Abstract
Background:
Keratoconus is a contraindication for photorefractive keratectomy (PRK). In the recent decade, some efforts have been made to perform PRK in patients with keratoconus whose corneas are stable naturally or by doing corneal collagen crosslinking. These studies have suggested residual central corneal thickness (CCT) ≥450 μm.
Aims:
The aim was to evaluate the long-term outcomes of PRK in patients with mild to moderate keratoconus in patients older than 40 with residual CCT ≥ 400 μm.
Settings and Design:
This prospective study was conducted in our Cornea Research Center, Mashhad, Iran.
Materials and Methods:
Patients over 40 years old, with a grade I/II keratoconus without progression in the last 2 years were recruited. Patients with a predicted postoperative CCT < 400 μm were excluded. PRK with tissue saving protocol was performed with Tecnolas 217 Z. Mitomycin-C was applied after ablation. The final endpoints were refraction parameters the last follow-up visit (mean: 35 months). Paired t-test and Chi-square were used for analysis.
Results:
A total of 38 eyes of 21 patients were studied; 20 eyes (52.6%) with a grade I and 18 eyes (47.4%) with grade II keratoconus. The mean uncorrected visual acuity, best corrected visual acuity (BCVA), spherical equivalent, cylindrical power and keratometric readings were significantly improved at the final endpoint compared to preoperation measurements (P < 0.001). Two eyes (5%) lost two lines of BCVA at the final visit. No case of ectasia occurred during the follow-up course.
Conclusions:
PRK did not induce keratoconus progression in patients older than 40 with a grade I/II keratoconus. Residual CCT ≥ 450 μm seems to be sufficient to prevent the ectasia.
Keywords: Ectasia, keratoconus, photorefractive keratectomy
Keratoconus is a common bilateral, asymmetric, noninflammatory ecstatic corneal disorder with a prevalence of about 1/20,000.[1] Although refractive correction with spectacles or contact lenses can provide acceptable improvement in visual acuity for many of these patients, the quality of vision would be still poor as a result of irregular astigmatism. Several treatment modalities have been introduced for the management of keratoconus.[2]
Studies on the biomechanical characteristics of the cornea have shown that senile changes of corneal collagen fibers lead to progressive corneal stiffness. The aforementioned studies have also exhibited a negative relationship between the corneal viscoelastic factor and age. Continuous corneal collagen crosslinking (CXL) takes place with aging and halts the progression of keratoconus or even reverses this condition.[3,4] Thus, it can be hypothesized that with increasing age (>40 years), when the cornea is stabilized, and the keratoconus progression has stopped, photorefractive keratectomy (PRK) could be performed with safety. Several basic studies have shown that CXL can be accelerated by treating the cornea with ultra violet light (370 nm) after instilling riboflavine 0.1% drop. This would stabilize the cornea, which tends to become progressively thin.[5,6] For example, one recent study has reported good results of PRK on myopia and astigmatism 1-year after performing the CXL procedure.[7] It should be noted that several other studies have reported acceptable results with laser in situ keratomileusis and PRK methods in patients with suspected or mild keratoconus that were stable for some time.[8,9,10,11,12,13] Two recent studies, conducted by Chelala et al. and Guedj et al. reported excellent outcome of PRK in a long-term follow-up in patients with grade I/II keratoconus and suspected keratoconus, respectively.[14,15] The residual central corneal thickness (CCT) was ≥450 μm in these two studies, which is considered to be safe in keratoconus patients, although we know that the safe residual thickness in considered ≈250 μm in nonkeratoconus patients. The purpose of the present study was to evaluate the long-term outcomes of PRK in patients over 40 years of age suffering from mild to moderate keratoconus with residual CCT of ≥400 μm regarding the natural collagen CXL which would halt the disease progression.
Materials and Methods
This prospective study comprised 21 patients over 40 years of age, diagnosed with mild to moderate keratoconus (grade I and II) according to the Amsler–Krumeich classification (grade 1, eccentric corneal bulging, myopia, and/or astigmatism <5 D and corneal radius ≤48 D, no corneal opacities; grade II, myopia and/or astigmatism >5 D and <8 D and/or corneal radius ≤53 D, no central opacities, pachymetry ≥400 μm), whom visited our two ophthalmology centers from June 2010 to January 2011. The study protocol was approved by the institutional review board and ethics committee of the Mashhad University of Medical Sciences and adhered to the tenets of the Declaration of Helsinki. A separate informed consent sheet was signed by all the patients prior to study entrance. They were fully informed about the possibility of progression of keratoconus after refractive surgery and that if so, the only therapeutic option could be keratoplasty. Patients who could do well with contact lenses and had a reasonable uncorrected visual acuity (UCVA) were not recruited.
