Abstract
Background
Chronic illnesses are significant to individuals and costly to society. When systematically implemented, the well-established and tested Chronic Care Model (CCM) is shown to improve health outcomes for people with chronic conditions. Since the development of the original CCM, tremendous information management, communication, and technology advancements have been established. An opportunity exists to improve the time-honored CCM with clinically efficacious eHealth tools.
Objective
The first goal of this paper was to review research on eHealth tools that support self-management of chronic disease using the CCM. The second goal was to present a revised model, the eHealth Enhanced Chronic Care Model (eCCM), to show how eHealth tools can be used to increase efficiency of how patients manage their own chronic illnesses.
Methods
Using Theory Derivation processes, we identified a “parent theory”, the Chronic Care Model, and conducted a thorough review of the literature using CINAHL, Medline, OVID, EMBASE PsychINFO, Science Direct, as well as government reports, industry reports, legislation using search terms “CCM or Chronic Care Model” AND “eHealth” or the specific identified components of eHealth. Additionally, “Chronic Illness Self-management support” AND “Technology” AND several identified eHealth tools were also used as search terms. We then used a review of the literature and specific components of the CCM to create the eCCM.
Results
We identified 260 papers at the intersection of technology, chronic disease self-management support, the CCM, and eHealth and organized a high-quality subset (n=95) using the components of CCM, self-management support, delivery system design, clinical decision support, and clinical information systems. In general, results showed that eHealth tools make important contributions to chronic care and the CCM but that the model requires modification in several key areas. Specifically, (1) eHealth education is critical for self-care, (2) eHealth support needs to be placed within the context of community and enhanced with the benefits of the eCommunity or virtual communities, and (3) a complete feedback loop is needed to assure productive technology-based interactions between the patient and provider.
Conclusions
The revised model, eCCM, offers insight into the role of eHealth tools in self-management support for people with chronic conditions. Additional research and testing of the eCCM are the logical next steps.
Keywords: chronic disease, mobile health, eHealth, telemedicine, personal health records, social networks, education of patients
Introduction
Background
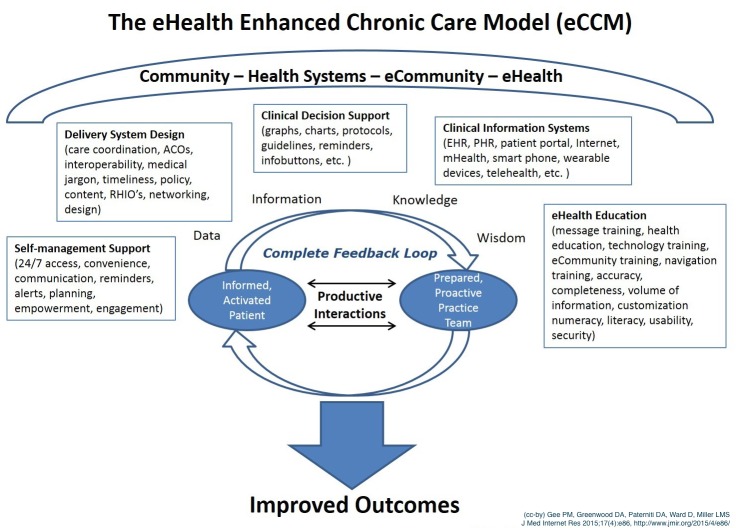
Chronic illness is a burden on individuals and society; nearly half of Americans have at least one chronic illness accounting for more than three-fourths of America’s health care spending [1,2]. The Chronic Care Model (CCM) is a well-established and validated framework that illustrates a comprehensive approach to caring for the chronically ill that supports increased functional and clinical outcomes. The model includes six key interdependent components: (1) community resources, (2) health system support, (3) self-management support, (4) delivery system design, (5) decision support, and (6) clinical information systems (Figure 1).
Figure 1.
The Chronic Care Model. Developed by the MacColl Institute, ©ACP-JSIM Journals and Books, reprinted with permission from ACP-ASIM Journals and Books.
The CCM places chronic care in the context of the community where the person will receive health care services and with the health systems involved in that care. The CCM highlights the importance of “Self-Management Support”—giving patients the knowledge, confidence, and skills for self-management of their condition. “Delivery System Design” is also important to promote a patient-centered interdisciplinary team approach to care. “Decision Support” is needed to assure providers and patients have access to the most current and relevant evidenced-based guidelines for care, Finally, the model emphasizes the role of “Clinical Information Systems” to provide access to data, information, and knowledge needed to improve health. Effective and productive patient and provider interactions are the heart of the CCM and the key to improving outcomes [3].
Over the last decade, the CCM has been implemented and evaluated in a variety of settings in both domestic and international studies. The CCM has proven to be a useful framework for patient empowerment, self-management support, and improving clinical and behavioral outcomes [4-9]. The purpose of this review is to update the CCM with emerging eHealth technologies. This goal is consistent with the self-management support for chronic disease using technology tools suggested in both the Affordable Care Act (ACA) and the Health Information Technology for Economic and Clinical Health Act (HITECH Act) [10-12].
eHealth for Chronic Illness
Leaders and policy makers on a global scale are strongly encouraging the use of eHealth technologies. Australia, Europe, South Korea, and the United States all have strong eHealth initiatives that are developing policy for using information technology to improve health and health care systems. The Washington think tank “eHealth Initiative” (promoting policy focused on research and education in eHealth), the Institute of Medicine (IOM), and the Agency for Healthcare Research and Quality (AHRQ) also recommend the use of eHealth as a tool to support self-management in chronic illness [13-15]. Large systematic reviews conducted by the AHRQ determined that eHealth tools can improve patient engagement and health outcomes, however, more research is needed [14,15]. Jimison et al [14] also identified that eHealth technology interventions must contain a closed or complete feedback loop (CFL) to have an impact on chronic illness outcomes. A complete feedback loop contains five stages: (1) transmission of data and information regarding the health status of the consumer, (2) interpretation of data and information using previously established knowledge and/or wisdom and use of evidence-based standards, (3) address the specific need of the individual consumer, (4) timely feedback to the consumer addressing their requirements, and (5) regular repetition of the feedback loop [14].
Despite the strong push for eHealth, there is no standard definition, which hinders research and implementation. Comprehensive systematic reviews have identified as many as 51 different definitions for eHealth in the literature [13,16-18]. Overall, the literature describes the definition of eHealth to be very broad and encompassing, ranging from the very business-oriented to more clinically focused. The authors of this paper have developed a definition of eHealth for chronic illness self-management: To promote positive health outcomes by using a new frame of mind that incorporates information and communication technologies in the presence of a complete feedback loop and enables the use of data and information, to generate health management knowledge and wisdom.
Previous eHealth definitions by Eysenbach and Eng, and the Informatics language from Staggers and Thompson [19-21] influenced the definition. In the literature, the components of eHealth typically consist of use of the Internet, telemedicine, and communication [16]. In the IOM report Health Literacy, eHealth, and Communication: Putting the Consumer First, the round table members noted that the eHealth Initiative was guided by Wagner’s vision of the CCM and used as the “blueprint” for eHealth to support chronic illness [13]. For enhanced use with the CCM, the authors suggest specific components highlighted in the information technology and communication literature including use of the Internet for health information, social networking, telehealth, mHealth (including wearable devices), electronic health records (EHRs), and electronic personal health records/patient portals (PHRs).
Use of the Internet for Self-Management Support
The Internet serves as a conduit for self-management support, connecting providers and consumers to secure portals, health applications, social networks, and large databases. Roughly 80% of adults have sought health information on the Internet, including 62% of adults with a chronic illness; of those, 75% of the chronically ill surveyed stated their most recent Internet encounter affected decisions about the self-management of their condition [22-24]. The Internet is also the vehicle used by many adults for access to social networking sites.
