Abstract
Objective
To evaluate the validity of the International Classification of Diseases, 10th Revision (ICD-10) diagnosis code for hyponatraemia (E87.1) in two settings: at presentation to the emergency department and at hospital admission.
Design
Population-based retrospective validation study.
Setting
Twelve hospitals in Southwestern Ontario, Canada, from 2003 to 2010.
Participants
Patients aged 66 years and older with serum sodium laboratory measurements at presentation to the emergency department (n=64 581) and at hospital admission (n=64 499).
Main outcome measures
Sensitivity, specificity, positive predictive value and negative predictive value comparing various ICD-10 diagnostic coding algorithms for hyponatraemia to serum sodium laboratory measurements (reference standard). Median serum sodium values comparing patients who were code positive and code negative for hyponatraemia.
Results
The sensitivity of hyponatraemia (defined by a serum sodium ≤132 mmol/l) for the best-performing ICD-10 coding algorithm was 7.5% at presentation to the emergency department (95% CI 7.0% to 8.2%) and 10.6% at hospital admission (95% CI 9.9% to 11.2%). Both specificities were greater than 99%. In the two settings, the positive predictive values were 96.4% (95% CI 94.6% to 97.6%) and 82.3% (95% CI 80.0% to 84.4%), while the negative predictive values were 89.2% (95% CI 89.0% to 89.5%) and 87.1% (95% CI 86.8% to 87.4%). In patients who were code positive for hyponatraemia, the median (IQR) serum sodium measurements were 123 (119–126) mmol/l and 125 (120–130) mmol/l in the two settings. In code negative patients, the measurements were 138 (136–140) mmol/l and 137 (135–139) mmol/l.
Conclusions
The ICD-10 diagnostic code for hyponatraemia differentiates between two groups of patients with distinct serum sodium measurements at both presentation to the emergency department and at hospital admission. However, these codes underestimate the true incidence of hyponatraemia due to low sensitivity.
Keywords: Epidemiology, Adult nephrology < Nephrology
Article summary.
Article focus
Validation of administrative database codes is necessary to guide their use in health outcomes research.
The aim of this study was to describe the validity of the ICD-10 diagnostic code for hyponatraemia compared to serum sodium measurements, the latter serving as the reference standard.
Key messages
The International Classification of Diseases, 10th Revision diagnostic code for hyponatraemia has low sensitivity but high specificity.
The code was successful in differentiating between two groups of patients with distinct serum sodium measurements.
Strengths and limitations of this study
This is the first study to validate the International Classification of Diseases, 10th Revision code for hyponatraemia.
It was a large population-based study that included serum sodium values from multiple hospitals.
Studies describing code validity in younger patients are needed.
Introduction
Large health administrative databases are widely used in pharmacoepidemiological and health services research.1 They offer several advantages including increased efficiency and large sample sizes. Despite their usefulness, an important limitation of these databases is that researchers frequently rely on hospital-based diagnostic codes contained within the databases to define conditions of interest, rather than reference standard diagnoses.2 The inaccuracy of codes may introduce measurement error which has a number of implications including underestimation of the true incidence of a condition. Accordingly, understanding the validity of various diagnostic codes remains of paramount importance.
Hyponatraemia is an electrolyte disorder and is generally defined by a low serum sodium concentration3 4 It is one of the most common types of abnormalities of its kind affecting 15–30% of hospitalised patients.5 6 Depending on its severity and rapidity of onset, hyponatraemia has been associated with morbidities such as confusion, seizures, falls, fractures as well as mortality.7–9 There are a number of causes of hyponatraemia such as dehydration from prolonged vomiting, congestive heart failure, some forms of kidney disease and medication use (eg, diuretics).
To date, the validity of the International Classification of Diseases, Ninth Revision (ICD-9) code for hyponatraemia has been described in two studies. Movig et al10 compared discharge records for hospitalised patients with laboratory data and found sensitivities of 1.7% and 13.4% for serum sodium measurements ≤135 and ≤125 mmol/l, respectively. Specificities were greater than 99%. Shea et al11 evaluated outpatient records against laboratory measurements and reported sensitivities of 3.5% and 29.6% using the same thresholds to define hyponatraemia. Specificities remained high at over 99%.
ICD-10 was introduced in Canada in 2002 and is currently used by 117 countries worldwide.12 To date, there has been no validation of the ICD-10 code for hyponatraemia. Therefore, the goal of our study was to evaluate the validity of the ICD-10 diagnosis code for hyponatremia (E87.1) in two settings: at presentation to the emergency department and at hospital admission.
Methods
Study design and setting
We conducted a population-based retrospective validation study using the health administrative databases and laboratory data in Southwestern Ontario, Canada. These data come from 12 hospitals that serviced a catchment area of approximately 80 000 adults aged 65 and older in 2006 (most recent available census information).13 All residents received universal access to hospital and physician services. Coverage for medical services and medications from a single provincial payer provided a comprehensive set of health administrative data.
