Abstract
Background:
Trivial use of antibiotics is a major reason for the spread of antibiotics resistance. The aim behind undertaking this investigation was to study the prevalence antibiotics self-medication among university students in Benghazi city.
Methods:
A questionnaire-based cross-sectional, survey was conducted at both Libyan International Medical University and Benghazi University. A total of 665 copies of questionnaires was distributed. A total of 363 forms were completed and returned (response rate 55%). Remaining responses were either with no antibiotics use history within the past 1 year or were provided incomplete.
Results:
Among the respondents, 45% were males and 55% females. Males practiced self-medication more compared to females. Approximately, 43% and 46% from medical and nonmedical students, respectively, were antibiotics self-medicated. A total of 153 students (42%) out of total respondents administered antibiotics for symptoms related to respiratory problems, among which 74 students (48%) took antibiotics based on doctor's prescription. Among the respondents, 94 students (27%) who had antibiotics, were covered under medical insurance, and 19 (29%) of the medically insured students had antibiotics without doctor's prescription. About 14% of students did not complete their antibiotics course. Of these, 57% were medical students, and 43% were nonmedical students. The rate of self-medication among higher classes was more as compared to lower classes. About 58% of students overdosed the antibiotic, while 15% had antibiotics for <3 days, for treatment of ailments such as acne, toothache, diarrhea, earache, and tonsillitis. About 75% of students purchased the antibiotics in consultation with a pharmacist.
Conclusion:
Self-medication is a frequent problem among university students in Benghazi city. There is a need for an immediate intervention to address this malpractice among both students and medical practitioners.
KEY WORDS: Antibiotics, Benghazi, Libya, medical and nonmedical students, self-medication
Inconsequential use of antibiotic is a key factor responsible for the emergence of antimicrobial resistance.[1] The term antibiotics misuse is also sometimes termed as antibiotics abuse or overuse.[2,3] The misuse of antibiotics has been linked to both patients and or physicians who irresponsibly prescribe these medications. The inappropriate overuse/misuse of antimicrobial drugs has resulted in the worst scenario of bacterial mutations and developing resistant strains.[4] Globally, many Staphylococcus aureus strains exhibited resistance to many important antibacterial drugs like vacomycin,[5] on the other hand, S. aureus resistant to methicillin has become one of the most frequent hospital-acquired pathogen.[6,7] The rate at which bacteria develop resistance to antibiotics is alarmingly high, demonstrating resistance to antibiotics that always showed high specificity and popularity such as tetracycline, amoxicillin, clarithromycin, and metronidazole.[8]
In some developed countries such as central and Eastern Europe, laws that restrict dispensing of antibiotics as over the counter drug has been legislated and strictly followed. On the contrary, western and southern parts of the continent still report high rates of self-medication by antibiotics.[9] Several factors have been attributed to the misuse of antibiotics such as doctor's knowledge on reason to use antibiotics, diagnostic uncertainty, patients’ expectations, lack of patient and health care professional's education, antibiotics being sold without a prescription, and economic and political reasons.[10]
Many previous studies were also devoted for prevalence, nature and reasons for self-medication among university undergraduates (nonmedical) and schools in different countries worldwide.[11,12,13,14,15]
This work was undertaken to determine the frequency and nature of antibiotics self-medication practice among university medical and nonmedical students in Benghazi, Libya. This study also aims to look into reasons for any relationship between the type of education, that is, either medical or nonmedical and the self-medication practice. This study of antibiotics self-medication practice among university medical undergraduates in Libya is significant since they belong to the educated class and has access to information regarding health. It is also very vital to analyze this trend since they represent the future generation of drug prescribers and health educationists. An understanding of the level of antibiotics self-medication practice and their reasons will enable us to take various corrective measures. It will also help policy makers to take steps for a more rational use of antibiotics in the community in general.
Materials and Methods
The study plan
The survey was conducted among 665 medical and nonmedical students from Libyan International Medical University and Benghazi University through a self-administered questionnaire, from September to December 2013. The respondents completed a self-administered questionnaire. Assistance was provided by the interviewer whenever requested. Sample copy of the distributed questionnaire is placed in this section.
Ethical clearance
Ethical approval was obtained prior to the commencement of the study from the Ethical Committee of Libyan International Medical University, Benghazi, Libya.
Signature-based written consent was obtained from each student after explaining the purpose of the study.
Section A: Demographic data
Age: .............
-
Education
-
Type:Medical Nonmedical
-
Level:1st year 2nd year 3rd year 4th year 5th year
-
-
Gender:
- Male Female
-
Family monthly income (Libyan Dinar):
- 500–800 800–1500 1500–3000 >3000
-
Medical insurance:
- Yes No
Section B
-
Did you take any antibiotics in last 1 year?
Yes NO
If yes/why did you take the antibiotics?
