Abstract
Background
Ethyl glucuronide (EtG) is an alcohol biomarker with potential utility as a clinical research and alcohol treatment outcome. Debate exists regarding the appropriate cutoff level for determining alcohol use, particularly with the EtG immunoassay. This study determined the EtG immunoassay cutoff levels that most closely correspond to self-reported drinking in alcohol dependent outpatients.
Methods
Eighty adults with alcohol dependence and mental illness, taking part in an alcohol treatment study, provided urine samples three times per week for up to 16-weeks (1589 samples). Self-reported drinking during 120 hours prior to each sample collection was assessed. Receiver Operating Characteristic analyses were conducted to assess the ability of the EtG immunoassay to detect self-reported alcohol use across 24–120 hour time periods. Sensitivity and specificity of EtG immunoassay cutoff levels was compared in 100 ng/mL increments (100 ng/mL–500 ng/mL) across 24–120 hours.
Results
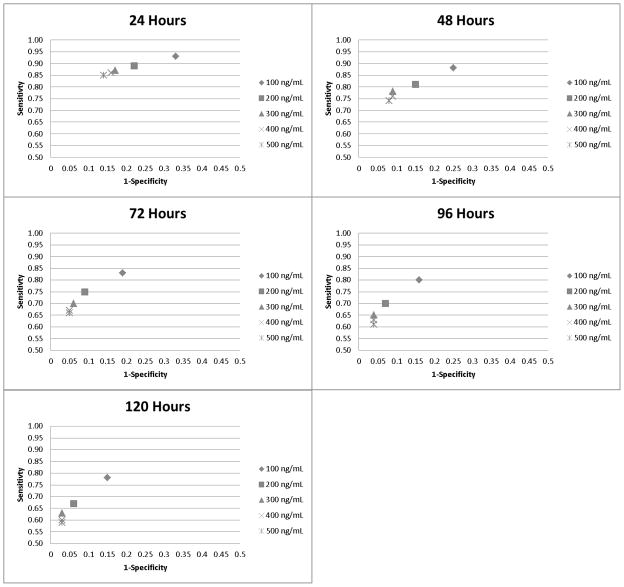
Over half (57%) of the 1589 samples indicated recent alcohol consumption. The EtG immunoassay closely corresponded to self-reported drinking from 24 (AUC=0.90, 95% CI:0.88, 0.92) to 120 hours (AUC=0.88, 95% CI:0.87, 0.90). When cutoff levels were compared across 24–120 hours, 100 ng/mL had the highest sensitivity (0.93–0.78) and lowest specificity (0.67–0.85). Relative to 100 ng/mL, the 200 ng/mL cutoff demonstrated a reduction in sensitivity (0.89–0.67), but improved specificity (0.78–0.94). The 300 ng/mL, 400 ng/mL, and 500 ng/mL cutoffs demonstrated the lowest sensitivity (0.86 to 0.33) and highest specificity (0.86–0.97) over 24 to 120 hours.
Conclusions
For detecting alcohol use for greater than 24 hours, the 200 ng/mL cutoff level is recommended for use as a research and clinical outcome.
Keywords: ethyl glucuronide, urine testing, alcohol biomarkers, alcohol treatment
An estimated 17 million Americans suffer from alcohol use disorders (Office of Applied Studies, 2013, Grant et al., 2004) and nearly 80,000 people die from alcohol-related causes every year (CDC, 2004). Accurate assessment of alcohol use is needed to identify alcohol use disorders and evaluate treatment effectiveness. Currently, self-report instruments such as the Alcohol Timeline Follow Back (ATLFB) and Alcohol Use Disorders Identification Test (AUDIT) are considered the “gold standard” of alcohol assessment in clinical research and treatment. However, the validity of self-reported alcohol use can vary (Babor et al., 2000, Del Boca and Noll, 2000), particularly when respondents face social, treatment, or legal contingencies for alcohol use (Langenbucher and Merrill, 2001).
