Abstract
This study examined the association between physical activity of older individuals with musculoskeletal conditions (IMCs) and their spouses’ physical activity, how physical activity related to one’s own and one’s partner’s depressive symptoms, and whether the similarity of partners’ physical activity related to each partner’s depressive symptoms using the actor–partner interdependence model. Seventy-seven dyads completed self-report measures of physical activity, depressive symptoms and potential covariates (socio-demographics, physical health conditions and marital satisfaction; IMCs’ functional impairment and pain; and spouses’ support-related stress). As hypothesized, we found a positive association between the IMC’s and the spouse’s physical activity. Also, spouses had more depressive symptoms when IMCs engaged in less physical activity. However, for both partners, one’s own physical activity was not significantly associated with one’s own depressive symptoms. The spouse’s physical activity was also not significantly associated with the IMC’s depressive symptoms, and the similarity between partners’ physical activity did not significantly relate to either partner’s depressive symptoms. Our findings suggest that interventions that help increase the physical activity of both partners, but particularly IMCs, may benefit spouses’ well-being.
Keywords: physical activity, pain, depressive symptoms, older adults, musculoskeletal conditions
Musculoskeletal conditions such as osteoarthritis and lower back pain are commonly experienced by older adults and can result in varying levels of pain and disability (NIAMS, 2010). Not only does having a musculoskeletal condition have important consequences for an individual’s well-being (Hawker et al., 2011) but also for the well-being of spouses because of the increased levels of stress associated with caring for a partner with pain and disability (Martire, Lustig, Schulz, Miller, & Helgeson, 2004). Examining factors that make couples more resilient or place them at heightened risk for negative mental health outcomes such as depression is important. One factor that is likely to play a role in how couples cope with a partner’s musculoskeletal condition is the extent to which each couple member engages in physical activity.
Intrapersonal associations between physical activity and depressive symptoms
Much of the work on physical activity and depressive symptoms has been intrapersonal, meaning that researchers have studied how physical activity relates to depressive symptoms (and vice versa) within an individual. Considerable evidence shows protective effects of physical activity on mental and physical health in younger (Penedo & Dahn, 2005; Wendel-Vos, Schuit, Tijhuis, & Kromhout, 2004) and older adults (Kahana et al., 2002; King et al., 2000). Prospective studies and clinical trials show that regular physical activity significantly decreases the risk for developing depression (Teychenne, Ball, & Salmon, 2008), alleviates depressive symptoms within individuals (Kerse et al., 2010; Lampinen & Heikkinen, 2002), and can even reduce depressive symptoms in older patients with major depressive disorder (Blumenthal et al., 1999).
Regular physical activity is also associated with lower depressive symptoms in adults with physical disabilities (Rosenberg, Bombardier, Artherholt, Jensen, & Motl, 2013). Among people with musculoskeletal conditions specifically, physical activity has been associated with greater health-related quality of life (Abell, Hootman, Zack, Moriarty, & Helmick, 2005). Research suggests that moderately intense physical activity provides therapeutic benefits and can relieve the pain and decline in physical functioning that often comes with musculoskeletal conditions (Ettinger et al., 1997; Penninx et al., 2001). Physical activity can also help people cope with psychological stress related to managing their chronic conditions (Morgan & Goldston, 2013).
For spouses of individuals with musculoskeletal conditions (IMCs), seeing a partner in pain or having to provide increasing levels of support can also be stressful (Monin et al., 2010). Not only is physical activity likely to help the partner with the musculoskeletal condition cope with stress but also the spouse. Indeed, past studies have shown that physical activity has positive mental health benefits for spouses of individuals with chronic conditions that cause pain (King, Baumann, O’Sullivan, Wilcox, & Castro, 2002). Taken together, past research suggests that physical activity is related to less depressive symptoms for individuals. In the context of couples coping with one person’s pain, this is likely to be the case for both the person with pain and his or her spouse.
Interpersonal associations between physical activity and depressive symptoms
Few studies have examined interpersonal associations between physical activity and depressive symptoms in couples in general, and no research to our knowledge has examined these associations among older couples dealing with a musculoskeletal condition. Physical behaviours and emotional states are heavily influenced by close relationship partners (Meyler, Stimpson, & Peek, 2007; Monin & Schulz, 2009); therefore, it is necessary to use dyadic models that account for interdependence and reciprocity (Kahana & Young, 1990; Pruchno, 1994). This is especially important when examining mental and physical health among older married couples, because as people age, their close relationships become more central for their well-being (Carstensen, Gottman, & Levenson, 1995; Hoppmann & Gerstorf, 2009).
We know from past research that older spouses’ physical activity levels are positively associated (Pettee et al., 2006), that when one spouse engages in greater physical activity, so does the other spouse. This is also the case for depressive symptoms; when one spouse experiences depressive symptoms, the other spouse is likely to experience depressive symptoms (Townsend, Miller, & Guo, 2001). What is not known is the extent to which each partner’s physical activity and depressive symptoms are interrelated. Furthermore, studies have not examined these associations in the context of spouses dealing with a musculoskeletal condition, in which couple members’ ability to engage in physical activity may be imbalanced because of functional limitations or pain.
Interdependence theory suggests that within a dyadic relationship, one partner’s beliefs and behaviours tend to affect those of the other partner (Kelley & Thibault, 1978; Meyler et al., 2007). In the context of spouses dealing with a partner’s musculoskeletal condition, we expect that physical activity levels will be linked, such that when one partner engages in more physical activity, the other partner will also engage in more physical activity. We also predict that not only will engaging in greater levels of physical activity have benefits for individuals in terms of less depressive symptoms but also for their partners. However, these interpersonal effects may differ in terms of whose physical activity levels are more important for well-being in the relationship. It may be that the spouse’s mental health is more affected by the physical activity of the partner with the musculoskeletal condition than vice versa. Past research shows that exposure to the physical and psychological suffering of a spouse has detrimental effects on the well-being of the partner through the spread of negative emotions, namely increased depressive symptoms (Monin & Schulz, 2009; Schulz et al., 2009). Thus, it is also necessary to examine how spouses’ physical activity levels relate to their IMC’s disabling condition, including factors such as pain, functional disability and spouses’ own support-related stress, in order to examine if IMCs’ physical activity is independently related to spouses’ depressive symptoms.
