Abstract
In industrialized nations diabetic retinopathy is the most frequent microvascular complication of diabetes mellitus and the most common cause of blindness in the working-age population. In the next 15 years, the number of patients suffering from diabetes mellitus is expected to increase significantly. By the year 2030, about 440 million people in the age-group 20-79 years are estimated to be suffering from diabetes mellitus worldwide (prevalence 7.7%), while in 2010 there were 285 million people with diabetes mellitus (prevalence 6.4%). This accounts for an increase in patients with diabetes in industrialized nations by 20% and in developing countries by 69% until the year 2030. Due to the expected rise in diabetic patients, the need for ophthalmic care of patients (i.e., exams and treatments) will also increase and represents a challenge for eye-care providers. Development of optimized screening programs, which respect available resources of the ophthalmic infrastructure, will become even more important. Main reasons for loss of vision in patients with diabetes mellitus are diabetic macular edema and proliferative diabetic retinopathy. Incidence or progression of these potentially blinding complications can be greatly reduced by adequate control of blood glucose and blood pressure levels. Additionally, regular ophthalmic exams are mandatory for detecting ocular complications and initiating treatments such as laser photocoagulation in case of clinical significant diabetic macular edema or early proliferative diabetic retinopathy. In this way, the risk of blindness can considerably be reduced. In advanced stages of diabetic retinopathy, pars-plana vitrectomy is performed to treat vitreous hemorrhage and tractional retinal detachment. In recent years, the advent of intravitreal medication has improved therapeutic options for patients with advanced diabetic macular edema.
Keywords: Laser photocoagulation, Diabetic macular edema, Diabetic retinopathy, Intravitreal injection, Prevention
Core tip: Diabetic retinopathy is a potentially blinding complication of diabetes mellitus. In patients with diabetes, regular retinal exams are essential. While laser photocoagulation is effective, if performed in time, advanced stages of diabetic retinopathy need to be treated by vitreo-retinal surgery and have limited visual prognosis. Even though new therapeutic options such as intravitreal medical therapy and sutureless pars-plana vitrectomy have improved ophthalmic care of patients with diabetes, interdisciplinary care of these patients is essential. Good metabolic and blood pressure control is indispensable for reducing the risk of ophthalmic complications.
INTRODUCTION
Diabetic retinopathy is a potentially blinding complication of diabetes mellitus. Reasons for loss of vision are diabetic maculopathy and complications of proliferative diabetic retinopathy (PDR) such as vitreous hemorrhage, tractional retinal detachment, and neovascular glaucoma. By 2030 developing countries will face an increase by 69% and industrialized countries by 20% of the number of patients with diabetes compared to 2010[1]. For Africa more than 18 million, according to some estimations even 24 million, diabetic patients are predicted for the year 2030[1,2].
Probability of retinal complications increases with increasing duration of disease. In up to 50% of patients with type 1 diabetes and 30% of those with type 2 diabetes potentially vision-threatening retinal changes develop over time, while early retinal changes are not noticed by the patients[3].
Diabetic retinopathy is the most common microvascular complication of diabetes mellitus and affects between 3%-4% of people in Europe, while the relative risk for developing diabetic retinopathy is higher in type 1 diabetes compared to type 2[4-6]. Diabetes mellitus is responsible for about 15% of all cases of legal blindness (best corrected visual acuity less than 0.02) in Germany[7]. It is the main cause of blindness within the working-age population in industrialized nations[4].
While retinal changes are rarely seen in patients with type 1 diabetes before adolescence, about one third of patients have signs of diabetic retinopathy at time of initial diagnosis of diabetes mellitus. The risk of PDR is higher in type 1 diabetes than in type 2, while diabetic macular edema is more commonly found in type 2 diabetes (prevalence after 15 years of disease: type 1 vs type 2 = 15% vs 25%)[8].
Kramer et al[9] reported in a recent study, that in patients with type 1 diabetes progression of diabetic retinopathy and development of nephropathy each increase the risk for incidence of the other. This association was independent of established risk factors for microvascular complications and the authors suggested a shared etiologic basis of these two complications of diabetes mellitus[9]. Another group also found proliferative diabetic retinopathy to be an independent marker of long-term nephropathy in patients with type 1 diabetes[10]. Other studies indicated association of the presence of diabetic retinopathy and increased overall-mortality and cardiovascular events both in type 1 and type 2 diabetes[11].
Therefore an interdisciplinary approach of physicians, endocrinologists, and ophthalmologists is needed for optimal care.
PATHOGENESIS OF DIABETIC RETINOPATHY
Micro-angiopathy due to hyperglycemia in patients with diabetes mellitus results in vascular leakage, which causes diabetic macular edema on one hand, and capillary occlusion on the other hand. Capillary occlusion then again causes retinal ischemia and increased levels of vascular endothelial growth factor (VEGF) which are responsible for the development of neovascularization and the proliferative stage of diabetic retinopathy.
More recently new pathways which may be involved in the pathogenesis of diabetic retinopathy have been identified, such as inflammation, nerve growth factor autophagy and epigenetics. A detailed discussion of all these pathways would go beyond the scope of this mini-review about clinical aspects of diabetic retinopathy, however some aspects should be addressed.
Biochemical alterations such as oxidative stress, activation of protein kinase C and formation of advanced glycation end products have been detected as a response of the retina to hyperglycemia[12]. Also kinin B1 and B2 are thought to increase vascular permeability, infiltration of leukocytes and inflammation. Especially kinin B1, which is almost non-existent in normal tissue, is upregulated in the retina of diabetic patients. These findings may be important for developing new therapeutic strategies aiming at antagonizing kinin receptors or at inhibiting kallikreins[13].
Recent investigations showed that the whole retinal neurovascular system is impaired by diabetes mellitus resulting in loss of neurovascular coupling, neurodegeneration and neuroinflammation, which can be detected even before the advent of vascular damage[14]. Clinically, reduced dark adaption, impaired colour and/or contrast vision and visual field defects are found during functional examinations of diabetic patients[15].
Diabetic retinopathy tends to deteriorate during hormonal changes such as adolescence and pregnancy[16].
CLASSIFICATION AND PATHOPYSIOLOGY OF DIABETIC RETINOPATHY
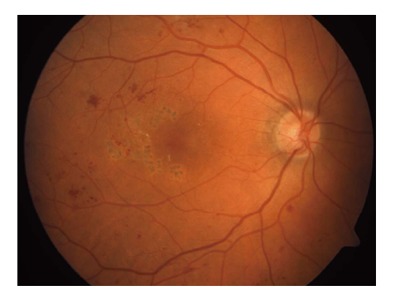
During fundoscopy, which should be performed after dilation of the pupil (mydriasis) to allow visualization of the entire retina, presence and grade of diabetic retinopathy can be assessed clinically. Typical changes seen in early diabetic retinopathy (non-PDR) are micro-aneurysms, retinal hemorrhages, and exudates (Figure 1). In the beginning, these alterations are often found slightly temporal to the central area of the macula (Figure 2). These are caused by deranged vascular integrity and loss of pericytes. In the later course of disease, intra-retinal micro-vascular anomalies may develop, which represent dilated and therefore during fundoscopy visible retinal capillaries, and indicate possible risk of neovascularization and proliferative diabetic retinopathy.
