Abstract
Background
There are two main methods of accessing arterio-venous fistulas (AVFs); the ‘buttonhole’ and the ‘rope-ladder’ cannulation technique. Several small studies have hypothesized that the buttonhole technique is associated with increased rates of fistula-associated infection. This study addresses this hypothesis.
Methods
A retrospective review of all patients attending a large outpatient haemodialysis clinic was performed. Data were collected on the method of cannulation, infection rates, implicated microorganisms, complications of infection and time on haemodialysis.
Results
A total of 127 patients had received haemodialysis via an AVF: 53 via the rope-ladder technique and 74 via the buttonhole technique. Nine episodes of clinically significant bacteraemia were recorded in the buttonhole group. This equated to a rate of 0.073 bacteraemia events per 1000 AVF days. There were no episodes of bacteraemia in the rope-ladder group. Eight infections were due to methicillin-sensitive Staphylococcus aureus (MSSA); one was due to Staphylococcus epidermidis. Three patients with MSSA bacteraemia subsequently developed infective endocarditis. Five patients who developed bacteraemia events had been undergoing home haemodialysis.
Conclusions
This study highlights the infectious complications associated with buttonhole cannulation techniques. All organisms isolated in our cohort were known skin colonizers. The reason for the increased rates of infection is unclear. Given this high rate of often life-threatening infection, we recommend regular audit of infection rates. We currently do not recommend this technique to our patients receiving haemodialysis.
Keywords: AVF buttonhole technique, haemodialysis, infectious complications
Introduction
Arterio-venous fistulae (AVF) have been the preferred vascular access for patients on haemodialysis since their development in 1966 [1]. The advantages of this access modality include lower risk of infection, fewer rates of hospitalization [2], longer patency rates and lower overall cost [3] when compared with arterio-venous grafts or central venous catheters.
There are two main methods of accessing an AVF: the ‘rope-ladder’ cannulation technique [4] and the ‘buttonhole’ cannulation technique [5].
The ‘rope-ladder’ technique has been in use since the introduction of AVF and involves cannulation of different sites along the entire length of the AVF. This technique involves rotation of the arterial and venous puncture site at each dialysis session with sharp cannulation needles. Repeated cannulation over the same general area is avoided as this could lead to aneurysm formation and stenosis.
The ‘buttonhole’ technique has been in use for the past 25 years, and involves the insertion of AVF needles at the same site at each dialysis session. This is also known as ‘constant site’ cannulation. AVFs that are cannulated in this manner form ‘tunnels’ or ‘tracks’ between the skin and the vessel lumen over time. This allows patients or nurses to use blunt needles to access the fistula. This cannulation technique has perceived advantages including better cosmetic outcomes with fewer aneurysmal complications, less pain, and better haemostasis after dialysis. There are few studies, however, directly comparing these two techniques [6, 7].
Strict hand hygiene and disinfection are thought to be particularly important with the buttonhole technique because the same site is repeatedly used and because removal of an overlying eschar is required. Despite these measures, the recent literature has suggested an increased incidence of infectious complications with the buttonhole technique [8, 9, 10].
We compared the infectious complications of the rope-ladder method of AVF cannulation with the buttonhole method of AVF cannulation.
Materials and methods
A retrospective cohort study of all patients undergoing haemodialysis via an AVF from May 2004 to May 2011 was carried out. These patients either dialysed in an outpatient unit attached to the hospital or were on our hospital's home haemodialysis programme. All patients who underwent haemodialysis three or more times per week for at least 3 hours per session were included. Each patient received standard haemodialysis therapy as per institutional protocol [11].
Since 2004, all patients on haemodialysis have been offered the option of having their AVF cannulated via the rope ladder or the buttonhole method. Patients received education on both the techniques from information leaflets, the practice support nurse and the medical staff. After full informed consent, they chose one of these modalities.
Prior to the introduction of the buttonhole technique, dialysis-nursing staff received specialist training in its use. This involved education on disinfection, scab removal and use of blunt needles. Education regarding the creation of a buttonhole track and its subsequent cannulation was also provided.
All patients who were commenced on home haemodialysis received 5 to 6 weeks of training. This involved 15 directly observed, but self-administered haemodialysis sessions in the hospital haemodialysis unit and 3 directly observed, self-administered haemodialysis sessions at home. This training included intensive education on hand hygiene, cannulation technique and aseptic protocols. These patients were not routinely audited thereafter to assess home haemodialysis techniques, including hygiene practices.
Blood cultures were obtained in all patients who had a temperature >38°C or were deemed to be clinically unwell. AVF cannulation site exudates were routinely cultured if thought to be clinically significant. C-reactive protein was not routinely measured.