All patients were followed for at least 2 years before surgery with slit lamp examination, manifest refraction, retinoscopy, corneal topography using the Tomey TMS-2 apparatus (Tomey, Erlangen, Germany) and Orbscan (IIZ-Bausch and Lomb, Germany) to make sure no progression would happen. Visual acuity was obtained using the standard 20 feet Snellen acuity chart and was converted to logMAR with the purpose of statistical analysis. Just prior to surgery, the above-mentioned examinations were repeated in addition to ultrasound pachymetry (Sonogage; Corneo-Gage Plus, Cleveland, Ohio). Dilated pupil ophthalmoscopy was performed to rule out retinal problems. Patients with a known absolute or relative contraindication for PRK and those with a predicted postoperative CCT of <400 μm were excluded.
Standard PRK with tissue saving protocol was carried out on both eyes of all but 4 of the patients who underwent unilateral PRK by a single experienced surgeon (H. K, MD) using a 193 nm Gaussian scan flying spot excimer laser system (Tecnolas 217 Z, Bausch and Lomb, USA). The procedure was performed under topical anesthesia with the tetracaine 1% eye drop. At first the epithelium was removed within an 8.5 mm diameter by exposing the epithelium to absolute alcohol placed in an 8.5 mm well for 20 s and then the debridement with a surgical sponge. The diameter of the ablation was between 6 and 6.5 mm. At the end of the ablation, the cornea was treated with mitomycin-C. The exposure time was set proportional to the depth of ablation; 10˝ for 60 μm, 20˝ for 61–80 μm, 30˝ for 81–100 μm and 45˝ for 101–120 μm. A bandage contact lens was then placed on the cornea and Ciprofloxacin 0.3% (Ciplex-Sina Daru, Tehran, Iran) drop was instilled. The Ciprofloxacin drop 6 times daily, Betamethasone 0.1% (Betasonite-Sina Daru, Tehran, Iran) drop 6 times daily, Diclofenac 0.1% (Dicloptine-Sina Daru, Tehran, Iran) drop 4 times daily (only for the first 48 h), and preservative free artificial tear drop were prescribed. Betamethasone drop was changed to fluorometholone 0.1% (Floucort-Sina Daru, Tehran, Iran) after 2 weeks from the surgery to reduce the risk of steroid-induced intraocular pressure rise. The steroid dosage was tapered during the 1st month after surgery. Artificial tear drops were used frequently in the first 3 months postoperatively.
Follow-up examinations were performed for all patients on the 1st day, 1st week, day 40, 3rd month and then every 12 months postoperatively. UCVA, best corrected visual acuity (BCVA), mean spherical equivalent (SE) of refractive error, cylindrical component of refractive error and mean keratometric reading on the 40th day postoperative visit were considered as the primary endpoint. The same parameters measured on the 12 months and the last follow-up (mean: 35 ± 8.5 months) visits were the secondary and final endpoints, respectively. Eleven patients performed Orbscan at their last follow-up visit.
Statistics
Statistical analysis was performed using the SPSS software (Statistical Package for Social Sciences, version 13 SPSS, Inc., Chicago, IL, USA). Qualitative variables were expressed as percentages, and quantitative data were expressed as mean values with standard deviations (SD). T-test was used for quantitative data, and Chi-square was used for qualitative variables analysis. To evaluate the evolution of the quantitative variables through the follow-up course, repeated measure analysis was used. P < 0.05 was regarded as statistically significant.
