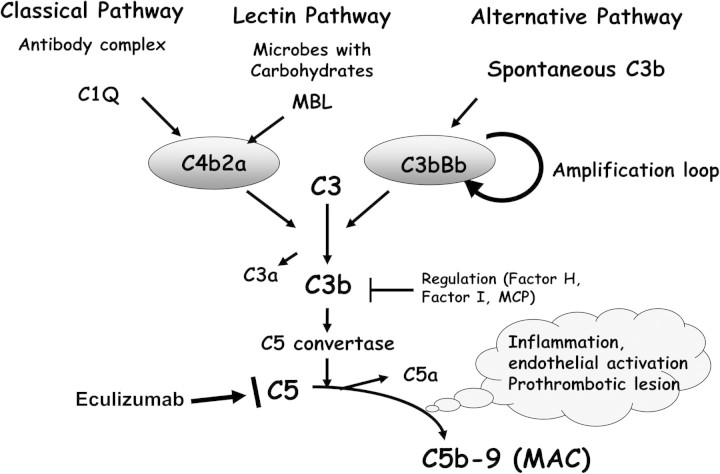
Atypical haemolytic–uraemic syndrome (aHUS) is characterized by endothelial damage leading to renal failure. aHUS has a proven genetic background [1]. To date, underlying genetic factors have been identified in complement components and complement regulators among ∼50% of aHUS patients [2, 3]. The disease-associated genes include C3 and factor B, which form the complement amplification convertase C3bBb and the regulators factor H (CFH, a plasma gycoprotein), membrane cofactor protein (CD46, MCP) and factor I (a plasma serine protease) which concur to controlling C3 convertase activity (Figure 1). In addition, autoantibodies recognizing factor H have been identified as being associated with haemolytic–uraemic syndrome (HUS) [4]. Over the last decade, a clear link has been demonstrated between this disorder and a defective regulation of the complement system components [5]. Thus, it is generally accepted that aHUS is a disease of excessive complement activation in the kidney glomerular and arteriolar cells. Following yet not well-identified triggering events, endothelial cells lose their integrity and become a target for an uncontrolled complement attack. The release of C5a and the inactive form—in terms of cytolytic effect—of the membrane attack complex (MAC) C5b-9 induces a procoagulant phenotype. This deleterious triggering of the complement and the coagulation cascades leads to the development of the thrombotic microangiopathy (TMA) that characterizes aHUS [6].
Fig. 1.
The complement system is a major innate immune defence mechanism. Complement may be activated by the classical, lectin or alternative pathways, all leading to the cleavage of the inactive central component C3 to biologically active C3b. C3b binds covalently to any surface, either foreign or self. When C3b is bound to positively charged surfaces (called alternative pathway activator surfaces as present in microorganisms) C3b interacts with factor B (FB) to form the C3 convertase (C3bBb) of the alternative pathway amplification loop and may generate a C5 convertase leading to the release of C5a, which is also an anaphylatoxin, and C5b which initiates the formation of the membrane attack complex (MAC), by binding C6 and C7. The C5b67 inserts into the membrane where it binds C8 and many molecules of C9, forming a pore. It can be cytolytic, forming a transmembrane channel, which causes osmotic lysis of the target cell or sublytic, associated with cell activation. In order to avoid complement hyperactivation, the alternative pathway C3 convertase is tightly regulated.
aHUS is a severe and frequently relapsing disorder comprising a typical triad of thrombocytopaenia, haemolysis and acute renal failure, in the absence of Shiga toxin-producing Escherichia coli infection, and detectable ADAMST13 in the serum. It portends a dismal prognosis. More than 50% of patients with aHUS progress to chronic renal failure and 10% die from complications of the disease. The disease can affect patients of all ages and its prognosis correlates to a certain extent with the identified genetic defects. Patients with CFH mutations carry the worst prognosis [7]. At the end of the first year following the onset of aHUS, 60% of patients with CFH mutations die or progress to dialysis dependency. In addition, when renal transplantation is undertaken, loss of the graft occurs in over 50% of renal transplants, due to HUS recurrence [8]. Despite the fact that plasma exchanges are the treatment of choice in severe thrombotic thrombocytopaenic purpura [9], their efficacy in aHUS is not guaranteed. Therefore, other therapeutic procedures, in particular complement-blocking agents, may be of benefit, and considering the severity of this condition are fully justified. As the activation of C5 plays a pivotal role in the pathophysiology of aHUS, the newly elaborated complement antagonist eculizumab represents a reasonable hope as a promising treatment for the disease [10].