Diarrhea, Runny nose, Flu, Toothache,
Sore throat, Chest tightness, Acne, Tonsil,
Ear infection, Coughs, Urinary tract infection)
-
Did a physician prescribe this medication for you?
Yes No
If “no” answer:
-
Why did you take antibiotics without a prescription?
- Poor economic status
- No access to physician care
- Previous experience
- Other (Please indicate)
- If Question 2 was No
-
What was the source of antibiotics supply?
- Pharmacist
- Relative or friend
- Leaflet
- Others (please indicate)
-
The duration of antibiotics intake was:
- 1–3 days
- 4–7 days
- >7 days.
Statistical data analysis
All data obtained by filled questionnaire were coded, entered, and analyzed using Statistical Package for Minitab program version 13 for Windows, developed by Minitab Inc. The analysis of answers for other questions involved descriptive quantitative statistics, for example, frequency and percentage. The differences in the participants’ responses were analyzed with Chi-square test. The 0.05 level of significance was used as a cutoff for statistical significance.
Results
The study population
The study population was of Libyan International Medical University and University of Benghazi, whose students amounted to nearly 31,855 in 2013. Of these, 7748 were medical, and 24,107 were nonmedical. The target study sample was divided into two groups: “A” and “B”. Group “A” represented students from medical and health science disciplines (medicine, dentistry, and pharmacy), which was designated as “medical” group; whereas, Group “B” represented the “nonmedical” group, which included students from specialties other than the ones from medical and health science disciplines.
The study tool: The questionnaire
The questionnaire used in this study was constructed by reviewing relevant previous literature on similar studies.
The questionnaire comprised of a total of nine questions divided into two sections:
The first section covered participant's demographic data such as sex and age.
The second section involved the source of antibiotics used by the participants over the past year. Students’ knowledge on the purpose of using antibiotics, such as runny nose, common cold, pain, fever, and toothache were included in this section. Questions on the duration over which the antibiotic was taken, source of the antibiotic supply, etc., were also incorporated.
Characteristics of the study population
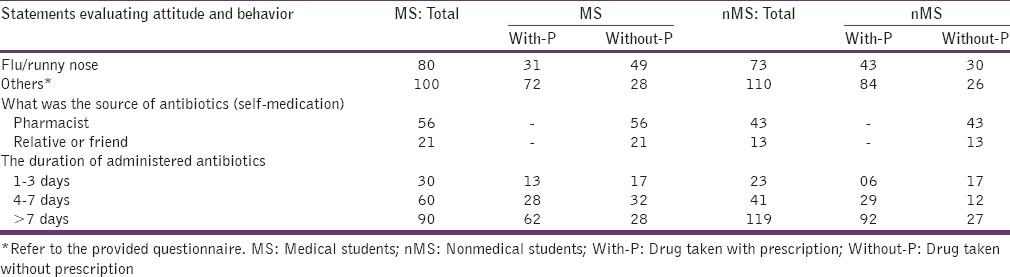
Table 1 summarizes the personal data and field of education, while Table 2 summarizes the extent of the antibiotics self-medication among medical and nonmedical students with varying educational levels as well as whether the students are medically insured. Table 3 exhibits the reason, source, and duration of the administered antibiotics.
Table 1.
Gender and educational discipline of students

Table 2.
The distribution of the students (medical or nonmedical) according to the level of education, mood of antibiotics medication, and access to medical insurance
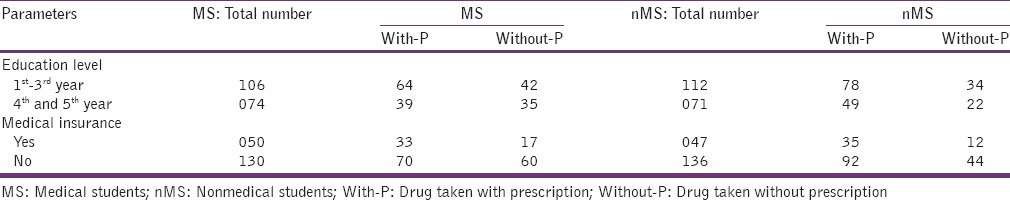
Table 3.
Reason, source, and duration of the administered antibiotics
Of 665 distributed questionnaires, 363 were returned filled as desired (response rate ~55%). The majority of respondents (55%) were females. A total of 180 students (49.6%) among the respondents were students from medical faculties, whereas 183 (50.4%) students were from nonmedical disciplines [Table 1].
Comparing the rate of self-medication among medical and nonmedical students, medical students were more self-medicated (43%) as compared to their peer group from the nonmedical fields (31%). This difference was statistically significant (P = 0.016) [Figure 1].
Figure 1.
