Abstract
Background
The objective of this study is to identify and review the methodological quality of health economic evaluations of medical devices performed in the People’s Republic of China. To our knowledge, no such investigations have been performed to date.
Methods
A systematic literature review involving searches of Medline, Medline In-Process, the National Health Service Economic Evaluation Database, the Cost-Effectiveness Analysis Registry of the Tufts Medical Center, and the Wanfang Database was performed. The search spanned the period from 1990 to 2013. Studies on health economic evaluations of medical devices, in-vitro diagnostics, procedures, and the use of medical devices in Chinese health care settings were included. Full-text articles and conference abstracts in English and Chinese were included.
Results
Fifty-seven publications were included, 26 (46%) of which were in English and 31 (54%) of which were in Chinese. The included publications covered a wide range of clinical areas, such as surgery (n=23, 40%), screening (n=9, 16%), imaging use (n=6, 11%), kidney intervention (n=4, 7%), and nine other technological areas. Most of the studies (n=31, 54%) were cost analyses. Among the others, 13 (50%) studies used modeling, and another 13 (50%) were within-trial evaluations. Among studies that used modeling, eleven (85%) conducted sensitivity analyses, six of which had one-way sensitivity analysis, whereas one conducted both one-way and two-way sensitivity analyses; four of these eleven modeling-based analyses included probabilistic sensitivity analyses. The incremental cost-effectiveness ratio was reported in ten (18%) studies, eight of which were screening studies. The remaining two modeling studies were in areas of imaging and oncology.
Conclusion
This study indicates that there are major limitations and deficiencies in the health economic evaluations on medical devices performed in the People’s Republic of China. Further efforts are required from different stakeholders – academic, governmental, and privatized – to improve health economic research capacity and to put it to use when informative decisions are made in the health care setting.
Keywords: health economics, cost-effectiveness analysis, cost–utility analysis, cost–consequences analysis, medical devices, People’s Republic of China
Introduction
Health economics helps to compare different health technologies, taking into account clinical and cost consequences, and supports resource allocation decisions.1 After safety, efficacy, and effectiveness, cost-effectiveness has been recognized as the major “fourth hurdle” to secure market access in many developed countries around the world.2,3 Health economics is successfully used to support decision making in medical device use, in-vitro diagnostics, and medical procedure areas.4
While having a long history of use in the United States, Europe, Canada, Australia, and other countries, health economics has only recently emerged as a decision-making supportive tool in Asian countries.5–8 The People’s Republic of China, with a population of >1.3 billion people and with a growing economy, is an attractive market for manufacturers of medical devices and pharmaceuticals.9 The People’s Republic of China’s medical device market has become the world’s second largest in 2010, with a market size having exceeded 15.8 billion US dollars (USD).10 However, reimbursement for medical devices is limited and complex, especially for innovative products.11 With the growing role of health economic evaluations, it is important to evaluate the status of this area in the People’s Republic of China in terms of quantitative data, characteristics, and methodological approaches for evaluations of devices.
There is a lack of information concerning how the People’s Republic of China performs as a stakeholder in terms of health economic evaluations revolving around medical devices and whether or not, or how cost-effectiveness is addressed in the Chinese health care setting. Therefore, the objective of this study was to review the methodological quality of health economic evaluations of medical devices performed in the People’s Republic of China.
Methods
Literature search and citation screening
A systematic literature search was performed in the following databases: Medline, Medline In-Process, the National Health Service Economic Evaluation Database (NHS EED), and the Cost-Effectiveness Analysis (CEA) Registry of the Tufts Medical Center,12 as well as the Wanfang Database13 for studies published in Chinese. The Wanfang Database is an affiliate of the Chinese Ministry of Science and Technology and provides access to a wide range of data, including medical and scientific areas. The full-search strategy for each specific database is presented in the Supplementary materials. The searches were conducted on February 20, 2013 for Medline, on February 25, 2013 for the NHS EED and the CEA Registry, and on March 1, 2013 for the Wanfang database. The search spanned the period from January 1, 1990 to January 31, 2013.
Screening of abstracts and evaluations of full-text publications was performed by a single reviewer using the inclusion/exclusion criteria provided below. A second reviewer checked the appropriateness of inclusion of studies. Disagreements were resolved by consensus.
Study selection
The following inclusion criteria were used:
Type of studies: CEA, cost–utility (CUA), cost–benefit (CBA), cost-minimization (CMA), cost–consequences (CCA), and budget impact analyses. Economic evaluations as a part of published health technology assessments were also considered.
Type of interventions: Medical devices, in-vitro diagnostics, and procedures using medical devices were considered.
Language: Publications in English or Chinese were included.
Type of publication: Full-text publications in peer-reviewed journals and abstracts of conference proceedings were included.
Setting: The study should have been conducted in a Chinese setting.
Data extraction and analysis
Data from included publications were extracted by one reviewer and presented in the format outlined below. The following information was extracted: title, first author, payer perspective, population/settings, intervention, comparator, time horizon, type of economic evaluation, type of study (economic evaluation alongside clinical trial, modeling), type of analysis (CEA, CUA, etc), cost and cost categories (direct, indirect, etc), source of unit cost, year of costing, resources used and their quantity reported separately (yes/no), clinical outcomes, economic outcomes, discounting, sensitivity analysis (one-way, two-way, etc), regression analysis of cost, source of funding, results (incremental cost-effectiveness ratio [ICER] or total cost per intervention), main conclusion, and language of publication. A second reviewer assessed the quality of the data extraction.
Summary statistics were calculated. No formal statistical analysis was used due to the descriptive nature of this study.
