Abstract
Background: Generalized anxiety disorder (GAD) is common in multiple sclerosis (MS) but understudied. Reliable and valid measures are needed to advance clinical care and expand research in this area. The objectives of this study were to examine the psychometric properties of the 7-item Generalized Anxiety Disorder Scale (GAD-7) in individuals with MS and to analyze correlates of GAD.
Methods: Participants (N = 513) completed the anxiety module of the Patient Health Questionnaire (GAD-7). To evaluate psychometric properties of the GAD-7, the sample was randomly split to conduct exploratory and confirmatory factor analyses.
Results: Based on the exploratory factor analysis, a one-factor structure was specified for the confirmatory factor analysis, which showed excellent global fit to the data (χ212 = 15.17, P = .23, comparative fit index = 0.99, root mean square error of approximation = 0.03, standardized root mean square residual = 0.03). The Cronbach alpha (0.75) indicated acceptable internal consistency for the scale. Furthermore, the GAD-7 was highly correlated with the Hospital Anxiety and Depression Scale–Anxiety (r = 0.70). Age and duration of MS were both negatively associated with GAD. Higher GAD-7 scores were observed in women and individuals with secondary progressive MS. Individuals with higher GAD-7 scores also endorsed more depressive symptoms.
Conclusions: These findings support the reliability and internal validity of the GAD-7 for use in MS. Correlational analyses revealed important relationships with demographics, disease course, and depressive symptoms, which suggest the need for further anxiety research.
Multiple sclerosis (MS) is a chronic neurologic disorder that affects the central nervous system and produces physical, cognitive, and psychological symptoms. Most psychological research in MS focuses on the high prevalence of depression1; however, a small body of research suggests that anxiety disorders might be more common.1–3 Unfortunately, anxiety is infrequently studied in MS, and the existing literature is challenging to synthesize owing to a variety of definitional, methodological, and assessment variations.
Anxiety disorders are the predominant mental health condition in the general population and in individuals visiting a medical provider.4,5 Generalized anxiety disorder (GAD) is the most common diagnosis and is characterized by excessive and persistent anxiety and worry.6 The point prevalence is approximately 6.2% in the general population7 and 8% in primary care.8 Among individuals with MS, the point prevalence is as high as 19%.9
In MS, GAD is associated with confirmed exacerbations, pseudo-exacerbations,10 poor medication adherence,11 overuse of health-care services, and lower quality of life.12 Suicide, suicidal ideation, and self-harm are also associated with GAD in MS.13 Although there are no treatment studies specifically for GAD in MS,14 successful remission of symptoms was demonstrated in primary-care patients.15 Therefore, early detection through screening for GAD symptoms may lead to improved treatment and long-term outcomes via earlier initiation of pharmacologic or behavioral interventions.
Until relatively recently, there was an absence of validated, brief screening instruments for GAD in the general population and primary care. The 7-item Generalized Anxiety Disorder Scale (GAD-7) was developed to fill this gap, serving as a brief questionnaire based on the GAD criteria found in the Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition, Text Revision) (DSM-IV-TR).6 This measure was validated in primary-care patients and further in international populations,16 the general population,17 psychiatric populations,18 and geriatric populations.19 Although the GAD-7 is used in MS,20 the psychometrics of the measure have not been evaluated.
Given the high occurrence and impact of GAD on individuals with MS, it would be useful to examine the utility of GAD screening instruments for clinical and research purposes in this population. To our knowledge, there is no validated screening measure for GAD in this population. The closest validated screen is the Hospital Anxiety and Depression Scale (HADS).21 Although the HADS effectively screens for generalized anxiety in patients with MS,21 the original intent of this screen was not focused on GAD.22 It is also copyright protected and must be purchased. Conversely, the GAD-7 is free, is readily accessible,23 and aligns with the diagnostic criteria for GAD. However, because the GAD-7 includes somatic symptoms, which may overlap with symptoms of MS, it is unclear whether this screen is an effective measure of GAD symptoms in MS populations.
The present study was conducted to 1) examine the psychometric properties of the GAD-7 to determine its appropriateness for use in individuals with MS and 2) analyze correlates of GAD symptoms in individuals with MS. The identification of a scientifically viable measure of GAD for people with MS can potentially serve as the foundation for improved clinical assessment and future research on GAD in this population.