Using a diagnostic test assessment framework, we obtained metrics of sensitivity, specificity, positive predictive value and negative predictive value comparing various ICD-10 diagnostic coding algorithms for hyponatraemia to serum sodium laboratory measurements (the latter serving as the reference standard; see online supplementary appendix A for sample two-by-two table). Since serum sodium concentration is a continuous measure, we also compared these values in patients who were code positive with those who were code negative. We conducted our study according to a prespecified protocol that was approved by the institutional review board at Sunnybrook Health Sciences Centre (Toronto, Ontario). The relevant datasets and the analyses were held and conducted at the Institute for Clinical Evaluative Sciences. The reporting of this study follows guidelines set out for studies on diagnostic accuracy (see online supplementary appendix B).14
Data sources
Records from seven databases were linked using encrypted unique identifiers. We identified laboratory measurements, including serum sodium using Cerner (Kansas City, Missouri, USA), a system that keeps patient electronic medical records.13 15 This system contains inpatient, outpatient and emergency room laboratory measurements. We identified emergency department visits using the National Ambulatory Care Reporting System (NACRS) database, and inpatient hospital admissions using the Canadian Institutes of Health Information Discharge Abstract Database (CIHI-DAD). These databases contain detailed diagnostic and procedural information coded using ICD-9 (pre-2002) and ICD-10 (post-2002). We obtained patient demographic data from the Registered Persons Database, which contains demographic information on all Ontarians ever issued a health card. We collected additional covariate information from the CIHI-DAD, the Ontario Health Insurance Plan database, which contains health claims information for both inpatient and outpatient services and the Ontario Drug Benefits database, which contains highly accurate records of all outpatient prescriptions dispensed to patients ≥65 years of age (error rate <1%).16 For a subpopulation, we also obtained baseline laboratory measurements prior to hospital encounters from Gamma-Dynacare, a provider of outpatient laboratory services to residents in Southwestern Ontario. These databases have been used extensively to research health outcomes and health services.17–20
Participants
In order to assess the validity of the hyponatraemia code, we created two separate cohorts restricting cohort entry to patients with at least one serum sodium measurement at presentation to an emergency department or at hospital admission, respectively. These measurements were available beginning 1 June 2003, which is when we began accrual for the study and continued to 30 September 2010. To ensure all participants had at least one full year of medication use data, we restricted entry to those aged 66 years and older at the time of the serum sodium measurement. The selection criteria are described below and outlined in online supplementary appendix C.
We excluded measurements when the date of an emergency department or inpatient serum sodium test did not align with an emergency department visit or inpatient hospital admission included in the administrative databases (see online supplementary appendix C for alignment definitions). To ensure we had data for the full hospital admission to the time of discharge (particularly for patients accrued in the second half of 2010) we excluded admissions where the duration of the visit exceeded 90 days. As such, study follow-up occurred until 31 December 2010. To assess hyponatraemia upon presentation to the emergency department, patients had to have at least one emergency department serum sodium measurement on the day of or 1 day after the emergency department registration date. To assess hyponatraemia at hospital admission, we restricted to patients who had at least one emergency department serum sodium measurement 2 days prior to the hospital admission date or one inpatient serum sodium measurement the day of or 1 day after the hospital admission date. For both settings, when multiple serum sodium tests were performed, we selected the lowest value to define the presence of hyponatraemia. In cases where multiple emergency department visits or hospital encounters were identified per patient over the study period, we randomly selected one visit/encounter. We denoted the emergency department registration date or inpatient hospital admission date as the index date.
Diagnostic test (hyponatraemia ICD-10 coding algorithms)
In Canada, trained coders record appropriate diagnostic codes and their associated attributes based on information from a patient's chart. Coders follow the Canadian Coding Standards developed by CIHI.21 Based on these guidelines, coders are not permitted to interpret laboratory test results but can record a laboratory-based condition if the physician has documented the diagnosis in the medical chart. Within the NACRS database, coders are allowed to include up to 10 diagnoses per visit. The first diagnosis listed is the main problem for the client's visit that required evaluation and/or treatment or management as determined by the physician at the end of the visit. CIHI-DAD provides the ability to record up to 25 diagnoses, each with a corresponding diagnosis type. For example, a diagnosis type of ‘M’ is used to refer to the diagnosis that was most responsible for the greatest portion of the length of stay or greatest use of resources, while a diagnosis type of ‘1’ refers to a condition that existed prior to admission.
In this study, we developed two unique algorithms to assess hyponatraemia at presentation to the emergency department and four unique algorithms at hospital admission based on possible diagnosis types. We used the ICD-10 code E87.1, which is defined as ‘hypo-osmolality and hyponatraemia’. The two emergency department algorithms identified records with code E87.1 recorded: (1) as the main problem (referred to as ‘main diagnosis’), or (2) in any of the 10 potential diagnostic fields (referred to as ‘all diagnosis’). The four hospital admission algorithms identified records with code E87.1 recorded: (1) with the diagnosis type of ‘M’ (most responsible) (referred to as ‘most responsible diagnosis’), (2) with the diagnosis type of ‘1’ (pre-admit comorbidity) or ‘W’, ‘X’ or ‘Y’ (service transfer diagnosis) (referred to as ‘admission diagnosis’), (3) with a diagnosis type of ‘M’ and a diagnosis type of ‘1’ (referred to as ‘admission diagnosis and most responsible diagnosis’) or (4) in any one of 25 potential diagnosis fields and any diagnosis type (referred to as ‘all diagnosis’).
