Abstract
Context:
Rituximab depletes CD20+ B cells and has shown potential benefit in thyroid-associated ophthalmopathy (TAO). The impact of rituximab on T cell phenotype in TAO is unexplored.
Objective:
The objective of the study was to quantify the abundance of IGF-I receptor-positive (IGF-1R+) CD4 and CD8 T cells in active TAO before and after treatment with rituximab.
Design:
This was a retrospective case series assessing IGF-1R+ T cells before and after treatment with rituximab with an 18-month follow-up.
Setting:
The study was conducted at a tertiary care medical center.
Patients:
Study participants included eight patients with severe TAO.
Interventions:
Two infusions of rituximab (1 g or 500 mg each) were administered 2 weeks apart.
Main Outcome Measures:
Quantification of IGF-1R+ T cells using flow cytometry was measured.
Results:
Eight patients with moderate to severe TAO [mean pretreatment clinical activity score (CAS) 5.1 ± 0.2 (SEM)] were treated. Four to 6 weeks after treatment, CAS improved to 1.5 ± 0.3, whereas the proportion of IGF-1R+ CD3+ T cells declined from 41.9% to 28.3% (P = .004). The proportion of IGF-1R+ CD4+ and IGF-1R+ CD8+ T cells declined 4–6 weeks after treatment (from 45.6% to 21.5% and from 32.0% to 15.8%, P = .003 and P = .001, respectively). In two patients, IGF-1R+ CD4+ and IGF-1R+ CD8+ subsets approximated pretreatment levels after 16 weeks.
Conclusions:
Frequency of IGF-1R+ T cells in patients with TAO declines within 4–6 weeks after rituximab treatment. This phenotypic shift coincides with clinical improvement. Thus, assessment of the abundance of IGF-1R+ T cells in response to rituximab may provide a biomarker of clinical response. Our current findings further implicate the IGF-1R pathway in the pathogenesis of TAO.
Insight into the pathogenesis of Graves' disease (GD) has improved over the past decade. However, its most devastating manifestation, thyroid-associated ophthalmopathy (TAO), remains enigmatic. Stimulating autoantibodies against the TSH receptor (TSHR) appear to underlie the endocrine manifestations of GD (1), but the role of TSHR in the development of extrathyroidal consequences of GD autoimmunity must be substantiated. Additional autoantigens including the IGF-I receptor (IGF-1R) may participate in the pathogenesis of TAO (2–4). Moreover, the close physical and functional relationship between IGF-1R and TSHR underscore the complex mechanisms at play in this syndrome (5).
IGF-1R was cloned more than 2 decades ago, based on its role in proliferative and metabolic regulation of precancerous cells. More recent observations have implicated IGF-1R in autoimmunity of GD. Autoantibodies to IGF-1R are present in a subset of patients with GD but are absent in healthy donors (6, 7); others have failed to implicate these antibodies in GD (8), and the topic remains controversial (2). In patients with TAO, IGF-1R is overexpressed on orbital fibroblasts (6, 9), and IGF-1R+ peripheral blood T cells (10) and B cells (11) are more abundant in patients with GD compared with healthy donors. IGF-1R display appears to carry functional consequences to immune function through the enhancement of proliferation, reduced susceptibility to apoptosis (12), stimulation of cytokine production by T cells and monocytes (13, 14), and increased antibody production by peripheral B cells (15–18). Thus, IGF-1R may act both as an autoantigen and a growth factor receptor in TAO.
Although our understanding of the pathogenesis of TAO has progressed, therapeutic options have remained limited. Intravenous steroids and orbital irradiation may reduce inflammatory signs, whereas decompression surgery can reverse optic neuropathy or facial disfigurement. However, no treatment has been shown to significantly alter the natural history of TAO. Several authors have reported clinical benefit from rituximab (Rituxan; Genentech, Inc), a human-murine chimeric monoclonal antibody that depletes CD20+ B cells (19–21). Although their reports are encouraging, the precise mechanism(s) of rituximab action in TAO remains obscure. As clinical trials of rituximab move forward, it will be important to identify this mechanism and to develop biomarkers for assessing disease activity.