Finally, it is important to consider the similarity of partner’s physical activity. When both partners engage in high levels of physical activity, this may benefit both partners’ psychological health. For example, Graham’s (2008) self-expansion model suggests that when couples within intimate relationships engage in physical exercise with one another, they feel more connected and more satisfied in their relationship, which has important implications for both partners’ mental and physical well-being (Robles, Slatcher, Trombello, & McGinn, 2013). However, it may also be the case that when both partners engage in low levels of physical activity, this is also beneficial for psychological health. Research suggests that if health behaviours of husbands and wives are similar, even if they are both negative behaviours (e.g. physical inactivity, smoking and excessive alcohol consumption), spouses tend to show less depressive symptomatology and have higher marital satisfaction compared with dyads who have regular disagreement in their health behaviours (Meyler et al., 2007).
In the case of older adult couples coping with a partner’s musculoskeletal condition, it is unknown whether the similarity of partners’ physical activity levels relates to both partners’ well-being and whether there are differential effects of physical activity for the partner with the musculoskeletal condition and the spouse. Although we would predict both partners engaging in high levels of physical activity to be beneficial for both partners, the picture may be more complex when both partners engage in low levels of physical activity. For example, if a spouse engages in low levels of activity because the partner with the musculoskeletal condition engages in low physical activity, this may be particularly harmful to the spouse’s well-being because the spouse may feel constrained by his or her partner. In the caregiving literature, this is known as activity restriction, which has been shown to negatively affect caregivers’ psychological health (Nieboer, Schulz, Matthews, Scheier, Ormel, & Lindenberg, 1998; Williamson, Shaffer, & Schulz, 1998). Alternatively, partners who both engage in low levels of activity may be more similar to each other and spend more time together engaging in sedentary activities. To address this question, this study explored the similarity between partners’ physical activity and its relation to each partner’s depressive symptoms in a common late-life situation, where the abilities of partners may differ because of a musculoskeletal condition.
The present study
The main objectives of the present study were to examine the associations between partners’ physical activity levels, each individual’s physical activity level and his or her own depressive symptoms (actor effect), each individual’s physical activity level and his or her partner’s depressive symptomatology (partner effect), and whether similarity between partners’ physical activity related to each partner’s depressive symptoms (similarity effect).
Firstly, we hypothesized that partners’ physical activity would be positively associated, that when one partner engages in high levels of physical activity, the other partner is likely to engage in high levels of physical activity (H1). Secondly, we hypothesized that greater physical activity would be associated with less depressive symptoms within an individual (H2). Thirdly, we hypothesized that greater physical activity in one partner would be associated with less depressive symptoms in the other partner (H3). Finally, we hypothesized that partners’ similarity in physical activity would be related to less depressive symptoms for both individuals (H4). In testing each hypothesis, we also explored whether these associations differed depending on the role of the partner. In other words, does physical activity relate to depressive symptoms only for IMCs? Also, does the physical activity level of the IMC impact their spouse’s depressive symptoms but not the other way around?
Method
Participants
Seventy-seven individuals with a self-reported musculoskeletal condition (IMCs; osteoarthritis or lower back pain) and their spouses (77 dyads) participated in the study. Recruitment was from newspaper advertisements and community bulletins. In order to be eligible to participate, (1) IMCs had to be at least 50 years of age; (2) the couple had to be married or in a marriage-like relationship and living together for at least 6 months; (3) the spouse could not have a musculoskeletal condition; and (4) if the spouse had another chronic condition that caused pain, the spouse had to have less pain on average than the IMC.1 Participants also completed the Short Portable Mental Status Questionnaire—Mini-Mental State Examination (Pfeiffer, 1975), which evaluated their cognitive functioning. Those who correctly answered at least seven out of 10 items were considered eligible for the study. Spouses who were taking beta-blockers, a class of drug affecting heart rate, were excluded because of the aims of the parent study.
Thirty-two of the IMCs were male, and 45 were female. The mean age of IMCs was 65.90 years (SD = 7.88), and the mean age of spouses was 64.81 years (SD = 8.41). Both IMCs and spouses were highly educated, with most having completed at least some college education (66.2% for IMCs and 62.3% for spouses). Seventy-seven per cent of couples had children. Most IMCs and spouses were Caucasian (97.4% for IMCs and 93.5% for spouses). Household income was distributed such that 48% reported less than $50,000, 42.5% reported $50,000 to $99,999, and 10% reported more than $100,000. IMCs reported experiencing chronic pain from a musculoskeletal condition for 123.77 months on average (SD = 129.79, Range = 0–636). Couples reported being married for an average of 372.67 months (SD = 196.46).
Procedure
This study was part of a larger, multi-method, IRB approved study (see also Monin, Zhou, & Kershaw, in press). After indicating informed consent and performing a series of tasks, spouses completed a background questionnaire in separate rooms that included the following measures. Each participant received $40 for their efforts.
