Abstract
Background
Metabolic syndrome (MetS) is associated with carotid intima-media thickness (CIMT), which is a good predictor of cardiovascular disease (CVD). However, among individuals with MetS, direct comparative data regarding the utility of the apoB/apoAΙ ratio and the non-HDL-C/HDL-C ratio to diagnose carotid atherosclerosis are scarce, particularly in Chinese populations. We aimed to determine the relationship between the apoB/apoAΙ ratio and the non-HDL-C/HDL-C ratio and carotid atherosclerosis among Chinese individuals with MetS.
Methods
We performed a retrospective study of 5822 Chinese participants who underwent a routine health screening examination. Lipid profiles, fasting glucose, fasting insulin, CRP, apoB, apoAΙ and CIMT were measured.
Results
We observed that among Chinese individuals with MetS, men (53.95 ± 0.58 ys) developed carotid atherosclerosis at a younger age than women (58.47 ± 1.17 ys) (P < 0.001). Both the apoB/apoAΙ ratio and the non-HDL-C/HDL-C ratio positively correlated with carotid atherosclerosis among Chinese individuals with MetS, particularly among women. Meanwhile, CIMT increased progressively across the quartiles of the non-HDL-C/HDL-C ratio (P for trend, < 0.05). Receiver Operating Characteristic (ROC) analysis indicated that the AUC of the apoB/apoAΙ ratio (0.561) was higher than that of the non-HDL-C/HDL-C ratio (0.522) in men (P < 0.05) and the AUC of the apoB/apoAΙ ratio (0.640) was lower than that of the non-HDL-C/HDL-C ratio (0.695) in women (P < 0.05). Among Chinese individuals with MetS, the AUC of the non-HDL-C/HDL-C ratio was more prominent among women compared with men (P < 0.05).
Conclusion
Our findings indicate that among individuals with MetS, Chinese men develop carotid atherosclerosis at a much younger age than women. There were no significant differences between the apoB/apoAΙ ratio and the non-HDL-C/HDL-C ratio for the prediction of carotid atherosclerosis among Chinese individuals with MetS. Among Chinese individuals with MetS, the utility of the non-HDL-C/HDL-C ratio was found to be greater among women than among men.
Keywords: Carotid atherosclerosis, Carotid intima-media thickness, Metabolic syndrome, ApoB/apoAΙ, Non-HDL-C/HDL-C
Introduction
Metabolic syndrome (MetS) is strongly associated with various cardiovascular risk factors, including visceral obesity, hypertension, hypertriglyceridemia, a low level of high density lipoprotein cholesterol, and impaired glucose tolerance [1,2]. Individuals with MetS are at an increased risk of developing cardiovascular disease, cardiovascular morbidity, mortality, and all-cause mortality [3,4]. The prevalence is estimated to be approximately 34% among adults in the USA [5], and 14%-17% among adults in China [6]. These rates are likely to increase due to the aging of the population.
Carotid intima-media thickness (CIMT) is an early indicator of atherosclerosis [7,8], and is a validated measurement of subclinical atherosclerosis [9]. Among the indicators of cardiovascular disease, CIMT is considered to be an early marker of the disease; therefore, it is widely used as a diagnostic tool [10,11]. Several studies have used both the apolipoprotein B (apoB)/apolipoprotein AΙ (apoAΙ) ratio and the non-HDL-C/HDL-C ratio to estimate the likelihood of having carotid atherosclerosis. In the setting of both type 2 diabetes mellitus and normal glucose tolerance (NGT), the apoB/apoAΙ ratio is more strongly associated with CIMT than conventional lipids [12,13]. Generally, the non-HDL-C/HDL-C ratio is believed to be superior to traditional lipid variables in estimating arterial stiffness among middle-aged and elderly Chinese individuals [14].
Several studies have described the relationship between MetS and CIMT [3,15-17]. However, direct comparative data regarding the utility of the apoB/apoAΙ ratio, the non-HDL-C/HDL-C ratio, insulin resistance (IR), conventional lipids and the relationship between these parameters and increased CIMT are scarce among individuals with MetS. Given the increasing incidence of MetS in China, it is important to identify the best method with which to assess the risk of cardiovascular disease (CVD). Very few studies have assessed the utility of apolipoprotein and lipoprotein cholesterol measurements in determining the risk of CVD among Chinese individuals. In the present study, we examined the relationship among carotid atherosclerosis, the apoB/apoAΙ ratio, and the non-HDL-C/HDL-C ratio, as well as conventional lipids, IR, and C reactive protein (CRP), among Chinese individuals with MetS. We also aimed to determine whether gender differences exist in this association [18].
Methods
Subjects
We collected data from 5822 subjects between 18 and 85 years of age who underwent a health examination at the Second Affiliated Hospital, School of Medicine, Zhejiang University, between September 2011 and December 2012. Most of the patients were from Zhejiang province. 4908 individuals were included in the statistical analysis, of whom 3039 men, aged 45.12 ± 9.10 years, and 1869 women, aged 44.92 ± 9.79 years (P > 0.05) were ultimately included in the study, following the exclusion of individuals with either cardiovascular or cerebrovascular disease, cancer, diabetes, severe mental disorders, or chronic kidney disease [19], as well as individuals receiving lipid-lowering agents, anti-thyroid agents, and individuals with acute and chronic liver disease, infectious diseases, acute and chronic fevers of unknown origin, and who consumed excessive alcohol [20]. Among these individuals, 1863 were diagnosed with MetS, 1492 of which were men, with a mean age of 46.80 ± 8.83 years, and 371 were women, with a mean age of 51.09 ± 9.39 years (P < 0.001). This study was reviewed and approved by the institutional review board of the Second Affiliated Hospital of Zhejiang University School of Medicine (ethical review code: Research 2014–113). All subjects provided written informed consent.
