Introduction
Hemangiomas and other vascular anomalies are common in infants and sometimes involve periocular areas. Amblyopia can occur by any or all of three mechanisms in this situation: occlusion of the visual axis by the tumor, anisometropia or strabismus. Some children have periocular masses that intermittently obstruct vision when the child looks in the direction of the lesion, but no clinical signs of amblyopia. Vernier acuity measures are sensitive for the detection of amblyopia1, 2 and other types of visual deprivation, including cortical visual impairment3. To learn whether these infants showed evidence of amblyopia despite normal clinical examinations, we measured vernier acuity, comparing the affected eye with the fellow eye.
Methods
Four consecutive infants with unilateral periocular vascular lesions that intermittently obstructed vision in the affected eye, and no clinical evidence of amblyopia were evaluated. Children ranged in age from 7 to 19 months (Figure 1). All underwent a complete eye examination, which showed normal findings except for the vascular marks. No child had anisometropia greater than 0.50 D in the greatest meridian as measured by cyclopleged exam, human observation. None had strabismus, and no child showed a fixation preference. One infant (Figure 1 Top left) had evidence of PHACES syndrome (posterior fossa, hemangioma, arterial, cardiac, sternal abnormality) with CNS arterial anomalies but no associated retinal/ocular pathology. One child had an orbital venous malformation at birth which caused nearly complete visual axis obstruction prompting partial debulking surgery at 4 weeks of age (Figure 1 Bottom right). Three (Figure 1 Top left, Top right and Bottom left) had infantile hemangiomas. Sweep Visual Evoked Potential (VEP) vernier acuity