Results
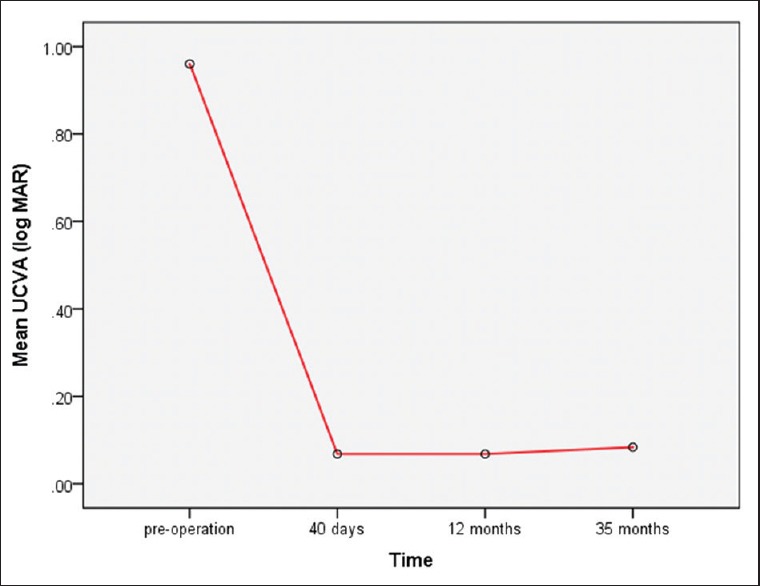
A total of 38 eyes of 21 patients with the mean age of 43.94 ± 3.16 years (range: 40–51 years) were studied. Twenty eyes (52.6%) were in grade I and 18 (47.4%) were in grade II of keratoconus based on the Amsler–Krumeich classification. Table 1 summarizes the demographic data of the study population.
Table 1.
Demographic data and corneal characteristics of the studied patients
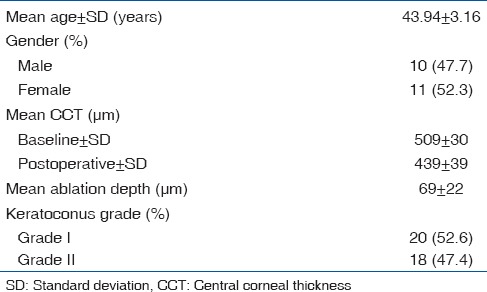
Uncorrected visual acuity, BCVA, SE and the cylindrical component of refractive error of the patients showed a significant improvement at both the first (40th day postoperative visit) and the last (35th month postoperative visit) endpoints (paired t-test, P < 0.05) [Table 2]. On the last follow-up visit, in 22 eyes (58%) UCVA had improved to 20/20 and in 8 eyes (21%) it had reached to 20/25. Two eyes (5%) lost 2 lines at the last follow-up visit. BCVA was also lost for two lines in 2 eyes (5%) while the other eyes maintained their preoperative BCVA. The evolution of UCVA, BCVA, SE and the cylindrical component of the refractive error are presented in Figs. 1–4, respectively.
Table 2.
Comparison between the baseline refraction parameters of the studied eyes and postoperative values
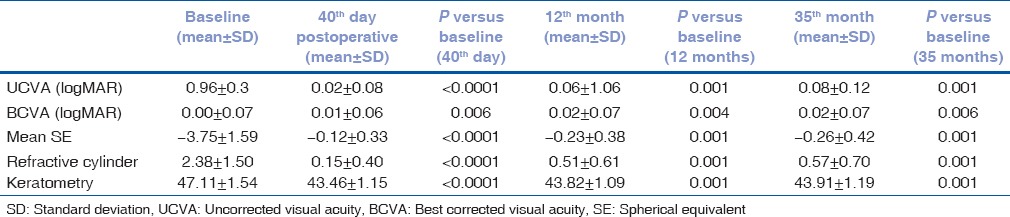
Figure 1.
Evolution of uncorrected visual acuity from preoperation through the last follow-up visit (repeated measure analysis)
Figure 4.