Reference standard (serum sodium values)
Serum sodium was analysed in the laboratory using a Roche Modular Ion Selective Electrode system (Basel, Switzerland). We considered four thresholds when defining our reference standard of hyponatraemia: serum sodium <135, ≤132, ≤130 and ≤125 mmol/l. Our primary definition of hyponatraemia was a serum sodium ≤132 mmol/l while the other definitions were explored to investigate the impact of disease severity.7–8
Statistical analysis
We used descriptive statistics to summarise demographic characteristics, comorbidities, prescription drug claim information and prior laboratory testing for patients in both settings. We calculated sensitivity, specificity, positive predictive value and negative predictive value for each diagnostic coding algorithm (formulas presented in online supplementary appendix A). We calculated 95% CI for single proportions using the Wilson Score method.22 We repeated these calculations for each hyponatraemia threshold. We expressed continuous variables as medians with IQR. We compared means using independent samples t-tests. We conducted all analysis using SAS (Statistical Analysis Software) V.9.2 (SAS Institute Incorporated, Cary, North Carolina, USA, 2008).
Results
Over the 7 year study period, there were a total of 64 581 patients with serum sodium measurements at presentation to the emergency department and 64 499 at hospital admission. Of these patients, 7446 (11.5%) and 9135 (14.2%) had serum sodium measurements ≤132 mmol/l, respectively. Baseline characteristics of the two cohorts are presented in table 1. The median age of the patients on the index date was 77 years and just over half the patients were women. Over 50% of each cohort had serum sodium measurements available prior to the index date and mean values were normal (table 1).
Table 1.
Baseline characteristics for patients with serum sodium measurements obtained at presentation to the emergency department and at hospital admission
| Emergency department (n=64 581) | Hospital admission (n=64 499) | |
|---|---|---|
| Demographics | ||
| Median age (IQR), years | 77 (71–83) | 77 (71–83) |
| Women, n (%) | 35631 (55.2) | 32965 (51.1) |
| Income Quintile, n (%) | ||
| One (lowest) | 14224 (22.0) | 13879 (21.5) |
| Two | 12862 (19.9) | 12974 (20.1) |
| Three (middle) | 12564 (19.5) | 12795 (19.8) |
| Four | 11511 (17.8) | 11601 (18.0) |
| Five (highest) | 12431 (19.3) | 12435 (19.3) |
| Year of cohort entry*, n (%) | ||
| 2003–2004 | 6535 (10.1) | 11599 (18.0) |
| 2005–2006 | 15208 (23.6) | 15639 (24.3) |
| 2007–2008 | 20586 (31.9) | 18437 (28.6) |
| 2009–2010 | 22252 (34.5) | 18824 (29.2) |
| Rural location, n (%) | 11417 (17.7) | 13268 (20.6) |
| From a long-term care facility, n (%) | 4147 (6.4) | 3674 (5.7) |
| Comorbidities†, n (%) | ||
| Chronic kidney disease | 5339 (8.3) | 6399 (9.9) |
| Diabetes mellitus‡ | 13148 (20.4) | 13640 (21.2) |
| Peripheral vascular disease | 1685 (2.6) | 2940 (4.6) |
| Coronary artery disease§ | 26963 (41.8) | 30608 (47.5) |
| Congestive heart failure | 13674 (21.2) | 15249 (23.6) |
| Systemic malignancy¶ | 27003 (41.8) | 29835 (46.3) |
| Stroke/transient ischaemic attack | 2508 (3.9) | 2671 (4.1) |
| Chronic liver disease | 1217 (1.9) | 1684 (2.6) |
| Medication use in preceding 6 months, n (%) | ||
| Angiotensin-converting enzyme inhibitor | 22706 (35.2) | 23759 (36.8) |
| Angiotensin-receptor blocker | 10474 (16.2) | 10005 (15.5) |
| Potassium sparing diuretic | 5699 (8.8) | 6166 (9.6) |
| Non-potassium sparing diuretic | 25930 (40.2) | 27144 (42.1) |
| Calcium channel blocker | 19092 (29.6) | 19895 (30.9) |
| β-Adrenergic antagonist | 21957 (34.0) | 23417 (36.3) |
| Statins | 24873 (38.5) | 25303 (39.2) |
| NSAIDs (excluding aspirin) | 11637 (18.0) | 12530 (19.4) |
| Anticonvulsants | 3828 (5.9) | 3733 (5.8) |
| Antidepressants | 15710 (24.3) | 15102 (23.4) |
| Antipsychotics | 3944 (6.1) | 3611 (5.6) |
| Benzodiazepines | 15274 (23.7) | 15532 (24.1) |
| Antineoplastic agents | 3280 (5.1) | 3631 (5.6) |
| Hypothyroidism agents | 10444 (16.2) | 9954 (15.4) |
| Baseline laboratory measurements** | ||
| Serum sodium levels, mmol/l | ||
| Median (IQR) | 139 (137–141) | 139 (137–141) |
| Range | 95–180 | 95–173 |
| Hyponatraemia category, n (%) | ||
| <135 mmol/l | 5587 (17.0) | 6561 (16.7) |
| ≤132 mmol/l | 2064 (6.3) | 2397 (6.1) |
| ≤130 mmol/l | 1030 (3.1) | 1169 (3.0) |
| ≤125 mmol/l | 130 (0.4) | 171 (0.4) |
| Serum potassium levels, mmol/l, median (IQR) | 4.2 (3.8–4.5) | 4.1 (3.8–4.5) |
| Serum creatine levels, µmol/l, median (IQR) | 90 (74–114) | 90 (74–114) |
| eGFR ml/min/1.73 m2††, median (IQR) | 62.8 (46.6–78.6) | 63.1 (46.9–78.9) |
| eGFR category, n (%) | ||
| ≥60 ml/min/1.73 m2 | 20809 (54.7) | 23726 (55.1) |
| 45–59 ml/min/1.73 m2 | 8521 (22.4) | 9600 (22.3) |
| 30–44 ml/min/1.73 m2 | 5520 (14.5) | 6036 (14.0) |
| 15–29 ml/min/1.73 m2 | 2368 (6.2) | 2687 (6.2) |
| <15 ml/min/1.73 m2 | 842 (2.2) | 1035 (2.4) |
*The year of cohort entry is also referred to as the index date.