In the current communication, we assess the impact of B cell depletion after rituximab therapy on the phenotype of T cells in individuals with TAO. We report that the disease-associated bias toward the IGF-1R+ phenotype is nearly normalized and that the drug effects appear transient. Our findings suggest a potentially interesting association between changes in T cell phenotypes and the clinical responses to rituximab. They also identify a possible role for B cells in supporting the IGF-1R+ phenotype of T cells in severe TAO.
Materials and Methods
Subjects
These activities were approved by the Institutional Review Boards of the University of Michigan Health System, the University of California at Los Angeles Health Sciences Center, and the Harbor-University of California Los Angeles Medical Center. They were conducted according to the tenets of the Declaration of Helsinki. Informed consent was obtained from all study participants. Patients with severe TAO being cared for at the Eye Plastic, Orbital, and Facial Cosmetic Surgery Clinic at Kellogg Eye Center and the Jules Stein Eye Institute and who had received rituximab treatment over the time interval from October 1, 2007, through the present were considered for inclusion. Study participants included eight patients from whom peripheral blood mononuclear cells were available for IGF-1R analysis. GD was diagnosed using standard clinical parameters including signs and symptoms of hyperthyroidism, thyrotoxicosis, diffuse goiter, elevated free T4, low or undetectable serum thyroid-stimulating hormone, and the presence of thyroid-stimulating Igs. TAO was identified by the findings of proptosis, lid retraction, restrictive strabismus, conjunctival injection, chemosis, periocular erythema, and swelling. Disease activity was graded using the seven-item clinical activity score (CAS) as described (22).
Treatment criteria
The subjects received rituximab infusion therapy for the following medical indications: 1) poor response to corticosteroids (CS) as defined by a decrease in CAS of 2 or less; 2) recurrence of TAO as judged by an increased CAS of 2 or greater after the taper of CS; 3) progression of disease despite CS treatment; and 4) persistence of compressive optic neuropathy after medical or surgical therapy. The following were assessed as a prelude to therapy: complete blood count, liver and kidney function, serum Ig levels, and hepatitis B and C serology. Prior immunizations for tetanus, pneumococcus, and diphtheria were verified and updated if necessary. Two infusions of rituximab (1 g or 500 mg each) were administered 2 weeks apart, in accordance with the protocol approved by the US Food and Drug Administration for the treatment of rheumatoid arthritis. Premedication included 100 mg iv methylprednisolone, 1 g oral acetaminophen, and 50 mg diphenhydramine, given 30 minutes before rituximab infusion. Patients were assessed at 4–6 weeks after rituximab therapy with comprehensive ophthalmic examination. Two patients were also assessed at 2, 16, and more than 72 weeks after their final dose of rituximab. The posttherapy evaluation included CAS, visual acuity, color vision, pupillary response, fundus examination, and Goldmann applanation tonometry.
Flow cytometry
Assessment of IGF-1R display on lymphocytes has been described in detail elsewhere (23). Briefly, peripheral blood mononuclear cells were washed in staining buffer containing PBS with 0.1% sodium azide and 1% BSA and then incubated with heat-inactivated mouse serum for 5 minutes. They were then incubated with peridinin chlorophyll protein (PerCP)-conjugated antihuman CD19, CD3, CD4, CD8, and phycoerythrin (PE)-conjugated antihuman CD221 (IGF-1R) for 30 minutes at 4°C. Samples were washed and resuspended in staining buffer at 4°C and analyzed with an LSRII or FACS Calibur flow-cytometer (BD Biosciences). Mean fluorescent intensity was calculated as a ratio of mean fluorescence sample/isotype control fluorescence, whereas percentage-positive expression was defined as percentage-positive cells relative to isotype control. Viable cells were gated on the basis of forward light scatter, and the data were analyzed with the FCS Express software program (De Novo Software).
