Abstract
Objective
To evaluate the effectiveness of a worksite health promotion program on improving cardiovascular disease risk factors.
Methods
In St Louis, Missouri from 2005 to 2006, 151 employees (134 F, 17 M, 81% overweight/obese) participated in a cohort-randomized trial comparing assessments + intervention (worksite A) with assessments only (worksite B) for 1 year. All participants received personal health reports containing their assessment results. The intervention was designed to promote physical activity and favorable dietary patterns using pedometers, healthy snack cart, WeightWatchers® meetings, group exercise classes, seminars, team competitions, and participation rewards. Outcomes included BMI, body composition, blood pressure, fitness, lipids, and Framingham 10-year coronary heart disease risk.
Results
123 participants, aged 45 ± 9 yr, with BMI 32.9 ± 8.8 kg/m2 completed 1 year. Improvements (P ≤ 0.05) were observed at both worksites for fitness, blood pressure, and total-, HDL-, and LDL-cholesterol. Additional improvements occurred at worksite A in BMI, fat mass, Framingham risk score, and prevalence of the metabolic syndrome; only the changes in BMI and fat mass were different between worksites.
Conclusion
A multi-faceted worksite intervention promoted favorable changes in cardiovascular disease risk factors, but many of the improvements were achieved with worksite health assessments and personalized health reports in the absence of an intervention.
Keywords: Health promotion, Physical activity, Diet, Weight, Pedometer, Fitness
Introduction
Obesity is a major public health problem in the United States because of its high prevalence (Flegal et al., 2002), causal relationship with serious medical illnesses (Allison et al., 1999; Hu et al., 2001; Hubert et al.,1983; Manson et al.,1990), economic impact, and negative effects on work performance (Pronk et al., 2004). In 2003, the National Business Group on Health established The Institute on the Costs and Health Effects of Obesity, with a core objective being to “propose innovative solutions that large employers can implement to control costs related to lifestyle-related behaviors” (National Business Group on Health, 2008). The worksite offers a unique setting to implement health promotion programs and provides an ideal opportunity to engage large numbers of individuals in a very efficient and cost-effective manner (Hennrikus and Jeffery, 1996; Kumanyika et al., 2002).
There is substantial evidence from several large-scale, prospective, longitudinal studies, such as the Framingham Heart Study (Grundy et al., 1998), Diabetes Prevention Program (Diabetes Prevention Program Research Group, 2002), Multiple Risk Factor Intervention Trial (Leon et al., 1997), and the Nurses' Health Study (Stampfer et al., 2000), that improving dietary habits and/or increasing physical activity can effectively reduce risks for developing cardiovascular diseases and type 2 diabetes, thereby enhancing overall health. Exercise also provides psychological benefits and enhances quality of life (LaCroix et al., 1993). Therefore, a worksite health promotion program that is feasible, enjoyable, and effective may have significant benefits not only for employees, but for employers and society as well.
A variety of worksite interventions have been implemented, with most assessing the feasibility of environmental changes (Biener et al., 1999) or relatively short-term changes in dietary (Beresford et al., 2001; French et al., 2001; Jeffery et al.,1993,1994; Tilley et al.,1999) or physical activity (Emmons et al., 1999) patterns. Several worksite programs included an evaluation of cardiovascular disease risk factors, some of which lasted more than 6 months (Engbers et al., 2007; Gemson et al., 2008; Glasgow et al., 1995, 1997; Naito et al., 2008), but the results were variable. In the present study, we implemented a novel, 1-year worksite intervention called “Worksite Opportunities for Wellness” (WOW) among medical center employees and compared it to an assessment only condition that included personalized health reports. We hypothesized that our WOW intervention would be feasible and effective for reducing the prevalence or severity of obesity and cardiovascular disease risk factors.
Methods
Eligible subjects included females and males 18 years of age and older who were employed at 1 of 2 selected worksites within a large medical center in St. Louis, Missouri, USA. We recruited subjects during an informational presentation about the study at each worksite, as well as with flyers and email messages. All employees were eligible, including those who smoked, had pre-existing disease (e.g., hypertension, diabetes), or used medications, but medication use was documented at each assessment time point. The target for enrollment was 150 subjects (75 per worksite), which represented approximately 46% of the employee population at these worksites. This sample size was deemed optimal to detect a 2 kg difference in body weight between worksites, with power of 0.80, significance of 0.05, and 15% attrition. Enrollment of each cohort was conducted within 1 week. All applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during this research. The study was approved by the Human Studies Committee of Washington University School of Medicine, and written informed consent was obtained from each employee before enrollment.
After enrollment, baseline health assessments were performed in 2005 at each worksite in the fasted state in the morning, and included measures of height, weight, waist circumference, body composition, resting heart rate, blood pressure, fasting lipids and glucose, and cardiovascular fitness, as described below. All measurements were made by a team of trained investigators and research staff, and were repeated after 1 year.
Body weight was measured in triplicate to the nearest 0.1 kg on an electronic scale after the removal of shoes, sweaters, belts, jewelry, and items from pockets. Height was measured without shoes to the nearest 0.1 cm using a portable stadiometer. Body mass index (BMI) was calculated by dividing body weight in kilograms by height in meters squared (kg/m2) (U.S. Department of Health and Human Services, 1998). Waist circumference was measured with a Gulick II tape measure at the superior border of the iliac crest (National Institutes of Health et al., 2000) over bare skin or minimal clothing.
Fat mass and fat-free mass were estimated using bioelectrical impedance analysis (BIA, RJL BIA-Quantum II, Clinton Township, MI) (Kushner, 1992), which is portable, fast, and feasible at worksites, and which has been shown to be valid and reliable in many populations (Kotler et al., 1996; Segal et al., 1985). After electrodes were placed on the right hand, wrist, foot, and ankle in the right ipsilateral configuration, resistance and reactance were measured in triplicate with the subject in the supine position. A comparison of 222 body composition results obtained with this BIA machine and with dual-energy X-ray absorptiometry as part of another study (Racette et al., 2006) revealed significant correlations between the 2 methods for both whole-body fat mass (r = 0.932, P < 0.01) and % fat mass (r = 0.942, P < 0.01, unpublished data).