Methods
Recruitment and Procedures
Individuals participating in a longitudinal study of MS completed a series of self-report surveys to collect information about their psychosocial well-being, disease severity, and other factors (eg, pain and fatigue). Cross-sectional data for this study came from the 4-month follow-up survey conducted between April 1 and August 31, 2007. More information about the research participants and procedures is published elsewhere.24 Briefly, individuals were recruited from the Greater Northwest Chapter of the National Multiple Sclerosis Society. The National Multiple Sclerosis Society mailed invitation letters (n = 7805), and 1628 individuals responded. Interested and eligible individuals aged 18 years or older with self-reported MS were mailed a paper survey (n = 1367) or a link to the online survey (n = 229). Of the 1270 individuals who completed this baseline assessment, 562 were randomly invited to continue participating in the longitudinal survey. A total of 513 individuals (91% response) completed the 4-month follow-up survey either online (n = 119) or on paper (n = 394). All the participants provided informed consent and received $25 per completed survey; the procedures were approved by the University of Washington's Human Subjects Division.
Measures
Demographics
Participants provided demographic and basic medical information, including sex, race/ethnicity, age, MS type, years of MS, and Expanded Disability Status Scale (EDSS)–Mobility score. The EDSS-Mobility used in this study is a self-reported version, which is highly correlated with the physician-administered EDSS.25
7-Item Generalized Anxiety Disorder Scale
The GAD-7 is a widely used self-report measure developed to screen for GAD.26 Brief tools such as this measure symptoms of a disease rather than a diagnosis (in this case GAD). This study used the GAD-7 module included in the full Patient Health Questionnaire (PHQ), in which participants rate the presence of symptoms on a 3-point scale as occurring “not at all” (0), “several days” (1), or “more than half the days” (2) during the past 2 weeks. Items are summed to create a symptom severity score ranging from 0 to 14. Participants met the measure's established categorical criteria of GAD if the total score on the GAD-7 was 8 or higher, they also endorsed the first question (“Feeling nervous, anxious, on edge, or worrying a lot about different things”), and three or more of the remaining items were rated “more than half the days.” For the purposes of this study, continuous and categorical scores were considered.
Hospital Anxiety and Depression Scale–Anxiety
The HADS-Anxiety (HADS-A) is a 7-item subscale of a 14-item measure used to screen for anxiety and depression in medical settings.27 Items are rated on a 4-point Likert scale, with higher scores indicating greater self-reported anxiety. The HADS was previously validated for use in MS populations21; a cutoff score of greater than 8 yielded 88.5% sensitivity and 80.7% specificity in this population.21
9-Item PHQ
The 9-item PHQ (PHQ-9) was developed to facilitate identification and diagnosis of major depressive disorder (MDD) in medical samples.28 Consistent with DSM-IV-TR MDD diagnostic criteria, each item is rated according to how persistent symptoms have been in the past 2 weeks, from 0 (not at all) to 3 (nearly every day), with the total score ranging from 0 to 27. The PHQ-9 showed good internal consistency (Cronbach α = 0.89) and test-retest reliability (r = 0.84) in a study of primary-care patients.29
Data Analysis
To evaluate the psychometric properties of the GAD-7, descriptive statistics, item correlations, and Cronbach alpha values were obtained using a statistical software program (IBM SPSS Statistics, version 20.0; IBM Corp, Armonk, NY). Listwise deletion based on all the variables in the procedure was used for missing data to calculate Cronbach alpha values (three total cases). To examine the GAD-7's factor structure, we used the following steps: 1) the sample was randomly split into two subsamples; 2) an exploratory factor analysis (EFA) was conducted on the GAD-7 with one of the random-split subsamples (n = 261) using Mplus statistical software, version 7.11; and 3) based on results from the EFA, a confirmatory factor analysis (CFA) of the hypothesized factor structure was conducted on the GAD-7 with the other half of the random-split sample (n = 252). Full information maximum likelihood estimation was used to account for partially missing values in the factor analyses.
Goodness of fit was evaluated using the χ2 test, the comparative fit index, the root mean square error of approximation and its 90% confidence interval, and the standardized root mean square residual. These fit indices provide different types of information (ie, absolute fit, fit adjusting for model parsimony, fit relative to a null model) and provide a reliable and conservative evaluation of model fit. Acceptance or rejection of the EFA and CFA models was based on 1) conventional criteria for good model fit, a comparative fit index greater than 0.95, a root mean square error of approximation less than 0.05, and a standardized root mean square residual less than 0.0630; 2) the strength of parameter estimates (primary factor loadings >0.35, absence of significant cross-loadings); and 3) the factor solution being interpretable and making sense on a conceptual level.