Statistics
Statistical analysis was performed with commercially available software [Excel 2007 (Microsoft); SPSS version 13.0 (SPSS, Inc); and GraphPad Prism 5 (GraphPad Software)]. Data were expressed as the mean ± SEM.
Results
Patients treated with rituximab exhibited profound improvement in inflammatory symptoms, as evidenced by a substantial reduction in their seven-point CAS. Patient demographics are detailed in Table 1. Although inflammatory signs and symptoms improved with rituximab, proptosis and strabismus failed to do so, consistent with previous reports (21). CAS improved from an average of 5.1 ± 0.2 SEM before treatment to 1.5 ± 0.3 SEM 4–6 weeks after treatment with rituximab (Figure 1A).
Table 1.
Demographical Information for the Eight Study Patients
| Patient Number | P1 | P2 | P3 | P4 | P5 | P6 | P7 | P8 |
|---|---|---|---|---|---|---|---|---|
| Age, y | 59 | 55 | 47 | 54 | 62 | 60 | 51 | 68 |
| Sex | M | M | F | F | F | M | F | F |
| Smoking status | Current | Current | NS | NS | Current | Current | NS | NS |
| PMH | Splenectomy due to trauma, hemochromatosis | HTN, hyperlipidemia | NIDDM | HTN | HTN | HTN | ITP, sleep apnea, migraine | CA breast, DM, HTN, RA, Sjogren |
| Endocrinological treatment of GD | ATD | ATD | RAI | ATD | RAI | ATD | None | T4 |
| Chronology of TAO in relation to thyroid disease | Before GD | After GD | After GD | After GD | After GD | After GD | With GD | After GD |
| Duration of TAO prior to corticosteroids | 3 | N/A | N/A | 4 | 2 | N/A | 2 | 5 |
| Duration of corticosteroids prior to RTX | 13 | 0 | 0 | 1 | 2 | 0 | 1 | 10 |
| Duration of TAO prior to RTX | 16 | 4 | 6 | 5 | 4 | 5 | 7 | 15 |
| Clinical response to CS | Progression; CON during CS taper | Progression | Progression | Progression | Progression | Progression | Progression | Progression; CON |
| Additional immunosuppressant before RTX | Cellcept | None | None | None | None | None | None | PMP |
| Episode of CON (side) | Right | Bilateral | Left | Left | Right | Bilateral | None | Right |
| Orbital decompression (number eyes) | 1 (9 mo prior to RTX) | None | None | 1 (9 mo after RTX) | None | None | 2 (2 mo after RTX) | 1 (after first RTX infusion) |
Abbreviations: ATD, antithyroid drugs; CA, cancer; CS for corticosteroids; DM, diabetes mellitus; HTN, hypertension; PMP for pulsed methylprednisolone; CS, current smoker; F, female; M, male; N/A, not available; NIDDM, non-insulin-dependent diabetes mellitus; NS, nonsmoker; RAI, radioactive iodine; RA, rheumatoid arthritis; ITP, idiopathic thrombocytopenic purpurea; RTX, rituximab; CON, compressive optic neuropathy; GO, Graves' ophthalmopathy. The table includes patient age, gender, smoking status, medical history, treatment of hyperthyroidism, chronology of GD, duration of GO prior to corticosteroids, duration of corticosteroids prior to rituximab treatment, duration of GO prior to rituximab treatment, additional immunosuppressant before rituximab (if applicable), whether compressive optic neuropathy was present, and whether orbital decompression surgery had been done.
Figure 1.
