Abstract
Background
Estimates of dengue transmission intensity remain ambiguous. Since the majority of infections are asymptomatic, surveillance systems substantially underestimate true rates of infection. With advances in the development of novel control measures, obtaining robust estimates of average dengue transmission intensity is key for assessing both the burden of disease from dengue and the likely impact of interventions.
Methodology/Principal Findings
The force of infection (λ) and corresponding basic reproduction numbers (R0) for dengue were estimated from non-serotype (IgG) and serotype-specific (PRNT) age-stratified seroprevalence surveys identified from the literature. The majority of R0 estimates ranged from 1–4. Assuming that two heterologous infections result in complete immunity produced up to two-fold higher estimates of R0 than when tertiary and quaternary infections were included. λ estimated from IgG data were comparable to the sum of serotype-specific forces of infection derived from PRNT data, particularly when inter-serotype interactions were allowed for.
Conclusions/Significance
Our analysis highlights the highly heterogeneous nature of dengue transmission. How underlying assumptions about serotype interactions and immunity affect the relationship between the force of infection and R0 will have implications for control planning. While PRNT data provides the maximum information, our study shows that even the much cheaper ELISA-based assays would provide comparable baseline estimates of overall transmission intensity which will be an important consideration in resource-constrained settings.
Author Summary
With an estimated 390 million infections each year, dengue imposes a significant global public health burden. Yet estimates of the intensity of dengue transmission in different settings are still sparse, making it difficult to plan efficient control programs. Since many dengue infections have no symptoms, cases reported through hospitals are only a small proportion of true cases. The authors used seroprevalence surveys which can detect all past infections to estimate dengue transmission intensity in 22 countries. Estimates derived from data collected using cheaper diagnostic tests were comparable to those making use of more expensive tests, an important conclusion for surveillance in resource constrained countries. We found dengue transmission intensity varied up to 4-fold in endemic settings, with estimates showing some sensitivity to how many dengue infections were assumed to confer complete immunity.
Introduction
Affecting more than one hundred countries with 2.5 billion people at risk and 50–100 million infections per year as estimated by the World Health Organisation (WHO), dengue is a global public health burden [1]. Estimates of global dengue distribution and transmission intensity (as quantified by either the force of infection—the per capita rate at which susceptible individuals acquire infection, or the basic reproduction number, (R 0) remain ambiguous [2]. Infection with any of the four serotypes of dengue virus (DENV-1, 2, 3, and 4) can cause dengue fever with increased risk of more severe dengue with subsequent heterologous infections. Individuals develop protective monotypic immunity upon infection with a single serotype. Cross-reactive immunity is short-lived and the waning of antibodies below a threshold can facilitate antibody-dependent enhancement (ADE) upon secondary heterologous infection increasing the risk of more severe outcomes of dengue (such as dengue haemorrhagic fever (DHF) and shock syndrome (DSS)) [3–5]. The impact of cross-immunity and tertiary and quaternary infections are controversial. The estimated duration of short-term cross-protection varies widely from four months to 9 years [6], 5–12 months [7], 2 years [8], and 1–3 years [9]. However whether this protects against infection or clinically apparent disease is unknown. Therefore individuals may still contribute to onward transmission [8,10,11]. Clinically apparent tertiary and quaternary infections are rarely reported, and cannot be tested for retrospectively [10]. Wikramaratna et al. showed that tertiary and quaternary infections allows for the high seroprevalence at very young ages observed in Haiti [12] and Nicaragua [13] better than when assuming complete protection after two heterologous infections [10]. There are no antiviral therapies available as yet and disease control is restricted to vector control, community education and the development of an effective dengue vaccine.
Recent estimates of the global distribution of dengue and the resulting disease burden have refined our understanding, but remain controversial [2]. Shepard et al. highlight some of the difficulties in accurate dengue burden estimation including differences in surveillance systems leading to underestimation of dengue incidence, the lack of standardized reporting procedures or diagnostic criteria, and the lack of integration between private and public sectors [14]. Previous studies have attempted to estimate the burden of dengue and associated economic costs in South East Asia and South America by calculating expansion factors from systematic literature reviews, collation of existing data, and population-based cohorts [15–18]. In particular, Bhatt et al.’s estimate of 390 million dengue infections per year is three times higher than previous official WHO estimates, with India accounting for 34% of that total [2]. Motivated by previous work on malaria, the Bhatt et al. analysis relied on correlating their geographic niche-modelling based estimates of dengue presence with burden estimates derived from serological surveys. While an improvement on previous approaches, the fact that dengue infection induces serotype specific neutralising immunity weakens the parallels with malaria, in that the maximum number of dengue infections an individual can experience is strictly limited (while a person can experience dozens of malaria infections in their lifetime). Here we argue that obtaining robust estimates of the geographic variation in average dengue transmission intensity—as quantified by the basic reproduction number, R 0 (the average number of secondary cases resulting from the introduction of a single infectious individual into a large susceptible population [19]), of each serotype—is key to improving the reliability of burden estimates. In addition, a quantitative understanding of variation in transmission intensity is essential to assessing the likely impact of interventions such as vaccine [20,21] or novel vector control measures [22–24].
However, with no standardised diagnostic method, challenging clinical diagnosis (Box 1) and highly variable surveillance systems, there is no consistent way to estimate global dengue transmission [25–27]. Dengue transmission is geographically highly heterogeneous, even down to very fine spatial scales [28]. Most model-based estimates of dengue transmission intensity and reproduction number have utilised case-notification data, which heavily depend on the quality of the surveillance system and the health infrastructure of the country in question [29–36]. Additionally, since the majority of dengue infections generate only mild symptoms, are asymptomatic, or are clinically diagnosed as a viral infection, even sensitive healthcare-based surveillance systems substantially underestimate true rates of infection [37,38]. Serological data are therefore invaluable in quantifying dengue transmission, in being able to identify both symptomatic and asymptomatic past infections and thus quantify infection prevalence and incidence in the population as a whole.
Box 1. Main issues associated with current diagnostic methods.
Although highly accurate and sensitive, virus isolation and PCR can be time consuming and expensive and relies on sampling (and therefore detection) of symptomatic cases.
Routinely used serological methods—IgM and IgG ELISAs—are unable to differentiate between the 4 dengue serotypes and are affected by cross-reactivity with other flaviviruses (e.g. yellow fever or Japanese encephalitis).
IgG ELISAs are unable to differentiate between past, recent, and current infection [5].
IgM ELISAs can be confounded by false positives and are only useful for a limited time post-infection [86].
In secondary or later infections, serological diagnosis of the most recent infecting dengue serotype is difficult due to the presence of pre-existing cross-neutralising and cross-reactive antibodies [39,87].
Serological protocols (e.g. thresholds used to define seropositivity) are not standardised across laboratories [26].
Laboratory capacity and general public health infrastructure and surveillance systems vary widely within and between countries.
Here we utilise published age-stratified seroprevalence surveys and estimate the force of infection (λ) and corresponding basic reproduction number (R 0) for dengue in a variety of settings. Due to the much lower costs, future seroprevalence studies are still likely to depend on IgM or IgG enzyme-linked immunosorbant assays (ELISAs) rather than the more labour intensive plaque-reduction neutralisation tests (PRNTs). The comparison of estimates derived from IgG, IE and PRNT data allows us to determine the usefulness of less expensive assays.