Resting heart rate was assessed in duplicate by palpating a radial artery for 30 s after the subject had been seated quietly for 10 min. Blood pressure (BP) was measured in duplicate, with 2 min between measurements, after the subject had been seated quietly for 10 min (Chobanian et al., 2003). An appropriately-sized cuff was placed on the subject's right arm and a mercury sphygmomanometer was used to measure systolic and diastolic BP. Cardiorespiratory fitness was estimated based upon heart rate recovery after a 3-minute step test performed with an 8-inch step and a metronome set to 96 beats per min (Montoye et al., 1969). Subjects were instructed to maintain the pace of the metronome for 3 min unless cardiovascular symptoms, pain, or fatigue precluded completion. One minute after completion of the test, the subject's pulse was measured for 10 s, multiplied by 6, and used to determine the percentile rank for recovery heart rate and fitness category based upon sex and age.
A venous blood sample was drawn to determine total cholesterol, HDL-cholesterol, LDL-cholesterol, triglycerides, and fasting plasma glucose concentration. Analyses were performed in the Barnes-Jewish Hospital Laboratory. Total cholesterol and glycerol-blanked triglycerides were measured by automated enzymatic commercial kits. HDL-cholesterol was measured in serum after precipitation of apo B-containing lipoproteins by dextran sulfate and magnesium. LDL-cholesterol was calculated using the Friedewald equation (Friedewald et al., 1972). Plasma glucose concentration was measured using hexokinase reagents.
The Framingham Coronary Heart Disease (CHD) Risk Score was calculated according to the National Cholesterol Education Program (NCEP) Adult Treatment Panel III (ATP III) guidelines (Expert Panel on Detection, 2001) at baseline and 1 year to estimate each subject's 10-year risk for CHD (i.e., the probability of having a CHD event within 10 years). The algorithm is sex-specific and assigns points based upon categorical values for age, total cholesterol, HDL-cholesterol, systolic BP, pharmacologic treatment for hypertension, and cigarette smoking. The points were summed to derive the total score for each participant, and the corresponding 10-year risk percentage was calculated. Subjects were classified as low risk (<2 risk factors), moderate risk (≥ 2 risk factors and <10% risk), moderate-high risk (10–20% risk), or high risk (>20% risk) (Gillespie et al., 2007).
The presence of the metabolic syndrome was based upon the NCEP ATP III definition (Expert Panel on Detection, 2001), which requires at least 3 of the following risk factors to be present: abdominal obesity (waist circumference >102 cm in men, >88 cm in women); elevated triglycerides (≥ 150 mg/dL); low HDL-cholesterol (<40 mg/dL in men, <50 mg/dL in women); elevated BP (systolic BP ≥ 130 mm Hg or diastolic BP ≥ 85 mm Hg); and elevated fasting glucose (≥ 100 mg/dL, based upon the recent recommendations of the American Diabetes Association (American Diabetes Association, 2008)).
Dietary and physical activity patterns were estimated using the National Institutes of Health Fruit and Vegetable Screener (Thompson et al., 2000), the Kristal Fat and Fiber Behavior Questionnaire (Kristal et al., 1990, 2000), and the International Physical Activity Questionnaire (IPAQ) (Booth, 2000; Craig et al., 2003). Reported reliability estimates for the latter two instruments were 0.63 and 0.80, respectively. Subjects also completed a medication form, listing the name and dose of drugs they were taking, along with starting and ending dates. These questionnaires were administered at baseline, 6 months, and 1 year.
After baseline health assessments were completed, the worksites were randomized to either Assessments + Intervention (worksite A) or Assessments Only (worksite B) for 1 year. Subjects were notified of their site's randomization status by the WOW worksite coordinator employed at each site. Members of the research team distributed WOW Personal Health Reports (containing individualized assessment results) to each participant. The WOW intervention commenced with a kick-off event at worksite A and was comprised of a constellation of nutrition components, physical activity components, and incentives designed to promote healthy dietary and physical activity behaviors, with the goals of promoting weight control and reducing risk factors for cardiovascular disease. The theoretical framework was the Transtheoretical Model of Behavior Change (Prochaska and DiClemente, 1983), which posits that individuals vary in their readiness to adopt a healthy behavior or to cease an unhealthy one. Although the intervention was not individually tailored to each subject's stage of readiness, the array of intervention components was designed to address the different stages of readiness that subjects were in, and to help them progress to more advanced stages.
Specific intervention components included pedometers, weekly healthy snack cart, on-site WeightWatchers® group meetings, on-site group exercise program, monthly lunchtime seminars, monthly newsletters, walking maps, team competitions, participation cards, and participation rewards. Each week a registered dietitian/exercise specialist was available at the worksite to hand out new material, punch participation cards, give rewards, measure blood pressure, and discuss individual health questions. Rewards included kitchen gadgets and exercise gear of varying value, which were given upon completion of each 20-punch participation card. An employee advisory committee guided and facilitated delivery of the intervention.
Statistical analyses
Analyses were performed using Statistical Analysis Software (SAS Institute, Cary, NC, version 9.1). The effects of site over time were explored first by fitting two separate doubly multivariate ANOVA models (Timm and Mieczkowski, 1997). The first model explored the relationship between site over time for five anthropometric measures (BMI, weight, fat mass, fat-free mass, percentage fat mass) while controlling for smoking status and use of weight-affecting drugs. The second model explored differences between sites over time for 4 groups of CHD risk factors (resting and recovery heart rate, blood pressure, lipids, fasting glucose), while controlling for smoking status and use of anti-diabetic, anti-hypertensive, and lipid-lowering drugs. A list of drug classes that were included in the 4 drug categories is provided in Table 1. Medication use was used as a proxy of pre-existing conditions; therefore, pre-existing conditions were not included as covariates in order to avoid redundancy.
Table 1.