The definition of metabolic syndrome
In our study, metabolic syndrome was defined by the presence of 3 or more of the following conditions, based on the NECP ATP III criteria [21]: 1) waist circumference (WC) ≥ 90 cm in men and ≥ 80 cm in women, 2) triglycerides ≥ 150 mg/dL, 3) HDL cholesterol < 40 mg/dL in men and < 50 mg/dL in women, 4) blood pressure ≥ 130/85 mm Hg or receiving antihypertensive medication, and 5) fasting glucose ≥ 100 mg/dL.
Questionnaire and physical examination
A standardised questionnaire was generated by a physician to collect baseline information such as age, gender, smoking habits and drinking habits. A physical examination was performed by a physician to collect information such as weight, height and waist circumstance. The body mass index was calculated as the weight in kilograms divided by the height in meters squared. Both systolic and diastolic blood pressure were measured in the right following 5 minutes of rest, with the patient in a sitting position, using an automated device (Omron 711, USA), and the mean of two consecutive blood pressure measurements was recorded.
Laboratory tests
All subjects fasted for 12 hours, and their venous blood samples were collected for the measurement of fasting plasma glucose (FPG), blood profiles (total cholesterol: TC, triglyceride: TG, high density lipoprotein–cholesterol: HDL-C, low density lipoprotein- cholesterol: LDL-C, apolipoprotein B: apoB, apolipoprotein AΙ: apoAΙ), homocysteine (HCY), gamma-glutamyl transpeptidase (GGT), uric acid (UA), fasting insulin (FINS), and C-reactive protein (CRP). FPG was measured via the hexokinase (HK) method; TC was measured via the cholesterol oxidase-peroxidase method (CHO-POD); TG was measured via the glycerol phosphate oxidase-peroxidase method; HDL-C was measured via the direct method-surfactant clearance method; LDL-C was measured via the direct method-selected inhibitor method; HCY was measured using an enzymatic cycling assay; GGT was measured via the modified SZASZ method; UA was measured via the urease-peroxidase method; ApoB, apoAΙ, and CRP were each measured using a turbidimetric immunoassay with a BECKMAN COULTER AU5400 Analyzer. FINS was measured via direct chemical luminescence using with a SIEMENS ADVIA CENTAUR XP Analyzer. The homeostasis model assessment of insulin resistance (HOMA-IR) was calculated based on the HOMA model, as follows: HOMA-IR = fasting glucose (mmol/L) * fasting plasma insulin (mU/L)/22.5.
To guarantee both the accuracy and the comparability of the results, two quality control materials (products of BIO-RAD, lot numbers of liquid assayed multiqual: 45641 and 45643, lipids control: 57251 and 57252) of different concentrations were tested each day. The cumulative CVs were as follows: FPG (1.83%; 1.73%), TG (4.0%; 2.56%), TC (2.05%; 1.92%), HDL-C (2.60%; 2.70%), LDL-C (3.03%; 3.01%), apoB (<10%; <10%), apoAΙ (<10%; <10%), GGT (<6%; <4%), HCY (<6%; <6%), UA (<3%; <3%), FINS (<10%; <10%), and CRP (<10%; <10%).
Carotid ultrasound measurement
CIMT measurements were performed by an experienced sonographer, using a high-resolution B-mode tomographic ultra-sound system (GE LOGIQ E9, USA), with a linear 9 MHz transducer. The distal segment and stigma compartments of the cephalic artery and the proximal segment of the internal carotid artery were measured on both sides [22]. The transducer was manipulated so that the luminal diameter was maximised in the longitudinal plane. Each of the above blood vessels was measured in three different sections, within a range of 1 cm in the proximal wall and distant from the sidewalls. Carotid atherosclerosis was diagnosed when CIMT was ≥ 0.9 mm [23,24].
Statistical analysis
All statistical analyses were performed using SPSS 17 software. Data were expressed either as means ± S.D. or as geometrical means (95% confidence intervals [CIs]) for the continuous variables, and as percentages for the categorical variables. TG was analysed after log-transformation due to a skewed distribution. General characteristics were compared separately among participants with and without carotid atherosclerosis, in both men and women with MetS, using the Student’s t-test. The categorical variables were analysed via the Chi-square test. Spearman correlation coefficients were used to study the relationships between the different risk factors and carotid atherosclerosis. The relationships between the different lipid ratios and carotid atherosclerosis were each assessed using binary logistic regression analysis with forward selection method and multinomial logistic regression analysis. Odds ratios (ORs) and 95% confidence intervals (CIs) for carotid atherosclerosis were each calculated. Regarding the multinomial logistic regression analysis, age, body mass index (BMI), systolic blood pressure (SBP), diastolic blood pressure (DBP), TC, TG, HDL-C, LDL-C, apoB, apoAΙ, INS, IR, CRP, HCY, GGT, and UA were included as covariates. To assess the utility of the different lipid ratios as markers of MetS, we constructed sex-specific Receiver Operating Characteristic (ROC) curves and compared the areas under the ROC curves (AUCs) with the Z-statistic. A P value less than 0.05 was considered to be statistically significant.