Measures
Physical activity
Both partners were asked to report their level of physical activity using the Paffenbarger PA Questionnaire (PPAQ; Paffenbarger, Blair, Lee, & Hyde, 1993). The PPAQ is a self-report measure designed to assess leisure-time physical activity. The PPAQ asks participants to report the average number of blocks walked per day (1 city block = 1/12 mile; 8 kcal/block), the average number of flights of stairs climbed per day (1 flight = 10 steps; 4 kcal/flight) and types of physical activities participated per day (light sport/recreation: 5 kcal/min; moderate sport/recreation: 7.5 kcal/min; strenuous sport/recreation: 10 kcal/min). Activities that require relatively low energy input (e.g. bowling, golf, boating and yard work) were classified as ‘light’; sports that require a moderate level of energy input (e.g. tennis, baseball and ballroom dancing) were classified as ‘moderate’; and sports that require a high level of energy input (e.g. basketball, competitive swimming and mountaineering) were classified as ‘strenuous’. Answers to these questions were then summed to generate a physical activity index (PAI) for each participant in kilocalories (kcal)/week, which can then be computed as follows: (flights of stairs/day × 4 kcal/flight × 7 days/week) + (blocks/day × 8 kcal/block × 7 days/week) + for each activity reported (activity intensity kcal/min × min/episode × episodes/week) (Paffenbarger, Wing, & Hyde, 1978), giving an estimate of the average energy expenditure per week. The PAI scores for both the spouses and IMCs were not normally distributed; therefore, we converted the PAI using a logarithmic function with base 10 (log PAI) to a more normally distributed variable before conducting inferential analyses. To capture the construct of physical activity, we calculated energy expenditure, which is a valid and reliable assessment of physical activity in the ageing literature.
Depressive symptoms
Both partners completed the Center for Epidemiologic Studies Depression (CES-D) Scale (Radloff, 1977). This 20-item scale assesses participant’s feelings and behaviours during the past week with the following response options: 0 (rarely or none of the time) to 3 (most or all of the time). The Chronbach’s alpha was 0.76 for IMCs and 0.84 for spouses. The possible range of scores is 0 to 60, with the higher scores indicating the presence of more depressive symptoms. Examples of items are ‘I was bothered by things that don’t usually bother me’ and ‘I enjoyed life (reversed)’. Exploratory factor analysis with principal axis factoring was performed to ensure that all items loaded on one factor. The Kaiser–Meyer–Olkin measure of sampling adequacy was 0.80 for the spouse scale and 0.69 for the IMC scale, above the commonly recommended value of 0.6, and Bartlett’s tests of sphericity was significant [χ2(190) = 750.75, p <0.05] for spouses and [χ2(190) = 439.81, p <0.05] for IMCs. For the spouses’ scale, the total initial eigenvalue from the principal axis factoring for one factor was 6.52, and one factor explained 33% of the variance. For the IMC’s scale, the total initial eigenvalue for one factor was 4.74, and one factor explained 23.68% of the variance. Scree plots were also used to determine that items fit one factor. All items were above a 0.35 loading on one factor, except ‘poor appetite’, ‘restless sleep’, ‘less talkative’ and ‘enjoy life’ for spouses, and ‘bothered’, ‘as good as other people’, ‘concentration’, ‘less talkative’ and ‘unfriendly’ for IMCs.
Covariates
The following measures were analysed for potential covariation with predictor and criterion measures. Both partners’ physical health was measured using the physical condition index (PCI; Katz, Ford, Moskowitz, Jackson, & Jaffe, 1963). The PCI is a 24-item self-report survey measuring the prevalence of chronic conditions. Questions inquire about the respondent’s history with cardiovascular, respiratory and digestive problems as well as surgery and cancer, among other health issues. Scores range from 0 to 24 with higher scores indicating more chronic conditions and hence worse health.
Spouses reported their stress associated with providing help to their partners with four instrumental activities of daily living (IADLs). For each IADL (shopping for groceries, preparing meals, doing laundry and household tasks) with which they provided assistance, they indicated how stressful it was from 1 (not at all stressful) to 4 (very stressful). Mean scores were calculated indicating spouse stress. IMCs reported the extent to which they needed help with each IADL. A sum score was calculated to indicate IADL need. IMCs also reported their average pain on a scale from 0 to 10.
Finally, both couple members were asked to report their level of marital satisfaction using the 16-item Locke–Wallace Marital Adjustment Test (Locke & Wallace, 1959). The measure contains one question about the participant’s general level of happiness in the marriage; eight questions about agreement or disagreement between spouses on issues such as friends, sex relations and philosophy of life; and seven questions that explore issues such as regret marrying the current spouse, whether they would choose to marry a different person if given the opportunity and whether they engage in outside interests together. Items are weighted based on their criterion validity in predicting maladjustment and divorce. The range of possible scores is 2–158, with higher scores indicating greater marital satisfaction. The Cronbach’s alphas were 0.74 for IMCs and 0.80 for spouses. Exploratory factor analysis was performed to ensure that all items loaded on one factor. The Kaiser–Meyer–Olkin measure of sampling adequacy was 0.74 for the spouse scale and 0.66 for the IMC scale, above the commonly recommended value of 0.6, and Bartlett’s test of sphericity was significant [χ2(120) = 390.11, p <0.05] for spouses and [χ2(120) = 275.37, p <0.05] for IMCs. The total initial eigenvalue for one factor was 4.94, and one factor explained 30.87% of the variance for spouses. The total initial eigenvalue for one factor was 3.86, and one factor explained 24.11% of the variance for IMCs. Scree plots also revealed one factor in each case. All items loaded on one factor above 0.35, with the exceptions of ‘friend’, ‘leisure-personal’, ‘leisure-partner’ and ‘commitment’ for spouses, and ‘leisure-personal’, ‘leisure-partner’, ‘commitment’ and ‘confide’ for IMCs.