Drug categories and drugs used by participants.
| Anti-diabetic | Anti-hypertensive | Lipid-lowering | Weight-affecting |
|---|---|---|---|
| Alpha-glucosidase inhibitor | ACE inhibitor | Anti-lipemic | Anti-depressant |
| Biguanide | Alpha blocker | Bile acid resin | Anti-anxiety |
| Insulin | Angiotensin II antagonist | Cholesterol absorption inhibitor | Appetite suppressant |
| Meglitinide | Beta blocker | Fibric acid derivative | Anti-convulsant |
| Sulfonylurea | Calcium channel blocker | HMG-CoA reductase inhibitor | Anti-diabetic |
| Diuretic | Lipid-lowering | Corticosteroid | |
| Hormone |
In both ANOVA models, multiple indices (anthropometric measures and CHD risk factors) were assessed for participants (multivariate) repeated across two time points (doubly multivariate). For each effect in the doubly multivariate ANOVA model we report the Pillai's trace test statistic because it is the most robust and conservative multivariate statistic (Tabachnick and Fidell, 2007); significance of effects is determined assuming a Type I error rate of 5%. Significant multivariate effects were then explored via a series of univariate repeated measures ANOVAs derived via general linear mixed models (i.e., Proc Mixed in SAS) with a type-I error rate fixed at 0.05. These models used the same controlling variables as the corresponding doubly multivariate model. This approach results in a conservative overall experiment- wise error rate that does not exceed that specified for the multivariate analysis. In all cases, primary emphasis involved testing the interaction between time (baseline vs. 1-year) and worksite (A vs. B) in the general linear mixed model. In cases where no significant interaction was found, we explored differences over time averaged across the worksites.
The assessment of changes in categorical and dichotomous variables over time within each worksite was made using an exact version of McNemar's test (Fleiss et al., 2003). The analysis of changes in Framingham CHD Risk categorization was simplified to examining differences in the proportion of participants who were classified as ‘low risk’ versus all other higher risk categories combined due to the sparse nature of the higher risk categories. Differences between worksites in the proportion of participants having a binary characteristic of interest at the 1-year time point were assessed using logistic regression, with site as the between-subject factor and the baseline proportion with the particular characteristic as a fixed time-invariant covariate.
Results
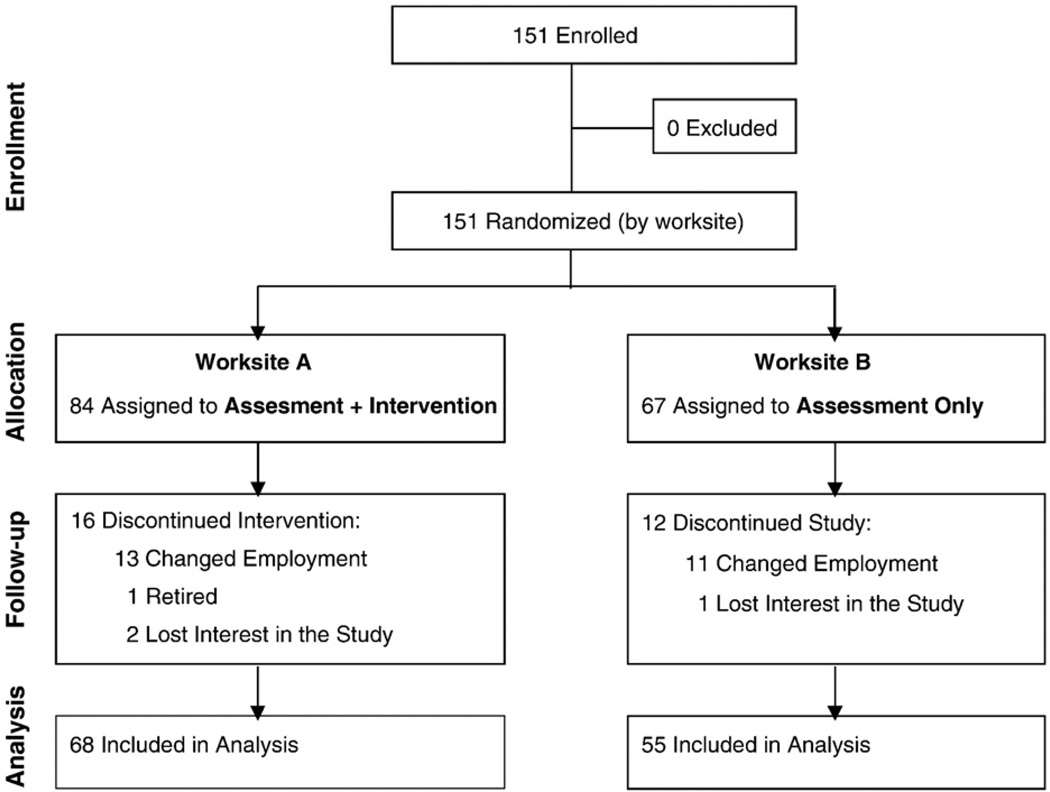
Subjects included 151 employees (134F, 17M). The disproportionate number of females is reflective of the sex distribution at our worksites. There were more African Americans at worksite A (42%) than at worksite B (15%, P < 0.01), and more college graduates at worksite B (70%) than at worksite A (37%), but the sites were matched on sex and age. During the year-long study, 16 of 84 subjects at worksite A and 12 of 67 subjects at worksite B were lost to follow-up and therefore did not have final measures (Fig. 1). Attrition was predominantly due to subjects changing employment or retiring. No adverse events occurred. A total of 123 subjects (108F, 15M; 68 at worksite A, 55 at worksite B) completed all measures and are included in these analyses.
Fig. 1.
Flow of participants through the trial.
The mean age of participants upon enrollment was 45 ± 9 years (range 25–64 years). At baseline, 81% of subjects were classified as either obese (i.e., BMI ≥ 30.0 kg/m2, 58% of subjects) or overweight (i.e., BMI 25.0–29.9 kg/m2, 23% of subjects); the average BMI was 32.9 ± 8.8 kg/m2. Anthropometric results by worksite are shown in Table 2. BMI and other measures of adiposity were significantly higher among employees at worksite A than at worksite B at baseline. The doubly multivariate ANOVA revealed a significant time-by-site interaction (Pilai's Trace = 0.082; F(4,112) = 2.48; P = 0.048). Univariate repeated measures models revealed that reductions in body weight, BMI, and fat mass were greater for worksite A (Assessments + Intervention) than for worksite B (Assessments Only), as shown in Table 2.
Table 2.