Figure 1.
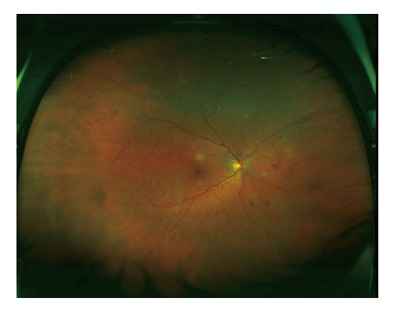
Non-proliferative diabetic retinopathy. Wide-field fundus photo of a 65-year-old female patient (right eye) showing several retinal hemorrhages.
Figure 2.
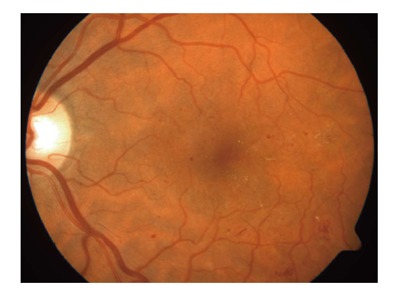
Non-proliferative diabetic retinopathy. Color fundus photo of a 51-year-old male patient with micro-aneurysms and lipid exudates.
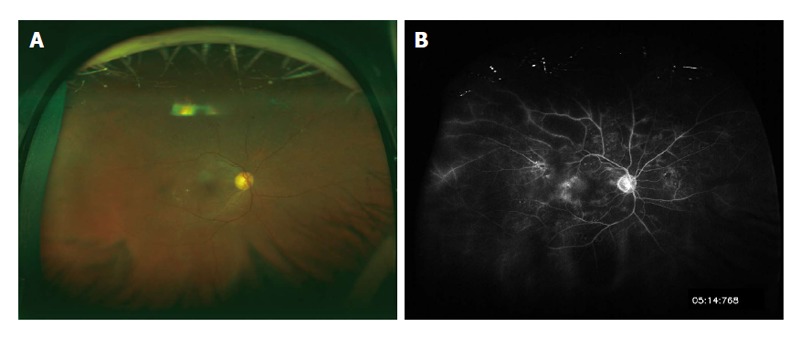
Proliferative diabetic retinopathy is caused by increased intraocular VEGF-levels due to retinal ischemia because of capillary occlusion of retinal vessels. Proliferation may grow at the optic disc (neovascularization at the disk) or elsewhere in the retina (neovascularization elsewhere ) into the vitreous (Figure 3). These newly formed vessels leak on fluorescein angiography and may cause vitreous hemorrhage and finally tractional retinal detachment (Figures 4 and 5). Tractional retinal detachment results in separation of the neurosensory retina from the retinal pigment epithelium. Detached sections of the retina cause relative visual-field defects (scotoma) and loss of visual acuity in cases with macular involvement.
Figure 3.
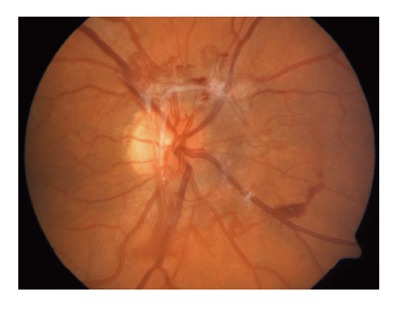
Proliferative diabetic retinopathy with neovascularization at disk.
Figure 4.
Advanced proliferative diabetic retinopathy with neovascularization and limited vitreous hemorrhage.
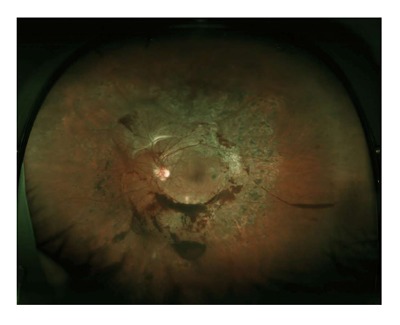
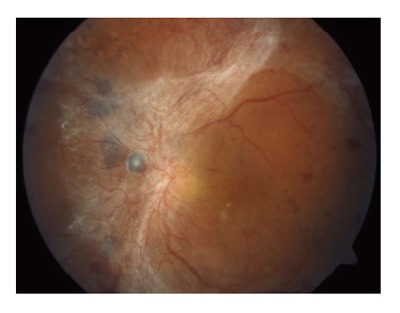
Figure 5.
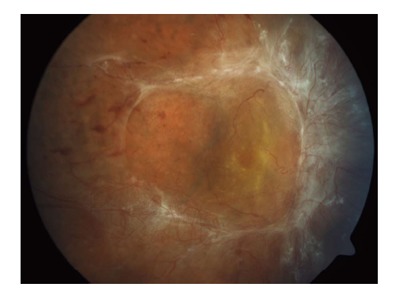
Advanced proliferative diabetic retinopathy with tractional retinal detachment.
Further, neovascularization on the iris in the anterior segment of the eye may evolve as anterior segment sequel of ischemia (Figure 6). These new blood vessels grow towards the anterior chamber angle and may obstruct the trabecular meshwork, thus increasing outflow resistance of aqueous humor. This results in increased intraocular pressure followed by optic atrophy (neovascular glaucoma).
Figure 6.

Neovascularization of the iris. These neovascular vessels may block the trabecular meshwork and cause neovascular glaucoma.
CLASSIFICATION AND PATHOPHYSIOLOGY OF DIABETIC MACULOPATHY
Diabetic maculopathy may develop in the non-proliferative and in the proliferative stage of diabetic retinopathy. While complications of untreated proliferative diabetic retinopathy, such as vitreous hemorrhage and tractional retinal detachment involving the macula may cause the most severe loss of vision in diabetic retinopathy, diabetic maculopathy is the main cause of visual impairment in patients with type 2 diabetes[17].
Diabetic macular edema is caused by a disruption of the inner blood-retinal barrier, formed by the retinal vascular endothelium, due to hyperglycemia, increased levels of growth-factors, inflammation and cytokines. This also causes impairment of pericytes and leads to consecutive exudation of fluid, proteins and lipids by para cellular and trans cellular transport mechanisms[18]. Clinically, areas of thickened retina are often demarcated by surrounding yellowish lipid exudates (Figure 7). Diabetic macular edema may be limited or affect a large retinal area and it may also involve the macula (center-involving) or spare the central area (non-center-involving) (Figure 8).
