Abstract
Proopiomelanocortin (POMC)-derived peptides like α-melanocyte-stimulating hormone (MSH) substantially improve hepatic insulin sensitivity and regulate energy expenditure. Melanocortinergic agents are also powerful inducers of sexual arousal that are being investigated for a possible therapeutic role in erectile dysfunction. It is currently unclear whether reduced melanocortin (MC) activity may contribute to the sexual dysfunction accompanying obesity and type 2 diabetes. Male rodents with leptin and insulin resistance targeted to POMC neurons (leptin receptor [LepR]/insulin receptor [IR]POMC mice) exhibit obesity, hyperinsulinemia, hyperglycemia, and systemic insulin resistance. In this study, we demonstrate that LepR/IRPOMC males are also subfertile due to dramatic alterations in sexual behavior. Remarkably, these reproductive changes are accompanied by decreased α-MSH production not present when a single receptor type is deleted. Unexpectedly, behavioral sensitivity to α-MSH and MC receptor expression are also reduced in LepR/IRPOMC males, a potential adaptation of the MC system to altered α-MSH production. Together, these results suggest that concurrent insulin and leptin resistance in POMC neurons in individuals with obesity or type 2 diabetes can reduce endogenous α-MSH levels and impair sexual function.
Sexual health is an important, but frequently neglected, aspect of diabetes care (1). Sexual dysfunction (SD) among this population may include disorders of libido, ejaculatory problems, erectile dysfunction (ED), decreased sexual desire, and reduced intercourse satisfaction (2, 3). Similarly, obesity or prediabetes increases rates of infertility and ED by 30%–46% (4, 5). The impact of these symptoms can be profound, resulting in psychological distress, altered self-perception, dysfunctional family dynamics, and reduced quality of life (6–9). Although phosphodiesterase inhibitors like Viagra have advanced ED management, these drugs have limited efficacy in diabetic patients (10), and other treatment approaches are needed.
Endogenous melanocortins (MCs) like α-melanocyte-stimulating hormone (MSH) are derived from posttranslational modification of the proopiomelanocortin (POMC) polypeptide precursor (11, 12). These peptides activate MC3 and MC4 receptors in the brain. A substantial body of research in humans supports the use of MC receptor agonists for SD. Injections of melanotan II (MTII), a peptide analog of α-MSH, have been found to cause intermittent penile erections along with stretching and yawning for 1–5 hours in normal men (13, 14). In men with ED, 80%–90% report erections and over half note increased libido after receiving MTII (15, 16). Other MC4 receptor agonists work as well as Viagra in men with ED (17) and increase penile erections in diabetic men and others who fail to respond to Viagra (18, 19). These studies show that activating MC pathways can reverse SD in men. However, it is unclear whether this approach targets a causal mechanism for SD; specifically, it is not known whether obesity or type 2 diabetes (T2D) is accompanied by reduced activity in MC pathways that influence sexual function.
Activation of POMC neurons, located in the arcuate nucleus of the hypothalamus, is well known to promote caloric expenditure and glucose management appropriate for the postprandial state (20). We have previously shown that these effects require input by insulin and the adipokine leptin (21, 22). Evidence suggests that obesity and T2D is accompanied by neuronal insulin and leptin resistance (23–26), likely leading to decreased α-MSH release (12, 27, 28). We therefore hypothesized that MC deficiency accompanying obesity and T2D leads to or exacerbates SD. To test this hypothesis preclinically, we have examined the sexual function of obese, hyperglycemic male mice with POMC neurons that are insensitive to both leptin and insulin (leptin receptor [LepR]/insulin receptor [IR]POMC mice).
Materials and Methods
Animals and genotyping
Mice that carry loxp-flanked genes for the IR (30) and LepR (31) were crossed with mice carrying a POMC promoter-driven Cre recombinase to create the LepR/IRPOMC (double knockout) mice. All of the mice used in these experiments were males maintained on a C57Bl6 background. Each experimental group was compared with littermate controls carrying the floxed alleles but without altered gene expression (LepR/IRFloxed mice) and, when informative, to mice with a single LepR deletion (LepRPOMC mice) or single IR deletion (IRPOMC mice). Mice were housed in the University of Toledo College of Medicine animal facility at 22°C–24°C on a 12-hour light, 12-hour dark cycle and were fed standard rodent chow (2016 Teklad Global 16% Protein Rodent Diet, 12% fat by calories; Harlan Laboratories). Mice were weaned on postnatal day 21. Blood samples were obtained via submandibular bleed. Animals were killed by CO2 asphyxiation or by cardiac puncture under 2% isoflurane anesthesia to draw blood and collect tissues. All procedures were reviewed and approved by University of Toledo College of Medicine Animal Care and Use Committee. The genotyping was carried out by Transnetyx, Inc using a real-time PCR-based approach. Any mouse showing floxed gene deletion in tail tissue was excluded from the studies.
Metabolic phenotype assessment
Body composition in 4-month-old males was assessed by nuclear magnetic resonance (minispec mq7.5; BrukerOptics) to determine the percentage of fat mass, as described previously (see reference 42 below). After a 6-hour fast on α-Dri bedding, tail blood glucose was measured using a mouse-specific glucometer (AlphaTRAK; Abbott Laboratories). Serum collected from the tail blood was also used to analyze basal insulin levels using an UltraSensitive insulin ELISA (Crystal Chem, Inc). Homeostatic model assessment (HOMA) was calculated using the resulting serum insulin and glucose measurements in order to quantify insulin resistance and β-cell function (insulin [mU/L] × glucose [mmol/L]/22.5).
Puberty and reproductive phenotype assessment
At 3 weeks of age, LepR/IRPOMC and LepR/IRFloxed control male mice were paired with a 5-week-old C57Bl/6 female. Over the next 13 weeks, age of sexual maturation, pairings producing offspring, litter size, and latency between litters were analyzed. At 16 weeks of age, mounting behavior of LepR/IRPOMC, LepRPOMC, IRPOMC, and floxed control males was assessed under red lighting 2 hours after the beginning of the dark phase. Specifically, a female in proestrus (determined by vaginal cytology) was introduced to the male's home cage, and the number and timing of attempts to mount were recorded for a 20-minute period. If 10 minutes passed without the male mounting the female, the first female was replaced with a second stimulus female for the remaining 10 minutes. To decrease variation in the data, only 1 observer was used in the analysis of mounting behavior.
Aggression tests using a resident-intruder paradigm
Singly housed LepR/IRPOMC and littermate control males were tested in their home cage (as a resident) against an olfactory bulbectomized male intruder mouse (The Jackson Laboratory) for 15 minutes. For each experimental male, cumulative durations of chasing and aggressive bouts were scored. An aggressive bout was defined as a continuous series of behavioral interactions, including at least 1 aggressive behavioral act. Boxing, lateral thrust, and biting, previously shown to be typical for intermale (male vs male) aggression (32–34), were defined as aggressive behavior acts. Three seconds was the maximum amount of time that could elapse between aggressive behavioral acts to be considered part of the same aggressive bout; if intervals between the occurrences of 2 behavioral aggressive acts exceeded 3 seconds, the 2 behavioral acts were scored as 2 separate aggressive bouts.
Hormone assays
Submandibular blood was collected at 9–11 am in 17- to 18-week-old males to detect basal LH and testosterone levels. T was measured via RIA performed by the Endocrine Technology Support Core Lab at the Oregon National Primate Research Center (Beaverton, OR). LH was measured via RIA performed by the University of Virginia Center for Research in Reproduction Ligand Assay and Analysis Core (Charlottesville, VA). The assay for LH and testosterone had a sensitivity of 0.2 and 0.1 ng/mL, respectively. The intraassay variation (n = 3) was less than 6%. Serum 17β-estradiol levels were measured in 16- to 18-week-old males via in house ELISA (Calbiotech Mouse/Rat Estradiol (E2) ELISA kit ES180S-100), which has an analytical sensitivity level of 3 pg/mL.
GnRH stimulation and assessment of testosterone negative feedback in male LepR/IRPOMC mice
A GnRH stimulation test was performed to analyze pituitary function. Blood was collected from mice via submandibular bleed before sc injections of 100-ng/kg GnRH (L7134; Sigma-Aldrich). Ten minutes after injection, blood was collected again from the other cheek. Fold change in serum LH was assessed (35).
To evaluate testosterone sensitivity of negative feedback, serum LH levels were evaluated after gonadectomy (GDX) with and without testosterone (T1500; Sigma-Aldrich) administration. On the day of surgery (d 0), 16-week-old males were anesthetized by ketamine and xylazine between 9 and 11 am to undergo GDX. Serum LH levels were determined from submandibular blood samples from intact wildtype (WT) and LepR/IRPOMC males collected at 9–11 am (basal group; WT [n = 5]; and LepR/IRPOMC [n = 7]). On day 6 after GDX, blood samples were collected, and all subjects (GDX untreated, WT [n = 5]; GDX untreated, LepR/IRPOMC [n = 7]) were sc implanted with a 1- to 2-cm SILASTIC tube (Dow Corning Corp) filled with 10-μg crystalline testosterone (T1500; Sigma) and sealed with Silicone Type A Medical Adhesive (Dow Corning Corp). To measure the resulting LH levels, blood samples were collected again on day 13 after GDX at 9–11 am.