Results
Literature search and citation screening
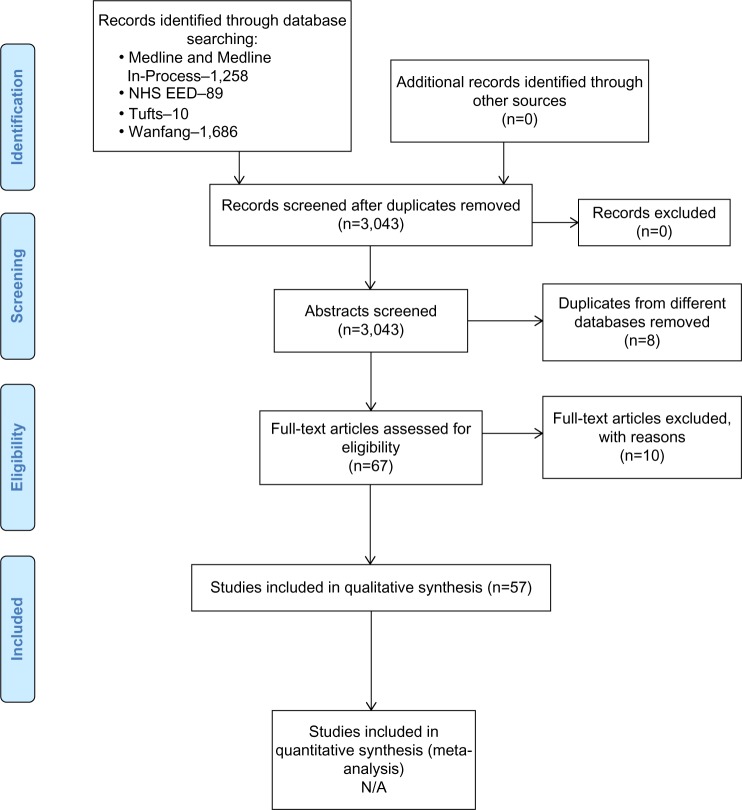
The literature search of electronic databases returned 3,043 initial hits. In total, 57 publications were included in the study. Detailed information about the search process is presented in Figure 1. A list of excluded publications with the reasons for exclusion is presented in the Supplementary materials.
Figure 1.
PRISMA flow chart.
Abbreviations: N/A, not applicable; NHS EED, National Health Service Economic Evaluation Database; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Description of identified studies
Fifty-seven studies in total were available, 26 (46%) of which were in English and 31 (54%) of which were in Chinese. Methodological characteristics of included publications are presented in Table 1.
Table 1.
Methodological characteristics of publications included in the analysis
| Author, reference | Type of intervention | Type of evaluation | Type of analysis | Perspective | Time horizon | Cost categories | Year of costing | Discounting | Economic outcomes | Sensitivity analysis | Source of funding |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Wang and Huang14 | Imaging | M | CEA, CUA | H | – | DM | 2010 | C-5% | ICER, total cost | One-way | A |
| Zhang and Yang15 | Screening | TBE | CCA | HCP | – | DM | – | – | Total cost | – | – |
| Wei et al16 | Surgery | CA | CCA | H | Hospital stay | DM | – | NAa | Total cost | – | – |
| Kim et al17 | Screening | M | CUA | S | Lifetime | DM, DNM, I | 1999/2000 | CB-3% | ICER, total cost | – | – |
| Woo et al18 | Screening | M | CEA, CUA | S | Study follow-up | DM, DNM, I | – | CB-3% | ICER, total cost | Prob | P |
| Wong et al19 | Screening | M | CEA, CUA | S | Study follow-up | DM | 2005 | CB-3% | ICER, lifetime costs, QALY | Prob | G |
| Wong et al20 | Screening | M | CEA, CUA | S | Study follow-up | DM, DNM | 2005 | CB-3% | ICER, lifetime costs | Prob | G |
| Wong et al21 | Oncology | M | CEA, CUA | S | Study follow-up | DM | 2010 | CB-3% | ICER, lifetime costs | Prob | G, A |
| Chen et al22 | Cardiac surgery | CA | CCA | H | Hospital stay | DM | – | NAa | Total cost | – | – |
| Cheng et al23 | Imaging | M | CCA | H | – | DM | 2007 | C-3% after 5 years | Total cost | One-way, two-way | – |
| Gong et al24 | Surgery | TBE | CCA | H | Study follow-up, hospital stay | DM | – | – | Total cost | – | – |
| Feng et al25 | Surgery | TBE | CCA | S | Study follow-up, hospital stay | DM, I | – | – | Total cost | – | G |
| Chen et al26 | Cardiac surgery | CA | CCA | H | Study follow-up, hospital stay | DM | – | – | Total cost | – | – |
| Zang et al27 | Surgery | CA | CCA | H | – | DM | – | – | Total cost | – | – |
| Gurbanov et al28 | Life support | CA | CCA | H | – | DM, DNM | – | – | Total cost | – | N |
| Zhang et al29 | Kidney intervention | TBE | CCA | H | Hospital stay | DM | – | NAa | Total cost | – | – |
| Liu et al30 | Imaging | TBE | CCA | H | Study follow-up | DM, DNM | – | NAa | Total cost | – | – |
| Wong et al31 | Surgery | TBE | CCA | H | Study follow-up | DM | – | – | Total cost | – | G, A |
| Xie et al32 | Bone surgery | CA | CCA | H | Study follow-up, hospital stay | DM | – | – | Total cost | – | N |
| Lu et al33 | Surgery | CA | CCA | H | Study follow-up, hospital stay | DM, DNM | – | – | Total cost | – | – |
| Yang et al34 | Screening | M | CBA | S | Lifetime | DM, I | 2008 | CB-3% | ICER, total cost | One-way | G |
| Sheng et al35 | Surgery | TBE | CCA | H | Study follow-up, hospital stay | DM | – | – | Total cost | – | – |
| Wang et al36 | Screening | M | CEA | S | Study follow-up, hospital stay | DM | 2010 | CB-3% | ICER, total cost | One-way | – |
| Huang et al37 | Screening | M | CEA, CUA | S | Lifetime | DM, DNM, I | 2009 | – | ICER, total cost | One-way | – |
| Wu et al38 | Surgery | CA | CCA | H | Study follow-up, hospital stay | DM | – | – | Total cost | – | – |
| Xia et al39 | Obstetrics | CA | CCA, CMA | H | Study follow-up | DM | – | NAa | Total cost | – | – |
| Chen et al40 | Kidney intervention | TBE | CUA | S | Study follow-up, hospital stay | DM, DNM, I, recessive cost | 2003 | – | ICUR, total cost | One-way | G |
| Chen et al41 | Surgery | CA | CCA | S | – | DM, DNM, I | – | – | Total cost | – | – |
| Fan42 | Imaging | CA | CEA | HCP | – | DM | – | – | Total cost | One-way | – |
| Gu et al43 | Imaging | M | CCA | HCP | – | DM | – | – | Total cost | – | G, A |
| Fu et al44 | Vascular surgery | CA | CEA | H | – | DM | 2007 | C-3% | Total cost | – | – |
| Guan et al45 | Surgery | CA | CCA | S | – | DM, DNM, I | – | – | Total cost | One-way | – |