Methods
Literature search
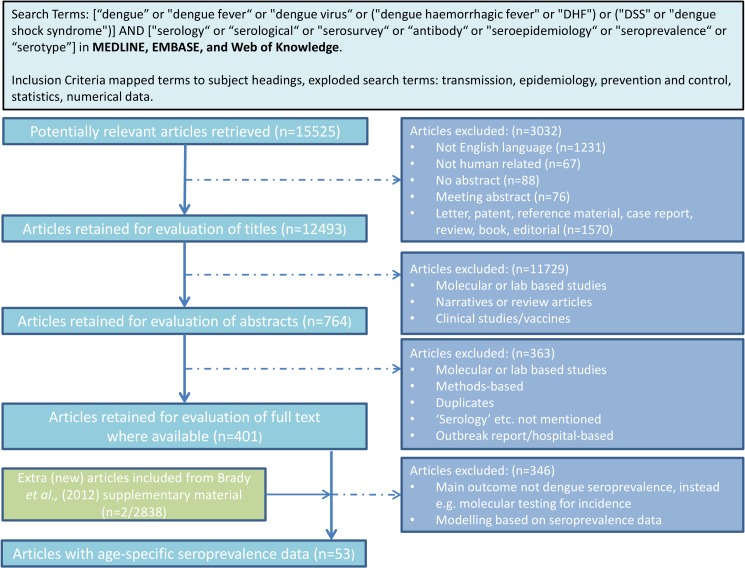
We searched MEDLINE, EMBASE, and Web of Knowledge for publications reporting age-stratified dengue serological surveys. Fig 1 describes the search process and search terms used. Studies published before 1980 were not included in the analysis as we were interested in contemporary dengue transmission. Studies reporting age-specific seroprevalence for at least 5 age groups were included and categorised according to the assay type used. Studies reporting less than 5 age groups were excluded as these studies tended to have wide age groups where the mean seroprevalence did not accurately reflect the variability in seroprevalence within that age group. Data were extracted from published datasets where age-specific seroprevalence was tested by IgG ELISAs, inhibition ELISAs (IEs) or PRNTs. IgG and IE data are both non-serotype specific and we refer to them interchangeably.
Fig 1. Flowchart describing the literature search process for dengue seroprevalence surveys.
Estimating the force of infection (λ)
In the context of dengue, seroprevalence measures obtained with IgG ELISAs only give an indication of whether an individual has ‘ever’ been infected and do not differentiate between infecting serotypes or identify the number of past infections.
Since infection with one serotype only provides homologous immunity, a seropositive individual may still be susceptible to secondary heterotypic infection [39]. We fitted the single cross-sectional IgG datasets using a simple catalytic model (model A). The model assumes a constant infection hazard λ, with infection causing individuals of age a to move from a seronegative x(a) to a seropositive z(a) state [19].
Since some datasets appeared to have declining seroprevalence with age, we extended model A by assuming that protection could decay with age at a rate α (model B). Whenever yearly cross-sectional IgG data were available from the same location, these data were fitted using a time-varying catalytic model (model C) which allowed estimation of the periodicity (T), seasonal amplitude (δ) and within-year timing (θ) of dengue outbreaks, and the critical age (A crit) and scale (S) at which exposure levels change. See the Supporting Information for full details (S1 Text).
In order to fit serotype-specific PRNT data, we applied the multi-strain catalytic model developed by Ferguson et al. [40]. Different model variants were assessed, which explored different assumptions on serotype interactions. Model D1 assumed no serotype-interaction. Model D2 assumed that cross-protection or enhancement did not vary by serotype. Model D3 assumed that the magnitude of cross-protection or enhancement varied by the primary infection serotype. Last, model D4 assumed that the magnitude of cross-protection or enhancement depended on the serotype of the secondary infection.
Moreover, for comparison purposes, we fitted model A to PRNT data, having defined individuals with PRNT titres below the detection limit for all four dengue serotypes as seronegative and individuals with at least one PRNT titre over the detection limit as seropositive. Since assays differed between surveys, here the detection limit also varied from study to study.
We defined a beta-binomial likelihood for models A—C and a multinomial likelihood for models D1-D4. Models were fitted to the data using the Metropolis-Hasting Markov Chain Monte Carlo (M-H MCMC) algorithm using the R Statistical Package (version 3.1.0, R Development Core Team, Vienna, Austria) [41]. Full details are given in S1 Text.
Estimating the basic reproduction number R 0i
We assumed that dengue is at endemic equilibrium and that the force of infection λ is constant in time in all cases except model C. Unless otherwise stated, we assumed that all four serotypes of dengue were in circulation. Since IgG data contain no information on the infecting serotype, we assumed that the four dengue serotypes are equally transmissible and estimated a single reproduction number applicable to each serotype. For the PRNT data, since we were able to estimate serotype-specific forces of infection, we computed strain-specific reproduction numbers as described by Ferguson et al. [40].
We computed the reproduction numbers under two different assumptions on the number of infections required to obtain full protection against infection by any dengue serotype. This allows us to explore whether tertiary and quaternary infections contribute to transmission significantly. Under assumption 1 complete protection is obtained upon quaternary infection (all four infections contribute equally); whilst under assumption 2 complete protection is reached upon secondary infection (only primary and secondary infections are infectious). Under assumption 2 we were also able to incorporate cross-immunity leading to inhibition or enhancement of susceptibility to secondary infection. For each model variant other than B, we computed the serotype-specific basic reproduction number under assumptions 1 and 2. We only considered model B under assumption 1, as decay of immunity by definition allows an arbitrary number of infections to occur. Full details are given in S1 Text.
Results
We identified 53 studies reporting age-specific seroprevalence from a total of 15,525 potentially relevant papers (Fig 1). Of these, 38 used non-serotype specific assays including IgG and inhibition ELISAs (IE). Only nine studies used PRNTs and five studies reported results from multiple assays. Excluding studies with less than 5 reported age groups from further analysis left a total of 30 surveys from 18 countries for IgG data, and 7 studies from 5 countries for PRNT data. 28 (out of 30) surveys from 17 countries were cross-sectional IgG seroprevalence surveys from a single year. The remaining 2 (out of 30) surveys were conducted in Nicaragua and combined provided 7 years’ worth of cross-sectional inhibition ELISA (IE) data. Most IgG surveys identified were conducted in 2000–2010 (23/30), while most PRNT surveys were conducted in the 1990s (4/7). Although recent serosurveys used commercial diagnostics, many studies used in-house assays. Tables 1 and 2 summarises the study and demographics of the datasets retained for analysis from the corresponding or closest year. All studies summarised in Table 1 were fitted using model A and B, and model C was also fitted to the two Nicaraguan datasets (Table 1). Models D1—D4 were fitted to studies summarised in Table 2.
Table 1. Summary of cross-sectional non-serotype specific datasets identified and associated demographics.
