Abstract
Objectives
Evaluate the validity of the International Classification of Diseases, 10th revision (ICD-10) code for hyperkalaemia (E87.5) in two settings: at presentation to an emergency department and at hospital admission.
Design
Population-based validation study.
Setting
12 hospitals in Southwestern Ontario, Canada, from 2003 to 2010.
Participants
Elderly patients with serum potassium values at presentation to an emergency department (n=64 579) and at hospital admission (n=64 497).
Primary outcome
Sensitivity, specificity, positive-predictive value and negative-predictive value. Serum potassium values in patients with and without a hyperkalaemia code (code positive and code negative, respectively).
Results
The sensitivity of the best-performing ICD-10 coding algorithm for hyperkalaemia (defined by serum potassium >5.5 mmol/l) was 14.1% (95% CI 12.5% to 15.9%) at presentation to an emergency department and 14.6% (95% CI 13.3% to 16.1%) at hospital admission. Both specificities were greater than 99%. In the two settings, the positive-predictive values were 83.2% (95% CI 78.4% to 87.1%) and 62.0% (95% CI 57.9% to 66.0%), while the negative-predictive values were 97.8% (95% CI 97.6% to 97.9%) and 96.9% (95% CI 96.8% to 97.1%). In patients who were code positive for hyperkalaemia, median (IQR) serum potassium values were 6.1 (5.7 to 6.8) mmol/l at presentation to an emergency department and 6.0 (5.1 to 6.7) mmol/l at hospital admission. For code-negative patients median (IQR) serum potassium values were 4.0 (3.7 to 4.4) mmol/l and 4.1 (3.8 to 4.5) mmol/l in each of the two settings, respectively.
Conclusions
Patients with hospital encounters who were ICD-10 E87.5 hyperkalaemia code positive and negative had distinct higher and lower serum potassium values, respectively. However, due to very low sensitivity, the incidence of hyperkalaemia is underestimated.
Keywords: EPIDEMIOLOGY
Article summary.
Article focus
This study described the validity of the International Classification of Diseases, 10th revision (ICD-10) code for hyperkalaemia (E87.5) compared with serum potassium laboratory values, where the latter served as the reference standard.
Knowledge of the accuracy of the code at hospital encounters guides its judicious use in health services research.
Key messages
The ICD-10 hyperkalaemia code has very high specificity, but very low sensitivity, which underestimates the true incidence of hyperkalaemia at presentation to an emergency department and at hospital admission.
Being positive or negative for the code does distinguish between two groups of patients with distinct serum potassium measurements.
Strengths and limitations of this study
This is the first study to provide diagnostic information on the validity of the ICD-10 code for hyperkalaemia.
It was a large population-based study and included serum potassium values from 12 hospitals across Ontario.
Code validity in younger populations should be examined in future studies.
Introduction
Use of information in healthcare administrative databases is a relatively easy and efficient way to identify patients with prior or current disease. It is also a simple way for the medical community to assess resources and usage of healthcare services. However, administrative codes are not always accurate.1 This can lead to the under-reporting or over reporting of some diseases (ie, individuals who have the disease but where there is no evidence of the respective database code; or individuals who have evidence of the database code but where there is no evidence of the disease). Knowledge of the validity of various database codes guides their optimal use for research, quality assurance and health system planning.
Hyperkalaemia, or high serum potassium, is a fairly common adverse event. Normal levels of serum potassium range from 3.3 to 5.1 mmol/l, with hyperkalaemia often defined by a value of 5.5 mmol/l or higher.2 High serum potassium levels can have serious deleterious effects including arrhythmia and death.3 Some comorbidities that predispose to hyperkalaemia include chronic kidney disease and cancer. Hyperkalaemia can also occur due to the use of a variety of prescription medications, including ACE inhibitors, angiotensin receptor blockers (ARB),β-blockers and certain types of diuretics.4 Approximately 10% of patients prescribed an ACE inhibitor develop hyperkalaemia in the year following their initial prescription.5
The 10th revision of the International Classification of Diseases (ICD-10) system has been used to code healthcare encounters in Canada since 2002, and has also been implemented in over 100 other countries since its inception.6 Yet, after careful bibliographic database searching, we could find no published validation for the ICD-10 hyperkalaemia code using serum potassium laboratory values as the reference standard. There was a single validation study that considered the ICD-9 hyperkalaemia code from the Kaiser Permanente Health Management Organization in the USA, but this study only focused on how accurately it was used in automated healthcare data.7
We conducted the current study to determine the accuracy of the ICD-10 code for hyperkalaemia (E87.5) in two acute care settings: at presentation to an emergency department and at hospital admission. We compared the ICD-10 code with actual serum potassium laboratory values.
Methods
Study design
We conducted a retrospective population-based validation study using linked administrative databases housed at the Institute for Clinical Evaluative Sciences. The province of Ontario, Canada has approximately 13 million residents, 14% of whom are 65 years of age or older.8 Residents have universal access to hospital care and physician services and those 65 years of age or older have universal prescription drug coverage. Within Southwestern Ontario, we considered a catchment area that included approximately 80 000 adults 65 years of age and older, according to census information from 2006.9 There were 12 hospitals that served this area from which we gathered laboratory information. We compared the ICD-10 hyperkalaemia code E87.5 with serum potassium laboratory values as the reference standard in two settings: (1) at presentation to an emergency department and (2) at hospital admission. We calculated the sensitivity, specificity, positive-predictive value and negative-predictive value of several ICD-10 coding algorithms. Also, because serum potassium is a continuous measure, we compared patients who were positive for the code with those with hospital encounters who were negative for the code. The reporting of this study follows guidelines set out for studies of diagnostic accuracy (see online supplementary appendix A).10 We conducted our study according to a prespecified protocol that was approved by the institutional review board at Sunnybrook Health Sciences Centre (Toronto, Ontario).