| Guo et al46 | Screening | M | CEA | S | – | DM | 2002 | C-3% | ICER, total cost | One-way | – |
| Han et al47 | Respiratory support | CA | CCA | HCP | Hospital stay | DM | – | NAa | Total cost | – | – |
| He et al48 | Surgery | CA | CCA | S | Study follow-up, hospital stay | DM, DNM, I | – | NAa | Total cost | – | – |
| Hou et al49 | Imaging | CA | CCA | H | – | DM | – | – | Total cost | – | A |
| Gen50 | Kidney intervention | CA | CCA | HCP | – | DM | – | – | Total cost | – | – |
| Guo51 | Surgery | CA | CCA | S | Study follow-up, hospital stay | DM, DNM, I | 1999 | – | Total cost | – | – |
| Lan et al52 | Respiratory support | TBE | CCA | H | – | DM | – | – | Total cost | – | – |
| Li and Liu53 | Surgery | CA | CCA | S | – | DM, DNM, I | – | – | Total cost | – | – |
| Liu et al54 | Bone surgery | TBE | CEA, CUA | H | Study follow-up | DM, DNM | – | – | Total cost | One-way | – |
| Ma et al55 | Vascular surgery | CA | CCA | H | Study follow-up, hospital stay | DM | 2010 | NAa | Total cost | One-way | – |
| Peng et al56 | Surgery | M | CUA | S | – | DM, DNM | – | – | Total cost | One-way | G |
| Tan et al57 | Surgery | CA | CCA | H | Hospital stay | DM | – | NAa | Total cost | – | – |
| Tan58 | Surgery | CA | CCA | S | Hospital stay | DM, I | – | NAa | Total cost | – | – |
| Wang et al59 | Surgery | CA | CEA | H | Study follow-up | DM | – | NAa | Total cost | – | G |
| Wang et al60 | Bone surgery | CA | CCA | H | Study follow-up | DM | – | NAa | Total cost | – | – |
| Wei et al61 | Surgery | CA | CCA | S | Hospital stay | DM, DNM, I | – | NAa | Total cost | – | G |
| Wen et al62 | Kidney intervention | CA | CCA | H | Study follow-up | DM | – | – | Total cost | – | G |
| Xia63 | Surgery | CA | CCA | H | Hospital stay | DM, DNM | – | NAa | Total cost | – | – |
| Yu64 | Surgery | CA | CCA | S | Study follow-up, hospital stay | DM, DNM, I | 2005 | C-3% | Total cost | One-way | – |
| Zhou et al65 | Surgery | CA | CCA | H | – | DM | – | – | Total cost | – | – |
| Wu and Zen66 | Ophthalmology | TBE | CCA | H | – | DM | – | – | Total cost | – | – |
| Liu et al67 | Surgery | TBE | CCA | H | Study follow-up, hospital stay | DM | – | NAa | Total cost | – | – |
| Han et al68 | Ophthalmology | CA | CCA | H | – | DM, DNM | – | – | Total cost | – | – |
| Liu et al69 | Airway surgery | TBE | CCA | H | – | DM | – | – | Total cost | – | G |
| Lv et al70 | Surgery | CA | CCA | H | – | DM | – | – | Total cost | – | A |
Note:
NA, not applicable for studies with duration of < 1 year.
Abbreviations: A, academia; CA, cost analysis of routine care; CCA, cost–consequence analysis; CEA, cost-effectiveness analysis; CMA, cost-minimization analysis; CUA, cost–utility analysis; C-%, cost discounted – annual discount rate; CB-%, cost and benefit discounted – annual discount rate; DM, direct medical cost; DNM, direct nonmedical cost; G, government; H, hospital; HCP, health care payer; I, indirect cost; ICER, incremental cost-effectiveness ratio; M, modeling; N, none; NA, not applicable; P, personal; Prob, probabilistic; QALY, quality-adjusted life year; S, society; TBE, trial-based evaluation; –, not reported; CBA, cost-benefit analysis.
Design and methodology of economic evaluations
Most of the studies (n=31, 54%) were cost analyses of routine care. Among the others (n=26, 46%), 13 (50%) used decision analytic modeling, whereas the other 13 were trial-based evaluations. Thirty-two studies (56%) adopted a hospital perspective, whereas five (9%) adopted a third-party payer perspective, while the remaining studies (n=20, 35%) were from a societal perspective.
Time horizon was reported in 36 (63%) articles. Most studies (n=25, 44%) used the respective study’s follow-up as the time horizon. There were 22 (39%) and three (5%) studies that used hospital stay and lifetime as time horizons, respectively.
Discounting was applied in 12 (21%) studies; four of these discounted future costs with 3% of the annual rate, one discounted future costs with 5% of the annual rate, and seven discounted both future costs and benefits with 3% of the annual rate.
The source of funding was reported in 19 (33%) studies. Of these, three articles had funding from academia, ten studies had funding by the government, three articles had funding by both government and academia, one study had personal support, and two studies specified that there was no supporting funding. There was no single study reporting funding from the industry.
Among all studies involving a health economic analysis, 40 (69%) used a CCA; seven (12%), both a CCA and a CEA; five (9%), a CEA; three (5%), a CUA; one (2%), a CBA; and one (2%), both a CCA and a CMA.