| Country | Author | Survey Year | Region | Assay Type+ | # Serotypes circulating | Age range sampled | N | Population size of study region (thousands) | Rural/Urban | % <15 years old | Models used |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Brazil | Braga et al.[42] | 2005/06 | Recife | PanBio | 4 | 5–65 | 2817 | 40 | Urban | 28 | A and B |
| Costa Rica | Iturrino-Monge et al.[43] | 2002/03 | Puntarenas/San Jose | PanBio | 4 | 1–10 | 206 | 358/1373 | Urban | 31.5 | A and B |
| Dominican Republic | Yamashiro et al.[44] | 2002 | Santo Domingo | Focus Tech | 4 | 0–60 | 1209 | 1887 | Urban | 35 | A and B |
| El Salvador | Hayes et al.[45] | 2000/01 | Las Pampitas | CDC | NA | 0–69 | 371 | 944 | Rural | 38 | A and B |
| FrenchPolynesia | Deparis et al.[46] | 1996 | Teroma | In-house | 4 | 0–21 | 169 | 16 | Urban | 34 | A and B |
| India | Padbidri et al.[47] | 1988/89 | Andaman | HI/N | NA | 0–40 | 2401 | 356 | Rural | 38 | A and B |
| Laos | Vallée et al.[48] | 2006 | Vientiane | In-house | 4 | 0–6 | 143 | 277 | Urban | 40 | A and B |
| Hiscox et al.[49] | 2007/08 | Khammouane | HI | 4 | 0–90 | 1708 | 337 | Rural | A and B | ||
| Mayotte | Sissoko et al.[50] | 2006 | Mayotte | Focus Tech | NA | 2–55 | 1154 | 175 | Whole island | 41 | A and B |
| Mexico | Brunkard et al.[51] | 2004 | Matamoros | PanBio | 4 | 15–75 | 600 | 412 | Urban | 32 | A and B |
| Ramos et al.[52] | 2005 | Quantitative | 4 | 5–65 | 131 | 412 | Urban | A and B | |||
| Pakistan | Ali et al.[53] | Pre-2003^ | Khyber Pakhtunkhawa | Cortez | NA | 0–60 | 613 | 20000 | Urban/rural | 42 | A and B |
| Mahmood et al.[54] | 2012 | Lahore | NovaTech | NA | 15–55 | 274 | 7566 | Urban | 35 | A and B | |
| Papua New Guinea | Senn et al.[55] | 2007/08 | Madang Province | PanBio | NA | 0–25 | 577 | 493 | Urban/rural | 39 | A and B |
| Peru | Hayes et al.[56] | 1992 | Loreto | In-house | 2 | 0–60 | 1608 | 9 | Urban/Rural/Jungle | 38 | A and B |
| Reiskind et al.[57] | 1996 | Santa Clara | In-house | 2 | 5–87 | 1225 | 2.4 | Suburban | 36 | A and B | |
| Singapore | Goh et al.[58] | 1984 | National | HI | 4 | 0–40 | 425 | 2709 | Urban | 24 | A and B |
| Yew et al.[59] | 2004 | National | PanBio | 4 | 18–74 | 4152 | 2709 | Urban | 19 | A and B | |
| Yap et al.[60] | 2007 | National | PanBio | 4 | 7–85 | 3939 | 2709 | Urban | 17 | A and B | |
| Sri Lanka | Malavige et al.[61] | Pre-2006^ | Colombo district | PanBio | 4 | 6–18 | 313 | 2309 | Urban | 25 | A and B |
| Tissera et al.[62] | 2008 | Columbo City | In-house | 4 | 0–12 | 797 | 647 | Urban | 25 | A and B | |
| Tam et al.[63] | 2008 | Colombo City | In-house | 4 | 0–12 | 797 | 647 | Urban | 25 | A and B | |
| Thailand | Perret et al.[64] | 2000 | Bangkok | In-house | 4 | 5–12 | 283 | 6355 | Urban | 24 | A and B |
| Tuntaprasart et al.[65] | 2000 | Ratchaburi | In-house | 4 | 15–40 | 245 | 842 | Urban | 21 | A and B | |
| USA | Brunkard et al.[51] | 2004 | Brownsville | PanBio | NA | 15–75 | 600 | 139 | Urban | A and B | |
| Ramos et al.[52] | 2005 | Quantitative | NA | 5–65 | 139 | 139 | Urban | 36 | A and B | ||
| Vietnam | Bartley et al.[66] | 1996/97 | Dong Thap Province | PanBio | 4 | 0–20 | 308 | 309 | Urban/Rural | 32 | A and B |
| Thai et al.[67] | Pre-2005^ | Binh Thuan Province | MRL | 4 | 7–14 | 961 | 1100 | Rural | 27 | A and B | |
| Nicaragua - | Balmaseda et al.[68] | 2001–03 | Managua | IE | 4 | 5–16 | 1971 | 2101 | Urban | 41 | A and C |
| Balmaseda et al.[13] | 2004–07 | Managua | IE | 4 | 2–9 | 14182 | 2101 | Urban | 38 | A and C |
^ Survey date not given, noted as ‘pre-year of publication’. +All assays were IgG or HI ELISAs. -Cross-sectional surveys from multiple years (2001–2007).
Table 2. Summary of PRNT surveys identified and associated demographics.
| Country | Author | Year | Region | Age Range (Yrs) | N | Serotypes^ | Population size of study region (thousands) | Rural/Urban | % Aged <15 yrs | Models used |
|---|---|---|---|---|---|---|---|---|---|---|
| Cuba | Guzman et al.[69] | 1983 | Cerro | 0–45 | 1295 | 2 | 125.5 | Urban | 26 | A, D1—D4 |
| Guzman et al.[70] | 1997/98 | Santiago | 0–95 | 1151 | 2 | 475.6 | Urban | 17.3 | A, D1—D4 | |
| Haiti | Halstead et al.[12] | 1996/99 | Port au Prince | 6–14 | 210 | 4 | 2000 | Urban | 43 | A, D1—D4 |
| Indonesia | Graham et al.[71] | 1995 | Yogyakarta | 4–10 | 1837 | 4 | 421 | Urban | 34 | A, D1—D4 |
| Peru | Morrison et al.[72] | 1999 | Iquitos | 5–60+ | 2524 | 2 | 350 | Urban | 34 | A, D1—D4 |
| Thailand | Sangkawibha et al.[73] | 1980 | Rayong | 0–10 | 1009 | 4 | 53 | Suburban | 39.4 | A, D1—D4 |
| Thailand | Rodriguez-Barraquer et al.[74] | 2010 | Rayong | 6–19 | 1647 | 4 | 230 | Urban | 19.3 | A, D1—D4 |
^Number of serotypes known to have been in circulation.
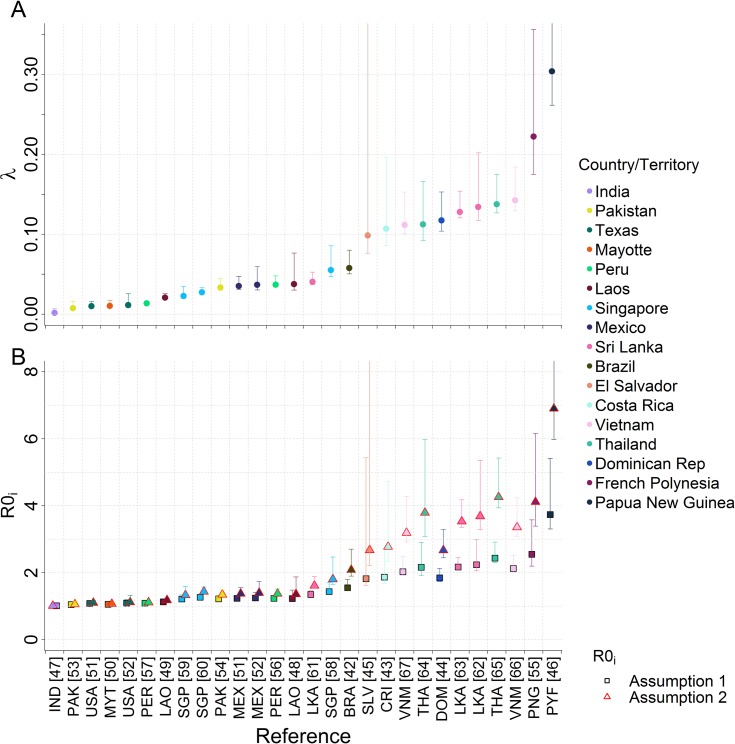
Only an overall force of infection could be estimated from non-serotype specific IgG data. As expected, estimates of the force of infection varied widely between countries and, to a lesser extent, within countries (Fig 2A). Southeast Asian countries known to be hyper-endemic for dengue, such as Vietnam and Thailand, had a higher force of infection compared with most sites in the Americas [75]. Corresponding estimates of R 0i varied according to the assumptions made regarding host immunity (Fig 2B). Assuming that two heterologous infections are sufficient for complete immunity (Assumption 2) produced up to two-fold higher estimates of R 0i compared to when we assumed that quaternary infections are required for complete immunity (Assumption 1). However, R 0i estimates under these two assumptions converge as the estimated force of infection decreases.