Intracerebroventricular (icv) injection of α-MSH and behavioral testing
LepR/IRPOMC, LepR/IRFloxed, LepRPOMC, and IRPOMC males were stereotaxically implanted with a single guide cannula (2.3 mm length, 33 internal gauge; Plastics One) positioned 1.0 mm above the lateral ventricle (coordinates: 0.22 mm posterior to bregma, 1.13 mm lateral to midline, and 1.95 mm below the surface of the skull) and fixed to the skull using dental cement. Animals were allowed 4–8 days for recovery from surgery. Intracerebroventricular injections were performed in conscious mice as previously described (36–38); each mouse received 0.3 μg of α-MSH (M4135; Sigma-Aldrich) in a volume of 1 μL or an equal volume of saline. Behavioral studies were performed following the methods previously described by Bertolini et al (39). Each stretch, yawn, and incidence of grooming was scored continuously every 15 seconds for 2 hours starting 10 minutes after treatment. To facilitate comparison, grooming data are reported as the percentage of the total number of 15-second-grooming scores possible.
Quantitative real-time PCR
After blood collection via cardiac puncture under 2% isoflurane anesthesia, brains and other tissues were removed. Total RNA was extracted from whole hypothalamic tissues by an RNeasy Lipid Tissue Mini kit (QIAGEN), and single-strand cDNA was synthesized by a High-Capacity cDNA Reverse Transcription kit (Applied Biosystems) using random hexamers as primers. A 10μM cDNA template was used in a 10-μL system in 384-well plates with iTaq Universal SYBR Green SMX 500 (Bio-Rad 1725121). Primers for amplification of gene transcripts are listed in Table 1. Each sample was analyzed in triplicate to measure gene expression levels. The reactions were run in a CFX384 Touch from Bio-Rad (Bio-Rad Laboratories), analyzed using the comparative (threshold cycle) Ct method (2−ΔΔCt), and normalized to 18S ribosomal RNA as an endogenous control.
Table 1.
Real-Time Primer Sequences for Genes of Interest
| Gene | Forward primer | Reverse primer |
|---|---|---|
| 18S ribosomal RNA (18S) | TTGACGGAAGGGCACCACAG | GCACCACCACCCACGGAATCG |
| Gonadotropin-releasing hormone 1 (GnRH1) | AGCACTGGTCCTATGGGTTG | GGGGTTCTGCCATTTGATCCA |
| Opioid receptor, μ1 (Oprm1) | TCCGACTCATGTTGAAAAACCC | CCTTCCCCGGATTCCTGTCT |
| Melanocortin 3 receptor (Mc3R) | TCCGATGCTGCCTAACCTCT | GGATGTTTTCCATCAGACTGACG |
| Melanocortin 4 receptor (Mc4R) | CCCGGACGGAGGATGCTAT | TCGCCACGATCACTAGAATGT |
| Proopiomelanocortin (POMC) | GTTACGGTGGCTTCATGACCTC | CGCGTTCTTGATGATGGCGTTC |
| Carboxypeptidase E (CPE) | GTCCTAACAATCACCTGCTGAA | AGTACCGCTCCGTGTCTCAT |
| Proprotein convertase subtilisin/Kexin type 1 (Pcsk1) | AGTTGGAGGCATAAGAATGCTG | GCCTTCTGGGCTAGTCTGC |
| Proprotein convertase subtilisin/Kexin type 2 (Pcsk2) | AGAGAGACCCCAGGATAAAGATG | CTTGCCCAGTGTTGAACAGGT |
Real-time PCR primer sequences.
Western blotting
For protein and peptide analysis, mice were transcardially exsanguinated and decapitated. Brains were removed immediately, and the whole hypothalamus, excluding the preoptic and mammillary regions, was removed en bloc by sharp dissection from a ventral approach. The boundaries of the block were: rostral, just posterior to the optic chiasm; lateral, the choroidal fissures; and caudal, the rostral pole of the mammillary bodies. The tissue was removed by a horizontal cut 2 mm from the ventral surface of the brain.
Tissues were snap frozen in liquid nitrogen and stored in −80°C until homogenized and processed using an All Prep DNA/RNA/Protein Mini kit (QIAGEN). Protein pellets were subsequently resuspended in Cell Lytic MT Cell Lysis Reagent (Sigma-Aldrich) supplemented with protease inhibitor and phosphatase inhibitor cocktails (Thermo Scientific). Protein concentrations were determined by BSA protein assay (Thermo Scientific). A total of 30 μg of denatured samples was subjected to SDS-PAGE electrophoresis and Western blotting using a rabbit anti-melanocortin 4 receptor (MC4R) (1:500; Abcam) or goat anti-melanocortin 3 receptor (MC3R) (1:200; Santa Cruz Biotechnology, Inc) primary antibodies. Mouse anti-β-actin (1:10 000; Sigma-Aldrich) or mouse antihistone 3 (1:1000; Cell Signaling) was used as a loading control. Images were developed within the Odyssey-1935 System (Li-Cor, Biosciences) using donkey antirabbit FL800 or donkey antigoat FL800 and goat antimouse FL680 fluorescent secondary antibodies (Li-Cor, Biosciences). ImageJ software was used for band intensity quantification.
POMC peptide and convertase protein assessment
Mice were decapitated after isoflurane anesthesia, and hypothalami were removed. Hypothalamic tissue blocks were placed in 2N acetic acid with 5-μL/mL protease inhibitor cocktail (P8340; Sigma-Aldrich) and were homogenized using an Omni TH Tissue Homogenizer on ice and then boiled for 10 minutes. Acid extracted peptides were freeze-dried and then resuspended in RIA buffer. Samples were subjected to specific RIA analyses for ACTH, β-endorphin (EP) and α-MSH as developed in the Nillni laboratory (28, 41) using both commercially available peptides and primary antibodies developed in house. ACTH, β-EP, and desacetyl-α-MSH were iodinated with 125I using the chloramine T oxidation-reduction method followed by HPLC separation, and the purified peptides were used as tracers. The ACTH and β-EP RIA assays were performed in 0.5 mL of RIA buffer (phosphate buffer [pH 7.4] with 500-mg/L sodium azide and 2.5-g/L BSA), containing anti-ACTH antiserum (1:30 000) or anti-β-EP (1:40 000) and 5000 cpm of 125I-ACTH or 125I-β-EP tracer. The sensitivity of the assays was approximately 10 pg/tube, and the intra- and interassay variability was approximately 5%–7% and approximately 10%–11%, respectively. The α-MSH RIA assay was performed in 0.5-mL RIA buffer, with primary anti-α-MSH antiserum (1:20 000), and 5000 cpm of 125I-desacetyl-α-MSH tracer. The sensitivity of the assay was approximately 11.5 pg/tube, and the intra- and interassay variability was approximately 10%–11%. The ACTH assay detects 100% of corticotropin-like intermediate peptide (CLIP) and ACTH forms; however, this assay does not cross-react with any form of α-MSH or β-EP. The ACTH assay cross-reacts with the POMC precursor, although the amount of cross-reactivity is unknown. The α-MSH antibody used in this condition can detect 100% of desacetyl α-MSH but does not cross-react with the free acid nonamidated form of α-MSH, ACTH, or corticotropin-like intermediate peptide. The β-EP antiserum does not cross-react with either ACTH or α-MSH assays.
Statistical analysis
Data are presented as mean ± SEM. Two-tailed unpaired t testing was used to compare 2 groups. The Mann-Whitney U test was used if the data did not assume a normal distribution. Two-way ANOVA was performed when needed to compare 4 groups, followed by the Holm-Sidak multiple comparison test. A value of P < .05 was considered to be significant. The primary outcomes of the behavioral experiments were considered to be continuous variables and analyzed with a t test or two-way ANOVA depending on the number of groups or experimental conditions compared.
For POMC peptide and convertase protein assessment, results are presented as mean ± SEM. A two-tailed t test was used to analyze differences between 2 groups. An ANOVA, followed by Tukey's honestly significant difference post hoc test, was used to analyze differences between more than 2 groups. A Shapiro-Wilk W goodness-of-fit test was used to test for normal distributions, and Levene's test (2-group comparisons) or Bartlett's test (comparisons between more than 2 groups) was used to test for homogenous variances in all variables. For variables with nonnormal distributions and unequal variances, a nonparametric Mann-Whitney U test or Kruskal-Wallis test was used. A Welch's correction was used for comparisons with unequal variances but normal distribution of the data. Differences were considered to be significant at P < .05. (GraphPad Software, Inc). Statistics for each comparison are presented in figure legends; *, P < .05; **, P < .01; ***, P < .001; and ****, P < .0001.
Results
Evaluation of metabolic phenotype
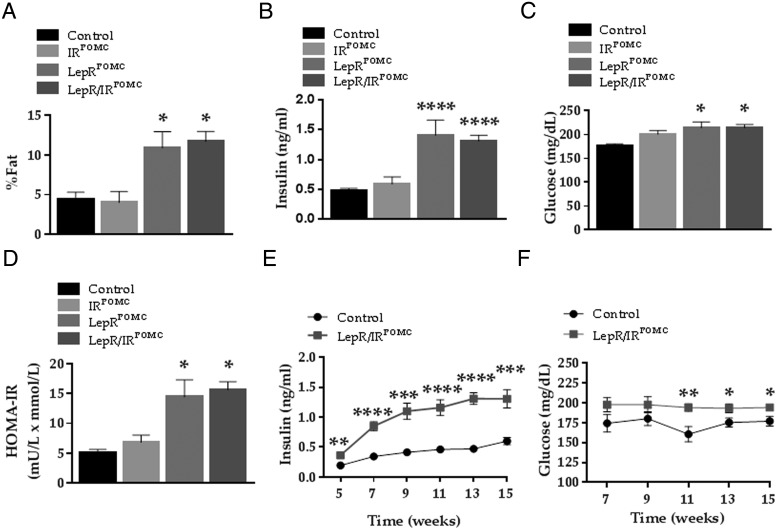
Mice lacking leptin signaling in POMC neurons (LepRPOMC mice) are mildly obese (31). We have previously reported that the addition of POMC neuronal insulin insensitivity modified both the adiposity and peripheral insulin sensitivity of mice lacking LepRs on POMC neurons from a mixed strain background (21). Therefore, we evaluated the metabolic status of the LepR/IRPOMC, LepRPOMC, IRPOMC, and littermate control males on a pure C57Bl6 background. LepR/IRPOMC and LepRPOMC males were found to have a significantly higher body fat percentage in comparison with the age matched littermate controls (Figure 1A). At 13 weeks of age, both LepR/IRPOMC and LepRPOMC males showed increased insulin and glucose levels (Figure 1, B and C). The HOMA score of the LepR/IRPOMC and LepRPOMC males was significantly higher than the controls at 13 weeks of age (Figure 1D), suggesting the presence of systemic insulin resistance (42).