Figure 7.
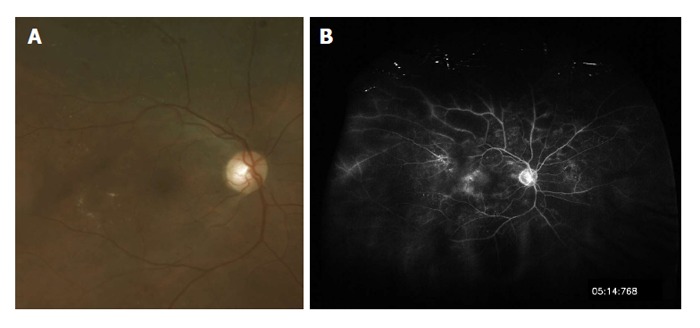
Clinically significant diabetic macular edema without involvement of the fovea. A: Fundus photo; B: Fluorescein angiogram depicting leakage of perifoveal retinal blood vessels.
Figure 8.
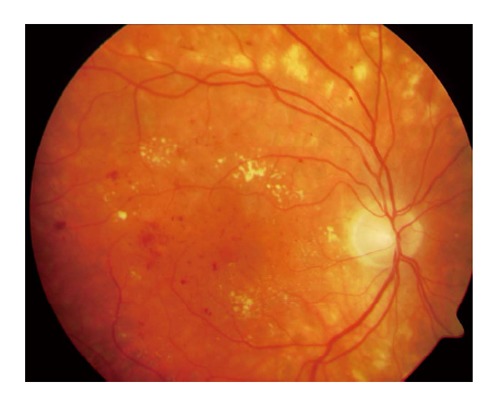
Center-involving diabetic macular edema with subfoveal edema and numerous lipid exudates.
Traction caused by vitreous attachment to the fovea may result in macular thickening, as well. Vitreous traction can excellently be documented by high-resolution optical coherence tomography (OCT, spectral-domain OCT). Vitrectomy is needed in patients with symptomatic tractional macular edema in order to release traction by surgical removal of the vitreous.
Apart from edema, diabetic maculopathy may also present as occlusion of perifoveal capillaries resulting in distinct visual impairment in the absence of edema on fundoscopy. In these cases, fluorescein angiography is needed to confirm the diagnosis by visualizing capillary occlusion in around the fovea.
Table 1 summarizes the different types of diabetic maculopathy (adapted from Nentwich et al[19]).
Table 1.
Types of diabetic maculopathy[19]
| Focal | Localized edema Lipid exudates Intraretinal hemorrhages Focal hyperfluorescence in late fluorescein angiography |
| Clinically significant without foveal thickening (non-center-involving) (sight-threatening) | Edema within 500 μm around the foveola Exudates within 500 μm around the foveola accompanied by edema Edema ≥ 1 optic-disk diameter within one optic-disk diameter around the foveola |
| Clinically significant with foveal thickening (center-involving) | Ill-defined edema, which may be cystoid Exudates Intraretinal hemorrhages Origin of leakage often not clearly identifiable by fluorescein angiography |
| Tractional | Due to vitreous traction to the fovea Thickened posterior hyaloid membrane OCT visualizes vitreal traction |
| Ischemic maculopathy (occlusion of the perifoveal capillaries) | Loss of vision without any clearly visible cause on fundoscopy Fluorescein angiography needed for diagnosis Difficult to diagnose by fundoscopy only Edema may be present or absent |
OCT: Optical coherence tomography.
CLINICAL DIAGNOSICS
Dilated fundoscopy is the most important clinical investigation in patients with diabetes during screening examinations by an ophthalmologist. Dilation of the pupil is necessary in order to enable a proper stereoscopic view, which is needed for evaluation of macular edema, and to allow visualization of the peripheral retina.
Fluorescein angiography was introduced by Novotny et al[20] in the 1960s into the clinical ophthalmic practice and allows evaluation of the retinal vascular status. Fluorescein, a fluorescent dye, is injected intravenously and distributes throughout the body. In the eye, fluorescence is activated by blue light of 490 nm. During fluorescein angiography vascular leakage, capillary occlusion, ischemic areas of the retina and neovascularization can be seen (Figure 9A and C). It provides information on the area of leakage as well as of the location of non-perfused parts of the retina. In patients with suspected diabetic maculopathy, fluorescein angiography is mandatory for excluding ischemic maculopathy and guiding possible focal laser photocoagulation.
Figure 9.
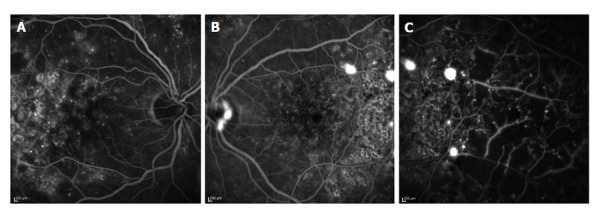
Fluorescein angiogram of a 49-year-old female patient. A: Fluorescein angiogram of the right eye 50 s after intravenous injection of fluorescein dye. Here, leaking micro-aneurysms in the macula can be seen; B: Fluorescein angiogram of the left eye 25 s after intravenous injection of fluorescein dye. Leakage from neovascular blood vessels causes spots of increased fluorescence at the optic disk and temporal to the fovea; C: Fluorescein angiogram of the temporal part of the left eye 30 s after intravenous injection of fluorescein dye. Areas of retinal non-perfusion can be seen as reason for neovascularization.
Wide-field fundus photography (2-laser wavelength nonmydriatic 200° ultra-wide-field scanning laser ophthalmoscopy) has been introduced recently. Wide-field images and traditional color fundus photography in mydriasis seem to correlate with regard to the classification of diabetic retinopathy and visualization of diabetic macular edema according to recent studies (Figure 10A)[21-23]. This wide-field imaging technique can be combined with fluorescein angiography and provides information about peripheral retinal ischemia or peripheral neovascularization (Figure 10B)[24].
Figure 10.
Wide-field picture of the right eye of a 65-year-old female patient. A: On scanning-laser-ophthalmoscope-Imaging some micro-aneurysms and lipid exudates can be seen; B: Fluorescein angiogram shows leakage from micro-aneurysms and extensive areas of retinal non-perfusion.
Probably the most important new imaging technique, which was introduced in ophthalmologic practice, is OCT. Recently, resolution and recording speed have been greatly improved by spectral-domain OCT technique (SD-OCT). OCT provides data on retinal volume and configuration of the macular region. In diabetic macular edema SD-OCT is a very valuable examination technique comparing follow-up visits with baseline data, as modern OCT-devices use eye-tracking for finding the same imaging position during follow-up examinations (Figure 11)[25].
Figure 11.