To evaluate construct reliability, we compared GAD-7 scores for the entire sample (n = 513) with HADS-A scores using the Pearson correlation. Furthermore, we examined how many individuals were identified as fitting categorical criteria for GAD according to the GAD-7 compared with individuals who met the greater than 8 cutoff score on the HADS-A.
Descriptive statistics, analyses of variance, and t tests were performed on the sample to determine whether there were significant differences in the continuous GAD-7 score as a function of demographic or MS-associated variables. The χ2 test and the t test were used to examine the same demographic and MS-associated variables in participants who met the categorical criteria for GAD. To examine the psychological correlates of the GAD-7, we ran correlations between the GAD-7 and the PHQ-9.
Results
Sample Characteristics
Participants (n = 513) were individuals diagnosed as having MS, predominantly non-Hispanic white (92%) and female (82%). The mean (SD) participant age was 51.4 (10.9) years (range, 20–85 years), and the mean (SD) duration of MS was 13.5 (9.8) years (range, 1–60 years). Regarding MS type, 57% of participants had relapsing-remitting MS, 20% secondary progressive, 13% primary progressive, and 10% progressive relapsing. In addition, 32.9% of participants had an EDSS-Mobility score of 4.0 or less, 48.1% had scores of 4.5 to 6.5, and 18.9% had scores of 7 or greater.
Exploratory Factor Analysis
As a first step, we conducted an EFA to explore the GAD-7's factor structure. We specified that solutions with one to three factors should be evaluated. The two- and three-factor solutions provided the best fit according to statistical criteria but were rejected because they contained factors consisting of just one or two items. The best solution was the one-factor solution, although fit indices indicated borderline model fit to data (Table 1). Eigenvalues greater than 1 for the unreduced correlation matrix were 2.83 and 1.08. All the items had salient and statistically significant loadings (0.43–0.64).
Table 1.
Goodness-of-fit indices and χ2 for EFA and CFA
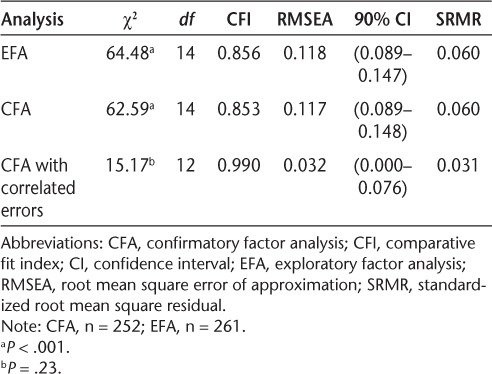
Confirmatory Factor Analysis
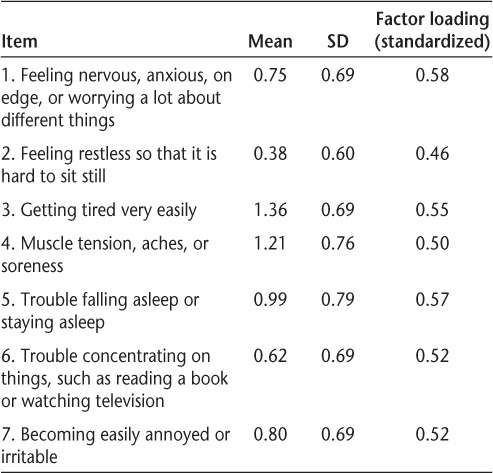
Based on results from the EFA, a one-factor CFA model was specified and yielded borderline global fit to the data (Table 1). Lagrange modification indices suggested several areas where model fit could be improved by allowing the residuals of items to correlate to account for a high degree of content overlap. Residuals for the following items were correlated: 1 with 2, and 3 with 4. This revised model provided an excellent fit for the data (Table 1) and a superior fit compared with the one-factor model based on EFA results (χ2diff2 = 47.42, P < .001). All the items had salient and statistically significant factor loadings ranging from 0.46 to 0.58 (standardized loadings, P < .001 for all). See Table 2 for item means, standard deviations, and factor loadings. All specified paths between residuals were significant (P < .005 for all). Standardized residuals and modification indices did not suggest any areas of strain. Model modification indices showed no areas where further changes to the model would be meaningful or could be theoretically justified.