Anthropometric results at baseline and after 1 year among 123 employees (St. Louis, MO, USA, 2005–2006).
| Outcome | Worksite Aa (Assessment + Intervention) |
Worksite Ba (Assessment Only) |
P value between sitesb |
95% confidence interval for changes from baseline to 1 year between sitesc |
||
|---|---|---|---|---|---|---|
| Baseline | 1 year | Baseline | 1 year | |||
| N | 68 | 68 | 55 | 55 | ||
| Weight (kg) | 92.4 (24.9) | 91.6 (25.5) | 84.5 (20.9) | 85.1 (23.2) | 0.02 | (−3.90, −0.31) |
| Body mass index (kg/m2) | 34.5 (9.7) | 34.1 (9.8) | 31.1 (7.2) | 31.2 (7.9) | 0.02 | (−1.44, −0.11) |
| % Fat mass | ||||||
| All subjects | 44.8 (11.9) | 44.2 (12.0) | 39.2 (11.9) | 38.7 (12.7) | 0.52 | (−1.44, 0.74) |
| Females | 46.4 (10.5) | 45.9 (10.8) | 43.1 (9.1) | 42.4 (10.8) | ||
| Males | 23.5 (4.3) | 23.4 (2.9) | 21.9 (5.7) | 22.4 (6.1) | ||
| Fat mass (kg) | ||||||
| All subjects | 43.6 (21.7) | 42.9 (22.0) | 33.9 (16.6) | 34.2 (18.3) | 0.04 | (−3.08, −0.05) |
| Females | 45.2 (21.6) | 44.5 (22.0) | 37.0 (16.7) | 37.1 (18.8) | ||
| Males | 22.6 (7.8) | 22.1 (7.1) | 20.7 (7.7) | 21.7 (8.5) | ||
| Fat-free mass (kg) | ||||||
| All subjects | 48.8 (8.6) | 48.8 (8.6) | 49.7 (11.5) | 50.0 (12.1) | 0.04 | (−1.05, −0.12) |
| Females | 47.0 (5.4) | 47.0 (5.4) | 45.1 (4.9) | 45.2 (5.3) | ||
| Males | 71.3 (9.2) | 70.7 (11.2) | 70.1 (9.8) | 71.0 (11.0) | ||
Values represent mean (SD).
Site-by-time interaction.
Smoking status and use of weight-affecting drugs over time were controlled for in the analysis.
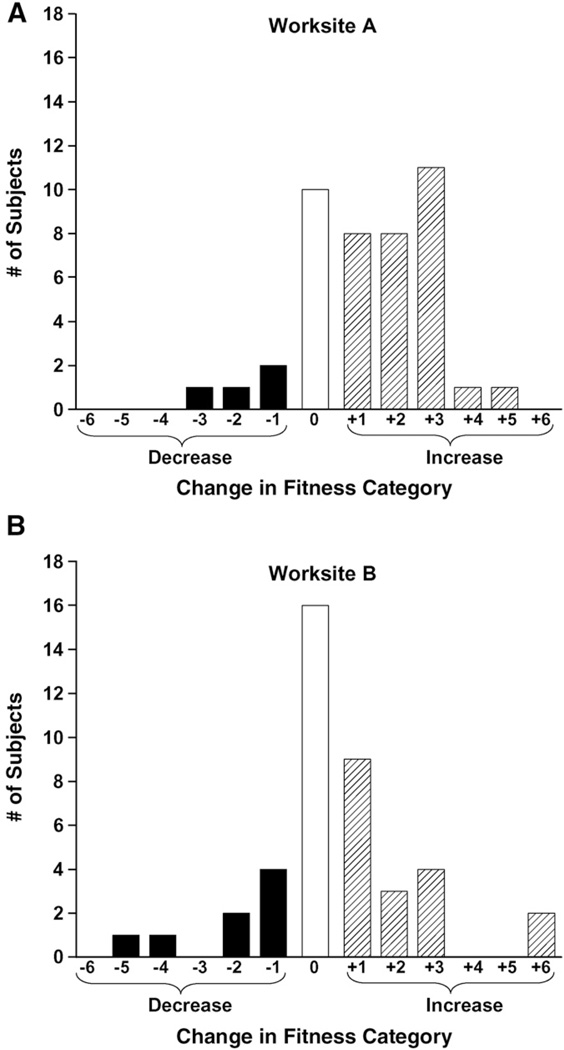
Cardiovascular disease risk factors are shown in Table 3. At baseline, 72% of subjects had elevated blood pressure (i.e., ≥ 120 mm Hg systolic or ≥ 80 mm Hg diastolic) and 75% had at least 1 lipid value outside the desirable range. The doubly multivariate ANOVA revealed a non-significant time-by-site interaction (Pillai's Trace = 0.167; F(10,84) = 1.69; P = 0.097), whereas significant aggregate changes (across worksites) were observed, as indicated by the multivariate effect of time (Pillai's Trace = 0.7016; F(10,84) = 19.75; P < 0.0001). As shown in Table 3, the subsequent univariate repeated measures analysis revealed that the multivariate time effect stemmed from improvements in post-exercise recovery heart rate, systolic and diastolic blood pressure, and all lipid measures except triglycerides. The reduction in post-exercise heart rate reflects an improvement in fitness, as depicted in Fig. 2.
Table 3.
Coronary heart disease (CHD) risk factor measures at baseline and after 1 year among 123 employees (St. Louis, MO, USA, 2005–2006).
| Outcome | Worksite Aa (Assessment + Intervention) |
Worksite Ba (Assessment Only) |
P value for change from baseline to 1 year, aggregated across sites |
95% confidence interval for changes from baseline to 1 year between sitesb |
||
|---|---|---|---|---|---|---|
| Baseline | 1 year | Baseline | 1 year | |||
| Heart rate (bpm) | ||||||
| Resting | 73 (11) | 71 (10) | 71 (9) | 69 (10) | 0.12 | (−3.20, 0.38) |
| Post-exercise recovery | 103 (18) | 93 (16) | 94 (14) | 90 (17) | <0.01 | (−9.79, −4.95) |
| Blood pressure (mm Hg) | ||||||
| Systolic | 127 (19) | 121 (16) | 121 (15) | 116 (18) | <0.01 | (−8.24, −2.96) |
| Diastolic | 84 (11) | 77 (9) | 79 (10) | 75 (11) | <0.01 | (−6.62, −3.44) |
| Lipids (mg/dL) | ||||||
| Total cholesterol | 200 (32) | 192 (32) | 199 (40) | 195 (36) | <0.01 | (−10.05, −2.63) |
| HDL-cholesterol | 56 (16) | 62 (18) | 54 (17) | 61 (18) | <0.01 | (5.41, 8.38) |
| LDL-cholesterol | 121 (27) | 106 (26) | 121 (35) | 109 (32) | <0.01 | (−17.03, −10.87) |
| Triglycerides | 116 (62) | 118 (60) | 115 (59) | 122 (63) | 0.29 | (−3.60, 12.10) |
| Total cholesterol: HDL ratio | 3.9 (1.1) | 3.3 (1.0) | 3.9 (1.2) | 3.4 (1.0) | <0.01 | (−0.65, −0.46) |
| Fasting glucose (mg/dL) | 96 (20) | 96 (23) | 92 (17) | 96 (20) | 0.21 | (−0.88, 3.97) |
Values represent Mean (SD).