Fig 2. A) Force of infection and B) corresponding R0i estimates of cross-sectional non-serotypes specific datasets fitted to Model A.
Posterior median and 95% credible intervals shown.
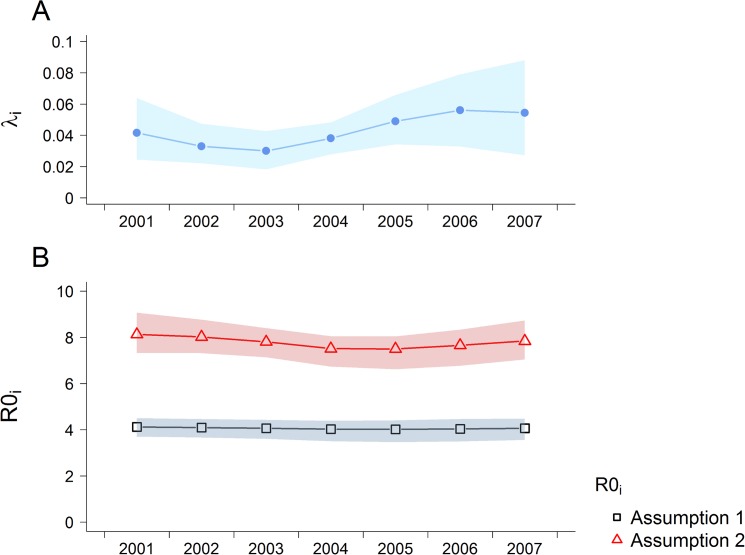
With age-structured serosurvey data from multiple sequential years (as was available for Nicaragua, Table S3), it is possible to estimate temporal and age-specific changes in exposure [13,68] (Fig 3A). We fitted a model (model C) to those data which allowed for the force of infection to vary sinusoidally over time and to change at (fitted) age threshold. We estimated that exposure increased in individuals over 3.9 years old (95% CI: 2.7–5.4 years), with the estimated force of infection during the study period (2001–2007) being 0.323 (95% CI: 0.261–0.377) above 3.9 years and 0.174 (95% CI: 0.118–0.280) below 3.9 years. These estimates represent the average total force of infection for all four serotypes in circulation. The force of infection was estimated to vary with a period of 8.8 years (95% CI: 1.3–12.5 years). Resulting estimates of R 0i (Fig 3B) showed the same dependence on immunity assumptions as the point estimates derived from single serosurveys (Fig 2), but interestingly showed less temporal variation than the force of infection estimates (Fig 3A).
Fig 3. Estimated time-varying A) serotype-specific force of infection in individuals under the threshold age and B) R0i derived by fitting Model C to Nicaraguan data (2001–2007).
Posterior median and 95% credible intervals shown.
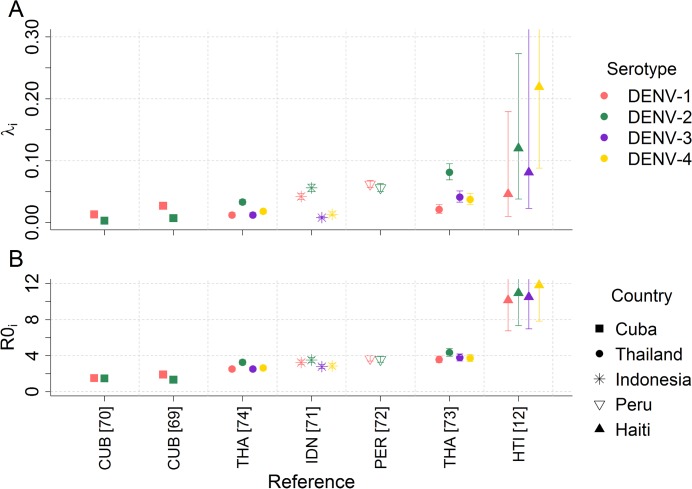
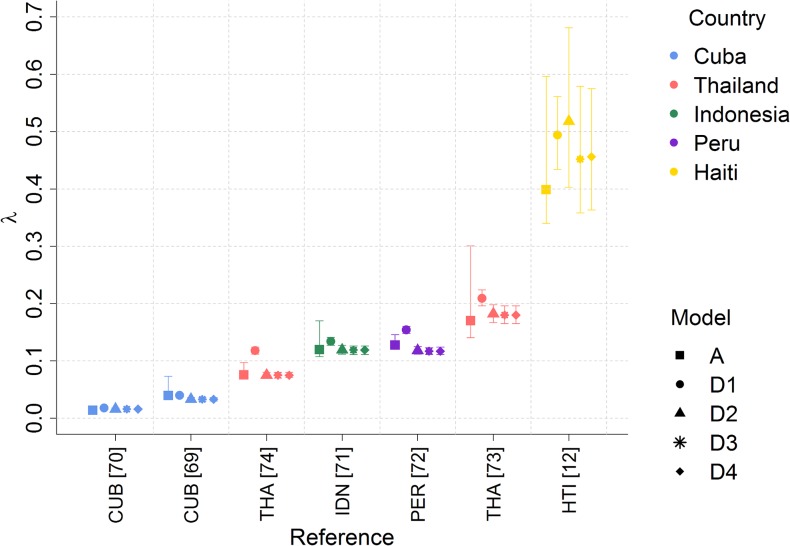
PRNT data are serotype-specific, allowing us to estimate the force of infection (λ i) and basic reproduction number (R 0i) for each serotype individually (Fig 4). Estimates varied widely between different surveys, again highlighting the heterogeneity of dengue transmission. Within the same survey, serotype-specific differences in transmission intensity were apparent, demonstrating how a certain serotype may be more dominant at any one time point. For example, for model D2, force of infection estimates for Haiti were 0.046 (95% CI: 0.010–0.179) for DENV-1 but 0.219 (95% CI: 0.088–0.445) for DENV-4.
Fig 4. Serotype-specific estimates of A) force of infection, λ i, and B) R 0i estimates derived from PRNT datasets fitted to Model D2.
Posterior median and 95% credible intervals shown.
Comparison of cross-protection or enhancement parameters under different assumptions allowed us to estimate the probable serotype causing primary and secondary infections. However, due to the wide credible interval of the estimated parameter, it is difficult to definitively determine the sequence of infections (Tables S5—S8 in S1 Text). For all datasets, the model fit improved when we assumed some level of inter-serotype interaction, demonstrating that inter-serotype interactions play an important role in dengue dynamics.
Interestingly, the serotype-specific estimates of the reproduction number did not scale linearly with the estimated values of the force of infection, although the relative order is maintained i.e. if λ 3 < λ 4 then R 03 < R 04. If one serotype dominates, as was the case in Haiti, changes in the force of infection of the other non-dominant serotypes marginally affect the estimates of the reproduction number of the non-dominating serotypes.
In order to compare the estimates of dengue force of infection derived from IgG and PRNT assays, we also analysed the PRNT data ignoring strain-specificity (i.e. treating PRNT data as if it were IgG data), by categorising individuals as ‘seronegative’ if their PRNT titers were negative for all serotypes, or seropositive if they tested positive for at least one serotype. We used the same thresholds for seronegativity used by each source study. The resulting force of infection estimates generated using model A were consistent with the sum of the individual serotype-specific λ estimates obtained from the full PRNT datasets. This consistency was highest when some level of inter-serotype interaction (cross-protection or enhancement) was allowed for (Fig 5).
Fig 5. Total force of infection (λ) estimates (for all 4 serotypes) derived from PRNT datasets fitted to Models A (treating PRNT data as IgG data) and D1–D4.
Models D2–D4 allow for cross-protection between serotypes. Posterior median and 95% credible intervals shown.
