Abstract
Participation in youth sports can be very beneficial, but children with Attention Deficit Hyperactivity Disorder (ADHD) may participate less often and less successfully. The current study evaluated functional sports outcomes for children with ADHD who attended an intensive behavioral treatment program that included a sports training component, and it compared outcomes to children with ADHD who did not attend the program. Results suggest that treatment resulted in significant improvements in many aspects of children’s sports functioning, including knowledge of game rules, in vivo game performance, and fundamental skill tasks (motor proficiency, ability to trap a soccer ball appropriately, reduced handball penalties in soccer, and improved ability to catch a baseball). Parents also reported improved sports skills and good sportsmanship in the treatment group. No differences between groups were evident on additional skill tasks evaluating accurately kicking a soccer ball, throwing a baseball, or hitting a baseball off a tee. These results suggest intensive behavioral intervention that includes sports training can significantly improve functional sports outcomes for young children with ADHD.
Keywords: ADHD, Sports, Behavioral treatment, Summer Treatment Program
Participation in organized sports is a common developmental milestone for many children in America, with more children participating every year (National Center for Education Statistics 2005), and such activities can be a very beneficial experience for youth (e.g., Fraser-Thomas and Côté, 2006). It is well-established that regular physical activity is associated with better overall fitness and physical health (Center for Disease Control 2008), and helps prevent chronic diseases in children (e.g., Sothern et al. 1999). Furthermore, patterns of adult physical activity can be influenced by participation in sports during childhood (Dishman et al. 1985), suggesting that long lasting physical health benefits are one positive outcome of increased sports participation in children.
In addition to garnering direct physical benefits from playing sports, youth may also benefit from the unique socialization setting sports represent. Team sports provide children with opportunities to practice prosocial skills such as effective communication, turn taking, cooperation, leadership, conflict resolution, affective self-regulation, and problem solving. Potentially, the frequency of these learning opportunities for children who participate in sports consistently throughout their youth should result in more socially skilled behaviors outside of the sports setting as well (e.g., O’Callaghan et al. 2003). Indeed, research suggests that children who are more athletically skilled are more popular, accepted, and respected by their peers (Gross and Johnson 1984; Gross et al. 1985; Lopez-Williams et al. 2005; Weiss and Duncan 1992). Positive involvement in sports may also enhance self-esteem and self-efficacy (Smoll et al. 1993). In contrast, poor athletic performance is associated with lower self-confidence and self-concept, greater social isolation, and increased social and behavioral problems (Guevremont and Dumas 1994).
Despite the clear advantages of sports participation, children with Attention-Deficit Hyperactivity Disorder (ADHD) often fail to successfully engage in youth sport activities (Harvey et al. 2009; Pelham et al. 1990). ADHD is characterized by developmentally inappropriate levels of inattention, hyperactivity-impulsivity, or both (American Psychiatric American Psychiatric 2000). Though the mechanism through which ADHD symptoms may impact sports performance is not clear, a number of functional impairments associated with the disorder may be interfering with success in the sports arena (e.g., Harvey et al. 2007). For example, children with impaired attention may have difficulty learning game rules and strategies and applying these rules in the fluid fashion required by live game situations. Similarly, exhibiting impulsive behaviors during a competitive game setting may lead to careless errors, such as scoring in the wrong goal or committing a penalty. In fact, parent-reports suggest that boys with ADHD more often exhibit aggression and other behaviors that cause them to be disqualified during team sports (Johnson and Rosen 2000). In addition to potentially poor performance, many children with ADHD exhibit negative social behavior, a quality that their peers may find aversive (Lopez-Williams et al. 2005). Consequently, children with ADHD may be invited to join group games less often. In fact, even coaches of youth sports report significantly less positive attitudes about including these children on their teams (Beyer et al. 2008).
Failure to access the many potential advantages of sports participation may be especially salient for children with ADHD. Recent converging evidence suggests that the very areas in which youth sports participation may be beneficial are those in which children with ADHD may be impaired. Specifically, children with ADHD may demonstrate lower overall fitness than children without the disorder (Harvey and Reid 1997). Also, studies have found that rates of obesity may be higher in the ADHD population than previously thought (see Cortese and Angriman 2008 for a review). Similarly, a substantial proportion of children with ADHD also exhibit high rates of comorbid Developmental Coordination Disorder (DCD; Kadesjo and Gillberg 1999). DCD is a motor skills disorder which “significantly interferes with academic achievement or activities of daily living” (American Psychiatric American Psychiatric 2000) and may share an etiology with ADHD (e.g., Martin et al. 2006).
Clearly, many children with ADHD are exhibiting poor movement skills, and some evidence suggests that deficits in motor proficiency may be a fundamental impairment of the disorder. For the purposes of the current discussion, motor proficiency refers to both specific motor tasks (e.g., grasping a ball), as well as the cumulative effects of motor processes, such as the ability to grip, balance, and throw to successfully play a game of catch. In children, motor proficiency is associated with better levels of fitness over time (Hands 2008), more time spent engaged in physical activity, less time spent in sedentary activities, a healthier body mass index (BMI), and greater enjoyment of physical activity (Wrotniak et al. 2009). However, children with ADHD tend to demonstrate poor motor performance (Harvey and Reid 1997; Harvey et al. 2007), which is both directly and indirectly associated with worse overall fitness (Bouffard et al. 1996). Further, children with ADHD perform worse than age-matched peers on both gross and fine motor tasks, as well as sport-specific motor processes, such as running, jumping, catching, throwing, and kicking (Harvey and Reid 2003). These deficits often produce scores that are well below age expectations, and have been found both when compared to typically developing age-matched peers, as well as to peers with other mental health disorders (e.g., learning disability). The lower motor proficiency of children with ADHD likely acts as a barrier to participation in active free-play and in organized team physical activities.
Another domain in which success in the youth sports context may be especially challenging for children with ADHD is in the social interaction opportunities that occur within the sports context (see McQuade and Hoza 2008, for a review). Significant difficulties in peer relationships ranging from dislike and exclusion to explicit rejection and lack of close dyadic friendships are common among children with this disorder (Hoza et al. 2005; Pelham and Bender 1982). Compounding these difficulties, children with ADHD who exhibit motor performance deficits may be at even greater risk of social impairment (Ayaz et al. 2013). Consistently adverse peer relationships are associated with a number of negative outcomes, such as substance abuse, academic problems and school dropout, delinquency, and psychopathology (Bagwell et al. 2001; Newcomb et al. 1993; Parker and Asher 1987). The sports setting offers the potential context to mitigate some of these peer difficulties, and it may also serve as a protective factor if successful participation begins in early childhood.
Unfortunately, many evidence-based treatments for ADHD do not currently address the full scope of these related deficits. Stimulant medication, commonly prescribed as a first line treatment for ADHD, does not significantly improve peer relationships (Hoza et al. 2005), specific sports skills (Pelham et al. 1990), or motor proficiency (Beyer 1999; Harvey and Reid 1997; Hefley and Gorman 1986). That is, although a small number of studies suggest stimulant medication treatment may improve motor proficiency (e.g., Doyle et al. 1995), it is generally believed that the mechanism through which medication improves motor task performance and actual game play is through increased attention to task demands and individual performance (Pelham et al. 1990; Reitman et al. 2001). However, stimulant medication does not sufficiently address sports performance deficits frequently exhibited by children with ADHD related to knowledge or skill.
In contrast to studies of medication, efforts to improve sports behaviors and motor proficiency via behavior modification have been more successful. Positive effects of behavioral interventions have been demonstrated for improving sportsmanship behaviors (Hupp and Reitman 1999; Hupp et al. 2002; Sharpe et al. 1995), specific sports skills (Hupp and Reitman 1999), attention to game situations (O’Callaghan et al. 2003; Reitman et al. 2001) and motor performance (Verret et al. 2012). However, though a clear pattern of response in most children is evident, most studies of sport performance and motor proficiency utilize somewhat small sample sizes and brief interventions.