Smoking status and use of anti-diabetic, anti-hypertensive, and lipid-lowering drugs were controlled for in the analysis.
Fig. 2.
Changes in fitness categories from baseline to 1 year among 123 employees (St. Louis, MO, USA, 2005–2006). Worksite A: Assessments + Intervention; Worksite B: Assessments Only. The black bars to the left of 0 reflect the number of subjects who decreased 6, 5, 4, 3, 2, or 1 fitness category; the white bar at 0 indicates those whose fitness did not change; the striped bars to the right of 0 indicate those who increased their fitness by 1, 2, 3, 4, 5, or 6 categories.
Composite disease risk indices are shown in Table 4. For Framingham CHD risk, 40% of worksite A participants were in the lowest risk category at baseline, which increased significantly to 57% at 1 year. The corresponding values for worksite B were 51% at baseline and 60% at 1 year (ns). Smokers comprised 20% of the overall sample at baseline and 18% at 1 year (ns). The metabolic syndrome was present among 38% of subjects at worksite A and 29% of subjects at worksite B at baseline. A significant reduction to 25% of subjects was observed at worksite A, due to improvements in HDL-cholesterol and blood pressure. There was a trend for improvement at worksite B, with 18% of subjects meeting the criteria for the metabolic syndrome at 1 year.
Table 4.
Framingham coronary heart disease (CHD) risk and metabolic syndrome classification at baseline and after 1 year among 123 employees (St. Louis, MO, USA, 2005–2006).
| Outcome | Criteria | Worksite A (Assessment + Intervention) |
Worksite B (Assessment Only) |
P value between sites |
||||
|---|---|---|---|---|---|---|---|---|
| Baseline | 1 year | P value | Baseline | 1 year | P value | |||
| % of Subjects | % of Subjects | |||||||
| Framingham 10 y CHD riska | ||||||||
| Low risk | <2 risk factors | 0.40 | 0.57 | <0.01b | 0.51 | 0.60 | 0.27b | 0.80c |
| Moderate risk | ≥2 risk factors and <10% risk | 0.47 | 0.32 | 0.36 | 0.31 | |||
| Moderate-high risk | 10%–20% risk | 0.04 | 0.03 | 0.05 | 0.04 | |||
| High risk | >20% risk | 0.09 | 0.07 | 0.07 | 0.05 | |||
| Smokers | 0.24 | 0.22 | 0.56 | 0.15 | 0.13 | 0.32 | 0.32 | |
| Metabolic syndrome present | ≥3 risk factors | 0.38 | 0.25 | 0.02 | 0.29 | 0.18 | 0.07 | 0.07 |
| Risk factors: | ||||||||
| Abdominal obesity | WC>88 cm (F), >102 cm (M) | 0.84 | 0.81 | 0.69 | 0.65 | 0.65 | 1.00 | 0.67 |
| High triglycerides | ≥150 mg/dL | 0.25 | 0.24 | 1.00 | 0.24 | 0.24 | 1.00 | 0.89 |
| Low HDL-cholesterol | <50 mg/dL (F), <40 mg/dL (M) | 0.39 | 0.24 | 0.02 | 0.31 | 0.18 | 0.02 | 0.77 |
| High blood pressure | elevated systolic or diastolic | 0.49 | 0.32 | 0.01 | 0.33 | 0.25 | 0.48 | 0.89 |
| Systolic | ≥130 mm Hg | 0.35 | 0.28 | 0.23 | 0.22 | 0.16 | 0.51 | 0.48 |
| Diastolic | ≥85 mm Hg | 0.41 | 0.16 | 0.00 | 0.27 | 0.20 | 0.45 | 0.29 |
| High fasting glucose | ≥100 mg/dL | 0.27 | 0.21 | 0.39 | 0.24 | 0.24 | 1.00 | 0.51 |
WC = waist circumference, F = female, M = male.
The percentage risk of having a coronary event within 10 years.
Low risk versus all other risk categories combined.
Subjects who remained at low risk or improved >1 risk category.
Based upon the behavioral questionnaires, subjects at worksite A increased their fruit and vegetable consumption from 4.7 servings/day at baseline to 7.8 at 6 months and 7.0 at 1 year (both P < 0.01). They also reported decreasing their intake of saturated fat, fatty meats, and fried foods at 6 months and 1 year (all P < 0.001 vs. baseline). Furthermore, total daily physical activity increased (P < 0.001), which was predominantly due to greater amounts of time spent walking and engaged in other moderate activities (both P < 0.01), but not to an increase in vigorous activities. At worksite B, significant but smaller improvements were observed for fruit and vegetable intake (4.3, 5.3, and 5.1 servings/day at baseline, 6 months, and 1 year, respectively), saturated fat intake, and moderate physical activity.
Discussion
We have demonstrated that a multi-faceted worksite health promotion program was feasible and effective for improving cardiovascular disease risk factors among employees, but that many of the improvements were achieved with worksite health assessments and personalized health reports in the absence of an intervention.
Two observations from the present study are noteworthy. First, improvements occurred in cardiovascular disease risk factors after 1 year even in the absence of dramatic weight loss. Although many subjects at worksite A did lose weight, some regained the weight they had lost during the first 6 months, some were weight stable throughout the study, and others gained weight (particularly at worksite B). Therefore, despite remaining obese or overweight, many subjects made behavioral changes that contributed to clinically meaningful health improvements. These findings highlight the value of lifestyle modifications in individuals who have been unsuccessful in losing weight or maintaining long-term weight loss.
A second important finding was that participation in the Assessment Only condition, which involved annual health assessments and cumulative Personal Health Reports, was sufficient to initiate behavior changes that produced modest health benefits. This phenomenon of health improvements in the absence of a comprehensive intervention was not surprising because the health professionals on our research team raised awareness by providing individualized results with an accompanying packet describing the significance of the health indices that we assessed. In addition, participants had the opportunity to ask individual questions about their results during the distribution session. Although this personalized feedback may have minimized our intervention effects, we believe it was important from an ethical perspective to inform subjects of their health measures and disease risk factors. Furthermore, we provided the same feedback to both worksites, so the impact of the assessments and Personal Health Reports should have been similar across sites. The significance of this finding is that worksites which lack the resources or personnel to offer a comprehensive intervention may have an opportunity to enhance employee health through assessments alone. As expected, the improvements observed at the Assessment Only worksite generally were more modest than at the Intervention worksite.