Concerning studies in clinical areas, 23 (40%) involved surgery, nine (16%) involved screening, six (11%) involved imaging, four (7%) involved kidney intervention, three (6%) involved bone surgery, two each involved cardiac surgery/vascular surgery/respiratory support/ophthalmology (3% each), and one each involved oncology/life support/obstetrics/airway surgery (2% each).
Resource use and cost inputs
Among 44 nonmodeling studies, only 14 (32%) reported resources used and the quantity used for each resource. Thirty studies reported the source of unit cost, 16 (53%) of which adopted local unit costs from hospitals, ten (33%) used regional unit costs, one (3%) used national unit cost as a reference, and three (10%) used both local and regional sources. There was only one study (2%) with a regression analysis on cost available. All (n=57) studies reported direct medical costs. Direct nonmedical costs were reported in 19 (33%) studies, and indirect costs were reported in 14 (25%) studies.
Sensitivity analysis
Among the 13 studies that used modeling, eleven (85%) conducted sensitivity analyses; six (55%) of these had a one-way sensitivity analysis, one (9% of 11) conducted both one-way and two-way sensitivity analyses, and four (36% of 11) reported a probabilistic sensitivity analysis.
Among nonmodeling studies that conducted one-way sensitivity analyses, there were two (4%) that conducted trial-based evaluations and four (7%) that conducted cost analyses of routine care.
Outcomes of economic evaluations
The ICER was presented in ten (18%) studies, eight (80%) of which were screening studies, while the remaining two (20%) were studies in imaging and oncology areas. The reported ICER (with year of costing available) ranged from 12 USD per life-year saved (USD/LYS) for the single colonoscopy screening strategy to 6,014 USD/LYS for an additional positron emission tomography/computed tomography (CT) screening when compared with conventional CT staging.
Detailed information on population, settings, comparators, results, and conclusions is provided in the Supplementary materials.
Discussion
The present study is one of the first attempts to evaluate the status of health economic evaluations of medical devices in the People’s Republic of China. This study complements existing literature on methodological quality of the health economic evaluations in regions by raising the issue of application of this concept in decision making.71–73 While other systematic reviews are focused on health economic evaluations in general and mainly include evaluations of pharmaceuticals, our review is aimed on research in medical device and in-vitro diagnostic areas. Specifics of economic evaluation of medical devices in comparison with pharmaceuticals have been extensively reviewed elsewhere.74 This includes difficulties in conducting randomized controlled trials, “learning curve” and usability aspects, wider organizational implications, a shorter life cycle, fast price erosion, etc. Moreover, reimbursement and funding for medical devices differ significantly than for pharmaceuticals, as a special approach is required for the evaluation of medical device studies.
This study reveals that literature on health economics of medical devices in the People’s Republic of China is limited (57 publications in total from the year 1990), and the majority of the publications (53%) include cost or CCAs of routine care. Decision analytic modeling and within-trial evaluations have been used equally.
To include the majority of relevant studies, the search was also conducted using a local Chinese bibliographic database. Although locally published studies bring value in terms of having a complete picture of available research, they may have different methodological quality. Interestingly, the majority of the studies published in Chinese (24 out of 31) used CCAs, mainly at the hospital level. On the other hand, nine out of the ten studies that reported ICER and nine out of 17 studies that conducted sensitivity analyses were published in English, while all the Chinese studies with sensitivity analyses conducted only one-way sensitivity analysis. Among the 13 studies that applied modeling approaches, ten studies were published in English. In addition, among 42 studies with study follow-ups longer than 1 year, only 13 had discounting available. Among these 13 studies, nine were published in English. This may reflect both interests from authors to increase exposure to international literature and to have the influence of international recommendations on good reporting practice on content of published articles. The development of clear guidelines for economic evaluations is clearly considered part of the strategy to increase application of these studies in decision making.75 Recently, Consolidated Health Economic Evaluation Reporting Standards were issued by the International Society for Pharmacoeconomics and Outcomes Research Task Force, which may help improve the quality of reporting of economic evaluations.76
A sensitivity analysis was also conducted to account for the time that passed after the primary analysis was completed (January 2013 to December 2014). The analysis was performed using Medline and Medline In-Process on January 15, 2015, with the same search strategy that was used during the primary analysis. Among the 181 hits generated from the search, eight studies were identified.77–84 Most of the studies (n=4, 50%) were trial-based evaluations, and the remainder were cost analyses of routine care (n=2, 25%) and decision analytic modeling (n=2, 25%). Discounting was not applied in any article (it was not applicable to one study). Apart from one study published in Chinese, the remaining studies were published in English. Six studies (75%) used CCA, and both CEA and CUA were used in two studies (25%). In the two studies that used modeling, both conducted sensitivity analyses – one study conducted only one-way sensitivity analyses, while the other performed one-way, two-way, and probabilistic sensitivity analyses. However, it is worth mentioning that the study that conducted a CEA and CUA with decision analytic modeling and sensitivity analyses (one-way, two-way, and probabilistic) was conducted in the setting of Hong Kong,83 which runs a different health care system and medical device funding system than Mainland China. With these results, it appears that over the extent of the latest time period specified, the quality of the health economic studies performed in the People’s Republic of China remains the same.
This systematic review reveals several areas in which improvements in methodology and reporting are possible for Chinese health economic studies. These include reporting of resource used, sensitivity analysis, presentation of study’s results with ICER, both internal and external validation of decision analytic models, transparency on source of funding, etc.
The limited role of economic evaluations in reimbursement for medical devices in the People’s Republic of China should be taken into account while interpreting the findings of our study. On the national level, the health care system was financed through out-of-pocket payments (35%), social insurance schemes (35%), and government subsidies (30%).85 However, tier III hospitals (highest tier with highly specialized services) dominated 70% of the medical device market among the top 12 cities (including Shanghai, Beijing, and Guangzhou). They have a different purchasing pattern due to a different source of revenue than tier II hospitals.86 Tier III hospitals are expected to generate at least 40% of their revenue from out-of-pocket payments, while tier II hospitals have 20% of revenue coming from out-of-pocket payments.86 This also drives tier III hospitals to procure the most advanced products to boost demand for high-end medical devices, as well as to attract complex disease treatment to enhance out-of-pocket revenue. Thus, with a demand for top medical products, the scarcity of health economic evaluations in the People’s Republic of China needs to change, to determine which of these, eg, are cost-effective so that the rural areas could also consider which of these products may be accessible for them. Fee-for-service remains the main and basic payment mechanism. In most cases, reimbursement does not cover the cost of medical devices completely and there is no established mechanism for evaluating the long-term benefits and cost-effectiveness of technologies. If the role of reimbursement from public sources grows in future, it may lead to increased demand for clinical and economic evidence of benefits of medical technologies.
