Abstract
Our aim in this paper is to describe the results of treatment of acute lymphoblastic leukaemia (ALL) in Mexican children treated from 2006 to 2010 under the protocol from the Dana-Farber Cancer Institute (DFCI) 00-01. The children were younger than 16 years of age and had a diagnosis of ALL de novo. The patients were classified as standard risk if they were 1–9.9 years old and had a leucocyte count <50 × 109/L, precursor B cell immunophenotype, no mediastinal mass, CSF free of blasts, and a good response to prednisone. The rest of the patients were defined as high risk. Of a total of 302 children, 51.7% were at high risk. The global survival rate was 63.9%, and the event-free survival rate was 52.3% after an average follow-up of 3.9 years. The percentages of patients who died were 7% on induction and 14.2% in complete remission; death was associated mainly with infection (21.5%). The relapse rate was 26.2%. The main factor associated with the occurrence of an event was a leucocyte count >100 × 109/L. The poor outcomes were associated with toxic death during induction, complete remission, and relapse. These factors remain the main obstacles to the success of this treatment in our population.
1. Introduction
Acute lymphoblastic leukaemia (ALL) is the most common cancer in children and adolescents and is the most frequent cancer in Hispanic children including Mexican children [1]. In developed regions, including North America, Eastern Europe, Australia, New Zealand, and Japan, the survival after 5 years is >90% and the cure rate is 85% [2–6]. These results are now possible because of the implementation of clinical assays involving cooperation between countries [7–11]. However, in developing countries, the survival rate is low, possibly because of the lower quality of medical attention [12]. Several factors are included in the classification of risk: clinical, cytogenetic, immunological, and molecular [13–17]. Despite the availability of these factors for classifying risk, in several developing countries the 1993 National Cancer Institute (NCI) criteria [18] continues to be used for the classification of relapse risk. These criteria take into account the age, leucocyte count, immunophenotype, and the recent response to prednisone, the latter of which has been proven as a strong predictor of response in several groups [19–21].
The Dana-Farber Cancer Institute (DFCI) ALL Consortium is a collaborative group that developed clinical assays from 1985 to 2000. The basis of the treatment is 20–30 dosages of asparaginase during intensification and frequent pulses of vincristine and steroid during maintenance. The survival rates obtained from treatments using this protocol were 82% in the 1980s and 88% in the 1990s [22, 23].
In this paper, we report on our results obtained in a group of Mexican children with acute lymphoblastic leukaemia treated with the DFCI 00-01 protocol modified for our local conditions.
2. Patients and Methods
2.1. Patients
From August 2006 to December 2010, paediatric patients with ALL who were younger than 16 years of age and who were treated at the paediatric haematology service at the Centro Médico Nacional “La Raza” IMSS were selected. Patients with a diagnosis of mature cells ALL-B mature were not included. The protocol was approved by the institutional committees, and informed consent was obtained from the parents of each patient.
2.2. Risk Groups
The patients were stratified according to their risk as standard risk (SR) or high risk (HR). SR was defined as patients 1–9.9 years old, leucocyte count <50 × 109/L, precursor B cell phenotype, absence of a mediastinal mass, spinal fluid without blastic cells, and good response to the prednisone window. HR was defined as all patients not in the SR group.
2.3. Therapy
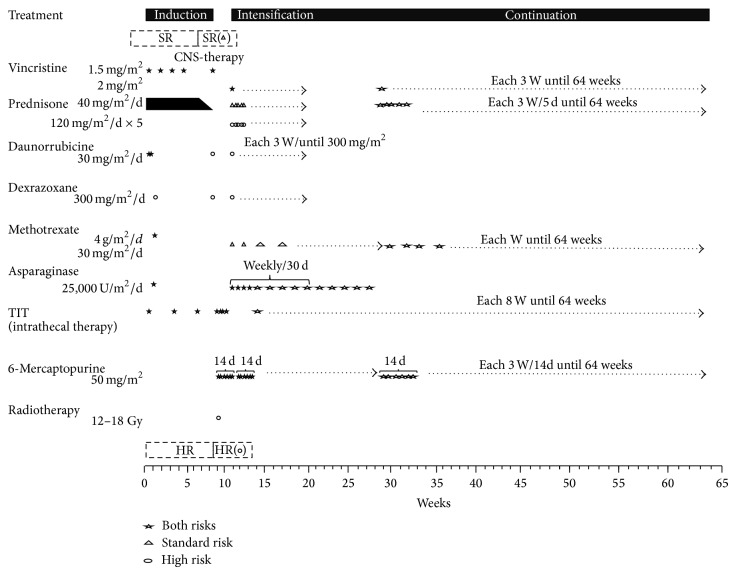
The treatment scheme is shown in Figure 1. Our patients have received the treatment mentioned previously since 1998. At that time, the classification was based on age and leucocyte count. In our hospital, the immunophenotype, cytogenetic study results, and molecular biology data were not available. In this report, we include those patients who were treated under the DFCI 00-01 protocol adapted to the local conditions without a window of investigation. All patients had been treated with a prednisone window comprising 60 mg/m2 SC for 7 days and intrathecal chemotherapy with methotrexate on day 0, and the induction to remission was 4 weeks. The anthracycline drug was daunorubicin instead of doxorubicin. CNS therapy was applied once complete haematological remission was reached. Afterwards, all patients received triple CNS intrathecal chemotherapy two times per week in four dosages adjusted according to the patient's age. The HR patients with major risk of relapse also received radiotherapy (12 Gy) to the brain.
Figure 1.
DCFI 00-01 therapy in paediatric patients with ALL who were younger than 16 years of age and who were treated at the paediatric haematology service of the specialist “La Raza” IMSS Medical Centre.