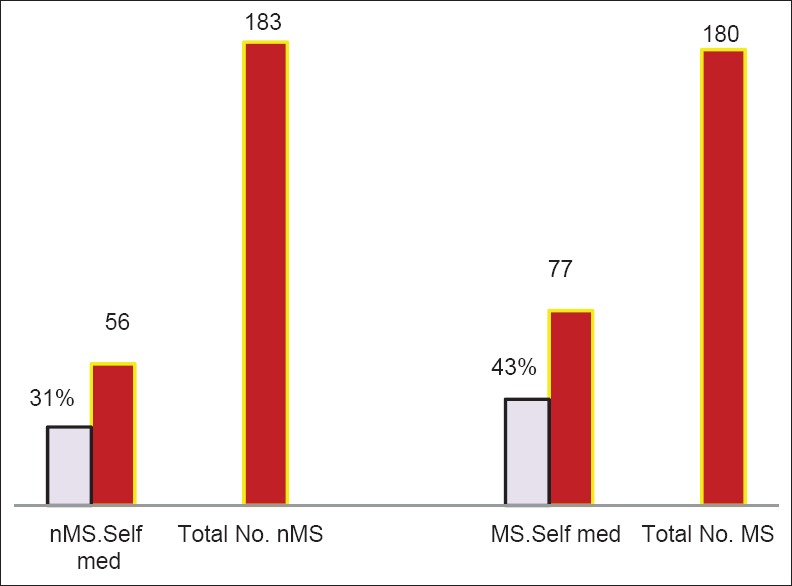
Antibiotics self-medication among medical and nonmedical students
A total of 42 students (40%) from the medical field, who were enrolled between 1st and 3rd classes, took antibiotics without prescription during the past year, while 35 students (47%) of medical respondents who were enrolled in class 4th and 5th year took antibiotics without medical prescription. On the other hand, 34 and 22 students (30% and 31%) were from the nonmedical faculties who took antibiotics without prescription for classes from 1st to 3rd and 4th and 5th year, respectively [Table 2]. Though the difference in rate of the self-medication is evident, this relation showed no statistical significance (P > 0.05).
Effect of class level of students’ behavior toward antibiotics
Higher classes (4th and 5th) of medical students exhibited higher rate of antibiotics self-medication (47%) as compared to lower classes 1st, 2nd, and 3rd (40%) (P > 0.05). On the contrary, there were no clear differences in self-medication among classes of nonmedical students (P > 0.05) [Table 2, Figure 2a and b].
Figure 2.
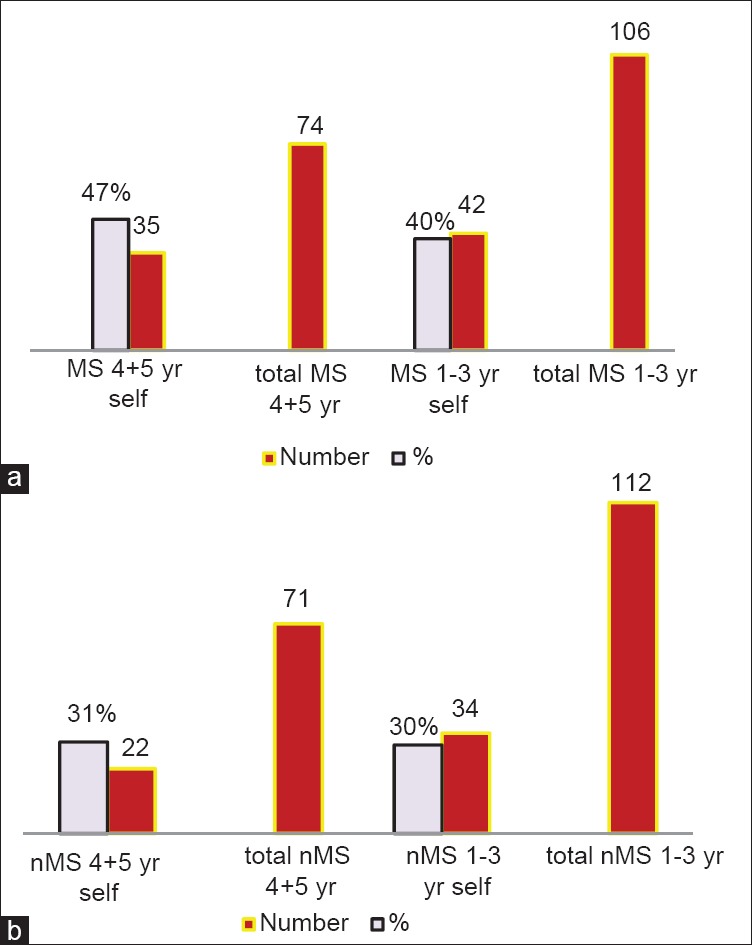
(a) Self-medication among varying classes of medical students. Total MS 1–3 yr: Total medical students of 1st to 3rd classes; MS 1–3 yr self: Self-medicated medical students of 1st to 3rd classes; Total MS 4 + 5 yr: Total medical students of 4th and 5th classes; MS 4 + 5 yr self: Self-medicated medical students of 4th and 5th classes (b) Self-medication among varying classes of nonmedical students. Total nMS 1–3 yr: Total nonmedical students of 1st to 3rd classes; nMS 1–3 yr self: Self-medicated nonmedical students of 1st to 3rd classes; Total nMS 4 + 5 yr: Total nonmedical students of 4th and 5th classes; nMS 4 + 5 yr self: Self-medicated nonmedical students of 4th and 5th classes
Effect of availability of medical insurance on students’ self-medication
Considering total students number (regardless their fields of education), 97 students were medically insured. Of this number, 50 students from medical fields (28%) were covered with medical insurance. A total of 17 students (34%) from these medically insured students took antibiotics without prescription. On the other hand, 47 students from nonmedical fields were medically insured; of this number, 12 students (26%) were antibiotics self-medicated [Table 2 and Figure 3]. The relationship between availability of medical insurance and behavior toward antibiotics were statistically nonsignificant (P > 0.05).