Discussion
From a literature review, we selected 39 studies reporting age-structured seroprevalence data obtained with IgG/IE (31 out of 39) or PRNT (8 out of 39) assays in 22 different locations from 1980 to 2010. From each dataset, we estimated dengue transmission intensity, quantified by the force of infection (λ) and the basic reproduction numbers (R 0i). Overall, our estimates highlight the highly heterogeneous nature of dengue transmission in both space and time, and by serotype. Our analysis also highlights how the relationship between the force of infection and R 0i is affected by underlying assumptions about serotype interactions and immunity. The majority of our estimates of R 0i from 22 countries ranged from 1–4 (28 out of 28 and 24 out of 28 from model A fitted to IgG datasets under assumption 1 and 2 respectively, and 6 out of 7 from model D2 fitted to the PRNT surveys).
Dengue epidemiology differs between the Americas and Southeast Asia. Severe dengue predominantly affects children in Southeast Asia in contrast to the Americas where disease more often manifests in adults as the milder dengue fever [75]. However the changing demographics in Thailand (lower birth and death rates) have increased the average age of DHF suggesting that the epidemiology will continue to evolve [36]. However with the cross-sectional data we use in this study it is difficult to determine whether the higher force of infection in South East Asia is a reflection of the length of time dengue has been in circulation. The recent Phase III dengue vaccine trial conducted in several countries in Latin America showed that the forces of infection are highly heterogeneous across Latin America, with some countries comparable to South East Asia (Columbia and Honduras) and others having much lower forces of infection (Mexico and Puerto Rico) [76]. However, multiple cross-sectional surveys or cohort studies would be needed to estimate how forces of infection by age have changed over time. The low R 0i estimated in the Indian subcontinent is probably due to the lack of datasets from this region and the spatial heterogeneity of transmission within that large region. The one serosurvey from India used in our study was conducted in Andaman, an island with a low population density where we estimated a very low force of infection. It is likely that the epidemiology of dengue on Andaman is not representative of dengue epidemiology on the mainland.
Seroprevalence surveys have the benefit of not being affected by surveillance system sensitivity or case reporting rates, but still have several limitations (Box 1) [77,78]. A particular issue is the wide variation in the assays used between studies (Table 1). Optimally, one would assess the sensitivity of transmission intensity estimates to factors that varied between assays, such as the threshold used to define seronegativity. However, such an analysis requires access to the raw titer data which was not provided in any of the publications we reviewed. Additionally seroprevalence surveys sometimes use serum samples collected for a different purpose and therefore may not be representative of the population. Six out of the 37 studies used such samples: from blood banks [44], ante-natal clinics [64], hospitals [55,79,80], or residual samples from a different study [66]. Use of convenience samples can increase the volume of serological data produced, but the potential biases such sampling introduces must be taken into account when analysing such data.
Although we can only calculate a total force of infection across all serotypes from non-serotype specific data (such as surveys using IgG ELISA assays), such data are still sufficient for assessing heterogeneity in overall dengue transmission intensity between different populations. However as demonstrated by the variable serotype specific λ i estimated from the PRNT data, even within the same population, the dominant serotype in circulation changes over time [8,81,82]. Furthermore, we found that estimates of R 0i varied between serotypes, suggesting serotypes (or genotypes) differ in their intrinsic transmissibility [40,74,82]. Therefore the assumption that all serotypes have identical λ i required to estimate serotype-specific transmission intensity from IgG data must be regarded as a crude simplification. However, we found that non-serotype specific data does yield an estimate of the total force of infection from all serotypes consistent with the sum of serotype-specific forces of infection able to be derived from PRNT data, particularly when analysis of the latter allowed for inter-serotype interaction (cross-protection or enhancement) [8].
It is not possible to disentangle temporal from any age-dependent variation in exposure from single cross-sectional seroprevalence surveys, requiring broad assumptions to be made about such variation. Hence, for simplicity, we generally assumed constant transmission intensity over time when analysing single cross-sectional surveys. However, for Nicaragua [13,68], data from multiple sequentially conducted serosurveys were available, so we were able to estimate time and age-dependent changes in the force of infection. We found evidence of long term variation in transmission intensity over a timescale of 1–12 years, and that exposure levels changed with age, with children aged 4 or older having twice the exposure of those under that age. We suspect that this may be associated with school attendence, with children spending more time away from home leading to an increase in exposure if the majority of transmission is occuring outside the domestic environment [72]. This school-cohort effect has also been observed in Sri Lanka, conversely with a decrease in exposure, where Tam et al. estimated an age-varying force of infection of 0.154 (95% CI: 0.132–0.177) for 0.5–6 year olds and 0.087 (95% CI: 0.020–0.154) for children aged 6 years and above also demonstrating the existence of different transmission environments [63].
Our analysis has a number of additional limitations. First, in translating force of infection estimates into estimates of R 0i we rely on a model which assumes exposure is due to endemic transmission, meaning all resulting R 0i estimates are by definition greater than one. Clearly this is less appropriate for settings with low seroprevalence such as Texas (USA), where some or all of the seropositivity detected is due to imported cases rather than local transmission.
Second, estimates of transmission intensity (particularly R 0i) are sensitive to assumptions about cross-protective immunity between serotypes—and most notably the extent to which tertiary and quaternary infections contribute to transmission. While there is increasing evidence that tertiary and quaternary infections occur [10,82], there is little quantitative data on the infectiousness of such infections relative to primary and secondary infections. Consistent with published theory [81], our estimates of R 0i were lower when we assumed tertiary and quaternary infections were as infectious as earlier infections (Assumption 1) than when we assumed complete immunity was acquired after secondary infection (Assumption 2). When one serotype had a very large force of infection relative to the other three serotypes (e.g. Haiti model 2: DENV-1 at 0.046 (95% CI: 0.010–0.179) compared to DENV-4 at 0.219 (95% CI: 0.088–0.445), then regardless of the value of λ i of the remaining serotypes, all R 0i estimates were large and similar to each other. Thus it appears that the value of R 0i is dominated by very large λ i and changes in the other three λ i play a minimal role. This uncertainty has relevance for planning interventions [8,11,83], since R 0 determines the coverage and effectiveness of vaccination or vector control measures required to achieve control of transmission [84]. The recent results from trials of the Sanofi live-attenuated chimeric vaccine [20,21] make this issue more pressing, since reliable estimates of transmission intensity—and of the health burden due to dengue—will be important in strategic planning and resource allocation for vaccination in different contexts.
Third, while PRNT assays are currently the gold standard for routine dengue serotyping, cross-reactivity means care must be taken when interpreting the results of serosurveys in areas where there is co-circulation of different flaviviruses or routine use of yellow fever or Japanese Encephalitis vaccine [3].
Finally, our literature search highlighted that use of serological surveys as a tool to assess transmission remains rare for dengue, with publications of outbreak reports and notified case incidence data being much more common. Generally, published models estimating dengue transmission risk have therefore used notification data, the reliability of which therefore heavily depend on the quality of the surveillance system [85]. Gaining a better global picture of the variation in transmission will improve both estimates of the disease burden caused by dengue and assist in control planning. We would therefore advocate much more widespread and routine use of serological surveys as a surveillance tool which provides invaluable data for an immunising infection such as dengue. While PRNT data provides the maximum information, our study shows that even the much cheaper ELISA-based assays would provide reasonable baseline estimates of overall transmission intensity.
Supporting Information
(DOCX)
Data Availability
Data are from previously published studies all listed in the references.
Funding Statement
NI was funded by the Medical Research Council as part of her PhD. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.(WHO) WHO (2012) Global Strategy for Dengue Prevention and Control, 2012–2020.