Table 2.
Items on the 7-item Generalized Anxiety Disorder Scale
Reliability and Construct Validity of GAD-7
Internal consistency of the GAD-7 was evaluated by calculating the Cronbach alpha, which indicated good reliability (0.75). Inter-item correlation ranged from 0.19 to 0.51. A correlation analysis to evaluate construct validity indicated that the GAD-7 was significantly correlated with the HADS-A (r = 0.70). According to the HADS-A cutoff score for patients with MS, 112 participants (21.8%) were identified as having GAD, which was significantly greater than the 41 participants (8.0%) identified as fitting the categorical criteria for GAD on the GAD-7. Overlap between the two measures was not complete; only 28 participants met both the HADS-A and GAD-7 criteria.
GAD-7 Descriptives and Correlates
See Table 3 for demographic and illness-related characteristics for continuous GAD-7 scores (total sample) and categorical GAD-7 scores. The GAD-7 scores for the entire sample ranged from 0 to 14. The mean (SD) GAD-7 score for the sample was 5.99 (3.12). Age (r = −0.12) was negatively associated with GAD-7 scores, with older participants having significantly lower GAD-7 scores (P < .005); a curvilinear regression model did not provide a better fit in this sample. Duration of MS (r = −0.14) was also negatively associated with GAD-7 scores (P < .005). Women endorsed significantly higher scores on the GAD-7 than men (t508 = 2.13, P = .03). Participants whose race/ethnicity was other than non-Hispanic white reported significantly higher GAD-7 scores than non-Hispanic white participants (t508 = 2.41, P < .02). One-way analysis of variance indicated significant differences in GAD-7 scores among MS types (F3,496 = 55.40, P = .001); participants with secondary progressive MS endorsed significantly higher GAD-7 scores than those with the relapsing-remitting and primary progressive types.
Table 3.
Demographic and medical characteristics of participants by continuous and categorical anxiety
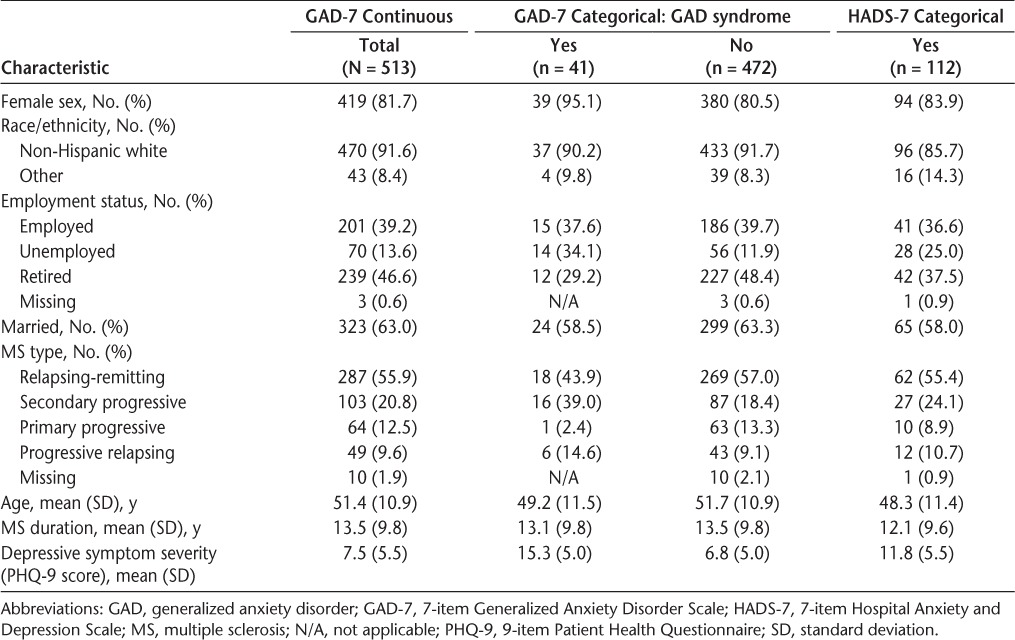
In this sample, only 41 of the 513 participants (8.0%) met the criteria for GAD (Table 3). The mean (SD) GAD-7 score in individuals who met the categorical criteria was 11.24 (1.26), compared with 5.53 (2.80) in participants who did not meet the criteria (t508 = 12.95, P < .001). Participants in this group were more likely to be female (χ21 = 33.39, P < .001) and non-Hispanic white (χ21 = 26.56, P < .001). Relapsing-remitting and secondary progressive types were most commonly found in participants who met the criteria for GAD (χ23 = 18.20, P < .001); however, comparing frequencies of MS types, only the secondary progressive type was more frequently found in participants who met the criteria for GAD (39% in this group vs. 20% of the entire sample). There were no significant differences in age and MS duration between the two groups.