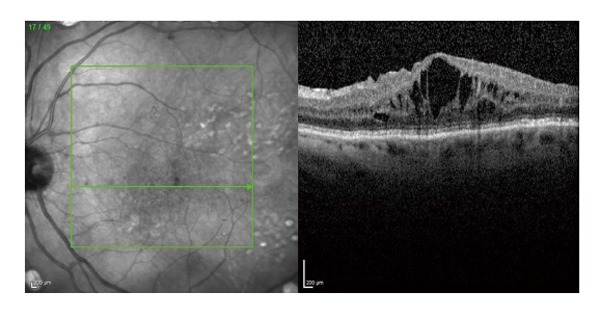
Spectral-domain optical coherence tomography of a female patient with center-involving diabetic macular edema. On the left side of the picture, an infra-red image shows the exact location of the OCT-scan on the right. The OCT-scan visualizes intraretinal edema with thickening of the fovea. OCT: Optical coherence tomography.
IMPORTANCE OF PREVENTION
In early diabetic retinopathy, laser photocoagulation can be used effectively for preventing loss of vision[26]. However, early diabetic retinopathy is not noticed by patients because of the absence of visual loss in early diabetic retinopathy. Thus, regular retinal exams with dilation of the pupil are necessary in patients with diabetes mellitus in order to detect sight-threatening changes timely and enable ophthalmologists to perform treatment.
Patients with type 1 diabetes should undergo retinal exams starting at the age 11 and/or after 5 years of diagnosis on a yearly basis. In case of retinal changes, shorter follow-up intervals are recommended.
In type 2 diabetes, the first retinal exam should be performed immediately after first diagnosis of diabetes, because the previous duration of the disease is unknown. Annual follow-up examinations are recommended in the absence of retinal changes, otherwise shorter intervals are recommended.
Pregnancy bears an increased risk of worsening of diabetic retinopathy due to hormonal changes. During pregnancy diabetic retinopathy may start in about 10% of cases and may worsen in an even higher percentage in case of preexisting diabetic retinopathy at time of conception[27]. In case of proliferative diabetic retinopathy before or shortly after conception, pan-retinal laser photocoagulation should be performed as retinal changes may worsen in one out of two women in this population. This risk can be reduced by half by thorough retinal laser photocoagulation. Therefore all females with diabetes, who are planning to get pregnant, should undergo fundoscopy prior to conception and then every three months during pregnancy to enable early intervention, if needed. Additionally good metabolic control should be achieved before conception[28].
On the other hand, the presence of diabetic retinopathy is no indication for cesarean section per se, as no study has indicated so far, that Valsalva-maneuvers during vaginal delivery bear an increased risk of vitreous hemorrhages[29].
The German Diabetes Society recommends scheduling of follow-up examinations depending on the grade of diabetic retinopathy as summarized in Table 2 (Adapted from[30]).
Table 2.
Recommended timing of retinal examinations in patients with type 2 diabetes[6]
| Patient characteristics | Timing of retinal examination |
| Initial diagnosis of type 2 diabetes | Soon |
| No diabetic retinopathy | Once a year |
| Presence of symptoms such as | During the next few days |
| Loss of vision | |
| New difficulties during reading | |
| Altered color perception | |
| New, moving dark spots in the eye | |
| Presence of diabetic retinopathy | Depending on the severity of retinopathy, e.g., every 3-6 mo |
These recommended examination intervals will result in an increased work-load for ophthalmologists due to the rising number of diabetic patients. Studies examined the effect of an extension of follow-up intervals and found no increased risk of progression to sight-threatening diabetic retinopathy in patients with good metabolic control (HbA1c < 8%) and no known diabetic retinopathy[31-35]. By adequate selection of patients, the number of necessary screening examinations could be reduced by 40% according to one study and even by 59% in case a special mathematical algorism is used[31,33]. However, feasibility of these strategies remains to be proven in routine clinical practice and until then ophthalmic screening intervals as indicated above are recommended.
GENERAL MEDICAL THERAPY AND INTERVENTIONS
Blood glucose and blood pressure control
Good metabolic and blood-pressure control are essential for successful ophthalmic care of patients with diabetes.
In type 2 diabetes, a reduction of HbA1c from 7.9% to 7.0% resulted in a decline in the frequency of laser treatments needed[36]. In type 1 patients, improved blood glucose control with a reduction of HbA1c values from 9.1% to 7.1% reduced the risk of developing diabetic retinopathy within 6.5 years by 76%, the risk of progression of diabetic retinopathy by 54%, and the risk of developing proliferative diabetic retinopathy by 47%[37]. Therefore an HbA1c level of about 7% should be aimed for from the ophthalmologist’s point of view[19], for the individual patient a bespoke treatment regime may be needed.
Rapid improvement of metabolic control may result in temporary worsening of diabetic retinopathy (“early-worsening”) in patients with long-lasting disease and high HbA1c levels. Thus, retinal exams should be performed every three months during the first year after initiation of an improved anti-diabetic treatment[5,38]. However, in the long-term, positive effects of good metabolic control outweigh these initial problems[37,39]. Also a slow decrease of blood sugar levels, which would be a therapeutic challenge, does not have any advantages in the long term and is not recommended from the ophthalmologist’s point of view[19].
Additionally, optimizing blood pressure helps to reduce the necessity of laser photocoagulation and the risk of loss of vision[40]. While some studies suggested a protective effect of ACE inhibitors, according to the results of studies available to date, reduction of blood pressure itself seems to be more important than the type of blood pressure lowering medication[41-43]. Levels of about 140/80 mmHg should be aimed for.
Acetylsalicylic acid and smoking
Acetylsalicylic acid has neither been shown to have any positive effect on diabetic retinopathy or diabetic macular edema, nor to be harmful for patients with diabetic retinopathy Therefore acetylsalicylic acid should be recommended for cardiovascular reasons in patients with early non-proliferative diabetic retinopathy, in case there are no contraindications[44].
Data on the effect of smoking on diabetic retinopathy is heterogeneous. While some studies did not find an association of smoking with diabetic retinal changes, others identified smoking in a multiple regression analysis as risk factor for any grade of diabetic retinopathy[45-47]. However, results of a recent experimental study suggest that nicotine expedites diabetes-induced retinal changes[48]. Additionally, patient characteristics such as selective mortality among smokers and patients with proliferative diabetic retinopathy at baseline may provide some explanation for the apparently absent association, reported in some studies[47]. Cessation of smoking should therefore be recommended from the ophthalmologist’s point of view.
OPHTHALMIC THERAPEUTIC OPTIONS
Diabetic macular edema
Until the advent of anti-VEGF medication, focal and grid laser photocoagulation was the standard of care for clinical significant diabetic macular edema (CSME) as well as for diffuse diabetic macular edema.