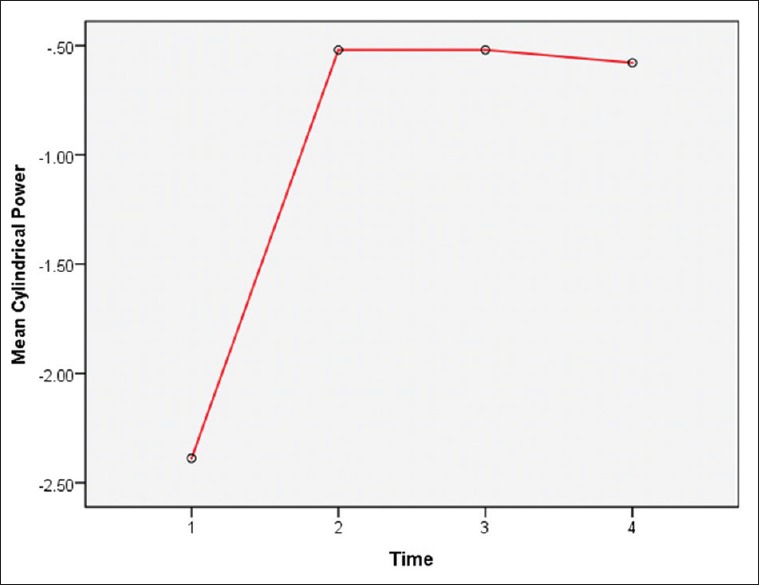
Evolution of the cylindrical component of the refractive error from preoperation through the last follow-up visit (repeated measure analysis)
Figure 2.
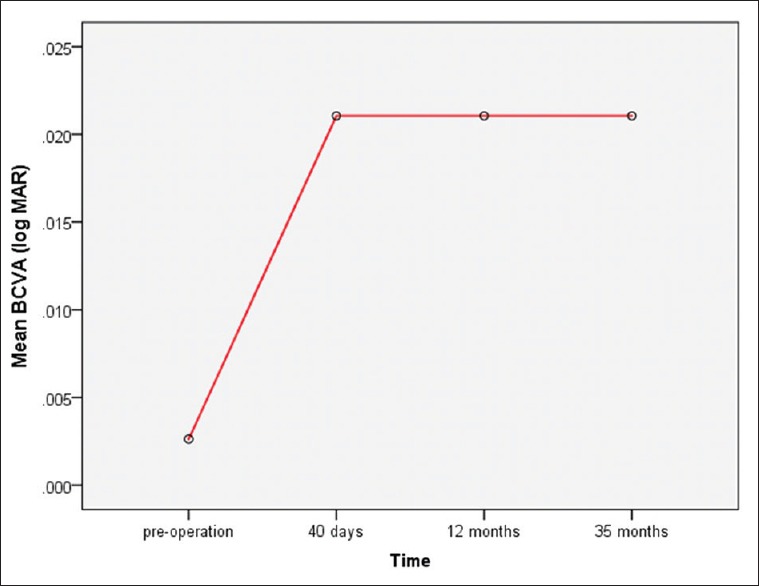
Evolution of best corrected visual acuity from preoperation through the last follow-up visit (repeated measure analysis)
Figure 3.
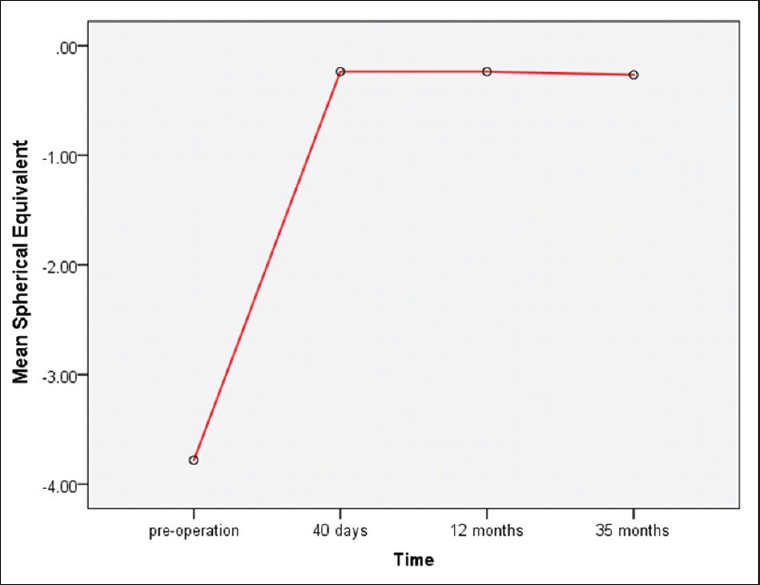
Evolution of the spherical equivalent of the refractive error from preoperation through the last follow-up visit (repeated measure analysis)
The mean keratometric reading was 47.11 ± 1.54 before surgery, 43.46 ± 1.15 at the primary endpoint and 43.93 ± 1.19 at the final endpoint. The difference between the mean keratometry before surgery and that of both the primary and final endpoints was statistically significant (paired t-test, P < 0.001) [Table 2 and Fig. 5]. The mean ratio of the keratometric power of the steepest to the flattest meridian in the central 3 mm of the cornea (S/F ratio) was 1/04 ± 0/02 preoperatively and 1/03 ± 0/02 at the final endpoint, showing a significant decrease (paired t-test, P < 0.001).