AVF infection was suspected if there was an overlying cellulitis or if there was an overlying suppurative exudate. Any patient with suspected AVF infection was empirically commenced on vancomycin intravenously 1 g until further microbiology data became available. If methicillin-sensitive Staphylococcus aureus (MSSA) was isolated, patients were changed to flucloxacillin 1–2 g four times per day; patients who grew methicillin-resistant S. aureus (MRSA) were continued on vancomycin. All patients diagnosed with S. aureus bacteraemia underwent transoesophageal echocardiography to assess their cardiac valves for endocarditis.
Data recorded included patient's age, sex, presence of diabetes mellitus, time on haemodialysis and number of AVF days. The primary end-point of our study was AVF-associated infection, as defined by a positive blood culture yielding typical pathogens with cellulitis overlying the AVF. For the purposes of this study, a localized suppurative exudate was not classified as an AVF infection in the absence of positive blood cultures.
Isolated microorganisms, method of cannulation and complications of infection were subsequently recorded in those who had an AVF infection. We defined AVF infections per 1000 AVF patient days as per Centers for Disease Control protocols [12]. The modified Duke criteria were used to diagnose endocarditis [13].
Buttonhole technique
Patients arriving for haemodialysis underwent standard hand washing with soap and a sterile dressing trolley was prepared using a combination of sodium dichloroisocyanurate disinfectant tablets and a surfactant-based detergent dissolved in water. The fistula area was then cleaned with alcohol-based chlorhexidine cleaning wipes. The areas overlying any eschar or scabs were then soaked with normal saline and the scabs were removed using sterile forceps. The area was fully cleaned again with alcohol-based chlorhexidine. Cannulation then occurred with blunt 15G needles along the site of previous tracks. If the needle did not pass easily into the fistula, it was removed and a further attempt at cannulation was performed.
Rope-ladder technique
Patients arriving for haemodialysis underwent standard hand washing with soap and a sterile dressing trolley was prepared using a combination of sodium dichloroisocyanurate disinfectant tablets and a surfactant-based detergent dissolved in water. The entire fistula was then cleaned with alcohol-based chlorhexidine wipes. Cannulation then occurred at rotating areas along the length of the fistula with 15G sharp fistula needles.
Baseline characteristics between the two groups were compared using univariate analysis. Infection rates between the groups were compared using the Wilcoxon rank sum test, and Kaplan–Meier survival curves were produced to highlight significant differences. Multivariate analyses using the Cox proportional hazards model were used to adjust for potential confounding factors including age, sex, time on haemodialysis and presence of diabetes mellitus.
Results
One hundred and twenty-seven patients were included in the study, 53 patients used the rope-ladder technique while 74 used the buttonhole technique (Table 1).
Table 1.
Baseline patient characteristics
| Technique | Rope-ladder | Buttonhole | P value |
|---|---|---|---|
| Number | 53 | 74 | n/a |
| AVF days | 73 139 | 123 464 | |
| Median Age (years) | 68 (55–77) | 50 (38–69) | 0.0002 |
| Caucasian ethnicity | 100% | 100% | |
| Sex (M) | 29 (55%) | 58 (78%) | 0.007 |
| Median time on haemodialysis (years) | 2.6 (1.1–6.5) | 3.2 (1.5–5.5) | 0.27 |
| Diabetes mellitus (%) | 18% | 9% | 0.185 |
| Dialysis duration/session (minutes) | 202 | 217 | 0.0005 |
| Home haemodialysis patients (number) | 0 | 11 | |
| Receiving immunosuppressive therapy | 0% | 0% |
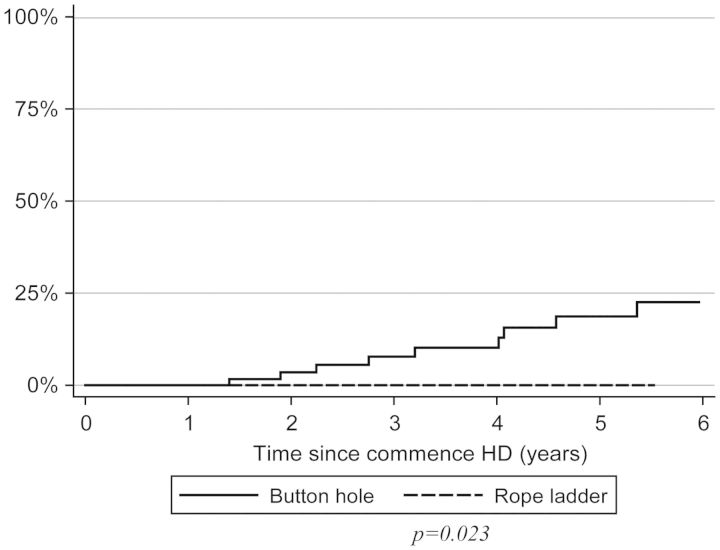
Patients in the buttonhole group were more likely to be younger, and were more likely to be male. There were no differences in home haemodialysis uptake between the sexes. Patients in the buttonhole group had an average longer dialysis duration per session. There were similar numbers of patients with diabetes mellitus in both the groups. There were nine episodes of AVF infection in the buttonhole group, which equates to 0.073 events per 1000 AVF days. There were no AVF infections in the rope-ladder group. This difference was statistically significant, P = 0.023 (Figure 1).