Data sources
We ascertained outcome data as well as the presence of relevant comorbidities for exclusions and baseline characteristics using records from seven linked databases. The Ontario Drug Benefit Plan database contains records of prescriptions from outpatient pharmacies. The dispensing of medications for patients aged 65 and older is accurately recorded in this database with an error rate of less than 1%.11 The Canadian Institute for Health Information (CIHI) National Ambulatory Care Reporting System (NACRS) contains ambulatory care information on emergency room visits, outpatient procedures and day surgeries. The CIHI Discharge Abstract Database (CIHI-DAD) reports inpatient procedures, diagnoses and discharge summaries for patients hospitalised in Ontario. The Ontario Health Insurance Plan (OHIP) database contains all physician and other specific healthcare provider claims for medical services covered under the provincial health insurance plan. Lastly, the Registered Persons Database contains demographic information, such as birth date and sex, for all Ontario residents who have ever been covered by OHIP.
In addition to the five administrative databases described above, we used two laboratory datasets to determine serum potassium values. An electronic medical record Cerner (Kansas City, Missouri, USA) contains inpatient, outpatient and emergency department laboratory values for 12 hospitals in Southwestern Ontario.12 Gamma-Dynacare performs outpatient laboratory tests in Southwestern Ontario and was used to obtain baseline laboratory values for a subpopulation. We have successfully used these datasets in previous studies.13–16
Participants
Individuals included in our study had at least one hospital-based serum potassium laboratory value between 1 June 2003 and 30 September 2010. We considered patients 66 years of age or older, to allow for a minimum of 1 year of baseline prescription information. Older patients often have important risk factors for hyperkalaemia and have full medication coverage through the provincial drug plan.17 We excluded laboratory tests with missing demographic information (approximately 0.75% of the tests). We also excluded hospital stays that were longer than 90 days to ensure that we had data for the entire hospitalisation, particularly when these occurred towards the end of our accrual period. For hyperkalaemia at presentation to an emergency department, the relevant potassium laboratory test must have occurred on an emergency department registration date or the day after. We allowed values for the date after registration to account for patients who may have come to an emergency department but did not receive their test until after midnight (ie, the day after). For hyperkalaemia at hospital admission, the relevant potassium laboratory test must have been done either in an emergency department up to 2 days prior to hospital admission, or up to 1 day after the date of hospital admission. We assigned this timeframe to account for any delays between an emergency department presentation and hospital admission, and any treatment that resulted in subsequent lower potassium values from the initial measurement. In both the emergency room and hospital settings, if multiple tests occurred, we took the highest available value. When multiple eligible hospital presentations were identified for a given patient over the study period, we randomly selected one.
Administrative database codes (diagnostic test)
In Canada, trained coders record appropriate diagnostic codes and their associated attributes based on information from a patient's chart. Coders in Canada follow specific rules and guidelines set out by CIHI when assigning diagnostic codes based on a patient's file. They are not allowed to interpret any diagnostic tests, such as x-rays or lab values, unless a diagnosis is specifically written by the physician in the medical chart.18 Within the NACRS database, coders are allowed to include up to 10 diagnoses per visit. The first diagnosis listed is the main problem for the patient's visit that required evaluation and/or treatment or management as determined by the physician at the end of the visit. The CIHI-DAD provides the ability to record up to 25 diagnoses during a hospital admission, each of which can have additional diagnosis types. For example, coders must assign one of the diagnoses the diagnosis type ‘M’, which represents the condition that was most responsible for the greatest portion of the length of stay or used the greatest amount of resources. They may also assign a diagnosis type ‘1’ to any of the listed diagnoses that existed prior to the admission and were treated during the hospital stay.
In this study, based on possible diagnosis types we developed two unique algorithms to assess hyperkalaemia at presentation to an emergency department and three unique algorithms to assess hyperkalaemia at hospital admission. We used the ICD-10 code E87.5, which is defined as ‘hyperkalaemia’. There is a Canadian Modification of the ICD-10 code system which provides additional information on other comorbidities but does not alter the hyperkalaemia coding. The two emergency department algorithms identified records with code E87.5 recorded: (1) as the main problem (referred to as ‘main diagnosis’) or (2) in any of the 10 potential diagnostic fields (referred to as ‘all diagnosis’). The three hospital admission algorithms identified records with code E87.5 recorded: (1) with the diagnosis type of ‘M’ (most responsible; referred to as ‘most responsible diagnosis’), (2) with the diagnosis type of ‘1’ (preadmit comorbidity; referred to as ‘preadmit diagnosis’) or (3) in any one of 25 potential diagnosis fields and any diagnosis type (referred to as ‘all diagnosis’).
Potassium laboratory values (reference standard)
Serum potassium laboratory tests were done either in an emergency department or in hospital and were used as the reference standard. The laboratory tests were performed with the Roche Modular Ion Selective Electrode system (Basel, Switzerland). The primary threshold to define hyperkalaemia was a serum potassium value >5.5 mmol/l. Other thresholds were also considered: >5.0, >6.0 and >6.5 mmol/l.