Social Networking or eHealth Communities
Social networking or virtual communities are newer components of eHealth. A recent study reported in JAMA regarding the diabetes online community (DOC), “TuDiabetes”, found that the use of the social network augmented hypoglycemia surveillance among the members of that virtual community [25]. To date, most research on the impact of social networks has been descriptive but there are a few studies that have shown improved health outcomes; no studies to date have shown adverse effects on consumers/patients [26]. One randomized controlled trial (RCT) followed overweight and sedentary adults and found that the use of an online community helped maintain adherence to the program and that the participants had lower attrition from the study [27]. In recent descriptive studies, virtual community members with diabetes and heart disease found that the environment was useful for asking questions, reporting personal experiences, and even supported eHealth literacy [28,29]. Social networking may be an effective tool to encourage consumer empowerment and promote patient-centered care [30,31].
Telehealth
One well-researched component of eHealth is in the area of telehealth, sometimes called telemedicine, which has been used extensively as an intervention across many aspects of health care. Telehealth (telecommunication, videoconferencing, remote monitoring, etc) can range from performing a detailed physical examination either synchronously or asynchronously, to using videoconferencing (audio/video technology) for the delivery of a class or training to individuals or groups in a remote setting [32,33].
The telehealth field is challenged with a clear definition. A recent study by Doarn et al [34] found there are seven United States government definitions for telemedicine. A standard definition of telehealth to facilitate the use and research eHealth tools is essential. To add strength to this movement, a federal telemedicine group was commissioned, FedTel, and legislation has recently been introduced to Congress to establish federal telehealth standards [34,35].
Telehealth has been especially effective in the management of diabetes. A recent systematic review evaluating 15 RCTs described that hemoglobin A1c (A1C), a laboratory examination that measures average blood glucose over the past 2-3 months, improved when telehealth interventions incorporated more elements of structured self-monitoring of blood glucose [33]. Telehealth also lends itself to use by all members of the health care team. In a recent RCT, Tang et al [36] found that nurse-led, multi-disciplinary telehealth interventions were effective in improving A1C outcomes. In another nurse-led telehealth intervention designed for high-risk dialysis patients, the participants reported being more empowered and better able to provide needed self-management of illness [37]. In a recent RCT, Young et al found that a telehealth nurse coaching model for people with diabetes produced higher self-efficacy scores in the control group than for those who received the usual care [38]. Health care leaders, clinicians, and policymakers view telehealth as a powerful resource for improving health outcomes, health care quality, and to promote patient engagement [15,39,40].
Mobile Health
Mobile health (mHealth) components of eHealth span a broad spectrum of technologies. mHealth includes technology that is wireless, mobile [41], or wearable (eg, sensors, medication pumps, or wristbands that monitor physical activity). mHealth also includes thousands of health apps designed for mobile devices. The market for mHealth apps is anticipated to grow 25% per year with no foreseeable end in sight [42]. mHealth is a “disruptive innovation” providing entrée to Internet-based health resources to groups who previously had barriers to these tools; 60% of Americans gain access to the Internet using a laptop, tablet computer, or mobile phone [43]. Older adults, Hispanics, and African-Americans are adopting mobile technologies at a faster rate than the general population [43]. Progress in the area of mobile phone text messaging has created a surge in using the tool for health self-management. Several recent studies and systematic reviews have reported modest health outcome improvement using text messaging as a targeted intervention [44-46].
Electronic Health Records/Personal Health Records (EHR/PHR)
The EHR is an electronic longitudinal record of care and patient information that may be shared across multiple health care settings [47]. The tethered PHR, or patient portal, is a component of the EHR that communicates with the provider’s EHR or is integrated within the provider’s EHR and provides access to health records for patients/consumers and/or caregivers. The Markle Foundation [48] defined the PHR as “an electronic application through which individuals can access, manage and share their health information, and that of others for whom they are authorized in a private, secure and confidential environment” (p. 14)(Markle Foundation, 2008)(Markle Foundation, 2008).
Health care leaders and policy makers highly recommend PHR use as a management tool for chronic illness [49-52]. However, the PHR literature including systematic reviews related to use and health outcomes were inconclusive and the few RTCs conducted on PHR interventions failed to make the case for efficacy [53]. While the scientific evidence does not demonstrate that using PHRs can improve health outcomes, the literature does support the impact on secondary outcomes related to self-management support [36]. In an observational cohort study of 8705 subjects, Sarkar et al [54] found that patients with diabetes who use the PHR to refill their prescriptions had better medication adherence. In spite of some demonstration for the efficacy of PHRs in optimizing care, the PHR literature, including systematic reviews related to use and health outcomes, has been inconclusive [53,55].
With the national and international push to implement eHealth technologies into the current care environment, there is an opportunity to augment the established CCM with integration of eHealth technology components. The remainder of this paper will describe how adding eHealth components to the CCM may provide more self-management tools for the person with chronic illness.
Methods
Theory Derivation
The Theory Derivation process was used to bring together the related eHealth concepts and to grasp the relatively new phenomenon of using eHealth tools for the self-management of chronic illness [56]. Theory derivation is a structured set of procedures where one chooses a parent theory or model that is used to guide the development of a new model or theory supported by a comprehensive understanding of the current literature [56]. In this paper, the CCM was carefully examined and supporting components were extrapolated for the development of a new model. Additionally, a methodical review of a wide range of literature was conducted. A draft framework was then developed and expanded by a continued review of new literature and evaluation of the established and new components of the revised model.
A thorough review of the published literature since 2000 was conducted using CINAHL, Medline, OVID, EMBASE, PsychINFO, Science Direct, and selected “grey” literature including government reports, industry reports, legislation, etc. The review involved using the search terms “CCM or Chronic Care Model” AND “eHealth” and then we searched the specific identified components of eHealth and Chronic disease self-management support (Virtual communities”, “Virtual health communities”, “e-Communities”, “on-line communities”, social networking”, “Telemedicine”, Telehealth”, “Internet use for health”, “mHealth”, “Electronic health records”, “Personal health records”, “Patient portals”, “User training”, “Technology”, “Chronic Illness”, “Chronic disease”, and “Self-management support”). Selection criteria included review papers, randomized controlled trials, cohort studies, cross-sectional studies, and qualitative studies. The researchers independently identified papers based on framework, design, sample, measures, and fit with self-management support and chronic illness. The CCM was carefully studied in the literature and then key components of the current CCM were used to provide a framework for new model construction.
Results
Summary
We identified 260 papers, but excluded 63.5% (165/260) due to concerns about study design, sample size, and/or methods. Overall, with the exception of telehealth interventions, there was a noted heterogeneity of methods and approaches used. We organized the literature into the components of the CCM, highlighting the role that eHealth tools and concepts can play in each component, modifying and adding components where needed to capture the emerging eHealth literature.
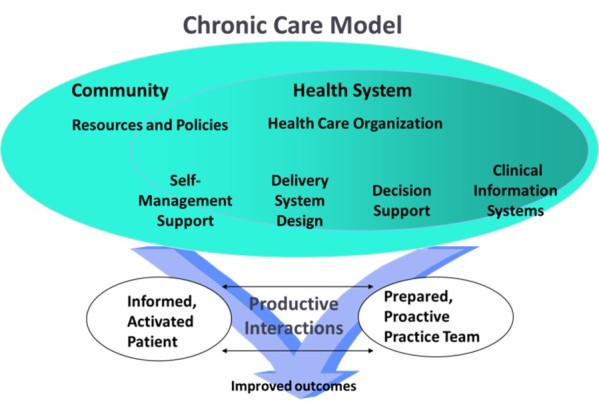
Adding the eCommunity and an Informatics Framework
The CCM has two major components: Community and Health Systems (Figure 1). The role of the community in the CCM is to provide support for patient engagement or activation and for self-management [57]. Based on the literature, the notion of community should be expanded to include online community and health-related social networks, or eCommunity (Figure 2). A total of 72% of American adults who use the Internet are already using social networks [58]. In a recent PEW poll, 26% of respondents stated they went online to observe the health postings about someone else’s medical condition and 16% search the Internet to find another person with the same health ailment [59,60]. Hu, Bell, Kravitz and Orrange [61] found that in a survey of 505 participants in an online support group the adult members accessed the group to prepare for upcoming medical appointments.Virtual communities including “TuDiabetes” or “PatientsLikeMe” are already supporting thousands of chronically ill adults; both groups have vigorous research activities [25,62]. Health care technology leaders and policy makers are touting a new PHR 2.0 with expected growth of 221% over the next 3 years [63]. The concept of PHR 2.0 will contain the typical components of the current PHR/patient portal systems but add social networking, gaming, and e-visits [63].