Conclusion
This study indicates that there are a limited number of economic evaluations of medical devices existing in the People’s Republic of China, and these are mainly focused on cost analysis and have methodological deficiencies. Further efforts are required from different stakeholders, including academia, state institutions, and the private industry, to improve health economic research capacity and to put the results of analyses into practice to ensure that decisions in health care are based on the best available clinical and economic evidence.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Drummond MF, Sculpher MJ, Torrance GW, O’Brien BJ, Stoddart GL. Methods for the Economic Evaluation of Health Care Programmes. 3rd ed. Oxford: Oxford University Press; 2005. [Google Scholar]
- 2.Paul JE, Trueman P. ‘Fourth hurdle reviews’, NICE, and database applications. Pharmacoepidemiol Drug Saf. 2001;10(5):429–438. doi: 10.1002/pds.600. [DOI] [PubMed] [Google Scholar]
- 3.Gulácsi L, Boncz I, Drummond M. Issues for countries considering introducing the “fourth hurdle”: the case of Hungary. Int J Technol Assess Health Care. 2004;20(3):337–341. doi: 10.1017/s0266462304001151. [DOI] [PubMed] [Google Scholar]
- 4.Girling A, Young T, Brown C, Lilford R. Early-stage valuation of medical devices: the role of developmental uncertainty. Value Health. 2010;13(5):585–591. doi: 10.1111/j.1524-4733.2010.00726.x. [DOI] [PubMed] [Google Scholar]
- 5.Liu GG, Eggleston K, Hu TW. Emerging health economics and outcomes research in the Asia-Pacific region. Value Health. 2008;11(Suppl 1):S1–S2. doi: 10.1111/j.1524-4733.2008.00360.x. [DOI] [PubMed] [Google Scholar]
- 6.Tarn YH, Hu S, Kamae I, et al. Health-care systems and pharmacoeconomic research in Asia-Pacific region. Value Health. 2008;11(Suppl 1):S137–S155. doi: 10.1111/j.1524-4733.2008.00378.x. [DOI] [PubMed] [Google Scholar]
- 7.Yang BM, Lee K. Growing application of pharmacoeconomics and outcomes research in health-care decision-making in the Asia-Pacific region. Value Health. 2009;12(Suppl 3):S1–S2. doi: 10.1111/j.1524-4733.2009.00618.x. [DOI] [PubMed] [Google Scholar]
- 8.Kulsomboon V, Yang BM, Hu S. Bridging the gap in pharmacoeconomics and outcomes research between researchers, policymakers, and practitioners in the Asia-Pacific region. Value Health. 2012;15(1 Suppl):S1–S2. doi: 10.1016/j.jval.2011.11.021. [DOI] [PubMed] [Google Scholar]
- 9.CIA The World Factbook. 2013. [Accessed August 13, 2013]. Available from: https://www.cia.gov/library/publications/the-world-factbook/geos/ch.html.
- 10.Chinese Association for Medical Device Industry Market Report. 2013. [Accessed August 13, 2013]. Available from: http://www.camdi.org/news!look.action?entityId=2480.
- 11.Medical Product Outsourcing A look at the Medical Reimbursement System in China. 2007. [Accessed August 13, 2013]. Available from: http://www.mpo-mag.com/issues/2007-07/view_breaking-news/a-look-at-the-medical-reimbursement-system-in-china/
- 12.Cost-effectiveness Analysis Registry. 2013. [Accessed February 20, 2013]. Available from: https://research.tufts-nemc.org/cear4/Home.aspx.
- 13.Wanfang Data. 2011. [Accessed February 20, 2012]. Availabla from: http://www.wanfangdata.com.cn/
- 14.Wang YT, Huang G. Is FDG PET/CT cost-effective for pre-operation staging of potentially operative non-small cell lung cancer? – from Chinese healthcare system perspective. Eur J Radiol. 2012;81(8):e903–e909. doi: 10.1016/j.ejrad.2012.05.006. [DOI] [PubMed] [Google Scholar]
- 15.Zhang B, Yang B. Combined alpha fetoprotein testing and ultrasonography as a screening test for primary liver cancer. J Med Screen. 1999;6(2):108–110. doi: 10.1136/jms.6.2.108. [DOI] [PubMed] [Google Scholar]
- 16.Wei Q, Wang JG, Li LB, Li JD. Management of choledocholithiasis: comparison between laparoscopic common bile duct exploration and intraoperative endoscopic sphincterotomy. World J Gastroenterol. 2003;9(12):2856–2858. doi: 10.3748/wjg.v9.i12.2856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim JJ, Leung GM, Woo PP, Goldie SJ. Cost-effectiveness of organized versus opportunistic cervical cytology screening in Hong Kong. J Public Health (Oxf) 2004;26(2):130–137. doi: 10.1093/pubmed/fdh138. [DOI] [PubMed] [Google Scholar]
- 18.Woo PP, Kim JJ, Leung GM. What is the most cost-effective population-based cancer screening program for Chinese women? J Clin Oncol. 2007;25(6):617–624. doi: 10.1200/JCO.2006.06.0210. [DOI] [PubMed] [Google Scholar]
- 19.Wong IO, Kuntz KM, Cowling BJ, Lam CL, Leung GM. Cost effectiveness of mammography screening for Chinese women. Cancer. 2007;110(4):885–895. doi: 10.1002/cncr.22848. [DOI] [PubMed] [Google Scholar]
- 20.Wong IO, Kuntz KM, Cowling BJ, Lam CL, Leung GM. Cost-effectiveness analysis of mammography screening in Hong Kong Chinese using state-transition Markov modelling. Hong Kong Med J. 2010;16(Suppl 3):38–41. [PubMed] [Google Scholar]