Figure 1. Effects on metabolic homeostasis.
A, Body composition (fat percentage) was measured by NMR in 16-week-old LepR/IRPOMC, LepRPOMC, IRPOMC, and littermate controls (n = 12/6/11/14). B and C, In the same males, we also measured blood insulin and glucose levels after a 6-hour fast. D, HOMA was used to assess insulin resistance and β-cell function. E and F, These LepR/IRPOMC, LepRPOMC, IRPOMC, and littermate controls were also subjected to biweekly tail blood draw to measure serum insulin and glucose levels after a 6-hour fast. Insulin was measured by UltraSensitive insulin ELISA (Crystal Chem, Inc) Data were analyzed using a one-way ANOVA followed by Holm-Sidak for multiple comparisons (A–D) or a two-tailed Student's t test at each time point (E and F).
In order to determine at what age LepR/IRPOMC males developed insulin resistance, we followed their glucose and insulin levels after puberty on a weekly basis. Hyperinsulinemia was shown in the LepR/IRPOMC males as early as 5 weeks of age. Hyperglycemia became apparent by 11 weeks of age, although it showed no evidence of age-related worsening (Figure 1, E and F). Given the similarity of the metabolic phenotype of LepR/IRPOMC and LepRPOMC males, these results suggest that leptin sensing by POMC neurons has a more dominant role than insulin sensing in the control of energy and glucose homeostasis on this strain background.
Evaluation of fertility and the hypothalamic-pituitary-gonadal axis
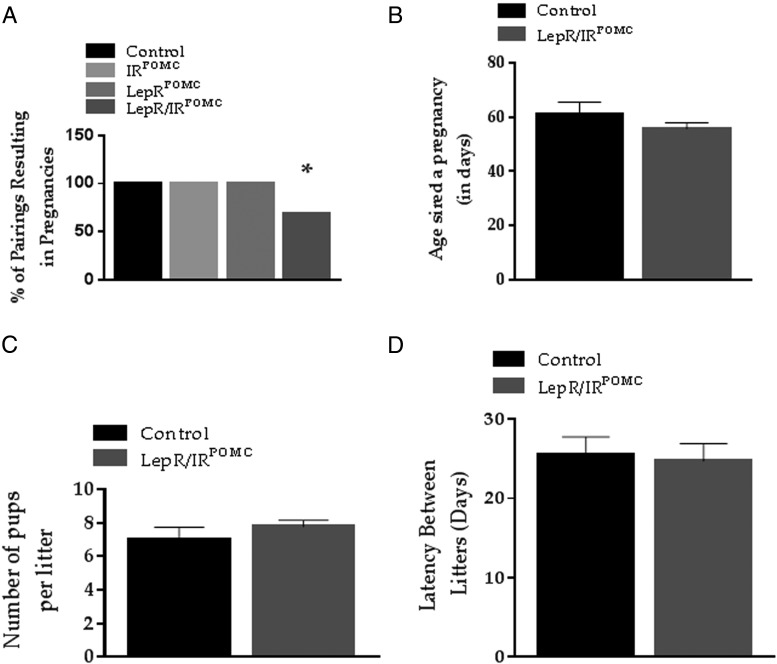
We examined the fertility of LepR/IRPOMC males by housing them with 5-week-old C57Bl6 female mice. Each LepR/IRPOMC or LepR/IRFloxed control male (n = 15 and n = 18, respectively) was individually housed with a female from 3 to 16 weeks of age. Under these conditions, we observed a significant difference in the number of pairings that produced offspring (Figure 2A). However, we saw no significant change in the age of sexual maturation, litter size, or latency between litters of fertile LepR/IRPOMC males when compared with littermate controls (Figure 2, B–D).
Figure 2. Effects on pubertal development and reproduction.
At the age of 21 days, LepR/IRPOMC and littermate controls (n = 12 and n = 13, respectively) males were paired with a 5-week-old C57Bl6 female for 13 weeks. A, The percentage of successful parings for each male was also determined. Data were analyzed using χ2. B, The age of sexual maturation was estimated from the birth of the first litter minus average pregnancy duration for mice (20 d). C and D, Litter size and latency between litters from calculated from successful pairings. Data were analyzed using a two-tailed Student's t test.
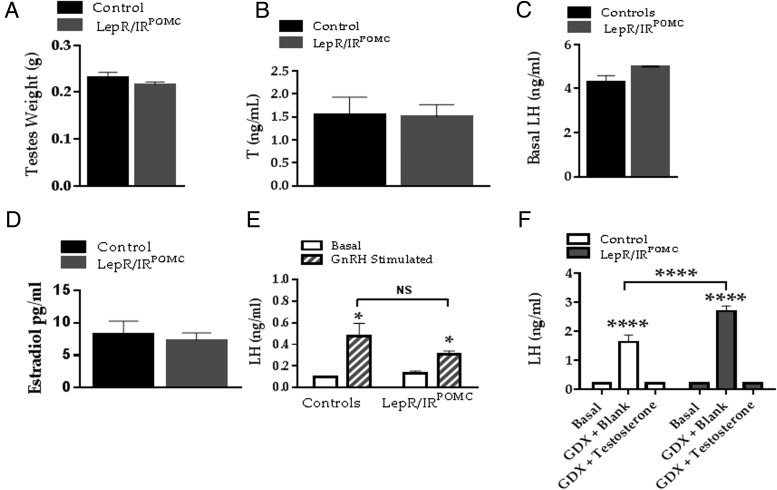
To determine whether impaired GnRH release led to reduced fertility, we examined the function of the hypothalamic-pituitary-gonadal (HPG) axis in both groups. There was no significant difference in testis weight, serum testosterone, or serum LH in the LepR/IRPOMC males vs the floxed controls (Figure 3, A–C). Hypothalamic GnRH gene expression also did not differ between the groups (t = 2.090; n = 9, 12; mean ± SEM = 0.9967, 1.348 ± 0.17). Testosterone levels did not differ between fertile and infertile LepR/IRPOMC males (fertile: 1.27 ± 0.52 ng/mL and infertile: 1.37 ± 0.38 ng/mL, n = 5, 8, P = .88). One proposed mechanism of obesity-related male infertility is excess production of estrogens by adipose tissue; however, 17β-estradiol levels were not altered in LepR/IRPOMC males (Figure 3D).
Figure 3. Negative feedback analysis.
A, Testis weight was measure at 16 weeks of age in LepR/IRPOMC and littermate controls (n = 11 and n = 15, respectively). B and C, Serum testosterone and LH was measured in the second group of 17- to 18-week-old LepR/IRPOMC and littermate controls (n = 11 and n = 13) by ELISA and RIA, respectively. D, Serum estradiol levels were measured by ELISA in the second group of 17- to 18-week-old LepR/IRPOMC and littermate controls (n = 11 and n = 13, respectively). E, Exogenous GnRH was administered to analyze pituitary function in a third group of LepR/IRPOMC and littermate controls (n = 8) at 16 weeks of age. F, Gonadectomy and steroid replacement were used to analyze the efficacy of steroidal negative feedback. Data were analyzed using a two-way ANOVA followed by Holm-Sidak for multiple comparison or a two-tailed Student's two-tailed t test where necessary.
A GnRH stimulation test was employed to examine the responsiveness of the pituitary to exogenous GnRH. There was no significant difference in the resulting LH release from the pituitary (Figure 3E). Given that opioids such as the POMC-derived peptide β-EP have been implicated in androgen negative feedback of GnRH/LH release (43–45), we specifically tested negative feedback response of testosterone in LepR/IRPOMC males vs their floxed controls. A week after removing the suppressive influence of endogenous testosterone, both groups displayed a significant increase in LH production. However, this increase was significantly greater in LepR/IRPOMC males in comparison with their control littermates (Figure 3F), suggesting stronger neuroendocrine negative feedback in these mice and/or increased underlying GnRH circuit activity. Nevertheless, LepR/IRPOMC mice showed no difference in expression of the Oprm1 gene for the μ-opioid receptor (t = 1.676; n = 8, 8; mean ± SEM = 1.002, 1.034 ± 0.13). Testosterone replacement after gonadectomy significantly repressed levels of LH to intact levels in both groups (Figure 3F).