†Assessed by administrative database ICD-9 and ICD-10 codes in the 5 years prior to the hospital encounter (unless stated otherwise).
‡Assessed by diabetic medication use (oral hypoglycaemic or insulin use) in previous 6 months.
§Coronary artery disease includes receipt of coronary artery bypass graft surgery, percutaneous coronary intervention and diagnoses of angina.
¶Includes the following types of malignancies: skin, mouth (lip, tonsil, etc), throat, stomach, small/large intestine, liver, gall bladder, pancreas, breast, male/female reproductive organs, heart, lung, bone, urinary system (kidney, bladder, etc), endocrine glands, as well as leukaemias and lymphomas.
**Available for a subpopulation. Emergency Department cohort: A total of 32 916 (51.0%), 33 190 (51.4%) and 38 060 (58.9%) of the 64 581 patients had a most recent baseline serum sodium, potassium and creatine measurement available in the 7–365 days prior to the index date, respectively. Among these patients, the baseline measurements were taken at a median (IQR) of 75 (26–175), 75 (26–175) and 76 (27–173) days prior to the index date, respectively. Hospital Admission cohort: a total of 39 373 (61.0%), 39 502 (61.2%) and 43 084 (66.8%) of the 64 499 patients had a most recent baseline serum sodium, potassium and creatine measurement available in the 7–365 days prior to the index date, respectively. Among these patients, the baseline measurements were taken at a median (IQR) of 29 (14–97), 29 (14–97) and 31 (14–101) days prior to the index date, respectively.
††eGFR was calculated using the CKD-Epi equation.
CKD-Epi equation: 141×min((serum creatine in μmol/l/88.4 )/κ, 1)α×max((serum creatine in μmol/l/88.4)/κ, 1)−1.209×0.993Age×1.018 (if female)×1.159 (if African American) κ=0.7 for females and 0.9 for males, α=−0.329 for females and −0.411 for males, min=the minimum of Scr/κ or 1, max=the maximum of Scr/κ or 1. Racial information was not available in our data sources and all patients were assumed not to be of non African-Canadian race. This was a reasonable assumption; as of 2006, African-Canadians represented less than 7% of the Ontario population. Source: http://www12.statcan.ca/census-recensement/2006/dp-pd/hlt/97–562/index.cfm?Lang=E.
eGFR, estimated glomerular filtration rate; NSAID, non-steroidal anti-inflammatory drugs.
The sensitivity of hyponatraemia when defined by a serum sodium ≤132 mmol/l was highest when considering evidence of code E87.1 among all potential diagnoses for both settings: at presentation to emergency department, 7.5% (95% CI 7.0% to 8.2%) and at hospital admission, 10.6% (95% CI 9.9% to 11.2%). In both settings the specificities were greater than 99%. The positive predictive values were 96.4% (95% CI 94.6% to 97.6%) and 82.3% (95% CI 80.0% to 84.4%) and the negative predictive values were 89.2% (95% CI 89.0% to 89.5%) and 87.1% (95% CI 86.8% to 87.4%), respectively (table 2).
Table 2.
Performance of the ICD-10 coding algorithms for hyponatraemia using a serum sodium measurement as the reference standard
| Reference standard hyponatraemia (≤132 mmol/l) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Emergency department |
Hospital admission |
||||||||
| ICD-10 E87.1 coding algorithms | + | − | Performance measures % | 95% CI | + | − | Performance measures % | 95% CI | |
| All diagnosis | + | 561 | 21 | Sn=7.53 | 6.96 to 8.16 | 964 | 207 | Sn=10.55 | 9.94 to 11.20 |
| Sp=99.96 | 99.94 to 99.98 | Sp=99.63 | 99.57 to 99.67 | ||||||
| − | 6885 | 57 114 | PPV=96.39 | 94.55 to 97.63 | 8171 | 55 157 | PPV=82.32 | 80.03 to 84.40 | |
| NPV=89.24 | 89.00 to 9.48 | NPV=87.10 | 86.83 to 87.36 | ||||||
| Main diagnosis | + | 309 | 11 | Sn=4.15 | 3.72 to 4.63 | ||||
| Sp=99.98 | 99.97 to 99.99 | ||||||||
| − | 7137 | 57 124 | PPV=96.56 | 93.95 to 98.07 | |||||
| NPV=88.89 | 88.65 to 89.13 | ||||||||
| Admission diagnosis | + | 773 | 90 | Sn=8.46 | 7.91 to 9.05 | ||||
| Sp=99.84 | 99.80 to 99.87 | ||||||||
| − | 8362 | 55 274 | PPV=89.57 | 87.35 to 91.44 | |||||
| NPV=86.86 | 86.59 to 87.12 | ||||||||
| Most responsible diagnosis | + | 251 | 4 | Sn=2.75 | 2.43 to 3.10 | ||||
| Sp=99.99 | 99.98 to 100.00 | ||||||||
| − | 8884 | 55 360 | PPV=98.43 | 96.04 to 99.39 | |||||
| NPV=86.17 | 85.90 to 86.44 | ||||||||
| Admission diagnosis+most responsible diagnosis | + | 248 | 4 | Sn=2.71 | 1.36 to 1.74 | ||||
| Sp=99.99 | 99.98 to 100.00 | ||||||||
| − | 8887 | 55 360 | PPV=98.41 | 95.99 to 99.38 | |||||
| NPV=86.17 | 74.99 to 75.66 | ||||||||
ICD-10, International Classification of Diseases, 10th revision; Sn, sensitivity; Sp, specificity; PPV, positive predictive value; NPV, negative predictive value; +, hyponatraemia yes; −, hyponatraemia no.