- 21.Wong IO, Tsang JW, Cowling BJ, Leung GM. Optimizing resource allocation for breast cancer prevention and care among Hong Kong Chinese women. Cancer. 2012;118(18):4394–4403. doi: 10.1002/cncr.27448. [DOI] [PubMed] [Google Scholar]
- 22.Chen Z, Chen L, Wu L. Transcatheter amplatzer occlusion and surgical closure of patent ductus arteriosus: comparison of effectiveness and costs in a low-income country. Pediatr Cardiol. 2009;30(6):781–785. doi: 10.1007/s00246-009-9440-3. [DOI] [PubMed] [Google Scholar]
- 23.Cheng MM, Lu B, Hu SS, et al. Optimizing CAD diagnosis in China with CT angiography. J Cardiovasc Comput Tomogr. 2009;3(3):153–158. doi: 10.1016/j.jcct.2009.03.005. [DOI] [PubMed] [Google Scholar]
- 24.Gong K, Zhang N, Lu Y, et al. Comparison of the open tension-free mesh-plug, transabdominal preperitoneal (TAPP), and totally extraperitoneal (TEP) laparoscopic techniques for primary unilateral inguinal hernia repair: a prospective randomized controlled trial. Surg Endosc. 2011;25(1):234–239. doi: 10.1007/s00464-010-1165-0. [DOI] [PubMed] [Google Scholar]
- 25.Feng B, Zhu QL, Xia Y, et al. Direct and indirect costs and long-term survival of laparoscopic anterior resection for rectal cancer. Med Sci Monit. 2010;16(12):H97–H102. [PubMed] [Google Scholar]
- 26.Chen Q, Chen LW, Cao H, Zhang GC, Chen DZ, Zhang H. Intraoperative device closure of atrial septal defects with inferior vena cava rim deficiency: a safe alternative to surgical repair. J Thorac Cardiovasc Surg. 2011;141(3):631–636. doi: 10.1016/j.jtcvs.2010.07.077. [DOI] [PubMed] [Google Scholar]
- 27.Zang J, Zhang C, Zhou H, Gao J. Early laparoscopic cholecystectomy after endoscopic common bile duct stone extraction: the experience from a developing country. Surg Laparosc Endosc Percutan Tech. 2011;21(2):120–122. doi: 10.1097/SLE.0b013e318213c7b8. [DOI] [PubMed] [Google Scholar]
- 28.Gurbanov E, Meng X, Cui Y, et al. Evaluation ECMO in adult cardiac transplantation: can outcomes of marginal donor hearts be improved? J Cardiovasc Surg (Torino) 2011;52(3):419–427. [PubMed] [Google Scholar]
- 29.Zhang J, Shi Q, Wang GZ, Wang F, Jiang N. Cost-effectiveness analysis of ureteroscopic laser lithotripsy and shock wave lithotripsy in the management of ureteral calculi in eastern China. Urol Int. 2011;86(4):470–475. doi: 10.1159/000324479. [DOI] [PubMed] [Google Scholar]
- 30.Liu X, Jia X, Guo W, et al. Ultrasound-guided foam sclerotherapy of the great saphenous vein with sapheno-femoral ligation compared to standard stripping: a prospective clinical study. Int Angiol. 2011;30(4):321–326. [PubMed] [Google Scholar]
- 31.Wong EM, Rainer TH, Ng YC, Chan MS, Lopez V. Cost-effectiveness of Dermabond versus sutures for lacerated wound closure: a randomised controlled trial. Hong Kong Med J. 2011;17(Suppl 6):4–8. [PubMed] [Google Scholar]
- 32.Xie Y, Fu Q, Chen ZQ, et al. Comparison between two pedicle screw augmentation instrumentations in adult degenerative scoliosis with osteoporosis. BMC Musculoskelet Disord. 2011;12:286. doi: 10.1186/1471-2474-12-286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lu Z, Yi X, Feng W, et al. Cost-benefit analysis of laparoscopic surgery versus laparotomy for patients with endometrioid endometrial cancer: experience from an institute in China. J Obstet Gynaecol Res. 2012;38(7):1011–1017. doi: 10.1111/j.1447-0756.2011.01820.x. [DOI] [PubMed] [Google Scholar]
- 34.Yang J, Wei WQ, Niu J, Liu ZC, Yang CX, Qiao YL. Cost-benefit analysis of esophageal cancer endoscopic screening in high-risk areas of China. World J Gastroenterol. 2012;18(20):2493–2501. doi: 10.3748/wjg.v18.i20.2493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sheng QS, Lin JJ, Chen WB, et al. Hand-assisted laparoscopic versus open right hemicolectomy: short-term outcomes in a single institution from China. Surg Laparosc Endosc Percutan Tech. 2012;22(3):267–271. doi: 10.1097/SLE.0b013e3182516577. [DOI] [PubMed] [Google Scholar]
- 36.Wang ZH, Gao QY, Fang JY. Repeat colonoscopy every 10 years or single colonoscopy for colorectal neoplasm screening in average-risk Chinese: a cost-effectiveness analysis. Asian Pac J Cancer Prev. 2012;13(5):1761–1766. doi: 10.7314/apjcp.2012.13.5.1761. [DOI] [PubMed] [Google Scholar]
- 37.Huang LH, Zhang L, Tobe RY, et al. Cost-effectiveness analysis of neonatal hearing screening program in China: should universal screening be prioritized? BMC Health Serv Res. 2012;12:97. doi: 10.1186/1472-6963-12-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wu JX, Li B, Liu T, et al. Eighty-six cases of laparoscopic vaginoplasty using an ileal segment. Chin Med J. 2009;122(16):1862–1866. [PubMed] [Google Scholar]
- 39.Xia W, She S, Lam TH. Medical versus surgical abortion methods for pregnancy in China: a cost-minimization analysis. Gynecol Obstet Invest. 2011;72:257–263. doi: 10.1159/000328313. [DOI] [PubMed] [Google Scholar]
- 40.Chen M, Li Z, He Q, et al. A prospective cost-utility study of early renal replacement therapy. Chin J Evid Based Med. 2004;4(7):453–459. [Google Scholar]