Figure 2.
The eHealth Enhanced Chronic Care Model. Created by Gee, P M; Greenwood, D A; Paterniti, D A; Ward, D; and Miller, L M S (JMIR, 2015). Adapted from The Chronic Care Model (see Figure 1).
Chronically ill adults who are activated, educated, engaged, and empowered, or e-patients, are already using eHealth tools [64,65]. E-patients, together with their providers, community, and social networks, have the ability to generate a collective knowledge and wisdom about their health care self-management needs greater than any of them working alone [65,66]. Figure 2, the eHealth enhanced CCM, contains the terms data, information, knowledge, and wisdom (DIKW). These words illustrate that the DIKW framework is underpinning the process of data and information used to create new knowledge and ultimately the collective wisdom to improve health outcomes [65,66].
Health Systems Enhancements
In the literature, it was noted that the health system must be designed to support organizations and providers and enable them to be prepared and proactive and to foster productive interactions with consumers; this is essential to improve health outcomes [67]. Kaiser Permanente and the Veterans Health Administration have made strategic efforts to implement eHealth technologies (PHRs, mHealth, telehealth, and Internet use) to improve access to care, reduce costs, and empower patients [68-71]. Between 2003 and 2010, Kaiser Permanente designed a system where patients could better manage their own health using a PHR [69,72]. Research at Kaiser showed a 25.3% reduction in the number of face-to-face office visits in primary care due to PHR use [73]. These findings suggest that health systems who consciously implement and encourage the use of eHealth technologies may achieve a higher level of patient engagement, satisfaction, and self-management support.
Delivery System Design Enhancements
“Meaningful Use” requires redesign of health care delivery systems to meet the emerging eHealth technologies to be implemented nation-wide. Meaningful Use Requirements state that providers are eligible for up to a US $44,000 payment from the centers of Medicare and Medicaid Services to implement provider electronic health record systems [10,74]. Stage II Meaningful Use further requires that providers and health care organizations implement a patient/provider communication portal system by 2014.
Access to and control over personal health data is a theme described by some health care consumers. This is an instance where the literature identified policy change and interoperability—the exchanging of data and information electronically between health care systems—as needed to provide the consumer more autonomy over their health data and information [75-77]. Access and control over personal health data are concepts similar to the “environmental factors” described by Tang and colleagues in their influential foundational PHR article [50]. Interoperability, lack of resources at the provider level, and PHR design and policy issues are factors outside the control of the individual participant and currently under the control of the provider or health care system. First, the decision makers in health systems or delivery systems should create policies to facilitate the correction of incorrect or missing data in the PHR. These policies would empower patients to work with their providers to assure the patient record is correct and current. Some health care organizations have had positive experiences with open access for consumers to the entire EHR/PHR including the provider notes [78]. Again, this is a policy issue that may promote productive interactions, engagement, and mutual trust.
Health system leaders can improve access issues for consumers by promoting policies that will encourage providers to release results sooner. Meaningful Use policy is currently encouraging more implementation of EHR/PHRs. Health care leaders are working on integration and interoperability of these records across health care systems and among individual providers [79].
Self-Management Support Enhancements
A review of the literature helped the authors to identify the core ideas of patient engagement and health self-management, empowered individuals, and the tools and knowledge to impact their own health. Research on PHRs shows improved patient engagement essential for self-management support [80]. The PHR encouraged engagement by facilitating preparation for appointments, tracking of laboratory results and diagnostic studies, encouraging involvement in preventive care and screening, and encouraging consumers to suggest a course of treatment with their providers [81,82].
The informed, “activated” patient is a key component of the CCM. Patient activation is the level of skills, knowledge, and confidence a person has in managing one’s own chronic illness [83]. The highly activated patient therefore is engaged, informed, and confident in their ability to self-manage their own condition [84]. Hibbard, Stockard, Mahoney, Tusler [85] developed a Patient Activation Measure (PAM) to determine the levels of patient activation. The use of a PHR can increase patient activation. An RCT of patients assigned a PHR as an intervention resulted in higher PAM scores compared to the control group, especially with those who started with lower scores [86]. Additional eHealth components such as telehealth and mHealth applications may also be useful in self-management support and to promote patient engagement [33,87]. The findings suggest that the use of a PHR can promote an informed, activated patient and augment the CCM in the areas of self-management support and productive interactions.
Clinical Decision Support Enhancements
Originally, the CCM identified clinical decision support (CDS) as a method to assure providers had access to the most current evidence-based clinical guidelines, protocols, and standard of care [67]. A study of the literature suggests the eCCM component of CDS should incorporate patient/consumer specific needs as follows: (1) visual access to data, (2) access to protocols, (3) care standards and evidence for self-management, (4) info buttons that access clinical guidelines, and (5) reminders for both the patients and providers. An RCT by Holbrook et al [88] found that people with type 2 diabetes had better outcomes when their intervention included a Web-based clinical decision support system shared by the patient and provider. Fox [22,23] found that chronically ill adults frequently go online to health sites to help make decisions about self-management of their condition. The Institute of Medicine [13,89,90] in three separate reports recommends incorporating eHealth tools for the promotion of CDS for both patients and providers to improve safety and self-management support.
Clinical Information Systems Enhancements
Originally, the clinical information systems (CIS) element of the CCM primarily focused on registries, databases, and systems in place to support the access to protocols and current standards of care. With rapid expansion of the eHealth components of the EHR/PHR, partially due to Meaningful Use implementations, the opportunity exists to engage with and evaluate these tools as part of the CCM. In 2001, 18% of provider offices had implemented EHRs; that number is up to 78% as of 2013 and about half of those implementations are meeting the Meaningful Use criteria [91]. Tethered patient portals/PHRs are part of the Meaningful Use stage II requirements and are dependent on EHR implementations to be a useful part of the enhanced CCM [50]. Other eHealth components such as telehealth and mobile devices are also on the rise. The inclusion of such tools in the CCM as part of the CIS element is a logical next step and one that has been proven to improve health outcomes [14]. Like the growth of PHRs, mHealth apps and mobile phones are expected to grow at a rate of 47.6% over the next six years [92].
Addition of eHealth Education to the CCM
Based on findings in the literature, an additional suggested major enhancement to the CCM is the addition of the support element “eHealth Education” (Figure 2). With health systems offering eHealth tools and consumers seeking eHealth solutions, providing the chronically ill adult with eHealth skills is needed [13]. Health literacy is essential for eHealth. Low health literacy is a long-standing problem in the current health care system [13]; 90 million Americans have poor health literacy—trouble understanding and managing their own health [93]. In a systematic review of eHealth interventions, Jacobs et al (2014) found that it is feasible to use eHealth tools to improve overall health literacy. Older adults make up the vast majority of those with chronic illness. And, while older adults are increasing their use of the Internet, social networking, and mobile phones, there is a gap in the literature in the evaluation of eHealth literacy for the older adult [94]. Choi and DiNitto studied older adults who are home-bound or poor and found opportunities for providing equipment and training that may improve eHealth literacy [95].
One component of health literacy that is problematic for many is health numeracy—people’s ability to understand numbers and mathematical principles in the management of their health care [96]. Findings by Lipkus, Samsa, and Rimer [97] also noted that highly educated individuals had numeracy problems. To compound this issue, eHealth tools give patients even more access to data, information, and knowledge that may be confusing. eHealth is changing so rapidly that researchers are recommending we re-assess how we should measure eHealth literacy including its numeracy component [98].
Training for both consumers and providers in how to construct and send Web-based and text messages that promote productive interactions may prove useful. Training on the selection and use of health-related websites may also prove useful. Adults are already using the Web to look for health information on the Internet and were not informed on how to identify who is providing the information and how to assess the quality of the information [99,100]. With the rapid expansion of mHealth apps for mobile phones, training on how to choose apps that can promote health outcomes may be needed for both patients and providers [101,102].