was measured under monocular viewing conditions with the fellow eye tested as the control. Details of this procedure have been described previously4. Briefly, subjects were shown a swept vernier offset stimulus where the vernier offsets ranged from 8 to 0.5 arc min. The offsets were periodically presented and withdrawn at 3.76 Hz (space average luminance of 110 cd/m2 and Michelson contrast of 80% condition; see Figure 2 for a schematic illustration of the stimulus sequence). Signals were averaged over multiple trials. Thresholds, sweep amplitudes, and temporal phase analyses were performed.
Figure 1. Preverbal children with orbital vascular birthmarks.
Photographs of the lesions in 7 to 19 month old preverbal children who had sweep VEP vernier acuity measurements. One had PHACES syndrome (Top left) but no associated retinal/ocular pathology. One child had an orbital veinous malformation which caused nearly complete visual axis obstruction at birth prompting partial debulking surgery at 4 weeks of age (Bottom right). Three (Top left, Top right and Bottom left) had infantile hemangiomas.
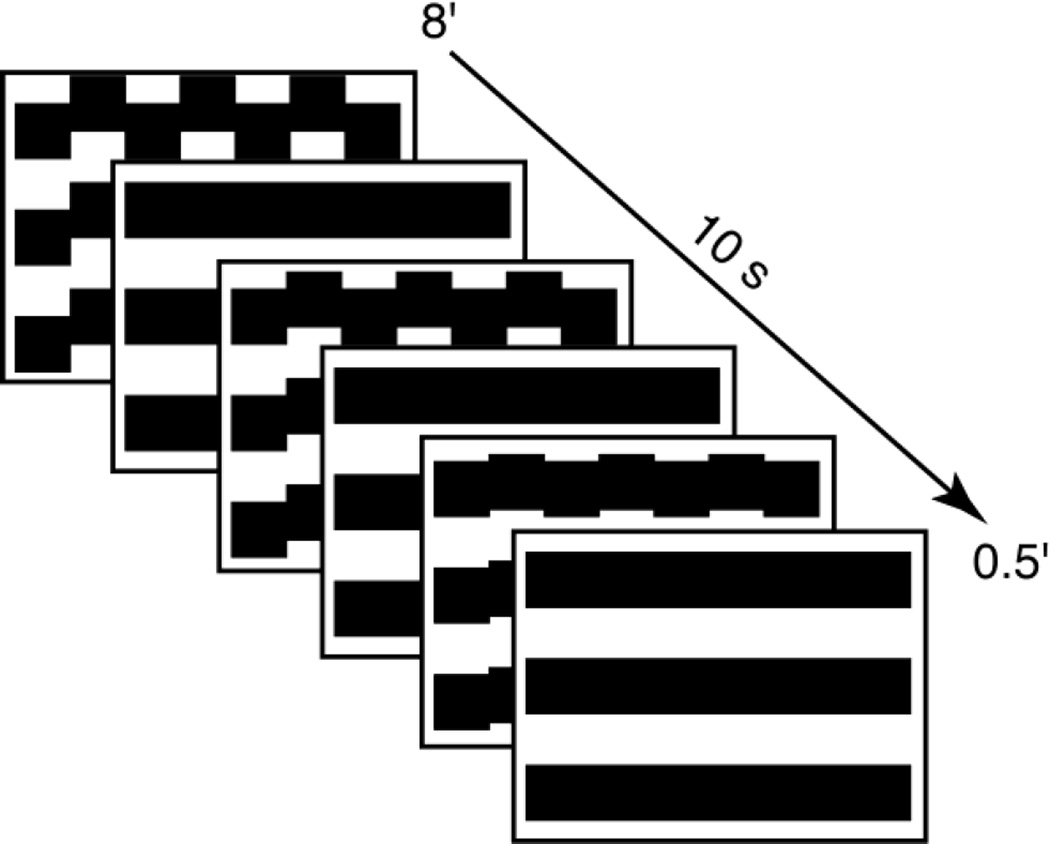
Figure 2. Schematic diagram of sweep VEP stimuli used to measure vernier acuity in preverbal children with orbital vascular birthmarks.
Square-wave gratings contain vernier displacements of every other column of the grating, which alternated between alignment and misalignment states at 3.76 Hz. Over a period of 10 seconds, the size of vernier displacement was decreased from 8 to 0.5 arc min in 10 equal logarithmic steps. There were approximately 400 vernier offsets over the 12° × 9° display area.
Results
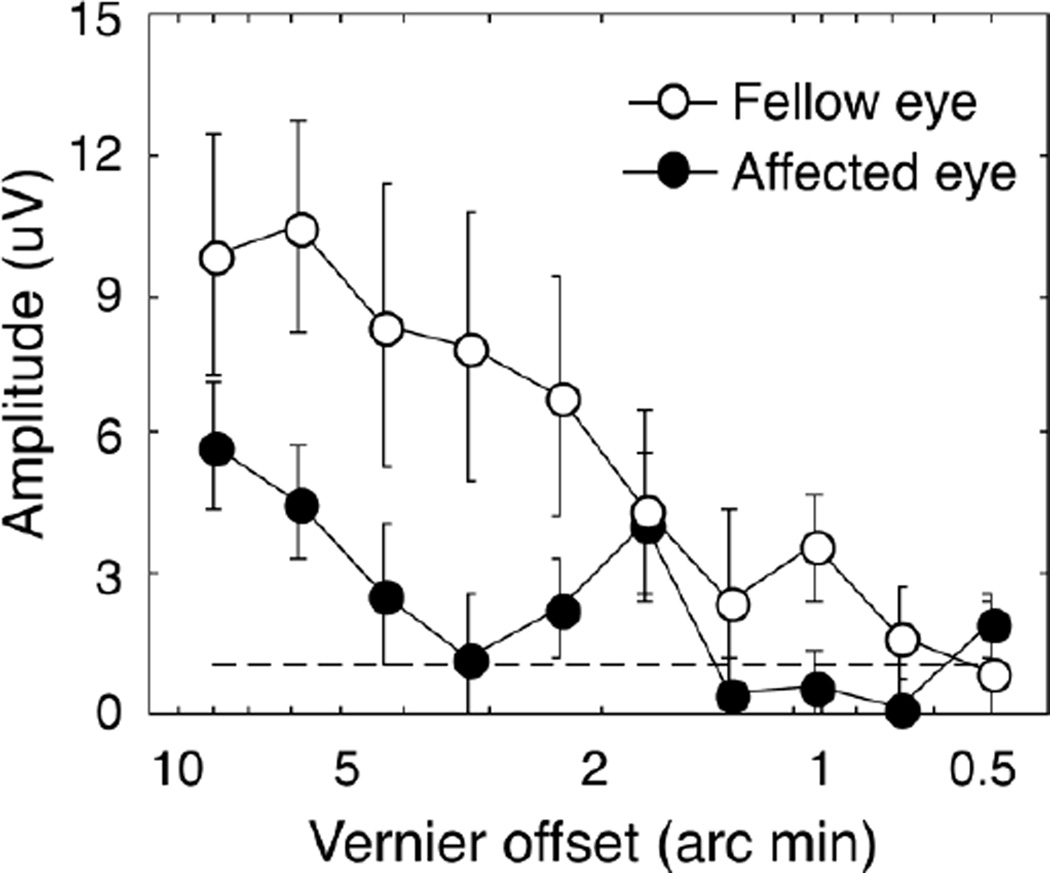