The combination of self-report and biological assessments of alcohol use, such as point-of-care drug immunoassay urine tests, is considered to be the best method for assessing illicit drug use (Donovan et al., 2012, Jatlow and O’Malley, 2010). These urine tests are frequently used in research and treatment settings because of their accuracy, rapid results, and detection period of at least 48 hours (Chermack et al., 2000, Ries et al., 2002, Donovan et al., 2012). Though many biomarkers of recent alcohol consumption exist, none to date have demonstrated a detection period of more than 48 hours while still being feasible for use in a clinical research or treatment setting. Measures of blood alcohol content such as breath-tests or urinary ethanol can only detect alcohol use during the preceding 12 hours, making them suitable for detecting current intoxication only (Helander et al., 1996). Transdermal alcohol monitors allow for continuous monitoring, but are relatively expensive and questions exist regarding their feasibility, convenience, and perceived stigma due to use in forensic settings (Gurvich et al., 2013). Enzymes such as gamma-glutamyltransferase (GGT) can be measured at increased levels in people with alcohol dependence, but have limited utility in detecting low levels of drinking, or infrequent, non-chronic binge drinking (Goldberg, 1980, Rosalki, 1975). Carbohydrate-deficient transferrin (CDT) is the most specific serum biomarker of heavy alcohol consumption, however the sensitivity is somewhat limited, especially in people with severe liver disease, and point-of-care analysis of CDT is not yet feasible (Anton 2001, Bertholet et al., 2014). Phosphatidylethanol (PEth) has shown potential for detecting heavy drinking episodes for approximately two weeks but may have difficulty detecting lower levels of alcohol consumption, and requires blood collection, which may not be feasible in addiction treatment settings (Helander et al., 2012). Finally, ethyl sulfate (EtS) has performed well as a biomarker for recent alcohol consumption (up to 36 hours); however, there is no commercially available EtS immunoassay (Helander et al., 2005, Wurst et al., 2006). Therefore these tests, while valuable in other contexts, have limited utility in clinical research or treatment settings.
Ethyl glucuronide (EtG) is a minor non-oxidative hepatic metabolite of ethanol. It can be detected in a variety of bodily tissues (e.g., hair, nails) and in urine. A commercially-available immunoassay test of this metabolite can be conducted by non-technical staff using a relatively small bench-top analyzer that delivers results of a semi-quantitative assessment of EtG concentration in urine within twenty minutes (Leickly et al., under review). This semi-quantitative assessment allows for the use of varying cutoff levels above which results are considered to be positive for alcohol consumption. Preliminary studies have shown EtG immunoassay to have detection rates similar to the more established liquid chromatography-tandem mass spectrometry (LC-MS/MS) method of EtG testing (McDonell et al., 2011a, Böttcher et al., 2008, Leickly et al., in press), which has limited utility in clinical settings as it requires transportation of samples to commercial laboratories, and carries a relatively high cost.
Despite its promise as an alcohol biomarker, widespread use of EtG remains limited outside of forensic settings. Due to concerns about over-detection of alcohol use based on incidental non-beverage alcohol exposure, the Substance Abuse and Mental Health Services Administration (SAMHSA) Advisory (2012) recommended a relatively conservative cutoff level of 500 ng/mL. However, few studies have examined this issue in alcohol dependent populations (Jatlow & O’Malley, 2010). Furthermore, when EtG is used as a clinical research or treatment outcome, the 500 ng/mL cutoff level may under-detect drinking (Anton, 2014, Jatlow & O’Malley, 2010, Jatlow et al., 2014). Therefore, research is needed to build consensus regarding an acceptable EtG cutoff level, as commercial laboratories, immunoassay manufacturers, and foreign regulatory authorities use cutoff levels ranging from 100 ng/mL to 1000 ng/mL (Thierauf et al., 2010, Thierauf et al., 2009, Rohrig et al., 2006).
In a recently published study, Jatllow and colleagues (2014) used an alcohol challenge paradigm and data gathered from two clinical trials to investigate appropriate EtG cutoff levels. In the alcohol challenge study, standardized low, medium, and high doses of alcohol were administered to a small sample (n=18) of non-alcohol dependent participants and their EtG levels were monitored via LC/MS-MS analysis over 12, 24, 48, and 72 hours. At 12 hours post-administration, detection rates of low-dose alcohol use by EtG at the 100 ng/mL and 200 ng/mL cutoffs were both 100%. In contrast, the 500ng/mL cutoff only detected 50% of cases of low dose alcohol use. Results from the clinical trials mirrored those of the challenge study, and saw slight increases in sensitivity at lower cutoffs. Data from the three phases of this study suggests that EtG cutoff levels much lower than 500 ng/mL are needed to detect moderate to low levels of drinking, particularly when detecting alcohol use for more than 48 hours. In addition, results of this study provide initial evidence that relatively low cutoff levels might be appropriate to detect alcohol use in clinical research.