The current study builds on the promising impact of behavioral interventions by investigating the impact of an intensive behavioral treatment in which teaching age-appropriate sport skills is a fundamental component. The Summer Treatment Program (STP) is an evidence-based treatment for children with ADHD that employs intensive behavior modification as the primary agent of change in a recreational camp-like setting (Pelham and Fabiano 2008; Pelham et al. 2005a; Pelham and Hoza 1996). Over many years, the STP has demonstrated broad behavioral and academic improvements, including parent and counselor reports of improved prosocial behavior and specific sports skills in children (Pelham et al. 2013; Pelham and Hoza 1996). Children attending the STP typically participate in 9 h of programming per day for approximately 8 weeks. Groups consist of 12–15 age-matched children with 4–5 counselors who implement the treatment. Groups rotate together through academic activities, recreational activities, lunch, recess, and swimming instruction. Importantly for the purposes of the current study, children spend substantial time each day learning about sports (rules, strategies) and practicing sports skills. Specifically, 1 h each day is spent in a skill drill period during which children engage in drills to practice and improve their sports abilities. An additional 2 h is spent playing age-appropriate team sports (e.g., soccer, tee-ball/softball, basketball). Groups rotate through sports within and across days so that children have some breadth of experience, but also adequate opportunities to practice basic skills necessary for each sport. Fundamental skills, game strategies, and rules are taught via repetition of skill building drills scaffolded on children’s ability, and frequent coaching, modeling, and didactic instruction from counselors. For a more thorough description of STP procedures, see previous work by Pelham et al. (2010).
The purpose of the current study was to investigate the impact of an intensive behavioral treatment (the STP) that emphasizes sports instruction on several functional sports outcomes in young children with ADHD. It was hypothesized that children with ADHD who attended the STP would improve significantly more than children with ADHD who did not attend treatment on post-treatment measures of rule-based sport knowledge, ability to perform in game-like situations, proficiency in specific sport skills, sportsmanship behaviors, and motor proficiency.
Methods
Participants
Participants were 98 children diagnosed with ADHD (74 % males; mean age =6.64, range 5.56–7.98) who were a subset of participants in a larger study examining the influence of different levels of behavior therapy on initiation and use of stimulant medication treatment. As recommended (Pelham et al. 2005b), ADHD diagnosis was determined using parent and teacher rating scales of the Diagnostic and Statistical Manual of Mental Disorders (DSM) symptoms (i.e., Disruptive Behavior Disorder rating scale; Pelham et al. 1992), a semi-structured interview with the parent (Disruptive Behavior Disorder semi-structured parent interview; available from http://casgroup.fiu.edu/ccf/), and parent and teacher ratings of cross-situational impairment (Impairment Rating Scale; Fabiano et al. 2006)1. Two Ph.D. or M.D. level clinicians reviewed this data to diagnose each participant. Disagreements (8 % of cases) were resolved by independent review completed by a third clinician.
Exclusionary criteria for initial enrollment in the larger study were as follows: (1) Full Scale IQ below 70; (2) history of seizures or other neurological problems and/or taking medication to prevent seizures; (3) history of other medical problems for which psychostimulant treatment may have involved considerable risk; (4) history or concurrent diagnosis of any of the following disorders: pervasive developmental disorder, schizophrenia or other psychotic disorders, sexual disorder, organic mental disorder, or eating disorder; (5) placement in a full time special education classroom, and (6) current or past treatment with medication for ADHD or any other mental health problem, for either the target child or siblings. Since a goal of the larger study was to explore the progression of treatment, families where siblings were medicated were excluded from the larger study to ensure that parents and the child were “medication-naïve”. Notably, families may have initiated stimulant medication treatment (e.g., methylphenidate) prior to assessments in the current study.
All families completed parental consent forms prior to enrolling in the larger study, and were subsequently invited to participate in the current study. The subset of children in the current study included 52 children who received treatment via the STP and 46 who participated as a comparison group (i.e., did not attend the STP but came in for assessments). Participant characteristics are listed in Table 1. Groups did not differ significantly on most demographics and baseline characteristics. Exceptions to this are that groups differed on ADHD subtype, χ2 (2)=7.31, p <0.05, and prior medication status, χ2 (1)=4.03, p <0.05. Consequently, both ADHD subtype and prior medication status were included in analyses as statistical covariates.
Table 1.
Baseline characteristics for STP and control participants
| STPa | Control/No STPb | Test statistic | |
|---|---|---|---|
| Child age in yearsc | 6.68 (0.6) | 6.77 (0.6) | t (96)=0.70 |
| Warren & Hauser SEI Family Totalc | 67.01 (34.36) | 61.25 (34.49) | t (96)= −0.83 |
| Percent male | 75 | 74 | χ2 (1)=0.015 |
| Child race/ethnicity (%) | |||
| Caucasian | 71 | 82 | χ2 (4)=3.60 |
| African American | 14 | 7 | |
| Asian | 2 | 4 | |
| American Indian | 2 | 0 | |
| Other | 11 | 7 | |
| Highest parent education level (%) | χ2 (5)=3.97 | ||
| High school/GED | 14 | 17 | |
| Partial college/technical training | 11 | 22 | |
| 2-year/associate’s degree | 23 | 15 | |
| 4-year degree | 27 | 22 | |
| Graduate training/degree | 25 | 24 | |
| ADHD subtype (%) | |||
| Inattentive | 0 | 13 | χ2 (2)=7.31* |
| Hyperactive/impulsive | 17 | 13 | |
| Combined | 83 | 74 | |
| Comorbid diagnosis (%) | |||
| ODD | 77 | 61 | χ2 (1)=2.96 |
| CD | 10 | 11 | χ2 (1)=0.84 |
| Medicated prior to baseline (%) | 27 | 11 | χ2 (1)=4.03* |
Except where indicated, all values are percentages, and all test statistics are not significant
n=52
n=46
means and standard deviations
p <0.05
Procedure
The study was approved by the Institutional Review Board at the Women’s and Children’s Hospital of Buffalo. All parents provided written consent and children provided verbal assent prior to participation. Data were collected pre- and post-treatment for all participants. For pre-treatment assessments, parents were invited to bring their children (target and siblings) to at least one of six child-care sessions offered before the start of the STP. Families were informed that the study children would participate in brief assessments pertaining to age-appropriate sports, and all children would participate in recreational activities. Post-treatment data were collected from children in the STP during the final 3 days of the program. Children in the comparison group were assessed at one of two child-care sessions that occurred within 1 week of the end of the STP. The structure of the sessions, behavior management procedures, and assessment administration were identical across time points and groups.
For all assessment days, children were divided into small groups with a ratio of approximately one counselor to every three children. Counselors were trained commensurate with previous descriptions of STP staff training (Pelham et al. 2010). Since all children were unmedicated the day of the assessments, and to ensure that the children found the experience a positive one, assessment procedures were designed to be brief and fun. Also, behavioral expectations were intentionally constructed to allow as many children as possible to be successful. Groups followed a schedule throughout the day that interspersed brief periods of assessment with fun activities similar to a typical daycare day (organized outdoor games, watching cartoons, lunch/snacks, arts and crafts, etc.). For some skill assessments, all children rotated through assessments (e.g., soccer skill drills), and at others, individual children were briefly pulled out of a larger activity to complete an assessment (e.g., motor proficiency task). Staff implemented basic behavior management procedures throughout the day, including verbal feedback for both positive and negative behavior and time outs for serious negative behavior (e.g., aggression). Upon arrival, children were informed that if they behaved appropriately (i.e. had no escalated time outs), they could choose a prize at lunch time (for morning behavior) and again at the end of the day (for afternoon behavior).
Counselors who administered assessments were trained to avoid any kind of performance-related feedback during assessments, but were told to provide praise and encouragement at the end of a task for the child’s participation and effort. Feedback for non task-related behavior (e.g., interruption) was provided; however, very few instances of negative behavior occurred during the tasks. In one case, disruptive behavior precluded completion of one task, so data are presented only for the completed tasks for that child.
Athletic Competence Measures
Athletic competence, as measured in this study, focused on the fundamental skills and knowledge necessary for success in soccer and tee ball. These sports are emphasized in the STP since they are among the most prevalent sport experiences for early elementary-aged children. After consulting common coaching practices for youth sports (American Sport Education Program 2007; Snow and Dorrance 2011), measures were developed to correspond to specific fundamental skills, game knowledge, and performance in game situations that would most likely correspond to improved game play. Detailed protocols were created that included instructions regarding equipment set up, scripts for describing the activity to the child, and operationalized coding procedures (detailed scripts and procedural manuals are available from the first author). Prior to the start of the study, staff members were trained to reliably and consistently perform the assessments, and were supervised during the tasks by several of the authors. Measures of inter-rater reliability are presented below.
