortes M.A., Dowell D., Hartmann K., Kim J.S. Clinical evaluation and treatment accuracy in diabetic macular edema using navigated laser photocoagulator NAVILAS. Ophthalmology. 2011;118(6):1119–1124. doi: 10.1016/j.ophtha.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 40.Kernt M., Cheuteu R., Vounotrypidis E., Haritoglou C., Kampik A., Ulbig M.W. Focal and panretinal photocoagulation with a navigated laser (NAVILAS®) Acta Ophthalmol. 2011;89(8):662–664. doi: 10.1111/j.1755-3768.2010.02017.x. [DOI] [PubMed] [Google Scholar]
- 41.Kernt M., Cheuteu R.E., Cserhati S., Seidensticker F., Liegl R.G., Lang J. Pain and accuracy of focal laser treatment for diabetic macular edema using a retinal navigated laser (Navilas) Clin Ophthalmol. 2012;6:289–296. doi: 10.2147/OPTH.S27859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ober M.D., Kernt M., Cortes M.A., Kozak I. Time required for navigated macular laser photocoagulation treatment with the Navilas. Graefes Arch Clin Exp Ophthalmol. 2013;251(4):1049–1053. doi: 10.1007/s00417-012-2119-0. [DOI] [PubMed] [Google Scholar]
- 43.Kozak I., Kim J.S., Oster S.F., Chhablani J., Freeman W.R. Focal navigated laser photocoagulation in retinovascular disease: clinical results in initial case series. Retina. 2012;32(5):930–935. doi: 10.1097/IAE.0b013e318227ab5b. [DOI] [PubMed] [Google Scholar]
- 44.Early Treatment Diabetic Retinopathy Study Research Group Photocoagulation for diabetic macular edema. Early Treatment Diabetic Retinopathy Study Report Number 1. Arch Ophthalmol. 1985;103:1796–1806. [PubMed] [Google Scholar]
- 45.Lee C.M., Olk R.J. Modified grid laser photocoagulation for diffuse diabetic macular edema: long-term visual results. Ophthalmology. 1991;98:1594–1602. doi: 10.1016/s0161-6420(91)32082-7. [DOI] [PubMed] [Google Scholar]
- 46.The Branch Vein Occlusion Study Group Argon laser photocoagulation for macular edema in branch vein occlusion. Am J Ophthalmol. 1984;98(3):271–282. doi: 10.1016/0002-9394(84)90316-7. [DOI] [PubMed] [Google Scholar]
- 47.Sanghvi C., McLauchlan R., Delgado C., Young L., Charles S.J., Marcellino G. Initial experience with the Pascal photocoagulator: a pilot study of 75 procedures. Br J Ophthalmol. 2008;92(8):1061–1064. doi: 10.1136/bjo.2008.139568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Modi D., Chiranand P., Akduman L. Efficacy of patterned scan laser in the treatment of macular edema and retinal neovascularization. Clin Ophthalmol. 2009;3:465–470. doi: 10.2147/opth.s6486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rufer F., Flohr C.M., Poerksen E., Roider J. Retinal laser coagulation with the pattern scanning laser-report of first clinical experience. Klin Monbl Augenheilkd. 2008;225(11):968–972. doi: 10.1055/s-2008-1027744. [DOI] [PubMed] [Google Scholar]
- 50.Pitcher J.D., Liu T., Prasad P.S., Schwartz S.D., Hubschman J.P. Short-duration focal pattern grid photocoagulation for macular edema secondary to branch retinal vein occlusion. Semin Ophthalmol. 2012;27(3–4):69–72. doi: 10.3109/08820538.2011.643272. [DOI] [PubMed] [Google Scholar]
- 51.Bolz M., Kriechbaum K., Simader C., Deak G., Lammer J., Treu C. Diabetic Retinopathy Research Group Vienna. In vivo retinal morphology after grid laser treatment in diabetic macular edema. Ophthalmology. 2010;117(3):538–544. doi: 10.1016/j.ophtha.2009.07.035. [DOI] [PubMed] [Google Scholar]