Statistical analysis
Firstly, we tested for potential covariation of the predictor (physical activity) and criterion (depressive symptoms) variables with socio-demographic, physical health, relationship and pain-related factors using correlational analyses. To examine hypothesis 1, we examined the correlation between partners’ physical activity measures. We also calculated the intraclass correlation between partners’ physical activity levels before conducting dyadic analysis to test hypotheses 2 through 4 (West, Popp, & Kenny, 2008).
To test hypotheses 2, 3 and 4, we used a dyadic data analytic technique, the actor–partner interdependence model (APIM; Kashy & Kenny, 1999; Kenny, Kashy, & Cook, 2006) with the mixed model procedure in SPSS to control for the dependency that is inherent in dyadic data and address questions of mutual influence. The APIM is a model of dyadic relationships that integrates a conceptual view of interdependence in two person relationships with the appropriate statistical techniques for measuring and testing it. In this model, individual unit measurements are analysed, but they are treated as nested within dyads (for a more detailed description of the APIM, see Cook & Kenny, 2005). This approach is becoming increasingly common in gerontology research with spouses (e.g. Godwin, Swank, Vaeth, & Ostwald, 2013). The APIM is a dual-intercept model that calculates ‘actor effects’ and ‘partner effects’. An actor effect represents the influence that an individual’s score on a predictor variable has on his or her own score on a criterion variable (e.g. the association between the physical activity and depression for the individual with the musculoskeletal condition; IMC). A partner effect represents the influence that an individual’s score on a predictor variable has on his or her partner’s score on a criterion variable (e.g. the association between IMCs’ physical activity and their spouses’ depressive symptoms). See Figure 1 for an illustration of our simplified, hypothesized model.
Figure 1.
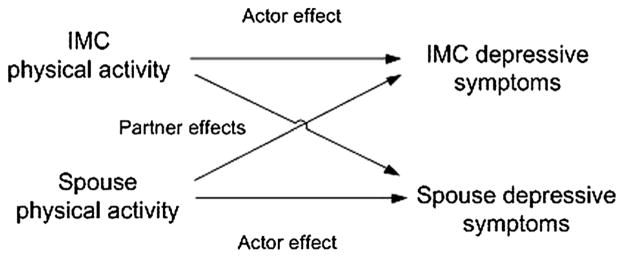
Actor–partner interdependence model. IMC, individual with musculoskeletal condition
In addition to examining actor and partner effects, we examined the similarity of partners’ physical activity by including the absolute difference term ‘abs(actor physical activity–partner physical activity)’ in the second step of the dyadic models (Kenny et al, 2006). Also, to explore whether or not each effect was specific to the outcome of the individual with a musculoskeletal condition or the spouse, we tested for interactions with a ‘role’ variable, where spouses were coded as −1 and IMCs were coded as 1. For instance, this allowed us to determine if the IMC’s physical activity was related to spouse’s depressive symptoms only or vice versa. All predictors were centred on the grand mean in our APIM model. Finally, we explored interactions with gender, but no significant effects were found.
Results
Descriptives
Firstly, we calculated the means and standard deviations for each primary variable. Spouse’s PAI mean score was 3135 kcal/week (SD = 5179). IMC’s PAI score was 2376 kcal/week (SD = 3120). Spouse’s scores were not significantly higher than the scores of the individuals with the musculoskeletal conditions [IMCs; t(76) = 1.31, p = 0.20]. The US Surgeon General’s physical activity recommendation for older adults is 1000 kcal/week. Spouse mean score for depressive symptoms was 9.60 (SD = 7.94), which was marginally significantly higher than for IMCs [M = 7.72, SD = 6.07; t(76) = 1.78, p = 0.08]. In terms of covariates, spouses had a mean physical comorbidity score of 2.91 (SD = 1.95), and IMCs had a mean physical comorbidity score of 3.69 [SD = 2.47; t(75) = −2.24, p = 0.03]. Spouses’ mean rating of stress with providing IADL support was 1.40 (SD = 0.52, range = 1–3.33), and IMC’s reported needing help with an average of 1.10 IADLs (SD = 1.34, range = 0–4). IMCs rated their average pain as 3.65 (SD = 2.49). Spouses’ mean marital satisfaction score was 95.69 (SD = 19.35), and the IMC’s mean score was 96.36 (SD = 15.99), which were not significantly different [t(76) = −0.32, p = 0.75].
Correlational analyses indicated that there were no significant covariates with both physical activity and depressive symptoms. However, we did find that spouses’ depressive symptoms were significantly related to more chronic conditions [r(76) = 0.28, p <0.05] and more stress with providing IADL support [r(76) = 0.27, p <0.05]. Also, IMCs’ depressive symptoms were related to lower IMC [r(76) = −0.49, p <0.001] and spouse [r(76) = −0.28, p <0.05] marital satisfaction.
Hypothesis 1: Association between partners’ physical activity
There was a positive correlation between spouse and IMC physical activity levels [r(76) = 0.23, p <0.05]. The greater the IMC’s physical activity, the greater the spouse’s physical activity. The intraclass correlation was 0.23 (p = 0.02).
Hypothesis 2: Association between physical activity and one’s own depressive symptoms (actor effects)
As shown in Table I, one’s physical activity was not significantly associated with own depressive symptoms. This finding did not differ by role (spouse versus IMC). Our hypothesis was not supported that greater physical activity relates to less depressive symptoms for either IMCs or spouses.
Hypothesis 3: Association between physical activity and the partner’s depressive symptoms (partner effects)
Table I.