Figure 3.
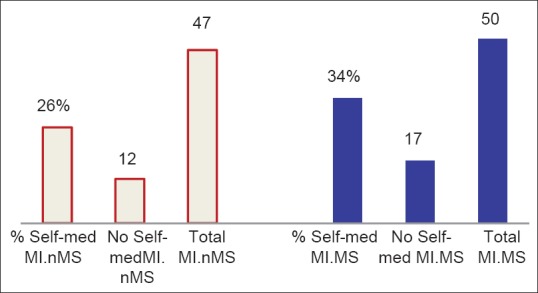
Effect of medical insurance on students’ behavior toward administration of antibiotics. No. self-med MI.MS: Number of self-medicated medically insured medical students; No. self-med MI.nMS: Number of self-medicated medically insured nonmedical students; % Self-med MI.MS: % of self-medicated medically insured medical students; % Self-med MI.nMS: % of self-medicated medically insured nonmedical students
Antibiotics source
Of total 363 students filled questionnaire in this investigation, antibiotics were used irrationally by 133 students (37%) [Figure 4].
Figure 4.
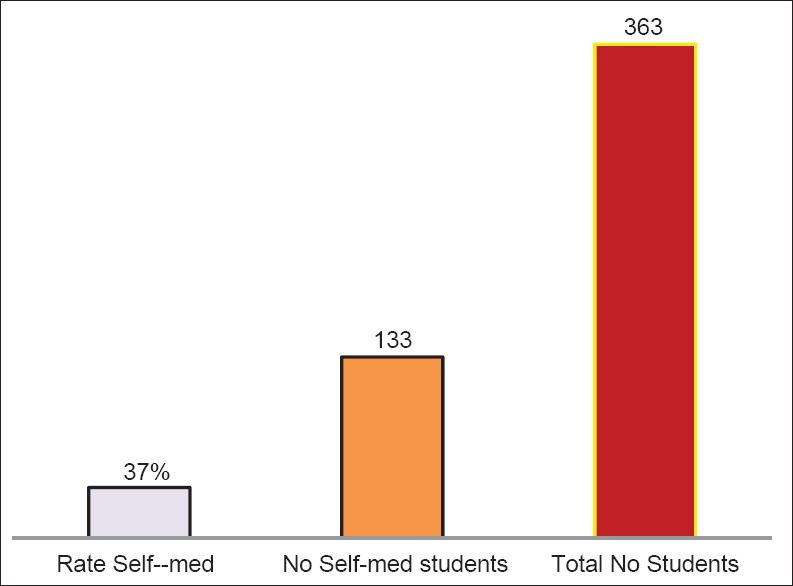
Rate of self-medication. No. self-med: Number of self-medicated; Rate self-med: Rate of self-medication
Of 180 medical students who had antibiotics, 80 students (44%) used it for treatment of flu or runny nose illnesses. Totally, 31 students (39%) of this group administered antibiotics which prescribed by physician [Figure 5a]. On contrary, 74 students (40%) from the nonmedical fields had antibiotics for flu or runny nose disease based on doctor's prescription (P > 0.05) [Figure 5b].
Figure 5.