All patients continued the intensification phase for 30 weeks. For the SR group, vincristine 2 mg/m2 at day 1 and each 3 weeks, asparaginase from Escherichia coli 25,000 UI/m2, and methotrexate 40 mg/m2 by intramuscular injection each week and 1 day after asparaginase were administrated. Prednisone was administered orally at 40 mg/m2 for 5 days and 6-mercaptopurine 50 mg/m2/day for 14 days. The HR group received additional intravenous daunorubicin 30 mg/m2 at day 1 and each three weeks. The stopping dose of daunorubicin was 300 mg/m2, dexrazoxane 300 mg/m2 before daunorubicin, and prednisone 120 mg/m2/day for 5 days. In patients who exhibited an allergic reaction to E. coli asparaginase, the treatment was suspended with no other option because another form of asparaginase was not available in our service. The maintenance was for 64 weeks. Either the SR or HR group the patients had received vincristine, prednisone, 6-mercaptopurine, and methotrexate equally than the intensification, but the HR group had received prednisone to 40 mg/m2 and intrathecal chemotherapy with triple drug every 8 weeks until the treatment was completed.
2.4. Response and Relapse Criteria
The prednisone response was determined using the absolute count of blasts in the peripheral blood on day 8 after 7 days of prednisone and one dose of intrathecal methotrexate on day 1. A poor response to prednisone (PRP) was defined as a blast count of ≥1 × 109/L, and a good response to prednisone (GRP) was defined as a blast count of <1 × 109 blasts. The response of the bone marrow to the induction therapy was evaluated on days 14 and 28. Complete remission was defined as <5% of blasts in bone marrow and without extramedullary disease.
Relapse was defined as an emergence of the disease with ≥25% of blasts in either bone marrow or extramedullary or both. Early death was defined as the death of a patient before evaluation of the remission stage on day 28 or 35 after the induction of remission. Event-free survival was defined as the time to the occurrence of resistance, relapse, death, or a second neoplasm. Global survival was defined as the time in months from the diagnosis to death from any cause or the last contact with the patient in the outpatient clinic or hospital.
2.5. Statistical Analysis
Qualitative variables are presented as absolute numbers or percentages. Quantitative variables are presented as a median value, as a measure of central tendency, and as a range between the minimum and maximum values. For quantitative variables without a normal distribution, the medians were compared using the Mann-Whitney U test for two independent groups. For qualitative variables, the chi-square or Fisher's exact test were used. P < 0.05 was considered to indicate that the difference had a low probability of a random error. The prednisone response was evaluated using a Kaplan-Meier survival analysis and the groups were compared using the log-rank test. Confounding variables in the analysis of the prednisone response were analysed using the Cox proportional-hazard model. All analyses were performed using SPSS statistical package version 21. Two analyses of survival were performed after 3 years and 5 years of follow-up. All of the children had complete data for the 3-year follow-up, but only 158 (52.3%) had data for the 5-year follow-up.
3. Results
A total of 302 children met the inclusion criteria and were included during the study period. There were more boys (53.3% boys). The median age was 7 years, and most of these patients were 1–5-year-old (40.4%). Most patients (92.4%) were classified with the precursor B phenotype.
The most frequent leucocyte count in these patients was <10 × 109/L; the median was 10,790 × 109/L. Interestingly, at the time of diagnosis, only 2.6% had CNS infiltration even though most patients (51.7%) were classified as HR.
Most of the patients had an initial good response to prednisone (80.1%) (Table 1), and 90.4% of these patients had a complete remission. The median follow-up was 3.9 years. The frequency of early mortality was 7%, and the frequency of relapse was 26.2%. Most cases of relapse were early relapse, mainly in the bone marrow (18.2%). The global mortality was 36.1% (Table 2). Because all patients had completed the 3 years of follow-up, the presence of events for relapse and death was estimated for 3 and 5 years.
Table 1.
Demographic and baseline characteristics of the study population (N = 302).
| Characteristic | n | % | Median (m/m) |
|---|---|---|---|
| Total | 302 | 100 | |
| Male | 167 | 53.3 | |
| Female | 135 | 44.7 | |
| Age (years) | 7 (<1–15) | ||
| Age groups (years) | |||
| <1 | 1 | 0.3 | |
| 1–5 | 122 | 40.4 | |
| 5.1–9.99 | 66 | 21.9 | |
| ≥10 | 113 | 37.4 | |
| Immunophenotype | |||
| B | 279 | 92.4 | |
| T | 23 | 7.6 | |
| Leucocyte count (1 × 109/L) | 10,790 (720–939,830) | ||
| Groups of leucocyte count | |||
| <10 | 147 | 48.7 | |
| 10–20 | 48 | 15.9 | |
| 20–50 | 34 | 11.3 | |
| 50–100 | 27 | 8.9 | |
| >100 | 46 | 15.2 | |
| NCS infiltration | 8 | 2.6 | |
| Testicular infiltration | 4 | 1.3 | |
| Prednisone response | |||
| Good | 242 | 80.1 | |
| Poor | 60 | 19.9 | |
| SR | 146 | 48.3 | |
| HR | 156 | 51.7 |
(m/m): minimum/maximum.
Table 2.
Treatment responses (N = 302).
| n | % | median (m/m) | |
|---|---|---|---|
| Complete remission | 273 | 90.4 | |
| Failure | 8 | 2.6 | |
| Early death | 21 | 7.0 | |
| Treatment dropout | 6 | 2.0 | |
| Relapse | |||
| No | 223 | 73.8 | |
| Yes | 79 | 26.2 | |
| Time of relapse | |||
| Very early | 27 | 8.9 | |
| Early | 40 | 13.2 | |
| Late | 12 | 4.0 | |
| Site of relapse | |||
| Bone marrow (BM) | 55 | 18.2 | |
| NCS | 8 | 2.6 | |
| BM + NCS | 13 | 4.3 | |
| Testicle | 3 | 1.0 | |
| Dead | 193 | 63.9 | |
| Alive | 109 | 36.1 | |
| Duration of follow-up (years) | 3.9 (7 days–7.3) |
m/m: minimum/maximum.
3.1. Three-Year Follow-Up (Tables 3, 4, and 5)
Table 3.