In patients with and without baseline hyponatraemia (7–365 days prior to hospital encounter), the sensitivity of the all diagnosis ICD-10 coding algorithm in the emergency department setting was 11.6% in those with baseline hyponatraemia and 5.4% in those without. For similar patients in the hospital admission setting, the sensitivities were 16.9% and 7.6%, respectively (see online supplementary appendix D).
In both settings, the sensitivity of each ICD-10 coding algorithm for hyponatraemia increased as the thresholds for serum sodium decreased (table 3). The positive predictive value of each ICD-10 coding algorithm for hyponatraemia decreased with decreasing thresholds for serum sodium, as lower thresholds are less common (ie, 25.0% of hospital admissions had a serum sodium <135 mmol/l vs 2.3% with a value ≤125 mmol/l).
Table 3.
Performance of the ICD-10 coding algorithms for hyponatraemia for different levels of serum sodium measurements
| ICD-10 E87.1 coding algorithms | Performance measures % | Serum sodium measurements (mmol/l)* |
|||||
|---|---|---|---|---|---|---|---|
| Emergency department |
Hospital admission |
||||||
| <135 | ≤130 | ≤125 | <135 | ≤130 | ≤125 | ||
| All diagnosis | Sensitivity | 4.49 | 12.58 | 34.43 | 6.42 | 17.06 | 41.68 |
| Specificity | 99.97 | 99.95 | 99.71 | 99.72 | 99.55 | 99.12 | |
| PPV | 97.42 | 94.33 | 68.21 | 88.30 | 77.20 | 52.43 | |
| NPV | 81.17 | 94.04 | 98.82 | 76.21 | 93.06 | 98.64 | |
| Main diagnosis | Sensitivity | 2.48 | 6.94 | 20.64 | |||
| Specificity | 99.99 | 99.97 | 99.87 | ||||
| PPV | 97.81 | 94.69 | 74.38 | ||||
| NPV | 80.86 | 93.68 | 98.58 | ||||
| Admission diagnosis | Sensitivity | 4.97 | 14.02 | 36.66 | |||
| Specificity | 99.87 | 99.80 | 99.49 | ||||
| PPV | 92.70 | 86.10 | 62.57 | ||||
| NPV | 75.96 | 92.84 | 98.53 | ||||
| Most responsible diagnosis | Sensitivity | 1.56 | 4.70 | 15.48 | |||
| Specificity | 99.99 | 99.99 | 99.96 | ||||
| PPV | 98.43 | 97.65 | 89.41 | ||||
| NPV | 75.33 | 92.14 | 98.06 | ||||
| Admission diagnosis+most responsible diagnosis | Sensitivity | 1.54 | 4.64 | 15.41 | |||
| Specificity | 99.99 | 99.99 | 99.96 | ||||
| PPV | 98.41 | 97.62 | 90.08 | ||||
| NPV | 75.33 | 92.14 | 98.06 | ||||
*95% CIs were calculated using the Wilson score method but were not reported. All intervals were within ±4% of the point estimate.
ICD-10, International Classification of Diseases, 10th revision; PPV, positive predictive value; NPV, negative predictive value.
When considering all potential diagnoses, 582 (0.9%) patients were code positive for hyponatraemia at presentation to the emergency department and 1171 (1.8%) at hospital admission. The median (IQR) serum sodium values among code positive patients were 123 (119–126) and 125 (120–130) mmol/l in each setting, respectively. For those patients who were code negative, the median values were 138 (136–140) and 137 (135–139) mmol/l, respectively (table 4).
Table 4.
Serum sodium concentration (mmol/l) describing those patients where the ICD-10 coding algorithms did and did not indicate hyponatraemia (code positive and code negative)
| Emergency department |
Hospital admission |
||||||
|---|---|---|---|---|---|---|---|
| ICD-10 E87.1 coding algorithms |
N | Median | IQR | N | Median | IQR | |
| All diagnosis | + | 582 | 123 | 119–126 | 1171 | 125 | 120–130 |
| − | 63999 | 138 | 136–140 | 63328 | 137 | 135–139 | |
| Main diagnosis | + | 320 | 122 | 117–126 | |||
| − | 64261 | 138 | 136–140 | ||||
| Admission diagnosis | + | 863 | 124 | 119–128 | |||
| − | 63636 | 137 | 135–139 | ||||
| Most responsible diagnosis | + | 255 | 120 | 116–123 | |||
| − | 64244 | 137 | 135–139 | ||||
| Admission diagnosis+most responsible diagnosis | + | 252 | 120 | 116–123 | |||
| − | 64247 | 137 | 135–139 | ||||
Code-positive and code-negative patients were significantly different (p values <0.0001) (means presented in box plot; figure 1).