Fig. 1.
Survival curve showing time to AVF infection in both groups P = 0.023.
Of the patients who developed infectious events, six were aged <60 years old, and two of these patients had been on haemodialysis for <2 years.
The most prevalent pathogen was MSSA; this was isolated in eight patients. The other patient developed Staphylococcus epidermidis infection. There were no MRSA-related infections. Four of the eight patients who developed MSSA-associated fistula infections also developed infective endocarditis (Table 2). This corresponds to a rate of 0.02 events of infective endocarditis per 1000 AVF days.
Table 2.
Characteristics of patients who developed AVF-associated infection
| Patient | Location of haemodialysis | Time on haemodialysisa | Age (years) | Diabetic (yes/no) | Infective endocarditis (yes/no) | Discitis (yes/no) |
|---|---|---|---|---|---|---|
| 1 | Hospital | 48 | 78 | No | No | No |
| 2 | Hospital | 33 | 81 | No | Yes | Yes |
| 3 | Home | 43 | 30 | No | No | No |
| 4 | Hospital | 84 | 46 | No | No | No |
| 5 | Hospital | 51 | 63 | No | No | No |
| 6 | Home | 20 | 33 | No | Yes | No |
| 7 | Home | 55 | 42 | Yes | Yes | No |
| 8 | Home | 8 | 43 | No | Yes | No |
| 9 | Hospital | 55 | 20 | No | No | No |
aMonths prior to AVF infection.
One patient with endocarditis died. One patient developed MSSA cervical discitis. This patient withdrew from haemodialysis and died.
Patients who underwent in-centre haemodialysis received standard hygiene procedures prior to treatment.
Five of the nine patients who developed AVF infections were undergoing home haemodialysis. This equates to a rate of 1.45 events per 1000 AVF days. All five patients developed MSSA fistula infections, and three of these developed infective endocarditis.
The presence of diabetes mellitus, visual impairment or immunosuppression was not a contributory factor to the development of infection. All patients were transitioned to the rope-ladder technique on review of this retrospective analysis.
Discussion
It is well accepted that the use of an AVF has significant advantages in terms of infection prevention when compared with all other haemodialysis modalities. The use of the buttonhole method of AVF cannulation has previously been thought to offer equivalent or superior outcomes to the rope-ladder technique. However, several small-scale studies have suggested an increase in infection rates in patients using the buttonhole method [14, 15, 16].
A recent observational study performed in Belgium noted higher rates of AVF infection in patients using the buttonhole method, and this rate was seen to decline after intensive staff education [9].
A similar Canadian study reports higher rates of S. aureus bacteraemia events related to AVF infection in home nocturnal haemodialysis patients using the buttonhole technique. This study also highlighted the potential benefit of Mupirocin prophylaxis in reducing infection rates [17].
Our study highlights a significantly increased rate of AVF infections in the buttonhole group. This study also highlights the potentially life-threatening complication of infective endocarditis associated with AVF infection. It is important to note that all nursing staff and patients using the buttonhole technique received full education on its use, and were also directly observed performing the technique prior to being certified as competent in the procedure. A support nurse also provided training and supervision.
The reason for increased infection rates has been explored in the studies mentioned previously, and in a large observational cohort study performed in Australia [18]. We support the evolving theory that specific features of the buttonhole technique lead to increased infection rates. As these patients cannulated the same site at each session, the cannulation site becomes similar to a chronic ulcer. Despite disinfection methods, it is possible that the overlying skin colonizers remain present at the time of cannulation. This would therefore lead to increased infectious events.
Patient and staff compliance with the buttonhole technique is also hypothesized as being a cause of increased infection rates. Patients who self-cannulated their AVF admitted to occasional lapses in hygiene techniques prior to cannulation. This can be particularly problematic in home haemodialysis patients, as they are largely unsupervised after their initial training.
Patients in our study who underwent home haemodialysis admitted to having some difficulties with the buttonhole technique. Full hygiene precautions were not always undertaken prior to each session. Patients often reported that they would not remove the buttonhole scab prior to dialysis. This had the potential to increase the infection rates.