Figure 3 shows vector-averaged response amplitudes as a function of stimulus visibility. VEP vernier amplitudes were diminished across most of the sweep range in the affected eyes, with the effect being most pronounced at the most visible end of the sweep. Vernier acuity thresholds were also higher (worse) in the affected eyes: two affected eyes had measurable thresholds that were a factor of 3–4 times worse than in the fellow eye. The other two affected eyes had immeasurable thresholds while the fellow eyes had measurable thresholds.
Figure 3. Average of sweep VEP signal responses for 4 children with orbital vascular birthmarks that caused intermittent occlusion of the visual axis.
Vector-averaged responses of first harmonics (1f1) at Oz derivation across 4 patients for affected eyes (filled circles) and fellow eyes (open circles). Error bars plot SEMs. The dash line shows the noise level of the EEG. Response amplitudes were diminished in the affected eyes compared with the fellow eyes.
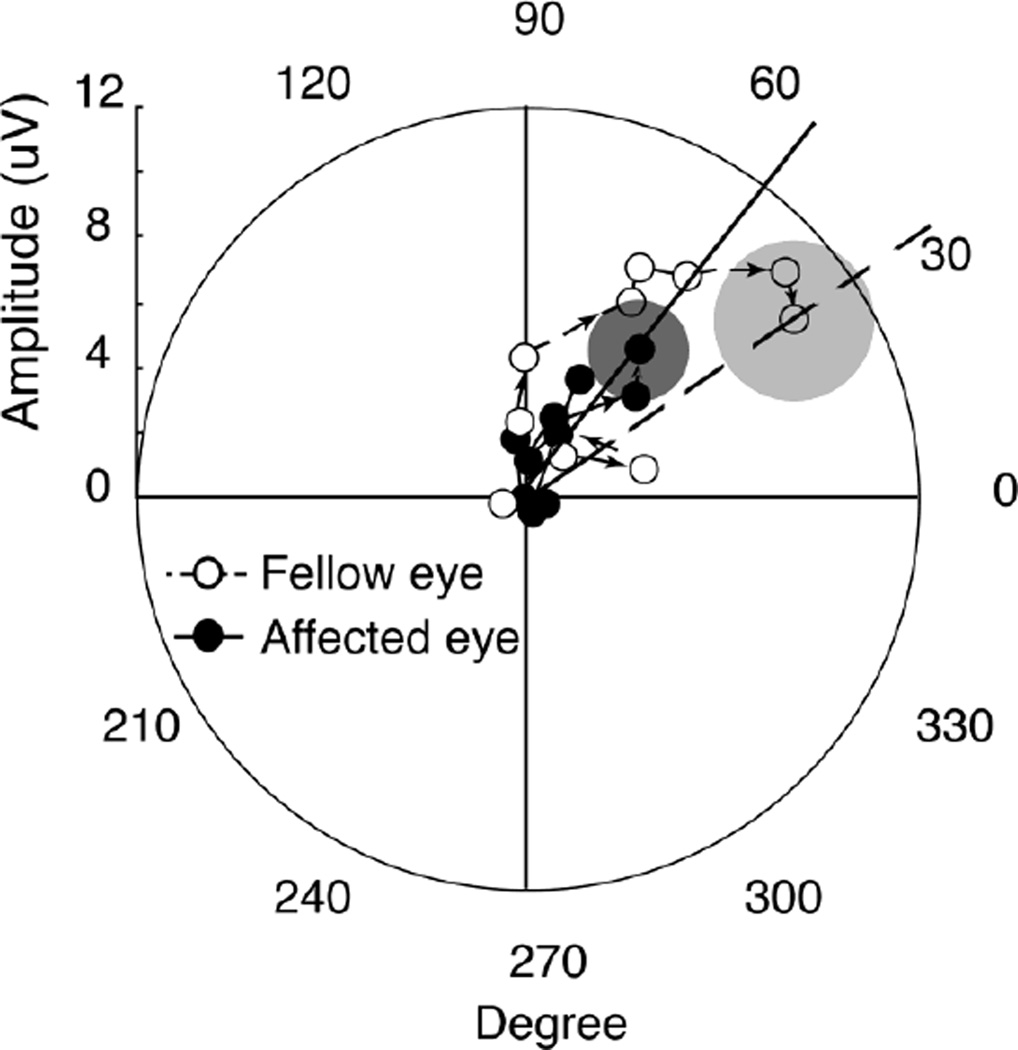
A phase analysis showed a significant slowing of the response in the affected eyes. Figure 4 shows a polar plot of the amplitude and phase of the first harmonic response at Oz derivation. The phase of the response, averaged across the four participants, was lagged by a greater amount than in the fellow eye, consistent with a slowing of the evoked response.
Figure 4. Polar plot showing amplitude and phase of responses for 4 children with orbital vascular birthmarks.
Polar plot of the amplitude and phase of the first harmonic response at Oz derivation in affected eyes (filled circles) and fellow eyes (open circles) are shown. Arrows indicate the direction of increasing vernier offsets; i.e., moving radially from the center and out increases the visibility of the offsets. The circles plot +/−1 SEM of the vector mean for the largest vernier offset (8 arc min). Lines