Individuals with higher GAD-7 scores endorsed more depressive symptoms (r = 0.70, P < .001). Similarly, participants who met the categorical criteria for GAD scored significantly higher on depressive symptoms (t508 = 10.47, P < .001). Meeting the PHQ-9 MDD criteria was more likely in individuals who met the criteria for GAD (58.5% vs. 10.4%).
Compared with participants who met the GAD-7 categorical criteria, those who met the HADS-A categorical criteria had similar demographic and illness-related characteristics (Table 3). Participants who met the HADS-A categorical criteria were more likely to be female (χ21 = 51.57, P < .001) and non-Hispanic white (χ21 = 57.14, P < .001), and, most commonly, they had a diagnosis of relapsing-remitting or secondary progressive MS (χ23 = 62.59, P < .001). In contrast to the GAD-7, participants who met the HADS-A categorical criteria were significantly younger than those who did not meet the criteria (t511 = 3.45, P < .001). There was no significant difference in disease duration between the two groups. Similar to the GAD-7, participants who scored higher on the HADS-A endorsed significantly more depressive symptoms (P < .001). Participants who met the HADS-A categorical criteria endorsed significantly more depressive symptoms (t508 = 10.41, P < .001). Meeting the PHQ-9 MDD criteria was also more likely in individuals who met the HADS-A categorical criteria (34.8% vs. 8.5%).
Discussion
The present study sought to examine the psychometric properties of the GAD-7 for use in people with MS. Factor analysis revealed a single-factor structure. Reliability, internal validity, and construct validity were also confirmed. These findings support use of the GAD-7 as a measure of anxiety symptoms in individuals with MS for clinical and research purposes. Secondary analyses also revealed important relationships between GAD-7 scores and demographic variables, disease-related variables, and secondary symptoms.
The present study carries important clinical implications for assessing generalized anxiety symptoms in individuals with MS. First, the GAD-7 items align with the DSM-IV-TR diagnostic criteria for GAD, making it a useful screen of relevant symptoms. Established categorical criteria make the measure easy to administer and interpret. Second, it is brief, free, and easy to obtain, making it convenient for immediate implementation in almost any medical clinic. Finally, an improved ability to detect GAD symptoms will help clinicians offer appropriate behavioral or pharmacologic interventions. Although there is already one validated measure of anxiety in MS, the HADS-A, this measure was not originally developed to screen for GAD, it is copyright protected, and it must be purchased. The GAD-7 overcomes these barriers and may be an alternative to the HADS-A. As an important next step, the GAD-7 should be compared with a gold standard, such as the Structured Clinical Interview for DSM, to draw definitive conclusions about the utility of this tool as a clinical screening measure for GAD.
Establishing the GAD-7 as an appropriate measure for generalized anxiety symptom screening is also important for research in MS. Given the paucity of research on generalized anxiety in MS, additional studies are needed on 1) prevalence; 2) relationship of GAD with other demographic, disease-related, and secondary symptom factors; 3) interventions for reducing the severity and impact of GAD symptoms; and 4) the extent to which other interventions also reduce GAD as a secondary effect. In all these cases, reliable and valid measures of GAD, such as the GAD-7, are needed. In other populations, the GAD-7 has been demonstrated to be responsive to change over time.31 Future research is needed to understand whether the GAD-7 would be similarly responsive to change in people with MS and, therefore, appropriate for longitudinal studies or to detect change in intervention studies.