- 2. Bhatt S, Gething PW, Brady OJ, Messina JP, Farlow AW, et al. (2013) The global distribution and burden of dengue. Nature 496: 504–507. 10.1038/nature12060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Halstead SB (2007) Dengue. Lancet 370: 1644–1652. [DOI] [PubMed] [Google Scholar]
- 4. Simmons CP, Farrar JJ, Nguyen v V, Wills B (2012) Dengue. N Engl J Med 366: 1423–1432. 10.1056/NEJMra1110265 [DOI] [PubMed] [Google Scholar]
- 5. World Health Organization, World Health Organisation (2009) Dengue: guidelines for diagnosis, treatment, prevention and control World Health Organization; x, 147 p. [PubMed] [Google Scholar]
- 6. Gibbons R V., Kalanarooj S, Jarman RG, Nisalak A, Vaughn DW, et al. (2007) Analysis of repeat hospital admissions for dengue to estimate the frequency of third or fourth dengue infections resulting in admissions and dengue hemorrhagic fever, and serotype sequences. Am J Trop Med Hyg 77: 910–913. [PubMed] [Google Scholar]
- 7. Salje H, Lessler J, Endy TP, Curriero FC, Gibbons R V., et al. (2012) Revealing the microscale spatial signature of dengue transmission and immunity in an urban population. Proc Natl Acad Sci 109: 9535–9538. 10.1073/pnas.1120621109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Reich NG, Shrestha S, King AA, Rohani P, Lessler J, et al. (2013) Interactions between serotypes of dengue highlight epidemiological impact of cross-immunity. J R Soc Interface 10: 20130414 10.1098/rsif.2013.0414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. OhAinle M, Balmaseda A, Macalalad AR, Tellez Y, Zody MC, et al. (2011) Dynamics of Dengue Disease Severity Determined by the Interplay Between Viral Genetics and Serotype-Specific Immunity. Sci Transl Med 3: 114ra128–114ra128. 10.1126/scitranslmed.3003084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wikramaratna PS, Simmons CP, Gupta S, Recker M (2010) The Effects of Tertiary and Quaternary Infections on the Epidemiology of Dengue. PLoS One 5: e12347 10.1371/journal.pone.0012347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wearing HJ, Rohani P (2006) Ecological and immunological determinants of dengue epidemics. Proc Natl Acad Sci U S A 103: 11802–11807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Halstead SB, Streit TG, Lafontant JG, Putvatana R, Russell K, et al. (2001) Haiti: Absence of dengue hemorrhagic fever despite hyperendemic dengue virus transmission. Am J Trop Med Hyg 65: 180–183. [DOI] [PubMed] [Google Scholar]
- 13. Balmaseda A, Standish K, Mercado JC, Matute JC, Tellez Y, et al. (2010) Trends in patterns of dengue transmission over 4 years in a pediatric cohort study in Nicaragua. J Infect Dis 201: 5–14. 10.1086/648592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Shepard DS, Undurraga E a., Betancourt-Cravioto M, Guzmán MG, Halstead SB, et al. (2014) Approaches to Refining Estimates of Global Burden and Economics of Dengue. PLoS Negl Trop Dis 8: e3306 10.1371/journal.pntd.0003306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Undurraga EA, Halasa YA, Shepard DS (2013) Use of Expansion Factors to Estimate the Burden of Dengue in Southeast Asia: A Systematic Analysis. PLoS Negl Trop Dis 7: 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Beaute J, Vong S, Beauté J (2010) Cost and disease burden of dengue in Cambodia. BMC Public Health 10: (31 August 2010)–(31 August 2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Shepard DS, Undurraga EA, Halasa YA (2013) Economic and Disease Burden of Dengue in Southeast Asia. PLoS Negl Trop Dis 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Suaya JA, Shepard DS, Siqueira JB, Martelli CT, Lum LCS, et al. (2009) Cost of Dengue Cases in Eight Countries in the Americas and Asia: A Prospective Study. Am J Trop Med Hyg 80: 846–855. [PubMed] [Google Scholar]
- 19. Anderson RM, May RM (1992) Infectious Diseases of Humans: Dynamics and Control. OUP; Oxford. [Google Scholar]
- 20. Sabchareon A, Wallace D, Sirivichayakul C, Limkittikul K, Chanthavanich P, et al. (2012) Protective efficacy of the recombinant, live-attenuated, CYD tetravalent dengue vaccine in Thai schoolchildren: a randomised, controlled phase 2b trial. Lancet 380: 1559–1567. 10.1016/S0140-6736(12)61428-7 [DOI] [PubMed] [Google Scholar]
- 21. Capeding MR, Tran NH, Hadinegoro SRS, Ismail HIHM, Chotpitayasunondh T, et al. (2014) Clinical efficacy and safety of a novel tetravalent dengue vaccine in healthy children in Asia: a phase 3, randomised, observer-masked, placebo-controlled trial. Lancet 384:1358–65. 10.1016/S0140-6736(14)61060-6 [DOI] [PubMed] [Google Scholar]
- 22. Werren JH, Baldo L, Clark ME (2008) Wolbachia: master manipulators of invertebrate biology. Nat Rev Microbiol 6: 741–751. 10.1038/nrmicro1969 [DOI] [PubMed] [Google Scholar]
- 23. Schraiber JG, Kaczmarczyk AN, Kwok R, Park M, Silverstein R, et al. (2012) Constraints on the use of lifespan-shortening Wolbachia to control dengue fever. J Theor Biol 297: 26–32. 10.1016/j.jtbi.2011.12.006 [DOI] [PubMed] [Google Scholar]
- 24. Jeffery JAL, Yen NT, Nam VS, Nghia LT, Hoffmann AA, et al. (2009) Characterizing the Aedes aegypti Population in a Vietnamese Village in Preparation for a Wolbachia-Based Mosquito Control Strategy to Eliminate Dengue. PLoS Negl Trop Dis 3: e552 10.1371/journal.pntd.0000552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Blacksell SD (2006) Serological and clinical diagnosis of dengue virus infection—a review of current knowledge. Aust J Med Sci 27: 26–33. [Google Scholar]
- 26. Groen J, Koraka P, Velzing J, Copra C, Osterhaus AD (2000) Evaluation of six immunoassays for detection of dengue virus-specific immunoglobulin M and G antibodies. Clin Diagn Lab Immunol 7: 867–871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.CDC C for DC and P (2012) Dengue: Laboratory Guidance and Diagnostic Testing. http://www.cdc.gov/dengue/clinicallab/laboratory.html.