Data analysis
We assessed severity of hyperkalaemia based on several thresholds of serum potassium values indicated above. In the emergency department and hospital admission settings, we calculated the sensitivity, specificity, positive-predictive value and negative-predictive value of each coding algorithm for each serum potassium level (see online supplementary appendix B for two-by-two contingency table describing the relevant formulae). For the different algorithms we also contrasted the mean, median and IQRs of serum potassium values for those who were positive for the code compared with patients with hospital encounters who had no evidence of the code (ie, code negative). We calculated 95% CI for single proportions using the Wilson Score method.19 We expressed continuous variables as medians with IQR and compared means using independent samples t tests. We performed all analyses with SAS V.9.2 (SAS Institute Incorporated, Cary, North Carolina, USA, 2008).
Results
The cohort creation and specific exclusions for both settings are shown in online supplementary appendix C. Patient baseline characteristics are shown in table 1.
Table 1.
Baseline characteristics for patients with serum potassium values obtained at presentation to the emergency department and at hospital admission
| At emergency department | At hospital admission | |||
|---|---|---|---|---|
| N=64 579 | N=64 497 | |||
| Demographics | ||||
| Age (years) median (IQR) | 77 (71–83) | 77 (71–83) | ||
| Women (n (%)) | 35630 (55.2) | 32965 (51.1) | ||
| Income quintile (n (%)) | ||||
| One (lowest) | 14231 (22.0) | 13900 (21.6) | ||
| Two | 12921 (20.0) | 12928 (20.0) | ||
| Three (middle) | 12542 (19.4) | 12792 (19.8) | ||
| Four | 11496 (17.8) | 11601 (18.0) | ||
| Five (highest) | 12407 (19.2) | 12446 (19.3) | ||
| Rural Location (n (%)) | 11438 (17.7) | 13248 (20.5) | ||
| Year of cohort entry (n (%)) | ||||
| 2003–2004 | 6586 (10.2) | 11601 (18.0) | ||
| 2005–2006 | 15188 (23.5) | 15640 (24.3) | ||
| 2007–2008 | 20569 (31.9) | 18474 (28.6) | ||
| 2009–2010 | 22236 (34.4) | 18782 (29.1) | ||
| Long-term care facility utilisation (n (%)) | 4137 (6.4) | 3681 (5.7) | ||
| comorbidities, (n (%)) | ||||
| Chronic kidney disease† | 5335 (8.3) | 6427 (10.0) | ||
| Diabetes mellitus‡ | 13142 (20.4) | 13632 (21.1) | ||
| Peripheral vascular disease | 1690 (2.6) | 2937 (4.6) | ||
| Coronary artery disease§ | 26979 (41.8) | 30528 (47.3) | ||
| Heart failure | 13691 (21.2) | 15173 (23.5) | ||
| Stroke/Transient ischemic attack | 2455 (3.8) | 2655 (4.1) | ||
| Chronic liver disease | 1238 (1.9) | 1645 (2.6) | ||
| Medication use in prior 6 months, n (%) | ||||
| ACE inhibitors | 22690 (35.1) | 23770 (36.9) | ||
| Angiotensin-receptor blockers | 10442 (16.2) | 10012 (15.5) | ||
| Potassium sparing diuretics | 5657 (8.8) | 6147 (9.5) | ||
| Loop diuretics | 13553 (21.0) | 14618 (22.7) | ||
| Thiazide diuretics | 12334 (19.1) | 12458 (19.3) | ||
| Calcium channel blockers | 19126 (29.6) | 19951 (30.9) | ||
| β-adrenergic antagonists | 21989 (34.1) | 23382 (36.3) | ||
| Statins | 24892 (38.6) | 25273 (39.2) | ||
| NSAIDS (excluding aspirin) | 11621 (18.0) | 12573 (19.5) | ||
| Anticonvulstants | 3847 (6.0) | 3740 (5.8) | ||
| Antidepressants | 15662 (24.3) | 15075 (23.4) | ||
| Antipsychotics | 4001 (6.2) | 3532 (5.5) | ||
| Benzodiazepine | 15295 (23.7) | 15515 (24.1) | ||
| Antineoplastic drugs | 3285 (5.1) | 3624 (5.6) | ||
| Baseline laboratory measurements¶ | ||||
| Serum creatinine levels | ||||
| Most recent serum creatinine (µmol/l) median (IQR) | 90 (74–114) | 90 (74–114) | ||
| GFRŦ levels | ||||
| Most recent eGFR (ml/min/1.73 m2), median (IQR) | 63 (47–79) | 63 (47–79) | ||
| eGFR category (n (%))(ml/min/1.73 m2) | ||||
| ≥60 | 20807 (54.7) | 23842 (55.3) | ||
| 45–59 | 8527 (22.4) | 9566 (22.2) | ||
| 30–44 | 5466 (14.4) | 5989 (13.9) | ||
| 15–29 | 2362 (6.2) | 2694 (6.2) | ||
| <15 | 850 (2.2) | 1021 (2.4) | ||
| Serum sodium levels | ||||
| Most recent serum sodium (mmol/l) median (IQR) | 139 (137–141) | 139 (137–141) | ||
| Serum potassium levels | ||||
| Most recent serum potassium (mmol/l) median (IQR) | 4.2 (3.8–4.5) | 4.1(3.8–4.5) | ||
*We defined index date as the time of cohort entry.
†Assessed by administrative database codes: CIHI ICD-9 codes—4030, 3031, 4039, 4040, 4041, 4049, 582, 583, 580, 581, 584, 585, 586, 587, 5880, 5888, 5889, 5937; CIHI ICD-10 codes—I12, I13, N01, N03, N05, N07, N14, N15, N00, N04, N08, N18, N19, N26, N25, N137, N280, N2888, N06, N391; OHIP diagnostic codes—403, 580, 581, 585.