Simplified SPSS mixed model testing the actor–partner interdependence model predicting depressive symptoms
| B | SE | df | t | |
|---|---|---|---|---|
| Step 1 | ||||
| Intercept | 5.98** | 1.61 | 72.64 | 3.71 |
| Role | 1.76 | 1.09 | 72.83 | 1.61 |
| Actor physical activity | −0.95 | 1.10 | 138.57 | −0.86 |
| Partner physical activity | −1.74 | 1.09 | 133.81 | −1.60 |
| Step 2 | ||||
| Intercept | 7.62** | 2.69 | 71 | 2.83 |
| Role | 0.16 | 1.82 | 71 | 0.09 |
| Actor physical activity | −3.75 | 3.42 | 110.63 | −1.10 |
| Partner physical activity | 5.66† | 3.37 | 114.43 | 1.68 |
| Role * actor physical activity | 1.88 | 2.30 | 126.88 | 0.82 |
| Role * partner physical activity | −5.46* | 2.31 | 124.14 | −2.36 |
| abs(actor physical activity –partner physical activity) | −3.29 | 4.18 | 71 | −0.79 |
| Role * abs(actor physical activity –partner physical activity) | 3.01 | 2.82 | 71 | 1.07 |
All predictor variables were centred on the mean and simultaneously entered into the models. Including theoretically related variables in the model did not significantly change the results: both partners’ age, gender, chronic conditions and marriage length, and IMC’s physical functioning.
p <0.01.
p <0.05.
p <0.10.
As shown in Table I, there was a significant interaction between partner physical activity and role predicting actor depressive symptoms. Using the guidelines suggested by Aiken and West, 1991, the simple slopes analysis revealed that the association between IMCs’ physical activity and spouses’ depressive symptoms was significant [B = −4.57, SE = 1.68, β = −0.30, t(76) = −2.73, p <0.01, R2 = 0.30]. Specifically, less physical activity in the IMCs was significantly related to more depressive symptoms in spouses. However, the simple slopes analysis revealed that the association between spouses’ physical activity and IMCs’ depressive symptoms was not significant [B = −0.25, SE = 1.34, β = −0.02, t(74) = −0.19, p = 0.85, R2 = 0.02], indicating that low physical activity in spouses was not related to increased depressive symptoms in IMCs. These findings partially support our hypothesis that one partner’s physical activity is associated with the other partner’s depressive symptoms.
Hypothesis 4: Similarity between partners’ physical activity levels predicting each partner’s depressive symptoms
As shown in Table I, the absolute difference term between actor physical activity and partner physical activity predicting depressive symptoms was not significant. The interaction with role (spouse versus IMC) also did not emerge significant. Thus, we did not find that the similarity of partners’ physical activity had a significant association with either partner’s depressive symptoms.
Discussion
We examined the associations between partners’ physical activity and depressive symptoms among older married couples in which one person suffered from a musculoskeletal condition. As expected, we found that when one partner engaged in high levels of physical activity, the other partner also engaged in high levels of physical activity (H1). Alternatively, when one partner engaged in low levels of physical activity, the other partner engaged in low levels of physical activity. This finding supports past research showing that older adult spouses’ physical activity levels are positively related (Pettee et al., 2006), but extends the literature to the context of older married couples dealing with a musculoskeletal condition. Thus, even when there is an imbalance in functional ability and/or symptoms of pain, spouses may have an important influence on one another in terms of physical activity. Alternatively, they may share an environment that influences both partners’ physical activity (Meyler et al., 2007).
We did not find that one’s own physical activity level was related to one’s own depressive symptoms (H2; the actor effect). This was true for both the individuals with the musculoskeletal conditions (IMCs) and spouses. This non-significant finding is inconsistent with past studies showing protective effects of physical activity on depressive symptoms among older adults (Kahana et al., 2002; King et al., 2000). It is possible that there was not adequate variability in both the depressive symptoms and physical activity levels for each individual in this sample to elicit significant associations. Most participants were highly active and experienced few depressive symptoms. Although we recruited couples in which a person had a musculoskeletal condition, our study required older couples to come into the lab and to be mobile. This potentially selected for more physically active and less depressed individuals. We suspect that future research with a larger, more diverse sample is likely to find significant actor effects of physical activity on depressive symptoms in the context of couples coping with one partner’s pain.
It is important to note that in the present study, correlation analysis indicated that low marital satisfaction was significantly (and marginally significantly) related to depressive symptoms for both partners, consistent with past research showing longitudinal associations (Whisman & Uebelacker, 2009). Thus, in this sample, marital satisfaction may have been a particularly important factor in determining psychological well-being for each individual. That said, our data showed a significant interpersonal association between physical activity and depressive symptoms that was unrelated to marital satisfaction.
Partially supporting hypothesis 3 (partner effect), the physical activity of the IMC was associated with their spouse’s depressive symptoms. This finding may suggest that low physical activity in the partner with the pain condition leads the spouse to feel restricted in their activities and in turn leads to feelings of guilt or frustration (Williamson et al. 1998), and these feelings may in turn predict depressive symptoms (Trief, Ploutz-Snyder, Britton, & Weinstock, 2004). It may also be that spouses are more distressed by seeing the lack of physical activity in their partner compared with not engaging in physical activity themselves. It is possible that spouses view low levels of physical activity as a personal choice for themselves but as a sign of a limitation for their partner. Future research would benefit from examining the types of attributions spouses make for the physical activity or lack of physical activity for themselves and their partners. It is also important to note that the association between the physical activity of the partner with the condition and spouse depressive symptoms was independent of spouse’s stress with providing support to the partner. Instead of caregiving burden, spouses may have been more depressed because they were focusing on the partner’s limitations (Monin & Schulz, 2009; Schwartz, Slater, Birchler, & Atkinson, 1991), which was made salient in our study. Related to this point, the association between spouses’ physical activity and the depressive symptoms of the partner with the condition was not significant. As the partner’s condition may be of greater focus in the relationship, the health behaviours of the ‘healthier’ spouse may not be as of much concern for each partner’s psychological well-being.