Sport Knowledge and Performance Tasks
To ascertain children’s basic game knowledge and their ability to perform appropriately in a game situation, a series of direct questions and live action game scenarios were conducted. These were standardized game performance scenarios that were designed to measure the child’s game knowledge or game performance. For example, in soccer the child was asked general knowledge questions such as “What goal are you trying to score in?” and (after the ball went out of bounds) “Which team gets the ball now?” Examples of performance items included asking the child to perform a kick off and a throw in. In tee-ball, examples of knowledge gathering questions included “What is a strike?” and “How many strikes are in an out?” Performance was scored for both batting and fielding. To maximize external validity and perform assessments in game-like situations, questions were interspersed with relevant game play. For example, when it was the child’s turn to hit in tee ball, he or she was first asked a few questions about how many strikes are in a strikeout, how many outs in an inning, and so on. The child was only asked questions during natural pauses in the game, such as when the ball went out of bounds or between batters. Furthermore, to make the game situations as realistic as possible, several staff members participated as other players, according to a script that closely resembled a real game. The script was standardized so that all children participated in identical game situations.
Mean scores (percent correct) for each scenario were computed. The series of knowledge recall items were combined to create an overall knowledge score. Likewise, the combined performance items (e.g., throw in, fielding play) created an overall performance score. The final knowledge scores and performance scores were analyzed separately for each sport.
Skill Tasks: Overview
Staff first demonstrated the appropriate way to perform the skill for each task. The child then performed one practice trial, during which feedback was given if the child broke a rule of the procedure that affected accurate measurement (e.g., stepping over a line). Staff did not give feedback that could affect performance, such as improving form. Except where noted, mean accuracy scores were calculated by dividing the number of accurate trials by the total trials.
Skill Tasks: Dribbling Penalties
Since a common error during soccer for children in this age range is to attempt to control the ball with their hands, the purpose of this drill was to evaluate the frequency of handball penalties during a dribbling drill. The dribbling course consisted of five cones set up in an M-shape within a 15 ft. by 15 ft. square. The child was instructed to dribble through the pattern as fast as possible while keeping control of the ball and following the rules of soccer. The frequency of handball penalties was recorded.
Skill Tasks: Kicking Accuracy
A 3 ft. by 3 ft. pop-up goal was attached to the ground, and the child was instructed to make 2 attempts to kick a soccer ball into the goal at each of three locations (indicated by painted marks on the ground; 6 trials total). One spot was 18 ft. directly in front of the center of the goal, and the others were 18 ft. to either side of the center marker. An attempt was coded as successful if the ball landed in the goal with only one kick (i.e., if a child kicked the ball and it stopped short of the target, it was coded as a miss).
Skill Tasks: Trapping Accuracy
The child stood at a painted mark 15 ft. from a staff member. Staff instructed the child to attempt to stop the ball so that it stayed within two steps of the child (eight trials). Commensurate with youth coaching guidelines (e.g., Snow and Dorrance 2011), a trap was coded as successful if the child was able to stop the ball as described without committing any penalties (i.e., handball) or stepping on the ball. If the ball went past the child or the trap attempt did not keep the ball within two steps of the child, it was coded as unsuccessful.
Skill Tasks: Throwing Accuracy
A two foot diameter round poster board target was attached to the backstop of a baseball field such that the center of the target was 4 f from the ground. From a line painted on the ground 15 f away, the child attempted to hit the target with a baseball (10 trials). A throw was coded as accurate if it hit the target without bouncing or hitting anything else first.
Skill Tasks: Catching Accuracy
The child was instructed to stand next to a cone that was placed 10 ft from the staff member for a game of catch. To determine handedness, the child was asked to pick up a baseball off of the ground and then throw it to the staff member. Age-appropriate gloves were provided for the child’s non-dominant hand. The ball was thrown overhand, directly towards the child. Appropriate catches were operationalized as the ball remaining in the child’s glove and the child maintaining possession (10 trials).
Skill Tasks: Hitting Accuracy
To determine how many baseballs the child could hit into fair territory from a standard tee (10 trials), staff first showed the child the location of fair territory and the batters’ box (1 ft. × 2 ft. box on either side of home plate). After the practice trial, each full swing was counted as an attempt. If the bat hit the tee before the ball, regardless of forward progress of the ball, it was coded as a miss.
Motor Proficiency
Motor proficiency was assessed using the short form of the Bruininks-Oseretsky Test of Motor Proficiency (BOTMP; Bruininks 1978). The BOTMP is an individually administered test, standardized across age and sex, for children between 4.5 and 14.5 years of age. The BOTMP provides a comprehensive index of motor proficiency, as well as separate measures of both gross and fine motor skills. The short form has been validated against the complete battery and consists of 14 items assessing gross motor development (running speed and agility, balance, bilateral coordination, strength, and upper-limb coordination) and fine motor development (response speed, visual-motor control, and upper-limb speed and dexterity). A single composite t-score is obtained as a general index of motor proficiency (Bruininks 1978).
Parent Improvement Ratings
At the end of the STP, parents were asked to rate the degree of improvement their child demonstrated using a rating used by others evaluating outcome of behavioral treatments (e.g., Fabiano et al. 2009; Haas et al. 2011). Parents of children who did not attend the STP also completed the rating based on general improvement over the course of the summer. Likertstyle ratings ranged from 1 (very much worse) to 7 (very much improved), with 4 indicating the behavior was unchanged. Parents could also indicate “no problem” for any domain in which the child did not experience impairment at the beginning of the STP; these items were excluded from analysis. Presented in the current study are parents’ responses to two items: “How much did your child improve in sports skills?” and “How much did your child improve in good sportsmanship?” Responses were combined separately for each item to represent improvement (scores 5–7), no change (score of 4), and worsening (scores 1–3).
Results
Reliability
Inter-observer reliability was estimated for the knowledge and performance tasks and for the specific skills tasks using correlations and t-tests of absolute mean differences. Across the tasks, between 4 and 9% of trials were selected at random and observed by an independent reliability rater. Comparisons between observers indicated that there were no differences between raters (see Table 2). Based on these estimates, inter-observer reliability scores for all novel measures were determined to be acceptable.
Table 2.
Descriptive information and reliability estimates of novel dependent variables
| Variable | n1 | Mean (SD) | Range | Skew (SE) | Kurtosis (SE) | n2 | Mean difference M (SD) | t | r |
|---|---|---|---|---|---|---|---|---|---|
| Knowledge | |||||||||
| Soccer | 181 | 0.30 (0.20) | 0.02–0.93 | 0.94 (0.18) | 0.36 (0.36) | 16 | 0.05 (0.07) | 0.76 | 0.90*** |
| Tee Ball | 182 | 0.54 (0.25) | 0–1.0 | 0.10 (0.18) | −0.84 (0.36) | 17 | 0.02 (0.05) | −0.006 | 0.98*** |
| Performance | |||||||||
| Soccer | 181 | 0.83 (0.17) | 0.30–1.0 | −0.22 (0.18) | −1.12 (0.36) | 16 | 0.08 (0.11) | 1.11 | 0.86*** |
| Tee ball | 181 | 0.56 (0.22) | 0–1.0 | −0.09 (0.18) | −0.47 (0.36) | 17 | 0.05 (0.07) | 0.53 | 0.94*** |
| Controlled tasks | |||||||||
| Kicking accuracy | 184 | 0.32 (0.21) | 0–1.0 | 0.44 (0.18) | −0.31 (0.36) | 9 | 0.13 (0.32) | 0.58 | 0.77* |
| Trapping appropriately | 186 | 0.20 (0.25) | 0–1.0 | 1.39 (0.18) | 1.43 (0.36) | 10 | 0.73 (0.90) | 1.19 | 0.87** |
| Dribbling penalties | 184 | 0.23 (0.58) | 0–3.0 | 2.87 (0.18) | 8.81 (0.36) | 7 | 0.14 (0.38) | 0.62 | 0.65 |
| Catching accuracy | 187 | 0.27 (0.26) | 0–1.0 | 0.99 (0.18) | 0.28 (0.36) | 16 | 0.07 (0.24) | −0.16 | 0.98*** |
| Throwing accuracy | 186 | 0.20 (0.19) | 0–1.0 | 1.16 (0.18) | 1.76 (0.36) | 17 | 0.07 (0.23) | −0.13 | 0.94*** |
| Hitting accuracy | 185 | 0.52 (0.23) | 0–1.0 | −0.23 (0.18) | −0.6 (0.36) | 15 | 0.09 (0.25) | −0.02 | 0.95*** |
The total number of assessments given is indicated by n, including pre-and post-treatment time points. Discrepancies are due to missing data (e.g., child had to leave early or did not attend post-treatment session)
All assessments administered across both groups and time points
Number of assessments also coded by an independent second rater
p <0.001,
p <0.01,
p <0.05
Data Analysis
Eleven dependent variables were created: knowledge of basic rules of sports (soccer and tee ball), in vivo game performance (soccer and tee ball), and performance on controlled tasks including the BOTMP, kicking accuracy, trapping accuracy, handball penalties while dribbling, catching accuracy, throwing accuracy, and hitting accuracy. All dependent variables were normally distributed. Data were coded as missing if less than 75 % of the components of a composite measure were present. To address the primary hypothesis of interest, that children who were in treatment improved performance on the outcome measures, a series of one-way analysis of covariance (ANCOVA) models were used. These models were estimated controlling for ADHD subtype, prior medication status, and pre-treatment scores, with treatment (STP vs. no STP) as the grouping factor, and post-treatment scores as the dependent variables. The false discovery rate (FDR) procedure, which has been described as an appropriate correction for Type I error for novel research questions (Benjamini and Hochberg 1995), was used to evaluate statistical significance. Finally, parent improvement ratings were examined using 2 (Group: STP vs. No STP) × 3 (Improvement: Worse vs. No Change vs. Improved) Pearson’s chi-square tests.