Despite results of Jatlow et al. (2014) and similar studies, no previous research has investigated optimal cutoff levels for detecting any recent drinking using the EtG immunoassay. Further, most previous studies of EtG rely on small samples sizes (Albermann et al., 2012, Dahl, et al., 2011), few within subject observations (Jatlow et al., 2014, Wurst, 2008), and include participants with relatively low levels of alcohol consumption (Anton, 2014, Wurst, et al., 2004). The current study compares the sensitivity and specificity of varying EtG immunoassay cutoff levels, ranging from 100 ng/mL to 500 ng/mL, when detecting any self-reported alcohol use across 24 to 120 hours in a total of 1589 samples submitted by 80 alcohol dependent adults.
Materials and Methods
Participants
Participants were 80 adults with DSM-IV (American Psychiatric Association, 2000) diagnoses of alcohol dependence and co-occurring mood (72.4%, n=55) or psychotic (27.6%, n=21) disorder. Their average age was 47.2 (SD=11.2), and 71.3% (n=57) of participants were male. Reported ethnicities were 53.8% (n=43) Caucasian, 30% (n=24) African-American, 7.6% (n=6) Hispanic, 2.5% (n=2) American Indian, 1.3% (n=1) Asian/Pacific, 3.8% (n=3) multiracial and 1.3% (n=1) other ethnicities. At baseline, participants reported drinking on average 16.2 days (SD=8.1) out of the previous 30 days.
Study Procedures
All study procedures were approved by the Institutional Review Board of the University of Washington. Participants were enrolled in a randomized controlled trial of a contingency management intervention for alcohol dependence. More information about the parent grant can be found at clinicaltrials.gov (identifier: NCT01567943). All participants participated in a four-week baseline observation period where they submitted urine samples and provided self-reported alcohol use three times per week. They received reimbursement in the form of prizes for submitting these data. Participants were then randomized to 12 weeks of a contingency management group where they received prizes for submitting urine samples negative for alcohol and gift cards for attending intensive outpatient addiction treatment groups, or a non-contingent control group where they received prizes for submitting urine samples and self-report data. All participants received treatment-as-usual, which included intensive outpatient addiction treatment located in an urban community mental health center in Seattle, WA. As part of their involvement in this study, participants submitted up to 51 urine samples (M=19.0, SD=16.0) for EtG immunoassay testing. These urine samples were collected three times per week across a 16-week assessment period, and monthly during a 3-month follow-up period. A total of 1589 urine samples were collected.
EtG immunoassays were conducted onsite at an outpatient addiction clinic by clinical research staff using spectrophotometry on a commercially available ThermoFisher Indiko analyzer (Fremont, CA). Bachelor’s degree-level research staff with no formal laboratory or technical training participated in a one-day training on the operations and maintenance of the analyzer before performing analyses. Diagnostic Reagents Incorporated EtG enzyme immunoassay tests were conducted using EtG 100 ng/mL, 500 ng/mL, 1000 ng/mL, 2000 ng/mL, and Negative calibrators and EtG 100 ng/mL and 375 ng/mL controls. Antibody/Substrate and Enzyme Conjugate reagents were used and the analyzer was calibrated weekly. To prevent bacterial hydrolysis, a reported source of exogenous EtG in urine samples (Helander et al., 2007), all samples were analyzed on the day of collection, and stored until analysis in a 4°C refrigerator with all calibrators, controls, and reagents. The DRI EtG immunoassay is linear up to 2000 ng/mL, with a reportable range of 0 ng/mL to 2000 ng/mL (the range of the lowest and highest calibrators). As per manufacturer recommendation, dilution procedures were conducted when EtG immunoassay concentrations displayed an error message indicating high absorbance. Only ten samples (0.6%) required dilution due to high absorbance.