‡Assessed by diabetic medication use in previous 6 months.
§Coronary artery disease includes receipt of coronary artery bypass graft surgery, percutaneous coronary intervention and diagnoses of angina.
¶Available from emergency department, inpatient or outpatient settings for a subpopulation. A total of 33 104 (51.3%), 32 844 (50.9%) and 38 012 (58.9%) patients at presentation to emergency department had a baseline serum potassium, sodium and creatine measurement available in the 7–365 days prior to the index date, respectively. Among these patients, the baseline measurements were taken at a median (IQR) of 75 (25–174), 75(25–174) and 76 (26–173) days, respectively. A total of 39 552 (61.3%), 39 422 (61.1%) and 43 112 (66.9%) patients at hospital admission had a baseline serum potassium, sodium and creatine measurement available in the 7–365 days prior to the index date, respectively. Among these patients, the baseline measurements were taken at a median (IQR) of 29 (14–97), 29 (14–97) and 32(14–101) days, respectively.
ŦeGFR was calculated using the CKD-Epi equation.
CKD-Epi equation:141×min((serum creatine in µmol/l/88.4)/κ, 1)α × max((serum creatine in µmol/l/88.4)/κ, 1)−1·209×0.993Age × 1.018 (if female)×1.159 (if African American) κ=0.7 for females and 0.9 for males, α=−0.329 for females and −0.411 for males, min=the minimum of Scr/κ or 1, max=the maximum of Scr/κ or 1. Racial information was not available in our data sources and all patients were assumed not to be of non African-Canadian race. This was a reasonable assumption; as of 2006, African-Canadians represented less than 7% of the Ontario population. Source: http://www12.statcan.ca/census-recensement/2006/dp-pd/hlt/97–562/index.cfm?Lang=E
eGFR, estimated glomerular filtration rate.
Of the 64 579 patients who presented to an emergency department, 1679 (2.6%) had a potassium value of >5.5 mmol/l. Of 64 497 patients who were admitted to hospital, 2289 (3.5%) patients had a serum potassium level > 5.5 mmol/l. The diagnostic performance characteristics of the coding algorithms for hyperkalaemia (defined by serum potassium >5.5 mmol/l) in the two settings are presented in table 2. The algorithm that considered the E87.5 code as ‘all diagnoses’ demonstrated the best sensitivity, recognising the value still remained low. For example, the sensitivity of the ‘all diagnoses’ algorithm to detect a serum potassium >5.5 mmol/l in an emergency department was 14.1% and the specificity was 99.9%. Similar results were obtained for individuals with hyperkalaemia at hospital admission.
Table 2.
Diagnostic performance characteristics for ICD-10 E87.5 coding algorithms for hyperkalaemia defined by a serum potassium value >5.5 mmol/l at presentation to an emergency department and at hospital admission
| Emergency department |
Hospital admission |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ICD-10 E87.5 coding algorithm | + | − | Per cent (95% CI) | + | − | Per cent (95% CI) | ||||
| All diagnoses | + | 237 | 48 | Sn | 14.12 (12.53 to 15.86) | + | 335 | 205 | Sn | 14.64 (13.25 to 16.14) |
| − | 1442 | 62852 | Sp | 99.92 (99.90 to 99.94) | − | 1954 | 62003 | Sp | 99.67 (99.62 to 99.71) | |
| PPV | 83.16 (78.38 to 87.06) | PPV | 62.04 (57.87 to 66.03) | |||||||
| NPV | 97.76 (97.64 to 97.87) | NPV | 96.94 (96.81 to 97.08) | |||||||
| + | − | + | − | |||||||
| Main/most responsible diagnosis | + | 98 | 19 | Sn | 5.84 (4.81 to 7.06) | + | 59 | 8 | Sn | 2.58 (2.00 to 3.31%) |
| − | 1581 | 62881 | Sp | 99.97 (99.95 to 99.98) | − | 2230 | 62200 | Sp | 99.99 (99.97 to 99.99) | |
| PPV | 83.76 (76.03 to 89.35) | PPV | 88.06 (78.17 to 93.82) | |||||||
| NPV | 97.55 (97.43 to 97.66) | NPV | 96.54 (96.39 to 96.68) | |||||||
| + | − | |||||||||
| Preadmit diagnosis | + | 276 | 94 | Sn | 12.06 (10.79 to 13.46) | |||||
| − | 2013 | 62 114 | Sp | 99.85 (99.82 to 99.88) | ||||||
| PPV | 74.59 (69.92 to 78.76) | |||||||||
| NPV | 96.86 (96.72 to 96.99) | |||||||||
+, Hyperkalaemia yes; −, hyperkalaemia no; ICD-10, International Classification of Diseases, 10th revision; NPV, negative-predictive value; PPV, positive-predictive value; Sn, sensitivity; Sp, specificity.
The performance characteristics of the coding algorithms for the additional thresholds of serum potassium (> 5, >6 and >6.5 mmol/l) are presented in table 3. Of all the coding algorithms, those that considered the E87.5 code as ‘all diagnoses’ continued to demonstrate the best sensitivity across all the serum potassium thresholds. As well the sensitivity of the coding algorithm increased as hyperkalaemia became more severe (ie, a higher serum potassium level). For example, in an emergency department, for the ‘all diagnoses’ algorithm, the sensitivity was 6.6% for a potassium >5 mmol/l, and 21.8% for a potassium >6.5 mmol/l. Similarly, at hospital admission, for the ‘all diagnoses’ algorithm the sensitivity was 7.5% for a potassium >5 mmol/l and 29.5% for a potassium >6.5 mmol/l. The specificities were >99% and comparable across the different thresholds of serum potassium.