- 52.Lammer J., Bolz M., Baumann B., Pircher M., Gotzinger E., Mylonas G. Diabetic Retinopathy Research Group Vienna. Imaging retinal pigment epithelial proliferation secondary to PASCAL photocoagulation in vivo by polarization-sensitive optical coherence tomography. Am J Ophthalmol. 2013;155(6):1058–1607. doi: 10.1016/j.ajo.2012.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Han D.P., Croskrey J.A., Dubis A.M., Schroeder B., Rha J., Carroll J. Adaptive optics and spectral-domain optical coherence tomography of human photoreceptor structure after short-duration Pascal macular grid and panretinal laser photocoagulation. Arch Ophthalmol. 2012;130(4):518–521. doi: 10.1001/archophthalmol.2011.2878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Luttrull J.K., Musch M.C., Mainster M.A. Subthreshold diode micropulse photocoagulation for the treatment of clinically significant diabetic macular edema. Br J Ophthalmol. 2005;89(1):74–80. doi: 10.1136/bjo.2004.051540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Luttrull J.K., Sramek C., Palanker D., Spink C.J., Musch D.C. Long-term safety, high-resolution imaging, and tissue temperature modeling of subvisible diode micropulse photocoagulation for retinovascular macular edema. Retina. 2012;32(2):375–386. doi: 10.1097/IAE.0b013e3182206f6c. [DOI] [PubMed] [Google Scholar]
- 56.Lavinsky D., Cardillo J.A., Melo L.A., Jr, Dare A., Farah M.E., Belfort R., Jr. Randomized clinical trial evaluating mETDRS versus normal or high-density micropulse photocoagulation for diabetic macular edema. Invest Ophthalmol Vis Sci. 2011;52:4314–4323. doi: 10.1167/iovs.10-6828. [DOI] [PubMed] [Google Scholar]
- 57.Chhablani J., Kozak I., Barteselli G., El-Emam S. A novel navigated laser system brings new efficacy to the treatment of retinovascular disorders. Oman J Ophthalmol. 2013;6(1):18–22. doi: 10.4103/0974-620X.111898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Jung J.J., Gallego-Pinazo R., Lleo-Perez A., Huz J.I., Barbazetto I.A. NAVILAS laser system focal treatment for diabetic macular edema – one year results of a case series. Open Ophthalmol J. 2013;7:48–53. doi: 10.2174/1874364101307010048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Doft B.H., Blakenship G. Retinopathy risk factor regression after laser panretinal photocoagulation for proliferative diabetic retinopathy. Ophthalmology. 1984;91(12):1453–1457. doi: 10.1016/s0161-6420(84)34123-9. [DOI] [PubMed] [Google Scholar]
- 60.Blakenship G.W. Fifteen-year argon laser and xenon photocoagulation results of Bascom Palmer Eye Institute’s patients participating in the diabetic retinopathy study. Ophthalmology. 1991;98(2):125–128. doi: 10.1016/s0161-6420(91)32326-1. [DOI] [PubMed] [Google Scholar]
- 61.Bandello F., Brancato R., Menchini U., Virgili G., Lanzetta P., Ferrari E. Light panretinal photocoagulation (LPRP) versus classic panretinal photocoagulation (CPRP) in proliferative diabetic retinopathy. Semin Ophthalmol. 2001;16(1):12–18. doi: 10.1076/soph.16.1.12.4223. [DOI] [PubMed] [Google Scholar]
- 62.Seiberth V., Schatanek S., Alexandridis E. Panretinal photocoagulation in diabetic retinopathy: argon versus dye laser coagulation. Graefes Arch Clin Exp Ophthalmol. 1993;231(6):318–322. doi: 10.1007/BF00919027. [DOI] [PubMed] [Google Scholar]
- 63.Atmaca L.S., Idil A., Gunduz K. Dye laser in proliferative diabetic retinopathy and maculopathy. Acta Ophthalmol Scand. 1995;73(4):303–307. doi: 10.1111/j.1600-0420.1995.tb00031.x. [DOI] [PubMed] [Google Scholar]
- 64.The Krypton Argon Regression Neovascularization Study report number 1 Randomized comparison of krypton versus argon scatter photocoagulation for diabetic disc neovascularization. Ophthalmology. 1993;100(11):1655–1664. doi: 10.1016/s0161-6420(93)31421-1. [DOI] [PubMed] [Google Scholar]
- 65.Bandello F., Brancato R., Trabucchi G., Lattanzio R., Malegori A. Diode versus argon-green laser panretinal photocoagulation in proliferative diabetic retinopathy: a randomized study in 44 eyes with a long follow-up time. Greafes Arch Clin Exp Ophthalmol. 1993;231(9):491–494. doi: 10.1007/BF00921112. [DOI] [PubMed] [Google Scholar]
- 66.Bandello F., Brancato R., Lattanzio R., Trabucchi G., Azzolini C., Malegori A. Double-frequency Nd:YAG laser vs. argon-green laser in the treatment of proliferative diabetic retinopathy: randomized study with long-term follow-up. Lasers Surg Med. 1996;19(2):173–176. doi: 10.1002/(SICI)1096-9101(1996)19:2<173::AID-LSM8>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 67.Muqit M.M., Marcellino G.R., Henson D.B., Young L.B., Patton N., Charles S.J. Single-session vs multiple-session pattern scanning laser panretinal photocoagulation in proliferative diabetic retinopathy: Manchester Pascal Study. Arch Ophthalmol. 2010;128(5):525–533. doi: 10.1001/archophthalmol.2010.60. [DOI] [PubMed] [Google Scholar]