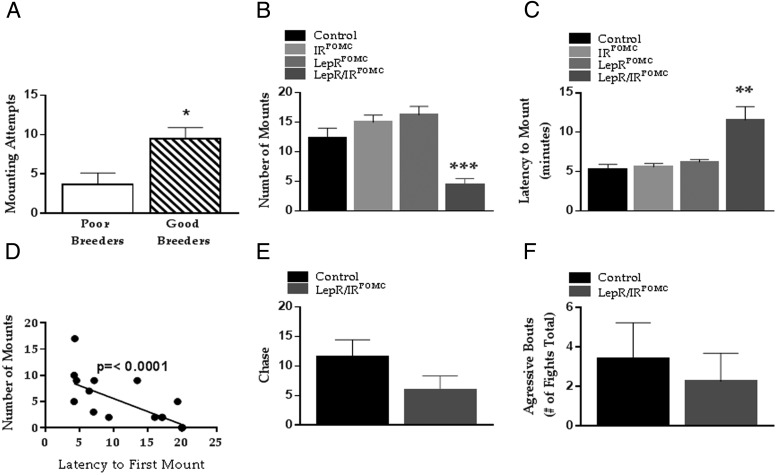
Assessment of copulatory behavior
Given that we found no evidence of hypothalamic hypogonadism that would contribute to a reduction in fertility in LepR/IRPOMC mice, we examined their mounting behavior. For all mice, males that were good breeders (who produced 3–4 litters) during the 3-month reproductive testing period had a significantly increased number of mounting attempts when placed with a novel female compared with poor breeders (who produced 0–1 litter) (Figure 4A). We found a significant reduction in the number of times LepR/IRPOMC males attempted to mount receptive females, and a significant increase in the time required for these males to exhibit mounting behavior (Figure 4, B and C). Furthermore, these 2 traits were highly correlated (Figure 4D). Therefore, the main cause of reduced fertility in LepR/IRPOMC males appears to be impaired sexual behavior.
Figure 4. Effects on sexual behavior.
The LepR/IRPOMC, IRPOMC, LepRPOMC, and control males (n = 13/4/4/18 mice, respectively, from the first experimental group) were observed at 16 weeks of age under red lighting at the beginning of the dark phase over a 10-minute period after the introduction of the female in proestrus to the male's home cage. A, All mice that sired 3 or 4 litters during the reproductive study were compared with those that sired 0 or 1 litter. Mounting behavior was quantified as (A and B) number of mounting attempts and (C) minutes until mounting was attempted. D, Latency to first mount negatively correlated with attempts to mount. E and F, Resident-intruder paradigm test was used to analyze aggressive behavior in the fourth group of LepR/IRPOMC and control males (n = 6 and n = 5, respectively). The number of chase attempts and overall aggressive bouts were scored. Data were analyzed using a two-tailed Student's t test.
We next sought to evaluate whether these deficits were specific to sexual behavior or whether they resulted from impaired perception of pheromone cues, impaired social behavior in general, or some form of movement disorder not apparent during observation. To accomplish this goal, we evaluated another form of social behavior, namely aggression towards a male intruder. To minimize the aggressiveness of mice introduced to the LepR/IRPOMC and control male resident cages, we used olfactory bulbectomized males as intruders (18, 19). We found no significant difference between LepR/IRPOMC and littermate controls (n = 6 and n = 5, respectively) in the number of times they chased the intruder male or initiated aggressive bouts (Figure 4, D and E). Thus, LepR/IRPOMC males are motivated to engage in nonsexual social behaviors and perform them normally.
Insulin and leptin regulation of POMC transcription and processing
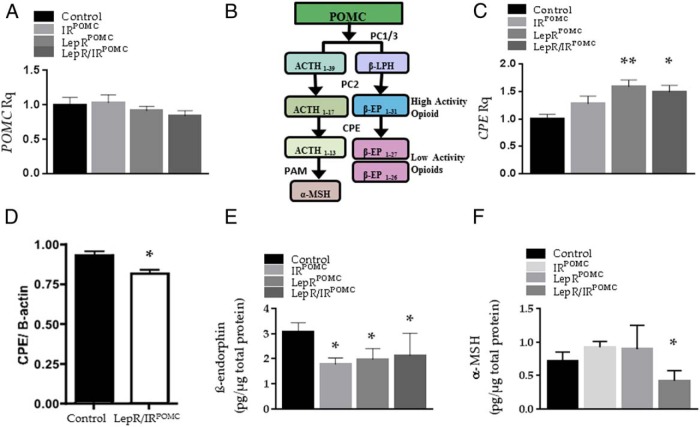
To unravel the mechanism underlying the specific deficits in sexual activity, we first examined POMC gene expression by real-time quantitative PCR in 16-week-old LepR/IRPOMC, LepRPOMC, IRPOMC, and littermate controls. Given our previous findings in LepR/IRPOMC mice on a mixed strain background (21, 22), we were surprised to see no significant reduction in POMC expression (Figure 5A). Notably, impaired leptin signaling in POMC neurons is often (28, 31), but not always (46, 47), associated with reduced POMC transcription.
Figure 5. Effects on POMC transcription and peptide processing.
A and C, Hypothalamic POMC and CPE gene expression was measured by real-time PCR in the second group of LepR/IRPOMC, LepRPOMC, IRPOMC, and littermate controls (n = 8/9/9/11, respectively) at 16 weeks of age. B, Simplified illustration of POMC processing. LPH, lipotropin. D, Western blotting quantification of CPE protein synthesis. E and F, β-EP and α-MSH levels measured by RIA in the third group of LepR/IRPOMC, LepRPOMC, IRPOMC, and littermate controls (n = 5–8) at 16 weeks of age. Data were analyzed using a one-way ANOVA followed by Holm-Sidak for multiple comparison or a two-tailed Student's t test (D).
We therefore examined the effect of the insulin and LepR gene deletion on POMC processing enzymes (Figure 5B). In the hypothalamus, POMC is cleaved to form pro-ACTH and β-lipotropin. Pro-ACTH is cleaved by prohormone convertase (PC)1/3 to form ACTH1–39, which is then cleaved by PC2 to form ACTH1–17. Carboxypeptidase E (CPE) then removes the C-terminal basic residues to produce ACTH1–13, whose C terminus is then amidated by peptidyl α-amidating monooxygenase (PAM) to create ACTH(1–3)NH2, also known as desacetyl α-MSH. PC2 also cleaves β-lipotropin to form the endogenous opioid β-EP1–31. The C terminus of β-EP1–31 can be cleaved by PC2 or CPE to form β-EP1–27 and β-EP1–26, which have markedly reduced opioid activity (48).
Gene expression of proprotein convertase subtilisin/kexin type 1 (t = 0.6168; n = 9, 10; mean ± SEM = 0.8833, 0.9611 ± 0.13) and proprotein convertase subtilisin/kexin type 2 (t = 0.6456; n = 9, 8; mean ± SEM= −0.1778 ± 0.23) (PCSK1 and 2) were unchanged, whereas CPE gene expression was significantly increased in the LepRPOMC and LepR/IRPOMC males (Figure 5C). Nevertheless, hypothalamic protein synthesis of CPE was significantly decreased in the LepR/IRFloxed males (Figure 5D), suggesting that insulin and leptin sensing by POMC cells regulates hypothalamic CPE maturation. We saw no alteration in hypothalamic PC1 (n = 4,4; P = .0161; Student's t test) or PC2 protein levels (n = 4, 4; P = .0746; Student's t test). Using HPLC and RIA, we found that the production of total β-EP was significantly decreased in mice lacking leptin, insulin, or both receptors in POMC neurons (Figure 5E). However, only in LepR/IRPOMC males did we see a significant decrease in the production of α-MSH (Figure 5F), suggesting that the deficits of sexual behavior in this model are attributable to a reduction in α-MSH release.
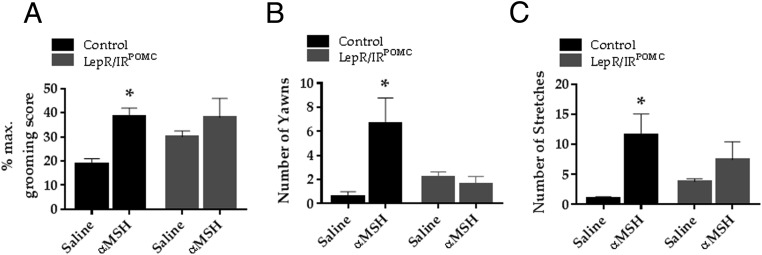
α-MSH-induced reproductive behavior assessment
α-MSH induces a variety of behavioral responses when injected icv. The best known of these responses is the so-called stretching-yawning syndrome, which involves penile erection and ejaculation, yawning and grooming, and sociosexual behaviors (49). Given the overall decrease in α-MSH production in the LepR/IRPOMC males, we postulated that POMC neurons in LepR/IRPOMC males release less α-MSH, thereby leading to a reduction in sexual behavior. To confirm that the reproductive deficits in LepR/IRPOMC males were dependent on presynaptic alterations in neuropeptide release, we characterized their behavioral responsiveness to centrally administered α-MSH. Erectile responses proved difficult to measure visually in either group, and grooming responses suppressed sociosexual behaviors in control animals at the concentration tested. Grooming, stretching, and yawning were increased in the untreated LepR/IRPOMC males compared with untreated controls. In contrast, none of these behaviors significantly increased in response to α-MSH administration in LepR/IRPOMC males (Figure 6, A–C).
Figure 6. Testing of α-MSH behavioral responses.
The behavioral syndrome induced by the icv injection of α-MSH peptide (grooming, stretching, and yawning) was visually scored for 2 hours and analyzed in the second group of LepR/IRPOMC and control males (n = 10 and n = 8, respectively). A, Percent grooming score in mice for 1 hour beginning 10 minutes after icv injection of 0.3 μg of α-MSH or saline. Data were transformed into the percentages of the total number of 15-second-grooming or genital grooming scores possible. B and C, Total number of yawns and stretches scored for 2 hours after icv injection of α-MSH or saline. Data were analyzed using a two-way ANOVA followed by Holm-Sidak for multiple comparison.