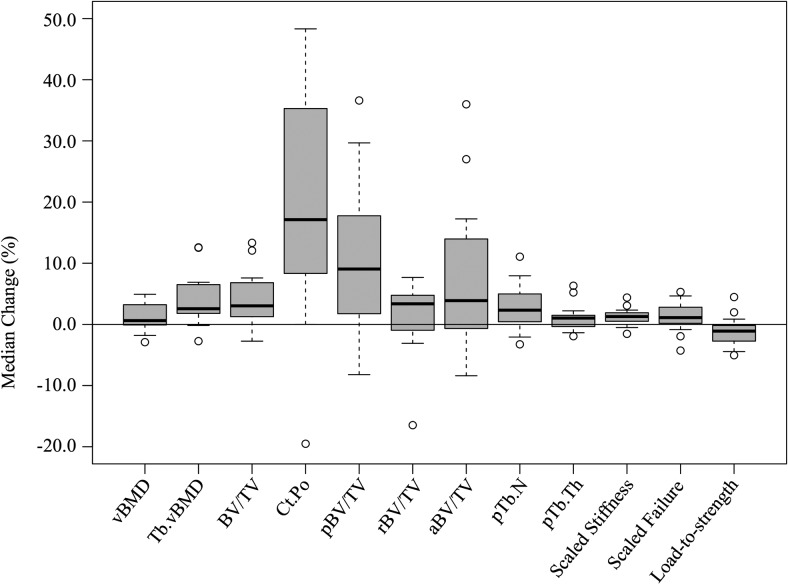
A, CASs for the eight study patients (P1–P8) significantly decreased after rituximab treatment. CAS improved from an average of 5.1 ± 0.2 SEM before treatment to 1.5 ± 0.3 SEM 4–6 weeks after treatment with rituximab. B and C, Flow cytometric analysis of peripheral blood monocunlear cells from a representative patient were incubated with antihuman CD 19, CD3, CD4, CD8, or CD 221 (IGF-1R), as described in Materials and Methods. B, Each black dot represents the data for a single cell. The open black circles delineate IGF-1R+ cells. B cells (CD19+) are abundant at baseline but vanish, as expected, 4–6 weeks after rituximab treatment. C, Flow cytometric analysis of IGF-1R+ display on T cell subsets before, 2 weeks, 4–6 weeks, and 16 weeks after treatment with rituximab. Both CD4 and CD8+ T cells demonstrate reduced IGF-1R display after rituximab (from 53% to 17% and from 24% to 15% 4–6 weeks after treatment in CD4 and CD8+ T cells, respectively). These data are representative of results for eight patients.
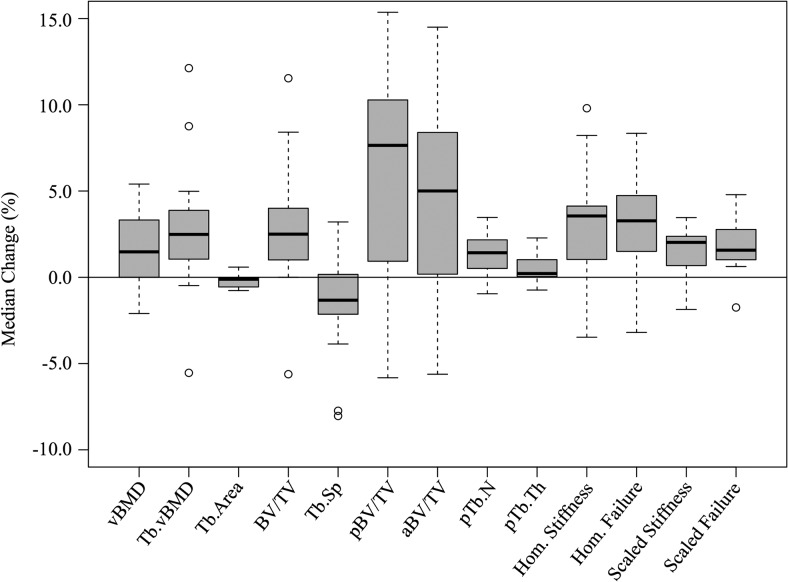
The proportion of IGF-1R+ B and IGF-1R+ T cells was compared before and after completion of rituximab treatment using flow cytometry. Results shown in Figure 1, B and C, are representative. CD19+ B cells were dramatically reduced in all patients after treatment (Figure 1B). Similarly, IGF-1R+ T cells were abundant in TAO patients before treatment and declined within 4–6 weeks after treatment (Figure 1C). CD3+ IGF-1R+ T cells declined from 41.9% ± 5.9% to 28.3% ± 7.6% (mean ± SEM, n = 8, P = .004; Figure 2, A and B). CD4+ IGF-1R+ cells also declined from 45.6% ± 7.9% to 21.5% ± 4.8% (mean ± SEM, n = 8, P = .003; Figure 2C), whereas CD8+ IGF-1R+ cells declined from 32.0% ± 4.4% to 15.8% ± 4.5% (mean ± SEM, n = 6, P = .001; Figure 2D).