Impact of Treatment
Descriptive information for dependent measures is shown in Table 3. Children in both groups demonstrated improvement at post-treatment on measures of sports knowledge, tee ball performance, kicking accuracy, and appropriately trapping a soccer ball. Children who attended the STP also demonstrated improvement on measures of soccer performance, the BOTMP, catching accuracy and handball penalties while dribbling. On the hitting accuracy task, mean scores appear to have decreased from pre-to post-treatment for all children.
Table 3.
Dependent variable means and standard deviations by treatment group and assessment time point
| Pre-treatment |
Post-treatment |
||||
|---|---|---|---|---|---|
| n | M(SD) | n | M(SD) | ||
| Knowledge | |||||
| Soccer | STP | 51 | 0.24 (0.15) | 51 | 0.45 (0.20) |
| Control | 39 | 0.23 (0.15) | 40 | 0.25 (0.20) | |
| Tee ball | STP | 52 | 0.52 (0.24) | 52 | 0.72 (0.21) |
| Control | 39 | 0.40 (0.24) | 39 | 0.47 (0.21) | |
| Performance | |||||
| Soccer | STP | 51 | 0.83 (0.17) | 51 | 0.89 (0.16) |
| Control | 39 | 0.81 (0.17) | 40 | 0.76 (0.16) | |
| Tee ball | STP | 52 | 0.52 (0.21) | 52 | 0.70 (0.19) |
| Control | 38 | 0.47 (0.21) | 39 | 0.51 (0.19) | |
| Controlled tasks | |||||
| BOTMP | STP | 50 | 50.46 (10.96) | 49 | 53.86 (10.19) |
| Control | 40 | 49.63 (10.97) | 39 | 47.67 (10.19) | |
| Catching accuracy | STP | 52 | 0.24 (0.22) | 52 | 0.41 (0.27) |
| Control | 43 | 0.23 (0.22) | 40 | 0.19 (0.27) | |
| Throwing accuracy | STP | 52 | 0.18 (0.18) | 52 | 0.25 (0.19) |
| Control | 43 | 0.15 (0.18) | 39 | 0.22 (0.19) | |
| Hitting accuracy | STP | 51 | 0.53 (0.22) | 52 | 0.47 (0.24) |
| Control | 42 | 0.57 (0.22) | 40 | 0.52 (0.23) | |
| Kicking accuracy | STP | 51 | 0.32 (0.22) | 52 | 0.33 (0.2) |
| Control | 41 | 0.29 (0.22) | 40 | 0.34 (0.2) | |
| Trapping appropriately | STP | 51 | 0.12 (0.17) | 52 | 0.36 (0.27) |
| Control | 43 | 0.12 (0.17) | 40 | 0.18 (0.27) | |
| Dribbling penalties a | STP | 50 | 0.34 (0.64) | 52 | 0.06 (0.48) |
| Control | 42 | 0.26 (0.64) | 40 | 0.30 (0.49) | |
STP Attended Summer Treatment Program, Control Did not attend Summer Treatment Program
Lower scores indicate improved performance
As shown in Table 4, when controlling for pre-treatment scores, ADHD subtype, and prior medication status, children who attended the STP demonstrated greater proficiency on assessments of sport knowledge and performance for both soccer and tee ball at post-treatment as compared to children who did not attend the STP. In addition, children who attended the STP scored higher at post-treatment on the BOTMP, suggesting greater improvements in gross and fine motor skills. Children in the treatment group also improved significantly more than children not attending the STP on trapping appropriately, reducing handball penalties while dribbling, and catching accuracy. There were no differences between groups on kicking, throwing, or hitting accuracy.
Table 4.
Results of ANCOVA models controlling for baseline scores, ADHD subtype, and prior medication status
| STP | Control/No STP | ||||
|---|---|---|---|---|---|
| M (SE) | M (SE) | F(df) | p | ηp2 | |
| Knowledge | |||||
| Soccer | 0.46 (0.05) | 0.25 (0.05) | F(1, 81) =26.90 | 0.000b | 0.250 |
| Tee ball | 0.75 (0.06) | 0.50 (0.06) | F(1,83) =26.62 | 0.000b | 0.243 |
| Performance | |||||
| Soccer | 0.94 (0.04) | 0.83 (0.04) | F(1,81) =10.13 | 0.002b | 0.111 |
| Tee ball | 0.74 (0.05) | 0.56 (0.05) | F(1,82) =17.85 | 0.000b | 0.179 |
| Controlled tasks | |||||
| BOTMP | 53.82 (2.07) | 49.26 (2.04) | F(1,77) =6.56 | 0.012b | 0.080 |
| Kicking accuracy | 0.28 (0.05) | 0.32 (0.05) | F(1,82) =0.95 | 0.332 | 0.011 |
| Trapping appropriately | 0.42 (0.07) | 0.26 (07) | F(1,84) =7.34 | 0.008b | 0.080 |
| Dribbling penalties a | −0.12 (0.13) | 0.16 (0.12) | F(1,82) =7.23 | 0.009b | 0.081 |
| Catching accuracy | 0.44 (0.06) | 0.26 (0.06) | F(1,85) =11.95 | 0.001b | 0.123 |
| Throwing accuracy | 0.24 (0.05) | 0.24 (0.05) | F(1,84) =0.001 | 0.979 | 0.000 |
| Hitting accuracy | 0.35 (0.06) | 0.42 (0.06) | F(1,83) =2.12 | 0.149 | 0.025 |
Effect of treatment group on post-treatment dependent variable controlling for baseline performance on measure
ADHD subtype, and prior medication status, M estimated marginal mean, SE standard error
Lower scores indicate improved performance
Significant after controlling Type I Error using the FDR procedure
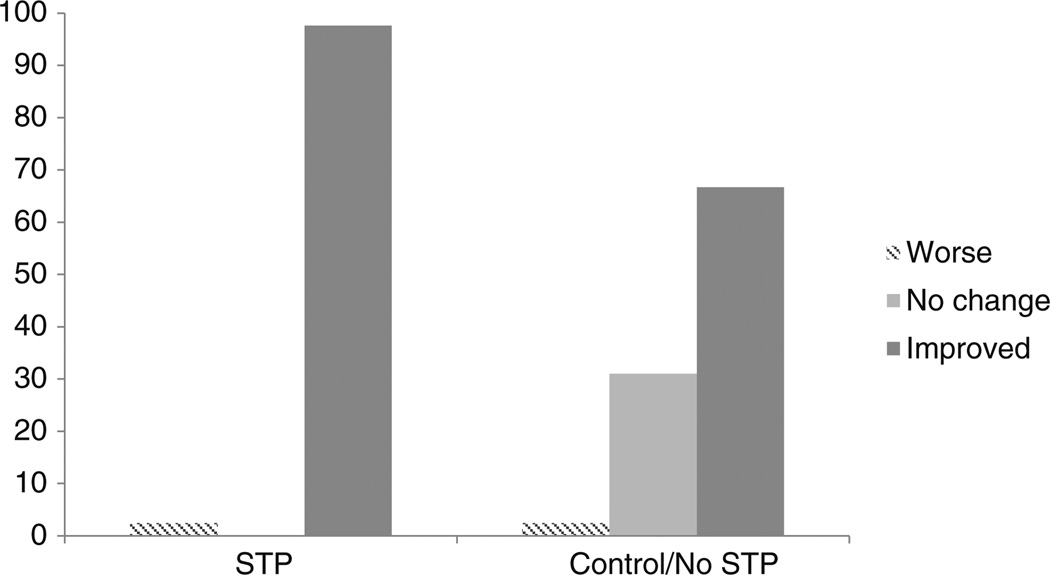
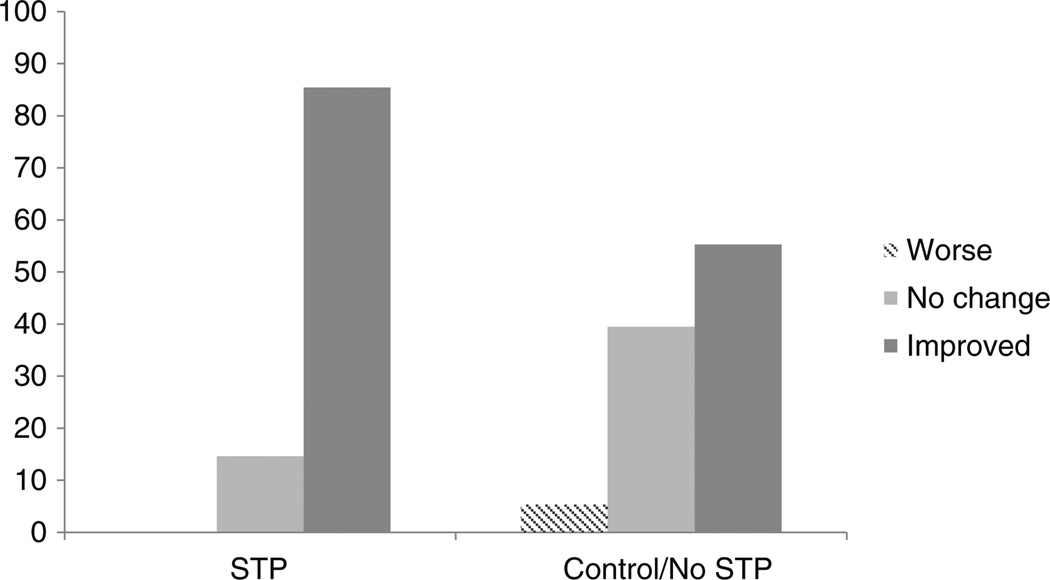
Parent ratings suggested that children attending the STP improved significantly more than children who did not attend the STP on both specific sports skills; χ2 (2)=15.45, p <0.001 (see Fig. 1), and good sportsmanship; χ2 (2)=9.26, p <0.05 (see Fig. 2).
Fig. 1.
Parent ratings of children’s improvement in sports skills. Notes: Percent of responses for “how much your child has improved over this summer in sports skills” for parents of children who attended the STP, compared to parents of children who did not attend (Control/No STP)
Fig. 2.
Parent ratings of children’s improvement in good sportsmanship. Notes: Percent of responses for “how much your child has improved over this summer in good sportsmanship” for parents of children who attended the STP, compared to parents of children who did not attend (Control/No STP)
Discussion