Results
The relationship between MetS and carotid atherosclerosis
A total of 4908 subjects were included in the analysis. The sample consisted of 3039 men and 1869 women. The age range was 20–84 years in men and 20–83 years in women. Based on the NECP ATP III criteria, 1863 people were diagnosed with MetS, which was present in 49.1% (1492/3039) of men and 19.9% (371/1869) of women. Among Chinese individuals with MetS, 16.6% (309/1863) of the individuals had carotid atherosclerosis, including 16.6% (247/1492) of men and 16.7% (62/371) of women. Among Chinese individuals without MetS, 9.5% (289/3045) of the individuals had carotid atherosclerosis. MetS remained significantly associated with carotid atherosclerosis (OR 1.90, 95% CI 1.58–2.25, P < 0.001). Therefore, MetS is a significant risk factor for carotid atherosclerosis.
The clinical and biochemical characteristics of the participants with and without carotid atherosclerosis among Chinese individuals with MetS
Among Chinese individuals with MetS, the clinical and biochemical characteristics including the metabolic components and the lipid profiles of both men and women with and without carotid atherosclerosis are shown in Table 1. The characteristics are stratified by the presence of carotid atherosclerosis. The mean apoB/apoAΙ ratios were significantly higher among the participants with carotid atherosclerosis (0.91 ± 0.02 in men and 0.85 ± 0.03 in women) compared to participants without carotid atherosclerosis (0.85 ± 0.01 in men and 0.75 ± 0.01 in women) (P < 0.05). Additionally, there were significant differences in the TC, LDL-C, FINS, SBP, DBP, UA and apoB levels between the two groups (P < 0.05). There were also significant differences in the HOMA-IR and FPG levels among men, and the TG and the non-HDL-C/HDL-C ratio levels among women. The men (53.95 ± 0.58 ys) developed carotid atherosclerosis at a younger age than the women (58.47 ± 1.17 ys), among Chinese individuals with MetS (P < 0.001).
Table 1.
Clinical and biochemical characteristics in cluding metabolic components and lipid measures in participant with and without the carotid atherosclerosis in both genders
| Variables | Men | Women | ||||
|---|---|---|---|---|---|---|
| Carotid atherosclerosis (−); n = 1245 | Carotid atherosclerosis (+); n = 247 | P -value | Carotid atherosclerosis (−); n = 309 | Carotid atherosclerosis (+); n = 62 | P -value | |
| Age (ys) | 45.14 ± 0.23 | 53.95 ± 0.58 | <0.001 | 49.61 ± 0.50 | 58.47 ± 1.17 | <0.001 |
| SBP (mm Hg) | 137.83 ± 0.31 | 142.69 ± 1.01 | <0.001 | 137.28 ± 0.61 | 142.52 ± 1.55 | <0.001 |
| DBP (mm Hg) | 80.10 ± 0.27 | 90.16 ± 0.73 | <0.001 | 86.40 ± 0.53 | 88.53 ± 1.39 | <0.001 |
| BMI (kg/m2) | 25.75 ± 0.08 | 25.63 ± 0.17 | 0.544 | 24.26 ± 0.17 | 25.23 ± 0.39 | 0.021 |
| FPG (mmol/L) | 5.70 ± 0.03 | 5.96 ± 0.10 | 0.016 | 5.62 ± 0.06 | 5.65 ± 0.09 | 0.848 |
| FINS (pmol/L) | 70.01 ± 1.10 | 60.49 ± 2.21 | <0.001 | 62.99 ± 1.75 | 72.06 ± 4.63 | 0.041 |
| HOMA-IR | 2.58 ± 0.05 | 2.34 ± 0.11 | 0.034 | 2.28 ± 0.07 | 2.62 ± 0.18 | 0.056 |
| TC (mmol/L) | 5.28 ± 0.03 | 5.46 ± 0.06 | 0.007 | 5.38 ± 0.05 | 5.74 ± 0.12 | 0.005 |
| HDL-C (mmol/L) | 1.36 ± 0.01 | 1.38 ± 0.02 | 0.284 | 1.64 ± 0.02 | 1.53 ± 0.04 | 0.01 |
| non-HDL-C/HDL-C | 2.97 ± 0.02 | 3.06 ± 0.06 | 0.149 | 2.37 ± 0.04 | 2.82 ± 0.08 | <0.001 |
| LDL-C (mmol/L) | 3.44 ± 0.02 | 3.55 ± 0.05 | 0.041 | 3.29 ± 0.04 | 3.65 ± 0.09 | 0.001 |
| TG (mmol/L) | 2.31 ± 0.04 | 2.13 ± 0.08 | 0.054 | 1.72 ± 0.04 | 2.14 ± 0.13 | <0.001 |
| ApoAΙ (g/L) | 1.38 ± 0.01 | 1.40 ± 0.01 | 0.321 | 1.54 ± 0.01 | 1.51 ± 0.02 | 0.26 |
| ApoB (g/L) | 1.17 ± 0.01 | 1.25 ± 0.02 | <0.001 | 1.13 ± 0.02 | 1.27 ± 0.04 | 0.001 |