ICD-10, International Classification of Diseases, 10th revision; N, number; +, code positive; −, code negative.
In both settings there were significant differences in mean serum sodium values between patients who were code positive and code negative for hyponatraemia for all ICD-10 coding algorithms (p values <0.0001 in each setting). The mean difference in serum sodium values between patients who were code positive and code negative in the two settings was 15.2 (95% CI 14.6 to 15.7) and 11.4 (95% CI 10.9 to 11.9) mmol/l, respectively (figure 1).
Figure 1.
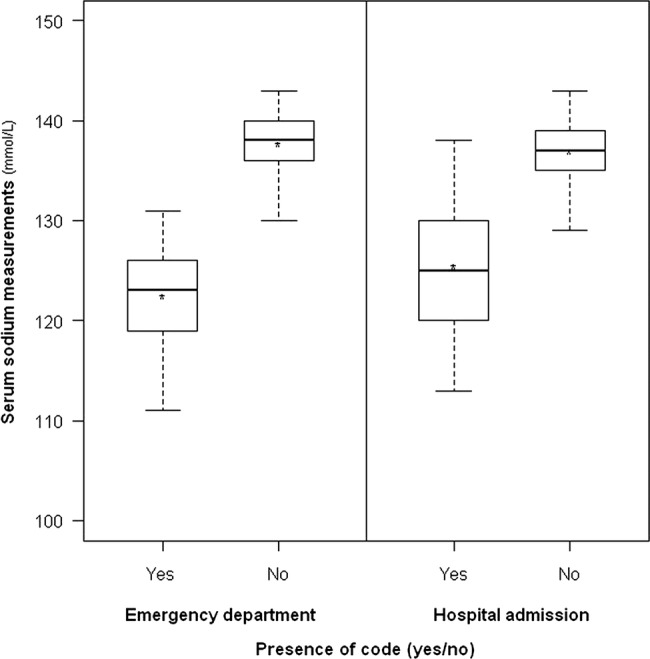
Serum sodium measurements among patients who are code positive and code negative for hyponatraemia when considering any evidence of hyponatraemia (all diagnosis). For both presentation to emergency department and at hospital admission, patients who were code positive for hyponatraemia had significantly lower serum sodium measurement than patients who were code negative. The boxes represent the IQR (50% of the values). The line across the box indicates the median. The star indicates the mean. The whiskers extend to the 95th and 5th percentile.
In the subgroup of patients with baseline prehospital encounter serum sodium measurements, the median (IQR) decrement in serum sodium values among patients who were code positive was 10.0 (6.0–15.0) mmol/l at presentation to the emergency department and 8.0 (4.0–13.0) mmol/l at hospital admission. Similar results in patients who were code negative were 1.0 (1.0–4.0) and 2.0 (0.0–4.0) mmol/l, respectively. The mean difference in the decrement in serum sodium values between patients who were code positive and code negative in the two settings was 9.4 (95% CI 8.6 to 10.2) and 6.8 (95% CI 6.2 to 7.4) mmol/l, respectively (p values <0.0001 in each setting) (see online supplementary appendix E).
Discussion
In this population-based validation study, we found that the best-performing ICD-10 coding algorithm for hyponatraemia for presentation to the emergency department and at hospital admission settings was when the code was included in any diagnosis field, regardless of the associated diagnosis type. Overall, while the ICD-10 code for hyponatraemia was highly specific, the sensitivity of the code was low. In both settings, there was a high false-negative rate—a large number of patients with a serum sodium measurement below 133 mmol/l were not coded as having hyponatraemia (≥90%). Even for severe hyponatraemia (serum sodium ≤125 mmol/l), the sensitivity was maximally about 42%. The most responsible diagnosis is one that is responsible for the longest length of stay/greatest use of resources and may also be one that was present at admission. This was the poorest performing algorithm in our study possibly because the hospital admission is attributed to the underlying condition that caused the hyponatraemia (eg, congestive heart failure) rather than the hyponatraemia per se.
The sensitivities we observed are similar to those reported by Movig et al and Shea et al for ICD-9 coding although the sensitivities and positive predictive values found in our study are slightly higher for all thresholds of hyponatraemia (depending on the specific ICD-10 coding algorithm). Also consistent with the previous validation studies, the sensitivity increased as the severity of hyponatraemia increased. This may be because more mild forms of hyponatraemia tend to be asymptomatic and do not usually require treatment, making the physician less inclined to record a diagnosis of hyponatraemia in the medical chart.23–25
Of the patients who had hyponatraemia at presentation to the emergency department and at hospital admission (defined by a value ≤132 mmol/l), only 7.5 and 10.6% were correctly coded as demonstrating this. In other words, the diagnosis was not being written by a physician in the medical chart and may suggest the condition receives less attention than it deserves. Despite this, the code was successful in differentiating between two groups of patients with distinctly different serum sodium measurements at the hospital encounter. Patients who where code negative for hyponatraemia had measurements in the normal range (135–145 mmol/l) and code-positive patients had much lower measurements (≤125 mmol/l). Patients who were code positive at hospital admission also demonstrated an average decrement of 8.7 mmol/l in serum sodium from a baseline value, the latter taken at a median of 29 days prior to hospital admission. This further exemplifies the point that new and more severe forms of hyponatraemia tend to be recorded.