Eculizumab (Soliris; Alexion) is a humanized monoclonal antibody indicated for the treatment of paroxysmal nocturnal haemoglobinuria [11]. It binds specifically and with high affinity to the complement protein C5, thereby preventing the release of the anaphylatoxin C5a and the assembly of the terminal complement complex C5b-9. To this day, >50 cases of patients who received eculizumab for aHUS have been published or included in an international multicentre prospective Phase II trial [8, 12–24, 25]. Eculizumab was used in patients who had experienced aHUS in their native kidney, in order to rescue or prevent post-transplant recurrence. There are still few reports indicating that the C5 mAb antagonist eculizumab may be an effective form of treatment for aHUS. The results of clinical trials have now confirmed that the drug arrests the TMA process and improves renal function or stabilizes its decline [26, 27]. Kim et al. [28] and Garjou et al. [29], in two articles that appear in this issue of the Clinical Kidney Journal, describe the outcome of aHUS in two additional cases of patients who received eculizumab for this syndrome occurring in their native kidneys. In both cases, a mutation in complement genes was identified and intensive plasmaphaereses were of no avail to abate the HUS. Plasma exchanges were inefficient to arrest the haematological and renal symptoms in a little girl with CFH mutation who presented with the disease at the age of 7 months. It comes as no surprise that plasma exchanges were not beneficial in the patient with MCP mutation. MCP is classically associated with a childhood onset, a spontaneous abortion of the TMA and recurrent episodes. Interestingly, this observation highlights the poor outcome of patients with an MCP mutation who presented with an onset of the disease at adult age. After failure of plasma exchanges, eculizumab induced an increase in platelet counts and haemolysis was stopped. The patient with MCP mutation who was treated later than 3 months after the onset did not recover his kidney function. Conversely, in the paediatric case with CFH mutation, eculizumab was started 4 months after the onset. In this patient, a slow improvement in the kidney function was observed after a period of peritoneal dialysis. Duran et al. [30], in this issue of the Clinical Kidney Journal, report a significant recovery of renal function in a patient with a CFH mutation who received eculizumab 3 months after being started on dialysis following recurrence of HUS after kidney transplantation.
By blocking the terminal pathway of the complement cascade, eculizumab entails an increased risk of Neisseria meningitides infection. As recommended, the patients were vaccinated before they were commenced on eculizumab. In these cases, the tolerability was good. It appears that eculizumab, the first targeted terminal complement inhibitor, is able to provide an effective and generally well-tolerated treatment for patients suffering from aHUS. Eculizumab should therefore be considered for treating all patients with childhood or adult onset of atypical HUS. Unfortunately, renal function recovery cannot be expected when irreversible histologic injury to the kidney has already been established before the treatment is undertaken. In other cases, this new targeted monoclonal antibody represents a real hope as a promising treatment to rescue the kidney function following the onset of TMA.
Acknowledgments
Conflict of interest statement. V.F.B. acts as a scientific advisor for Alexion.
(See related articles by: Duran et al. Rescue therapy with eculizumab in a transplant recipient with atypical haemolytic-uraemic syndrome. Clin Kidney J 2012; 5: 28–30; Garjau et al. Early treatment with eculizumab in atypical haemolytic uraemic syndrome. Clin Kidney J 2012; 5: 31–33; and Kim et al. Eculizumab in atypical haemolytic uraemic syndrome allows cessation of plasma exchange and dialysis. Clin Kidney J 2012; 5: 34–36.)