Finally, the similarity of physical activity of partners did not have a significant association with either partner’s depressive symptoms (H4). Although we found that partner’s physical activity levels were positively related (H1), we did not find evidence that when both partners engaged in high levels of physical activity, either partner was protected in terms of less depressive symptoms. We also did not find that when both partners were low in physical activity, depressive symptoms were particularly high or low for either partner. This suggests that similarities of couple members’ physical activity habits were not enough to predict positive outcomes in terms of less depressive symptoms. It may be the case that in couples where there is an imbalance in functionality or physical symptoms, such as pain, a discrepancy between partners’ physical activity is less meaningful for the psychological well-being of both partners. The musculoskeletal condition may be viewed as accounting for the discrepancy in physical activity, whereas in healthy couples, a discrepancy may be a sign that partners’ do not share the same ideals or have the same motivation for being physically active (Meyler et al, 2007). Taken together, our findings suggest that physical activity of individuals with musculoskeletal conditions and their spouses are related, but that the physical activity of the person with the musculoskeletal condition seems to be more impactful for the spouse’s well-being.
Strengths, limitations and future directions
A major strength of this study is that it takes into account the social context in which physical activity and disability occurs. In doing so, we examined a wide range of factors associated with each individual’s health and their relationship that may have affected each partner’s physical activity and well-being. However, when interpreting our findings, a number of limitations need to be considered. Firstly, physical activity data were obtained through self-report methods and could be influenced by a number of factors, such as the inability to accurately recall physical activity participation. We also did not have information about participants’ exercise history or more objective indicators of physical health, such as weight. Moreover, the majority of the participants were Caucasian; therefore, results may not be generalizable to the larger US population. In addition, participants were ‘younger’ older adults; they were not randomly sampled; and they were all cognitively high functioning. Also, it is important to acknowledge that the CES-D has been shown to have four dimensions (somatic, depressed affect, positive affect and interpersonal processes; Shafer, 2006). In the present study, our measure loaded on one factor, and we used the overall score as the criterion variable, allowing us to make clinical comparisons with other studies using the 20-item score. However, it will be important to examine how physical activity relates to the different dimensions of depressive symptomatology in future research. Finally, causal associations could not be inferred due to the cross-sectional nature of the data. It is likely that the associations between physical activity and depressive symptoms are bidirectional. For example, it is plausible that a spouse’s depressive symptoms influence the physical activity levels of their partner with a musculoskeletal condition. Research shows that people who are depressed tend to be more sedentary (Weyerer & Kupfer, 1994), and it has been suggested that depression may lead to decreased levels of exercise due to low motivation and energy (Roshanaei-Moghaddam, Katon, & Russo, 2009). When spouses are depressed, they may also be less likely to encourage their partners with the condition to engage in physical activity. In addition, a spouse’s depression may directly influence the partner’s depression through emotional contagion leading to lower physical activity in both partners. That said, we encourage replication of all tested paths, with a focus on establishing causal associations between physical activity and depression among older spousal pairs.
Implications
Our focus on examining older couples’ physical activity from a dyadic level is critical for the future development of tailored couple-oriented interventions (Martire, Schulz, Helgeson, Small, & Saghafi, 2010). Findings from the current study suggest that couple-oriented interventions for individuals with musculoskeletal conditions and their spouses should aim to enhance the physical activity level of both individuals. However, focusing on increasing the physical activity of the individual with the musculoskeletal condition may be particularly impactful for the spouse’s mental health, especially because it may relieve patient suffering (Monin & Schulz, 2009). In addition, older adults’ health and well-being may benefit when clinicians take into account the interdependency of health behaviours with close relationship partners. For instance, when treating an individual patient, it may be beneficial for physicians to consider the patient’s close social environment, particularly spouses, as their health behaviours may facilitate or inhibit the patient’s health behaviours. At the same time, physicians should monitor the psychological well-being of spouse’s of patients with musculoskeletal conditions who are engaging in low levels of physical activity.
Acknowledgments
Funding sources include a career development award to Joan Monin from the National Institute on Aging, National Institutes of Health (K01 AG042450-01A1) and an award from Yale’s Pepper Center (P30AG021342).
Footnotes
Three of the spouses indicated at the lab session that they had osteoarthritis or lower back pain. Excluding them from analysis did not change the results.
Conflict of interest
The authors have declared that they have no conflict of interest.