| ApoB/apoAΙ | 0.85 ± 0.01 | 0.91 ± 0.02 | 0.001 | 0.75 ± 0.01 | 0.85 ± 0.03 | 0.001 |
| CRP (mg/L) | 5.35 ± 0.12 | 5.67 ± 0.48 | 0.363 | 5.34 ± 0.21 | 4.57 ± 0.35 | 0.117 |
| HCY (μmol/L) | 11.16 ± 0.15 | 11.6 ± 0.29 | 0.186 | 8.28 ± 0.18 | 9.76 ± 0.38 | 0.001 |
| GGT (U/L) | 61.54 ± 1.60 | 54.47 ± 3.72 | 0.074 | 23.69 ± 1.13 | 30.95 ± 3.86 | 0.075 |
| UA (μmol/L) | 371.29 ± 2.15 | 360.94 ± 4.51 | 0.048 | 257.46 ± 3.07 | 283.81 ± 7.56 | 0.001 |
| Current smoker(%) | 41.5 | 39.7 | >0.05 | 0.6 | 0 | >0.05 |
SBP: systolic blood pressure; DBP: diastolic blood pressure; BMI: body mass index; FPG: fasting plasma glucose; FINS: fasting insulin; HOMA-IR: homeostasis model assessment of insulin resistance; TC: total cholesterol; HDL-C: high density lipoprotein cholesterol; LDL-C: low density lipoprotein cholesterol; non-HDL-C: non-high density lipoprotein cholesterol; TG: triglycerides; ApoAΙ: apolipoprotein AΙ; ApoB: apolipoprotein B; CRP: C-reactive protein; HCY: Homocysteine; GGT: gamma-glutamyl transpeptidase; UA: uric acid; Carotid atherosclerosis(+): CIMT was ≥ 0.9 mm; Carotid atherosclerosis(−): CIMT was < 0.9 mm.
Relationship between carotid atherosclerosis and blood lipid profile and ratios
Spearman correlations between carotid atherosclerosis and the apoB/apoAΙ ratio and the non-HDL-C/HDL-C ratio are shown in Table 2. Both the apoB/apoAΙ ratio and the non-HDL-C/HDL-C ratio positively correlated with carotid atherosclerosis. The Spearman correlation coefficients between carotid atherosclerosis and the apoB/apoAΙ ratio and the non-HDL-C/HDL-C ratio were higher in women compared to men. Binary logistic regression analysis with forward selection method was used to assess the OR for CIMT, as shown in Table 3. Among men, the apoB/apoAΙ ratio was more prominent than age, SBP, and TG. Among women, the non-HDL-C/HDL-C ratio was more prominent than age.
Table 2.
Spearman correlations between carotid atherosclerosis and risk factors for atherosclerosis in both genders
| Variables | Men | Women | ||
|---|---|---|---|---|
| Correlation coefficient | P -value | Correlation coefficient | P -value | |
| ApoB/apoAΙ | 0.079 | 0.002 | 0.181 | <0.001 |
| Non-HDL-C/HDL-C | 0.067 | 0.01 | 0.2 | <0.001 |
| HDL-C (mmol/L) | 0.017 | 0.508 | −0.151 | 0.004 |
| LDL-C (mmol/L) | 0.052 | 0.044 | 0.181 | <0.001 |
| TC (mmol/L) | 0.07 | 0.007 | 0.141 | 0.006 |
| ApoB (g/L) | 0.103 | <0.001 | 0.162 | 0.002 |
| ApoAΙ (g/L) | 0.018 | 0.485 | −0.06 | 0.25 |
| HOMA-IR | −0.082 | 0.002 | 0.102 | 0.05 |
| CRP (mg/L) | −0.017 | 0.514 | −0.069 | 0.187 |
| Current smoker | −0.014 | 0.59 | −0.033 | 0.527 |
HDL-C: high density lipoprotein cholesterol; non-HDL-C: non-high density lipoprotein cholesterol; LDL-C: low density lipoprotein cholesterol; TC: total cholesterol; ApoB: apolipoprotein B; ApoAΙ: apolipoprotein AΙ; HOMA-IR: homeostasis model assessment of insulin resistance; CRP: C-reactive protein.
Table 3.
Odds ratio and 95% confidence interval of carotid atherosclerosis associated with blood lipid profile or ratio in both genders
| Variables | OR | 95% CI | P -value | |
|---|---|---|---|---|
| men | ||||
| apoB/apoAΙ | 6.142 | 3.219-11.720 | <0.001 | |
| Age (ys) | 1.129 | 1.107-1.151 | <0.001 | |
| SBP (mm Hg) | 1.014 | 1.003-1.026 | 0.015 | |
| TG (mmol/L) | 0.671 | 0.475-0.949 | 0.024 | |
| women | ||||
| non-HDL-C/HDL-C | 2.054 | 1.338-3.153 | 0.001 | |
| Age (ys) | 1.112 | 1.072-1.153 | <0.001 |
ApoB: apolipoprotein B; ApoAΙ: apolipoprotein AΙ; SBP: systolic blood pressure; TG: triglyceride; HDL-C: high density lipoprotein cholesterol; non-HDL-C: non-high density lipoprotein cholesterol.