Our study has several strengths. It is the first study to validate the ICD-10 code for hyponatraemia. We validated the ICD-10 code in both the emergency department and at hospital admission examining different types of diagnoses. Previous studies have not looked at these settings nor did they examine all the possible diagnosis types as we did.
The study was made possible by the province of Ontario's universal healthcare and provincial drug plan benefits with collection of all healthcare encounters of all citizens. We had a large sample size to base our validation on using laboratory data from a number of hospitals across the province. This helped improve study generalisability and differs from the ICD-9 validation study of Movig et al who used only a single hospital. Our large sample also provided good precision around the point estimates.
The validity measures that we used in this study have also been used in several other studies comparing ICD codes with clinical outcomes.8 9 26–29 Many validation studies compare diagnostic codes to information written in medical charts, whereas we compared the diagnostic code for hyponatraemia to a reference standard of laboratory values. Where appropriate, this is the most accurate way to determine the presence of hyponatraemia.
Our study does have some limitations. We evaluated the validity of the hyponatraemia code in an elderly population and the results best generalise to adults over the age of 65. This patient population is very vulnerable to developing hyponatraemia.3 30 In addition, since most pharmacoepidemiological research using the Ontario databases is conducted on the elderly where receipt of prescription medications is a universal benefit, these findings would be especially applicable. Additional studies are required to validate these codes in younger patients, where hospitalisation with hyponatraemia is expected to be less frequent.
Laboratory data were available for about 5% of Ontario elderly residents. This should be considered when generalising the results to the entire province, Canada, or other countries. Given that the results obtained from this study are similar to those found with the ICD-9 code for hyponatraemia in the USA and the Netherlands, we anticipate that the results are broadly applicable.
We did not know the degree to which patients with hyponatraemia were symptomatic from their low sodium values or the indication that prompted presentation to the emergency department or hospital admission. However, we do know the codes did identify acute decrements in serum creatine as previously described. Patients with acute changes in serum sodium are those most likely to be symptomatic from the condition.
We could not examine the validity of outpatient claims for hyponatraemia in this study as there is no code available for this in our jurisdiction. Nevertheless, emergency department and hospital records do detect more severe forms of hyponatraemia making this of particular interest to clinicians and policy decision makers.
Finally, we recognise we did not capture those patients who may have had severe hyponatraemia but did not present to the emergency department or hospital, or those who presented but failed to have serum sodium measured. However, the latter is less of a concern given serum sodium measurements are a ubiquitous and standard test for most patients who present for acute medical care.
Conclusion
Although administrative databases have inherent advantages, they have limitations in identifying certain conditions such as hyponatraemia. As observed in this study, the ICD-10 code for hyponatraemia was able to differentiate between two groups of elderly patients with distinct serum sodium measurements during presentation to the emergency department and at hospital admission. However, the sensitivity of hyponatraemia was very low, particularly at less severe forms of the condition, which will underestimate the true incidence of the condition. The results from this study will guide the judicious use of the hyponatraemia code in future research which uses healthcare administrative databases.
Acknowledgments
This study was supported by the Institute for Clinical Evaluative Sciences (ICES), which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). The opinions, results and conclusions reported in this paper are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred. We thank Barbara Jones, Jeff Lamond and the late Milton Haines for their help in providing access to Gamma-Dynacare laboratory data. We thank the team at London Health Sciences Centre, St Joseph's Health Care and the Thames Valley Hospitals for providing access to the Cerner laboratory data.
Footnotes
Contributors: SG participated in the coordination of the study, study design, provided interpretation of study results and drafted the manuscript. SZS participated in the study design, performed the analysis and provided interpretation of study results. JF contributed to the study design and interpretation of study results. MAW and AKJ contributed to the study design and provided feedback on the manuscript. AXG conceived of the study, participated in its design and interpretation and provided feedback on the manuscript. All authors read and approved the final manuscript.
Funding: SG was supported by a Canadian Institutes of Health Research Drug Safety and Effectiveness Cross-Disciplinary Training Program Award. AXG was supported by a Clinician Scientist Award from the Canadian Institutes of Health Research. This research was supported by an operating grant from the Canadian Institutes of Health Research.
Competing interests: None.
Ethics approval: Sunnybrook Health Sciences Centre.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data cannot be shared due to reasons of privacy. The research protocol can be shared with a written agreement.