Our results are in agreement with those of Nilsson et al. (2001), who observed modest risk improvements among female employees in Sweden after 18 months. Relatively few previous worksite intervention studies included an assessment of cardiovascular disease risk factors over a long period of time (Aldana et al., 2005; Engbers et al., 2007; Gemson et al., 2008; Glasgow et al., 1995, 1997; Naito et al., 2008; Nilsson et al., 2001; Shimizu et al., 2004), even fewer were conducted in the United States (Aldana et al., 2005; Gemson et al., 2008; Glasgow et al., 1995, 1997), and the results were sometimes negative (Glasgow et al., 1995, 1997), despite careful study designs and large sample sizes. One important difference between studies that may help to explain the discrepant findings is that the larger Take Heart trials (Glasgow et al., 1995, 1997) involved numerous worksites, with high variability between worksites in terms of response to the interventions, and their analysis was at the level of the worksite rather than the individual. Other differences between studies that make it difficult to compare efficacy include subject characteristics, type of worksite, specific intervention components, intervention duration, and assessment methodology.
A potential confounder of the present study was medication use. Because our goal was to promote health awareness and favorable behavior changes that would reduce cardiovascular disease risk, it was neither realistic nor desirable to exclude employees who were taking medications. Importantly, there were no significant changes in medication use at either worksite throughout the study, and medication use was controlled for in the analyses. A notable limitation is the low percentage of males in our target worksites and therefore in our sample, which limits the generalizability of our findings. In addition, feasibility and cost precluded the use of extensive dietary interviews and accelerometers, and, our study did not include return-on-investment analyses, which is an important area for future investigation.
Despite the limitations of self-reported behavioral data, our questionnaire results help to explain the physiological changes that we observed. Specifically, the increase in fruit and vegetable consumption and the decrease in saturated fat, fried food, and fast food consumption at worksite A help to explain the observed improvements in blood pressure and lipid concentrations. These benefits are consistent with results of the DASH (i.e., Dietary Approaches to Stop Hypertension) diet studies (Appel et al., 1997; Sacks et al., 2001; Obarzanek et al., 2001), and are the reason that the DASH eating plan (U.S. Department of Health and Human Services, 2006) is recommended in the current Dietary Guidelines for Americans (U.S. Department of Health and Human Services and U.S. Department of Agriculture, 2005). Furthermore, our observation in the present study that moderate physical activities such as walking promoted higher fitness levels is in agreement with previous intervention studies (Duncan et al., 1991; Dunn et al., 1999; Murphy et al., 2007) and observational studies (Blair and Brodney, 1999).
Finally, we had an overall attrition rate of 18.5%, which was due predominantly to participants changing employment, with only 2% of subjects dropping out of the study while still employed at the worksites. Elements which we believe enhanced participation and promoted retention were the program's convenience, the inclusion of free and reduced-cost intervention activities that were engaging, provision of participation rewards, and social support provided by coworkers. Our employee turnover rate is typical of other worksites, according to the U.S. Department of Labor, Bureau of Labor Statistics, which sites an 18.6% voluntary turnover rate for employees in the field of education and health services (Nobscot Corporation, 2006). Attrition from worksite health promotion programs lasting 6 months or longer is often higher than what we observed, with estimates of 6% (Aldana et al., 2005), 21% (Nilsson et al., 2001), and up to ≥ 50% (Blair et al., 1986; Glasgow et al., 1995, 1997).
Conclusions
In summary, our multi-component worksite intervention was associated with significant improvements in cardiovascular disease risk factors and physical fitness among employees, but many of the health benefits appeared to be attributable to the health assessments and personalized feedback rather than the intervention. Conducting annual health assessments and providing personalized health reports are important steps that many employers should take to enhance the health of their employees.
Acknowledgments
We thank Laura Weber, MS RD, for creating the monthly newsletters; DPT students in the Program in Physical Therapy at Washington University School of Medicine for their assistance with data collection, intervention delivery, and data entry; and our subjects for their participation and enthusiasm.
This study was funded by CDC R01 DP000092 (location of grant support: Saint Louis/Missouri/USA).
Footnotes
Conflict of interest statement
The authors declare that there are no conflicts of interest.