Table 3.
Diagnostic performance characteristics for other thresholds of serum potassium values at presentation to an emergency department and at hospital admission
| ICD-10 E87.5 coding algorithm | Emergency department |
Hospital admission (mmol/l) |
|||||
|---|---|---|---|---|---|---|---|
| >5 | >6 | >6.5 | >5 | >6 | >6.5 | ||
| Per cent (95% CI) | Per cent (95% CI) | Per cent (95% CI) | Per cent (95% CI) | Per cent (95% CI) | Per cent (95% CI) | ||
| All diagnoses | Sn | 6.55 (5.84 to 7.35) | 19.32 (16.73 to 22.21) | 21.81 (18.17 to 25.95) | 7.50 (6.83 to 8.22) | 23.34 (20.95 to 25.91) | 29.49 (25.76 to 33.51) |
| Sp | 99.98 (99.96 to 99.98) | 99.79 (99.76 to 99.83) | 99.70 (99.66 to 99.74) | 99.79 (99.75 to 99.82) | 99.56 (99.50 to 99.61) | 99.40 (99.34 to 99.46) | |
| PPV | 94.74 (91.50 to 96.78) | 54.04 (48.23 to 59.73) | 32.98 (27.78 to 38.64) | 76.85 (73.11 to 80.21) | 48.15 (43.96 to 52.36) | 28.89 (25.23 to 32.85) | |
| NPV | 94.01 (93.83 to 94.19) | 99.00 (98.92 to 99.07) | 99.48 (99.42 to 99.53) | 92.00 (91.78 to 92.20) | 98.66 (98.57 to 98.75) | 99.42 (99.35 to 99.47) | |
| Main/most responsible diagnosis | Sn | 2.65 (2.20 to 3.18) | 8.53 (6.79 to 10.68) | 9.05 (6.69 to 12.13) | 1.16 (0.91 to 1.47) | 4.94 (3.81 to 6.37) | 7.94 (5.93 to 10.56) |
| Sp | 99.99 (99.97 to 99.99) | 99.92 (99.90 to 99.94) | 99.88 (99.85 to 99.90) | 99.99 (99.99 to 100) | 99.98 (99.97 to 99.99) | 99.96 (99.94 to 99.97) | |
| PPV | 93.16 (87.09 to 96.49) | 58.12 (49.06 to 66.66) | 33.33 (25.44 to 42.28) | 95.52 (87.64 to 98.47) | 82.09 (71.25 to 89.45) | 62.69 (50.72 to 73.28) | |
| NPV | 93.78 (93.59 to 93.96) | 98.87 (98.78 to 98.95) | 99.39 (99.33 to 99.45) | 91.51 (91.29 to 91.72) | 98.36 (98.26 to 98.45) | 99.24 (99.17 to 99.31) | |
| Preadmit diagnosis | 5.84 (5.25 to 6.49) | 19.93 (17.69 to 22.38) | 25.71 (22.17 to 29.60) | ||||
| 99.92 (99.89 to 99.94) | 99.77 (99.73 to 99.80) | 99.63 (99.58 to 99.68) | |||||
| 87.30 (83.52 to 90.31) | 60.00 (54.93 to 64.86) | 36.76 (32.00 to 41.78) | |||||
| 91.87 (91.66 to 92.08) | 98.61 (98.52 to 98.70) | 99.39 (99.32 to 99.44) | |||||
ICD-10, International Classification of Diseases, 10th revision; NPV, negative-predictive value: PPV, positive-predictive value; Sn, sensitivity; Sp, specificity.
Serum potassium values as a continuous measure in groups of patients with hospital encounters that were code positive or negative are presented in table 4 and figure 1. There were highly statistically significant differences in serum potassium levels between the individuals who were code positive and code negative (for all algorithms; independent samples t test; all p values <0.0001). For example, in an emergency department using the ‘all diagnosis’ coding algorithm, the median (IQR) serum potassium value for patients who were code positive was 6.1 mmol/l (5.7 to 6.8 mmol/l) and 4.0 mmol/l (3.7 to 4.4 mmol/l) for those who were code negative. Similar results were evident for patients at hospital admission and for all algorithms.
Table 4.
Serum potassium values (mmol/l) in patients who were code positive and code negative for ICD-10 code E87.5 at presentation to the emergency department and at hospital admission according to different algorithms
| Emergency department |
Hospital admission |
|||||||
|---|---|---|---|---|---|---|---|---|
| N | Median | IQR | N | Median | IQR | |||
| All diagnosis | No | 64294 | 4.0 | 3.7–4.4 | No | 63957 | 4.1 | 3.8–4.5 |
| Yes | 285 | 6.1 | 5.7–6.8 | Yes | 540 | 6.0 | 5.1–6.7 | |
| Main/most responsible diagnosis | No | 64462 | 4.0 | 3.7–4.4 | No | 64430 | 4.1 | 3.8–4.5 |
| Yes | 117 | 6.2 | 5.7–6.9 | Yes | 67 | 6.9 | 6.1–7.5 | |
| Preadmit diagnosis | No | 64127 | 4.1 | 3.8–4.5 | ||||
| Yes | 370 | 6.3 | 5.5–6.9 | |||||
ICD-10, International Classification of Diseases, 10th revision; N, number of patients.