Figure 2.
A, IGF-1R display on CD3+ T cells is significantly reduced after treatment with rituximab in the eight study patients (P < .004). Data are shown for all eight patients in A, and averages with error bars representing SEM are shown in B. The IGF-1R display is reduced, on average, from 42% to 28% (B, all patients, n = 8). The IGF-1R display is also significantly reduced after rituximab treatment in CD4+ (C) and CD8+ T cells (D), with values of P < .003 and P < .001, respectively. In two patients for whom extended surveillance was possible (P7 and P8), the IGF-1R display on CD4+ T cells declined within 4–6 weeks after rituximab treatment and then recovered toward baseline at 16 weeks (E). The CASs for the same two patients showed clinical improvement (lower scores) within 4–6 weeks and remained at nadir through the point of last follow-up (F).
Reduction in IGF-1R+ T cells correlated with the initial clinical response after treatment with rituximab, reflected by an improving CAS. In the two patients in whom extended surveillance was possible, IGF-1R+ T cell frequency began to recover at 16 weeks (Figure 2D), whereas the clinical improvement endured through the point of the last follow-up (16 wk and 18 mo; Figure 2E).
Discussion
The mechanisms underlying clinical benefit after treatment with rituximab in autoimmunity remain uncertain. In this study, we demonstrate that the abundance of IGF-1R+ T cells is reduced after rituximab treatment. This finding suggests that the drug influences cell-mediated immunity not only through B cell depletion but also through a phenotypic shift in T cells. It is unclear whether the change in T cell phenotypes is a direct consequence of rituximab or is mediated by B cell depletion. In either case, the fractional decline of these cells may represent a surrogate for disease activity and response to therapy. Although a previous study reported no change in the abundance of IGF-1R+ T cells after rituximab therapy (21), T cells were characterized in a single patient at fewer time points.
Because TAO represents an organ-specific autoimmune disease, it would be interesting to analyze IGF-1R+ T cells before and after rituximab therapy at the orbital tissue level. The present study was limited to peripheral blood analysis. However, Nielsen et al (24) found a change in lymphocyte subpopulations in orbital tissues after rituximab therapy, and concluded that rituximab influences TAO through a reduction of B cell antigen presentation to T cells. Our findings reinforce the idea that B cell depletion can influence lymphocyte subpopulations (24).
Although overall T cell counts are not altered by rituximab, our study found that the proportion of IGF-1R+ T cells decreased. It is unclear whether this is due to decreased expression of IGF-1R by T cells or by their turnover. The mechanism underlying this phenotypic shift is uncertain. The stability of the overall T cell count would favor the reduced expression of IGF-1R rather than their selective turnover. A reduction of IGF-1R+ T cells could be secondary to reduced B cell help after the elimination of these cells. Interestingly, the frequency of IGF-1R+ T cells appears to recover partially after 6–8 weeks, prior to B cell reconstitution. Yet the clinical effects of rituximab on TAO and GD remission may last for more than 1 year. Thus, the changes in IGF-1R expression alone are unlikely to explain the durable clinical response. The hypothesis that rituximab therapy has a lasting effect on disease activity by reducing autoantibody production, destroying the B cells that support inflammatory plasma cell niches in which autoantibodies are produced, deserves further investigation (25).