References
- Aldana SG, Greenlaw RL, Diehl HA, Salberg A, Merrill RM, Ohmine S. The effects of a worksite chronic disease prevention program. J. Occup. Environ. Med. 2005;47:558–564. doi: 10.1097/01.jom.0000165743.18570.66. [DOI] [PubMed] [Google Scholar]
- Allison DB, Fontaine KR, Manson JE, Stevens J, VanItallie TB. Annual deaths attributable to obesity in the United States. JAMA. 1999;282:1530–1538. doi: 10.1001/jama.282.16.1530. [DOI] [PubMed] [Google Scholar]
- American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2008;31(Suppl. 1):S55–S60. doi: 10.2337/dc08-S055. [DOI] [PubMed] [Google Scholar]
- Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N. Engl. J. Med. 1997;336:1117–1124. doi: 10.1056/NEJM199704173361601. [DOI] [PubMed] [Google Scholar]
- Beresford SA, Thompson B, Feng Z, Christianson A, McLerran D, Patrick DL. Seattle 5 a Day worksite program to increase fruit and vegetable consumption. Prev. Med. 2001;32:230–238. doi: 10.1006/pmed.2000.0806. [DOI] [PubMed] [Google Scholar]
- Biener L, Glanz K, McLerran D, et al. Impact of the Working Well Trial on the worksite smoking and nutrition environment. Health Educ. Behav. 1999;26:478–494. doi: 10.1177/109019819902600407. [DOI] [PubMed] [Google Scholar]
- Blair SN, Brodney S. Effects of physical inactivity and obesity on morbidity and mortality: current evidence and research issues. Med. Sci. Sports Exerc. 1999;31:S646–S662. doi: 10.1097/00005768-199911001-00025. [DOI] [PubMed] [Google Scholar]
- Blair SN, Piserchia PV, Wilbur CS, Crowder JH. A public health intervention model for work-site health promotion. Impact on exercise and physical fitness in a health promotion plan after 24 months. JAMA. 1986;255:921–926. [PubMed] [Google Scholar]
- Booth M. Assessment of physical activity: an international perspective. Res. Q. Exerc. Sport. 2000;71:S114–S120. [PubMed] [Google Scholar]
- Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- Craig CL, Marshall AL, Sjostrom M, et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003;35:1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N. Engl. J. Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan JJ, Gordon NF, Scott CB. Women walking for health and fitness. How much is enough. JAMA. 1991;266:3295–3299. [PubMed] [Google Scholar]
- Dunn AL, Marcus BH, Kampert JB, Garcia ME, Kohl HW, Blair SN. Comparison of lifestyle and structured interventions to increase physical activity and cardiorespiratory fitness. JAMA. 1999;281:327–334. doi: 10.1001/jama.281.4.327. [DOI] [PubMed] [Google Scholar]
- Emmons KM, Linnan LA, Shadel WG, Marcus B, Abrams DB. The Working Healthy Project: a worksite health-promotion trial targeting physical activity, diet, and smoking. J. Occup. Environ. Med. 1999;41:545–555. doi: 10.1097/00043764-199907000-00003. [DOI] [PubMed] [Google Scholar]
- Engbers LH, van Poppel MN, Van Mechelen W. Modest effects of a controlled worksite environmental intervention on cardiovascular risk in office workers. Prev. Med. 2007;44:356–362. doi: 10.1016/j.ypmed.2006.11.005. [DOI] [PubMed] [Google Scholar]
- Expert Panel on Detection. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999–2000. JAMA. 2002;288:1723–1727. doi: 10.1001/jama.288.14.1723. [DOI] [PubMed] [Google Scholar]
- Fleiss JL, Levin B, Paik MY. Statistical Methods for Rates and Proportions. New Jersey: Wiley; 2003. [Google Scholar]
- French SA, Jeffery RW, Story M, et al. Pricing and promotion effects on low-fat vending snack purchases: the CHIPS Study. Am. J. Public Health. 2001;91:112–117. doi: 10.2105/ajph.91.1.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin. Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- Gemson DH, Commisso R, Fuente J, Newman J, Benson S. Promoting weight loss and blood pressure control at work: impact of an education and intervention program. J. Occup. Environ. Med. 2008;50:272–281. doi: 10.1097/JOM.0b013e318162f628. [DOI] [PubMed] [Google Scholar]
- Gillespie MJ, Davis CJ, Lambert ND, et al. Measuring and treating serum lipids in patients in a chest pain observation unit. Am. J. Cardiol. 2007;99:1718–1720. doi: 10.1016/j.amjcard.2007.01.061. [DOI] [PubMed] [Google Scholar]
- Glasgow RE, Terborg JR, Hollis JF, Severson HH, Boles SM. Take heart: results from the initial phase of a work-site wellness program. Am. J. Public Health. 1995;85:209–216. doi: 10.2105/ajph.85.2.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasgow RE, Terborg JR, Strycker LA, Boles SM, Hollis JF. Take Heart II: replication of a worksite health promotion trial. J. Behav. Med. 1997;20:143–161. doi: 10.1023/a:1025578627362. [DOI] [PubMed] [Google Scholar]
- Grundy SM, Balady GJ, Criqui MH, et al. Primary prevention of coronary heart disease: guidance from Framingham. A statement for healthcare professionals from the AHA task force on risk reduction. Circulation. 1998;97:1876–1887. doi: 10.1161/01.cir.97.18.1876. [DOI] [PubMed] [Google Scholar]
- Hennrikus DJ, Jeffery RW. Worksite intervention for weight control: a review of the literature. Am. J. Health Promot. 1996;10:471–498. doi: 10.4278/0890-1171-10.6.471. [DOI] [PubMed] [Google Scholar]
- Hu FB, Manson JE, Stampfer MJ, et al. Diet, lifestyle, and the risk of type 2 diabetes mellitus in women. N. Engl. J. Med. 2001;345:790–797. doi: 10.1056/NEJMoa010492. [DOI] [PubMed] [Google Scholar]
- Hubert HB, Feinleib M, McNamara PM, Castelli WP. Obesity as an independent risk factor for cardiovascular disease: a 26-year follow-up of participants in the Framingham Heart Study. Circulation. 1983;67:968–977. doi: 10.1161/01.cir.67.5.968. [DOI] [PubMed] [Google Scholar]
- Jeffery RW, Forster JL, French SA, et al. The Healthy Worker Project: a worksite intervention for weight control and smoking cessation. Am. J. Public Health. 1993;83:395–401. doi: 10.2105/ajph.83.3.395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeffery RW, French SA, Raether C, Baxter JE. An environmental intervention to increase fruit and salad purchases in a cafeteria. Prev. Med. 1994;23:788–792. doi: 10.1006/pmed.1994.1135. [DOI] [PubMed] [Google Scholar]
- Kotler DP, Burastero S, Wang J, Pierson RN., Jr Prediction of body cell mass, fat-free mass, and total body water with bioelectrical impedance analysis: effects of race, sex, disease. Am. J. Clin. Nutr. 1996;64:489S–497S. doi: 10.1093/ajcn/64.3.489S. [DOI] [PubMed] [Google Scholar]
- Kristal AR, Shattuck AL, Henry HJ. Patterns of dietary behavior associated with selecting diets low in fat: reliability and validity of a behavioral approach to dietary assessment. J. Am. Diet Assoc. 1990;90:214–220. [PubMed] [Google Scholar]