- 41.Chen L, Huang R, Xiao J, et al. Cost analysis of laparoscopy in treatment of acute abdomen. Zh J Traumatic. 2012;17(4):436–438. [Google Scholar]
- 42.Fan H. Validity evaluation and cost-effectiveness of CT and MRI for diagnosis of cerebrovascular disease, Thesis. Shanxi Medical University; Shanxi: 2007. [Google Scholar]
- 43.Gu A, Liu J, Sun X, Shi Y, Huang G. Cost-effective analysis of PET application in NSCLC. Chin J Nucl Med. 2006;26(2):89–92. [Google Scholar]
- 44.Fu M, Gu Y, Song D, Leng B, Wang Q, Ying X. Comparison of outcome and cost of endovascular coiling versus surgical clipping in the treatment of ruptured anterior or posterior communicating artery aneurysm aneurysms. Int J Cerebrovasc Dis. 2011;19(4):269–274. [Google Scholar]
- 45.Guan Y, Cao B, Liu X, Zhao X, Liu J, Huang L. Comparison in health economics between laparoscopic and open myomectomy. Chin Med Factory Mine. 2007;20(3):253–254. [Google Scholar]
- 46.Guo X, Liu M, Yan R, Li W, Zhang J, Guo Y. Economic analysis of the imaging diagnosis for small hepatoma. Chin Med Dev. 2009;24(7):9–13. [Google Scholar]
- 47.Han Q, Qi M, Jia Y, Zhao H. Cost-effectiveness analysis of long-time domiciliary noninvasive positive pressure ventilation in the treatment of chronic obstructive pulmonary disease complicated with chronic respiratory failure. Int J Respir. 2011;31(5):348–350. [Google Scholar]
- 48.He T, Liu L, Liang X, Zhou J, Xie X, Dai Q. Analysis of effectiveness and health economics of myomectomy using laparoscopy and laparotomy. J Gannan Med Uni. 2012;32(1):78–79. [Google Scholar]
- 49.Hou X, Yang X, Zen Q, Huang H, Huang J. Cost-effectiveness of dual-source CT in the evaluation of patients with chest pain. Chin Mod Med. 2011;18(25):83–84. [Google Scholar]
- 50.Gen Y. Retrospective economic analysis in the cost and disease burden of hemodialysis and peritoneal dialysis, Thesis. Tianjin Medical University; Tianjin: 2008. [Google Scholar]
- 51.Guo Y. Percutaneous transhepatic metal versus plastic stent implantation for treating malignant biliary obstruction: influence factors of clinical efficacy and cost-effectiveness analysis (A multiple center research), Thesis. First Military Medical University; Guangzhou: 2001. [Google Scholar]
- 52.Lan H, Huang B, Wang S, Tan X, Liao Y, Qin T. Analysis of care costs of tube-humidifying systems in different breathing machines. J Nur. 2007;14(6):1–4. [Google Scholar]
- 53.Li W, Liu Y. Cost analysis of laparoscopy in treatment of tubal pregnancy. Acad J Sec Mil Med Univ. 2003;24(3):282–284. [Google Scholar]
- 54.Liu J, Liu H, Li T, et al. Coflex interspinous dynamic reconstruction and 360° fusion for single level lumbar degenerative disease: a cost-utility analysis. Chin J Evid Based Med. 2011;11(8):893–898. [Google Scholar]
- 55.Ma C, Bu X, Zhou W, et al. Efficacy and cost analysis of microsurgical clipping and vascular embolization in treatment of patients with cerebral aneurysms. Chin J Neuromed. 2012;11(7):709–712. [Google Scholar]
- 56.Peng L, Tan C, Chen G, et al. Studies on the methods of cost-utility analysis for cholelithiasis surgery patients. J Chin Pharm. 2007;18(29):2245–2247. [Google Scholar]
- 57.Tan XJ, Lang JH, Shen K, et al. Operative approaches, indications, and medical economics evaluation of 4180 cases of hysterectomy. Acta Acad Med Sin. 2003;25(4):406–409. [PubMed] [Google Scholar]
- 58.Tan H. Laparoscopic versus open common bile duct exploration and choledocholithotomy: a review study of outcomes, quality of life, and costs, Thesis. Peking Union Medical College; Beijing: 2007. [Google Scholar]
- 59.Wang D, Wang M, Liu K, et al. Cost-effectiveness analysis on surgical treatment for intracerebral hemorrhage. Chin J Med Guide. 2006;8(2):127–130. [Google Scholar]
- 60.Wang X, Lu J, Yu W, Wei Y, Fang M, Ouyang J. Comparison of clinical effect and costs between percutaneous vertebroplasty and kyphoplasty for the treatment of acute osteoporotic vertebral mild compression fractures. Cli Orthop. 2012;15(2):125–128. [Google Scholar]
- 61.Wei X, Lu Y, Yang H, et al. Cost-effectiveness and outcome analysis of laparoscopic modity hysterectomy for cervical carcinoma in early stage. Chin J Endoscopy. 2011;17(3):243–246. [Google Scholar]
- 62.Wen J, Ji Y, Zheng Z, Ma Z, Peng Y, Yu X. Cost-effectiveness analysis of hemodialysis, CAPD and kidney transplantation. Chin J Nephrol. 2005;21(10):616–619. [Google Scholar]
- 63.Xia J. Efficacy and cost analysis of laparoscopic and open surgery for colon cancer. Guide Chin Med. 2010;8(22):141–143. [Google Scholar]
- 64.Yu N. Assessment of laparoscopic hernia repair: its safety, effectiveness and economy, Thesis. Fudan University; Shanghai: 2007. [Google Scholar]
- 65.Zhou S, Liu Q, Gong L. Comparison of laparoscopic and open anterior resection for rectal cancer with anal sphincter preservation. Chin J Endoscopy. 2011;17(7):695–698. [Google Scholar]
- 66.Wu S, Zen Z. Health economic evaluation of the small incision phacoemulsification cataract surgery by the clinical pathway in the primary hospital. Int J Ophthalmol. 2010;10(11):2171–2173. [Google Scholar]