The risk of carotid atherosclerosis based on the apoB/apoAΙ ratio and the non-HDL-C/HDL-C ratio quartiles in each sex among Chinese individuals with MetS
Following an adjustment for age, BMI, SBP, DBP, TC, TG, HDL-C, LDL-C, apoB, apoAΙ, INS, IR, CRP, HCY, GGT, and UA, the ORs of the two ratios increased significantly in both men and women, as shown in Table 4. As compared with quartile 1 (reference), quartile 2 (OR = 1.205), quartile 3 (OR = 1.541) and quartile 4 (OR = 2.465) of the apoB/apoAΙ ratio in men and quartile 2 (OR = 1.587), quartile 3 (OR = 2.034) and quartile 4 (OR = 2.772) of the apoB/apoAΙ ratio in women were significantly associated with carotid atherosclerosis. Similar relationships were observed for the non-HDL-C/HDL-C ratio, with the same adjusted, ORs for the increasing quartiles of the non-HDL-C/HDL-C ratio of quartile 1 (reference), 1.287, 1.627 and 1.843 in men, and quartile 1 (reference), 1.383, 3.200 and 5.847 in women. The ORs were significantly greater in the highest apoB/apoAΙ ratio quartile compared with the lowest apoB/apoAΙ ratio quartile, as well as the non-HDL-C/HDL-C ratio, in both men and women (P < 0.05). Meanwhile, CIMT increased progressively across the quartiles of the non-HDL-C/HDL-C ratio (P for trend, < 0.05). The increase in ORs was more prominent among women than among men.
Table 4.
The risk of carotid atherosclerosis according to quartiles of apoB/apoAΙ ratio and non-HDL-C/HDL-C ratio in both genders
| Ratio levels * | P for trend | |||||
|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | |||
| Men | ||||||
| range of apoB/apoAΙ | <0.690 | 0.690-0.841 | 0.841-1.000 | >1.000 | ||
| ORs for carotid atherosclerosis | 1 | 1.205(0.768-1.890) | 1.541(1.003-2.336) | 2.465(1.598-3.803) | <0.001 | |
| range of non-HDL-C/HDL-C | <2.390 | 2.390-2.937 | 2.937-3.508 | >3.508 | ||
| ORs for carotid atherosclerosis | 1 | 1.287(0.834–1.987) | 1.627(1.060-2.499) | 1.843(1.189-2.856) | 0.177 | |
| Women | ||||||
| range of apoB/apoAΙ | <0.594 | 0.594-0.764 | 0.764-0.888 | >0.888 | ||
| ORs for carotid atherosclerosis | 1 | 1.587(0.573-4.392) | 2.034(0.758-5.496) | 2.772(1.051-7.315) | <0.001 | |
| range of non-HDL-C/HDL-C | <1.885 | 1.885-2.393 | 2.393-2.955 | >2.955 | ||
| ORs for carotid atherosclerosis | 1 | 1.383(0.424–4.511) | 3.200(1.077-9.511) | 5.847(1.982-17.245) | 0.001 | |
*Covariates for adjustment including age, BMI, SBP, DBP, TC, TG, HDL-C, LDL-C, apoB, apoAΙ, INS, IR, CRP, HCY, GGT, and UA. ApoB: apolipoprotein B; ApoAΙ: apolipoprotein AΙ; HDL-C: high density lipoprotein cholesterol; non-HDL-C: non-high density lipoprotein cholesterol.
The diagnostic values of different lipid ratios in detecting carotid atherosclerosis among Chinese individuals with MetS
To compare the predictive values of the different ratios in predicting carotid atherosclerosis, we analysed the ROC curves of the two ratios (apoB/apoAΙ and non-HDL-C/HDL-C). ROC analysis indicated that the AUC of the apoB/apoAΙ ratio (0.561) was higher than that of the non-HDL-C/HDL-C ratio (0.522) in men (P < 0.05) and the AUC of the apoB/apoAΙ ratio (0.640) was lower than that of the non-HDL-C/HDL-C ratio (0.695) in women (P < 0.05). Graphical comparisons of the ROC curves of these ratios relative to carotid atherosclerosis are presented in Figure 1. Figures A and B depicted the discriminatory value of these two ratios relative to carotid atherosclerosis in men and women, respectively. There was no significant difference between the apoB/apoAΙ ratio and the non-HDL-C/HDL-C ratio regarding the AUC with the Z-statistic (P > 0.05). The AUC of the apoB/apoAΙ ratio was not larger in women than in men (P > 0.05), whereas the AUC of the non-HDL-C/HDL-C ratio was larger in women than men (P < 0.05). The AUCs for the other parameters were as follows: TG (AUC = 0.457 in men, AUC = 0.637 in women), non-HDL-C (AUC = 0.552 in men, AUC = 0.654 in women), HDL-C (AUC = 0.513 in men, AUC = 0.383 in women), TC (AUC = 0.555 in men, AUC = 0.609 in women), LDL-C (AUC = 0.540 in men, AUC = 0.640 in women), IR (AUC = 0.436 in men, AUC = 0.579 in women), CRP (AUC = 0.487 in men, AUC = 0.447 in women), apoB (AUC = 0.580 in men, AUC = 0.626 in women), and apoAΙ (AUC = 0.514 in men, AUC = 0.454 in women).
Figure 1.