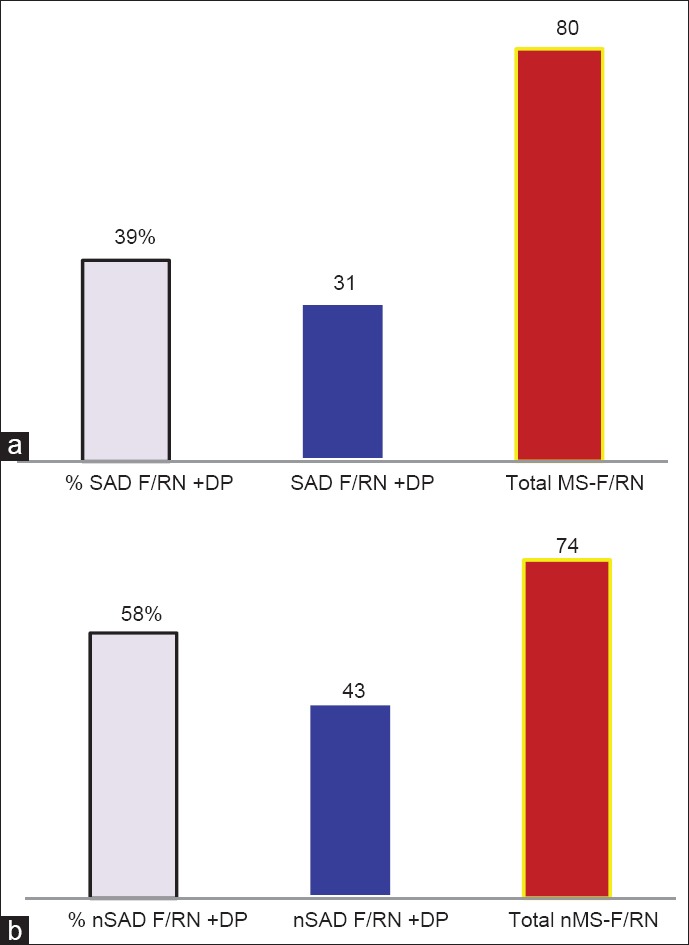
(a) Medical students who administered antibiotics for treatment of flu/runny nose. Total MS-F/RN: Total number of medical students who had antibiotics for treatment of flu/runny nose; SAD F/RN+DP: Medical students who had antibiotics for treatment of flu/runny nose illnesses with doctor's prescription; % SAD+DP: % of Medical students who had antibiotics for treatment of flu/runny nose illnesses with doctor's prescription. (b) Nonmedical students who administered antibiotics for treatment of flu/runny nose. Total nMS-F/RN: Total number of nonmedical students who had antibiotics for treatment of flu/runny nose; nSAD F/RN+DP: Nonmedical students who had antibiotics for treatment of flu/runny nose illnesses with doctor's prescription; % nSAD + DP: % of nonmedical students who had antibiotics for treatment of flu/runny nose illnesses with doctor's prescription
Duration of administered antibiotics
Most of the students (209, 58%) took antibiotics for >7 days for treatments of ailments such as acne, toothache, diarrhea, earache, and tonsillitis, whereas 53 students (15%) had antibiotics for <3 days. A total of 101 students (28%) completed the course of the antibiotics. The relationship between field of study and duration of antibiotics administration was significant (P = 0.014) [Figure 6].
Figure 6.
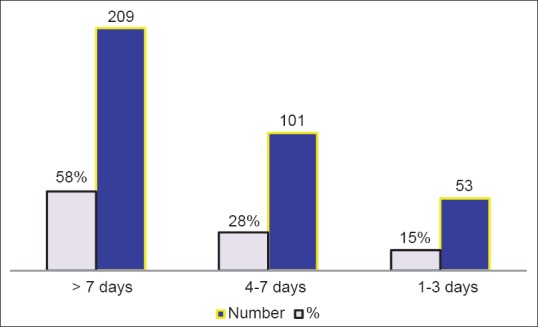
Duration of administered antibiotics
Source of the antibiotics of self-medication
A total of 99 students (74%) of those who were self-medicated got their antibiotics purchased based on pharmacist consultancy, whereas 34 students (26%) taken the antibiotics from a relative or friend [Figure 7].
Figure 7.
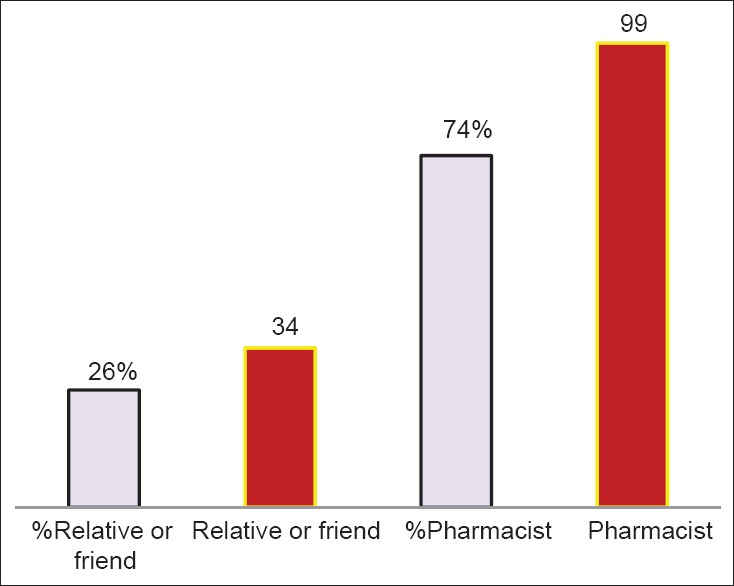
Source of antibiotics used for self-medication. Pharmacist: Antibiotics was obtained by a pharmacist consultancy; Relative or friend: Antibiotics was obtained from friend or relative
Genders and self-medication
Males were largely self-medicated (91, 55%) as compared to female colleagues (67, 37%) [Figure 8].