Figure 5.
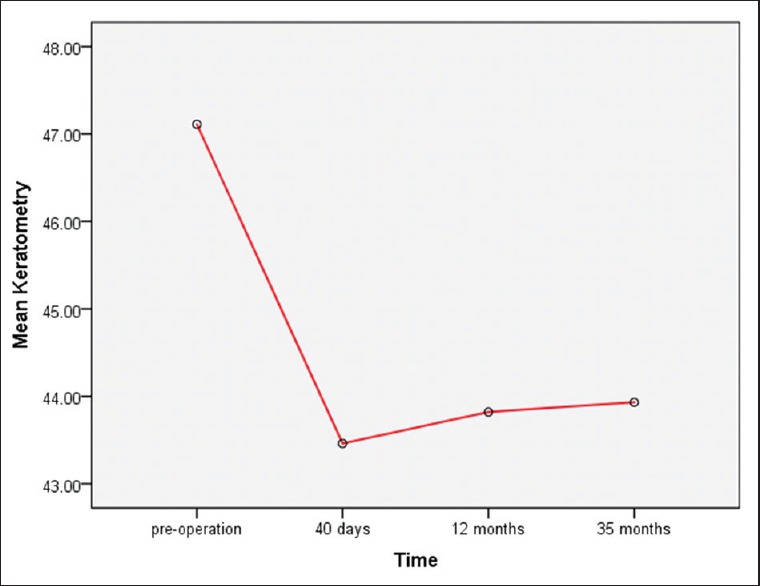
Evolution of the mean keratometric reading from preoperation through the last follow-up visit (repeated measure analysis)
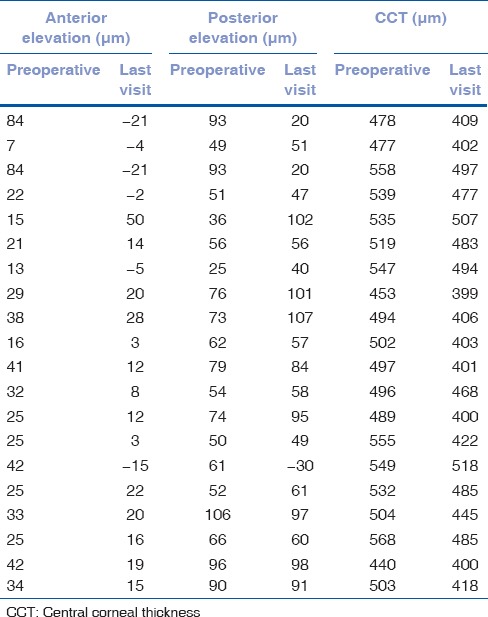
Anterior corneal elevation showed a statistically significant decrease in 20 eyes of 11 patients who performed Orbscan both preoperatively and postoperatively (P = 0.004). Posterior corneal elevation didn’t change significantly after PRK (paired t-test, P = 0.641) [Table 3]. Mean CCT of the patients provided with Orbscan was 512 μm (range: 440–568) preoperatively and 440 μm (range: 400–518) at the last visit [Table 3].
Table 3.
Anterior and posterior corneal elevation from best fit sphere, and CCT, preoperatively and at the last follow-up visit in 20 eyes
To evaluate the surgical outcome, patients were classified into three groups, according to refraction, pachymetry and Orbscan findings, as follows:
Group 1: Those eyes within the ± 0.5 D spherical or cylindrical refractive error at both the primary and final endpoints were considered as emmetropic
Group 2: The eyes with >−0.50 D residual SE refractive error at the primary endpoint, were defined as undercorrected
Group 3: Eyes with more than 0.5 D spherical or cylindrical power change from the primary endpoint through the final endpoint were considered ectasia, as theoretically there is no possibility of regression in this range of age.
Through the last follow-up visit, 33 eyes (86.8%) had reached emmetropia, and five eyes (13.2%) were undercorrected. None of the studied eyes met the definition of ectasia during the study period, and there was no significant difference between the grade I and grade II keratoconus in the outcome (Chi-square test, P = 0.648).