In patients with focal CSME without involvement of the fovea, focal laser photocoagulation of micro-aneurisms and localized areas of leakage reduces the relative risk of moderate loss of vision by 50% (from 24% to 12%) as demonstrated by the ETDRS Group (Figure 12)[49]. In case of persisting areas of leakage two to three months after initial focal laser photocoagulation, repeated laser treatment should be considered[26].
Figure 12.
Color fundus photo of a 53-year-old male patient several months after focal laser photocoagulation because of clinical significant diabetic macular edema. While the laser scars and some remaining dot-hemorrhages are visible, lipid exudates and retinal edema have disappeared.
Apart from the direct effect by coagulating micro-aneurysms, focal laser photocoagulation is thought to increase oxygenation of the retina by improving diffusion of oxygen from choroidal vessels and to reestablish the blood-retinal barrier by thermal stimulation of the retinal pigment epithelium and of endothelial cells of retinal capillaries[50].
Grid laser photocoagulation of diffuse diabetic macular edema with involvement of the fovea (“center-involving”) has a limited functional prognosis[49]. Therefore, grid laser photocoagulation has been replaced by intravitreal anti-VEGF therapy, which provides superior functional results[51].
VEGF is associated with a breakdown of blood-retinal barrier causing leakage and retinal edema[52]. Intravitreal application of anti-VEGF medication enables high local concentrations in the vitreous and a low systemic exposure. However, repeated intravitreal injections of anti-VEGF medications are necessary in patients with center-involving diabetic macular edema. The average number of injections is around 7 in the first year of treatment and 4 in the second year as indicated by recent studies[53,54]. Intravitreal anti-VEGF therapy is generally safe with regard to side-effects of medication, although the incidence of systemic thromboembolic events varies among trials[55]. As the intravitreal application of medication is a surgical procedure, it is associated with the possible risk of postoperative infection, which is called endophthalmitis in case of severe infection of the inner eye and its internal structures. For this reason several recommendations of ophthalmologic societies have been published concerning prevention of post-injection endophthalmitis. Recent studies reported very low rates of post-injection endophthalmitis of less than 1 in 8000 injections performed in an operating theater setting after diligent disinfection of the conjunctiva with povidone-iodine, using sterile gloves and wearing face-masks[56,57]. Other studies report somewhat higher rates of infectious endophthalmitis after intravitreal injection, both after procedures performed in an office-setting and in a theater-setting[58]. The effect of meticulous povidone-iodine prophylaxis on the conjunctival bacterial load and contamination of needles used for injection prophylaxis has been shown in several studies[59-62].
Apart from anti-VEGF medication intravitreal steroids have been evaluated for the treatment of diabetic macular edema. Compared to anti-VEGF medication, steroids have additional anti-inflammatory effects and sustained-release devices can lengthen the intervals between re-treatments[63]. In Europe, a non-absorbable implant containing 190 μg fluocinolone acetonide has been approved as second-line treatment of chronic diabetic macular edema not responding to other therapeutic options. Also approval of an absorbable dexamethasone implant for the treatment of diabetic macular edema is expected by the end of 2014. While intravitreal steroids are effective in reducing diabetic macular edema, patients need to be informed about possible progression of cataract and increased intraocular pressure[64-67].
Proliferative diabetic retinopathy
In early proliferative diabetic retinopathy, pan-retinal laser photocoagulation is effective in reducing the risk of visual loss, while surgery needs to be performed in very advanced proliferative diabetic retinopathy[68]. The suggested screening intervals of patients with diabetes are intended to enable the treating ophthalmologist to detect proliferation amendable for laser treatment early. Pan-retinal laser photocoagulation should be performed when retinal neovascularization is detected during fundoscopy or via fluorescein angiography in order to prevent complications of proliferative diabetic retinopathy such as vitreous hemorrhage or tractional retinal detachment (Figure 13)[68]. Pan-retinal laser photocoagulation aims at eliminating non-perfused parts of the retina, thus reducing ischemia, intravitreal VEGF-levels, and the stimulus for proliferation. The efficacy of pan-retinal laser photocoagulation in reducing the risk of loss of vision has already been shown more than 30 years ago[68]. However, patients need to be informed about side-effects of pan-retinal laser treatments such as constriction of visual fields and reduced dark-adaption due to loss of rod function. These side-effects may also interfere with the patients’ driving ability.
Figure 13.
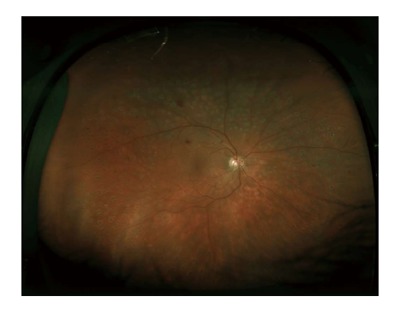
Wide-field picture of the right eye of a 48-year-old male patient after pan-retinal laser photocoagulation because of proliferative diabetic retinopathy. The peripheral laser scars can be seen in the picture, while neovascularization have regressed.
Pars-plana vitrectomy is performed in advanced cases of proliferative diabetic retinopathy, the presence of extensive tractional membranes, vitreous hemorrhage, and tractional retinal detachment (Figure 14). About ten years ago trans conjunctival sutureless 23 gauge vitrectomy started to replace conventional 20 gauge technique and offers comparable safety and efficacy as well as reduced surgery-times and faster rehabilitation of patients[69].
Figure 14.
Proliferative diabetic retinopathy with extensive fibro-vascular membranes.
Combination of diabetic macular edema and proliferative diabetic retinopathy
In patients with diabetic macular edema and proliferation, treatment of macular edema should be performed before pan-retinal laser photocoagulation in order to prevent worsening of macular edema due to peripheral pan-retinal laser photocoagulation.
CONCLUSION
In patients with diabetes, regular retinal exams are essential. While laser photocoagulation is effective, if performed in time, advanced stages of diabetic retinopathy need to be treated by vitreo-retinal surgery and have limited visual prognosis. Even though new therapeutic options such as intravitreal medical therapy and sutureless pars-plana vitrectomy have improved ophthalmic care of patients with diabetes, interdisciplinary care remains essential. Good metabolic and blood pressure control is indispensable for reducing the risk of ophthalmic complications.