The results of the current study corroborate previous research suggesting that behavioral interventions implemented in a sports context can significantly improve sports functioning in children with ADHD (Hupp and Reitman 1999; O’Callaghan et al. 2003; Reitman et al. 2001). Children who attended the STP demonstrated significantly greater improvements on several functional measures of sports outcomes, relative to children who did not attend the STP. Specifically, the treatment group showed significantly greater improvements on measures of game knowledge and in vivo game performance tasks for soccer and tee-ball, motor proficiency (as measured by the BOTMP), appropriately trapping a soccer ball, reducing the number of handball penalties while dribbling a soccer ball, and catching a baseball. Children in the treatment group were also rated by their parents as significantly more improved than children in the comparison group on specific sports skills and good sportsmanship behavior. However, between groups differences were not found on measures of accurately kicking a soccer ball, accurately throwing a baseball, or hitting a baseball off a tee.
Children who attended the STP were able to correctly answer significantly more rule/fundamental knowledge questions at post-treatment. Correct responses on the knowledge tasks reflect better understanding of how to make appropriate plays and avoid committing errors and penalties; each of which contribute to team success. Youth athletes who are better able to articulate facts and strategies also tend to be better able to respond appropriately to game situations, plan for possible actions, and predict subsequent game scenarios (Thomas et al. 1986). Thus, gaining knowledge of rules and fundamentals may play a role in improving performance and may increase the willingness of peers to want children with ADHD to play in active games and to be on their team.
In the current study, the treatment group’s significant improvements on measures of in vivo game performance demonstrated similar trends as their gains in sport rule knowledge. The performance assessments primarily targeted specific capabilities associated with committing fewer errors (e.g., handballs in soccer, failure to run to first base after hitting in tee ball). Reduction of errors is highly relevant to appropriate team play, as youth athletes place a strong emphasis on their peers’ competence and rate of errors (Vazou et al. 2005). Interestingly, children’s performance on some components of the in vivo assessments may warrant future explorations of whether game strategy was also improved at post-treatment. For example, in the tee ball task, attempting the nearest out on the lead runner as opposed to holding the ball or attempting to make a less advantageous out was deemed an indication of better overall strategy (e.g., American Sport Education Program 2007). Though a more thorough evaluation would clearly be needed to determine whether improved game strategy could be reliably demonstrated, the combination of improved rule awareness and game performance as indicated by the measures in the current study supports other work suggesting increased knowledge may be associated with superior team performance and more complex game awareness (Thomas et al. 1986).
Improvements on several of the controlled tasks also suggest better game performance at post-treatment for the STP group. For example, BOTMP results confirmed that children who attended the STP performed significantly better than the comparison group on overall motor proficiency. Skilled motor movements are a necessary foundation of sport performance (e.g., Scmidt and Wrisberg 2000), and, not surprisingly, children who score higher on standardized assessments of motor proficiency often also perform sport-specific tasks in a more skilled manner (Harvey et al. 2007). In addition, children with ADHD tend to demonstrate poor motor performance (see Harvey and Reid 2003). It is encouraging, therefore, that a relatively brief intervention was able to significantly improve motor performance.
Of note, the BOTMP scores in the current sample were normally distributed. This is in contrast to many studies that find positively skewed motor proficiency scores in children with ADHD (e.g., Harvey et al. 2007; Beyer 1999). It is possible that children in the current study are too young to evidence sizeable discrepancies, though deficits have been demonstrated in similarly young children (e.g., Harvey et al. 2007). Also, as others have noted (Goulardins et al. 2013; Harvey and Reid 2003), variability in motor performance deficits may be a key feature of children with ADHD, such that there is a subset of children for whom motor performance (or particular aspects of motor performance) is impaired, while other children with ADHD may excel at sports and evidence normative levels of motor proficiency.
Further improvements for children attending the STP were seen in controlled tasks of catching a baseball, reducing handball penalties while dribbling a soccer ball, and appropriately trapping a soccer ball passed to them. Arguably, success at each of these skills requires specific instruction, such as how to hold the glove open and put the opposite hand over the ball after catching. In contrast, between group differences were not evident for kicking accuracy, throwing accuracy, or hitting baseballs off a tee. Lack of differences in these skills may be attributed to maturation and development of motor skills. Specifically, given the young age of the children in the current study, it may be that those skills that require greater strength or coordination of multiple motor processes may require additional time or practice to develop. For example, it is generally accepted that most typically developing children will perform fundamental movement skills in a mature pattern by the age of approximately 10 years (Burton and Miller 1998).
Finally, parent ratings further substantiate our finding that notable gains were made over the short duration of the program. It is particularly notable that the improvements for children in the STP group made in the sports arena were substantial enough to be noticed by their parents. Additionally, while children in the STP spent a portion of each day in academic activities and children in the comparison group may have spent the summer in active play or day camps, greater gains were still evident for the treatment group.