In summary, we show that IGF-1R+ T cells become less frequent in individuals with severe TAO after rituximab treatment. Thus, in addition to the depletion of peripheral B cells, rituximab may mediate its effects, in part, through influencing T cell phenotype. The relative abundance of IGF-1R+ T cells may be a useful biomarker for TAO disease activity and therapeutic response. We propose that these levels be monitored in future clinical trials.
Acknowledgments
This work was supported in part by National Institutes of Health Grants EY008976, EY011708, EY021197, and DK063121; and Core Center for Vision Grant EY007003 from the National Eye Institute; Research to Prevent Blindness; and the Bell Charitable Foundation.
Disclosure Summary: The authors have nothing to declare.
Footnotes
- CAS
- clinical activity score
- CS
- corticosteroids
- GD
- Graves' disease
- IGF-1R
- IGF-I receptor
- TAO
- thyroid-associated ophthalmopathy
- TSHR
- TSH receptor.
References
- 1. Rapoport B, McLachlan SM. The thyrotropin receptor in Graves' disease. Thyroid. 2007;17:911–922. [DOI] [PubMed] [Google Scholar]
- 2. Wiersinga WM. Autoimmunity in Graves' ophthalmopathy: the result of an unfortunate marriage between TSH receptors and IGF-1 receptors? J Clin Endocrinol Metab. 2011;96:2386–2394. [DOI] [PubMed] [Google Scholar]
- 3. Weightman DR, Perros P, Sherif IH, Kendall-Taylor P. Autoantibodies to IGF-1 binding sites in thyroid associated ophthalmopathy. Autoimmunity. 1993;16:251–257. [DOI] [PubMed] [Google Scholar]
- 4. Smith TJ. Insulin-like growth factor-I regulation of immune function: a potential therapeutic target in autoimmune diseases? Pharmacol Rev. 2010;62:199–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tsui S, Naik V, Hoa N, et al. Evidence for an association between thyroid-stimulating hormone and insulin-like growth factor 1 receptors: a tale of two antigens implicated in Graves' disease. J Immunol. 2008;181:4397–4405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pritchard J, Han R, Horst N, Cruikshank WW, Smith TJ. Immunoglobulin activation of T cell chemoattractant expression in fibroblasts from patients with Graves' disease is mediated through the insulin-like growth factor I receptor pathway. J Immunol. 2003;170:6348–6354. [DOI] [PubMed] [Google Scholar]
- 7. Varewijck AJ, Boelen A, Lamberts SWJ, et al. Circulating IgGs may modulate IGF-I receptor stimulating activity in a subset of patients with Graves' ophthalmopathy. J Clin Endocrinol Metab. 2013;98:769–776. [DOI] [PubMed] [Google Scholar]
- 8. Minich WB, Dehina N, Welsink T, et al. Autoantibodies to the IGF1 receptor in Graves' orbitopathy. J Clin Endocrinol Metab. 2013;98:752–760. [DOI] [PubMed] [Google Scholar]
- 9. Pritchard J, Horst N, Cruikshank W, Smith TJ. Igs from patients with Graves' disease induce the expression of T cell chemoattractants in their fibroblasts. J Immunol. 2002;168:942–950. [DOI] [PubMed] [Google Scholar]
- 10. Douglas RS, Gianoukakis AG, Kamat S, Smith TJ. Aberrant expression of the insulin-like growth factor-1 receptor by T cells from patients with Graves' disease may carry functional consequences for disease pathogenesis. J Immunol. 2007;178:3281–3287. [DOI] [PubMed] [Google Scholar]