Relapses and deaths in paediatric patients with ALL who were younger than 16 years of age and who were treated at the paediatric haematology service of the specialist “La Raza” IMSS Medical Centre.
| N = 302 | Total | Relapse (at 3 years) |
Not Relapse (at 3 years) |
Relapse (at 5 year) |
No Relapse (at 5 years) |
Death (at 3 years) |
Lives (at 3 years) |
Death (at 5 years) |
Lives (at 5 years) |
|---|---|---|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| Sex | |||||||||
| Male (%) | 167 (100) | 41 (24.6) | 126 (75.4) | 51 (30.5) | 116 (69.5) | 48 (28.7) | 119 (71.3) | 54 (32.3) | 113 (67.7) |
| Female (%) | 135 (100) | 26 (19.3) | 109 (80.7) | 28 (20.7) | 107 (79.3) | 44 (32.6) | 91 (67.4) | 52 (38.5) | 83 (61.5) |
| Age (years) | |||||||||
| <1 | 1 (100) | 1 (100) | 0 (0.0) | 1 (100) | 0 (0.0) | 0 (0) | 1 (100) | 1 (100) | 0 (0.0) |
| 1–5 | 122 (100) | 25 (20.5) | 97 (79.5) | 31 (25.4) | 91 (74.0) | 29 (23.8) | 93 (76.2) | 35 (28.7) | 87 (71.3) |
| 5.1–9.99 | 66 (100) | 17 (25.8) | 49 (74.2) | 19 (28.8) | 47 (71.2) | 22 (33.3) | 44 (66.7) | 26 (39.4) | 40 (60.6) |
| ≥10 | 113 (100) | 24 (21.2) | 89 (78.7) | 28 (24.8) | 85 (75.2) | 41 (36.3) | 72 (63.7) | 44 (38.9) | 69 (61.1) |
| Lineage | |||||||||
| B | 279 (100) | 73 (22.6) | 216 (77.4) | 75 (26.9) | 204 (73.1) | 81 (29.0) | 198 (71.0) | 94 (33.7) | 185 (66.3) |
| T | 23 (100) | 4 (17.4) | 19 (82.6) | 4 (17.9) | 19 (82.6) | 11 (47.8) | 12 (52.2) | 12 (52.2) | 11 (47.8) |
| Risk group | |||||||||
| Standard | 146 (100) | 37 (25.3) | 109 (74.7) | 44 (30.1) | 102 (69.9) | 44 (30.1) | 102 (69.9) | 48 (32.9) | 98 (67.1) |
| High | 156 (100) | 30 (19.2) | 126 (80.8) | 35 (22.4) | 121 (77.6) | 48 (30.8) | 108 (69.2) | 58 (37.2) | 98 (62.8) |
| WBC (1 × 109/L) | |||||||||
| <10 | 147 (100) | 34 (23.1) | 113 (76.9) | 38 (25.9) | 109 (74.1) | 40 (27.2) | 107 (72.8) | 43 (29.3) | 104 (70.7) |
| 10–20 | 48 (100) | 10 (20.8) | 38 (79.2) | 14 (29.2) | 34 (70.8) | 18 (37.5) | 30 (62.5) | 20 (41.7) | 28 (58.3) |
| 20–50 | 34 (100) | 3 (8.8) | 31 (91.2) | 5 (14.7) | 29 (85.3) | 11 (32.4) | 23 (67.6) | 12 (35.3) | 22 (64.7) |
| 50–100 000 | 27 (100) | 7 (25.9) | 20 (74.1) | 8 (29.6) | 19 (70.4) | 6 (22.2) | 21 (77.8) | 10 (37.0) | 17 (63.0) |
| ≥100 | 46 (100) | 13 (28.3) | 33 (71.7) | 14 (30.4) | 32 (69.6) | 17 (37.0) | 29 (63.0) | 21 (45.7) | 26 (54.3) |
Table 4.
Events and deaths in paediatric patients with ALL who were younger than 16 years of age and who were treated at the paediatric haematology service of the specialist “La Raza” IMSS Medical Centre.
| Characteristic | Event | Death | ||||||
|---|---|---|---|---|---|---|---|---|
| 3 years | 5 years | 3 years | 5 years | |||||
| No | Yes | No | Yes | No | Yes | No | Yes | |
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| Sex | ||||||||
| Male | 99 (59.3) | 68 (40.7) | 89 (53.3) | 78 (46.7) | 119 (71.3) | 48 (28.7) | 113 (67.7) | 54 (32.3) |
| Female | 78 (57.8) | 57 (42.2) | 72 (53.3) | 63 (46.7) | 91 (67.4) | 44 (32.6) | 83 (61.5) | 52 (38.5) |
| Age (years) | ||||||||
| <1 | 0 (0) | 1 (100) | 0 (0) | 1 (100) | 1 (100) | 0 (100) | 0 (0) | 1 (100) |
| 1–5 | 79 (64.8) | 43 (35.2) | 71 (58.2) | 51 (41.8) | 93 (76.2) | 29 (23.8) | 87 (71.3) | 35 (28.7) |
| 5.1–9.99 | 35 (53.0) | 31 (47.0) | 32 (48.5) | 34 (51.5) | 44 (66.7) | 22 (33.3) | 40 (60.6) | 26 (39.4) |
| ≥10 | 63 (55.8) | 50 (44.2) | 58 (51.3) | 55 (48.7) | 72 (63.7) | 41 (36.3) | 69 (61.1) | 44 (38.9) |
| Immunophenotype | ||||||||
| B | 166 (59.5) | 113 (40.5) | 150 (53.8) | 129 (46.2) | 198 (71.0) | 81 (29.0) | 185 (66.3) | 94 (33.7) |
| T | 11 (47.8) | 12 (52.2) | 11 (47.8) | 12 (52.2) | 12 (52.2) | 11 (47.8) | 11 (47.8) | 12 (52.2) |
| WBC count (1 × 109/L) | ||||||||
| <10 | 91 (61.9) | 56 (38.1) | 87 (59.2) | 60 (40.8) | 107 (72.8) | 40 (27.2) | 104 (70.7) | 43 (29.3) |
| 10–20 | 26 (54.2) | 22 (45.8) | 21 (43.8) | 27 (56.3) | 30 (62.5) | 18 (37.5) | 28 (58.3) | 20 (41.7) |
| 20–50 | 20 (58.8) | 14 (41.2) | 18 (52.9) | 16 (47.1) | 23 (67.6) | 11 (32.4) | 22 (64.7) | 12 (35.3) |
| 50–100 | 17 (63.0) | 10 (37.0) | 16 (59.3) | 11 (40.7) | 21 (77.8) | 6 (22.2) | 17 (63.0) | 10 (37.0) |
| >100 | 23 (50.0) | 23 (50.0) | 19 (41.3) | 27 (58.7) | 29 (63.0) | 17 (37.0) | 25 (54.3) | 21 (45.7) |
| Risk group | ||||||||
| Standard | 84 (57.5) | 62 (42.5) | 76 (52.1) | 70 (47.9) | 102 (69.9) | 44 (30.1) | 98 (67.1) | 48 (32.9) |
| High | 93 (59.6) | 63 (40.4) | 85 (54.3) | 71 (45.5) | 108 (69.2) | 48 (30.8) | 98 (62.8) | 58 (37.2) |
Table 5.