Taken together, the results of the current study indicate that children who attended the STP improved significantly more than children who did not attend treatment on several measures of sports functioning. As reviewed above, improved sports functioning is important for children with ADHD due to their risk for poor physical fitness and impairments in peer relationships. That the STP results in improvements across a number of behavioral and social domains is well-established (e.g., Pelham et al. 2013; Pelham et al. 2005a; Pelham and Hoza 1996). It may be that improvements in the sports context are one pathway through which broader social and behavioral improvements occur, as proficiency in sports involves adhering to structured rules, cooperating and communicating effectively with peers, and prolonged attention to a task. In fact, facility with athletic recreational games has been shown to predict positive outcomes such as improved school adjustment, greater social competence and peer acceptance, and decreased problem behaviors (Causgrove Dunn et al. 2007; Howie et al. 2010; Lopez-Williams et al. 2005; Pellegrini et al. 2004; Weiss and Duncan 1992).
Furthermore, behavioral interventions that target direct teaching of prosocial and sportsmanlike behaviors in children with ADHD in the context of a sport activity or game setting have also been successful (Hupp et al. 2002; Hupp and Reitman 1999; O’Callaghan et al. 2003). Some studies suggest that the prosocial behaviors learned in a sports setting may even generalize to other settings (Hupp et al. 2002; Hupp and Reitman 1999), though maybe to a lesser degree (O’Callaghan et al. 2003). One key feature of generalization may be to include parents in a coaching role (Reitman et al. 2005). For example, as parents learn important parenting skills, appropriate behavioral interventions may be incorporated into the coaching of children, and parents can reinforce prosocial behaviors outside of the sports setting (e.g., Fabiano et al. 2009). Since many children with ADHD experience impaired social relationships (see McQuade and Hoza 2008), the potential impact of sports participation on social competence for these children cannot be overemphasized.
Clearly, there is potential to intervene in clinically meaningful ways with children with ADHD in the sports setting. Appropriate sports involvement may be a useful context in which to teach the value of rule following, consequences, and the benefits of prosocial behaviors. In the current study, treatment was primarily behavioral, though a small proportion of children who were medicated prior to the STP were also being treated with stimulant medication during the summer. Though future studies should further investigate the impact of combined behavioral and pharmacological interventions, medication was not expected to play a large part in affecting the performance of either group (Pelham et al. 1990). First, the majority of studies exploring the role of methylphenidate on motor performance do not reliably demonstrate improvements (Beyer 1999; Harvey et al. 2007; Harvey and Reid 1997; Hefley and Gorman 1986; Pelham et al. 1990). In the few studies that have shown moderate improvements, increases in individual performance have been attributed to increased attention to task demands and behavioral inhibition (Doyle et al. 1995; Pelham et al. 1990; Reitman et al. 2001; Stray et al. 2009). However, it is unclear whether these improvements sufficiently address the myriad of sports performance deficits exhibited by children with ADHD (e.g., Harvey et al. 2007; Pelham et al. 1990).
There are several limitations of the current study. First, without a control group of children without a diagnosis of ADHD, the degree to which treatment improved skills to a level comparable to typically developing children is not known, with the exception of the standardized BOTMP. Similarly, the current study did not assess for DCD, a comorbidity which may represent a subset of youth with more severe motor impairments (Kadesjo and Gillberg 1999). In addition, we do not have data about the type and duration of activities children not enrolled in the STP participated in during the summer. If, for example, they spent a majority of the summer in sedentary activities (e.g., watching television and playing video games), increases in motor skills would not be expected. Additionally, it was not possible to conduct blinded assessments, as this was an ongoing study and staff were familiar with the children and their treatment condition. Given the concrete nature of the measures (e.g., ball hit the target or did not), as well as the reliability between independent raters, bias due to knowledge of group assignment is not believed to be an issue. The exception to this may be parent reports; however, parent ratings showed the same pattern of improvements as objective measures of sports functioning. Another limitation is that several of the measures were created specifically for this study. Though reliability of the measures was acceptable (see Table 2) and the measures adhere to suggestions and similar situation-based assessments described elsewhere (Thomas et al. 1986), future replication and validation of these novel measures is needed. Specifically, staff requirements for several of the assessments (e.g., in vivo measures) precluded a higher percentage of trials being observed and rated for reliability. Finally, though all children were unmedicated during the assessments, a small percentage of children were receiving concurrent stimulant medication treatment prior to the current study. Though the goal of the current study was to evaluate the impact of the STP on sports functioning in addition to any concurrent treatments the child was receiving, this limitation is common among studies of ADHD and physical activity (Harvey and Reid 2005) and should be addressed in future replications.
It is also important to note that the STP consisted of intensive behavioral treatment delivered in the context of a typical camp day, including 3 h of sports instruction, practice, and coaching. The current study cannot parse out the degree to which sports instruction or behavioral intervention were necessary agents of change. Future replications may shed light on this distinction by evaluating outcomes for youth who attend intensive sport-specific camps or programs that do not directly target ADHD symptoms and impairments. However, since behavioral treatment facilitates skill acquisition and performance in a classroom setting (Pffifner and Barkley 1998), it is likely that improvements in sports functioning demonstrated by the treatment group may also have been due to effective behavioral interventions potentiating sport skill acquisition. Furthermore, behavioral components of the STP are designed to increase on task behavior and reduce disruptive behavior, both of which likely contributed to a more conducive learning environment.
Additional future directions following from the current study include a more longitudinal design, whereby the impact of improved performance on subsequent sports participation can be measured. Specifically, future research should determine whether gains evident in the current study are sustained. In addition, it will be important to evaluate whether participation in the STP increases self-esteem and physical activity self-efficacy of children with ADHD and whether it promotes greater participation in unorganized and organized team sports outside of the treatment program. Given the positive association between sports participation and social impairment, future studies should also explore the extent to which improved sports functioning has a direct impact on improved social skills in youth with ADHD. Similarly, children with ADHD may garner benefits from extracurricular activities outside of sports (Bluechardt and Shephard 1995), so the impact of participating in other activities on social impairment should also be assessed. Studies might also investigate in a well-controlled fashion how these procedures implemented over the summer could be effectively integrated into school or community programs (e.g., Lufi and Parish-Plass 2011). Finally, including a control group of typically developing children could be important for developing a more comprehensive picture of how children with ADHD differ in their sports participation and performance.
In summary, the current study represents a controlled evaluation of the impact of the Summer Treatment Program on young children’s sports functioning across a number of measures. The results suggest that behavioral treatment has a significant impact on many domains of sports functioning. Sports participation is a very common activity for children that is often positive and may provide an opportunity for intervention for children with ADHD to address specific impairments, such as motor proficiency and social functioning. As treatment for children with ADHD progresses, the sports setting may be a valuable component of treatment that addresses multiple domains of functioning and impairment.
Acknowledgments
This research was funded by a grant from the National Institute of Mental Health (MH069614). Dr. Pelham was also supported in part by grants from (MH069434, MH092466, MH53554, MH065899, MH62988), the Institute of Education Sciences (R324B060045, R324J060024, LO30000665A), the National Institute of Alcohol Abuse and Alcoholism (AA11873), and the National Institute on Drug Abuse (DA12414, DA12986).
Footnotes
For children who were not yet enrolled in school, daycare providers, or someone with knowledge of the child’s behavior outside of the home, completed the rating forms.