Figure 8.
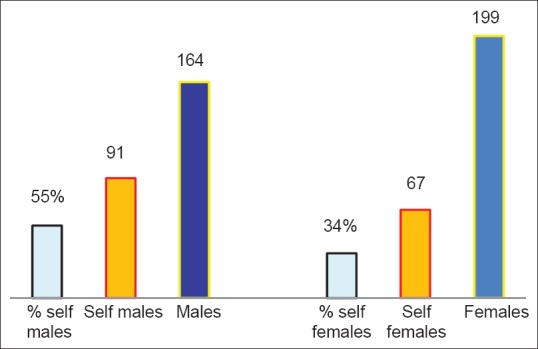
Self-medication among male and female students. Self-females: Number of self-medicated females; % self-females: % of self-medicated females; Self males: Number of self-medicated males; % self-males: % of self-medicated males
Discussion
Good prescribing practice has an essential role to play in order to fight antimicrobial resistance. On the other hand, irrational use of antibiotics is a key reason for the increase and spread of antibiotics resistance. Several factors may enhance irrational antibiotics usage, which could be doctors’ knowledge, diagnostic uncertainty, patients’ expectations, lack of patient and health care professionals’ education, pharmaceutical marketing, antibiotics selling without a prescription as well as economic and political reasons.[10]
In Libya, like many other developing countries, there are no clear regulations or policies concerning the distribution and selling of antibiotics as over the counter drugs with no medical prescription. Self-medication with antibiotics is defined as the acquisition of antibiotics and self-administering them with the aim of treating the infection. This practice is a worldwide problem, with emphasis to developing countries such as Sudan,[16] Trinidad and Tobago,[17] India,[18] and Emirates,[19] however, the same practice is also prevalent in the developed countries such as Israel,[20] Spain,[21] and many European countries.[9] The presence of antibiotics through doctor's prescription does not rule out the possibility that they can be used for self-medication. The incomplete course of antibiotics could be supplied by friends or acquaintances who experienced similar symptoms.
Comparing the present investigation on the rate of the self-medication with the equivalent ones reported in other countries; the percentage of self-medication in Libya is alarmingly high.
In Jordan, self-medication with antibiotics among population is 23%.[22] A percentage as high as 53% was reported among Iranian college students.[23]
Using antibiotics for a short period, usually till the symptoms subside would expose infective bacteria to sub-therapeutic levels of antibiotics. From the current study, majority of students who did not complete the course of antibiotics were from nonmedical fields, on the other hand, students from medical fields seems to be more alert on the use of antibiotics than those from nonmedical disciplines. Most of the students completed the course of antibiotics. However, a few used antibiotics for <3 days.
In this investigation, most of the students who indulged in antibiotics self-medication were males. These, results are contradictory to Kumar et al. results, in which they have shown more than 80% of self-medication was contributed by females.[24]
Totally, 104 students (29%) of the total number of students (who took antibiotics without prescription), regardless of their educational field, were not covered by any medical insurance. The socioeconomic and educational variability are one of the main culprits for the self-medication practice in many countries around the world. To correlate between the reason behind administering antibiotics without prescription and the students’ socioeconomic background, the question on student's/families monthly income was incorporated in the questionnaire. Unfortunately, majority of the students were reluctant to furnish such information. Though 97 students, which represents 27% of total respondents were medically insured, 29 students (30% of total insured students) were self-medicated. This fact may, therefore, abolish or argue against the probability of any economical factor that may justify for this self-medication practice. Interestingly, 43% of medical students were self-medicated; whereas only 30% of nonmedical students were self-medicated. By conducting such studies among both medical and nonmedical fields, it was feasible to establish the possible impact of discipline of education on student's attitude toward administration of antibiotics in particular and other drugs in general. The prominent propensity of medical students for self-medication than their peer groups from nonmedical fields may be ascribed to the fact that medical students are more exposed to the scientific background of antibiotics. In addition, it could also be attributed to the possible feeling of medical students that they may no longer need medical consultancy. The later may be enforced by the easy access to antibiotics as over the counter drug. Our results concerning administration of antibiotics among medical students as compared to nonmedical ones are in accordance with the results obtained by Fadare and Tamuno,[25] however, in contrary with James et al. results.[26] Medical students who enrolled in higher classes practice antibiotics self-medication more than their colleagues in lower classes [Figure 2a]. Our finding is in accordance with the results reported by Osemene and Lamikanra, where a proportional relation between self-medication and students’ class level in the university was reported.[27] The tendency to indulge in self-medication behavior would be assumed to decrease with an increase in age and respondents’ class level in the university in correlation with corresponding increases in age and educational knowledge and status.