Cox proportional-hazards model. Disease-free survival and death in paediatric patients with ALL who were younger than 16 years of age and who were treated at the paediatric haematology service of the specialist “La Raza” IMSS Medical Centre.
| Characteristic | DFS 3 years | DFS 5 years | Death 3 years | Death 5 years | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RR | 95% CI | P | RR | 95% CI | P | RR | 95% CI | P | RR | 95% CI | P | |
| Sex | ||||||||||||
| Male | ||||||||||||
| Female | 1.202 | 0.839–1.721 | 0.316 | 1.137 | 0.811–1.595 | 0.457 | 1.307 | 0.861–1.984 | 0.208 | 1.413 | 0.956–2.088 | 0.082 |
| Age (years) | ||||||||||||
| <1 | 4.288 | 0.531–34.611 | 0.172 | 3.947 | 0.495–31.454 | 0.195 | 0.000 | 0.000 | 0.000 | 3.616 | 0.446–29.352 | 0.229 |
| 1–5 | 1 | 1 | 1 | 1 | ||||||||
| 5.1–9.99 | 1.504 | 0.942–2.403 | 0.087 | 1.384 | 0.891–2.148 | 0.148 | 1.556 | 0.887–2.728 | 0.123 | 4.573 | 0.940–2.633 | 0.085 |
| >10 | 1.464 | 0.958–2.239 | 0.078 | 1.358 | 0.912–2.021 | 0.132 | 1.699 | 1.036–2.787 | 0.036 | 1.561 | 0.982–2.479 | 0.060 |
| Leucocytes (1 × 109/L) | ||||||||||||
| <10 | ||||||||||||
| 10–20 | 1.302 | 0.792–2.140 | 0.297 | 1.489 | 0.942–2.354 | 0.089 | 1.437 | 0.821–2.516 | 0.205 | 1.495 | 0.876–2.550 | 0.140 |
| 20–50 | 1.193 | 0.655–2.175 | 0.564 | 1.253 | 0.712–2.205 | 0.435 | 1.286 | 0.650–2.545 | 0.470 | 1.322 | 0.688–2.541 | 0.402 |
| 50–100 | 1.133 | 0.520–2.470 | 0.753 | 1.167 | 0.556–2.449 | 0.683 | 0.990 | 0.390–2.510 | 0.982 | 1.374 | 0.620–3.044 | 0.434 |
| >100 | 1.842 | 1.033–3.285 | 0.038 | 2.025 | 1.172–3.496 | 0.011 | 1.604 | 0.833–3.088 | 0.158 | 1.860 | 1.011–3.422 | 0.046 |
| Phenotype | ||||||||||||
| B | ||||||||||||
| T | 1.676 | 0.893–3.145 | 0.108 | 1.479 | 0.794–2.754 | 0.218 | 2.071 | 1.054–4.070 | 0.035 | 1.930 | 1.017–3.664 | 0.044 |
| Risk | ||||||||||||
| Standard | ||||||||||||
| High | 0.765 | 0.481–1.216 | 0.258 | 0.753 | 0.485–1.169 | 0.206 | 0.823 | 0.487–1.388 | 0.464 | 0.830 | 0.503–1.371 | 0.467 |
DFS: disease-free survival; RR: relative risk; CI: confidence interval.
Relapse was more frequent in the boys (24.6%). However, the girls had a higher frequency of events at 42.2%.
The highest relapse frequency was observed in the group aged 5.1–9.9 years (25.8%), who experienced a high frequency of events (47%). The age group with the highest mortality was the group aged >10 years (36.3%; RR 1.70, 95% CI 1.0–2.8).
The patients with the T cell immunophenotype had the highest frequency of death (47.8%; RR 2.1, 95% CI 1.1–4.1).
The SR patients had higher frequencies of relapse (25.3%) and events (42.5%). Most relapses (28.3%) occurred in patients with a leucocyte count >100 × 109/L. This group of patients also had the highest frequency of events (50%; RR 1.84, 95% CI 1.0–3.3). However, 37.5% of the patients who died had a range of leucocyte count of 10–20 × 109/L.
3.2. Five-Year Follow-Up
Boys had a higher frequency of relapse (30.5%), but there was no difference between boys and girls for the frequency of events. The frequency of death was 38.5% in the girls (RR 1.41; 95% CI 1.0–2.1).
The highest frequency of relapse was in the group age >10 years (75.2%) and this group had the highest frequency of events (58.7%).
The highest frequency of relapse was observed in patients with leukaemia of B cell lineage (26.9%). The mortality rate was highest in patients with T cell leukaemia (52.2%; RR 1.93, 95% CI 1.0–3.7).
The SR group had a higher frequency of relapse (30.1%) and higher frequency of events (47.9%). The highest frequency of relapse was observed in the group with a leucocyte count >100 × 109/L (30.4%). This group also had the highest frequency of events (58.7%; RR 2.02, 95% CI 1.2–3.5) and highest mortality (45.7%; RR 1.86, 95% CI 1.0–3.7).