- 67.Liu B, Chen X, Lin X, et al. The cost-effective comparison of laparoscopic splenectomy by two different pedicle division strategy for the treatment of ITP. J Hepatopancreatobil Surg. 2011;23(1):31–34. [Google Scholar]
- 68.Han Y, Hao G, Chen B, Zen L, Liu Q. Clinical economical evaluation for three surgery methods of angle-closure glaucoma combined cataract. J Clin Ophthalmol. 2006;14(3):238–240. [Google Scholar]
- 69.Liu C, Li JG, Zhou Q, et al. The cost-efficiency and safety of bedside forceps dilatational tracheostomy in the intensive care unit. Chin Crit Care Med. 2010;22(9):537–539. [PubMed] [Google Scholar]
- 70.Lv F, Tang J, Luo Y, et al. Cost-effectiveness analysis of the focal injection treatment of the severe abdominal parenchymal organs trauma. Chin J Ultrasonogr. 2011;20(1):34–37. [Google Scholar]
- 71.Garattini L, De Compadri P, Clemente R, Cornago D. Economic evaluations in Italy: a review of the literature. Int J Technol Assess Health Care. 2003;19(4):685–691. doi: 10.1017/s0266462303000643. [DOI] [PubMed] [Google Scholar]
- 72.Al-Aqeel SA. State of health economic evaluation research in Saudi Arabia: a review. Clinicoecon Outcomes Res. 2012;4:177–184. doi: 10.2147/CEOR.S31087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Machado M, Iskedjian M, Einarson TR. Quality assessment of published health economic analyses from South America. Ann Pharmacother. 2006;40(5):943–949. doi: 10.1345/aph.1G296. [DOI] [PubMed] [Google Scholar]
- 74.Sorenson C, Tarricone R, Siebert M, Drummond M. Applying health economics for policy decision making: do devices differ from drugs? Europace. 2011;13(Suppl 2):ii54–ii58. doi: 10.1093/europace/eur089. [DOI] [PubMed] [Google Scholar]
- 75.Yothasamut J, Tantivess S, Teerawattananon Y. Using economic evaluation in policy decision-making in Asian countries: mission impossible or mission probable? Value Health. 2009;12(Suppl 3):S26–S30. doi: 10.1111/j.1524-4733.2009.00623.x. [DOI] [PubMed] [Google Scholar]
- 76.Husereau D, Drummond M, Petrou S, et al. ISPOR Health Economic Evaluation Publication Guidelines-CHEERS Good Reporting Practices Task Force Consolidated Health Economic Evaluation Reporting Standards (CHEERS) – explanation and elaboration: a report of the ISPOR Health Economic Evaluation Publication Guidelines Good Reporting Practices Task Force. Value Health. 2013;16(2):231–250. doi: 10.1016/j.jval.2013.02.002. [DOI] [PubMed] [Google Scholar]
- 77.Kang M, Zhao Y, Huang Y, Li J, Liu L, Li H. Accuracy and direct medical cost of different screening modalities for breast cancer among Chinese women. Zhonghua Zhong Liu Za Zhi. 2014;36(3):236–240. Chinese. [PubMed] [Google Scholar]
- 78.Zhang XG, Zhang ZL, Hu SY, Wang YL. Ultrasound-guided ablative therapy for hepatic malignancies: a comparison of the therapeutic effects of microwave and radiofrequency ablation. Acta Chir Belg. 2014;114(1):40–45. [PubMed] [Google Scholar]
- 79.Tao MF, Rong R, Shao HF, Xia J. The cost-effectiveness analysis of laparoscopic treatment of ectopic pregnancy: a single-center review of a five-year experience. Clin Exp Obstet Gynecol. 2014;41(1):24–27. [PubMed] [Google Scholar]
- 80.Cheng Y, Jiang ZS, Xu XP, et al. Laparoendoscopic single-site cholecystectomy vs three-port laparoscopic cholecystectomy: a large-scale retrospective study. World J Gastroenterol. 2013;19(26):4209–4213. doi: 10.3748/wjg.v19.i26.4209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Shen D, Ye H, Wang Y, et al. Comparison of short-term outcomes between laparoscopic greater curvature plication and laparoscopic sleeve gastrectomy. Surg Endosc. 2013;27(8):2768–2774. doi: 10.1007/s00464-013-2805-y. [DOI] [PubMed] [Google Scholar]
- 82.Ke S, Ding XM, Gao J, et al. A prospective, randomized trial of Roux-en-Y reconstruction with isolated pancreatic drainage versus conventional loop reconstruction after pancreaticoduodenectomy. Surgery. 2013;153(6):743–752. doi: 10.1016/j.surg.2013.02.008. [DOI] [PubMed] [Google Scholar]
- 83.Wong C, Luk IW, Ip M, You JH. Prevention of gram-positive infections in peritoneal dialysis patients in Hong Kong: a cost-effectiveness analysis. Am J Infect Control. 2014;42(4):412–416. doi: 10.1016/j.ajic.2013.12.008. [DOI] [PubMed] [Google Scholar]
- 84.Tobe RG, Mori R, Huang L, Xu L, Han D, Shibuya K. Cost- effectiveness analysis of a national neonatal hearing screening program in China: conditions for the scale-up. PLoS One. 2013;8(1):e51990. doi: 10.1371/journal.pone.0051990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.China Ministry of Health 2012 China Healthcare Development Report. 2013. [Accessed August 19, 2013]. Available from: http://www.moh.gov.cn/mohwsbwstjxxzx/s7967/201306/fe0b764da4f74b858eb55264572eab92.shtml.
- 86.Yarwood J. Growth status and market environment of medical supplies in China; 4th China International Medical Device Summit; Shanghai, China. 2013. [Google Scholar]