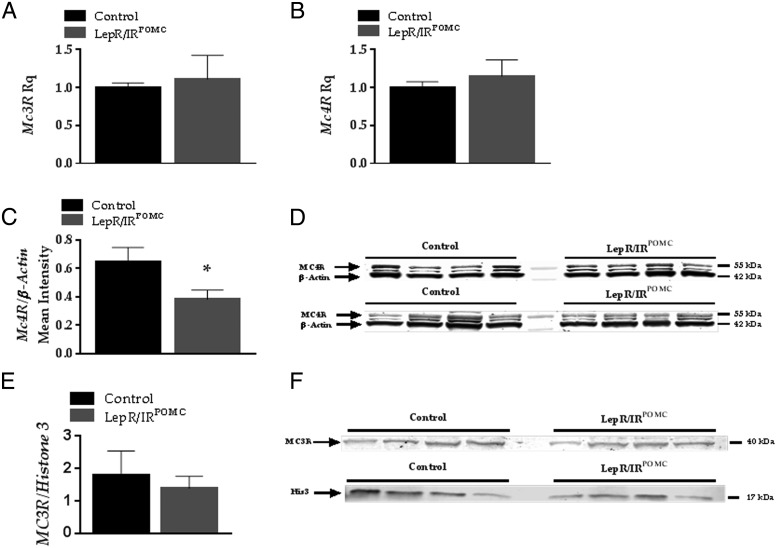
These results suggested additional alterations to neuronal circuits downstream from POMC neurons as a result of POMC insulin and LepR ablation. To understand the origin of the loss of responsiveness of LepR/IRPOMC males to icv α-MSH, we used real-time quantitative PCR to examine the expression of hypothalamic MC3 and MC4 receptors. We found no changes in MC3R or MC4R hypothalamic mRNA expression in the LepR/IRPOMC males (Figure 7, A and B). In contrast, the hypothalamic MC4R protein levels were significantly decreased in the LepR/IRPOMC males (Figure 7, C and D), whereas hypothalamic MC3R protein levels were unchanged (Figure 7, E and F).
Figure 7. Evaluation of MC receptor activity.
A and B, Each sample was analyzed in triplicate to measure MC3R and MC4R mRNA expression. The reactions were run in a CFX384 Touch from Bio-Rad (Bio-Rad Laboratories) and analyzed using the comparative Ct method (2−ΔΔCt) with 18S ribosomal RNA as the normalizer. C and D, Western blot analysis of LepR/IRPOMC and littermate controls (n = 4 and n = 4, respectively) hypothalamic MC4R protein expression. A total of 30 μg of protein was loaded into each well, and histone 3 was used as a loading control. E and F, Western blot analysis of LepR/IRPOMC and littermate controls (n = 8) hypothalamic MC3R protein expression. A total of 30 μg of protein was loaded into each well, and β-actin was used as a loading control. Band intensity was measured and analyzed using ImageJ. Data were analyzed using a two-tailed Student's t test.
Discussion
Using assays for both protein and gene expression, we have demonstrated that insulin and LepR gene deletion has a profound effect on POMC-derived peptide production. Specifically, β-EP production is suppressed by leptin insensitivity and is similarly suppressed with insulin insensitivity. We did not observe an additive effect when both receptors were deleted simultaneously. Given that leptin-sensitive and insulin-sensitive POMC neurons are largely nonoverlapping populations (50), insulin and leptin appear to serve similar and equally powerful roles promoting β-EP production in POMC populations containing one of these receptor types. In contrast, single insulin or LepR deletion from POMC neurons had no effect on α-MSH levels. Rather, only deletion of both receptor types significantly suppressed α-MSH protein levels.
Our findings strongly suggest that reduced α-MSH production can lead to SD. The MC system has previously been shown to influence sexual behavior and penile erection in rodents (38, 51). For example, blocking the central actions of α-MSH with an MC4R antagonist delays sexual behavior in male rats (52). Furthermore, the absence of MC4Rs leads to diminished copulatory behavior (mounting and intromission latency) in mice, whereas an MC4R agonist improves sexual function, motivation, and performance (53). Our results suggest that loss of insulin and leptin sensing by POMC neurons leads to an overall decrease in α-MSH production and thus sexual motivation and/or performance.
In addition to these effects on POMC product production, it is possible that the connections formed by POMC neurons during pre and postnatal development are altered in these mice. Leptin is a powerful neurotrophic agent (54–58). For instance, leptin treatment increases the density and length of axons from the arcuate nucleus (ARC) from isolated explants in vitro (59). In leptin-deficient mice, the density of ARC axons innervating the paraventricular nucleus (PVH) is roughly 10% of that in wild-type animals (59). Leptin treatment reverses this deficit only in the neonatal period (59) but still changes ARC synaptic organization in adulthood (60). LepR ablation also disrupts ARC neural projections, including from POMC neurons (56, 61). In addition, insulin has important neurotrophic roles. Pups with hyperinsulinemia show altered density of α-MSH-immunoreactive fibers innervating the PVH and an overall decrease in the number of POMC neurons (58, 62, 63). The decrease in projections to the posterior preautonomic compartment of the PVH, but not the anterior neuroendocrine PVH, is due to direct insulin action, because it is not seen in pups lacking IRs on POMC neurons (64). Significant differences in POMC axonal formation were not seen in the absence of hyperinsulinemia, suggesting that IR signaling is not essential for POMC axonal organization under normal developmental conditions (64). Nevertheless, although we have not investigated the projections of the POMC neurons in these mice, it is reasonable to assume that altered connectivity may also underlie some of their phenotype.
Our finding that responsiveness to α-MSH administration is suppressed in LepR/IRPOMC males suggests that chronic reduction in α-MSH production as a result of insulin and leptin insensitivity in POMC neurons reduces hypothalamic MC4R protein synthesis. It is currently unclear how rapidly this down-regulation occurs. The important role of MC4Rs in the development of hypothalamic circuitry (29, 40, 65, 66) also raises the possibility that developmental changes contribute to the sexual phenotype of LepR/IRPOMC mice.
Although we did not find hypogonadism in these mice, we did see significantly higher LH production after gonadectomy. Taking our findings of reduced β-EP production into account, these findings may reflect reduced tonic suppression of GnRH neuron activity as a result of POMC insulin and leptin insensitivity. In contrast, intact and testosterone-replaced LepR/IRPOMC males showed LH levels similar to controls, a finding that can be interpreted as a stronger negative feedback response to testosterone. Because the ultimate output by the pituitary is normal, we cannot attribute the impaired fertility of LepR/IRPOMC males to endocrine defects.
We found hypothalamic CPE protein content was significantly reduced in LepR/IRPOMC males (despite higher gene expression). These findings suggest that leptin and insulin signaling can alter the maturation of CPE, possibly by reducing CPE translation efficiency or enhancing clearance of unfolded CPE. To our knowledge, such a mechanism has not yet been investigated in models of insulin and leptin resistance. Reduced CPE levels may contribute to the observed reduction in α-MSH in LepR/IRPOMC males. Because the desacetyl α-MSH antibody used in these studies does not cross-react with the free acid nonamidated form of α-MSH, it cannot distinguish between ACTH1–17 and ACTH1–13 processed by CPE before its amidation by PAM. Therefore, although a reduction in α-MSH could be due to reduced CPE levels, it is possible that a change in the levels of PAM may also contribute. We are not able to account for the reduction of total β-EP levels. Our β-EP antiserum cannot distinguish between β-EP1–31 and β-EP1–17 or β-EP1–26. However, mice with mutant CPE have decreased C-terminal processing of β-EP1–31 to β-EP1–27 and β-EP1–26 (67). It is possible that our mice have a larger percentage of active β-EP1–31 that is masked by the overall reduction in β-EP levels.
Interestingly, male CPEfat/fat mice also exhibit low fertility due primarily to abnormal sexual behavior, specifically failure to mount and show intromission or ejaculation behaviors (68). These obese and hyperproinsulinemic mice (69) contain a single Ser202 to Pro202 substitution that renders CPE catalytically inactive and subject to rapid degradation in the endoplasmic reticulum (68–70). Interestingly, these mice also show decreased α-MSH levels (67). Overall, POMC is poorly processed and secreted in an unregulated manner (ie, constitutively) in CPE-deficient mice (71–74). Although the nonspecific loss of CPE function disrupts the processing of multiple peptides in these mice (75), it is possible that low α-MSH levels in the CPEfat/fat model causes deficits in male sexual behavior.
It is unknown whether insulin and leptin resistance can impair sexual function in humans through a similar reduction in α-MSH release. Obese individuals are usually leptin resistant (76–78). In addition, obese and T2D patients exhibit signs of hypothalamic inflammation and mitochondrial dysfunction associated with cellular insulin resistance (26, 79). Therefore, leptin and insulin resistance in POMC neurons may well develop in obese or diabetic individuals. The hypothalamus is believed to play a role in the motivational and autonomic/neuroendocrine aspects of human sexual arousal (80). Indeed, the level of perceived sexual arousal correlates with the magnitude of hypothalamic activity (81, 82). Similarly, positron emission tomography (PET) and functional magnetic resonance imaging (fMRI) studies have found that hypothalamic activity correlates with the level of penile tumescence in response to visual stimuli (83–85). To date, however, studies have not examined whether hypothalamic activity in response to visual sexual stimuli are reduced in leptin and insulin resistant men.