The factor that was most strongly associated with the occurrence of events at the 5-year follow-up was a leucocyte count >100 × 109/L. Leucocyte count and the T cell immunophenotype were also associated with a higher risk of mortality at 5 years.
Of the 302 patients, 21 (7%) died during induction to remission (IR) and 43 (14.2%) died during complete remission. The causes of death were sepsis (65, 21.5%), haemorrhage (9, 8.7%), pneumonia (7, 6.7%), and typhlitis (4, 3.8%). The global mortality was of 36.1%, and 13 (12.5%) died in leukaemic activity. Toxicity associated with asparaginase was observed in 29% of all patients. The most common toxicity was an allergic reaction in 19%, pancreatitis in 7%, thrombosis in 3%, and only one involving the CNS. All of these reactions led to a definitive suspension of the drug.
4. Discussion
In our patient population, which was treated using the DFCI 00-01 protocol, after a median follow-up of 3.9 years, the global survival and event-free survival rates were lower than those obtained from the DFCI Consortium reports in a 5-year follow-up (63.9% and 52.3% versus 90% and 81%, resp., for the group treated with prednisone). There were other differences between our patients and those reported by other groups. For example, in our study, most patients were in the HR group [7–11], which may have influenced our results. The high mortality rate during induction (7%) may be associated with the delayed arrival of the patient at our hospital, bad conditions, tumour load, malnutrition, presence of infection, or toxicity of the treatment [24]. Our results are similar to those reported previously by another centre in Mexico [25] and by a multicentre study in Central America (AHOPCA and Pacheco et al.) [26, 27], which reported mortality rates of 3% and 7% during IR. In our study, 80.1% showed a prednisone good response (PGR), whereas >90% of patients showed a PGR in two other studies (8, 29). To our knowledge, no studies have reported on a diminished response to steroid in the Hispanic population.
Other factors were hyperleukocytosis (15.2%), which has been reported previously. When the leucocyte count is >200 × 109/L [28, 29], the toxicity of the treatment is associated with a high percentage of deaths during complete remission (14.2%) and with the presence of an infectious disease leading to septic shock (21.5%).
A higher frequency of relapse (26.2%) was observed in our patients compared with other studies [22, 23, 29]. The factors associated with relapse at the 3- and 5-year follow-ups in our population were gender (male), age (5.1–9.9 years), B cell lineage, leucocyte count >100 × 109/L), and SR. By contrast, there was a protective effect in the HR group (RR 0.83, 95% CI 0.5–1.4). This finding suggests that determining the risk group using the NCI criteria may be imprecise and that the correct classification of risk is needed for the proper application of therapy to increase the chance that the patient can remain free of events. If precise data are not available (i.e., cytogenetic or molecular biology), a third classification of intermediate risk, as noted previously [5], may be needed. This third classification is based on minimal residual disease (MRD), determined by polymerase chain reaction (PCR) at two times, which redefines all prognostic factors. Attarbaschi et al. [30] showed that only the MRD was reliable enough to discriminate the SR and HR of relapse in a group of patients with ALL of the precursor B cell phenotype (P = 0.02).
In our population, most of the relapses occurred early and were most frequent in bone marrow (18.2%). Studies of MRD have shown that the leukaemic cells found during relapse originate from residual cells and are resistant to chemotherapy [31–33], as was observed in our results (i.e., a high percentage of deaths (12.5%) were associated with leukaemic activity). Other factors that could have influenced the relapse rate in our study were the use of methotrexate (4 g/m2) in a 1 h infusion followed by generous doses of leucovorin, because the levels of monitoring were not available. Mikkelsen et al. [34] reported that shortening the time of infusion of methotrexate reduced the accumulation of active methotrexate in the leukaemic cells and therefore the antileukaemic effect is reduced. Skärby et al. [35] reported that high doses of leucovorin during the treatment with high doses of methotrexate reduced the average cure rate in children with ALL.
The rate of isolated CNS relapse was low (2.6%) and was associated with the intensive use of directed therapy to the CNS (3 IT in IR, 4 in the 2 weeks of the therapy directed to the CNS in a total of 12 until the 24 months of treatment were completed, joined to radiotherapy in the patients with HR) and the systemic chemotherapy, as was proven in clinical assays in the groups of leukaemia: CCG [7], BFM [8], and St. Jude [9]. These studies have shown that if additional therapy is directed to the CNS early, it is possible to replace radiotherapy, which may be reserved only for those patients with a higher risk of relapse or with CNS3 status, because of its secondary effects, which have been observed in long-term survivors of ALL after either chemotherapy or radiotherapy [36–38].
The factors more strongly associated were ages <1 year and >10 years, leucocyte count >100 × 109/L, and T cell phenotype. These factors have also been identified previously as indicators of poor prognosis [23, 28, 29, 39–41]. In our study, the factor most strongly associated with the occurrence of events was a leucocyte count >100 × 109/L. We used this criterion to classify our patients as very high risk and then treated them with more intensive chemotherapy. Our poor results were associated with toxic death during induction, complete remission during treatment, and relapse. Toxicity remains as a main obstacle to the success of treatment of our population. Our results are similar to those reported from other Central American countries (Nicaragua, Costa Rica, El Salvador, Honduras, and Panama) by the AHOPCA ALL 2008 study [26], in which the treatment was based on local regimens adapted from the BFM group to the local situation. We now have two projects underway to reduce the frequency of toxicity in children with ALL, especially in malnourished children.
Several groups have observed that the results of the treatment of children with ALL depend on the biological diversity of the leukaemic cells, the multidrug treatment scheme, and individual variability in the metabolism of the drugs. However, in developing countries, socioeconomic status is also a strong predictor that is independent of the relapse and mortality associated with the treatment [42, 43]. In Mexico, this can be an important factor because most of our patients live far from the treatment centres, which causes delays in the timely management of their disease. Bhatia et al. [44] showed that the lack of adherence to mercaptopurine increased the risk of relapse in Hispanic patients compared with non-Hispanics. Recently, polymorphisms such as ARID5B have been associated with a higher incidence of ALL and greater risk of relapse in Hispanic patients, a finding that may explain the higher incidence and worse results in Hispanic patients [45, 46]. Additionally, there arrangement of CRLF2 associated with mutations in JAK and alterations in IKZF1 in Hispanics may be responsible for the poor response of ALL of B cell lineage [47].