To avoid positive EtG immunoassay results due to inadvertent alcohol exposure, participants were advised at the beginning of the study and reminded at each appointment to avoid using non-beverage sources of ethanol, including hand sanitizers and mouthwashes. Use of chloral hydrate, the only medication known to interfere with EtG immunoassay analysis (Arndt et al., 2009), was not reported by study participants when asked monthly about prescription medications used.
A measure was created for the purposes of this study to assess the hours since the last drinking episode, as well as the number of standard drinks consumed at the last drinking episode. These variables are known to have the greatest impact on EtG test results. These data were collected using a calendar method, similar to the Alcohol Timeline Follow Back (TLFB; Sobell & Sobell, 2000). Self-reported hours since last alcohol use (up to 120 hours) were assessed as a continuous integer when each urine sample was collected. Standard drinks consumed at the most recent drinking episode were also assessed as a continuous integer. Using these data a summary variable was created that indicated whether or not any alcohol use occurred in the prior 24, 48, 72, 96, and 120 hour period (e.g., the 48-hr detection period includes drinking that occurred between 1 to 48 hours).
Data Analysis
Receiver operator characteristics (ROC) analyses were conducted to investigate the sensitivity and specificity of EtG immunoassay in terms of predicting self-reported alcohol use. Hours since last drink, recorded as a continuous integer at each urine sample collection, was coded into a binary measure for positive/negative self-reported alcohol use at 24, 48, 72, 96, and 120-hour detection periods. ROC analyses were conducted separately for each of the detection periods and the Area Under the Curve (AUC) and 95% confidence intervals were calculated. For each of the five assessment periods the sensitivity and specificity of EtG immunoassay cutoff was reported in 100 ng/mL intervals, ranging from 100 ng/mL to 500 ng/mL. Statistical analyses were conducted in SPSS version 19.0 (IBM, 2010).
Results
Participants self-reported alcohol use within the previous 5 days on 57.2% (909/1589) of assessments. The mean number of standard drinks reported during the last drinking episode was 4.12 (SD=6.37, range 0–96). EtG immunoassay results were positive in 50.7% (805/1589) and 34.8% (553/1589) of the samples at the 100 ng/mL and 500 ng/mL cutoff levels, respectively. EtG immunoassay results suggested a bimodal distribution, with values clustering near the lower (0 ng/mL) and upper limits of the immunoassay (2,000 ng/mL). Therefore, while the mean EtG immunoassay value was 682 ng/mL (SD=865 ng/mL), the median value was 104 ng/mL.
Sensitivity and Specificity
Overall, the EtG immunoassay was able to correctly identify self-reported drinking from 24 (AUC=0.90, 95% CI: 0.88, 0.92) to 120 hours (AUC=0.88, 95% CI: 0.87, 0.90). When balancing sensitivity and specificity, optimal EtG immunoassay cutoff levels for different times periods since last drink were as follows: 420 ng/mL (24 hours, sensitivity=0.86, specificity=0.85), 150 ng/mL (48 hours, sensitivity=0.84, specificity=0.83), 100 ng/mL (72 hours, sensitivity=0.83, specificity=0.81), 86 ng/mL (96 hours, sensitivity=0.81, specificity=0.80), and 80 ng/mL (120 hours, sensitivity=0.81, specificity=0.78). Figure 1 displays the sensitivity and specificity of the EtG immunoassay cutoff levels from 100–500 ng/mL in 100 ng/mL increments across the 24 to 120 hour assessment periods. As Figure 1 demonstrates, the 100 ng/mL cutoff level had the highest sensitivity, relative to higher cutoff levels across all time periods ranging from 0.93 (24 hours) to 0.78 (120 hours). The 100 ng/mL cutoff level also had the lowest level of specificity across all time periods, relative to other cutoff levels. Across all time periods the 200 ng/mL cutoff level provided higher sensitivity than 300 ng/mL and higher cutoff levels, while providing improved specificity, relative to the 100 ng/mL. Cutoff levels above 200 ng/mL performed similarly across all assessment periods, with relatively low sensitivity and high specificity.
Fig. 1.