References
- 1.Loirat C, Fremeaux-Bacchi V. Atypical hemolytic uremic syndrome. Orphanet J Rare Dis. 2011;6:60. doi: 10.1186/1750-1172-6-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sellier-Leclerc AL, Fremeaux-Bacchi V, Dragon-Durey MA, et al. Differential impact of complement mutations on clinical characteristics in atypical hemolytic uremic syndrome. J Am Soc Nephrol. 2007;18:2392–2400. doi: 10.1681/ASN.2006080811. [DOI] [PubMed] [Google Scholar]
- 3.Noris M, Caprioli J, Bresin E, et al. Relative role of genetic complement abnormalities in sporadic and familial aHUS and their impact on clinical phenotype. Clin J Am Soc Nephrol. 2010;5:1844–1859. doi: 10.2215/CJN.02210310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dragon-Durey MA, Sethi SK, Bagga A, et al. Clinical features of anti-factor H autoantibody-associated hemolytic uremic syndrome. J Am Soc Nephrol. 2011;21:2180–2187. doi: 10.1681/ASN.2010030315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Noris M, Remuzzi G. Atypical hemolytic-uremic syndrome. N Engl J Med. 2009;361:1676–1687. doi: 10.1056/NEJMra0902814. [DOI] [PubMed] [Google Scholar]
- 6.de Jorge EG, Macor P, Paixao-Cavalcante D, et al. The development of atypical hemolytic uremic syndrome depends on complement C5. J Am Soc Nephrol. 2011;22:137–145. doi: 10.1681/ASN.2010050451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Le Quintrec M, Roumenina L, Noris M, et al. Atypical hemolytic uremic syndrome associated with mutations in complement regulator genes. Semin Thromb Hemost. 2010;36:641–652. doi: 10.1055/s-0030-1262886. [DOI] [PubMed] [Google Scholar]
- 8.Zuber J, Le Quintrec M, Sberro-Soussan R, et al. New insights into postrenal transplant hemolytic uremic syndrome. Nat Rev Nephrol. 2010;7:23–35. doi: 10.1038/nrneph.2010.155. [DOI] [PubMed] [Google Scholar]
- 9.Hovinga JA, Vesely SK, Terrell DR, et al. Survival and relapse in patients with thrombotic thrombocytopenic purpura. Blood. 2009;115:1500–1511. doi: 10.1182/blood-2009-09-243790. quiz 1662. [DOI] [PubMed] [Google Scholar]
- 10.Salant DJ. Targeting complement C5 in atypical hemolytic uremic syndrome. J Am Soc Nephrol. 2011;22:7–9. doi: 10.1681/ASN.2010111145. [DOI] [PubMed] [Google Scholar]
- 11.Rother RP, Rollins SA, Mojcik CF, et al. Discovery and development of the complement inhibitor eculizumab for the treatment of paroxysmal nocturnal hemoglobinuria. Nat Biotechnol. 2007;25:1256–1264. doi: 10.1038/nbt1344. [DOI] [PubMed] [Google Scholar]
- 12.Al-Akash SI, Almond PS, Savell VH, Jr, et al. Eculizumab induces long-term remission in recurrent post-transplant HUS associated with C3 gene mutation. Pediatr Nephrol. 2011;26:613–619. doi: 10.1007/s00467-010-1708-6. [DOI] [PubMed] [Google Scholar]
- 13.Chatelet V, Fremeaux-Bacchi V, Lobbedez T, et al. Safety and long-term efficacy of eculizumab in a renal transplant patient with recurrent atypical hemolytic-uremic syndrome. Am J Transplant. 2009;9:2644–2645. doi: 10.1111/j.1600-6143.2009.02817.x. [DOI] [PubMed] [Google Scholar]
- 14.Davin JC, Gracchi V, Bouts A, et al. Maintenance of kidney function following treatment with eculizumab and discontinuation of plasma exchange after a third kidney transplant for atypical hemolytic uremic syndrome associated with a CFH mutation. Am J Kidney Dis. 2010;55:708–711. doi: 10.1053/j.ajkd.2009.08.011. [DOI] [PubMed] [Google Scholar]
- 15.Gruppo RA, Rother RP. Eculizumab for congenital atypical hemolytic-uremic syndrome. N Engl J Med. 2009;360:544–546. doi: 10.1056/NEJMc0809959. [DOI] [PubMed] [Google Scholar]