It was tempting to know which antibiotics was used majorly by students, however, to our surprise, most of the questioned students, including those from medical fields, were unable to recollect the name of antibiotics administered.
Strikingly, most of the students (154 students, 42%) had antibiotics for treatment of illness like flu or runny nose [Table 3]. These diseases are often viral rather than bacterial infections and require no antibiotics treatment. Added more to our surprise the finding that majority of students who had antibiotics for treatment of flu or runny nose took it according to doctors’ prescription [Figures 5a and b]. Moreover, while analyzing the filled questionnaires several students had antibiotics for prolonged durations ranging from 21 days to as long as several months for treatment of diseases such as a common cold, toothache, and tonsillitis. The doctors who prescribed antibiotics to treat common cold, could not only put students at unnecessary risk for contracting infections with resistant pathogens, but also at the same time might misguide them with a wrong understanding that common cold are treated by antibiotics.
Conclusion and Recommendation
This study has shown that self-medication with antibiotics is common among both medical and nonmedical undergraduates in Benghazi city, North-east of Libya. This study revealed a considerable rate of antibiotics self-medication among medical and nonmedical students community, which should drive the attention of the authorities to this problem, especially when medical students are the ones who pursue this practice. A need for the re-evaluation of the educational curricula is felt, especially, teaching of clinical pharmacology. This must include awareness programs on ill effects of self-medication. At the policy-making level, there is an urgent demand to legislate and enforce laws restricting access to antibiotics in Libya. Most importantly, there is a need to incorporate curriculum on abuse of antibiotics and the harm of such practice on short and long run.
Acknowledgments
The authors are thankful for all volunteer students who participated in this study. We are also grateful for authorities at the University of Benghazi for allowing easy access to their students.
We also like to thank Mr. Biju Nair and Dr. Iswarduth Soojhawon for critically revising the manuscript.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Tamma PD, Cosgrove SE. Antimicrobial stewardship. Infect Dis Clin North Am. 2011;25:245–60. doi: 10.1016/j.idc.2010.11.011. [DOI] [PubMed] [Google Scholar]
- 2.Siddig W, Salim M, Mohamed A, Ibrahim I, Farid M, Konozy E. Regardless of the antibiotic group or type, misuse of antibiotics adversely impair liver, kidneys and heart functions “biochemical and histopathological assessment”. Am J Pharm Health Res. 2014;2:73–94. [Google Scholar]
- 3.Woappi Y, Gabani P, Singh A, Singh OV. Antibiotrophs: The complexity of antibiotic-subsisting and antibiotic-resistant microorganisms. Crit Rev Microbiol. 2014 doi: 10.3109/1040841X.2013.875982. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 4.Mathur S, Singh R. Antibiotic resistance in food lactic acid bacteria - A review. Int J Food Microbiol. 2005;105:281–95. doi: 10.1016/j.ijfoodmicro.2005.03.008. [DOI] [PubMed] [Google Scholar]
- 5.Gould IM. Treatment of bacteraemia: Meticillin-resistant Staphylococcus aureus (MRSA) to vancomycin-resistant S. aureus (VRSA) Int J Antimicrob Agents. 2013;42(Suppl):S17–21. doi: 10.1016/j.ijantimicag.2013.04.006. [DOI] [PubMed] [Google Scholar]
- 6.McKinnell JA, Miller LG, Eells SJ, Cui E, Huang SS. A systematic literature review and meta-analysis of factors associated with methicillin-resistant Staphylococcus aureus colonization at time of hospital or intensive care unit admission. Infect Control Hosp Epidemiol. 2013;34:1077–86. doi: 10.1086/673157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Daniel A. Anti-infective drug development for MRSA. Methods Mol Biol. 2014;1085:311–31. doi: 10.1007/978-1-62703-664-1_17. [DOI] [PubMed] [Google Scholar]
- 8.Peretz A, Paritsky M, Nasser O, Brodsky D, Glyatman T, Segal S, et al. Resistance of Helicobacter pylori to tetracycline, amoxicillin, clarithromycin and metronidazole in Israeli children and adults. J Antibiot (Tokyo) 2014;67:555–7. doi: 10.1038/ja.2014.38. [DOI] [PubMed] [Google Scholar]