Training in eHealth is proven to increase confidence and self-efficacy in using the tools but training lags behind in the roll-out of new technologies to the general public [15,103]. In fact in telehealth applications, the lack of training was reported frequently as a barrier to use [15]. In a mixed-methods study, low-income patients with human immunodeficiency virus (HIV) who were trained to use the PHR had better self-efficacy, patient activation, and disease knowledge at follow-up [104]. To promote productive interactions between the informed, activated patient and the prepared, proactive practice team, the authors of this paper would also recommend provider team training in the use of eHealth tools. In a study involving randomly assigned group practices, the providers trained to use the eHealth tools had measurable changes in the effectiveness of their information management skills [105]. Training for both consumers and providers may improve the efficacy of the use of eHealth tools and should be considered in future research.
Communication and the Addition of the Complete Feedback Loop (CFL)
Findings in the literature show that interventions that include the complete feedback loop are required for technology to promote improved health status in the chronically ill [14]. A key factor in the CCM is productive interactions between patients and providers. The activated patient is best suited to participate in the cooperative effort. In a qualitative study among chronically ill patients with a variety of levels of patient activation, it was found that being in control and working in a cooperative partnership with the provider was consistent with those patients who had the highest PAM scores [84]. This finding is similar with Yellowlees’ [106] definition of “mutual participation” where patients work in an equal, trusting, and cooperative manner using the Internet to facilitate communication (p. 117). The secure patient-provider email messaging portal in a PHR is an area where this mutual participation and cooperation will occur. A cross-sectional study found that patients who were working cooperatively with their providers and setting very specific and concrete goals and focusing on self-monitoring had much higher PAM scores [107]. The PHR, mobile devices, and text messaging are eHealth tools that can give consumers control over the timing and content of their messages.
Provider response times to messaging are very important to patients [108,109] and can negatively affect CFL communication cycle. Patient satisfaction with provider response times to patient messages and requests have been studied. One study noted that patient satisfaction using a patient portal email system is positively affected by shorter message response times [108]. Reti et al found that response times varied across health care organizations and that usual patient portal email messaging response times varied from 24 to 72 hours [110]. With the importance of the CFL for self-management support and productive interactions, we recommend enhancing the CCM with the formal insertion of the CFL into the model. Perhaps the visual representation of the CFL in the model surrounding the productive interactions will remind researchers and developers of eHealth tools they need to include this element into their interventions and research (see Figure 2).
Discussion
Principal Findings
The purpose of this paper was to use Theory Derivation process to review the chronic care and eHealth literature and to articulate how the CCM could be expanded to include eHealth tools. The research is clear in showing that eHealth technologies related to a variety chronic conditions can be used to enhance self-management and revise the CCM [87,111]. The evidence also suggests that eHealth tools can support productive patient-provider interactions and improve health outcomes [112,113].
This review and model development highlights several gaps in the literature. First, clear definitions for eHealth, telehealth, and PHRs are needed to move forward in formulating appropriate research questions. Second, a gap in the literature exists in the efficacy of using online health communities for self-management support. While social support itself is shown to improve engagement and health outcomes with adults who have chronic illness [114,115], little is known about whether social support offered in online health communities has the same effect. A review of the literature and research in this area are needed. Third, research findings where elements of the CCM were used in conjunction with the CFL need to be identified and evaluated. Jimison et al (2008) identified that eHealth interventions that included the CFL improved outcomes [14]. Greenwood, Young, and Quinn found that telehealth interventions for people with diabetes is the kind of eHealth intervention that can foster a CFL [33]. The CFL as it relates to eHealth interventions is an important component to assure the success of eHealth interventions and will require future research [14]. Last, health education and technology experts are needed to develop a curriculum to train patients/consumers to use the eHealth tools that have been shown to improve health outcomes for the chronically ill person. Additionally, health care providers will need training on how to implement eHealth interventions and how to educate their chronically ill patients to use these tools.
Limitations
Limitations of this Theory Derivation process started with the fact that an exhaustive literature review was not completed for each of the eHealth components or the new elements added to the eCCM. Additionally, new and important literature is being added daily and with the scope of this project being so large, focused attention to the new knowledge was difficult to track. The opportunity exists for researchers to now concentrate on systematic reviews of the literature and conduct research specifically focusing on the individual components of the new eCCM model.
Conclusion
In conclusion, there is strong evidence demonstrating that eHealth tools can strengthen and enhance the already successful CCM. Research to explicitly test the new eCCM and its components is the logical next step.
Acknowledgments
The authors would like to thank Dr Robert Bell for his assistance in providing knowledge and literature supporting patient-provider communication. We would also like to thank the Gordon and Betty Moore Foundation for their generous support of the Betty Irene Moore School of Nursing at the University of California, Davis.
Abbreviations
- A1C
hemoglobin A1C
- ACA
Affordable Care Act
- AHRQ
Agency for Healthcare Research and Quality
- CCM
Chronic Care Model
- CDS
clinical decision support
- CFL
complete feedback loop
- CIS
clinical information system
- DIKW
Data, Information, Knowledge and Wisdom Model
- DOC
diabetes online community
- eCCM
eHealth Enhanced Chronic Care Model
- EHR
electronic health record
- HITECH
Health Information Technology for Economic and Clinical Health Act
- HIV
human immunodeficiency virus
- IOM
Institute of Medicine
- PAM
patient activation measure
- PHR
electronic patient health record/patient portal
- RCT
randomized controlled trial
Footnotes
Authors' Contributions: PG conceptualized the project, reviewed the literature, constructed the initial eCCM, and prepared the manuscript drafts. DG offered exceptional knowledge of eHealth, the CCM, and self-management support for persons with chronic illness and assisted in project design. DP assisted with concept and model and development and understanding the needs of the patient. DW assisted with her vast nursing knowledge and wisdom, and her expertise in the area of health policy. LM offered her knowledge of the needs of the older adult, and human and cognitive factors related to the use of technology, health literacy, and with project design and drafting and revising parts of the manuscript.
Conflicts of Interest: None declared.
References
- 1.Ward BW, Schiller JS, Goodman RA. Multiple chronic conditions among US adults: A 2012 update. Preventing chronic disease. 2014;11(130389):1–4. doi: 10.5888/pcd11.130389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hoyert DL, Xi J. Deaths: Preliminary data for 2011. Hayattsville, MD: National Center for Health Statistics; 2012. [2015-03-24]. http://www.cdc.gov/nchs/data/nvsr/nvsr61/nvsr61_06.pdf. [PubMed] [Google Scholar]
- 3.Wagner E H. Chronic disease management: what will it take to improve care for chronic illness? Eff Clin Pract. 1998;1(1):2–4. http://www.acponline.org/journals/ecp/augsep98/cdm.htm. [PubMed] [Google Scholar]
- 4.Piatt GA, Orchard TJ, Emerson S, Simmons D, Songer TJ, Brooks MM, Korytkowski M, Siminerio LM, Ahmad U, Zgibor JC. Translating the chronic care model into the community: results from a randomized controlled trial of a multifaceted diabetes care intervention. Diabetes Care. 2006 Apr;29(4):811–7. doi: 10.2337/diacare.29.04.06.dc05-1785. [DOI] [PubMed] [Google Scholar]
- 5.Coleman Katie, Austin Brian T, Brach Cindy, Wagner Edward H. Evidence on the Chronic Care Model in the new millennium. Health Aff (Millwood) 2009;28(1):75–85. doi: 10.1377/hlthaff.28.1.75. http://content.healthaffairs.org/cgi/pmidlookup?view=long&pmid=19124857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tsai Alexander C, Morton Sally C, Mangione Carol M, Keeler Emmett B. A meta-analysis of interventions to improve care for chronic illnesses. Am J Manag Care. 2005 Aug;11(8):478–88. http://www.ajmc.com/pubMed.php?pii=2921. [PMC free article] [PubMed] [Google Scholar]
- 7.Siminerio Linda M, Piatt Gretchen, Zgibor Janice C. Implementing the chronic care model for improvements in diabetes care and education in a rural primary care practice. Diabetes Educ. 2005;31(2):225–34. doi: 10.1177/0145721705275325. [DOI] [PubMed] [Google Scholar]
- 8.Siminerio Linda M, Piatt Gretchen A, Emerson Sharlene, Ruppert Kristine, Saul Melissa, Solano Francis, Stewart Andrew, Zgibor Janice C. Deploying the chronic care model to implement and sustain diabetes self-management training programs. Diabetes Educ. 2006;32(2):253–60. doi: 10.1177/0145721706287156. [DOI] [PubMed] [Google Scholar]
- 9.Stellefson Michael, Dipnarine Krishna, Stopka Christine. The chronic care model and diabetes management in US primary care settings: a systematic review. Prev Chronic Dis. 2013;10:E26. doi: 10.5888/pcd10.120180. http://www.cdc.gov/pcd/issues/2013/12_0180.htm. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Blumenthal David. Implementation of the federal health information technology initiative. N Engl J Med. 2011 Dec 22;365(25):2426–31. doi: 10.1056/NEJMsr1112158. [DOI] [PubMed] [Google Scholar]
- 11.Blumenthal David, Tavenner Marilyn. The meaningful use regulation for electronic health records. N Engl J Med. 2010 Aug 5;363(6):501–4. doi: 10.1056/NEJMp1006114. [DOI] [PubMed] [Google Scholar]
- 12.Patient Protection and Affordable Care Act, 42 U.S.C. § 18001 et seq. 2010. [2015-03-25]. http://www.ihs.gov/ihcia/documents/home/PL111_148_PPACA.pdf.