References
- Abell JE, Hootman JM, Zack MM, Moriarty D, Helmick CG. Physical activity and health related quality of life among people with arthritis. Journal of Epidemiology and Community Health. 2005;59(5):380–385. doi: 10.1136/jech.2004.028068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Thousand Oaks: Sage; 1991. [Google Scholar]
- Blumenthal JA, Babyak MA, Moore KA, Craighead E, Herman S, Khatri P, Krishnan R. Effects of exercise training on older patients with major depression. Archives of Internal Medicine. 1999;159:2349–2356. doi: 10.1001/archinte.159.19.2349. [DOI] [PubMed] [Google Scholar]
- Carstensen LL, Gottman JM, Levenson RW. Emotional behavior in long-term marriage. Psychology and Aging. 1995;10(1):140–149. doi: 10.1037//0882-7974.10.1.140. [DOI] [PubMed] [Google Scholar]
- Cook WL, Kenny DA. The actor–partner interdependence model: A model of bidirectional effects in developmental studies. International Journal of Behavioral Development. 2005;29(2):101–109. [Google Scholar]
- Ettinger WH, Burns R, Messier SP, Applegate W, Rejeski WJ, Morgan T, Craven T. A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis: The Fitness Arthritis and Seniors Trial (FAST) JAMA. 1997;277(1):25–31. [PubMed] [Google Scholar]
- Godwin KM, Swank PR, Vaeth P, Ostwald SK. The longitudinal and dyadic effects of mutuality on perceived stress for stroke survivors and their spousal caregivers. Aging & Mental Health. 2013;17(4):423–431. doi: 10.1080/13607863.2012.756457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham JM. Self-expansion and flow in couples’ momentary experiences: An experience sampling study. Journal of Personality and Social Psychology. 2008;95(3):679–694. doi: 10.1037/0022-3514.95.3.679. [DOI] [PubMed] [Google Scholar]
- Hawker GA, Gignac MA, Badley E, Davis AM, French MR, Li Y, Lou W. A longitudinal study to explain the pain–depression link in older adults with osteoarthritis. Arthritis Care & Research. 2011;63(10):1382–1390. doi: 10.1002/acr.20298. [DOI] [PubMed] [Google Scholar]
- Hoppmann C, Gerstorf D. Spousal interrelations in old age—A mini-review. Gerontology. 2009;55(4):449–459. doi: 10.1159/000211948. [DOI] [PubMed] [Google Scholar]
- Kahana E, Lawrence RH, Kahana B, Kercher K, Wisniewski A, Stoller E, Stange K. Long-term impact of preventive proactivity on quality of life of the old-old. Psychosomatic Medicine. 2002;64(3):382–394. doi: 10.1097/00006842-200205000-00003. [DOI] [PubMed] [Google Scholar]
- Kahana E, Young R. Clarifying the caregiving paradigm: Challenges for the future. In: Beigel DE, Blum A, editors. Aging and caregiving: Theory, research, and policy. Thousand Oaks: Sage; 1990. pp. 76–97. [Google Scholar]
- Kashy DA, Kenny DA. The analysis of data from dyads and groups. In: Reis HT, Judd CM, editors. Handbook of research methods in social psychology. New York: Cambridge University Press; 1999. [Google Scholar]
- Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of ADL: A standardized measure of biological and psychosocial function. JAMA. 1963;185(12):914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- Kelley HH, Thibault JW. Interpersonal relations. New York: Wiley; 1978. [Google Scholar]
- Kenny DA, Kashy DA, Cook WL. Dyadic data analysis. New York: Guilford Press; 2006. [Google Scholar]
- Kerse N, Hayman KJ, Moyes SA, Peri K, Robinson E, Dowell A, Arroll B. Home-based activity program for older people with depressive symptoms: DeLLITE—A randomized controlled trial. The Annals of Family Medicine. 2010;8(3):214–223. doi: 10.1370/afm.1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King AC, Pruitt LA, Phillips W, Oka R, Rodenburg A, Haskell WL. Comparative effects of two physical activity programs on measured and perceived physical functioning and other health-related quality of life outcomes in older adults. The Journals of Gerontology A: Biological Sciences Medical Sciences. 2000;55(2):M74–M83. doi: 10.1093/gerona/55.2.m74. [DOI] [PubMed] [Google Scholar]
- King AC, Baumann K, O’Sullivan P, Wilcox S, Castro C. Effects of moderate-intensity exercise on physiological, behavioral, and emotional responses to family caregiving: A randomized controlled trial. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2002;57(1):M26–M36. doi: 10.1093/gerona/57.1.m26. [DOI] [PubMed] [Google Scholar]
- Lampinen P, Heikkinen E. Gender differences in depressive symptoms and self-esteem in different physical activity categories among older adults. Women in Sports and Physical Activity Journal. 2002;11:171–197. [Google Scholar]
- Locke HJ, Wallace KM. Short marital-adjustment and prediction tests: Their reliability and validity. Marriage & Family Living. 1959;21(3):251–255. [Google Scholar]
- Martire LM, Lustig AP, Schulz R, Miller GE, Helgeson VS. Is it beneficial to involve a family member? A meta-analysis of psychosocial interventions for chronic illness. Health Psychology. 2004;23(6):599–611. doi: 10.1037/0278-6133.23.6.599. [DOI] [PubMed] [Google Scholar]
- Martire LM, Schulz R, Helgeson VS, Small BJ, Saghafi EM. Review and meta-analysis of couple-oriented interventions for chronic illness. Annals of Behavioral Medicine. 2010;40(3):325–342. doi: 10.1007/s12160-010-9216-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyler D, Stimpson JP, Peek MK. Health concordance within couples: A systematic review. Social Science & Medicine. 2007;64(11):2297–2310. doi: 10.1016/j.socscimed.2007.02.007. [DOI] [PubMed] [Google Scholar]
- Monin JK, Schulz R. Interpersonal effects of suffering in older adult caregiving relationships. Psychology and Aging. 2009;24(3):681–695. doi: 10.1037/a0016355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monin JK, Schulz R, Martire LM, Jennings JR, Lingler JH, Greenberg MS. Spouses’ cardiovascular reactivity to their partners’ suffering. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2010;65(2):195–201. doi: 10.1093/geronb/gbp133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monin JK, Zhou L, Kershaw T. Attachment and psychological health in older couples coping with pain. GeroPsych. doi: 10.1024/1662-9647/a000110. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan WP, Goldston SE. Exercise and mental health. New York: Taylor & Francis; 2013. [Google Scholar]