- 68.Muqit M.M., Marcellino G.R., Henson D.B., Young L.B., Turner G.S., Stanga P.E. Pascal panretinal laser ablation and regression analysis in proliferative diabetic retinopathy: Manchester Pascal Study Report 4. Eye. 2011;25(11):1447–1456. doi: 10.1038/eye.2011.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Chappelow A.V., Tan K., Waheed N.K., Kaiser P.K. Panretinal photocoagulation for proliferative diabetic retinopathy: pattern scan laser versus argon laser. Am J Ophthalmol. 2012;153(1):137–142. doi: 10.1016/j.ajo.2011.05.035. [DOI] [PubMed] [Google Scholar]
- 70.Luttrull J.K., Spink C.J., Musch D.A. Subthreshold diode micropulse panretinal photocoagulation for proliferative diabetic retinopathy. Eye. 2008;22(5):60. doi: 10.1038/sj.eye.6702725. [DOI] [PubMed] [Google Scholar]
- 71.Bressler S.B., Qin H., Melia M., Bressler N.M., Beck R.W., Chan C.K. Diabetic Retinopathy Clinical Research Network. Exploratory analysis of the effect of intravitreal ranibizumab or triamcinolone on worsening of diabetic retinopathy in a randomized clinical trial. JAMA Ophthalmol. 2013;131(8):1033–1040. doi: 10.1001/jamaophthalmol.2013.4154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kozak I, Chhablani J, Mathai A, Rani P, Alshahrani S, Gupta V, et al. Comparison of the visible effect on the fundus in peripheral laser photocoagulation between conventional pattern laser and Navilas, presented at the13th EURETINA Congress, Hamburg, Germany, September 26–29, 2013.
- 73.Blakenship G.W. A clinical comparison of central and peripheral argon laser panretinal photocoagulation for proliferative diabetic retinopathy. Ophthalmology. 1988;95(2):170–177. doi: 10.1016/s0161-6420(88)33212-4. [DOI] [PubMed] [Google Scholar]
- 74.Reddy S., Hu A., Schwartz S.D. Ultra wide field fluorescein angiography guided targeted retinal photocoagulation (TRP) Semin Ophthalmol. 2009;24:9–14. doi: 10.1080/08820530802519899. [DOI] [PubMed] [Google Scholar]
- 75.Manivannan A., Plskova J., Farrow A., Mckay S., Sharp P.F., Forrester J.V. Ultra-wide-field fluorescein angiography of the ocular fundus. Am J Ophthalmol. 2005;140(3):525–527. doi: 10.1016/j.ajo.2005.02.055. [DOI] [PubMed] [Google Scholar]
- 76.Mackenzie P.J., Russell M., Ma P.E., Isbister C.M., Maberley D.A. Sensitivity and specificity of the Optos optomap for detecting peripheral retinal lesions. Retina. 2007;27(8):1119–1124. doi: 10.1097/IAE.0b013e3180592b5c. [DOI] [PubMed] [Google Scholar]
- 77.Friberg T.R., Gupta A., Yu J., Huang L., Suner I., Puliafito C.A. Ultrawide angle fluorescein angiographic imaging: a comparison to conventional digital acquisition systems. Ophthalmic Surg Lasers Imaging. 2008;39(4):304–311. doi: 10.3928/15428877-20080701-06. [DOI] [PubMed] [Google Scholar]
- 78.Muqit M.M., Young L.B., McKenzie R., John B., Marcellino G.R., Henson D.B. Pilot randomized clinical trial of Pascal TargETEd Retinal versus variable fluence PANretinal 20 ms laser in diabetic retinopathy: PETER PAN study. Br J Ophthalmol. 2013;97(2):220–227. doi: 10.1136/bjophthalmol-2012-302189. [DOI] [PubMed] [Google Scholar]
- 79.Muqit M.M., Marcellino G.R., Henson D.B., Young L.B., Patton N., Charles S.J. Optos-guided pattern scan laser (Pascal)-targeted retinal photocoagulation in proliferative diabetic retinopathy. Acta Ophthalmol. 2013;91(3):251–258. doi: 10.1111/j.1755-3768.2011.02307.x. [DOI] [PubMed] [Google Scholar]
- 80.Spaide R.F. Prospective study of peripheral panretinal photocoagulation of areas of nonperfusion in central retinal vein occlusion. Retina. 2013;33(1):56–62. doi: 10.1097/IAE.0b013e3182641875. [DOI] [PubMed] [Google Scholar]