- 11. Douglas RS, Naik V, Hwang CJ, et al. B cells from patients with Graves' disease aberrantly express the IGF-1 receptor: implications for disease pathogenesis. J Immunol. 2008;181:5768–5774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Navarro M, Baserga R. Limited redundancy of survival signals from the type 1 insulin-like growth factor receptor. Endocrinology. 2001;142:1073–1081. [DOI] [PubMed] [Google Scholar]
- 13. Kooijman R, Coppens A, Hooghe-Peters E. IGF-I stimulates IL-8 production in the promyelocytic cell line HL-60 through activation of extracellular signal-regulated protein kinase. Cell Signal. 2003;15:1091–1098. [DOI] [PubMed] [Google Scholar]
- 14. Kooijman R, Coppens A. Insulin-like growth factor-I stimulates IL-10 production in human T cells. J Leukoc Biol. 2004;76:862–867. [DOI] [PubMed] [Google Scholar]
- 15. Jardieu P, Clark R, Mortensen D, Dorshkind K. In vivo administration of insulin-like growth factor-I stimulates primary B lymphopoiesis and enhances lymphocyte recovery after bone marrow transplantation. J Immunol. 1994;152:4320–4327. [PubMed] [Google Scholar]
- 16. Kimata H, Fujimoto M. Growth hormone and insulin-like growth factor I induce immunoglobulin (Ig)E and IgG4 production by human B cells. J Exp Med. 1994;180:727–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kimata H, Yoshida A. Effect of growth hormone and insulin-like growth factor-I on immunoglobulin production by and growth of human B cells. J Clin Endocrinol Metab. 1994;78:635–641. [DOI] [PubMed] [Google Scholar]
- 18. Robbins K, McCabe S, Scheiner T, Strasser J, Clark R, Jardieu P. Immunological effects of insulin-like growth factor-I—enhancement of immunoglobulin synthesis. Clin Exp Immunol. 1994;95:337–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. El Fassi D, Nielsen CH, Bonnema SJ, Hasselbalch HC, Hegedüs L. B lymphocyte depletion with the monoclonal antibody rituximab in Graves' disease: a controlled pilot study. J Clin Endocrinol Metab. 2007;92:1769–1772. [DOI] [PubMed] [Google Scholar]
- 20. Salvi M, Vannucchi G, Campi I, et al. Treatment of Graves' disease and associated ophthalmopathy with the anti-CD20 monoclonal antibody rituximab: an open study. Eur J Endocrinol. 2007;156:33–40. [DOI] [PubMed] [Google Scholar]
- 21. Khanna D, Chong KKL, Afifiyan NF, et al. Rituximab treatment of patients with severe, corticosteroid-resistant thyroid-associated ophthalmopathy. Ophthalmology. 2010;117:133–139.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wiersinga WM, Perros P, Kahaly GJ, et al. Clinical assessment of patients with Graves' orbitopathy: the European Group on Graves' Orbitopathy recommendations to generalists, specialists and clinical researchers. Eur J Endocrinol. 2006;155:387–389. [DOI] [PubMed] [Google Scholar]
- 23. Douglas RS, Afifiyan NF, Hwang CJ, et al. Increased generation of fibrocytes in thyroid-associated ophthalmopathy. J Clin Endocrinol Metab. 2010;95:430–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Nielsen JF, El Fassi D, Nielsen CH, et al. Evidence of orbital B and T cell depletion after rituximab therapy in Graves' ophthalmopathy. Acta Ophthalmol. 2009;87:927–929. [DOI] [PubMed] [Google Scholar]
- 25. Ferraro AJ, Drayson MT, Savage COS, MacLennan ICM. Levels of autoantibodies, unlike antibodies to all extrinsic antigen groups, fall following B cell depletion with Rituximab. Eur J Immunol. 2008;38:292–298. [DOI] [PubMed] [Google Scholar]