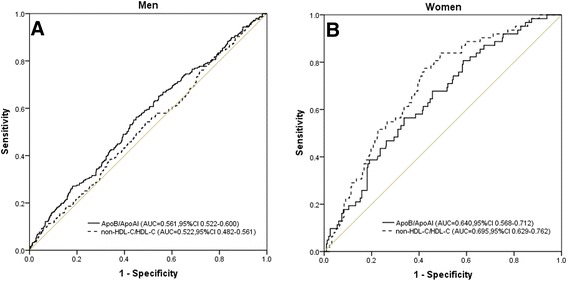
Discriminatory power of apoB/apoAΙ and non-HDL-C/HDL-C for carotid atherosclerosis by Receiver Operating Characteristic (ROC) curves in men (A) and women (B) ApoB: apolipoprotein B; ApoAΙ: xapolipoprotein AΙ; HDL-C: high density lipoprotein cholesterol; non-HDL-C: non-high density lipoprotein cholesterol.
Discussion
Previous studies have shown that patients with MetS are at increased risk of developing vascular diseases, including endothelial dysfunction [3,4,25,26]. The Botnia Study demonstrated that the risk of both coronary heart disease and stroke increased three-fold among subjects with metabolic syndrome [4]. In a retrospective analysis of 5822 men and women, we observed that the risk of carotid atherosclerosis in a Chinese population with MetS was approximately twice that of individuals without MetS (P < 0.001).
In the present study, men were found to be at a higher risk for carotid atherosclerosis compared with women. Among patients with carotid atherosclerosis, men were found to be younger than women, which may be the result of a lower level of apoB, as apoB protects against the development of atherosclerosis, and is a good predictor of CVD [13,27-29]. The anti-atherosclerotic action of oestrogen may also play a role in this process [30]. Based on these results, we believe that men with Mets should be screened for CIMT at a much younger age compared with women.
Several studies have demonstrated that the apoB/apoAΙ ratio and the non-HDL-C/HDL-C ratio may be used to predict the risk of carotid atherosclerosis [12-14]. Chiadi E Ndumele reported that there were no significant differences between the ability of the apoB/apoAΙ ratio and the ability of the non-HDL-C/HDL-C ratio to predict coronary heart disease in the setting of MetS [31]. However, none of these previous studies compared the ratio of apoB/apoAΙ with the ratio of non-HDL-C/HDL-C relative to carotid atherosclerosis among Chinese individuals with MetS. Therefore, in addition to the correlation between these two ratios and carotid atherosclerosis among Chinese individuals with MetS, we compared their discriminatory values relative to carotid atherosclerosis among Chinese individuals with MetS. We noted that the ratios of apoB/apoAΙ and non-HDL-C/HDL-C each positively correlated with carotid atherosclerosis among Chinese individuals with MetS, particularly women. The results of the ROC analysis indicated that there were no significant differences in the abilities of the ratios of apoB/apoAΙ and non-HDL-C/HDL-C to predict carotid atherosclerosis among Chinese individuals with MetS.
The AUC of the non-HDL-C/HDL-C ratio was significantly lower among men than among women, suggesting that women were more sensitive and relatively more susceptible to the burden of this ratio compared with men. This phenomenon was also observed in both white and black individuals [32]. The exact reason for this result must be determined in future studies. This phenomenon may result from changes in the levels of both HDL-C and TG, which have been found to exert stronger effects among women [33].
This study had several limitations. The number of women subjects was small; therefore, the observed effects may not be applicable to the general population. As this was a retrospective study, medication histories (except lipid-lowering agents), histories of previous medical or surgical diseases, durations of diabetes, or possible intolerance to medications may have been additional limiting factors in the extrapolation of the present findings to the general population. Given the cross-sectional nature of our study, the impact of these two ratios and their interaction with MetS components on cardiovascular outcomes could not be ascertained. Hence, we hope to learn the impacts of the comparisons and the diagnostic values of the investigated ratios in detecting cardiovascular events or diabetes in a future study. Despite these limitations, the non-HDL-C/HDL-C ratio and the apoB/apoAΙ ratio may each be useful in predicting cardiovascular events.
Conclusion
Our findings indicate that Chinese men with MetS develop carotid atherosclerosis at a much younger age than women with MetS. There were no significant differences in the ability to predict the risk of carotid atherosclerosis between the apoB/apoAΙ ratio and the non-HDL-C/HDL-C ratio among Chinese individuals with MetS. Among Chinese individuals with MetS, the utility of the non-HDL-C/HDL-C ratio was found to be greater among women than among men.
Sources of funding
This research project was supported by grants from the National Health Key Special Fund (No. 200802112), the Health Department Fund (No. 2007A093 and No. 201343550), the Traditional Chinese Medicine Bureau Fund (No. 2007ZA019), the Natural Science Fund of Zhejiang Province (No. Y2080001 and Y12H160121), the Zhejiang Province Education Department Fund (No. Y201121724), the Key Project of Zhejiang Province (No. 2009C03012-5 and No. 2013C03044-5) and the National Natural Science Foundation of China (general project No.81372302).
Footnotes
Guangming Qin and Jiangfeng Tu contributed equally to this work.
Competing interests
The authors have no conflicts of interest to declare regarding the publication of this manuscript.
Authors’ contribution
WP and GQ designed the study; CZ, XT, LL and JW participated in acquisition of data; LL, WL, LT, SS and UD researched and evaluated the literature; GQ and JT undertook the statistical analysis and wrote the first draft of the manuscript. All authors read and approved the final manuscript.
Contributor Information
Guangming Qin, Email: zejykqgm@163.com.
Jiangfeng Tu, Email: 826139284@zju.edu.cn.
Chenjing Zhang, Email: zhangcj2000@shou.com.
Xiaoxiao Tang, Email: tangxx2000@163.com.
Laisheng Luo, Email: luolaishengzju@163.com.