Discussion
The purpose of the present study was to evaluate the outcome of PRK in mild to moderate keratoconus (grade I and II Amsler–Krumeich). Our study showed significant improvement of UCVA in the eyes with mild to moderate keratoconus after refractive surgery and remained so over the course of 35 months follow-up. The results of our study are comparable with those of Cennamo et al.[16] In their study, twenty-five eyes with grade II keratoconus were treated by topography-guided PRK and followed for 24 months. They reported a significant and stable improvement in UCVA, BCVA and both the spherical and cylindrical components of the refractive error during a 24 months follow-up course. Chelala et al. reported good refractive and topographic results of PRK in grade I and II keratoconus after 5 years follow-up.[14] Similarly, Alpins and Stamatelatos reported stable UCVA and BCVA, 1-year after PRK in forme fruste and mild keratoconus with no case of keratoconus progression observed during the follow-up course.[8] Although, not clinically and statistically significant, the mean UCVA in our study decremented from the first through the final endpoint [Fig. 1]. Unlike UCVA, BCVA remained nearly unchanged through the last follow-up visit, demonstrating corneal stability after surgery. As Koller et al. recommended in their study,[12] Chelala kept a minimum residual corneal thickness of ≥450 μm. The mean age of patients in our study was ≈ 44 years old which was more than 10 years older than the patients in Chelala's study (31.5 years old), which means much more stiffness of the cornea secondary to natural collagen CXL. Hence, we accepted the minimum residual CCT of ≥400 μm as to be safe. This way, some patients who would be excluded with the cut-off point of 450 μm could now benefit from the treatment. The finding of the present study, reporting no case of ectasia, is similar to Cennamo's study. Similarly, no adverse effect of this type of surgery on the cornea and the disease process was observed in Bilgihan et al. and Mortensen and Ohrström studies.[17,18] However, Chelala et al. reported two cases of keratoconus progression out of 119 eyes with grade I and II whom ultimately underwent CXL. Using intraoperative mitomycin C, no visually significant subepithelial corneal haze was observed in our patients as in Chelala's study.[14]
Conclusions
The results of the present study, with a mean follow-up period of 35 months, support the idea that PRK is a safe and effective procedure for improving the visual function of patients suffering from grade I and II keratoconus, with minimal risk of progression or ectasia. However, careful patient selection is needed to prevent side effects. Moreover, making sure of corneal stability and cessation of keratoconus progression is vital to avoid ectasia. We could show that a minimum residual CCT of 400 μm would be enough for preventing keratoconus progression and ectasia after PRK in patients over 40 years old in a follow-up course of 3 years. Nevertheless, ectasia may occur even 10 years following PRK.[19] Hence, longer follow-up is needed for the evaluation of post-PRK ectasia.
Acknowledgment
The authors received generous free technical support from “Navid Didegan” Eye Clinic.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Rabinowitz YS. Keratoconus. Surv Ophthalmol. 1998;42:297–319. doi: 10.1016/s0039-6257(97)00119-7. [DOI] [PubMed] [Google Scholar]
- 2.Jhanji V, Sharma N, Vajpayee RB. Management of keratoconus: Current scenario. Br J Ophthalmol. 2011;95:1044–50. doi: 10.1136/bjo.2010.185868. [DOI] [PubMed] [Google Scholar]
- 3.Kirwan C, O’Keefe M, Lanigan B. Corneal hysteresis and intraocular pressure measurement in children using the reichert ocular response analyzer. Am J Ophthalmol. 2006;142:990–2. doi: 10.1016/j.ajo.2006.07.058. [DOI] [PubMed] [Google Scholar]