The precise neural pathways downstream of POMC neurons that mediate the effects of MCs on sexual motivation and performance have yet to be elucidated in humans. The PVH has been repeatedly implicated in the control of erection in animals (86, 87) and shows high levels of MC4Rs (88–90). For instance, electrical stimulation of the PVH induces penile erection in awake or anesthetized male rats (91). Microinjections of ACTH or α-MSH in the PVH reproduce the stretching, yawning, and penile erection syndrome (86). Administration of MTII in the PVH also induces erection in anesthetized rats (92). In humans, smelling an estrogen-like substance activated the hypothalamus of heterosexual men with clusters centered in the PVH (93). The medial preoptic area (mPOA), another location with MC4R-positive neurons (88–90), has been frequently implicated in sexual motivation (94–96). As an example, α-MSH facilitates sexual behavior when injected in picomole amounts into the mPOA of sexually experienced male rats (97). In male monkeys, the rate of discharge of neurons in the mPOA increases when viewing a receptive female and when performing button presses resulting in bringing the female closer (98). In freely moving monkeys, mounting responses were obtained by electrical stimulation of the mPOA (99). Finally, in human functional magnetic resonance imaging (fMRI) studies, the anterior location of clusters activated by visual sexual stimuli is compatible with an activation in the mPOA (80). Additional hypothalamic nuclei, such as the lateral hypothalamus and dorsomedial nucleus, have also been implicated in sexual function (93, 99). Given the role of the MC system in regulating energy balance, glucose homeostasis, blood pressure, and other critical functions, it will be essential to disentangle the downstream pathway controlling sexual function to permit precise therapeutic targeting in cases of SD (100, 101). Likewise, sexual side effects of obesity or blood pressure medications targeting this system must be avoided. Studies are currently underway to identify which α-MSH-responsive hypothalamic or extrahypothalamic targets are functionally impaired in states of leptin and insulin resistance, leading to SD.
In sum, we have identified 2 male mouse models on a C57bl6 background, the first (LepRPOMC mice) with isolated metabolic function associated with normal α-MSH levels and the second (LepR/IRPOMC mice) with both metabolic dysfunction and impaired copulatory behavior, associated with low α-MSH levels. Thus, insulin resistance and obesity does not drive impaired fertility in these male mice; rather, they may share related mechanisms. Specifically, endogenous α-MSH production and responsiveness to α-MSH have a profound effect on the ability of male mice to mate. It remains to be determined whether this copulatory defect is primarily behavioral in nature, or whether it results from ED. These results have important implications for the etiology of SD in men with obesity and type 2 diabetes in whom hypothalamic resistance to leptin and insulin may reduce endogenous α-MSH production.
Acknowledgments
We thank Dr Joel Elmquist for enabling the original production of this mouse line. We also thank Dr Raymond Bourey, Dr Nikolai Modyanov, Laura Nedorezov, Dr Sara DiVall, Benjamin Bryant, and Lance Stechschulte for their technical assistance with these studies.
This work was supported by National Institute of Diabetes and Digestive and Kidney Diseases/National Institutes of Health Grants R01 DK085916–04 and R01 DK085916–03S1 (to E.A.N.) and National Institute of Child Health and Development/National Institutes of Health Grants R00 HD056491 and R21 HD071529 and a deArce-Koch Fund award (J.W.H.). The University of Virginia Center for Research in Reproduction Ligand Assay and Analysis Core and The Endocrine Technology Support Core Lab at the Oregon National Primate Research Center were supported by the Eunice Kennedy Shriver NICHD/NIH Specialized Cooperative Centers Program in Reproduction (SCCPIR) Grant U54-HD28934.
Disclosure Summary: The authors have nothing to disclose.
Footnotes
- CPE
- carboxypeptidase E
- Ct
- threshold cycle
- ED
- erectile dysfunction
- EP
- endorphin
- GDX
- gonadectomy
- HOMA
- homeostatic model assessment
- icv
- intracerebroventricular
- IR
- insulin receptor
- LepR
- leptin receptor
- MC
- melanocortin
- MC3R
- melanocortin 3 receptor
- MC4R
- melanocortin 4 receptor
- mPOA
- medial preoptic area
- MSH
- melanocyte-stimulating hormone
- MTII
- melanotan II
- PAM
- peptidyl α-amidating monooxygenase
- PC
- prohormone convertase
- POMC
- proopiomelanocortin
- PVH
- paraventricular nucleus
- SD
- sexual dysfunction
- T2D
- type 2 diabetes
- WT
- wildtype.
References
- 1. Grant PS, Lipscomb D. How often do we ask about erectile dysfunction in the diabetes review clinic? Development of a neuropathy screening tool. Acta Diabetol. 2009;46:285–290. [DOI] [PubMed] [Google Scholar]
- 2. Owiredu WK, Amidu N, Alidu H, Sarpong C, Gyasi-Sarpong CK. Determinants of sexual dysfunction among clinically diagnosed diabetic patients. Reprod Biol Endocrinol. 2011;9:70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A. The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49:822–830. [DOI] [PubMed] [Google Scholar]
- 4. Nguyen RH, Wilcox AJ, Skjaerven R, Baird DD. Men's body mass index and infertility. Hum Reprod. 2007;22:2488–2493. [DOI] [PubMed] [Google Scholar]
- 5. Grover SA, Lowensteyn I, Kaouache M, et al. The prevalence of erectile dysfunction in the primary care setting: importance of risk factors for diabetes and vascular disease. Arch Intern Med. 2006;166:213–219. [DOI] [PubMed] [Google Scholar]
- 6. Penson DF, Latini DM, Lubeck DP, Wallace KL, Henning JM, Lue TF. Do impotent men with diabetes have more severe erectile dysfunction and worse quality of life than the general population of impotent patients? Results from the Exploratory Comprehensive Evaluation of Erectile Dysfunction (ExCEED) database. Diabetes Care. 2003;26:1093–1099. [DOI] [PubMed] [Google Scholar]
- 7. De Berardis G, Franciosi M, Belfiglio M, et al. Erectile dysfunction and quality of life in type 2 diabetic patients: a serious problem too often overlooked. Diabetes Care. 2002;25:284–291. [DOI] [PubMed] [Google Scholar]
- 8. NIH. NIH Consensus Conference. Impotence. NIH consensus development panel on impotence. JAMA. 1993;270:83–90. [PubMed] [Google Scholar]
- 9. Melman A, Gingell JC. The epidemiology and pathophysiology of erectile dysfunction. J Urol. 1999;161:5–11. [PubMed] [Google Scholar]
- 10. Costabile RA. Optimizing treatment for diabetes mellitus induced erectile dysfunction. J Urology. 2003;170:S35–S38. [DOI] [PubMed] [Google Scholar]
- 11. Nillni EA. Regulation of prohormone convertases in hypothalamic neurons: implications for prothyrotropin-releasing hormone and proopiomelanocortin. Endocrinology. 2007;148:4191–4200. [DOI] [PubMed] [Google Scholar]
- 12. Wardlaw SL. Hypothalamic proopiomelanocortin processing and the regulation of energy balance. Eur J Pharmacol. 2011;660:213–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hadley ME. Discovery that a melanocortin regulates sexual functions in male and female humans. Peptides. 2005;26:1687–1689. [DOI] [PubMed] [Google Scholar]
- 14. Dorr RT, Lines R, Levine N, et al. Evaluation of melanotan-II, a superpotent cyclic melanotropic peptide in a pilot phase-I clinical study. Life Sci. 1996;58:1777–1784. [DOI] [PubMed] [Google Scholar]
- 15. Wessells H, Fuciarelli K, Hansen J, et al. Synthetic melanotropic peptide initiates erections in men with psychogenic erectile dysfunction: double-blind, placebo controlled crossover study. J Urology. 1998;160:389–393. [PubMed] [Google Scholar]
- 16. Wessells H, Gralnek D, Dorr R, Hruby VJ, Hadley ME, Levine N. Effect of an α-melanocyte stimulating hormone analog on penile erection and sexual desire in men with organic erectile dysfunction. Urology. 2000;56:641–646. [DOI] [PubMed] [Google Scholar]
- 17. Lansdell MI, Hepworth D, Calabrese A, et al. Discovery of a selective small-molecule melanocortin-4 receptor agonist with efficacy in a pilot study of sexual dysfunction in humans. J Med Chem. 2010;53:3183–3197. [DOI] [PubMed] [Google Scholar]
- 18. Rosen RC, Diamond LE, Earle DC, Shadiack AM, Molinoff PB. Evaluation of the safety, pharmacokinetics and pharmacodynamic effects of subcutaneously administered PT-141, a melanocortin receptor agonist, in healthy male subjects and in patients with an inadequate response to Viagra. Int J Impot Res. 2004;16:135–142. [DOI] [PubMed] [Google Scholar]
- 19. Safarinejad MR, Hosseini SY. Salvage of sildenafil failures with bremelanotide: a randomized, double-blind, placebo controlled study. J Urology. 2008;179:1066–1071. [DOI] [PubMed] [Google Scholar]