- 9.Grigoryan L, Monnet DL, Haaijer-Ruskamp FM, Bonten MJ, Lundborg S, Verheij TJ. Self-medication with antibiotics in Europe: A case for action. Curr Drug Saf. 2010;5:329–32. doi: 10.2174/157488610792246046. [DOI] [PubMed] [Google Scholar]
- 10.Suaifan GA, Shehadeh M, Darwish DA, Al-Ije H, Yousef AM, Darwish RM. A cross-sectional study on knowledge, attitude and behavior related to antibiotic use and resistance among medical and nonmedical university students in Jordan. Afr J Pharm Pharmacol. 2012;6:763–70. [Google Scholar]
- 11.Almalak H, Albluwi AI, Alkhelb DA, Alsaleh HM, Khan TM, Hassali MA, et al. Students’ attitude toward use of over the counter medicines during exams in Saudi Arabia. Saudi Pharm J. 2014;22:107–12. doi: 10.1016/j.jsps.2013.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Napolitano F, Izzo MT, Di Giuseppe G, Angelillo IF. Public knowledge, attitudes, and experience regarding the use of antibiotics in Italy. PLoS One. 2013;8:e84177. doi: 10.1371/journal.pone.0084177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Donkor ES, Tetteh-Quarcoo PB, Nartey P, Agyeman IO. Self-medication practices with antibiotics among tertiary level students in Accra, Ghana: A cross-sectional study. Int J Environ Res Public Health. 2012;9:3519–29. doi: 10.3390/ijerph9103519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Klemenc-Ketis Z, Hladnik Z, Kersnik J. A cross sectional study of sex differences in self-medication practices among university students in Slovenia. Coll Antropol. 2011;35:329–34. [PubMed] [Google Scholar]
- 15.Zafar SN, Syed R, Waqar S, Zubairi AJ, Vaqar T, Shaikh M, et al. Self-medication amongst university students of Karachi: Prevalence, knowledge and attitudes. J Pak Med Assoc. 2008;58:214–7. [PubMed] [Google Scholar]
- 16.Awad A, Eltayeb I, Matowe L, Thalib L. Self-medication with antibiotics and antimalarials in the community of Khartoum State, Sudan. J Pharm Pharm Sci. 2005;8:326–31. [PubMed] [Google Scholar]
- 17.Parimi N, Pinto Pereira LM, Prabhakar P. Caregivers’ practices, knowledge and beliefs of antibiotics in paediatric upper respiratory tract infections in Trinidad and Tobago: A cross-sectional study. BMC Fam Pract. 2004;5:28. doi: 10.1186/1471-2296-5-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Badiger S, Kundapur R, Jain A, Kumar A, Pattanshetty S, Thakolkaran N, et al. Self-medication patterns among medical students in South India. Australas Med J. 2012;5:217–20. doi: 10.4066/AMJ.2012.1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abasaeed A, Vlcek J, Abuelkhair M, Kubena A. Self-medication with antibiotics by the community of Abu Dhabi Emirate, United Arab Emirates. J Infect Dev Ctries. 2009;3:491–7. doi: 10.3855/jidc.466. [DOI] [PubMed] [Google Scholar]
- 20.Raz R, Edelstein H, Grigoryan L, Haaijer-Ruskamp FM. Self-medication with antibiotics by a population in northern Israel. Isr Med Assoc J. 2005;7:722–5. [PubMed] [Google Scholar]
- 21.Granizo JJ. Antimicrobial drug use in Spain. A problem with no solution. Rev Esp Quimioter. 2001;14:317–8. [PubMed] [Google Scholar]
- 22.Al-Azzam SI, Al-Husein BA, Alzoubi F, Masadeh MM, Al-Horani MA. Self-medication with antibiotics in Jordanian population. Int J Occup Med Environ Health. 2007;20:373–80. doi: 10.2478/v10001-007-0038-9. [DOI] [PubMed] [Google Scholar]
- 23.Sarahroodi S, Arzi A. Self-medication with antibiotics, Is it a problem among Iranian college students in Tehran? J Biol Sci. 2009;9:829–32. [Google Scholar]
- 24.Kumar N, Kanchan T, Unnikrishnan B, Rekha T, Mithra P, Kulkarni V, et al. Perceptions and practices of self-medication among medical students in coastal South India. PLoS One. 2013;8:e72247. doi: 10.1371/journal.pone.0072247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fadare JO, Tamuno I. Antibiotic self-medication among university medical undergraduates in Northern Nigeria. J Public Health Epidemiol. 2011;3:217–20. [Google Scholar]
- 26.James H, Handu SS, Khaja KA, Sequeira RP. Influence of medical training on self-medication by students. Int J Clin Pharmacol Ther. 2008;46:23–9. doi: 10.5414/cpp46023. [DOI] [PubMed] [Google Scholar]
- 27.Osemene KP, Lamikanra A. A study of the prevalence of self-medication practice among university students in Southwestern Nigeria. Trop J Pharm Res. 2012;11:683–9. [Google Scholar]