- 13.Institute of Medicine . Health literacy, eHealth, and communication: Putting the consumer first: Workshop summary. Washington, DC: The National Academies Press; 2009. [PubMed] [Google Scholar]
- 14.Jimison H, Gorman P, Woods S. Barriers and drivers of health information technology use for the elderly, chronically ill, and underserved: Evidence report/technology assessment No. Rockville, MD: Agency for Healthcare Research and Quality; 2008. pp. 09–E004. [PMC free article] [PubMed] [Google Scholar]
- 15.Finkelstein J, Knight A, Marinopoulos S, Gibbons MC, Berger Z, Aboumater H, Wilson RF, Lau BD, Sharma R, Bass EB. Enabling patient-centered care through health information technology: Evidence report/technology assessment No. Rockville, MD: Agency for Healthcare Research and Quality; 2012. pp. 12–E005. [PMC free article] [PubMed] [Google Scholar]
- 16.Oh H, Rizo C, Enkin M, Jadad A. What is eHealth (3): a systematic review of published definitions. J Med Internet Res. 2005;7(1):e1. doi: 10.2196/jmir.7.1.e1. http://www.jmir.org/2005/1/e1/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pagliari Claudia, Sloan D, Gregor P, Sullivan Frank, Detmer Don, Kahan James P, Oortwijn Wija, MacGillivray Steve. What is eHealth (4): a scoping exercise to map the field. J Med Internet Res. 2005;7(1):e9. doi: 10.2196/jmir.7.1.e9. http://www.jmir.org/2005/1/e9/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Showell C, Nohr C. How should we define eHealth, does the definition matter?. Quality of Life thrugh Quality of Information; August 26-29, 2012; Pisa, IT. 2012. [Google Scholar]
- 19.Staggers Nancy, Thompson Cheryl Bagley. The evolution of definitions for nursing informatics: a critical analysis and revised definition. J Am Med Inform Assoc. 2002;9(3):255–61. doi: 10.1197/jamia.M0946. http://jamia.oxfordjournals.org/lookup/pmidlookup?view=long&pmid=11971886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Eysenbach G. What is e-health? J Med Internet Res. 2001;3(2):E20. doi: 10.2196/jmir.3.2.e20. http://www.jmir.org/2001/2/e20/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Eng Thomas R. Population health technologies: emerging innovations for the health of the public. Am J Prev Med. 2004 Apr;26(3):237–42. doi: 10.1016/j.amepre.2003.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fox S. Online health search 2006. Washington, DC: Pew Internet and American Life Project; 2006. [2015-03-24]. http://www.pewinternet.org/files/old-media/Files/Reports/2006/PIP_Online_Health_2006.pdf.pdf. [Google Scholar]
- 23.Fox S. E-patients with a disability or chronic disease. Washington, DC: Pew Internet and American Life Project; 2007. [2015-03-24]. http://www.pewinternet.org/2007/10/08/e-patients-with-a-disability-or-chronic-disease/ [Google Scholar]
- 24.Fox S, Purchell K. Chronic disease and the Internet. Washington, DC: Pew Internet and American Life Project; 2010. [2015-03-24]. http://www.pewinternet.org/2010/03/24/chronic-disease-and-the-internet/ [Google Scholar]
- 25.Weitzman Elissa R, Kelemen Skyler, Quinn Maryanne, Eggleston Emma M, Mandl Kenneth D. Participatory surveillance of hypoglycemia and harms in an online social network. JAMA Intern Med. 2013 Mar 11;173(5):345–51. doi: 10.1001/jamainternmed.2013.2512. [DOI] [PubMed] [Google Scholar]
- 26.Merolli Mark, Gray Kathleen, Martin-Sanchez Fernando. Health outcomes and related effects of using social media in chronic disease management: a literature review and analysis of affordances. J Biomed Inform. 2013 Dec;46(6):957–69. doi: 10.1016/j.jbi.2013.04.010. http://linkinghub.elsevier.com/retrieve/pii/S1532-0464(13)00067-1. [DOI] [PubMed] [Google Scholar]
- 27.Richardson Caroline R, Buis Lorraine R, Janney Adrienne W, Goodrich David E, Sen Ananda, Hess Michael L, Mehari Kathleen S, Fortlage Laurie A, Resnick Paul J, Zikmund-Fisher Brian J, Strecher Victor J, Piette John D. An online community improves adherence in an internet-mediated walking program. Part 1: results of a randomized controlled trial. J Med Internet Res. 2010;12(4):e71. doi: 10.2196/jmir.1338. http://www.jmir.org/2010/4/e71/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Greene Jeremy A, Choudhry Niteesh K, Kilabuk Elaine, Shrank William H. Online social networking by patients with diabetes: a qualitative evaluation of communication with Facebook. J Gen Intern Med. 2011 Mar;26(3):287–92. doi: 10.1007/s11606-010-1526-3. http://europepmc.org/abstract/MED/20945113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jorgensen CB, Hansen J, Spindler H, Andreasen JJ, Nielsen G, Dinesen B. Heart patients' experiences and use of social media in their rehabilitation: A qualitative study. Scandinavian Conference on Health Informatics; August 20, 2013; Copenhagen, Denmark. 2013. [Google Scholar]
- 30.Lober William B, Flowers Janine L. Consumer empowerment in health care amid the internet and social media. Semin Oncol Nurs. 2011 Aug;27(3):169–82. doi: 10.1016/j.soncn.2011.04.002. [DOI] [PubMed] [Google Scholar]
- 31.Moorhead S Anne, Hazlett Diane E, Harrison Laura, Carroll Jennifer K, Irwin Anthea, Hoving Ciska. A new dimension of health care: systematic review of the uses, benefits, and limitations of social media for health communication. J Med Internet Res. 2013;15(4):e85. doi: 10.2196/jmir.1933. http://www.jmir.org/2013/4/e85/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.American Telemedicine Association. 2014. [2015-03-24]. What is Telemedicine? http://www.americantelemed.org/about-telemedicine/what-is-telemedicine.
- 33.Greenwood DA, Young HM, Quinn CC. Telehealth remote monitoring systematic review: structured self-monitoring of blood glucose and impact on A1C. J Diabetes Sci Technol. 2014 Feb 21;8(2):378–389. doi: 10.1177/1932296813519311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Doarn CR, Pruitt S, Jacobs J, Harris Y, Bott DM, Riley W, Lamer C, Oliver AL. Federal efforts to define and advance telehealth--a work in progress. Telemed J E Health. 2014 May;20(5):409–18. doi: 10.1089/tmj.2013.0336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Matsui D. Telehealth Modernization Act of 2013. 2013. [2015-03-24]. https://www.govtrack.us/congress/bills/113/hr3750/text.