Sensitivity and specificity of multiple ethyl glucuronide immunoassay cutoff levels when detecting drinking during the previous 24–120 hours. For each time interval, N = 80.
Discussion
The current study builds upon the growing literature suggesting that relatively low EtG cutoff levels are needed to detect alcohol use for more than 24 hours (Hegstad et al., 2013, Stewart et al., 2013, Dahl et al., 2011, Jatlow et al., 2014). Results of this study suggest that the 100 ng/mL cutoff level had the highest level of self-reported drinking detection, relative to higher cutoff levels throughout the 120 hour assessment period. The relatively lower specificity of the 100 ng/mL cutoff level (particularly during the 24 and 48 hour assessment periods) may be reflective of the limitations of assay specificity (Leickly et al., in press), or may be due to the fact that this low cutoff level may likely be detecting use that occurred beyond the 24–48 hour assessment period, rather than non-beverage alcohol use.
Consistent with previous literature (Wurst et al., 2004), cutoff levels of 300 ng/mL and higher appear to be suitable for detection of drinking during the first 24 hours after alcohol use. However, they appeared to be less effective at detecting drinking for more than 24 hours. Importantly, the 500 ng/mL cutoff level used by most commercial laboratories did not demonstrate a benefit in terms of specificity, relative to the 300 ng/mL or 400 ng/mL cutoff levels. The 200 ng/mL cutoff level offered specificity that is nearly comparable to higher cutoffs while offering increased sensitivity; therefore, it may be an ideal cutoff for those wishing to balance sensitivity and specificity when detecting drinking in clinical and research settings. This mirrors Jatlow and colleague’s (2014) recommendation that a cutoff of 200 ng/mL be used in clinical research.
There are several limitations to the present study. First, this study compares EtG immunoassay results to self-reported alcohol consumption data rather than data collected from an alcohol challenge or controlled drinking experiment. Self-reported alcohol use data has been shown to be vulnerable to inaccurate reporting, particularly under-reporting of alcohol use when drinking carries real or perceived negative consequences (Langenbucher and Merrill, 2001). More severe drinking problems, higher levels of pre-treatment drinking, and greater levels of cognitive impairment have all been shown to be correlated with less accurate self-report in clinical trials (Babor et al., 2000). It is possible that the under-reporting of alcohol use could have contributed to decreased specificity in this study.
During the 120-hour assessment period, 100 (6.3%) false positives were recorded at the 100 ng/mL cutoff level, 42 (2.6%) at the 200 ng/mL cutoff, 22 (1.4%) at the 300 ng/mL cutoff, 21 (1.3%) at the 400 ng/mL cutoff, and 18 (1.1%) at the 500 ng/mL cutoff. The data were collected in the context of a contingency management treatment study. When reinforcers were contingent on EtG negative results, 8% of the time participants submitted an EtG positive (>100 ng/mL) urine sample they denied drinking during the previous 120 hours. When reinforces were not-contingent on EtG test results, 5% of the time participants who submitted an EtG positive (100 ng/mL) urine sample denied drinking during the previous 120 hours. This was a small but statistically significant difference, chi square = (1) 4.5, p=0.033. Regardless of study condition, the levels of agreement between EtG-I and self-report in the present study are similar to agreement between urine tests of illicit drugs and self-report in previous research (Chermack et al., 2000, Decker et al., 2014, Hilario et al., 2014). Although self-report has limitations as a validity outcome, it nevertheless provides valuable information in terms of evaluating the accuracy of EtG, particularly in samples where alcohol challenge experiments might not be appropriate, such as those receiving alcohol treatment.