Figure 1.
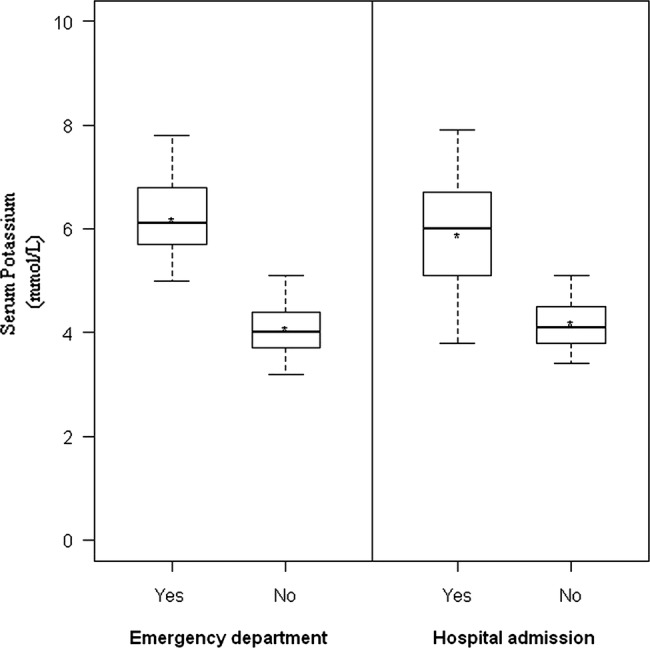
Serum potassium measurements among patients who are code positive and code negative for hyperkalaemia (when the code was considered in the format ‘all diagnoses’). For both presentation to an emergency department and at hospital admission, patients who for positive for the hyperkalaemia code had a significantly higher serum potassium measurement than patients who were code negative. The boxes represent the IQR (50% of the values). The line across the box indicates the median. The star indicates the mean. The whiskers extend to the 95th and 5th percentile.
A total of 51.3% of patients that presented to an emergency department had a baseline prehospital encounter serum potassium value. These baseline tests occurred at a median (IQR) of 75 (25 to 174) days prior to the emergency department presentation. This allowed us to examine the median change in serum potassium values (ie, emergency department value minus the baseline value). These results are presented in online supplementary appendix D. In an emergency department, for code-positive patients (using the ‘all diagnoses’ algorithm), the median (IQR) change in serum potassium values was 1.5 mmol/l (0.8 to 2.3 mmol/l) and for those who were code negative the change was –0.1 mmol/l (–0.5 to 0.3 mmol/l). The mean difference in the change in serum potassium values between code-positive and code-negative patients was 1.6 mmol/l (95% CI 1.5 to 1.7 mmol/l). Similar results were evident for the 61.3% of patients at hospital admission who had a baseline serum potassium measurement (which was taken a median (IQR) of 29 (14 to 97) days prior to hospital admission). In these patients using the ‘all diagnosis’ algorithm, the median (IQR) change (hospital value minus baseline value) in serum potassium was 1.3 mmol/l (0.4 to 2.3 mmol/) for those who were code positive and 0.0 mmol/l (–0.3 to 0.4 mmol/l) for those who were code negative. The mean difference in the change in serum potassium values between code-positive and code-negative patients was 1.4 mmol/l (95% CI 1.2 to 1.5 mmol/l).
Discussion
In this population-based validation study, we found that the best-performing ICD-10 coding algorithm for hyperkalaemia at presentation to an emergency department and at hospital admission was when the code was present in any diagnosis field (‘all diagnosis’), regardless of the threshold of serum potassium used to define hyperkalaemia. Overall, the specificity for the ICD-10 hyperkalaemia code was very high while the sensitivity was very low. There was a high false-negative rate in both the emergency room and hospital admission settings: just over 90% of patients with a serum potassium value of 5.5 mmol/l or more did not receive a code for hyperkalaemia using the all diagnoses category. Even when considering severe hyperkalaemia (serum potassium >6.5 mmol/l), the sensitivity only reached a maximum of about 29%.
The most responsible diagnosis is defined as the illness responsible for the longest length of stay or the greatest use of hospital resources. This algorithm demonstrated the lowest sensitivity among all the algorithms in our study, likely because the most responsible illness was attributed to the underlying problem that caused the hyperkalaemia rather than the hyperkalaemia itself.
We found that sensitivity increased as the severity of hyperkalaemia increased. Milder forms of hyperkalaemia tend to be asymptomatic and can be managed without aggressive treatment. Consequently, the physician may be less inclined in such cases to record a diagnosis of hyperkalaemia in the medical chart. In addition, hyperkalaemia often co-occurs with other more serious disorders that the physician may find to be paramount to hyperkalaemia when recording conditions in the medical chart. Furthermore, if the physician writes serum potassium 5.7 mmol/l for example, but does not write ‘hyperkalaemia’ or ‘high potassium’ the coders are unable to assume any diagnosis and some events are not recorded for this reason.18
Of the patients who had hyperkalaemia at presentation to an emergency department and at hospital admission (defined by a value >5.5 mmol/l), only 14.1% and 14.6%, respectively, were correctly coded as hyperkalaemic. The low sensitivity at this threshold may be due to less enthusiasm to act on values that are only modestly elevated. Despite this, the code was successful in differentiating between two groups of patients with distinct serum potassium values. Code-negative patients had serum potassium values in the normal range (3.5 to 5.1 mmol/l) and when the code was present, values were much higher (≥6 mmol/l).