indicate the phase at the largest vernier offset in affected eyes (solid line) and fellow eyes (dashed line). The phase of the largest vernier offset response shows slowing of the response in the affected eyes (53°) compared with the fellow eyes (34°). Response amplitudes were diminished in the affected eyes, relative to the fellow eyes. This is demonstrated by the distance of the vector from the center of the plot.
Discussion
When children look in the direction of an adnexal mass, the affected eye may be covered, resulting in intermittent occlusion of vision in the affected eye. Any resultant visual deprivation in this clinical situation is transient, occurs for a few seconds, but is repeatedly present throughout the day. In this report, four such children showed vernier acuity deficits consistent with amblyopia. In three, the mass was on the upper eyelid, and in one, the lower lid. None had any clinical signs of amblyopia, including no anisometropia or strabismus
Vernier acuity measures are sensitive for the detection of amblyopia1, 2, 5 and other types of visual deprivation, including cortical visual impairment3. In this experiment, we measured vernier acuity because the ability to detect linear offsets is a surrogate for optoptype acuity measures6, 7 and could be more sensitive for the detection of amblyopia than grating acuity1.
The children we studied showed elevated (worse) vernier acuity thresholds, reduced signal amplitudes, and delayed signal conduction, all findings pointing to an adverse effect on the visual system, caused by intermittent occlusion of the visual axis. These findings are similar to those seen in amblyopia and other conditions that adversely affect vision, including cortical visual impairment seen in children with central nervous system injury3, 8.