- 36.Tang Paul C, Overhage J Marc, Chan Albert Solomon, Brown Nancy L, Aghighi Bahar, Entwistle Martin P, Hui Siu Lui, Hyde Shauna M, Klieman Linda H, Mitchell Charlotte J, Perkins Anthony J, Qureshi Lubna S, Waltimyer Tanya A, Winters Leigha J, Young Charles Y. Online disease management of diabetes: engaging and motivating patients online with enhanced resources-diabetes (EMPOWER-D), a randomized controlled trial. J Am Med Inform Assoc. 2013 May 1;20(3):526–34. doi: 10.1136/amiajnl-2012-001263. http://jamia.oxfordjournals.org/lookup/pmidlookup?view=long&pmid=23171659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Minatodani Dayna E, Chao Puihan J, Berman Steven J. Home telehealth: facilitators, barriers, and impact of nurse support among high-risk dialysis patients. Telemed J E Health. 2013 Aug;19(8):573–8. doi: 10.1089/tmj.2012.0201. [DOI] [PubMed] [Google Scholar]
- 38.Young Heather, Miyamoto Sheridan, Ward Deborah, Dharmar Madan, Tang-Feldman Yajarayma, Berglund Lars. Sustained effects of a nurse coaching intervention via telehealth to improve health behavior change in diabetes. Telemed J E Health. 2014 Sep;20(9):828–34. doi: 10.1089/tmj.2013.0326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Computer Sciences Corporation . Telemedicine: An essential technology for reformed healthcare. Falls Church, VA: Computer Sciences Corporation; 2011. [2015-03-24]. http://www.gatelehealth.org/wp-content/uploads/2011/06/Telemedicine_An_Essential_Technology_for_Reformed_Healthcare.pdf. [Google Scholar]
- 40.Institute of Medicine . Fostering independence, participation, and health aging through technology: Workshop summary. Washington, DC: The National Academies Press; 2013. [PubMed] [Google Scholar]
- 41.US Department of Health and Human Services Using health text messages to improve consumer health knowledge, behaviors, and outcomes: an environmental scan. 2014. [2015-03-24]. http://www.hrsa.gov/healthit/txt4tots/environmentalscan.pdf.
- 42.Borel B. Health policy brief: mHealth and FDA guidance. 2013. [2015-03-24]. http://healthaffairs.org/healthpolicybriefs/brief_pdfs/healthpolicybrief_104.pdf.
- 43.Smith A. Mobile access 2010. Washington, DC: Pew Internet & American Life Project; 2010. [2015-03-24]. http://www.pewinternet.org/2010/07/07/mobile-access-2010/ [Google Scholar]
- 44.de Jongh T, Gurol-Uranci I, Vodopivec-Jamsek V, Car J, Atun R. Mobile phone messaging for facilitating self-management of long-term illness. Cochrane Database of Systematic Reviews. 2012;12(CD007459):1–40. doi: 10.1002/14651858.CD007459.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Siopis G, Chey T, Allman-Farinelli M. A systematic review and meta-analysis of interventions for weight management using text messaging. J Hum Nutr Diet. 2015 Feb;28 Suppl 2:1–15. doi: 10.1111/jhn.12207. [DOI] [PubMed] [Google Scholar]
- 46.Nundy Shantanu, Razi Rabia R, Dick Jonathan J, Smith Bryan, Mayo Ainoa, O'Connor Anne, Meltzer David O. A text messaging intervention to improve heart failure self-management after hospital discharge in a largely African-American population: before-after study. J Med Internet Res. 2013;15(3):e53. doi: 10.2196/jmir.2317. http://www.jmir.org/2013/3/e53/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Healthcare Information and Management Systems Society Electronic health records. 2014. [2015-03-24]. http://www.himss.org/library/ehr/?navItemNumber=13261.
- 48.Markle Foundation The personal health working group: Final report. 2003. [2015-03-24]. http://www.markle.org/publications/1429-personal-health-working-group-final-report.
- 49.Ball Marion J, Smith Carla, Bakalar Richard S. Personal health records: empowering consumers. J Healthc Inf Manag. 2007;21(1):76–86. [PubMed] [Google Scholar]
- 50.Tang Paul C, Ash Joan S, Bates David W, Overhage J Marc, Sands Daniel Z. Personal health records: definitions, benefits, and strategies for overcoming barriers to adoption. J Am Med Inform Assoc. 2006;13(2):121–6. doi: 10.1197/jamia.M2025. http://jamia.oxfordjournals.org/lookup/pmidlookup?view=long&pmid=16357345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kaelber David C, Jha Ashish K, Johnston Douglas, Middleton Blackford, Bates David W. A research agenda for personal health records (PHRs) J Am Med Inform Assoc. 2008;15(6):729–36. doi: 10.1197/jamia.M2547. http://jamia.oxfordjournals.org/lookup/pmidlookup?view=long&pmid=18756002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tang Paul C, Lansky David. The missing link: bridging the patient-provider health information gap. Health Aff (Millwood) 2005;24(5):1290–5. doi: 10.1377/hlthaff.24.5.1290. http://content.healthaffairs.org/cgi/pmidlookup?view=long&pmid=16162575. [DOI] [PubMed] [Google Scholar]
- 53.Goldzweig CL, Orshansky G, Paige Neil M, Towfigh Ali Alexander, Haggstrom David A, Miake-Lye Isomi, Beroes Jessica M, Shekelle Paul G. Electronic patient portals: evidence on health outcomes, satisfaction, efficiency, and attitudes: a systematic review. Ann Intern Med. 2013 Nov 19;159(10):677–87. doi: 10.7326/0003-4819-159-10-201311190-00006. [DOI] [PubMed] [Google Scholar]
- 54.Sarkar Urmimala, Lyles Courtney R, Parker Melissa M, Allen Jill, Nguyen Robert, Moffet Howard H, Schillinger Dean, Karter Andrew J. Use of the refill function through an online patient portal is associated with improved adherence to statins in an integrated health system. Med Care. 2014 Mar;52(3):194–201. doi: 10.1097/MLR.0000000000000069. http://europepmc.org/abstract/MED/24374412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Saparova D. Motivating, influencing, and persuading patients through personal health records: a scoping review. Perspect Health Inf Manag. 2012;9:1f. http://europepmc.org/abstract/MED/22783154. [PMC free article] [PubMed] [Google Scholar]
- 56.Walker LO, Avant KC. Theory Derivation. Strategies for Theory Construction in Nursing. Boston, MA: Prentice Hall; 2011. [Google Scholar]
- 57.Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: translating evidence into action. Health Aff (Millwood) 2001;20(6):64–78. doi: 10.1377/hlthaff.20.6.64. http://content.healthaffairs.org/cgi/pmidlookup?view=long&pmid=11816692. [DOI] [PubMed] [Google Scholar]
- 58.Duggan M, Smith A. Social media update. Washington, DC: Pew Research Center; 2013. [2015-03-24]. http://www.pewinternet.org/2013/12/30/social-media-update-2013/ [Google Scholar]
- 59.Fox S, Duggan M. Health online 2013. Washington, DC: Pew Internet & American Life Project; 2013. [2015-03-24]. http://www.pewinternet.org/2013/01/15/health-online-2013/ [Google Scholar]
- 60.Fox S. The social life of health information. Washington, DC: Pew Research Center; 2011. [2015-03-24]. http://www.pewinternet.org/2011/05/12/the-social-life-of-health-information-2011/ [Google Scholar]
- 61.Hu X, Bell RA, Kravitz RL, Orrange S. The prepared patient: information seeking of online support group members before their medical appointments. J Health Commun. 2012;17(8):960–78. doi: 10.1080/10810730.2011.650828. [DOI] [PubMed] [Google Scholar]
- 62.Bove Riley, Secor Elizabeth, Healy Brian C, Musallam Alexander, Vaughan Timothy, Glanz Bonnie I, Greeke Emily, Weiner Howard L, Chitnis Tanuja, Wicks Paul, De Jager Philip L. Evaluation of an online platform for multiple sclerosis research: patient description, validation of severity scale, and exploration of BMI effects on disease course. PLoS One. 2013;8(3):e59707. doi: 10.1371/journal.pone.0059707. http://dx.plos.org/10.1371/journal.pone.0059707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Market disruption imminent as hospitals and physicians aggressively adopt patient portal technology. Frost & Sullivan; 2013. [2015-03-24]. http://www.frost.com/prod/servlet/press-release.pag?docid=285477570. [Google Scholar]