Jiaqi Wu, Email: wujiaqi_12@126.com.
Lingang Liu, Email: 1181860793@qq.com.
Wen Lu, Email: 875026510@qq.com.
Lisha Tao, Email: tao_lisha@126.com.
Shengrong Shen, Email: shrshen@zju.edu.cn.
Undurti N Das, Email: undurti@hotmail.com.
Wensheng Pan, Email: wspan223@163.com.
References
- 1.Syvanne M, Taskinen MR. Lipids and lipoproteins as coronary risk factors in non-insulin-dependent diabetes mellitus. Lancet. 1997;350:Si20–Si23. doi: 10.1016/S0140-6736(97)90024-6. [DOI] [PubMed] [Google Scholar]
- 2.Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome - an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112:2735–2752. doi: 10.1161/CIRCULATIONAHA.105.169404. [DOI] [PubMed] [Google Scholar]
- 3.Sengul C, Cevik C, Ozveren O, Oduncu V, Sunbul A, Akgun T, et al. Echocardiographic epicardial fat thickness is associated with carotid intima-media thickness in patients with metabolic syndrome. Echocardiography. 2011;28:853–858. doi: 10.1111/j.1540-8175.2011.01471.x. [DOI] [PubMed] [Google Scholar]
- 4.Isomaa B, Almgren P, Tuomi T, Forsen B, Lahti K, Nissen M, et al. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care. 2001;24:683–689. doi: 10.2337/diacare.24.4.683. [DOI] [PubMed] [Google Scholar]
- 5.Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults - findings from the Third National Health and Nutrition Examination Survey. JAMA. 2002;287:356–359. doi: 10.1001/jama.287.3.356. [DOI] [PubMed] [Google Scholar]
- 6.Rong D, Jianfei M, Changqing Y, Changyan W, Hongyuan L. morbidity of metaboiism syndrome in middle and aged crowd. Med J west China. 2010;1:130–132. [Google Scholar]
- 7.Lorenz MW, Markus HS, Bots ML, Rosvall M, Sitzer M. Prediction of clinical cardiovascular events with carotid intima-media thickness - a systematic review and meta-analysis. Circulation. 2007;115:459–467. doi: 10.1161/CIRCULATIONAHA.106.628875. [DOI] [PubMed] [Google Scholar]
- 8.Chambless LE, Heiss G, Folsom AR, Rosamond W, Szklo M, Sharrett AR, et al. Association of coronary heart disease incidence with carotid arterial wall thickness and major risk factors: The Atherosclerosis Risk in Communities (ARIC) study, 1987–1993. Am J Epidemiol. 1997;146:483–494. doi: 10.1093/oxfordjournals.aje.a009302. [DOI] [PubMed] [Google Scholar]
- 9.O’Leary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL. carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. N Engl J Med. 1999;340:14–22. doi: 10.1056/NEJM199901073400103. [DOI] [PubMed] [Google Scholar]
- 10.Polak JF, Pencina MJ, Pencina KM, O’Donnell CJ, Wolf PA, D’Agostino RB. Carotid-wall intima-media thickness and cardiovascular events. N Engl J Med. 2011;365:213–221. doi: 10.1056/NEJMoa1012592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bots ML, Baldassarre D, Simon A, de Groot E, O’Leary DH, Riley W, et al. Carotid intima-media thickness and coronary atherosclerosis: weak or strong relations? Eur Heart J. 2007;28:398–406. doi: 10.1093/eurheartj/ehl482. [DOI] [PubMed] [Google Scholar]
- 12.Dahlen EM, Lanne T, Engvall J, Lindstrom T, Grodzinsky E, Nystrom FH, et al. Carotid intima-media thickness and apolipoprotein b/apolipoprotein a-i ratio in middle-aged patients with type 2 diabetes. Diabet Med. 2009;26:384–390. doi: 10.1111/j.1464-5491.2009.02693.x. [DOI] [PubMed] [Google Scholar]
- 13.Huang F, Yang Z, Xu BH, Bi YF, Xu M, Xu Y, et al. Both serum apolipoprotein B and the Apolipoprotein B/Apolipoprotein A-I ratio are associated with carotid intima-media thickness. Plos One. 2013;8:e54628. doi: 10.1371/journal.pone.0054628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhao WW, Gong W, Wu N, Li YT, Ye KP, Lu B, et al. Association of lipid profiles and the ratios with arterial stiffness in middle-aged and elderly Chinese. Lipids Health Dis. 2014;13:37. doi: 10.1186/1476-511X-13-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Scuteri A, Najjar SS, Muller DC, Andres R, Hougaku H, Metter EJ, et al. metabolic syndrome amplifies the age-associated increases in vascular thickness and stiffness. J Am Coll Cardiol. 2004;43:1388–1395. doi: 10.1016/j.jacc.2003.10.061. [DOI] [PubMed] [Google Scholar]
- 16.McNeill AM, Rosamond WD, Girman CJ, Heiss G, Golden SH, Duncan BB, et al. Prevalence of coronary heart disease and carotid arterial thickening in. patients with the metabolic syndrome (The ARIC Study) Am J Cardiol. 2004;94:1249–1254. doi: 10.1016/j.amjcard.2004.07.107. [DOI] [PubMed] [Google Scholar]
- 17.Sipila K, Moilanen L, Nieminen T, Reunanen A, Jula A, Salomaa V, et al. Metabolic syndrome and carotid intima media thickness in the health 2000 survey. Atherosclerosis. 2009;204:276–281. doi: 10.1016/j.atherosclerosis.2008.08.029. [DOI] [PubMed] [Google Scholar]