A second limitation is that participants in this study were suffering from co-occurring mental illness in addition to alcohol dependence. Therefore, results may not generalize to other alcohol-dependent populations. Third, regular dilution was not performed and EtG/creatinine ratios were not calculated to account for varying urine dilution. Recent research (Stewart et al., 2013, Jatlow et al., 2014) has shown these adjustments to be unnecessary, and tests were conducted in this manner to emulate the way in which they would be performed in an actual outpatient addiction clinic. Additionally, confirmatory testing of EtG immunoassay results by EtG-LC-MS/MS was conducted on a random selection of urine samples, rather than all EtG immunoassay positive samples. However, this was likely unnecessary as there appears to be a high level of agreement between EtG immunoassay and EtG-LC-MS/MS (Böttcher et al., 2008, Leickly et al., in press)
Despite these limitations, results of this study suggest that EtG immunoassay can be used to accurately assess recent alcohol use in a clinical setting. When used as a clinical research or treatment outcome measure, EtG immunoassay can be a relatively low-cost alternative to the more expensive EtG LC-MS/MS testing. The ability to conduct tests onsite at an outpatient addiction clinic and receive results rapidly using an easily operable analyzer adds to the utility of EtG immunoassay for researchers and clinicians interested in monitoring client alcohol consumption. Additionally, a point-of-care EtG immunoassay dipstick test was recently released (Premier Biotech). While the dipstick test utilizes a cutoff level of 500 ng/mL and little independent information is available about its accuracy, this technology further increases the feasibility of onsite EtG testing. Like all other alcohol and drug biomarkers, sensitivity declines with increasing time since alcohol consumption. Therefore, rates of detection are improved with shorter testing intervals, which advances in technology continue to make more feasible. In conclusion, study results suggest that a cutoff level of 200 ng/mL provides the best balance between sensitivity and specificity in detecting alcohol use within the past 24–120 hours. When used in conjunction with self-report, EtG is a valuable tool that is likely to improve the accuracy of alcohol use assessment in clinical research and addiction treatment settings.
Acknowledgments
This study was supported by the National Institutes of Health (R01AA020248-01 PI: MGM; 1K99DA037276-01 PI: RV).
References
- Albermann ME, Musshoff F, Doberentz E, Heese P, Banger M, Madea B. Preliminary investigations on ethyl glucuronide and ethyl sulfate cutoffs for detecting alcohol consumption on the basis of an ingestion experiment and on data from withdrawal treatment. Int J Legal Med. 2012;126:757–764. doi: 10.1007/s00414-012-0725-3. [DOI] [PubMed] [Google Scholar]
- Anton RF. Carbohydrate-deficient transferrin for detection and monitoring of sustained heavy drinking. What have we learned? Where do we go from here? Alcohol. 2001;25(3):185–8. doi: 10.1016/s0741-8329(01)00165-3. [DOI] [PubMed] [Google Scholar]
- Arndt T, Gierten B, Güssregen B, Werle A, Grüner J. False-positive ethyl glucuronide immunoassay screening associated with chloral hydrate medication as confirmed by LC-MS/MS and self-medication. Forensic Sci Int. 2009;184:e27–29. doi: 10.1016/j.forsciint.2008.10.022. [DOI] [PubMed] [Google Scholar]
- Babor TF, Steinberg K, Anton R, Del Boca F. Talk is cheap: measuring drinking outcomes in clinical trials. J Stud Alcohol Drugs. 2000;61:55–63. doi: 10.15288/jsa.2000.61.55. [DOI] [PubMed] [Google Scholar]
- Bertholet N, Winter MR, Cheng DM, Samet JH, Saitz R. How accurate are blood (or breath) tests for identifying self-reported heavy drinking among people with alcohol dependence? Alcohol Alcohol. 2014;49(4):423–9. doi: 10.1093/alcalc/agu016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Böttcher M, Beck O, Helander A. Evaluation of a new immunoassay for urinary ethyl glucuronide testing. Alcohol Alcohol (Oxford, Oxfordshire) 2008;43:46–48. doi: 10.1093/alcalc/agm153. [DOI] [PubMed] [Google Scholar]