- 4.Zadnik K, Barr JT, Edrington TB, Everett DF, Jameson M, McMahon TT, et al. Baseline findings in the Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study. Invest Ophthalmol Vis Sci. 1998;39:2537–46. [PubMed] [Google Scholar]
- 5.Seiler T, Hafezi F. Corneal cross-linking-induced stromal demarcation line. Cornea. 2006;25:1057–9. doi: 10.1097/01.ico.0000225720.38748.58. [DOI] [PubMed] [Google Scholar]
- 6.Wollensak G, Spörl E, Seiler T. Treatment of keratoconus by collagen cross linking. Ophthalmologe. 2003;100:44–9. doi: 10.1007/s00347-002-0700-3. [DOI] [PubMed] [Google Scholar]
- 7.Kanellopoulos AJ, Binder PS. Collagen cross-linking (CCL) with sequential topography-guided PRK: A temporizing alternative for keratoconus to penetrating keratoplasty. Cornea. 2007;26:891–5. doi: 10.1097/ICO.0b013e318074e424. [DOI] [PubMed] [Google Scholar]
- 8.Alpins N, Stamatelatos G. Customized photoastigmatic refractive keratectomy using combined topographic and refractive data for myopia and astigmatism in eyes with forme fruste and mild keratoconus. J Cataract Refract Surg. 2007;33:591–602. doi: 10.1016/j.jcrs.2006.12.014. [DOI] [PubMed] [Google Scholar]
- 9.Reinstein DZ, Archer TJ, Gobbe M. Stability of LASIK in topographically suspect keratoconus confirmed non-keratoconic by Artemis VHF digital ultrasound epithelial thickness mapping: 1-year follow-up. J Refract Surg. 2009;25:569–77. doi: 10.3928/1081597X-20090610-02. [DOI] [PubMed] [Google Scholar]
- 10.Sun R, Gimbel HV, Kaye GB. Photorefractive keratectomy in keratoconus suspects. J Cataract Refract Surg. 1999;25:1461–6. doi: 10.1016/s0886-3350(99)00234-5. [DOI] [PubMed] [Google Scholar]
- 11.Bahar I, Levinger S, Kremer I. Wavefront-supported photorefractive keratectomy with the Bausch and Lomb Zyoptix in patients with myopic astigmatism and suspected keratoconus. J Refract Surg. 2006;22:533–8. doi: 10.3928/1081-597X-20060601-04. [DOI] [PubMed] [Google Scholar]
- 12.Koller T, Iseli HP, Donitzky C, Ing D, Papadopoulos N, Seiler T. Topography-guided surface ablation for forme fruste keratoconus. Ophthalmology. 2006;113:2198–202. doi: 10.1016/j.ophtha.2006.06.032. [DOI] [PubMed] [Google Scholar]
- 13.Kremer I, Shochot Y, Kaplan A, Blumenthal M. Three year results of photoastigmatic refractive keratectomy for mild and atypical keratoconus. J Cataract Refract Surg. 1998;24:1581–8. doi: 10.1016/s0886-3350(98)80346-5. [DOI] [PubMed] [Google Scholar]
- 14.Chelala E, Rami HE, Dirani A, Fadlallah A, Fakhoury O, Warrak E. Photorefractive keratectomy in patients with mild to moderate stable keratoconus: A five-year prospective follow-up study. Clin Ophthalmol. 2013;7:1923–8. doi: 10.2147/OPTH.S52281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guedj M, Saad A, Audureau E, Gatinel D. Photorefractive keratectomy in patients with suspected keratoconus: Five-year follow-up. J Cataract Refract Surg. 2013;39:66–73. doi: 10.1016/j.jcrs.2012.08.058. [DOI] [PubMed] [Google Scholar]
- 16.Cennamo G, Intravaja A, Boccuzzi D, Marotta G, Cennamo G. Treatment of keratoconus by topography-guided customized photorefractive keratectomy: Two-year follow-up study. J Refract Surg. 2008;24:145–9. doi: 10.3928/1081597X-20080201-04. [DOI] [PubMed] [Google Scholar]
- 17.Bilgihan K, Ozdek SC, Konuk O, Akata F, Hasanreisoglu B. Results of photorefractive keratectomy in keratoconus suspects at 4 years. J Refract Surg. 2000;16:438–43. doi: 10.3928/1081-597X-20000701-06. [DOI] [PubMed] [Google Scholar]
- 18.Mortensen J, Ohrström A. Excimer laser photorefractive keratectomy for treatment of keratoconus. J Refract Corneal Surg. 1994;10:368–72. [PubMed] [Google Scholar]
- 19.Kim H, Choi JS, Joo CK. Corneal ectasia after PRK: Clinicopathologic case report. Cornea. 2006;25:845–8. doi: 10.1097/01.ico.0000224634.72309.43. [DOI] [PubMed] [Google Scholar]