Consistent with studies of primary-care patients,8 8.0% of participants in the present sample met the criteria for GAD based on their answers on the GAD-7, but this is less than the rate observed in other studies of individuals with MS (19%).9 This difference may be attributed to the sample (eg, selection bias) or to the use of alternative measures (eg, HADS-A vs. GAD-7). For comparison, in this sample, 22% of participants met the HADS-A categorical criteria. Although prevalence differed from the general population, the demographic associations with GAD symptoms were consistent with those of previous studies. Higher GAD-7 scores were associated with younger age32 and being female33; we also observed a higher prevalence in non-Hispanic white participants.34
Participants with secondary progressive MS endorsed significantly more anxiety symptoms than those with the relapsing-remitting and primary progressive types. This stands in contrast to a recent study that reported no significant differences in anxiety level for people with different MS disease courses. However, that study used the HADS-A,35 which raises the question of whether the different results in the present study contradict this previous study or whether they reflect the HADS-A and GAD-7 measuring different constructs. In the present sample, there was a substantial difference found for the categorical prevalence estimates using the HADS-A and GAD-7, which suggests that the scales may measure different constructs as the items for each scale differ. For instance, the GAD-7 items were based on diagnostic criteria for GAD, and the HADS-A items were not. Also, the HADS-A contains items that assess only nonsomatic symptoms of anxiety, whereas the GAD-7 includes both somatic and nonsomatic anxiety symptoms. Further research is warranted in this area.
Finally, generalized anxiety symptoms were highly correlated with depression, meaning that higher scores on the GAD-7 were associated with endorsing more depressive symptoms; approximately half of the participants meeting the cutoff criteria for GAD also met the criteria for depression. The correlation between anxiety symptoms and depressive symptoms is consistent with previous studies,12 as was the tendency for people with greater depressive symptoms to also meet the criteria for anxiety disorders,13 in this case GAD. The GAD-depression relationship is worthy of consideration in future research. For example, questions arise about independence (To what extent are these symptoms a manifestation of unique conditions vs. symptoms that represent a single construct?), temporal relationship (Do the mood symptoms precede the anxiety symptoms or vice versa?), and correlates (To what extent are the correlates of GAD and low mood similar?). The questions of GAD and depression comorbidity are of particular importance given that recent studies12,13 demonstrated that depression often co-occurs with anxiety. One explanation might be shared maladaptive cognitions; either these disorders share unhelpful thought patterns or individuals with both diagnoses are prone to certain maladaptive beliefs. One might wonder whether more effort should be put into understanding and treating GAD.
This study has several limitations. First, it relied on self-report data. To definitively provide a DSM-IV-TR diagnosis of GAD-7, a clinical diagnostic interview is required; however, in many cases, this is not possible, and having a reliable self-report screening measure available becomes even more important in clinical settings. A logical next step would be to validate the GAD-7 against a gold standard, such as the Structured Clinical Interview for DSM or another clinical interview. Second, the data collected from these 513 community-dwelling adults from the Pacific Northwest with a diagnosis of MS are not population based and, therefore, cannot be assumed to be representative of the entire MS population. Third, the GAD-7 used in this study was the version that is incorporated into the full PHQ rather than the version that has been published as a standalone module; although the items on this questionnaire are consistent with items on the stand-alone GAD-7, the scale on the version used herein ranged from 0 to 3, compared with 0 to 4 (omitted “nearly every day”). Although this difference does not affect validation outcomes, it limits direct comparison with studies using the alternative version of the GAD-7 and may have other implications. For instance, internal reliability (Cronbach alpha) is typically lower with fewer response categories. Also, the observed differences between categorical GAD-7 and HADS-A scores may be due, in part, to different scaling of the two measures; however, these differences in categorical overlap may also be due to a variety of other reasons, as previously discussed. Finally, a relatively small number of study participants (n = 41) met the GAD-7 categorical criteria; therefore, analyses examining descriptive properties in this group compared with the remaining sample of participants may be skewed and should be interpreted with caution. The reasons for this relatively low prevalence of GAD are unclear, but it may reflect use of a different measure relative to previous studies or a selection bias such that people who are less distressed may be more likely to participate in this type of study.
Conclusion
The present study addressed an important gap in the MS anxiety literature by being the first to examine the psychometric properties and evaluate the appropriateness of the GAD-7 for use in people with MS. Moreover, this study is among only a few to consider the correlates of GAD in people with MS. Results support use of the GAD-7 for populations with MS and suggest that the measure could be a useful addition for clinical and research purposes. Furthermore, the results raise a variety of interesting questions for much-needed future research on this topic.
PracticePoints.
Generalized anxiety disorder is common in MS but understudied. Reliable and valid measures are needed to advance clinical care and expand research in this area.