To improve our results, we decided that, during the induction phase, methotrexate should be given at a dose of 1 g/m2 infused for 24 h instead of 4 g/m2 infused for 1 h, and we then changed the dose of leucovorin to 25 mg/m2 SC to 48 and 52 h. And the next dosage should be given according to the level of methotrexate. To improve the stratification of risk, we suggest redefining the risk groups by introducing an intermediate risk group, another HR group, and a very HR group. We also recommend promoting the implementation of reference centres for the cytogenetic and molecular diagnosis of MRD and the formation of national cooperative groups linked to international groups.
We consider that protocol DFCI 00-01 is an excellent of chemotherapy scheme. With the exception of induction, all of the treatments can be applied to outpatients, which will decrease the cost. However, the disadvantage for low- or middle-income countries such as Mexico is the lack of alternatives for asparaginase, which could contribute to the relapse observed in some patients when asparaginase is suspended.
Acknowledgments
This work was funded by the National Council of Science and Technology (CONACyT), Grant 2010-1-141026 and by Mexican Institute of Social Security, Grants FIS/IMSS/PROT/PRIO/11/017 and FIS/IMSS/PROT/G12/1134, (all to Juan Manuel Mejía-Aranguré). Funding to cover the costs of the translation and publishing was provided by the División de Desarrollo de la Investigación del IMSS.
Conflict of Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
References
- 1.Pérez-Saldívar M. L., Fajardo-Gutiérrez A., Bernaldéz-Ríos R., et al. Chilhodhood acute leukemias are frecuent in México City: descriptive epidemiology. BMC Cancer. 2011;11:355–365. doi: 10.1186/1471-2407-11-355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pritchard-Jones K., Pieters R., Reaman G. H., et al. Sustaining innovation and improvement in the treatment of childhood cancer: Lessons from high-income countries. The Lancet Oncology. 2013;14(3):e95–e103. doi: 10.1016/S1470-2045(13)70010-X. [DOI] [PubMed] [Google Scholar]
- 3.Hunger S. P. Expanding clinical trial networks in pediatric acute lymphoblastic leukemia. Journal of Clinical Oncology. 2014;32(3):e169–e170. doi: 10.1200/JCO.2013.53.2754. [DOI] [PubMed] [Google Scholar]
- 4.Hunger S. P., Lu X., Devidas M., et al. Improved survival for children and adolescents with acute lymphoblastic leukemia between 1990 and 2005: a report from the children's oncology group. Journal of Clinical Oncology. 2012;30(14):1663–1669. doi: 10.1200/JCO.2011.37.8018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Conter V., Bartram C. R., Valsecchi M. G., et al. Molecular response to treatment redefines all prognostic factors in children and adolescents with B-cell precursor acute lymphoblastic leukemia: Results in 3184 patients of the AIEOP-BFMALL 2000 study. Blood. 2010;115(16):3206–3214. doi: 10.1182/blood-2009-10-248146. [DOI] [PubMed] [Google Scholar]
- 6.Tsuchida M., Ohara A., Manabe A., et al. Long-term results of Tokyo children's cancer study group trials for childhood acute lymphoblastic leukemia, 1984–1999. Leukemia. 2010;24(2):383–396. doi: 10.1038/leu.2009.260. [DOI] [PubMed] [Google Scholar]
- 7.Gaynon P. S., Angiolillo A. L., Carroll W. L., et al. Long-term results of the children's cancer group studies for childhood acute lymphoblastic leukemia 1983–2002: a children's oncology group report. Leukemia. 2010;24(2):285–297. doi: 10.1038/leu.2009.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Möricke A., Zimmermann M., Reiter A., et al. Long-term results of five consecutive trials in childhood acute lymphoblastic leukemia performed by the ALL-BFM study group from 1981 to 2000. Leukemia. 2010;24(2):265–284. doi: 10.1038/leu.2009.257. [DOI] [PubMed] [Google Scholar]
- 9.Pui C. H., Pei D., Sandlund J. T., et al. Long-term results of st jude total therapy studies 11, 12, 13A, 13B, and 14 for childhood acute lymphoblastic leukemia. Leukemia. 2010;24(2):371–382. doi: 10.1038/leu.2009.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Silverman L. B., Stevenson K. E., O'Brien J. E., et al. Long-term results of dana-farber cancer institute all consortium protocols for children with newly diagnosed acute lymphoblastic leukemia (1985–2000) Leukemia. 2010;24(2):320–334. doi: 10.1038/leu.2009.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Conter V., Aricò M., Basso G., et al. Long-term results of the Italian association of pediatric hematology and oncology (AIEOP) Studies 82, 87, 88, 91 and 95 for childhood acute lymphoblastic leukemia. Leukemia. 2010;24(2):255–264. doi: 10.1038/leu.2009.250. [DOI] [PubMed] [Google Scholar]
- 12.Magrath I., Steliarova-Foucher E., Epelman S., et al. Paediatric cancer in low-income and middle-income countries. The Lancet Oncology. 2013;14(3):e104–e116. doi: 10.1016/S1470-2045(13)70008-1. [DOI] [PubMed] [Google Scholar]
- 13.Möricke A., Reiter A., Zimmermann M., et al. Risk- ajusted therapy of acute lymphoblastic leukemia can decrece treatment burden and improve survival: treatment results of 2169 unselected pediatric and adolescent patients in the trial ALL-BFM 95. Blood. 2008;111:4477–4489. doi: 10.1182/blood-2007-09-112920. [DOI] [PubMed] [Google Scholar]