- National Institute of Arthritis and Musculoskeletal and Skin Diseases. 2011 [Google Scholar]
- Nieboer AP, Schulz R, Matthews KA, Scheier MF, Ormel J, Lindenberg SM. Spousal caregivers’ activity restriction and depression: a model for changes over time. Social Science & Medicine. 1998;47(9):1361–1371. doi: 10.1016/s0277-9536(98)00214-7. [DOI] [PubMed] [Google Scholar]
- Paffenbarger RS, Jr, Blair SN, Lee IM, Hyde RT. Measurement of physical activity to assess health effects in free-living populations. Medicine and Science in Sports and Exercise. 1993;25(1):60–70. doi: 10.1249/00005768-199301000-00010. [DOI] [PubMed] [Google Scholar]
- Paffenbarger RS, Wing AL, Hyde RT. Physical activity as an index of heart attack risk in college alumni. American Journal of Epidemiology. 1978;108:161–175. doi: 10.1093/oxfordjournals.aje.a112608. [DOI] [PubMed] [Google Scholar]
- Penedo FJ, Dahn JR. Exercise and well-being: A review of mental and physical health benefits associated with physical activity. Current Opinion in Psychiatry. 2005;18(2):189–193. doi: 10.1097/00001504-200503000-00013. [DOI] [PubMed] [Google Scholar]
- Penninx BW, Messier SP, Rejeski WJ, Williamson JD, DiBari M, Cavazzini C, Pahor M. Physical exercise and the prevention of disability in activities of daily living in older persons with osteoarthritis. Archives of Internal Medicine. 2001;161(19):2309–2316. doi: 10.1001/archinte.161.19.2309. [DOI] [PubMed] [Google Scholar]
- Pettee KK, Brach JS, Kriska AM, Boudreau ROBERT, Richardson CR, Colbert LH, Newman AB. Influence of marital status on physical activity levels among older adults. Medicine and Science in Sports and Exercise. 2006;38(3):541–546. doi: 10.1249/01.mss.0000191346.95244.f7. [DOI] [PubMed] [Google Scholar]
- Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. Journal of the American Geriatrics Society. 1975;23(10):433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- Pruchno RA. Studying caregiving families: Theoretical and methodological challenges. In: Light E, Niederhe G, Lebowitz BD, editors. Stress effects on family caregivers of Alzheimer’s patients. New York: Springer; 1994. pp. 333–350. [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurements. 1977;1:385–401. [Google Scholar]
- Robles TF, Slatcher RB, Trombello JM, McGinn MM. Marital quality and health: A meta-analytic review. 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg DE, Bombardier CH, Artherholt S, Jensen MP, Motl RW. Self-reported depression and physical activity in adults with mobility impairments. Archives of Physical Medicine and Rehabilitation. 2013;94:731–736. doi: 10.1016/j.apmr.2012.11.014. [DOI] [PubMed] [Google Scholar]
- Roshanaei-Moghaddam B, Katon WJ, Russo J. The longitudinal effects of depression on physical activity. General Hospital Psychiatry. 2009;31(4):306–315. doi: 10.1016/j.genhosppsych.2009.04.002. [DOI] [PubMed] [Google Scholar]
- Schulz R, Beach SR, Hebert RS, Martire LM, Monin JK, Tompkins CA, Albert SM. Spousal suffering and partner’s depression and cardiovascular disease: The cardiovascular health study. American Journal of Geriatric Psychiatry. 2009;17:246–254. doi: 10.1097/JGP.0b013e318198775b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz L, Slater MA, Birchler GR, Atkinson JH. Depression in spouses of chronic pain patients: the role of patient pain and anger, and marital satisfaction. Pain. 1991;44(1):61–67. doi: 10.1016/0304-3959(91)90148-Q. [DOI] [PubMed] [Google Scholar]
- Shafer AB. Meta-analysis of the factor structures of four depression questionnaires: Beck, CES-D, Hamilton, and Zung. Journal of clinical psychology. 2006;62(1):123–146. doi: 10.1002/jclp.20213. [DOI] [PubMed] [Google Scholar]
- Teychenne M, Ball K, Salmon J. Physical activity and likelihood of depression in adults: A review. Preventive Medicine. 2008;46(5):397–411. doi: 10.1016/j.ypmed.2008.01.009. [DOI] [PubMed] [Google Scholar]
- Townsend AL, Miller B, Guo S. Depressive symptomatology in middle-aged and older married couples a dyadic analysis. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2001;56(6):S352–S364. doi: 10.1093/geronb/56.6.s352. [DOI] [PubMed] [Google Scholar]
- Trief PM, Ploutz-Snyder R, Britton KD, Weinstock RS. The relationship between marital quality and adherence to the diabetes care regimen. Annals of Behavioral Medicine. 2004;27(3):148–154. doi: 10.1207/s15324796abm2703_2. [DOI] [PubMed] [Google Scholar]
- Wendel-Vos GCW, Schuit AJ, Tijhuis MAR, Kromhout D. Leisure time physical activity and health-related quality of life: Cross-sectional and longitudinal associations. Quality of Life Research. 2004;13(3):667–677. doi: 10.1023/B:QURE.0000021313.51397.33. [DOI] [PubMed] [Google Scholar]
- West TV, Popp D, Kenny DA. A guide for the estimation of gender and sexual orientation effects in dyadic data: An actor–partner interdependence model approach. Personality and Social Psychology Bulletin. 2008;34:321–336. doi: 10.1177/0146167207311199. [DOI] [PubMed] [Google Scholar]
- Weyerer S, Kupfer B. Physical exercise and psychological health. Sports Medicine. 1994;17(2):108–116. doi: 10.2165/00007256-199417020-00003. [DOI] [PubMed] [Google Scholar]
- Whisman MA, Uebelacker LA. Prospective associations between marital discord and depressive symptoms in middle-aged and older adults. Psychology and Aging. 2009;24(1):184–189. doi: 10.1037/a0014759. [DOI] [PubMed] [Google Scholar]
- Williamson GM, Shaffer DR, Schulz R. Activity restriction and prior relationship history as contributors to mental health outcomes among middle-aged and older spousal caregivers. Health Psychology. 1998;17(2):152–162. doi: 10.1037//0278-6133.17.2.152. [DOI] [PubMed] [Google Scholar]