The 7-item Generalized Anxiety Disorder Scale (GAD-7) may be an appropriate screen for generalized anxiety in people with MS. The GAD-7 is free and readily accessible for use by clinicians and researchers.
Younger age, being female, and having secondary progressive MS type were associated with higher GAD-7 scores in people with MS. The GAD-7 scores and depressive symptoms were also positively correlated.
Footnotes
Financial Disclosures: The authors have no conflicts of interest to disclose.
Funding/Support: The contents of this article were developed under grants from the Department of Education, National Institute on Disability and Rehabilitation Research (grants H133B031129 and H133B080025). However, these contents do not necessarily represent the policy of the Department of Education, and you should not assume endorsement by the federal government. In addition, this work was supported by a grant from the National Institutes of Health through the NIH Roadmap for Medical Research (grant 5U01AR052171-03 to the University of Washington) and by grants MB0008 and MB0026 from the National Multiple Sclerosis Society.
References
- 1.da Silva AM, Vilhena E, Lopes A et al. Depression and anxiety in a Portuguese MS population: associations with physical disability and severity of disease. J Neurol Sci. 2011;306:66–70. doi: 10.1016/j.jns.2011.03.042. [DOI] [PubMed] [Google Scholar]
- 2.Janssens A, Doorn PA, Boer JB, Meche FGA, Passchier J, Hintzen RQ. Impact of recently diagnosed multiple sclerosis on quality of life, anxiety, depression and distress of patients and partners. Acta Neurol Scand. 2003;108:389–395. doi: 10.1034/j.1600-0404.2003.00166.x. [DOI] [PubMed] [Google Scholar]
- 3.Feinstein A, O'Connor P, Gray T, Feinstein K. The effects of anxiety on psychiatric morbidity in patients with multiple sclerosis. Mult Scler. 1999;5:323–326. doi: 10.1177/135245859900500504. [DOI] [PubMed] [Google Scholar]
- 4.Kessler RC, Aguilar-Gaxiola S, Alonso J et al. The global burden of mental disorders: an update from the WHO World Mental Health (WMH) surveys. Epidemiol Psichiatr Soc. 2009;18:23–33. doi: 10.1017/s1121189x00001421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Diagnostic and StatisticalManual of Mental Disorders (Fourth Edition, Text Revision) Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 7.Somers JM, Goldner EM, Waraich P, Hsu L. Prevalence and incidence studies of anxiety disorders: a systematic review of the literature. Can J Psychiatry. 2006;51:100–113. doi: 10.1177/070674370605100206. [DOI] [PubMed] [Google Scholar]
- 8.Kroenke K, Spitzer RL, Williams JB, Monahan PO, Lowe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. 2007;146:317–325. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- 9.Korostil M, Feinstein A. Anxiety disorders and their clinical correlates in multiple sclerosis patients. Mult Scler. 2007;13:67–72. doi: 10.1177/1352458506071161. [DOI] [PubMed] [Google Scholar]
- 10.Burns MN, Nawacki E, Siddique J, Pelletier D, Mohr DC. Prospective examination of anxiety and depression before and during confirmed and pseudoexacerbations in patients with multiple sclerosis. Psychosom Med. 2013;75:76–82. doi: 10.1097/PSY.0b013e3182757b2b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mohr DC. Psychiatric Disorders, Stress, and Their Treatment Among People with Multiple Sclerosis. New York, NY: Springer; 2011. [Google Scholar]
- 12.Garfield AC, Lincoln NB. Factors affecting anxiety in multiple sclerosis. Disabil Rehabil. 2012;34:2047–2052. doi: 10.3109/09638288.2012.667503. [DOI] [PubMed] [Google Scholar]
- 13.Wood B, van der Mei IAF, Ponsonby AL et al. Prevalence and concurrence of anxiety, depression and fatigue over time in multiple sclerosis. Mult Scler J. 2013;19:217–224. doi: 10.1177/1352458512450351. [DOI] [PubMed] [Google Scholar]
- 14.Askey-Jones S, David AS, Silber E, Shaw P, Chalder T. Cognitive behaviour therapy for common mental disorders in people with multiple sclerosis: a bench marking study. Behav Res Ther. 2013;51:648–655. doi: 10.1016/j.brat.2013.04.001. [DOI] [PubMed] [Google Scholar]