References
- 1.Hennessy S. Use of health care databases in pharmacoepidemiology. Basic Clin Pharmacol Toxicol 2006;98:311–13. [DOI] [PubMed] [Google Scholar]
- 2.Suissa S, Garbe E. Primer: administrative health databases in observational studies of drug effects—advantages and disadvantages. Nat Clin Pract Rheumatol 2007;3:725–32. [DOI] [PubMed] [Google Scholar]
- 3.Palmer BF, Gates JR, Lader M. Causes and management of hyponatremia. Ann Pharmacother 2003;37:1694–702. [DOI] [PubMed] [Google Scholar]
- 4.Biswas M, Davies JS. Hyponatremia in clinical practice. Postgrad Med J 2007;83:373–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Upadhyay A, Jaber BL, Madias NE. Incidence and prevalence of hyponatremia. Am J Med 2006;119:S30–5. [DOI] [PubMed] [Google Scholar]
- 6.Liamis G, Milionis HJ, Elisaf M. Endocrine discorders: causes of hyponatremia not to neglect. Ann Med 2011;43:179–87. [DOI] [PubMed] [Google Scholar]
- 7.Renneboog B, Musch W, Vandemergel X, et al. Mild chronic hyponatremia is associated with falls, unsteadiness, and attention deficits. Am J Med 2006;119:71–8. [DOI] [PubMed] [Google Scholar]
- 8.Gankam KF, Andres C, Sattar L, et al. Mild hyponatremia and risk of fracture in the ambulatory elderly. Q J Med 2008;101:583–8. [DOI] [PubMed] [Google Scholar]
- 9.Waikar SS, Mount DB, Curhan GC. Mortality after hospitalization with mild, moderate, and severe hyponatremia. Am J Med 2009;122:857–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Movig KL, Leufkens HG, Lenderink AW, et al. Validity of hospital discharge International Classification of Diseases (ICD) codes for identifying patients with hyponatremia. J Clin Epidemiol 2003; 56:530–5. [DOI] [PubMed] [Google Scholar]
- 11.Shea AM, Curtis LH, Szczech LA, et al. Sensitivity of International Classification of Diseases codes for hyponatremia among commercially insured outpatients in the United States. BMC Nephrol 2008;9:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Health Organization. Fact Sheet May 2012: International Classification of Diseases (ICD). www.who.int/entity/classifications/icd/revision/icdfactsheet.pdf (accessed 16 May 2012).
- 13.Gandhi S, Shariff S, Beyea M, et al. Identifying geographical regions serviced by hospitals to assess laboratory based outcomes. BMJ Open (In press). [DOI] [PMC free article] [PubMed]
- 14.STAndards for the Reporting of Diagnostic accuracy studies. STARD Checklist. http://www.stard-statement.org/ (accessed 15 May 2012).
- 15.Cerner. Laboratory. http://www.cerner.com/solutions/Hospitals_and_Health_Systems/Laboratory/ (accessed 16 May 2012). [Google Scholar]
- 16.Levy AR, O'Brien BJ, Sellors C, et al. Coding accuracy of administrative drug claims in the Ontario Drug Benefit database. Can J Clin Pharmacol 2003;10:67–71. [PubMed] [Google Scholar]
- 17.Zhao YY, Weir MA, Manno M, et al. New fibrate use and acute renal outcomes in elderly adults: a population-based study. Ann Intern Med 2012;156:560–9. [DOI] [PubMed] [Google Scholar]
- 18.Jain AK, Cuerden MS, McLeod I, et al. Reporting of the estimated glomerular filtration rate was associated with increased use of angiotensin-converting enzyme inhibitors and angiotensin-II receptor blockers in CKD. Kidney Int 2012;81:1248–53. [DOI] [PubMed] [Google Scholar]
- 19.Weir MA, Gomes T, Mamdani M, et al. Impaired renal function modifies the risk of severe hypoglycaemia among users of insulin but not glyburide: a population-based nested case–control study. Nephrol Dial Transplant 2011;26:1888–94. [DOI] [PubMed] [Google Scholar]
- 20.Molnar AO, Coca SG, Devereaux PJ, et al. Statin use associates with lower incidence of acute injury after major elective surgery. J Am Soc Nephrol 2011;22:939–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Canadian Institute for Health Information. Canadian coding standards for Version 2012 ICD-10-CA and CCI https://secure.cihi.ca/free_products/canadian_coding_standards_2012_e.pdf (accessed 12 May 2012).
- 22.Newcombe RG. Two-sided confidence intervals for the single proportion: comparison of seven methods. Stat Med 1998;17:857–72. [DOI] [PubMed] [Google Scholar]
- 23.Decaux G. Is asymptomatic hyponatremia really asymptomatic? Am J Med 2006;119:S79–82. [DOI] [PubMed] [Google Scholar]
- 24.Schrier RW. Does ‘asymptomatic hyponatremia’ exist? Nat Rev Nephrol 2010;6:185. [DOI] [PubMed] [Google Scholar]
- 25.Tierney WM, Martin DK, Greenlee MC, et al. The prognosis of hyponatremia at hospital admission. J Gen Intern Med 1986;1:380–3855. [DOI] [PubMed] [Google Scholar]
- 26.Waiker SS, Wald R, Chertow GM, et al. Validity of International Classification of Diseases, Ninth Revision, Clinical Modification codes for acute renal failure. J Am Soc Nephrol 2006;17:1688–94. [DOI] [PubMed] [Google Scholar]
- 27.Romano PS, Roos LL, Luft HS, et al. A comparison of administrative versus clinical data: coronary artery bypass surgery as an example. Ischemic Heart Disease Patient Outcomes Research Team. J Clin Epidemiol 1994;47:249–60. [DOI] [PubMed] [Google Scholar]
- 28.Quan H, Parsons GA, Ghali WA. Validity of procedure codes in International Classification of Diseases, 9th revision, clinical modification administrative data. Med Care 2004;42:801–9. [DOI] [PubMed] [Google Scholar]
- 29.Raiford DS, Perez Gutthann S, Garcia Rodriguez LA. Positive predictive value of ICD-9 codes in the identification of cases of complicated peptic ulcer disease in the Saskatchewan hospital automated database. Epidemiology 1996;7:101–4. [DOI] [PubMed] [Google Scholar]
- 30.Kugler JP, Hustead T. Hyponatremia and hypernatremia in the elderly. Am Fam Phys 2000;61:3623–30. [PubMed] [Google Scholar]