- 14.Flohr T., Schrauder A., Cazzaniga G., et al. Minimal residual disease-directed risk stratification using real-time quantitative PCR analysis of immunoglobulin and T-cell receptor gene rearrangements in the international multicenter trial AIEOP-BFM ALL 2000 for childhood acute lymphoblastic leukemia. Leukemia. 2008;22(4):771–782. doi: 10.1038/leu.2008.5. [DOI] [PubMed] [Google Scholar]
- 15.Schrappe M., Valsecchi M. G., Bartram C. R., et al. Late MRD response determines relapse risk overall and in subsets of childhood T-cell ALL: results of the AIEOP-BFM-ALL 2000 study. Blood. 2011;118(8):2077–2084. doi: 10.1182/blood-2011-03-338707. [DOI] [PubMed] [Google Scholar]
- 16.Moorman A. V., Ensor H. M., Richards S. M., et al. Prognostic effect of chromosomal abnormalities in childhood B-cell precursor acute lymphoblastic leukaemia: results from the UK Medical Research Council ALL97/99 randomised trial. The Lancet Oncology. 2010;11(5):429–438. doi: 10.1016/S1470-2045(10)70066-8. [DOI] [PubMed] [Google Scholar]
- 17.Sutcliffe M. J., Shuster J. J., Sather H. N., et al. High concordance from independent studies by the Children's Cancer Group (CCG) and Pediatric Oncology Group (POG) associating favorable prognosis with combined trisomies 4, 10, and 17 in children with NCI Standard-Risk B-precursor Acute Lymphoblastic Leukemia: a Children's Oncology Group (COG) initiative. Leukemia. 2005;19(5):734–740. doi: 10.1038/sj.leu.2403673. [DOI] [PubMed] [Google Scholar]
- 18.Smith M., Arthur D., Camitta B., et al. Uniform approach to risk classification and treatment assignment for children with acute lymphoblastic leukemia. Journal of Clinical Oncology. 1996;14(1):18–24. doi: 10.1200/JCO.1996.14.1.18. [DOI] [PubMed] [Google Scholar]
- 19.Lauten M., Cario G., Asgedom G., Welte K., Schrappe M. Protein expression of the glucocorticoid receptor in childhood acute lymphoblastic leukemia. Haematologica. 2003;88(11):1253–1258. [PubMed] [Google Scholar]
- 20.Dördelmann M., Reiter A., Borkhardt A., et al. Prednisone response is the strongest predictor of treatment outcome in infant acute lymphoblastic leukemia. Blood. 1999;94(4):1209–1217. [PubMed] [Google Scholar]
- 21.Manabe A., Ohara A., Hasegawa D., et al. Significance of the complete clearance of peripheral blasts after 7 days of prednisolone treatment in children with acute lymphoblastic leukemia: the Tokyo Children's Cancer Study Group Study L99-15. Haematologica. 2008;93(8):1155–1160. doi: 10.3324/haematol.12365. [DOI] [PubMed] [Google Scholar]
- 22.LeClerc J. M., Billett A. L., Gelber R. D., et al. Treatment of childhood acute lymphoblastic leukemia: results of Dana-Farber ALL Consortium Protocol 87-01. Journal of Clinical Oncology. 2002;20(1):237–246. doi: 10.1200/JCO.20.1.237. [DOI] [PubMed] [Google Scholar]
- 23.Moghrabi A., Levy D. E., Asselin B., et al. Results of the dana-farber cancer institute all consortium protocol 95-01 for children with acute lymphoblastic leukemia. Blood. 2007;109(3):896–904. doi: 10.1182/blood-2006-06-027714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vrooman L. M., Stevenson K. E., Supko J. G., et al. Postinduction dexamethasone and individualized dosing of Escherichia coli l-asparaginase each improve outcome of children and adolescents with newly diagnosed acute lymphoblastic leukemia: Results from a randomized study-Dana-Farber Cancer Institute ALL Consortium Protocol 00-01. Journal of Clinical Oncology. 2013;31(9):1202–1210. doi: 10.1200/JCO.2012.43.2070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.López-Facundo N. A., Talavera-Piña J., Tejocote-Romero I. Mortalidad temprana en niños con leucemia linfoblástica aguda en un país en vías de desarrollo; factores asociados con el pronóstico. GAMO. 2008;7(3):93–101. [Google Scholar]
- 26.Navarrete M., Rossi E., Brivio E., et al. Treatment of childhood acute lymphoblastic leukemia in central America: a lower-middle income countries experience. Pediatric Blood and Cancer. 2014;61(5):803–809. doi: 10.1002/pbc.24911. [DOI] [PubMed] [Google Scholar]
- 27.Pacheco C., Lucchini G., Valsecchi M. G., et al. Childhood acute lymphoblastic leukemia in Nicaragua: long-term results in the context of an International Cooperative Program. Pediatric Blood and Cancer. 2014;61(5):827–832. doi: 10.1002/pbc.24871. [DOI] [PubMed] [Google Scholar]
- 28.Kong S. G., Seo J. H., Jun S. E., Lee B. K., Lim Y. T. Childhood acute lymphoblastic leukemia with hyperleukocytosis at presentation. Blood Research. 2014;49(1):29–35. doi: 10.5045/br.2014.49.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lowe E. J., Pui C.-H., Hancock M. L., Geiger T. L., Khan R. B., Sandlund J. T. Early complications in children with acute lymphoblastic leukemia presenting with hyperleukocytosis. Pediatric Blood & Cancer. 2005;45(1):10–15. doi: 10.1002/pbc.20178. [DOI] [PubMed] [Google Scholar]
- 30.Attarbaschi A., Mann G., Panzer-Grümayer R., et al. Minimal residual disease values discriminate between low and high relapse risk in children with B-cell precursor acute lymphoblastic leukemia and an intrachromosomal amplification of chromosome 21: the Austrian and German acute lymphoblastic leukemia Berlin-Frankfurt-Münster (ALL-BFM) trials. Journal of Clinical Oncology. 2008;26(18):3046–3050. doi: 10.1200/JCO.2008.16.1117. [DOI] [PubMed] [Google Scholar]