- 28. Thai KTD, Nagelkerke N, Phuong HL, Nga TTT, Giao PT, et al. (2010) Geographical heterogeneity of dengue transmission in two villages in southern Vietnam. Epidemiol Infect 138: 585–591. 10.1017/S095026880999046X [DOI] [PubMed] [Google Scholar]
- 29. Coelho GE, Burattini MN, Teixeira MD, Coutinho FAB, Massad E (2008) Dynamics of the 2006/2007 dengue outbreak in Brazil. Mem Inst Oswaldo Cruz 103: 535–U7. [DOI] [PubMed] [Google Scholar]
- 30. Chowell G, Diaz-Duenas P, Miller JC, Alcazar-Velazco A, Hyman JM, et al. (2007) Estimation of the reproduction number of dengue fever from spatial epidemic data. Math Biosci 208: 571–589. [DOI] [PubMed] [Google Scholar]
- 31. Chowell G, Fuentes R, Olea A, Aguilera X, Nesse H, et al. (2013) THE BASIC REPRODUCTION NUMBER R-0 AND EFFECTIVENESS OF REACTIVE INTERVENTIONS DURING DENGUE EPIDEMICS: THE 2002 DENGUE OUTBREAK IN EASTER ISLAND, CHILE. Math Biosci Eng 10: 1455–1474. 10.3934/mbe.2013.10.1455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Chowell G, Torre CA, Munayco-Escate C, Suarez-Ognio L, Lopez-Cruz R, et al. (2008) Spatial and temporal dynamics of dengue fever in Peru: 1994–2006. Epidemiol Infect 136: 1667–1677. 10.1017/S0950268808000290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Favier C, Degallier N, Rosa-Freitas MG, Boulanger JP, Costa Lima JR, et al. (2006) Early determination of the reproductive number for vector-borne diseases: the case of dengue in Brazil. Trop Med Int Heal 11: 332–340. [DOI] [PubMed] [Google Scholar]
- 34. Marques CA, Forattini OP, Massad E (1994) The basic reproduction number for dengue fever in São Paulo state, Brazil: 1990–1991 epidemic. Trans R Soc Trop Med Hyg 88: 58–59. [DOI] [PubMed] [Google Scholar]
- 35. Supriatna AK (2009) Estimating the basic reproduction number of dengue transmission during 2002–2007 outbreaks in Bandung, Indonesia. Dengue Bull 33: 21–33. [Google Scholar]
- 36. Cummings DAT, Iamsirithaworn S, Lessler JT, McDermott A, Prasanthong R, et al. (2009) The Impact of the Demographic Transition on Dengue in Thailand: Insights from a Statistical Analysis and Mathematical Modeling. PLoS Med 6: e1000139 10.1371/journal.pmed.1000139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Gordon A, Kuan G, Mercado JC, Gresh L, Avilés W, et al. (2013) The Nicaraguan Pediatric Dengue Cohort Study: Incidence of Inapparent and Symptomatic Dengue Virus Infections, 2004–2010. PLoS Negl Trop Dis 7: e2462 10.1371/journal.pntd.0002462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Endy TP, Chunsuttiwat S, Nisalak A, Libraty DH, Green S, et al. (2002) Epidemiology of inapparent and symptomatic acute dengue virus infection: A prospective study of primary school children in Kamphaeng Phet, Thailand. Am J Epidemiol 156: 40–51. [DOI] [PubMed] [Google Scholar]
- 39. Rothman AL (2011) Immunity to dengue virus: a tale of original antigenic sin and tropical cytokine storms. Nat Rev Immunol 11: 532–543. 10.1038/nri3014 [DOI] [PubMed] [Google Scholar]
- 40. Ferguson NM, Donnelly CA, Anderson RM (1999) Transmission dynamics and epidemiology of dengue: insights from age-stratified sero-prevalence surveys. Philos Trans R Soc London Ser B-Biological Sci 354: 757–768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. R Core Team, R Development Core Team R (2012) R: A language and environment for statistical computing. R Found Stat Comput 1: 409. [Google Scholar]
- 42. Braga C, Luna CF, Martelli CM, de Souza W V, Cordeiro MT, et al. (2010) Seroprevalence and risk factors for dengue infection in socio-economically distinct areas of Recife, Brazil. Acta Trop 113: 234–240. 10.1016/j.actatropica.2009.10.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Iturrino-Monge R, Avila-Agüero ML, Avila-Agüero CR, Moya-Moya T, Cañas-Coto A, et al. (2006) Seroprevalence of dengue virus antibodies in asymptomatic Costa Rican children, 2002–2003: a pilot study. Rev Panam Salud Pública 20: 39–43. [DOI] [PubMed] [Google Scholar]
- 44. Yamashiro T, Disla M, Petit A, Taveras D, Castro-Bello M, et al. (2004) Seroprevalence of IgG specific for dengue virus among adults and children in Santo Domingo Dominican Republic. Am J Trop Med Hyg 71: 138–143. [PubMed] [Google Scholar]
- 45. Hayes JM, García-Rivera E, Flores-Reyna R, Suárez-Rangel G, Rodríguez-Mata T, et al. (2003) Risk factors for infection during a severe dengue outbreak in El Salvador in 2000. Am J Trop Med Hyg 69: 629–633. [PubMed] [Google Scholar]
- 46. Deparis X, Roche C, Murgue B, Chungue E (1998) Possible dengue sequential infection: dengue spread in a neighbourhood during the 1996/97 dengue-2 epidemic in French Polynesia. Trop Med Int Heal 3: 866–871. [DOI] [PubMed] [Google Scholar]
- 47. Padbidri VS, Wairagkar NS, Joshi GD, Umarani UB, Risbud AR, et al. (2002) A serological survey of arboviral diseases among the human population of the Andaman and Nicobar Islands, India. Southeast Asian J Trop Med Public Health 33: 794–800. [PubMed] [Google Scholar]
- 48. Vallee J, Dubot-Peres A, Ounaphom P, Sayavong C, Bryant JE, et al. (2009) Spatial distribution and risk factors of dengue and Japanese encephalitis virus infection in urban settings: The case of Vientiane, Lao PDR. Trop Med Int Heal 14: 1134–1142. 10.1111/j.1365-3156.2009.02319.x [DOI] [PubMed] [Google Scholar]
- 49. Hiscox A, Winter CH, Vongphrachanh P, Sisouk T, Somoulay V, et al. (2010) Serological investigations of flavivirus prevalence in Khammouane Province, Lao People’s Democratic Republic, 2007–2008. Am J Trop Med Hyg 83: 1166–1169. 10.4269/ajtmh.2010.09-0480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Sissoko D, Ezzedine K, Giry C, Moendandze A, Lernout T, et al. (2010) Seroepidemiology of Dengue virus in Mayotte, Indian Ocean, 2006. PLoS One 5: e14141 10.1371/journal.pone.0014141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Brunkard JM, Robles Lopez JL, Ramirez J, Cifuentes E, Rothenberg SJ, et al. (2007) Dengue fever seroprevalence and risk factors, Texas-Mexico border, 2004. Emerg Infect Dis 13: 1477–1483. 10.3201/eid1310.061586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Ramos MM, Mohammed H, Zielinski-Gutierrez E, Hayden MH, Lopez JL, et al. (2008) Epidemic dengue and dengue hemorrhagic fever at the Texas-Mexico border: results of a household-based seroepidemiologic survey, December 2005. Am J Trop Med Hyg 78: 364–369. [PubMed] [Google Scholar]
- 53. Ali A, Rehman HU, Nisar M, Rafique S, Ali S, et al. (2013) Seroepidemiology of dengue fever in Khyber Pakhtunkhawa, Pakistan. Int J Infect Dis 17: E518–E523. 10.1016/j.ijid.2013.01.007 [DOI] [PubMed] [Google Scholar]
- 54. Mahmood S, Nabeel H, Hafeez S, Zahra U, Nazeer H (2013) Seroprevalence of Dengue IgG Antibodies among Healthy Adult Population in Lahore, Pakistan. ISRN Trop Med 2013: 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Senn N, Luang-Suarkia D, Manong D, Siba PM, McBride WJ (2011) Contribution of dengue fever to the burden of acute febrile illnesses in Papua New Guinea: an age-specific prospective study. Am J Trop Med Hyg 85: 132–137. 10.4269/ajtmh.2011.10-0482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Hayes CG, Phillips IA, Callahan JD, Griebenow WF, Hyams KC, et al. (1996) The epidemiology of dengue virus infection among urban, jungle, and rural populations in the Amazon region of Peru. Am J Trop Med Hyg 55: 459–463. [DOI] [PubMed] [Google Scholar]