Our study has several strengths. It is the first study to validate the ICD-10 code for hyperkalaemia and first to validate hyperkalaemia using laboratory values as the reference standard. We validated the ICD-10 code in both an emergency department and at hospital admission examining different types of diagnoses. Previous electrolyte validation studies have not looked at these settings nor did they examine all the possible diagnosis types as done in our study. Although there have been no similar hyperkalaemia validation studies, other electrolyte studies have demonstrated similarly low sensitivities of the ICD codes.20 21
All citizens in Ontario receive universal healthcare and patients over 65 have their medications paid for by the provincial government. These two factors facilitated the collection of health administrative data and gave us the ability to have a large sample size. We based our validation on laboratory data from 12 hospitals in the most populous province in Canada. Another study validating the ability of a computerised programme to correctly identify hyperkalaemia using the ICD-9 code restricted the analysis to a single centre and to the specific population of patient with diabetes.7 In addition, another study describing the frequency of hyperkalaemic events also focused on a specific population of veterans.22 Because we used a more varied and larger population, we were able to obtain good precision for estimates that are quite generalisable.
The validity measures that we used in this study have also been used in several other studies comparing ICD codes with clinical outcomes, including two validations of another electrolyte disorder, hyponatraemia.23–28 Many validation studies compare diagnostic codes with information written in medical charts. However, the most accurate way to determine whether hyperkalaemia is truly present is to use laboratory values as we did in the current study.
Our study does have some limitations. We validated the ICD-10 hyperkalaemia code in a population of patients over age 65. This patient population is particularly vulnerable to developing hyperkalaemia.29 In addition, these results inform future analyses of the Ontario healthcare databases since most pharmacoepidemiological research using these data sources are conducted in patients over age 65 (where receipt of prescription medications is a universal benefit). Moreover, a greater proportion of elderly patients receive a laboratory test compared with younger patients, reducing the potential for selection bias.30 Nonetheless, code validity in younger populations should be examined in future studies.
We were unable to determine if the patients who presented to an emergency department or at hospital admission showed arrhythmias or other sequelae of the high serum potassium value. However, we do know the code did identify acute changes, as demonstrated by a mean increase in serum potassium of 1.5 mmol/l above the baseline prehospital value. Patients with acute changes in serum potassium are most likely to be symptomatic from the condition.
Finally, we recognise that we did not capture those patients who may have had severe hyperkalaemia but did not go to an emergency department or hospital, or those who presented but failed to have serum potassium measured. However, the latter is less of a concern as serum potassium is a common test for most patients who present for acute medical care. We were unable to detect outpatient claims for hyperkalaemia in this study as there is no administrative code set available for this in our jurisdiction. Nevertheless, emergency department and hospital records do detect more severe forms of hyperkalaemia making this of particular interest to clinicians and policy decision makers.
Conclusion
Analyses of administrative codes are a cost-efficient way to assess patient comorbidity and disease in large population-based studies. However, as observed by the low sensitivity in the current study, many individuals with an ICD-10 database code for hyperkalaemia are missed leading to an underestimate of the true incidence of the condition at hospital encounters. It is important that members of the health community responsible for making decisions about healthcare be aware of the conditions and limitations of these codes to make fully informed evaluations. Nonetheless, the group of patients who were positive for this code were distinguishable from the group of patients who were negative for the code with distinct serum potassium values in both settings. The findings of this validation study guide proper use of the ICD-10 hyperkalaemia code in future research using health administrative data.
Acknowledgments
We thank Barbara Jones, Jeff Lamond, and the late Milton Haines for their help in providing access to Gamma-Dynacare laboratory data. We thank the team at London Health Sciences Centre, St. Joseph's Health Care, and the Thames Valley Hospitals for providing access to the Cerner laboratory data.
Footnotes
Contributors: JLF participated in the coordination of the study, study design, provided interpretation of study results and drafted the manuscript. SZS participated in the study design, performed the analysis and provided interpretation of study results. SG contributed to the study design and interpretation of study results. MAW and AKJ contributed to the study design and provided feedback on the manuscript. AXG conceived of the study, participated in its design and interpretation, helped draft the manuscript and provided feedback on the manuscript. All authors read and approved the final manuscript.
Funding: The study was supported by the Canadian Institutes of Health Research. AXG was supported by a Clinician Scientist Award from the Canadian Institutes of Health Research.
Competing interests: None.
Ethics approval: Sunnybrook Health Sciences Centre.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: There are no additional data available.
References
- 1.Elixhauser A, Steiner C, Harris RD, et al. Comorbidity measures for use with administrative data. Med Care 1998;36:8–27. [DOI] [PubMed] [Google Scholar]
- 2.Schaefer TJ, Wolford RW. Disorders of potassium. Emerg Med Clin N Am 2005;23:723–47. [DOI] [PubMed] [Google Scholar]
- 3.Elliott MJ, Ronksley PE, Clase CM, et al. Management of patients with acute hyperkalemia. CMAJ 2010;182:1631–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Palmer BF. Managing hyperkalemia caused by inhibitors of the renin-angiotensin-aldosterone system. N Engl J Med 2004;351:585–92. [DOI] [PubMed] [Google Scholar]
- 5.Reardon LC, Macpherson DS. Hyperkalemia in outpatients using angiotensin-converting enzyme inhibitors. Arch Intern Med 1998;158:26–32. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization. Fact Sheet May 2012: International Classification of Diseases (ICD). http://www.who.int/entity/classifications/icd/revision/icdfactsheet.pdf (accessed 18 May 2012).