- 64.Ferguson Tom, Frydman Gilles. The first generation of e-patients. BMJ. 2004 May 15;328(7449):1148–9. doi: 10.1136/bmj.328.7449.1148. http://europepmc.org/abstract/MED/15142894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gee PM, Greenwood DA, Kim KK, Perez SL, Staggers N, DeVon Holli A. Exploration of the e-patient phenomenon in nursing informatics. Nurs Outlook. 2012;60(4):e9–16. doi: 10.1016/j.outlook.2011.11.005. [DOI] [PubMed] [Google Scholar]
- 66.Matney Susan, Brewster Philip J, Sward Katherine A, Cloyes Kristin G, Staggers Nancy. Philosophical approaches to the nursing informatics data-information-knowledge-wisdom framework. ANS Adv Nurs Sci. 2011;34(1):6–18. doi: 10.1097/ANS.0b013e3182071813. [DOI] [PubMed] [Google Scholar]
- 67.Bodenheimer Thomas, Wagner Edward H, Grumbach Kevin. Improving primary care for patients with chronic illness: the chronic care model, Part 2. JAMA. 2002 Oct 16;288(15):1909–14. doi: 10.1001/jama.288.15.1909. [DOI] [PubMed] [Google Scholar]
- 68.Pearl Robert. Kaiser Permanente Northern California: current experiences with internet, mobile, and video technologies. Health Aff (Millwood) 2014 Feb;33(2):251–7. doi: 10.1377/hlthaff.2013.1005. [DOI] [PubMed] [Google Scholar]
- 69.Christensen K, Silvestre A. Making health personal. In: Liang L, editor. Connected for health: Using electronic health records to transform care delivery. San Francisco, CA: Jossey-Bass; 2010. pp. 139–156. [Google Scholar]
- 70.Saranto K, Brennan PF, Casey E. Personal health information management: tools and strategies for citizens' engagement. International Nursing Informatics Congress; June 26-July 1, 2009; Vanajanlinna, Finland. 2009. [Google Scholar]
- 71.Nazi KM, Woods SS. MyHealtheVet PHR: A description of users and patient portal use. AMIA Annual Symposium Proceedings; AMIA Annual Symposium; 2008; Washington, DC. 2008. [PubMed] [Google Scholar]
- 72.Liang L. Connected for health: Using electronic health records to transform care delivery. San Francisco, CA: Jossey-Bass; 2010. Kaiser Permanente Healthconnect: A primer. [Google Scholar]
- 73.Chen Catherine, Garrido Terhilda, Chock Don, Okawa Grant, Liang Louise. The Kaiser Permanente Electronic Health Record: transforming and streamlining modalities of care. Health Aff (Millwood) 2009;28(2):323–33. doi: 10.1377/hlthaff.28.2.323. http://content.healthaffairs.org/cgi/pmidlookup?view=long&pmid=19275987. [DOI] [PubMed] [Google Scholar]
- 74.Blumenthal David, Tavenner Marilyn. The meaningful use regulation for electronic health records. N Engl J Med. 2010 Aug 5;363(6):501–4. doi: 10.1056/NEJMp1006114. [DOI] [PubMed] [Google Scholar]
- 75.Patel Vaishali N, Abramson Erika, Edwards Alison M, Cheung Melissa A, Dhopeshwarkar Rina V, Kaushal Rainu. Consumer attitudes toward personal health records in a beacon community. Am J Manag Care. 2011 Apr;17(4):e104–20. http://www.ajmc.com/pubMed.php?pii=48672. [PubMed] [Google Scholar]
- 76.Patel Vaishali N, Dhopeshwarkar Rina V, Edwards Alison, Barrón Yolanda, Sparenborg Jeffrey, Kaushal Rainu. Consumer support for health information exchange and personal health records: a regional health information organization survey. J Med Syst. 2012 Jun;36(3):1043–52. doi: 10.1007/s10916-010-9566-0. [DOI] [PubMed] [Google Scholar]
- 77.Brennan Patricia Flatley, Downs Stephen, Casper Gail. Project HealthDesign: rethinking the power and potential of personal health records. J Biomed Inform. 2010 Oct;43(5 Suppl):S3–5. doi: 10.1016/j.jbi.2010.09.001. http://linkinghub.elsevier.com/retrieve/pii/S1532-0464(10)00133-4. [DOI] [PubMed] [Google Scholar]
- 78.Woods Susan S, Schwartz Erin, Tuepker Anais, Press Nancy A, Nazi Kim M, Turvey Carolyn L, Nichol W Paul. Patient experiences with full electronic access to health records and clinical notes through the My HealtheVet Personal Health Record Pilot: qualitative study. J Med Internet Res. 2013;15(3):e65. doi: 10.2196/jmir.2356. http://www.jmir.org/2013/3/e65/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Office of the National Coordinator for Health Information Technology Beacon community and EHR vendor collaboration: A catalyst for interoperability and exchange. 2012. [2015-03-24]. http://www.healthit.gov/sites/default/files/pdf/ehr-vendor-beacon-topic.pdf.
- 80.Archer N, Fevrier-Thomas U, Lokker C, McKibbon K A, Straus S E. Personal health records: a scoping review. J Am Med Inform Assoc. 2011;18(4):515–22. doi: 10.1136/amiajnl-2011-000105. http://jamia.oxfordjournals.org/lookup/pmidlookup?view=long&pmid=21672914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wagholikar Amol, Fung Maggie, Nelson Colleen. Improving self-care of patients with chronic disease using online personal health record. Australas Med J. 2012;5(9):517–21. doi: 10.4066/AMJ.2012.1358. http://europepmc.org/abstract/MED/23115588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Komura Kazue, Yamagishi Akemi, Akizuki Nobuya, Kawagoe Shohei, Kato Masashi, Morita Tatsuya, Eguchi Kenji. Patient-perceived usefulness and practical obstacles of patient-held records for cancer patients in Japan: OPTIM study. Palliat Med. 2013 Feb;27(2):179–84. doi: 10.1177/0269216311431758. [DOI] [PubMed] [Google Scholar]
- 83.Greene J, Hibbard JH. Why does patient activation matter? An examination of the relationships between patient activation and health-related outcomes. J Gen Intern Med. 2012 May;27(5):520–6. doi: 10.1007/s11606-011-1931-2. http://europepmc.org/abstract/MED/22127797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Dixon Anna, Hibbard Judith, Tusler Martin. How do people with different levels of activation self-manage their chronic conditions? Patient. 2009 Dec 1;2(4):257–68. doi: 10.2165/11313790-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 85.Hibbard Judith H, Stockard Jean, Mahoney Eldon R, Tusler Martin. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res. 2004 Aug;39(4 Pt 1):1005–26. doi: 10.1111/j.1475-6773.2004.00269.x. http://europepmc.org/abstract/MED/15230939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Solomon Michael, Wagner Stephen L, Goes James. Effects of a Web-based intervention for adults with chronic conditions on patient activation: online randomized controlled trial. J Med Internet Res. 2012;14(1):e32. doi: 10.2196/jmir.1924. http://www.jmir.org/2012/1/e32/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Siminerio Linda M. The role of technology and the chronic care model. J Diabetes Sci Technol. 2010 Mar;4(2):470–5. doi: 10.1177/193229681000400229. http://europepmc.org/abstract/MED/20307409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Holbrook Anne, Thabane Lehana, Keshavjee Karim, Dolovich Lisa, Bernstein Bob, Chan David, Troyan Sue, Foster Gary, Gerstein Hertzel. Individualized electronic decision support and reminders to improve diabetes care in the community: COMPETE II randomized trial. CMAJ. 2009 Jul 7;181(1-2):37–44. doi: 10.1503/cmaj.081272. http://www.cmaj.ca/cgi/pmidlookup?view=long&pmid=19581618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Institute of Medicine . Key capibilities of an electronic health record system. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 90.Institute of Medicine . Health IT and patient safety: Building safer systems for better care. Washington, DC: The National Academies Press; 2012. [PubMed] [Google Scholar]
- 91.Hsiao CJ, Hing E. Use and characteristics of electronic health record systems among office-based physician practices: United States, 2001-2012. Hyattsville, MD: National Center for Health Statistics; [2015-03-24]. http://www.cdc.gov/nchs/data/databriefs/db111.pdf. [PubMed] [Google Scholar]
- 92.Grand View Research mHealth market analysis and segment forecasts to 2020. 2014. [2015-03-24]. http://www.grandviewresearch.com/industry-analysis/mhealth-market.