- Chermack ST, Roll J, Reilly M, Davis L, Kilaru U, Grabowski J. Comparison of patient self-reports and urinalysis results obtained under naturalistic methadone treatment conditions. Drug and Alcohol Depend. 2000;59:43–49. doi: 10.1016/s0376-8716(99)00106-4. [DOI] [PubMed] [Google Scholar]
- Dahl H, Voltaire Carlsson A, Hillgren K, Helander A. Urinary ethyl glucuronide and ethyl sulfate testing for detection of recent drinking in an outpatient treatment program for alcohol and drug dependence. Alcohol Alcohol. 2011;46:278–282. doi: 10.1093/alcalc/agr009. [DOI] [PubMed] [Google Scholar]
- Decker SE, Frankforter T, Babuscio T, Nich C, Ball SA, Carroll KM. Assessment concordance and predictive validity of self-report and biological assay of cocaine use in treatment trials. Am J Addict. 2014;23:466–474. doi: 10.1111/j.1521-0391.2014.12132.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Del Boca FK, Noll JA. Truth or consequences: the validity of self-report data in health services research on addictions. Addiction. 2000;95:S347–360. doi: 10.1080/09652140020004278. [DOI] [PubMed] [Google Scholar]
- Donovan DM, Bigelow GE, Brigham GS, Carroll K, Cohen A, Gardin J, Hamilton J, Huestis M, Hughes J, Lindblad R, Marlatt AG, Preston KL, Selzer JA, Somoza EC, Wakim PG, Wells EA. Primary outcome indices in illicit drug dependence treatment research: systematic approach to selection and measurement of drug use end-points in clinical trials. Addiction. 2012;107:694–708. doi: 10.1111/j.1360-0443.2011.03473.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg DM. Structural, functional, and clinical aspects of gamma-glutamyltransferase. CRC Crit Rev Clin Lab Sci. 1980;12:1–5. doi: 10.3109/10408368009108725. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou PS, Dufour MC, Compton W, Pickering RP, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Gurvich EM, Kenna GA, Leggio L. Use of novel technology-based techniques to improve alcohol-related outcomes in clinical trials. Alcohol Alcohol. 2013;48:712–719. doi: 10.1093/alcalc/agt134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hegstad S, Helland A, Hagemann C, Michelson L, Spigset O. EtG/EtS in Urine from sexual assault victims determined by UPLC-MS-MS. J Anal Toxicol. 2013;37:227–232. doi: 10.1093/jat/bkt008. [DOI] [PubMed] [Google Scholar]
- Helander A, Beck O, Jones AW. Laboratory testing for recent alcohol consumption: comparison of ethanol, methanol, and 5-hydroxytryptophol. Clin Chem. 1996;42:618–624. [PubMed] [Google Scholar]
- Helander A, Beck O. Ethyl sulfate: A metabolite of ethanol in humans and a potential biomarker of acute alcohol intake. J Anal Toxicol. 2005;29:270–4. doi: 10.1093/jat/29.5.270. [DOI] [PubMed] [Google Scholar]
- Helander A, Olsson I, Dahl H. Postcollection synthesis of ethyl glucuronide by bacteria in urine may cause false identification of alcohol consumption. Clin Chem. 2007;53:1855–1857. doi: 10.1373/clinchem.2007.089482. [DOI] [PubMed] [Google Scholar]
- Helander A, Böttcher M, Fehr C, Dahmen N, Beck O. Detection times for urinary ethyl glucuronide and ethyl sulfate in heavy drinkers during alcohol detoxification. Alcohol Alcohol. 2009;44:55–61. doi: 10.1093/alcalc/agn084. [DOI] [PubMed] [Google Scholar]
- Helander A, Péter O, Zheng Y. Monitoring of the alcohol biomarkers PEth, CDT and EtG/EtS in an outpatient treatment setting. Alcohol Alcohol. 2012;47:552–557. doi: 10.1093/alcalc/ags065. [DOI] [PubMed] [Google Scholar]