Footnotes
P- Reviewer: Mitra A, Sui RF S- Editor: Tian YL L- Editor: A E- Editor: Liu SQ
Conflict-of-interest: None.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: July 17, 2014
First decision: November 27, 2014
Article in press: January 20, 2015
References
- 1.Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87:4–14. doi: 10.1016/j.diabres.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Diabetes Action Now: An Initiative of the World Health Organization and the International Diabetes Federation. Switzerland: World Health Organization; 2004. [Google Scholar]
- 3.Stefánsson E, Bek T, Porta M, Larsen N, Kristinsson JK, Agardh E. Screening and prevention of diabetic blindness. Acta Ophthalmol Scand. 2000;78:374–385. doi: 10.1034/j.1600-0420.2000.078004374.x. [DOI] [PubMed] [Google Scholar]
- 4.Prokofyeva E, Zrenner E. Epidemiology of major eye diseases leading to blindness in Europe: a literature review. Ophthalmic Res. 2012;47:171–188. doi: 10.1159/000329603. [DOI] [PubMed] [Google Scholar]
- 5.Hammes HP. Optimal treatment of diabetic retinopathy. Ther Adv Endocrinol Metab. 2013;4:61–71. doi: 10.1177/2042018813477886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Deutsche DG. Nationale VersorgungsLeitlinie Typ-2-Diabetes Prävention und Therapie von Netzhautkomplikationen. Berlin: Bundesärztekammer (BÄK); 2010. pp. 1–42. [Google Scholar]
- 7.Giani G, Janka HU, Hauner H, Standl E, Schiel R, Neu , A Epidemiologie und Verlauf des Diabetes mellitus in Deutschland. Evidenzbasierte Leitlinie DDG-Aktualisierung. 2004;5:1–12. [Google Scholar]
- 8.Nentwich MM, Ulbig M. Diabetische Retinopathie. Der Diabetologe. 2010;6:491–502. [Google Scholar]
- 9.Kramer CK, Retnakaran R. Concordance of retinopathy and nephropathy over time in Type 1 diabetes: an analysis of data from the Diabetes Control and Complications Trial. Diabet Med. 2013;30:1333–1341. doi: 10.1111/dme.12296. [DOI] [PubMed] [Google Scholar]
- 10.Karlberg C, Falk C, Green A, Sjølie AK, Grauslund J. Proliferative retinopathy predicts nephropathy: a 25-year follow-up study of type 1 diabetic patients. Acta Diabetol. 2012;49:263–268. doi: 10.1007/s00592-011-0304-y. [DOI] [PubMed] [Google Scholar]
- 11.Kramer CK, Rodrigues TC, Canani LH, Gross JL, Azevedo MJ. Diabetic retinopathy predicts all-cause mortality and cardiovascular events in both type 1 and 2 diabetes: meta-analysis of observational studies. Diabetes Care. 2011;34:1238–1244. doi: 10.2337/dc11-0079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ahsan H. Diabetic retinopathy--biomolecules and multiple pathophysiology. Diabetes Metab Syndr. 2015;9:51–54. doi: 10.1016/j.dsx.2014.09.011. [DOI] [PubMed] [Google Scholar]
- 13.Bhat M, Pouliot M, Couture R, Vaucher E. The kallikrein-kinin system in diabetic retinopathy. Prog Drug Res. 2014;69:111–143. doi: 10.1007/978-3-319-06683-7_5. [DOI] [PubMed] [Google Scholar]
- 14.Abcouwer SF, Gardner TW. Diabetic retinopathy: loss of neuroretinal adaptation to the diabetic metabolic environment. Ann N Y Acad Sci. 2014;1311:174–190. doi: 10.1111/nyas.12412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Verbraak FD. Neuroretinal degeneration in relation to vasculopathy in diabetes. Diabetes. 2014;63:3590–3592. doi: 10.2337/db14-0888. [DOI] [PubMed] [Google Scholar]
- 16.Hammes HP, Bertram B, Bornfeld N, Danne T, Kroll P, Lemmen KD. Diagnostik, Therapie und Verlaufskontrolle der diabetischen Retinopathie und Makulopathie. Germany: Evidenzbasierte Leitlinie DDG Aktualisierung; 2004. [Google Scholar]
- 17.Garweg JG, Wenzel A. [Diabetic maculopathy and retinopathy. Functional and sociomedical significance] Ophthalmologe. 2010;107:628–635. doi: 10.1007/s00347-010-2176-x. [DOI] [PubMed] [Google Scholar]
- 18.Klaassen I, Van Noorden CJ, Schlingemann RO. Molecular basis of the inner blood-retinal barrier and its breakdown in diabetic macular edema and other pathological conditions. Prog Retin Eye Res. 2013;34:19–48. doi: 10.1016/j.preteyeres.2013.02.001. [DOI] [PubMed] [Google Scholar]
- 19.Nentwich MM, Ulbig M. Diabetes und Auge. Diabetologe. 2014;10:69–82. [Google Scholar]
- 20.Novotny HR, Alvis DL. A method of photographing fluorescence in circulating blood in the human retina. Circulation. 1961;24:82–86. doi: 10.1161/01.cir.24.1.82. [DOI] [PubMed] [Google Scholar]
- 21.Kernt M, Hadi I, Pinter F, Seidensticker F, Hirneiss C, Haritoglou C, Kampik A, Ulbig MW, Neubauer AS. Assessment of diabetic retinopathy using nonmydriatic ultra-widefield scanning laser ophthalmoscopy (Optomap) compared with ETDRS 7-field stereo photography. Diabetes Care. 2012;35:2459–2463. doi: 10.2337/dc12-0346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Silva PS, Cavallerano JD, Sun JK, Noble J, Aiello LM, Aiello LP. Nonmydriatic ultrawide field retinal imaging compared with dilated standard 7-field 35-mm photography and retinal specialist examination for evaluation of diabetic retinopathy. Am J Ophthalmol. 2012;154:549–559.e2. doi: 10.1016/j.ajo.2012.03.019. [DOI] [PubMed] [Google Scholar]
- 23.Liegl R, Liegl K, Ceklic L, Haritoglou C, Kampik A, Ulbig MW, Kernt M, Neubauer AS. Nonmydriatic ultra-wide-field scanning laser ophthalmoscopy (Optomap) versus two-field fundus photography in diabetic retinopathy. Ophthalmologica. 2014;231:31–36. doi: 10.1159/000355092. [DOI] [PubMed] [Google Scholar]
- 24.Wessel MM, Aaker GD, Parlitsis G, Cho M, D’Amico DJ, Kiss S. Ultra-wide-field angiography improves the detection and classification of diabetic retinopathy. Retina. 2012;32:785–791. doi: 10.1097/IAE.0b013e3182278b64. [DOI] [PubMed] [Google Scholar]