- 7.Raebel MA, Smith ML, Saylor G, et al. The positive predictive value of a hyperkalemia diagnosis in automated health care data. Pharmacoepidemiol Drug Saf 2010;19:1204–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Statistics Canada. Age and Sex Highlights Table 2011 Census. http://www12.statcan.gc.ca/census-recensement/2011/dp-pd/hlt-fst/as-sa/?Lang=E (accessed 29 May 2012).
- 9.Gandhi S, Shariff S, Beyea M, et al. Identifying geographical regions serviced by hospitals to assess laboratory based outcomes. BMJ Open (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.STAndards for the Reporting of Diagnostic accuracy studies. STARD Checklist. http://www.stard-statement.org/ (accessed 13 Dec 2011).
- 11.Levy AR, O'Brien BJ, Sellors C, et al. Coding accuracy of administrative drug claims in the Ontario Drug Benefit database. Can J Clin Pharmacol 2003;10:67–71. [PubMed] [Google Scholar]
- 12.Cerner. Laboratory. http://www.cerner.com/solutions/Hospitals_and_Health_Systems/Laboratory/ (accessed 18 May 2012).
- 13.Zhao YY, Weir MA, Manno M, et al. New fibrate use and acute renal outcomes in elderly adults: a population-based study. Ann Intern Med 2012;156:560–9. [DOI] [PubMed] [Google Scholar]
- 14.Jain AK, Cuerden MS, McLeod I, et al. Reporting of the estimated glomerular filtration rate was associated with increased use of angiotensin-converting enzyme inhibitors and angiotensin-II receptor blockers in CKD. Kidney Int 2012;81:1248–53. [DOI] [PubMed] [Google Scholar]
- 15.Weir MA, Gomes T, Mamdani M, et al. Impaired renal function modifies the risk of severe hypoglycaemia among users of insulin but not glyburide: a population-based nested case–control study. Nephrol Dial Transplant 2011;26:1888–94. [DOI] [PubMed] [Google Scholar]
- 16.Molnar AO, Coca SG, Devereaux PJ, et al. Statin use associates with lower incidence of acute injury after major elective surgery. J Am Soc Nephrol 2011;22:939–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Juurlink DN, Mamdani MM, Lee DS, et al. Rates of hyperkalemia after publication of the Randomized Aldactone Evaluation Study. NEJM 2004;351:543–51. [DOI] [PubMed] [Google Scholar]
- 18.Canadian Institute for Health Information. Canadian coding standards for Version 2012 ICD-10-CA and CCI. https://secure.cihi.ca/free_products/canadian_coding_standards_2012_e.pdf (accessed 2 May 2012).
- 19.Newcombe RG. Two-sided confidence intervals for the single proportion: comparison of seven methods. Stat Med 1998;17:857–72. [DOI] [PubMed] [Google Scholar]
- 20.Movig KL, Leufkens HG, Lenderink AW, et al. Validity of hospital discharge International Classification of Diseases (ICD) codes for identifying patients with hyponatremia. J Clin Epidemiol 2003;56:530–5. [DOI] [PubMed] [Google Scholar]
- 21.Shea AM, Curtis LH, Szczech LA, et al. Sensitivity of International Classification of Diseases codes for hyponatremia among commercially insured outpatients in the United States. BMC Nephrol 2008;9:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Einhorn LM, Zhan M, Hsu VD, et al. The frequency of hyperkalemia and its significance in chronic kidney disease. Arch Intern Med 2009;169:1156–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Waiker SS, Wald R, Chertow GM, et al. Validity of International Classification of Diseases, Ninth Revision, Clinical Modification codes for acute renal failure. J Am Soc Nephrol 2006;17:1688–94. [DOI] [PubMed] [Google Scholar]
- 24.Romano PS, Roos LL, Luft HS, et al. A comparison of administrative versus clinical data: coronary artery bypass surgery as an example. Ischemic Heart Disease Patient Outcomes Research Team. J Clin Epidemiol 1994;47:249–60. [DOI] [PubMed] [Google Scholar]
- 25.Quan H, Parsons GA, Ghali WA. Validity of procedure codes in International Classification of Diseases, 9th revision, clinical modification administrative data. Med Care 2004;42:801–9. [DOI] [PubMed] [Google Scholar]
- 26.Raiford DS, Perez Gutthann S, Garcia Rodriguez LA, et al. Positive predictive value of ICD-9 codes in the identification of cases of complicated peptic ulcer disease in the Saskatchewan hospital automated database. Epidemiology 1996;7:101–4. [DOI] [PubMed] [Google Scholar]
- 27.Gankam KF, Andres C, Sattar L, et al. Mild hyponatremia and risk of fracture in the ambulatory elderly. Q J Med 2008;101:583–8. [DOI] [PubMed] [Google Scholar]
- 28.Waikar SS, Mount DB, Curhan GC. Mortality after hospitalization with mild, moderate, and severe hyponatremia. Am J Med 2009;122:857–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Obreli-Neto PR, Nobili A, de Oliveira Baldoni A, et al. Adverse drug reactions caused by drug-drug interactions in elderly outpatients: a prospective cohort study. Eur J Clin Pharmacol 2012;68:1667–76. [DOI] [PubMed] [Google Scholar]
- 30.Singal BM, Hedges JR, Rousseau EW, et al. Geriatric patient emergency visits. Part 1: comparison of visits by geriatric and younger patients. Ann Emerg Med 1992;21:802–7. [DOI] [PubMed] [Google Scholar]