- 20. Sohn JW, Elmquist JK, Williams KW. Neuronal circuits that regulate feeding behavior and metabolism. Trends Neurosci. 2013;36:504–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hill JW, Elias CF, Fukuda M, et al. Direct insulin and leptin action on pro-opiomelanocortin neurons is required for normal glucose homeostasis and fertility. Cell Metab. 2010;11:286–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Berglund ED, Vianna CR, Donato J, Jr, et al. Direct leptin action on POMC neurons regulates glucose homeostasis and hepatic insulin sensitivity in mice. J Clin Invest. 2012;122:1000–1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. De Souza CT, Araujo EP, Bordin S, et al. Consumption of a fat-rich diet activates a proinflammatory response and induces insulin resistance in the hypothalamus. Endocrinology. 2005;146:4192–4199. [DOI] [PubMed] [Google Scholar]
- 24. Thaler JP, Schwartz MW. Minireview: inflammation and obesity pathogenesis: the hypothalamus heats up. Endocrinology. 2010;151:4109–4115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Posey KA, Clegg DJ, Printz RL, et al. Hypothalamic proinflammatory lipid accumulation, inflammation, and insulin resistance in rats fed a high-fat diet. Am J Physiol-Endoc M. 2009;296:E1003–E1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Thaler JP, Yi CX, Schur EA, et al. Obesity is associated with hypothalamic injury in rodents and humans. J Clin Invest. 2012;122:778–778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Münzberg H, Huo L, Nillni EA, Hollenberg AN, Bjørbaek C. Role of signal transducer and activator of transcription 3 in regulation of hypothalamic proopiomelanocortin gene expression by leptin. Endocrinology. 2003;144:2121–2131. [DOI] [PubMed] [Google Scholar]
- 28. Cakir I, Cyr NE, Perello M, et al. Obesity induces hypothalamic endoplasmic reticulum stress and impairs proopiomelanocortin (POMC) post-translational processing. J Biol Chem. 2013;288:17675–17688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Melnick I, Pronchuk N, Cowley MA, Grove KL, Colmers WF. Developmental switch in neuropeptide Y and melanocortin effects in the paraventricular nucleus of the hypothalamus. Neuron. 2007;56:1103–1115. [DOI] [PubMed] [Google Scholar]
- 30. Könner AC, Janoschek R, Plum L, et al. Insulin action in AgRP-expressing neurons is required for suppression of hepatic glucose production. Cell Metab. 2007;5:438–449. [DOI] [PubMed] [Google Scholar]
- 31. Balthasar N, Coppari R, McMinn J, et al. Leptin receptor signaling in POMC neurons is required for normal body weight homeostasis. Neuron. 2004;42:983–991. [DOI] [PubMed] [Google Scholar]
- 32. Ogawa S, Washburn TF, Taylor J, Lubahn DB, Korach KS, Pfaff DW. Modifications of testosterone-dependent behaviors by estrogen receptor-α gene disruption in male mice. Endocrinology. 1998;139:5058–5069. [DOI] [PubMed] [Google Scholar]
- 33. Ogawa S, Robbins A, Kumar N, Pfaff DW, Sundaram K, Bardin CW. Effects of testosterone and 7 α-methyl-19-nortestosterone (MENT) on sexual and aggressive behaviors in two inbred strains of male mice. Horm Behav. 1996;30:74–84. [DOI] [PubMed] [Google Scholar]
- 34. Ogawa S, Lubahn DB, Korach KS, Pfaff DW. Aggressive behaviors of transgenic estrogen-receptor knockout male mice. Ann NY Acad Sci. 1996;794:384–385. [DOI] [PubMed] [Google Scholar]
- 35. Brothers KJ, Wu S, DiVall SA, et al. Rescue of obesity-induced infertility in female mice due to a pituitary-specific knockout of the insulin receptor. Cell Metab. 2010;12:295–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Wikberg JE, Muceniece R, Mandrika I, et al. New aspects on the melanocortins and their receptors. Pharmacol Res. 2000;42:393–420. [DOI] [PubMed] [Google Scholar]
- 37. Melis MR, Argiolas A, Gessa GL. Oxytocin-induced penile erection and yawning: site of action in the brain. Brain Res. 1986;398:259–265. [DOI] [PubMed] [Google Scholar]
- 38. Fan W, Boston BA, Kesterson RA, Hruby VJ, Cone RD. Role of melanocortinergic neurons in feeding and the agouti obesity syndrome. Nature. 1997;385:165–168. [DOI] [PubMed] [Google Scholar]
- 39. Bertolini A, Poggioli R, Vergoni AV. Cross-species comparison of the ACTH-induced behavioral syndrome. Ann NY Acad Sci. 1988;525:114–129. [DOI] [PubMed] [Google Scholar]
- 40. Xu Y, Wu Z, Sun H, et al. Glutamate mediates the function of melanocortin receptor 4 on Sim1 neurons in body weight regulation. Cell Metab. 2013;18:860–870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Perello M, Stuart RC, Nillni EA. Differential effects of fasting and leptin on proopiomelanocortin peptides in the arcuate nucleus and in the nucleus of the solitary tract. Am J Physiol Endocrinol Metab. 2007;292:E1348–E1357. [DOI] [PubMed] [Google Scholar]
- 42. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–419. [DOI] [PubMed] [Google Scholar]
- 43. Gilbeau PM, Almirez RG, Holaday JW, Smith CG. Opioid effects on plasma concentrations of luteinizing hormone and prolactin in the adult male rhesus monkey. J Clin Endocrinol Metab. 1985;60:299–305. [DOI] [PubMed] [Google Scholar]
- 44. Leadem CA, Kalra SP. Reversal of β-endorphin-induced blockade of ovulation and luteinizing hormone surge with prostaglandin E2. Endocrinology. 1985;117:684–689. [DOI] [PubMed] [Google Scholar]
- 45. Wardlaw SL, Ferin M. Interaction between β-endorphin and α-melanocyte-stimulating hormone in the control of prolactin and luteinizing hormone secretion in the primate. Endocrinology. 1990;126:2035–2040. [DOI] [PubMed] [Google Scholar]
- 46. Xu AW, Ste-Marie L, Kaelin CB, Barsh GS. Inactivation of signal transducer and activator of transcription 3 in proopiomelanocortin (Pomc) neurons causes decreased pomc expression, mild obesity, and defects in compensatory refeeding. Endocrinology. 2007;148:72–80. [DOI] [PubMed] [Google Scholar]
- 47. Reed AS, Unger EK, Olofsson LE, Piper ML, Myers MG, Jr, Xu AW. Functional role of suppressor of cytokine signaling 3 upregulation in hypothalamic leptin resistance and long-term energy homeostasis. Diabetes. 2010;59:894–906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Nicolas P, Li CH. β-Endorphin-(1–27) is a naturally-occurring antagonist to etorphine-induced analgesia. Proc Natl Acad Sci USA. 1985;82:3178–3181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Melis MR, Argiolas A. Yawning: role of hypothalamic paraventricular nitric oxide. Zhongguo Yao Li Xue Bao. 1999;20:778–788. [PubMed] [Google Scholar]
- 50. Williams KW, Margatho LO, Lee CE, et al. Segregation of acute leptin and insulin effects in distinct populations of arcuate proopiomelanocortin neurons. J Neurosci. 2010;30:2472–2479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Vergoni AV, Bertolini A, Mutulis F, Wikberg JE, Schiöth HB. Differential influence of a selective melanocortin MC4 receptor antagonist (HS014) on melanocortin-induced behavioral effects in rats. Eur J Pharmacol. 1998;362:95–101. [DOI] [PubMed] [Google Scholar]
- 52. Caquineau C, Leng G, Guan XM, Jiang M, Van der Ploeg L, Douglas AJ. Effects of α-melanocyte-stimulating hormone on magnocellular oxytocin neurones and their activation at intromission in male rats. J Neuroendocrinol. 2006;18:685–691. [DOI] [PubMed] [Google Scholar]
- 53. Van der Ploeg LH, Martin WJ, Howard AD, et al. A role for the melanocortin 4 receptor in sexual function. Proc Natl Acad Sci USA. 2002;99:11381–11386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. O'Malley D, MacDonald N, Mizielinska S, Connolly CN, Irving AJ, Harvey J. Leptin promotes rapid dynamic changes in hippocampal dendritic morphology. Mol Cell Neurosci. 2007;35:559–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Valerio A, Ghisi V, Dossena M, et al. Leptin increases axonal growth cone size in developing mouse cortical neurons by convergent signals inactivating glycogen synthase kinase-3β. J Biol Chem. 2006;281:12950–12958. [DOI] [PubMed] [Google Scholar]
- 56. Bouret SG, Bates SH, Chen S, Myers MG, Jr, Simerly RB. Distinct roles for specific leptin receptor signals in the development of hypothalamic feeding circuits. J Neurosci. 2012;32:1244–1252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Caron E, Sachot C, Prevot V, Bouret SG. Distribution of leptin-sensitive cells in the postnatal and adult mouse brain. J Comp Neurol. 2010;518:459–476. [DOI] [PubMed] [Google Scholar]
- 58. Steculorum SM, Bouret SG. Maternal diabetes compromises the organization of hypothalamic feeding circuits and impairs leptin sensitivity in offspring. Endocrinology. 2011;152:4171–4179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Bouret SG, Draper SJ, Simerly RB. Trophic action of leptin on hypothalamic neurons that regulate feeding. Science. 2004;304:108–110. [DOI] [PubMed] [Google Scholar]
- 60. Pinto S, Roseberry AG, Liu H, et al. Rapid rewiring of arcuate nucleus feeding circuits by leptin. Science. 2004;304:110–115. [DOI] [PubMed] [Google Scholar]