- 16.Kose O, Zimmerhackl LB, Jungraithmayr T, et al. New treatment options for atypical hemolytic uremic syndrome with the complement inhibitor eculizumab. Semin Thromb Hemost. 2010;36:669–672. doi: 10.1055/s-0030-1262889. [DOI] [PubMed] [Google Scholar]
- 17.Lapeyraque AL, Fremeaux-Bacchi V, Robitaille P. Efficacy of eculizumab in a patient with factor-H-associated atypical hemolytic uremic syndrome. Pediatr Nephrol. 2011;26:621–624. doi: 10.1007/s00467-010-1719-3. [DOI] [PubMed] [Google Scholar]
- 18.Mache CJ, Acham-Roschitz B, Fremeaux-Bacchi V, et al. Complement inhibitor eculizumab in atypical hemolytic uremic syndrome. Clin J Am Soc Nephrol. 2009;4:1312–1316. doi: 10.2215/CJN.01090209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nester C, Stewart Z, Myers D, et al. Pre-emptive eculizumab and plasmapheresis for renal transplant in atypical hemolytic uremic syndrome. Clin J Am Soc Nephrol. 2011;6:1488–1494. doi: 10.2215/CJN.10181110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nurnberger J, Witzke O, Saez AO, et al. Eculizumab for atypical hemolytic-uremic syndrome. N Engl J Med. 2009;360:542–544. doi: 10.1056/NEJMc0808527. [DOI] [PubMed] [Google Scholar]
- 21.Prescott HC, Wu HM, Cataland SR, et al. Eculizumab therapy in an adult with plasma exchange-refractory atypical hemolytic uremic syndrome. Am J Hematol. 2010;85:976–977. doi: 10.1002/ajh.21862. [DOI] [PubMed] [Google Scholar]
- 22.Tschumi S, Gugger M, Bucher BS, et al. Eculizumab in atypical hemolytic uremic syndrome: long-term clinical course and histological findings. Pediatr Nephrol. 2011;26:2085–2088. doi: 10.1007/s00467-011-1989-4. [DOI] [PubMed] [Google Scholar]
- 23.Weitz M, Amon O, Bassler D, et al. Prophylactic eculizumab prior to kidney transplantation for atypical hemolytic uremic syndrome. Pediatr Nephrol. 2011;26:1325–1329. doi: 10.1007/s00467-011-1879-9. [DOI] [PubMed] [Google Scholar]
- 24.Zimmerhackl LB, Hofer J, Cortina G, et al. Prophylactic eculizumab after renal transplantation in atypical hemolytic-uremic syndrome. N Engl J Med. 2010;362:1746–1748. doi: 10.1056/NEJMc1001060. [DOI] [PubMed] [Google Scholar]
- 25.Larrea CF, Cofan F, Oppenheimer F, et al. Efficacy of eculizumab in the treatment of recurrent atypical hemolytic-uremic syndrome after renal transplantation. Transplantation. 2010;89:903–904. doi: 10.1097/TP.0b013e3181ccd80d. [DOI] [PubMed] [Google Scholar]
- 26.Legendre C, Babu S, Furman R, et al. Safety and Efficacy of Eculizumab in aHUS Patients Resistant to Plasma Therapy: Interim Analysis from a Phase 2 Trial. Abstract presented at the 43rd annual meeting of the American Society of Nephrology, Denver, CO, USA, 16–21 November 2010. [Google Scholar]
- 27.Muus P, Legendre C, Douglas K, et al. Safety and Efficacy of Eculizumab in aHUS Patients on Chronic Plasma Therapy: Interim Analysis of a Phase 2 Trial. Abstract presented at the 43rd annual meeting of the American Society of Nephrology, Denver, CO, USA, 16–21 November 2010. [Google Scholar]
- 28.Kim JJ, Waller SC, Reid CJ. Eculizumab in atypical haemolytic uraemic syndrome allows cessation of plasma exchange and dialysis. Clin Kidney J. 2012;5:34–36. doi: 10.1093/ndtplus/sfr174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Garjau M, Azancot M, Ramos R, et al. Early treatment with eculizumab may be beneficial in atypical haemolytic uraemic syndrome. Clin Kidney J. 2012;5:31–33. doi: 10.1093/ndtplus/sfr157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Durán CE, Maduell FM, Campistol JM. Rescue therapy with eculizumab in a transplant recipient with atypical haemolytic uraemic syndrome. Clin Kidney J. 2012;5:28–30. doi: 10.1093/ndtplus/sfr107. [DOI] [PMC free article] [PubMed] [Google Scholar]