Contributor Information
Briannon C. O’Connor, Department of Psychology, State University of New York at Buffalo, 206 Park Hall, Buffalo, NY 14260, USA, bco@buffalo.edu
Gregory A. Fabiano, Department of Counseling, School and Educational Psychology, State University at Buffalo, Buffalo, NY, USA
Daniel A. Waschbusch, Center for Children and Families, Department of Psychology, Florida International University, Miami, FL, USA
Peter J. Belin, Center for Children and Families, Department of Psychology, Florida International University, Miami, FL, USA
Elizabeth M. Gnagy, Center for Children and Families, Department of Psychology, Florida International University, Miami, FL, USA
William E. Pelham, Center for Children and Families, Department of Psychology, Florida International University, Miami, FL, USA
Andrew R. Greiner, Center for Children and Families, Department of Psychology, Florida International University, Miami, FL, USA
James N. Roemmich, USDA, ARS, Grand Forks Human Nutrition Center, Grand Forks, ND 58203, USA
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 2000. Text Revision. [Google Scholar]
- American Sport Education Program (Ed.) Coaching youth baseball. Human Kinetics; 2007. [Google Scholar]
- Ayaz AB, Ayaz M, Yazgan Y, Akın E. The relationship between motor coordination and social behavior problems in adolescents with attention-deficit/hyperactivity disorder. Bulletin of Clinical Psychopharmacology. 2013;23:33–41. [Google Scholar]
- Bagwell CL, Schmidt ME, Newcomb AF, Bukowski WM. Friendship and peer rejection as predictors of adult adjustment. In: Nangle DW, Erdley CA, editors. The role of friendship in psychological adjustment. San Francisco: Jossey-Bass; 2001. pp. 25–49. [Google Scholar]
- Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. Journal of the Royal Statistical Society, Series B. 1995:289–300. [Google Scholar]
- Beyer R. Motor proficiency of boys with attention deficit hyper-activity disorder and boys with learning disabilities. Adapted Physical Activity Quarterly. 1999;16:403–414. [Google Scholar]
- Beyer R, Flores MM, Vargas-Tonsing TM. Coaches’ attitudes towards youth sport participants with attention deficit hyperactivity disorder. International Journal of Sports Science & Coaching. 2008;3:555–563. [Google Scholar]
- Bluechardt MH, Shephard RJ. Using an extracurricular physical activity program to enhance social skills. Journal of Learning Disabilities. 1995;28:160–169. doi: 10.1177/002221949502800305. [DOI] [PubMed] [Google Scholar]
- Bouffard M, Watkinson EJ, Thompson LP, Causgrove Dunn JL, Romanow SKE. A test of the activity deficit hypothesis with children with movement difficulties. Adapted Physical Activity Quarterly. 1996;13:61–73. [Google Scholar]
- Bruininks RH. Bruininks-Oseretsky test of motor proficiency: Examiner’s manual. Circle Pines: American Guidance Service; 1978. [Google Scholar]
- Burton AW, Miller DE. Movement skill assessment. Champaign: Human Kinetics; 1998. [Google Scholar]
- Causgrove Dunn J, Dunn JG, Bayduza A. Perceived athletic competence, sociometric status, and loneliness in elementary school children. Journal of Sport Behavior. 2007;30:249–269. [Google Scholar]
- Center for Disease Control. 2008 Physical activity guidelines for Americans. 2008 Retrieved from: http://www.health.gov/paguidelines/guidelines/default.asp#toc.
- Cortese S, Angriman M. Attention-deficit/hyperactivity disorder and obesity: moving to the next research generation. Pediatrics. 2008;122:1155. doi: 10.1542/peds.2008-2225. [DOI] [PubMed] [Google Scholar]
- Dishman RK, Sallis JF, Orenstein DR. The determinants of physical activity and exercise. Public Health Reports. 1985;100:158–171. [PMC free article] [PubMed] [Google Scholar]
- Doyle S, Wallen M, Whitmont S. Motor skills in Australian children with attention deficit hyperactivity disorder. Occupational Therapy International. 1995;2:229–240. [Google Scholar]
- Fabiano GA, Pelham WE, Waschbusch DA, Gnagy EM, Lahey BB, Chronis AM, Burrows-MacLean L. A practical measure of impairment: Psychometric properties of the Impairment Rating Scale in samples of children with attention deficit hyperactivity disorder and two school-based samples. Journal of Clinical Child and Adolescent Psychology. 2006;35:369–385. doi: 10.1207/s15374424jccp3503_3. [DOI] [PubMed] [Google Scholar]
- Fabiano GA, Chacko A, Pelham WE, Robb J, Walker KS, Wymbs F, Pirvics L. A comparison of behavioral parent training programs for fathers of children with attention-deficit/hyperactivity disorder. Behavior Therapy. 2009;40:190–204. doi: 10.1016/j.beth.2008.05.002. [DOI] [PubMed] [Google Scholar]
- Fraser-Thomas J, Côté J. Youth sports: implementing findings and moving forward with research. Athletic Insight: The Online Journal of Sport Psychology. 2006;8:1–14. [Google Scholar]
- Goulardins JB, Marques JCB, Casella EB, Nascimento RO, Oliveira JA. Motor profile of children with attention deficit hyperactivity disorder, combined type. Research in Developmental Disabilities. 2013;34:40–45. doi: 10.1016/j.ridd.2012.07.014. [DOI] [PubMed] [Google Scholar]
- Gross AM, Johnson TC. Athletic skill and social status in children. Journal of Social & Clinical Psychology. 1984;2:89–96. [Google Scholar]
- Gross AM, Johnson TC, Wojnilower DA, Drabman RS. The relationship between sports fitness training and social status in children. Behavioral Engineering. 1985;9:58–65. [Google Scholar]
- Guevremont DC, Dumas MC. Peer relationship problems and disruptive behavior disorders. Journal of Emotional and Behavioral Disorders. 1994;2:164–172. [Google Scholar]
- Haas SM, Waschbusch DA, Pelham WE, King S, Andrade BF, Carrey NJ. Treatment response in CP/ADHD children with callous/unemotional traits. Journal of Abnormal Child Psychology. 2011;39:541–552. doi: 10.1007/s10802-010-9480-4. [DOI] [PubMed] [Google Scholar]
- Hands B. Changes in motor skill and fitness measures among children with high and low motor competence: a 5-year longitudinal study. Journal of Science and Medicine in Sport. 2008;11:155–162. doi: 10.1016/j.jsams.2007.02.012. [DOI] [PubMed] [Google Scholar]
- Harvey WJ, Reid G. Motor performance of children with attention-deficit hyperactivity disorder: a preliminary investigation. Adapted Physical Activity Quarterly. 1997;14:189–202. [Google Scholar]
- Harvey WJ, Reid G. Attention-deficit/hyperactivity disorder: a review of research on movement skill performance and physical fitness. Adapted Physical Activity Quarterly. 2003;20:1–25. [Google Scholar]
- Harvey WJ, Reid G. Attention-deficit/hyperactivity disorder: APA research challenges. Adapted Physical Activity Quarterly. 2005;22:1–20. [Google Scholar]
- Harvey WJ, Reid G, Grizenko N, Mbekou V, Ter-Stepanian M, Joober R. Fundamental movement skills and children with attention-deficit hyperactivity disorder: peer comparisons and stimulant effects. Journal of Abnormal Child Psychology. 2007;35:871–882. doi: 10.1007/s10802-007-9140-5. [DOI] [PubMed] [Google Scholar]
- Harvey WJ, Reid G, Bloom GA, Staples K, Grizenko N, Mbekou V, Joober R. Physical activity experiences of boys with and without ADHD. Adapted Physical Activity Quarterly. 2009;26:131–150. doi: 10.1123/apaq.26.2.131. [DOI] [PubMed] [Google Scholar]
- Hefley RD, Gorman DR. Psychomotor performance of medicated and nonmedicated hyperactive emotionally handicapped children and normal children. American Corrective Therapy Journal. 1986;40:85–90. [Google Scholar]
- Howie LD, Lukacs SL, Pastor PN, Reuben CA, Mendola P. Participation in activities outside of school hours in relation to problem behavior and social skills in middle childhood. Journal of School Health. 2010;80:119–125. doi: 10.1111/j.1746-1561.2009.00475.x. [DOI] [PubMed] [Google Scholar]
- Hoza B, Gerdes AC, Mrug S, Hinshaw SP, Bukowski WM, Gold JA, et al. Peer-assessed outcomes in the multimodal treatment study of children with attention deficit hyperactivity disorder. Journal of Clinical Child and Adolescent Psychology. 2005;34:74–86. doi: 10.1207/s15374424jccp3401_7. [DOI] [PubMed] [Google Scholar]
- Hupp SD, Reitman D. Improving sports skills and sportsmanship in children diagnosed with attention-deficit/hyperactivity disorder. Child & Family Behavior Therapy. 1999;21:35–51. [Google Scholar]
- Hupp SD, Reitman D, Northup J, O’Callaghan P, LeBlanc M. The effects of delayed rewards, tokens, and stimulant medication on sportsmanlike behavior with ADHD-diagnosed children. Behavior Modification. 2002;26:148–162. doi: 10.1177/0145445502026002002. [DOI] [PubMed] [Google Scholar]
- Johnson RC, Rosen LA. Sports behavior of ADHD children. Journal of Attention Disorders. 2000;40:150–160. [Google Scholar]
- Kadesjo B, Gillberg C. Developmental coordination disorder in Swedish 7-year-old children. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38:820–828. doi: 10.1097/00004583-199907000-00011. [DOI] [PubMed] [Google Scholar]
- Lopez-Williams A, Chacko A, Wymbs BT, Onyango AN, Fabiano GA, Seymour, et al. Athletic performance and social behavior as predictors of peer acceptance in children diagnosed with attention-deficit hyperactivity disorder. Journal of Emotional and Behavioral Disorders. 2005;13:173–180. [Google Scholar]
- Lufi D, Parish-Plass J. Sport-based group therapy program for boys with ADHD or with other behavioral disorders. Child and Family Behavior Therapy. 2011;33:217–230. [Google Scholar]
- Martin NC, Piek JP, Hay D. DCD and ADHD: a genetic study of their shared aetiology. Human Movement Science. 2006;25:110–124. doi: 10.1016/j.humov.2005.10.006. [DOI] [PubMed] [Google Scholar]
- McQuade JD, Hoza B. Peer problems in attention deficit hyperactivity disorder: Current status and future directions. Developmental Disabilities Research Reviews. 2008;14:320–324. doi: 10.1002/ddrr.35. Special issue: ADHD and modifiers of the syndrome: Influences on educational outcomes. [DOI] [PubMed] [Google Scholar]
- National Center for Education Statistics. After school programs and activities: 2005. 2005 Retrieved from: http://nces.ed.gov/pubs2006/ afterschool/index.asp.