- 61. Bouret SG, Simerly RB. Development of leptin-sensitive circuits. J Neuroendocrinol. 2007;19:575–582. [DOI] [PubMed] [Google Scholar]
- 62. Plagemann A, Harder T, Janert U, et al. Malformations of hypothalamic nuclei in hyperinsulinemic offspring of rats with gestational diabetes. Dev Neurosci. 1999;21:58–67. [DOI] [PubMed] [Google Scholar]
- 63. Plagemann A, Heidrich I, Götz F, Rohde W, Dörner G. Lifelong enhanced diabetes susceptibility and obesity after temporary intrahypothalamic hyperinsulinism during brain organization. Exp Clin Endocrinol. 1992;99:91–95. [DOI] [PubMed] [Google Scholar]
- 64. Vogt MC, Paeger L, Hess S, et al. Neonatal insulin action impairs hypothalamic neurocircuit formation in response to maternal high-fat feeding. Cell. 2014;156:495–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Coupe B, Bouret SG. Development of the hypothalamic melanocortin system. Front Endocrinol (Lausanne). 2013;4:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Glavas MM, Joachim SE, Draper SJ, Smith MS, Grove KL. Melanocortinergic activation by melanotan II inhibits feeding and increases uncoupling protein 1 messenger ribonucleic acid in the developing rat. Endocrinology. 2007;148:3279–3287. [DOI] [PubMed] [Google Scholar]
- 67. Berman Y, Mzhavia N, Polonskaia A, Devi LA. Impaired prohormone convertases in Cpe(fat)/Cpe(fat) mice. J Biol Chem. 2001;276:1466–1473. [DOI] [PubMed] [Google Scholar]
- 68. Srinivasan S, Bunch DO, Feng Y, et al. Deficits in reproduction and pro-gonadotropin-releasing hormone processing in male Cpefat mice. Endocrinology. 2004;145:2023–2034. [DOI] [PubMed] [Google Scholar]
- 69. Naggert JK, Fricker LD, Varlamov O, et al. Hyperproinsulinaemia in obese fat/fat mice associated with a carboxypeptidase E mutation which reduces enzyme activity. Nat Genet. 1995;10:135–142. [DOI] [PubMed] [Google Scholar]
- 70. Varlamov O, Leiter EH, Fricker L. Induced and spontaneous mutations at Ser202 of carboxypeptidase E. Effect on enzyme expression, activity, and intracellular routing. J Biol Chem. 1996;271:13981–13986. [DOI] [PubMed] [Google Scholar]
- 71. Cawley NX, Normant E, Chen A, Loh YP. Oligomerization of pro-opiomelanocortin is independent of pH, calcium and the sorting signal for the regulated secretory pathway. FEBS Lett. 2000;481:37–41. [DOI] [PubMed] [Google Scholar]
- 72. Shen FS, Aguilera G, Loh YP. Altered biosynthesis and secretion of pro-opiomelanocortin in the intermediate and anterior pituitary of carboxypeptidase E-deficient, Cpe(fat)/ Cpe(fat)mice. Neuropeptides. 1999;33:276–280. [DOI] [PubMed] [Google Scholar]
- 73. Cool DR, Normant E, Shen F, et al. Carboxypeptidase E is a regulated secretory pathway sorting receptor: genetic obliteration leads to endocrine disorders in Cpe(fat) mice. Cell. 1997;88:73–83. [DOI] [PubMed] [Google Scholar]
- 74. Shen FS, Loh YP. Intracellular misrouting and abnormal secretion of adrenocorticotropin and growth hormone in cpefat mice associated with a carboxypeptidase E mutation. Proc Natl Acad Sci USA. 1997;94:5314–5319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Nillni EA, Xie W, Mulcahy L, Sanchez VC, Wetsel WC. Deficiencies in pro-thyrotropin-releasing hormone processing and abnormalities in thermoregulation in Cpefat/fat mice. J Biol Chem. 2002;277:48587–48595. [DOI] [PubMed] [Google Scholar]
- 76. Maffei M, Halaas J, Ravussin E, et al. Leptin levels in human and rodent: measurement of plasma leptin and ob RNA in obese and weight-reduced subjects. Nat Med. 1995;1:1155–1161. [DOI] [PubMed] [Google Scholar]
- 77. Heymsfield SB, Greenberg AS, Fujioka K, et al. Recombinant leptin for weight loss in obese and lean adults: a randomized, controlled, dose-escalation trial. JAMA. 1999;282:1568–1575. [DOI] [PubMed] [Google Scholar]
- 78. Hukshorn CJ, Saris WH, Westerterp-Plantenga MS, Farid AR, Smith FJ, Campfield LA. Weekly subcutaneous pegylated recombinant native human leptin (PEG-OB) administration in obese men. J Clin Endocr Metab. 2000;85:4003–4009. [DOI] [PubMed] [Google Scholar]
- 79. Kleinridders A, Lauritzen HP, Ussar S, et al. Leptin regulation of Hsp60 impacts hypothalamic insulin signaling. J Clin Invest. 2013;123:4667–4680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Stoléru S, Fonteille V, Cornélis C, Joyal C, Moulier V. Functional neuroimaging studies of sexual arousal and orgasm in healthy men and women: a review and meta-analysis. Neurosci Biobehav Rev. 2012;36:1481–1509. [DOI] [PubMed] [Google Scholar]
- 81. Karama S, Lecours AR, Leroux J, et al. Areas of brain activation in males and females during viewing of erotic film excerpts. Hum Brain Mapp. 2002;16:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Paul T, Schiffer B, Zwarg T, et al. Brain response to visual sexual stimuli in heterosexual and homosexual males. Hum Brain Mapp. 2008;29:726–735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Redouté J, Stoléru S, Grégoire MC, et al. Brain processing of visual sexual stimuli in human males. Hum Brain Mapp. 2000;11:162–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Arnow BA, Desmond JE, Banner LL, et al. Brain activation and sexual arousal in healthy, heterosexual males. Brain. 2002;125:1014–1023. [DOI] [PubMed] [Google Scholar]
- 85. Ferretti A, Caulo M, Del Gratta C, et al. Dynamics of male sexual arousal: distinct components of brain activation revealed by fMRI. Neuroimage. 2005;26:1086–1096. [DOI] [PubMed] [Google Scholar]
- 86. Argiolas A, Melis MR, Murgia S, Schiöth HB. ACTH- and α-MSH-induced grooming, stretching, yawning and penile erection in male rats: site of action in the brain and role of melanocortin receptors. Brain Res Bull. 2000;51:425–431. [DOI] [PubMed] [Google Scholar]
- 87. Argiolas A, Melis MR. Central control of penile erection: role of the paraventricular nucleus of the hypothalamus. Prog Neurobiol. 2005;76:1–21. [DOI] [PubMed] [Google Scholar]
- 88. Mountjoy KG, Mortrud MT, Low MJ, Simerly RB, Cone RD. Localization of the melanocortin-4 receptor (MC4-R) in neuroendocrine and autonomic control-circuits in the brain. Mol Endocrinol. 1994;8:1298–1308. [DOI] [PubMed] [Google Scholar]
- 89. Kishi T, Aschkenasi CJ, Lee CE, Mountjoy KG, Saper CB, Elmquist JK. Expression of melanocortin 4 receptor mRNA in the central nervous system of the rat. J Comp Neurol. 2003;457:213–235. [DOI] [PubMed] [Google Scholar]
- 90. Gelez H, Poirier S, Facchinetti P, et al. Neuroanatomical distribution of the melanocortin-4 receptors in male and female rodent brain. J Chem Neuroanat. 2010;40:310–324. [DOI] [PubMed] [Google Scholar]
- 91. Chen KK, Chan SHH, Chang LS, Chan JYH. Participation of paraventricular nucleus of hypothalamus in central regulation of penile erection in the rat. J Urology. 1997;158:238–244. [DOI] [PubMed] [Google Scholar]
- 92. Giuliano F, Clément P, Droupy S, Alexandre L, Bernabé J. Melanotan-II: investigation of the inducer and facilitator effects on penile erection in anaesthetized rat. Neuroscience. 2006;138:293–301. [DOI] [PubMed] [Google Scholar]
- 93. Savic I, Berglund H, Gulyas B, Roland P. Smelling of odorous sex hormone-like compounds causes sex-differentiated hypothalamic activations in humans. Neuron. 2001;31:661–668. [DOI] [PubMed] [Google Scholar]
- 94. Balthazart J, Ball GF. Topography in the preoptic region: differential regulation of appetitive and consummatory male sexual behaviors. Front Neuroendocrin. 2007;28:161–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Hull EM, Dominguez JM. Sexual behavior in male rodents. Horm Behav. 2007;52:45–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Swanson LW. Cerebral hemisphere regulation of motivated behavior. Brain Res. 2000;886:113–164. [DOI] [PubMed] [Google Scholar]
- 97. Hughes AM, Everitt BJ, Herbert J. The effects of simultaneous or separate infusions of some pro-opiomelanocortin-derived peptides (β-endorphin, melanocyte stimulating hormone, and corticotrophin-like intermediate polypeptide) and their acetylated derivatives upon sexual and ingestive behavior of male-rats. Neuroscience. 1988;27:689–698. [DOI] [PubMed] [Google Scholar]
- 98. Oomura Y, Aou S, Koyama Y, Fujita I, Yoshimatsu H. Central control of sexual behavior. Brain Res Bull. 1988;20:863–870. [DOI] [PubMed] [Google Scholar]
- 99. Perachio AA, Marr LD, Alexander M. Sexual behavior in male rhesus monkeys elicited by electrical stimulation of preoptic and hypothalamic areas. Brain Res. 1979;177:127–144. [DOI] [PubMed] [Google Scholar]
- 100. Girardet C, Butler AA. Neural melanocortin receptors in obesity and related metabolic disorders. Biochim Biophys Acta. 2014;1842:482–494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Sohn JW, Williams KW. Functional heterogeneity of arcuate nucleus pro-opiomelanocortin neurons: implications for diverging melanocortin pathways. Mol Neurobiol. 2012;45:225–233. [DOI] [PMC free article] [PubMed] [Google Scholar]