- 93.Institute of Medicine . Health literacy: A prescription to end confusion. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- 94.Watkins Ivan, Xie Bo. eHealth literacy interventions for older adults: a systematic review of the literature. J Med Internet Res. 2014;16(11):e225. doi: 10.2196/jmir.3318. http://www.jmir.org/2014/11/e225/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Choi Namkee G, Dinitto Diana M. The digital divide among low-income homebound older adults: Internet use patterns, eHealth literacy, and attitudes toward computer/Internet use. J Med Internet Res. 2013;15(5):e93. doi: 10.2196/jmir.2645. http://www.jmir.org/2013/5/e93/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lipkus Isaac M, Peters Ellen. Understanding the role of numeracy in health: proposed theoretical framework and practical insights. Health Educ Behav. 2009 Dec;36(6):1065–81. doi: 10.1177/1090198109341533. http://europepmc.org/abstract/MED/19834054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Lipkus I M, Samsa G, Rimer B K. General performance on a numeracy scale among highly educated samples. Med Decis Making. 2001;21(1):37–44. doi: 10.1177/0272989X0102100105. [DOI] [PubMed] [Google Scholar]
- 98.Norman Cameron. eHealth literacy 2.0: problems and opportunities with an evolving concept. J Med Internet Res. 2011;13(4):e125. doi: 10.2196/jmir.2035. http://www.jmir.org/2011/4/e125/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Rideout V, Neuman T, Kitchman M, Brodie M. e-Health and the elderly: How seniors use the internet for health information. Menlo Park, CA: Kaiser Family Foundation; 2005. [2015-03-24]. https://kaiserfamilyfoundation.files.wordpress.com/2013/01/e-health-and-the-elderly-how-seniors-use-the-internet-for-health-information-key-findings-from-a-national-survey-of-older-americans-survey-report.pdf. [Google Scholar]
- 100.Miller Lisa M Soederberg, Bell Robert A. Online health information seeking: the influence of age, information trustworthiness, and search challenges. J Aging Health. 2012 Apr;24(3):525–41. doi: 10.1177/0898264311428167. [DOI] [PubMed] [Google Scholar]
- 101.Powell AC, Landman AB, Bates DW. In search of a few good apps. JAMA. 2014 May 14;311(18):1851–2. doi: 10.1001/jama.2014.2564. [DOI] [PubMed] [Google Scholar]
- 102.Aitken M, Goauntlett C. Patient apps for improved healthcare: from novelty to mainstream. Parsippany, NJ: IMS Institute for Healthcare Informatics; 2013. [Google Scholar]
- 103.Chu Adeline, Huber Jeffrey, Mastel-Smith Beth, Cesario Sandra. Partnering with Seniors for Better Health: computer use and Internet health information retrieval among older adults in a low socioeconomic community. J Med Libr Assoc. 2009 Jan;97(1):12–20. doi: 10.3163/1536-5050.97.1.003. http://europepmc.org/abstract/MED/19159002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.McInnes DK, Solomon J, Shimada SL, Petrakis BA, Bokhour BG, Asch SM, Nazi KM, Houston Thomas K, Gifford AL. Development and evaluation of an internet and personal health record training program for low-income patients with HIV or hepatitis C. Med Care. 2013 Mar;51(3 Suppl 1):S62–6. doi: 10.1097/MLR.0b013e31827808bf. [DOI] [PubMed] [Google Scholar]
- 105.Schifferdecker Karen E, Reed Virginia A, Homa Karen. A training intervention to improve information management in primary care. Fam Med. 2008 Jun;40(6):423–32. http://europepmc.org/abstract/MED/18773781. [PMC free article] [PubMed] [Google Scholar]
- 106.Yellowlees PM. Your health in the information age - how you and your doctor can use the internet to work together. Bloomington, IN: iUniverse, Inc; 2008. [Google Scholar]
- 107.Parchman Michael L, Zeber John E, Palmer Raymond F. Participatory decision making, patient activation, medication adherence, and intermediate clinical outcomes in type 2 diabetes: a STARNet study. Ann Fam Med. 2010;8(5):410–7. doi: 10.1370/afm.1161. http://www.annfammed.org/cgi/pmidlookup?view=long&pmid=20843882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Liederman Eric M, Morefield Catrina S. Web messaging: a new tool for patient-physician communication. J Am Med Inform Assoc. 2003;10(3):260–70. doi: 10.1197/jamia.M1259. http://jamia.oxfordjournals.org/lookup/pmidlookup?view=long&pmid=12626378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Liederman Eric M, Lee Jerry C, Baquero Victor H, Seites Paul G. Patient-physician web messaging. The impact on message volume and satisfaction. J Gen Intern Med. 2005 Jan;20(1):52–7. doi: 10.1111/j.1525-1497.2005.40009.x. http://europepmc.org/abstract/MED/15693928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Reti Shane R, Feldman Henry J, Ross Stephen E, Safran Charles. Improving personal health records for patient-centered care. J Am Med Inform Assoc. 2010;17(2):192–5. doi: 10.1136/jamia.2009.000927. http://jamia.oxfordjournals.org/lookup/pmidlookup?view=long&pmid=20190063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Stellefson Michael, Chaney Beth, Barry Adam E, Chavarria Enmanuel, Tennant Bethany, Walsh-Childers Kim, Sriram P S, Zagora Justin. Web 2.0 chronic disease self-management for older adults: a systematic review. J Med Internet Res. 2013;15(2):e35. doi: 10.2196/jmir.2439. http://www.jmir.org/2013/2/e35/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Kuijpers Wilma, Groen Wim G, Aaronson Neil K, van Harten Wim H. A systematic review of web-based interventions for patient empowerment and physical activity in chronic diseases: relevance for cancer survivors. J Med Internet Res. 2013;15(2):e37. doi: 10.2196/jmir.2281. http://www.jmir.org/2013/2/e37/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Meglic Matic, Furlan Mirjana, Kuzmanic Marja, Kozel Dejan, Baraga Dusan, Kuhar Irma, Kosir Branko, Iljaz Rade, Novak Sarotar Brigita, Dernovsek Mojca Zvezdana, Marusic Andrej, Eysenbach Gunther, Brodnik Andrej. Feasibility of an eHealth service to support collaborative depression care: results of a pilot study. J Med Internet Res. 2010;12(5):e63. doi: 10.2196/jmir.1510. http://www.jmir.org/2010/5/e63/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Nicklett Emily J, Liang Jersey. Diabetes-related support, regimen adherence, and health decline among older adults. J Gerontol B Psychol Sci Soc Sci. 2010 May;65B(3):390–9. doi: 10.1093/geronb/gbp050. http://europepmc.org/abstract/MED/19541672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Strom JL, Egede LE. The impact of social support on outcomes in adult patients with type 2 diabetes: a systematic review. Curr Diab Rep. 2012 Dec;12(6):769–81. doi: 10.1007/s11892-012-0317-0. http://europepmc.org/abstract/MED/22949135. [DOI] [PMC free article] [PubMed] [Google Scholar]