- 15.Koponen H, Allgulander C, Erickson J et al. Efficacy of duloxetine for the treatment of generalized anxiety disorder: implications for primary care physicians. Prim Care Companion J Clin Psychiatry. 2007;9:100–107. doi: 10.4088/pcc.v09n0203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Donker T, van Straten A, Marks I, Cuijpers P. Quick and easy self-rating of Generalized Anxiety Disorder: validity of the Dutch web-based GAD-7, GAD-2 and GAD-SI. Psychiatry Res. 2011;188:58–64. doi: 10.1016/j.psychres.2011.01.016. [DOI] [PubMed] [Google Scholar]
- 17.Lowe B, Decker O, Muller S et al. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med Care. 2008;46:266–274. doi: 10.1097/MLR.0b013e318160d093. [DOI] [PubMed] [Google Scholar]
- 18.Kertz S, Bigda-Peyton J, Bjorgvinsson T. Validity of the Generalized Anxiety Disorder-7 scale in an acute psychiatric sample. Clin Psychol Psychother. 2013;20:456–464. doi: 10.1002/cpp.1802. [DOI] [PubMed] [Google Scholar]
- 19.Wild B, Eckl A, Herzog W et al. Assessing generalized anxiety disorder in elderly people using the GAD-7 and GAD-2 scales: results of a validation study. Am J Geriatr Psychiatry. 2014;22:1029–1038. doi: 10.1016/j.jagp.2013.01.076. [DOI] [PubMed] [Google Scholar]
- 20.Cooper CL, Hind D, Parry GD et al. Computerised cognitive behavioural therapy for the treatment of depression in people with multiple sclerosis: external pilot trial. Trials. 2011;12:259. doi: 10.1186/1745-6215-12-259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Honarmand K, Feinstein A. Validation of the Hospital Anxiety and Depression Scale for use with multiple sclerosis patients. Mult Scler. 2009;15:1518–1524. doi: 10.1177/1352458509347150. [DOI] [PubMed] [Google Scholar]
- 22.Snaith RP, Zigmond AS. The hospital anxiety and depression scale. Br Med J (Clin Res Ed) 1986;292:344. doi: 10.1136/bmj.292.6516.344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Patient Health Questionnaire (PHQ) Screeners. 2013. http://www.phqscreeners.com.
- 24.Amtmann D, Bamer AM, Noonan V, Lang N, Kim J, Cook KF. Comparison of the psychometric properties of two fatigue scales in multiple sclerosis. Rehabil Psychol. 2012;57:159–166. doi: 10.1037/a0027890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bowen J, Gibbons L, Gianas A, Kraft GH. Self-administered Expanded Disability Status Scale with functional system scores correlates well with a physician-administered test. Mult Scler. 2001;7:201–206. doi: 10.1177/135245850100700311. [DOI] [PubMed] [Google Scholar]
- 26.Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 27.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 28.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders: Patient Health Questionnaire. JAMA. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 29.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- 31.Dear BF, Titov N, Sunderland M et al. Psychometric comparison of the generalized anxiety disorder scale-7 and the Penn State Worry Questionnaire for measuring response during treatment of generalised anxiety disorder. Cogn Behav Ther. 2011;40:216–227. doi: 10.1080/16506073.2011.582138. [DOI] [PubMed] [Google Scholar]
- 32.Beiske AG, Svensson E, Sandanger I et al. Depression and anxiety amongst multiple sclerosis patients. Eur J Neurol. 2008;15:239–245. doi: 10.1111/j.1468-1331.2007.02041.x. [DOI] [PubMed] [Google Scholar]
- 33.Giordano A, Granella F, Lugaresi A et al. Anxiety and depression in multiple sclerosis patients around diagnosis. J Neurol Sci. 2011;307:86–91. doi: 10.1016/j.jns.2011.05.008. [DOI] [PubMed] [Google Scholar]
- 34.Asnaani A, Richey JA, Dimaite R, Hinton DE, Hofmann SG. A cross-ethnic comparison of lifetime prevalence rates of anxiety disorders. J Nerv Ment Dis. 2010;198:551–555. doi: 10.1097/NMD.0b013e3181ea169f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jones KH, Ford DV, Jones PA et al. A large-scale study of anxiety and depression in people with multiple sclerosis: a survey via the web portal of the UK MS Register. PLoS One. 2012;7:e41910. doi: 10.1371/journal.pone.0041910. [DOI] [PMC free article] [PubMed] [Google Scholar]