- 25.Chin EK, Sedeek RW, Li Y, Beckett L, Redenbo E, Chandra K, Park SS. Reproducibility of macular thickness measurement among five OCT instruments: effects of image resolution, image registration, and eye tracking. Ophthalmic Surg Lasers Imaging. 2012;43:97–108. doi: 10.3928/15428877-20111222-02. [DOI] [PubMed] [Google Scholar]
- 26.Nentwich MM, Lemmen K-D, Ulbig MW. Stadieneinteilung und Therapie der diabetischen Retinopathie und Makulopathie. Z prakt Augenheilk. 2010;31:491–499. [Google Scholar]
- 27.Pescosolido N, Campagna O, Barbato A. Diabetic retinopathy and pregnancy. Int Ophthalmol. 2014;34:989–997. doi: 10.1007/s10792-014-9906-z. [DOI] [PubMed] [Google Scholar]
- 28.Nentwich MM, Ulbig M. Diabetische Retinopathie. CME Springer. 2010;7:47–56. [Google Scholar]
- 29.Kleinwechter H, Schäfer-Graf U, Bührer C, Hösli I, Kainer F, Kautzky-Willer A, Pawlowski B, Schunck K, Somville T, Sorger M. Diabetes und Schwangerschaft. Diabetologie und Stoffwechsel. 2012;7:S185–S191. [Google Scholar]
- 30.Deutsche DG. Nationale VersorgungsLeitlinie Typ-2-Diabetes – Prävention und Therapie von Netzhautkomplikationen (Klinisch relevante Auszüge aus der Leitlinie) Dtsch Arztebl International. 2007;104:211–214. [Google Scholar]
- 31.Aspelund T, Thornórisdóttir O, Olafsdottir E, Gudmundsdottir A, Einarsdóttir AB, Mehlsen J, Einarsson S, Pálsson O, Einarsson G, Bek T, et al. Individual risk assessment and information technology to optimise screening frequency for diabetic retinopathy. Diabetologia. 2011;54:2525–2532. doi: 10.1007/s00125-011-2257-7. [DOI] [PubMed] [Google Scholar]
- 32.Echouffo-Tcheugui JB, Ali MK, Roglic G, Hayward RA, Narayan KM. Screening intervals for diabetic retinopathy and incidence of visual loss: a systematic review. Diabet Med. 2013;30:1272–1292. doi: 10.1111/dme.12274. [DOI] [PubMed] [Google Scholar]
- 33.Looker HC, Nyangoma SO, Cromie DT, Olson JA, Leese GP, Philip S, Black MW, Doig J, Lee N, Briggs A, et al. Predicted impact of extending the screening interval for diabetic retinopathy: the Scottish Diabetic Retinopathy Screening programme. Diabetologia. 2013;56:1716–1725. doi: 10.1007/s00125-013-2928-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Olafsdóttir E, Stefánsson E. Biennial eye screening in patients with diabetes without retinopathy: 10-year experience. Br J Ophthalmol. 2007;91:1599–1601. doi: 10.1136/bjo.2007.123810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stratton IM, Aldington SJ. Risk stratification for diabetic eye screening. Diabetologia. 2014;57:259. doi: 10.1007/s00125-013-3060-4. [DOI] [PubMed] [Google Scholar]
- 36.Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998;352:837–853. [PubMed] [Google Scholar]
- 37.The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. The Diabetes Control and Complications Trial Research Group. N Engl J Med. 1993;329:977–986. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 38.Rodriguez-Fontal M, Kerrison JB, Alfaro DV, Jablon EP. Metabolic control and diabetic retinopathy. Curr Diabetes Rev. 2009;5:3–7. doi: 10.2174/157339909787314176. [DOI] [PubMed] [Google Scholar]
- 39.The relationship of glycemic exposure (HbA1c) to the risk of development and progression of retinopathy in the diabetes control and complications trial. Diabetes. 1995;44:968–983. [PubMed] [Google Scholar]
- 40.Efficacy of atenolol and captopril in reducing risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 39. UK Prospective Diabetes Study Group. BMJ. 1998;317:713–720. [PMC free article] [PubMed] [Google Scholar]
- 41.Chaturvedi N, Porta M, Klein R, Orchard T, Fuller J, Parving HH, Bilous R, Sjølie AK. Effect of candesartan on prevention (DIRECT-Prevent 1) and progression (DIRECT-Protect 1) of retinopathy in type 1 diabetes: randomised, placebo-controlled trials. Lancet. 2008;372:1394–1402. doi: 10.1016/S0140-6736(08)61412-9. [DOI] [PubMed] [Google Scholar]
- 42.Chaturvedi N, Sjolie AK, Stephenson JM, Abrahamian H, Keipes M, Castellarin A, Rogulja-Pepeonik Z, Fuller JH. Effect of lisinopril on progression of retinopathy in normotensive people with type 1 diabetes. The EUCLID Study Group. EURODIAB Controlled Trial of Lisinopril in Insulin-Dependent Diabetes Mellitus. Lancet. 1998;351:28–31. doi: 10.1016/s0140-6736(97)06209-0. [DOI] [PubMed] [Google Scholar]
- 43.Sjølie AK, Klein R, Porta M, Orchard T, Fuller J, Parving HH, Bilous R, Chaturvedi N. Effect of candesartan on progression and regression of retinopathy in type 2 diabetes (DIRECT-Protect 2): a randomised placebo-controlled trial. Lancet. 2008;372:1385–1393. doi: 10.1016/S0140-6736(08)61411-7. [DOI] [PubMed] [Google Scholar]
- 44.Effects of aspirin treatment on diabetic retinopathy. ETDRS report number 8. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology. 1991;98:757–765. [PubMed] [Google Scholar]
- 45.Nittala MG, Keane PA, Zhang K, Sadda SR. Risk factors for proliferative diabetic retinopathy in a Latino American population. Retina. 2014;34:1594–1599. doi: 10.1097/IAE.0000000000000117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yang JY, Kim NK, Lee YJ, Noh JH, Kim DJ, Ko KS, Rhee BD, Kim DJ. Prevalence and factors associated with diabetic retinopathy in a Korean adult population: the 2008-2009 Korea National Health and Nutrition Examination Survey. Diabetes Res Clin Pract. 2013;102:218–224. doi: 10.1016/j.diabres.2013.10.016. [DOI] [PubMed] [Google Scholar]
- 47.Gaedt Thorlund M, Borg Madsen M, Green A, Sjølie AK, Grauslund J. Is smoking a risk factor for proliferative diabetic retinopathy in type 1 diabetes? Ophthalmologica. 2013;230:50–54. doi: 10.1159/000350813. [DOI] [PubMed] [Google Scholar]
- 48.Boretsky A, Gupta P, Tirgan N, Liu R, Godley BF, Zhang W, Tilton RG, Motamedi M. Nicotine accelerates diabetes-induced retinal changes. Curr Eye Res. 2015;40:368–377. doi: 10.3109/02713683.2014.924147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Early photocoagulation for diabetic retinopathy. ETDRS report number 9. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology. 1991;98:766–785. [PubMed] [Google Scholar]