- Newcomb AF, Bukowski WM, Pattee L. Children’s peer relations: a meta-analytic review of popular, rejected, neglected, controversial, and average sociometric status. Psychological Bulletin. 1993;113:99–128. doi: 10.1037/0033-2909.113.1.99. [DOI] [PubMed] [Google Scholar]
- O’Callaghan PN, Reitman D, Northup J, Hupp SDA, Murphy MA. Promoting social skills generalization with ADHD-diagnosed children in a sports setting. Behavior Therapy. 2003;34:313–330. [Google Scholar]
- Parker JG, Asher SR. Peer relations and later personal adjustment: are low accepted children at risk? Psychological Bulletin. 1987;102:357–389. doi: 10.1037//0033-2909.102.3.357. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Bender ME. Peer relationships in hyperactive children: Description and treatment. Advances in Learning & Behavioral Disabilities. 1982;1:365–436. [Google Scholar]
- Pelham WE, Fabiano GA. Evidence-based psychosocial treatments for attentiondeficit/hyperactivity disorder. Journal of Clinical Child and Adolescent Psychology. 2008;37:184–214. doi: 10.1080/15374410701818681. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Hoza B. Intensive treatment: A summer treatment program for children with ADHD. In: Hibbs E, Jensen P, editors. Psychosocial treatments for child and adolescent disorders: Empirically based strategies for clinical practice. New York: APA Press; 1996. pp. 311–340. [Google Scholar]
- Pelham WE, McBurnett K, Harper GW, Murphy DA, Milich R, Clinton J, Thiele C. Methylphenidate and baseball playing in ADHD children: Who’s on first? Journal of Consulting and Clinical Psychology. 1990;58:130–133. doi: 10.1037/0022-006X.58.1.130. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Gnagy EM, Greenslade KE, Milich R. Teacher ratings of DSM-III—R symptoms for the disruptive behavior disorders. Journal of the American Academy of Child & Adolescent Psychiatry. 1992;31:210–218. doi: 10.1097/00004583-199203000-00006. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Fabiano GA, Gnagy EM, Greiner AR, Hoza B. The role of Summer Treatment Programs in the context of comprehensive treatment for attention-deficit/hyperactivity disorder. In: Hibbs ED, Jensen PS, editors. Psychosocial treatments for child and adolescent disorders: Empirically based strategies for clinical practice. 2nd ed. Washington: American Psychological Association; 2005a. pp. 377–409. [Google Scholar]
- Pelham WE, Fabiano GA, Massetti GM. Evidence-based assessment of attention deficit hyperactivity disorder in children and adolescents. Journal of Clinical Child and Adolescent Psychology. 2005b;34:449–476. doi: 10.1207/s15374424jccp3403_5. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Gnagy EM, Greiner AR, Waschbusch DA, Fabiano GA, Burrows-MacLean L. Summer treatment programs for attention deficit/hyperactivity disorder. In: Kazdin AE, Weisz JR, editors. Evidence-basedpsychotherapies for children and adolescents. 2nd ed. New York: Guilford Press; 2010. [Google Scholar]
- Pelham WE, Burrows-MacLean L, Gnagy EM, Fabiano GA, Coles EK, Wymbs BT, Waschbusch DA. A dose-ranging study of behavioral and pharmacological treatment in social-recreational settings for children with ADHD. Journal of Abnormal Child Psychology. 2013 doi: 10.1007/s10802-013-9843-8. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pellegrini AD, Kato K, Blatchford P, Baines E. A short-term longitudinal study of children’s playground games across the first year of school: implications for social competence and adjustment to school. American Educational Research Journal. 2004;39:991–1015. [Google Scholar]
- Pffifner LJ, Barkley RA. Treatment of ADHD in school settings. In: Barkley RA, editor. Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment. 2nd ed. New York: Guilford; 1998. pp. 458–490. [Google Scholar]
- Reitman D, Hupp SDA, O’Callaghan PM, Gulley V, Northup J. The influence of a token economy and methylphenidate on attentive and disruptive behavior during sports with ADHD-diagnosed children. Behavior Modification. 2001;25:305–323. doi: 10.1177/0145445501252007. [DOI] [PubMed] [Google Scholar]
- Reitman D, O’Callaghan PM, Mitchell P. Parent as coach: enhancing sports participation and social behavior for ADHD-diagnosed children. Child & Family Behavior Therapy. 2005;27:57–68. [Google Scholar]
- Schmidt A, Wrisberg CA. Motor learning and performance. 2nd ed. Champaign: Human Kinetics; 2000. [Google Scholar]
- Sharpe T, Brown M, Crider K. The effects of a sportsmanship curriculum intervention on generalized positive social behavior of urban elementary school students. Journal of Applied Behavior Analysis. 1995;28:401–416. doi: 10.1901/jaba.1995.28-401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smoll FL, Smith RE, Barnett NP, Everett JJ. Enhancement of children’s self-esteem through social support training for youth sport coaches. Journal of Applied Psychology. 1993;78:602–610. doi: 10.1037/0021-9010.78.4.602. [DOI] [PubMed] [Google Scholar]
- Snow S, Dorrance A. Coaching youth soccer. Human Kinetics; 2011. [Google Scholar]
- Sothern MS, Loftin M, Suskind RM, Udall JN, Blecker U. The health benefits of physical activity in children and adolescents: implications for chronic disease prevention. European Journal of Pediatrics. 1999;158:271–274. doi: 10.1007/s004310051070. [DOI] [PubMed] [Google Scholar]
- Stray LL, Stray T, Iversen S, Ruud A, Ellertsen B, Tønnessen FE. Methylphenidate improves motor functions in children diagnosed with hyperkinetic disorder. Behavioral and Brain Functions. 2009;5 doi: 10.1186/1744-9081-5-21. ArtID 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas JR, French KE, Humphries CA. Knowledge development and sport skill performance: directions for motor behavior research. Journal of Sport Psychology. 1986;8:259–272. [Google Scholar]
- Vazou S, Ntoumanis N, Duda JL. Peer motivational climate in youth sport: a qualitative inquiry. Psychology of Sport and Exercise. 2005;6:497–516. [Google Scholar]
- Verret C, Guay MC, Berthiaume C, Gardiner P, Béliveau L. A physical activity program improves behavior and cognitive functions in children with ADHD an exploratory study. Journal of Attention Disorders. 2012;16:71–80. doi: 10.1177/1087054710379735. [DOI] [PubMed] [Google Scholar]
- Weiss MR, Duncan SC. The relationship between physical competence and peer acceptance in the context of children’s sports participation. Journal of Sport & Exercise Psychology. 1992;14:177–191. [Google Scholar]
- Wrotniak BH, Epstein LH, Dorn JM, Jones KE, Kondilis VA. The relationship between motor proficiency and physical activity in children. Pediatrics. 2009;118:e1758–e1765. doi: 10.1542/peds.2006-0742. [DOI] [PubMed] [Google Scholar]