- Hilario EY, Griffin ML, McHugh RK, McDermott KA, Connery HS, Fitzmaurice GM, Weiss RD. Denial of urinalysis-confirmed opioid use in prescription opioid dependence. J Subst Abuse Treat. 2014 doi: 10.1016/j.jsat.2014.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jatlow P, O’Malley SS. Clinical (nonforensic) application of ethyl glucuronide measurement: are we ready? Alcohol Clin Exp Res. 2010;34:968–975. doi: 10.1111/j.1530-0277.2010.01171.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jatlow PI, Agro A, Wu R, Nadim H, Toll BA, Ralevski E, Nogueira C, Shi J, Dziura JD, Petrakis IL, O’Malley SS. Ethyl Glucuronide and Ethyl Sulfate Assays in Clinical Trials, Interpretation, and Limitations: Results of a Dose Ranging Alcohol Challenge Study and 2 Clinical Trials. Alcohol Clin Exp Res. 2014 doi: 10.1111/acer.12407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langenbucher J, Merrill J. The validity of self-reported cost events by substance abusers. Limits, liabilities, and future directions. Review. 2001;25:184–210. doi: 10.1177/0193841X0102500204. [DOI] [PubMed] [Google Scholar]
- McDonell Michael G, Angelo F, Sugar A, Rainey C, Srebnik D, Roll J, Short R, Ries RK. A pilot study of the accuracy of onsite immunoassay urinalysis of illicit drug use in seriously mentally ill outpatients. Am J Drug Alcohol Abuse. 2011a;37:137–140. doi: 10.3109/00952990.2010.548015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musshoff F, Albermann E, Madea B. Ethyl glucuronide and ethyl sulfate in urine after consumption of various beverages and foods--misleading results? Int J Legal Med. 2010;124:623–630. doi: 10.1007/s00414-010-0511-z. [DOI] [PubMed] [Google Scholar]
- Ries RK, Dyck DG, Short R, Srebnik D, Snowden M, Comtois KA. Use of case manager ratings and weekly urine toxicology tests among outpatients with dual diagnoses. Psychiatr Serv. 2002;53:764–766. doi: 10.1176/appi.ps.53.6.764. [DOI] [PubMed] [Google Scholar]
- Rohrig TP, Huber C, Goodson L, Ross W. Detection of ethylglucuronide in urine following the application of Germ-X. J Anal Toxicol. 2006;30:703–704. doi: 10.1093/jat/30.9.703. [DOI] [PubMed] [Google Scholar]
- Rosalki SB. Gamma-glutamyl transpeptidase. Adv Clin Chem. 1975;17:53–107. doi: 10.1016/s0065-2423(08)60248-6. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Handbook of psychiatric measures. Washington DC: American Psychiatric Association; 2000. Alcohol timeline followback (TLFB) [Google Scholar]
- Stewart SH, Koch DG, Burgess DM, Willner IR, Reuben A. Sensitivity and specificity of urinary ethyl glucuronide and ethyl sulfate in liver disease patients. Alcohol Clin Exp Res. 2013;37:150–155. doi: 10.1111/j.1530-0277.2012.01855.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thierauf A, Halter CC, Rana S, Auwaerter V, Wohlfarth A, Wurst FM, Weinmann W. Urine tested positive for ethyl glucuronide after trace amounts of ethanol. Addiction. 2009;104:2007–2012. doi: 10.1111/j.1360-0443.2009.02722.x. [DOI] [PubMed] [Google Scholar]
- Thierauf A, Gnann H, Wohlfarth A, Auwärter V, Perdekamp MG, Buttler K, Wurst FM, Weinmann W. Urine tested positive for ethyl glucuronide and ethyl sulphate after the consumption of ‘non-alcoholic’ beer. Forensic Sci Int. 2010;202:82–85. doi: 10.1016/j.forsciint.2010.04.031. [DOI] [PubMed] [Google Scholar]
- Wurst FM, Wiesbeck GA, Metzger JW, Weinmann W. On sensitivity, specificity, and the influence of various parameters on ethyl glucuronide levels in urine--results from the WHO/ISBRA study. Alcohol Clin Exp Res. 2004;28:1220–1228. doi: 10.1097/01.alc.0000134230.21414.11. [DOI] [PubMed] [Google Scholar]
- Wurst FM, Dressen S, Allen JP, Wiesbeck G, Graf M, Weinmann W. Ethyl sulphate: A direct ethanol metabolite reflecting recent alcohol consumption. Addiction. 2006;101:204–211. doi: 10.1111/j.1360-0443.2005.01245.x. [DOI] [PubMed] [Google Scholar]
- Wurst FM, Dürsteler-MacFarland KM, Auwaerter V, Ergovic S, Thon N, Yegles M, Halter C, Weinmann W, Wiesbeck GA. Assessment of alcohol use among methadone maintenance patients by direct ethanol metabolites and self-reports. Alcohol Clin Exp Res. 2008;32:1552–1557. doi: 10.1111/j.1530-0277.2008.00724.x. [DOI] [PubMed] [Google Scholar]