- 57. Reiskind MH, Baisley KJ, Calampa C, Sharp TW, Watts DM, et al. (2001) Epidemiological and ecological characteristics of past dengue virus infection in Santa Clara, Peru. Trop Med Int Heal 6: 212–218. [DOI] [PubMed] [Google Scholar]
- 58. Goh KT, Yamazaki S (1987) Serological survey on dengue virus infection in Singapore. Trans R Soc Trop Med Hyg 81: 687–689. [DOI] [PubMed] [Google Scholar]
- 59. Yew YW, Ye T, Ang LW, Ng LC, Yap G, et al. (2009) Seroepidemiology of dengue virus infection among adults in Singapore. Ann Acad Med Singapore 38: 667–675. [PubMed] [Google Scholar]
- 60. Yap G, Li C, Mutalib A, Lai Y-L, Ng L-C (2013) High rates of inapparent dengue in older adults in Singapore. Am J Trop Med Hyg 88: 1065–1069. 10.4269/ajtmh.12-0150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Malavige GN, Fernando S, Aaskov J, Sivayogan S, Dissanayaka T, et al. (2006) Seroprevalence of anti-dengue virus antibodies in children in Colombo District, Sri Lanka. Dengue Bull 30: 12–68. [Google Scholar]
- 62. Tissera HA, De Silva AD, Abeysinghe MRN, de Silva AM, Palihawadana P, et al. (2010) Dengue Surveillance in Colombo, Sri Lanka: Baseline seroprevalence among children. Procedia Vaccinol 2: 107–110. 23203335 [Google Scholar]
- 63. Tam CC, Tissera H, de Silva AM, De Silva AD, Margolis HS, et al. (2013) Estimates of dengue force of infection in children in Colombo, Sri Lanka. PLoS Negl Trop Dis 7: e2259 10.1371/journal.pntd.0002259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Perret C, Chanthavanich P, Pengsaa K, Limkittikul K, Hutajaroen P, et al. (2005) Dengue infection during pregnancy and transplacental antibody transfer in Thai mothers. J Infect 51: 287–293. [DOI] [PubMed] [Google Scholar]
- 65. Tuntaprasart W, Barbazan P, Nitatpattana N, Rongsriyam Y, Yoksan S, et al. (2003) Seroepidemiological survey among schoolchildren during the 2000–2001 dengue outbreak of Ratchaburi Province, Thailand. Southeast Asian J Trop Med Public Health 34: 564–568. [PubMed] [Google Scholar]
- 66. Bartley LM, Carabin H, Vinh Chau N, Ho V, Luxemburger C, et al. (2002) Assessment of the factors associated with flavivirus seroprevalence in a population in Southern Vietnam. Epidemiol Infect 128: 213–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Thai KTD, Binh TQ, Giao PT, Phuong HL, Hung le Q, et al. (2005) Seroprevalence of dengue antibodies, annual incidence and risk factors among children in southern Vietnam. Trop Med Int Heal 10: 379–386. [DOI] [PubMed] [Google Scholar]
- 68. Balmaseda A, Hammond SN, Tellez Y, Imhoff L, Rodriguez Y, et al. (2006) High seroprevalence of antibodies against dengue virus in a prospective study of schoolchildren in Managua, Nicaragua. Trop Med Int Heal 11: 935–942. [DOI] [PubMed] [Google Scholar]
- 69. Guzman MG, Kouri GP, Bravo J, Soler M, Vazquez S, et al. (1990) DENGUE HEMORRHAGIC-FEVER IN CUBA, 1981—A RETROSPECTIVE SEROEPIDEMIOLOGIC STUDY. Am J Trop Med Hyg 42: 179–184. [DOI] [PubMed] [Google Scholar]
- 70. Guzman MG, Kouri G, Valdes L, Bravo J, Alvarez M, et al. (2000) Epidemiologic studies on dengue in Santiago de Cuba, 1997. Am J Epidemiol 152: 793–799. [DOI] [PubMed] [Google Scholar]
- 71. Graham RR, Juffrie M, Tan R, Hayes CG, Laksono I, et al. (1999) A prospective seroepidemiologic study on dengue in children four to nine years of age in Yogyakarta, Indonesia I. studies in 1995–1996. Am J Trop Med Hyg 61: 412–419. [DOI] [PubMed] [Google Scholar]
- 72. Morrison AC, Minnick SL, Rocha C, Forshey BM, Stoddard ST, et al. (2010) Epidemiology of dengue virus in Iquitos, Peru 1999 to 2005: interepidemic and epidemic patterns of transmission. PLoS Neglected Trop Dis 4: e670 10.1371/journal.pntd.0000670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Sangkawibha N, Rojanasuphot S, Ahandrik S, Viriyapongse S, Jatanasen S, et al. (1984) RISK-FACTORS IN DENGUE SHOCK SYNDROME—A PROSPECTIVE EPIDEMIOLOGIC-STUDY IN RAYONG, THAILAND. 1. THE 1980 OUTBREAK. Am J Epidemiol 120: 653–669. [DOI] [PubMed] [Google Scholar]
- 74. Rodriguez-Barraquer I, Buathong R, Iamsirithaworn S, Nisalak A, Lessler J, et al. (2013) Revisiting Rayong: Shifting Seroprofiles of Dengue in Thailand and Their Implications for Transmission and Control. Am J Epidemiol 179: 353–360. 10.1093/aje/kwt256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Halstead SB (2006) Dengue in the Americas and Southeast Asia: do they differ? Rev Panam Salud Publica 20: 407–415. [DOI] [PubMed] [Google Scholar]
- 76. Villar L, Dayan GH, Arredondo-García JL, Rivera DM, Cunha R, et al. (2015) Efficacy of a Tetravalent Dengue Vaccine in Children in Latin America. N Engl J Med 372: 113–123. 10.1056/NEJMoa1411037 [DOI] [PubMed] [Google Scholar]
- 77. Guzman MG, Kouri G (2004) Dengue diagnosis, advances and challenges. Int J Infect Dis 8: 69–80. [DOI] [PubMed] [Google Scholar]
- 78. Kao CL, King CC, Chao DY, Wu HL, Chang GJJ (2005) Laboratory diagnosis of dengue virus infection: Current and future perspectives in clinical diagnosis and public health. J Microbiol Immunol Infect 38: 5–16. [PubMed] [Google Scholar]
- 79. Ali A, Rehman HU, Nisar M, Rafique S, Ali S, et al. (2013) Seroepidemiology of dengue fever in Khyber Pakhtunkhawa, Pakistan. Int J Infect Dis 17: e518–e523. 10.1016/j.ijid.2013.01.007 [DOI] [PubMed] [Google Scholar]
- 80.Goh KT (1998) Seroepidemiology of dengue virus infection in Singapore. Goh KT, editor 50–72 p.
- 81. Recker M, Blyuss KB, Simmons CP, Hien TT, Wills B, et al. (2009) Immunological serotype interactions and their effect on the epidemiological pattern of dengue. Proc R Soc B-Biological Sci 276: 2541–2548. 10.1098/rspb.2009.0331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Reiner RC, Stoddard ST, Forshey BM, King A a, Ellis AM, et al. (2014) Time-varying, serotype-specific force of infection of dengue virus. Proc Natl Acad Sci U S A. [DOI] [PMC free article] [PubMed]
- 83. Adams B, Holmes EC, Zhang C, Mammen MP Jr., Nimmannitya S, et al. (2006) Cross-protective immunity can account for the alternating epidemic pattern of dengue virus serotypes circulating in Bangkok. Proc Natl Acad Sci U S A 103: 14234–14239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Fine P, Eames K, Heymann DL (2011) “Herd immunity”: a rough guide. Clin Infect Dis 52: 911–916. 10.1093/cid/cir007 [DOI] [PubMed] [Google Scholar]
- 85. Gubler DJ (1989) Surveillance for dengue and dengue hemorrhagic fever. Bull Pan Am Health Organ 23: 397–404. [PubMed] [Google Scholar]
- 86. A-nuegoonpipat A, Prakong S, Sa-ngasang A, Chanama S, Sawanpanyalert P, et al. (2006) Comparison between Haemagglutination inhibition (HI) test and IgM and IgG-capture ELISA in determination of primary and secondary dengue virus infections. Dengue Bull 30: 141–145. [Google Scholar]
- 87. Kuno G, Gubler DJ, Oliver A (1993) Use of “original antigenic sin” theory to determine the serotypes of previous dengue infections. Trans R Soc Trop Med Hyg 87: 103–105. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
Data Availability Statement
Data are from previously published studies all listed in the references.