- 31.Bailey L. C., Lange B. J., Rheingold S. R., Bunin N. J. Bone-marrow relapse in paediatric acute lymphoblastic leukaemia. The Lancet Oncology. 2008;9(9):873–883. doi: 10.1016/S1470-2045(08)70229-8. [DOI] [PubMed] [Google Scholar]
- 32.Bader P., Kreyenberg H., Henze G. H. R., et al. Prognostic value of minimal residual disease quantification before allogeneic stem-cell transplantation in relapsed childhood acute lymphoblastic leukemia: the ALL-REZ BFM Study Group. Journal of Clinical Oncology. 2009;27(3):377–384. doi: 10.1200/JCO.2008.17.6065. [DOI] [PubMed] [Google Scholar]
- 33.Einsiedel H. G., von Stackelberg A., Hartmann R., et al. Long-term outcome in children with relapsed ALL by risk-stratified salvage therapy: results of trial Acute Lymphoblastic Leukemia-Relapse Study of the Berlin-Frankfurt-Münster Group 87. Journal of Clinical Oncology. 2005;23(31):7942–7950. doi: 10.1200/JCO.2005.01.1031. [DOI] [PubMed] [Google Scholar]
- 34.Mikkelsen T. S., Sparreboom A., Cheng C., et al. Shortening infusion time for high-dose methotrexate alters antileukemic effects: a randomized prospective: clinical trial. Journal of Clinical Oncology. 2011;29(13):1771–1778. doi: 10.1200/JCO.2010.32.5340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Skärby T. V. C., Anderson H., Heldrup J., Kanerva J. A., Seidel H., Schmiegelow K. High leucovorin doses during high-dose methotrexate treatment may reduce the cure rate in childhood acute lymphoblastic leukemia. Leukemia. 2006;20(11):1955–1962. doi: 10.1038/sj.leu.2404404. [DOI] [PubMed] [Google Scholar]
- 36.Langer T., Martus P., Ottensmeier H., Hertzberg H., Beck J. D., Meier W. CNS late-effects after ALL therapy in childhood. Part III: neuropsychological performance in long-term survivors of childhood ALL: impairments of concentration, attention, and memory. Medical and Pediatric Oncology. 2002;38(5):320–328. doi: 10.1002/mpo.10055. [DOI] [PubMed] [Google Scholar]
- 37.Goldsby R. E., Liu Q., Nathan P. C., et al. Late-occurring neurologic sequelae in adult survivors of childhood acute lymphoblastic leukemia: a report from the childhood cancer survivor study. Journal of Clinical Oncology. 2010;28(2):324–331. doi: 10.1200/JCO.2009.22.5060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Singla A., O'Neill J. E. B., Smith E., Scott R. M. Cavernous malformations of the brain after treatment for acute lymphocytic leukemia: Presentation and long-term follow-up: clinical article. Journal of Neurosurgery: Pediatrics. 2013;11(2):127–132. doi: 10.3171/2012.11.PEDS12235. [DOI] [PubMed] [Google Scholar]
- 39.Stock W., La M., Sanford B., et al. What determines the outcomes for adolescents and young adults with acute lymphoblastic leukemia treated on cooperative group protocols? A comparison of children'scancer group and cancer an leukemia Group B studies. Blood. 2008;112(5):1646–1654. doi: 10.1182/blood-2008-01-130237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Möricke A., Zimmermann M., Reiter A., et al. Prognostic impact of age in children and adolescents with acute lymphoblastic leukemia: data from the trials ALL-BFM 86, 90, and 95. Klinische Padiatrie. 2005;217(6):310–320. doi: 10.1055/s-2005-872515. [DOI] [PubMed] [Google Scholar]
- 41.Goldberg J. M., Silverman L. B., Levy D. E., et al. Childhood T-cell acute lymphoblastic leukemia: the Dana-Farber Cancer Institute Acute Lymphoblastic Leukemia Consortium experience. Journal of Clinical Oncology. 2003;21(19):3616–3622. doi: 10.1200/JCO.2003.10.116. [DOI] [PubMed] [Google Scholar]
- 42.Gupta S., Antillon F. A., Bonilla M., et al. Treatment-related mortality in children with acute lymphoblastic leukemia in Central America. Cancer. 2011;117(20):4788–4795. doi: 10.1002/cncr.26107. [DOI] [PubMed] [Google Scholar]
- 43.Viana M. B., Fernandes' R. A. F., De Carvalho R. I., Murao M. Low socioeconomic status is a strong independent predictor of relapse in childhood acute lymphoblastic leukemia. International Journal of Cancer. 1998;78(11):56–61. [PubMed] [Google Scholar]
- 44.Bhatia S., Landier W., Shangguan M., et al. Nonadherence to oral mercaptopurine and risk of relapse in hispanic and non-hispanic white children with acute lymphoblastic leukemia: a report from the Children's Oncology Group. Journal of Clinical Oncology. 2012;30(17):2094–2101. doi: 10.1200/JCO.2011.38.9924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Xu H., Cheng C., Devidas M., et al. ARID5B genetic polymorphisms contribute to racial disparities in the incidence and treatment outcome of childhood acute lymphoblastic leukemia. Journal of Clinical Oncology. 2012;30(7):751–757. doi: 10.1200/JCO.2011.38.0345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chokkalingam A. P., Hsu L. I., Metayer C., et al. Genetic variants in ARID5B and CEBPE are childhood ALL susceptibility loci in Hispanics. Cancer Causes and Control. 2013;24(10):1789–1795. doi: 10.1007/s10552-013-0256-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Harvey R. C., Mullighan C. G., Chen I.-M., et al. Rearrangement of CRLF2 is associated with mutation of JAK kinases, alteration of IKZF1, Hispanic/Latino ethnicity, and a poor outcome in pediatric B-progenitor acute lymphoblastic leukemia. Blood. 2010;115(26):5312–5321. doi: 10.1182/blood-2009-09-245944. [DOI] [PMC free article] [PubMed] [Google Scholar]