- 50.Bhagat N, Grigorian RA, Tutela A, Zarbin MA. Diabetic macular edema: pathogenesis and treatment. Surv Ophthalmol. 2009;54:1–32. doi: 10.1016/j.survophthal.2008.10.001. [DOI] [PubMed] [Google Scholar]
- 51.Nentwich MM, Ulbig MW. Diabetisches Makulaödem: Alternative Indikation der Anti-VEGF-Therapie. Z prakt Augenheilk. 2011;32:162–166. [Google Scholar]
- 52.Qaum T, Xu Q, Joussen AM, Clemens MW, Qin W, Miyamoto K, Hassessian H, Wiegand SJ, Rudge J, Yancopoulos GD, et al. VEGF-initiated blood-retinal barrier breakdown in early diabetes. Invest Ophthalmol Vis Sci. 2001;42:2408–2413. [PubMed] [Google Scholar]
- 53.Mitchell P, Bandello F, Schmidt-Erfurth U, Lang GE, Massin P, Schlingemann RO, Sutter F, Simader C, Burian G, Gerstner O, Weichselberger A; RESTORE study group. The RESTORE study: ranibizumab monotherapy or combined with laser versus laser monotherapy for diabetic macular edema. Ophthalmology. 2011;118:615–625. doi: 10.1016/j.ophtha.2011.01.031. [DOI] [PubMed] [Google Scholar]
- 54.Stefanini FR, Badaró E, Falabella P, Koss M, Farah ME, Maia M. Anti-VEGF for the management of diabetic macular edema. J Immunol Res. 2014;2014:632307. doi: 10.1155/2014/632307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Stewart MW. Anti-VEGF therapy for diabetic macular edema. Curr Diab Rep. 2014;14:510. doi: 10.1007/s11892-014-0510-4. [DOI] [PubMed] [Google Scholar]
- 56.Nentwich MM, Yactayo-Miranda Y, Schwarzbach F, Wolf A, Kampik A, Mino de Kaspar H. Endophthalmitis after intravitreal injection: decreasing incidence and clinical outcome-8-year results from a tertiary ophthalmic referral center. Retina. 2014;34:943–950. doi: 10.1097/IAE.0000000000000011. [DOI] [PubMed] [Google Scholar]
- 57.Brynskov T, Kemp H, Sørensen TL. No cases of endophthalmitis after 20,293 intravitreal injections in an operating room setting. Retina. 2014;34:951–957. doi: 10.1097/IAE.0000000000000071. [DOI] [PubMed] [Google Scholar]
- 58.Tabandeh H, Boscia F, Sborgia A, Ciracì L, Dayani P, Mariotti C, Furino C, Flynn HW. Endophthalmitis associated with intravitreal injections: office-based setting and operating room setting. Retina. 2014;34:18–23. doi: 10.1097/IAE.0000000000000008. [DOI] [PubMed] [Google Scholar]
- 59.Nentwich MM, Rajab M, Ta CN, He L, Grueterich M, Haritoglou C, Gandorfer A, Kampik A, Mino De Kaspar H. Application of 10% povidone iodine reduces conjunctival bacterial contamination rate in patients undergoing cataract surgery. Eur J Ophthalmol. 2012;22:541–546. doi: 10.5301/ejo.5000093. [DOI] [PubMed] [Google Scholar]
- 60.Gines JC, Nentwich MM, Peggy Bedoya AH, Cibils P, Esteche A, Laspina F, Samudio M, Fariña N, de Kaspar HM. [Bacterial contamination of needles after intravitreal injection in Paraguay] Ophthalmologe. 2012;109:782–787. doi: 10.1007/s00347-012-2591-2. [DOI] [PubMed] [Google Scholar]
- 61.Nentwich M, Yactayo-Miranda Y, Weimann S, Froehlich S, Wolf A, Kampik A, Mino De Kaspar H. Bacterial contamination of needle points after intravitreal injection. Eur J Ophthalmol. 2009;19:268–272. doi: 10.1177/112067210901900215. [DOI] [PubMed] [Google Scholar]
- 62.Li B, Nentwich MM, Hoffmann LE, Haritoglou C, Kook D, Kampik A, Sheng M, Miño de Kaspar H. Comparison of the efficacy of povidone-iodine 1.0%, 5.0%, and 10.0% irrigation combined with topical levofloxacin 0.3% as preoperative prophylaxis in cataract surgery. J Cataract Refract Surg. 2013;39:994–1001. doi: 10.1016/j.jcrs.2013.02.039. [DOI] [PubMed] [Google Scholar]
- 63.Nentwich MM, Ulbig MW. The therapeutic potential of intraocular depot steroid systems: developments aimed at prolonging duration of efficacy. Dtsch Arztebl Int. 2012;109:584–590. doi: 10.3238/arztebl.2012.0584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Boyer DS, Yoon YH, Belfort R, Bandello F, Maturi RK, Augustin AJ, Li XY, Cui H, Hashad Y, Whitcup SM. Three-year, randomized, sham-controlled trial of dexamethasone intravitreal implant in patients with diabetic macular edema. Ophthalmology. 2014;121:1904–1914. doi: 10.1016/j.ophtha.2014.04.024. [DOI] [PubMed] [Google Scholar]
- 65.Dutra Medeiros M, Postorino M, Navarro R, Garcia-Arumí J, Mateo C, Corcóstegui B. Dexamethasone intravitreal implant for treatment of patients with persistent diabetic macular edema. Ophthalmologica. 2014;231:141–146. doi: 10.1159/000356413. [DOI] [PubMed] [Google Scholar]
- 66.Ciulla TA, Harris A, McIntyre N, Jonescu-Cuypers C. Treatment of diabetic macular edema with sustained-release glucocorticoids: intravitreal triamcinolone acetonide, dexamethasone implant, and fluocinolone acetonide implant. Expert Opin Pharmacother. 2014;15:953–959. doi: 10.1517/14656566.2014.896899. [DOI] [PubMed] [Google Scholar]
- 67.Campochiaro PA, Brown DM, Pearson A, Chen S, Boyer D, Ruiz-Moreno J, Garretson B, Gupta A, Hariprasad SM, Bailey C, et al. Sustained delivery fluocinolone acetonide vitreous inserts provide benefit for at least 3 years in patients with diabetic macular edema. Ophthalmology. 2012;119:2125–2132. doi: 10.1016/j.ophtha.2012.04.030. [DOI] [PubMed] [Google Scholar]
- 68.Photocoagulation treatment of proliferative diabetic retinopathy. Clinical application of Diabetic Retinopathy Study (DRS) findings, DRS Report Number 8. The Diabetic Retinopathy Study Research Group. Ophthalmology. 1981;88:583–600. [PubMed] [Google Scholar]
- 69.Park DH, Shin JP, Kim SY. Comparison of clinical outcomes between 23-gauge and 20-gauge vitrectomy in patients with proliferative diabetic retinopathy. Retina. 2010;30:1662–1670. doi: 10.1097/IAE.0b013e3181d95261. [DOI] [PubMed] [Google Scholar]