- Kristal AR, Curry SJ, Shattuck AL, Feng Z, Li S. A randomized trial of a tailored, self-help dietary intervention: the Puget Sound Eating Patterns study. Prev. Med. 2000;31:380–389. doi: 10.1006/pmed.2000.0711. [DOI] [PubMed] [Google Scholar]
- Kumanyika S, Jeffery RW, Morabia A, Ritenbaugh C, Antipatis VJ. Obesity prevention: the case for action. Int. J. Obes. Relat. Metab. Disord. 2002;26:425–436. doi: 10.1038/sj.ijo.0801938. [DOI] [PubMed] [Google Scholar]
- Kushner RF. Bioelectrical impedance analysis: a review of principles and applications. J. Am. Coll. Nutr. 1992;11:199–209. [PubMed] [Google Scholar]
- LaCroix AZ, Guralnik JM, Berkman LF, Wallace RB, Satterfield S. Maintaining mobility in late life. II. Smoking, alcohol consumption, physical activity, and body mass index. Am. J. Epidemiol. 1993;137:858–869. doi: 10.1093/oxfordjournals.aje.a116747. [DOI] [PubMed] [Google Scholar]
- Leon AS, Myers MJ, Connett J. Leisure time physical activity and the 16-year risks of mortality from coronary heart disease and all-causes in the Multiple Risk Factor Intervention Trial (MRFIT) Int. J. Sports Med. 1997;18:S208–S215. doi: 10.1055/s-2007-972717. [DOI] [PubMed] [Google Scholar]
- Manson JE, Colditz GA, Stampfer MJ. A prospective study of obesity and risk for coronary heart disease in women. N. Engl. J. Med. 1990;322:882–918. doi: 10.1056/NEJM199003293221303. [DOI] [PubMed] [Google Scholar]
- Montoye HJ, Willis PW, III, Cunningham DA, Keller JB. Heart rate response to a modified Harvard step test: males and females, age 10–69. Res. Q. 1969;40:153–162. [PubMed] [Google Scholar]
- Murphy MH, Nevill AM, Murtagh EM, Holder RL. The effect of walking on fitness, fatness and resting blood pressure: a meta-analysis of randomised, controlled trials. Prev. Med. 2007;44:377–385. doi: 10.1016/j.ypmed.2006.12.008. [DOI] [PubMed] [Google Scholar]
- Naito M, Nakayama T, Okamura T, et al. Effect of a 4-year workplace-based physical activity intervention program on the blood lipid profiles of participating employees: the high-risk and population strategy for occupational health promotion (HIPOP-OHP) study. Atherosclerosis. 2008;197:784–790. doi: 10.1016/j.atherosclerosis.2007.07.026. [DOI] [PubMed] [Google Scholar]
- National Business Group on Health. Institute on the Costs and Health Effects of Obesity. 2008 [Google Scholar]
- National Institutes of Health, National Heart Lung and Blood Institute, North American Association for the Study of Obesity. U.S. Department of Health and Human Services, Public Health Service, National Institutes of Health, National Heart, Lung, and Blood Institute; 2000. The Practical Guide; Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. NIH Publication Number 00-4084. [Google Scholar]
- Nilsson PM, Klasson EB, Nyberg P. Life-style intervention at the worksite—reduction of cardiovascular risk factors in a randomized study. Scand. J. Work Environ. Health. 2001;27:57–62. doi: 10.5271/sjweh.587. [DOI] [PubMed] [Google Scholar]
- Nobscot Corporation. BLS Employee Turnover Rates, 2006. [Accessed. May. 18, 2008];2006 [Google Scholar]
- Obarzanek E, Sacks FM, Vollmer WM, et al. Effects on blood lipids of a blood pressure-lowering diet: the Dietary Approaches to Stop Hypertension (DASH) Trial. Am. J. Clin. Nutr. 2001;74:80–89. doi: 10.1093/ajcn/74.1.80. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. J. Consult. Clin. Psychol. 1983;51:390–395. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- Pronk NP, Martinson B, Kessler RC, Beck AL, Simon GE, Wang P. The association between work performance and physical activity, cardiorespiratory fitness, and obesity. J. Occup. Environ. Med. 2004;46:19–25. doi: 10.1097/01.jom.0000105910.69449.b7. [DOI] [PubMed] [Google Scholar]
- Racette SB, Weiss EP, Villareal DT, et al. One year of caloric restriction in humans: feasibility and effects on body composition and abdominal adipose tissue. J. Gerontol., A, Biol. Sci. Med. Sci. 2006;61:943–950. doi: 10.1093/gerona/61.9.943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N. Engl. J. Med. 2001;344:3–10. doi: 10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
- Segal KR, Gutin B, Presta E, Wang J, Van Itallie TB. Estimation of human body composition by electrical impedance methods: a comparative study. J. Appl. Physiol. 1985;58:1565–1571. doi: 10.1152/jappl.1985.58.5.1565. [DOI] [PubMed] [Google Scholar]
- Shimizu T, Horiguchi I, Kato T, Nagata S. Relationship between an interview-based health promotion program and cardiovascular risk factors at Japanese companies. J. Occup. Health. 2004;46:205–212. doi: 10.1539/joh.46.205. [DOI] [PubMed] [Google Scholar]
- Stampfer MJ, Hu FB, Manson JE, Rimm EB, Willett WC. Primary prevention of coronary heart disease in women through diet and lifestyle. N. Engl. J. Med. 2000;343:16–22. doi: 10.1056/NEJM200007063430103. [DOI] [PubMed] [Google Scholar]
- Tabachnick B, Fidell L. Using Multivariate Statistics. Boston, MA: Pearson Education; 2007. [Google Scholar]
- Thompson FE, Kipnis V, Subar AF, et al. Evaluation of 2 brief instruments and a food-frequency questionnaire to estimate daily number of servings of fruit and vegetables. Am. J. Clin. Nutr. 2000;71:1503–1510. doi: 10.1093/ajcn/71.6.1503. [DOI] [PubMed] [Google Scholar]
- Tilley BC, Glanz K, Kristal AR, et al. Nutrition intervention for high-risk auto workers: results of the Next Step Trial. Prev. Med. 1999;28:284–292. doi: 10.1006/pmed.1998.0439. [DOI] [PubMed] [Google Scholar]
- Timm N, Mieczkowski T. Univariate and Multivariate General Linear Models: Theory and Applications using SAS Software. Gary, NC: SAS Institute; 1997. [Google Scholar]
- U.S. Department of Health and Human Services. Washington, DC: US DHHS; 1998. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report. 98-4083. [Google Scholar]
- U.S. Department of Health and Human Services and U.S. Department of Agriculture. 6th Edition. Washington: DC, U.S. Government Printing Office; 2005. Dietary Guidelines for Americans, 2005. [Google Scholar]
- U.S. Department of Health and Human Services, National Institutes of Health, National Heart, Lung, and Blood Institute. Your guide to lowering your blood pressure with DASH. [Accessed January 31, 2008];2006 NIH Publication No. 06-4082. Originally Printed 1998, Revised 2006 Available: at http://www.nhlbi.nih.gov/health/public/heart/hbp/dash/new_dash.pdf.