- 18.Tabatabaei-Malazy O, Fakhrzadeh H, Sharifi F, Mirarefin M, Badamchizadeh Z, Larijani B. Gender differences in association between metabolic syndrome and carotid intima media thickness. J Diabetes Metab Disord. 2012;11:13. doi: 10.1186/2251-6581-11-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kweon SS, Shin MH, Lee YH, Choi JS, Nam HS, Park KS, et al. Higher normal ranges of urine albumin-to-creatinine ratio are independently associated with carotid intima-media thickness. Cardiovasc Diabetol. 2012;11:112. doi: 10.1186/1475-2840-11-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alcohol-attributable deaths and years of potential life lost–United States, 2001. MMWR Morb Mortal Wkly Rep 53: 866–870 [PubMed]
- 21.Cleeman JI, Grundy SM, Becker D, Clark LT, Cooper RS, Denke MA, et al. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) JAMA. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 22.Johnsen SH, Mathiesen EB, Joakimsen O, Stensland E, Wilsgaard T, Lochen ML, et al. Carotid atherosclerosis is a stronger predictor of myocardial infarction in women than in men: A 6-year follow-up study of 6226 persons: The Tromso study. Stroke. 2007;38:2873–2880. doi: 10.1161/STROKEAHA.107.487264. [DOI] [PubMed] [Google Scholar]
- 23.Writing Group of 2010 Chinese Guidelines for the Management of Hypertension 2010 Chinese guidelines for the management of hypertension. Chin J Cardiol. 2011;39:579–614. [PubMed] [Google Scholar]
- 24.Ying Y, Qiang Y, Lirong L, Miao W, Wuxiang X, Jiangyi X, et al. Ultrasonic Testing of the Intima Media Thickness (IMT) in the carotid artery-repetitive comments. Ultrasonic Imag Mag. 2010;19:120–123. [Google Scholar]
- 25.Kaess BM, Jozwiak J, Mastej M, Lukas W, Grzeszczak W, Windak A, et al. Association between anthropometric obesity measures and coronary artery disease: a cross-sectional survey of 16 657 subjects from 444 polish cities. Heart. 2010;96:131–135. doi: 10.1136/hrt.2009.171520. [DOI] [PubMed] [Google Scholar]
- 26.Wassink AMJ, Van Der Graaf Y, Soedamah-Muthu SS, Spiering W, Visseren FLJ, Grp SS. Metabolic syndrome and incidence of type 2 diabetes in patients with manifest vascular disease. Diab Vasc Dis Res. 2008;5:114–122. doi: 10.3132/dvdr.2008.019. [DOI] [PubMed] [Google Scholar]
- 27.Walldius G, Jungner I. The apoB/apoA-I ratio: a strong, new risk factor for cardiovascular disease and a target for lipid-lowering therapy - a review of the evidence. J Intern Med. 2006;259:493–519. doi: 10.1111/j.1365-2796.2006.01643.x. [DOI] [PubMed] [Google Scholar]
- 28.Olofsson SO, Wiklund O, Boren J. Apolipoproteins A-I and B: Biosynthesis, role in the development of atherosclerosis and targets for intervention against cardiovascular disease. Vasc Health Risk Manag. 2007;3:491–502. [PMC free article] [PubMed] [Google Scholar]
- 29.Meisinger C, Loewel H, Mraz W, Koenig W. Prognostic value of Apolipoprotein B and A-I in the prediction of myocardial infarction in middle-aged men and women: results from the MONICA/KORA Augsburg cohort study. Eur Heart J. 2005;26:271–278. doi: 10.1093/eurheartj/ehi003. [DOI] [PubMed] [Google Scholar]
- 30.Barton M. Postmenopausal oestrogen replacement therapy and atherosclerosis: can current compounds provide cardiovascular protection? Expert Opin Investig Drugs. 2001;10:789–809. doi: 10.1517/13543784.10.5.789. [DOI] [PubMed] [Google Scholar]
- 31.Ndumele CE, Matsushita K, Astor B, Virani SS, Mora S, Williams EK, et al. Apolipoproteins do not add prognostic information beyond lipoprotein cholesterol measures among individuals with obesity and insulin resistance syndromes: The ARIC study. Eur J Prev Cardiol. 2014;21:866–875. doi: 10.1177/2047487312465523. [DOI] [PubMed] [Google Scholar]
- 32.Paul TK, Chen W, Srinivasan SR, Toprak A, He J, Berenson GS. Gender divergence on the impact of multiple cardiovascular risk factors on the femoral artery intima-media thickness in asymptomatic young adults: The Bogalusa heart study. Am J Med Sci. 2012;343:40–45. doi: 10.1097/MAJ.0b013e31821da9c0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shaw LJ, Merz CNB, Pepine CJ, Reis SE, Bittner V, Kelsey SF, et al. Insights from the NHLBI-sponsored women’s ischemia syndrome evaluation (WISE) Study part I: gender differences in traditional and novel risk factors, symptom evaluation, and gender-optimized diagnostic strategies. J Am Coll Cardiol. 2006;47:4S–20S. doi: 10.1016/j.jacc.2005.01.072. [DOI] [PubMed] [Google Scholar]