The human visual system shows remarkable plasticity. Part time occlusion in the management of amblyopia is now a well-established and effective approach9. The visual system in young children shows such plasticity, that it is likely that even an hour of daily patching of the normal eye can improve an amblyopic eye. In our study, where occlusion was not administered therapeutically, occlusion occurred at high frequency but short duration, and measurable effects resulted. However, until children with periodically-interrupted visual experience can be followed to a later age, the clinical significance of high-frequency, intermittent occlusion cannot be determined. While this is a small study (of only four infants), the findings raise enough concerns to suggest studying a larger number of Infants and continuing with longer term follow up of children with intermittent occlusion, to ensure that long term adverse clinical effects do not occur.
Acknowledgements
THIS STUDY WAS SUPPORTED BY THE NATIONAL EYE INSTITUTE, NATIONAL INSTITUTES OF HEALTH. All patients gave their written informed consent to participate. The research protocol was approved by the Institutional Review Board at Smith-Kettlewell Eye Research Institute. It was performed in accordance with the Declaration of Helsinki and in adherence of federal laws. The authors would like to thank National Institutes of Health for the financial support of the study.
Footnotes
The authors indicate no financial conflict of interest.
Contributions of Authors: conception and design (W.V.G; I.J.F.); analysis and interpretation, critical revision and final approval (W.V.G; C.H.; I.J.F.; A.M.N.); statistical expertise (W.V.G; C.H.; A.M.N.); obtaining funding (W.V.G; A.M.N.); writing the article (W.V.G; C.H.; A.M.N.); data collection (W.V.G; C.H.); provision of materials, patients, or resources (W.V.G; C.H.; I.J.F.); literature search (W.V.G; C.H.).
References
- 1.Levi DM, Klein S. Hyperacuity and amblyopia. Nature. 1982;298:268–270. doi: 10.1038/298268a0. [DOI] [PubMed] [Google Scholar]
- 2.Levi DM, Klein SA. Vernier acuity, crowding and amblyopia. Vision Res. 1985;25:979–991. doi: 10.1016/0042-6989(85)90208-1. [DOI] [PubMed] [Google Scholar]
- 3.Skoczenski AM, Good WV. Vernier acuity is selectively affected in infants and children with cortical visual impairment. Dev Med Child Neurol. 2004;46:526–532. doi: 10.1017/s001216220400088x. [DOI] [PubMed] [Google Scholar]
- 4.Mirabella G, Kjaer PK, Norcia AM, Good WV, Madan A. Visual development in very low birth weight infants. Pediatr Res. 2006;60:435–439. doi: 10.1203/01.pdr.0000238249.44088.2c. [DOI] [PubMed] [Google Scholar]
- 5.Levi DM, Klein S. Differences in vernier discrimination for grating between strabismic and anisometropic amblyopes. Invest Ophthalmol Vis Sci. 1982;23:398–407. [PubMed] [Google Scholar]
- 6.Hou C, Good WV, Norcia AM. Validation study of VEP vernier acuity in normal-vision and amblyopic adults. Invest Ophthalmol Vis Sci. 2007;48:4070–4078. doi: 10.1167/iovs.06-1368. [DOI] [PubMed] [Google Scholar]
- 7.McKee SP, Levi DM, Movshon JA. The pattern of visual deficits in amblyopia. J Vis. 2003;3:380–405. doi: 10.1167/3.5.5. [DOI] [PubMed] [Google Scholar]
- 8.Good WV. Development of a quantitative method to measure vision in children with chronic cortical visual impairment. Trans Am Ophthalmol Soc. 2001;99:253–269. [PMC free article] [PubMed] [Google Scholar]
- 9.Wallace DK, Edwards AR, Cotter SA, et al. A randomized trial to evaluate 2 hours of daily patching for strabismic and anisometropic amblyopia in children. Ophthalmology. 2006;113:904–912. doi: 10.1016/j.ophtha.2006.01.069. [DOI] [PMC free article] [PubMed] [Google Scholar]