Nursing staff who are not fully competent with the buttonhole technique could also increase the risk of infection by creating ‘false tracks’ while attempting cannulation. AVF needling was noted to be complicated in some of the patients in our study group. In certain situations, false tracks were created in the fistula, which had the potential to serve as a nidus for infection. Similarly, scab removal was noted to be difficult during some sessions.
Maintaining a core group of dialysis staff who are expert in this technique is essential. This becomes difficult in units where there are relatively high turnover of staff, false tracks can be created due to poor familiarity with the buttonhole technique and the patient's AVF.
Our study suggests that more intensive staff and patient education needs to be carried out before further buttonhole cannulation should be continued. Periodic re-education and re-assessment of staff and patients should also reduce complications associated with this technique.
Our study is limited by its retrospective, observational method. Ideally, a randomized controlled trial would compare infection rates between the two techniques. That said, an observational study measures ‘real life’ experience as opposed to the somewhat artificial scenario of the randomized controlled trial. Our study adds to the growing literature that the use of the buttonhole technique is associated with more infections. This is particularly relevant given the rates of infective endocarditis noted in our group of patients. It emphasizes that staff and patients using this technique require intensive (and probably) repeated training and that regular audit of infection rates with this technique is needed.
All haemodialysis patients were transitioned to the rope-ladder technique on review of this retrospective analysis. Given the high rates of potentially life-threatening infections associated with the buttonhole technique, we currently do not recommend this technique to our patients undergoing haemodialysis.
Conflict of interest statement
None declared.
References
- 1.Brescia MJ, Cimino JE, Appell K, et al. Chronic haemodialysis using venepuncture and surgically recreated arteriovenous fistula. N Engl J Med. 1966;275:1089–1092. doi: 10.1056/NEJM196611172752002. doi:10.1056/NEJM196611172752002. [DOI] [PubMed] [Google Scholar]
- 2.Dhingra RK, Young EW, Hulbert Shearon TE, et al. Type of vascular access and mortality in US haemodialysis patients. Kidney Int. 2002;13:2117–2124. doi: 10.1046/j.1523-1755.2001.00947.x. [DOI] [PubMed] [Google Scholar]
- 3.Dixon BS, Novak L, Fangman J. Hemodialysis vascular access survival: upper arm native arterio venous fistula. Am J Kidney Dis. 2002;39:92. doi: 10.1053/ajkd.2002.29886. doi:10.1053/ajkd.2002.29886. [DOI] [PubMed] [Google Scholar]
- 4.Twardowski Z, Kubara H. Different site vs constant sites of needle insertion into arterio venous fistulae for treatment by repeated dialysis. Dial Transplant. 1979;8:978–980. [Google Scholar]
- 5.Twardowski Z. The ‘buttonhole’ method of needle insertion takes center stage in the attempt to revive home haemodialysis. Contemp Dial Nephrol. 1977;18:18–19. [Google Scholar]
- 6.Verhallen AM, Koistra MP, van Jaarsveld BC. Cannulating in haemodialysis: rope ladder or buttonhole technique? Nephrol Dial Transplant. 2007;22:2601–2604. doi: 10.1093/ndt/gfm043. doi:10.1093/ndt/gfm043. [DOI] [PubMed] [Google Scholar]
- 7.Van Loon MM, Goovaerts T, Kessels AG, et al. Buttonhole needling of haemodialysis arteriovenous fistulae results in less complications and interventions compared to the rope-ladder technique. Nephrol Dial Transplant. 2010;25:225–230. doi: 10.1093/ndt/gfp420. doi:10.1093/ndt/gfp420. [DOI] [PubMed] [Google Scholar]
- 8.Doss S, Schiller B, Moran J. Buttonhole cannulation––an unexpected outcome. Nephrol Nurs J. 2008;35:417–419. [PubMed] [Google Scholar]
- 9.Ludlow V. Buttonhole cannulation in haemodialysis: improved outcomes and increased expense––is it worth it? CANNT J. 2010;20:29–37. [PubMed] [Google Scholar]
- 10.Labriola L, Crott R, Desmet C, et al. Infectious complications following conversion to buttonhole cannulation of native arteriovenous fistulas: a quality improvement report. Am J Kidney Dis. 2011;57:442–448. doi: 10.1053/j.ajkd.2010.10.045. doi:10.1053/j.ajkd.2010.10.045. [DOI] [PubMed] [Google Scholar]
- 11.Khilji S, Denton MD, Magee CC, et al. Guidelines for haemodialysis. Dublin: Beaumont Hospital; 2009. [Google Scholar]
- 12.Center for Disease Control and Prevention. Device associated module; Dialysis events. Bethesda MD; http://www.cdc.gov/nhsn/PDFs/pscManual/6.4/8-Dialysis_Event_06_11.pdf . [Google Scholar]
- 13.Li JS, Sexton DJ, Mick N, et al. Proposed modifications to the Duke criteria for the diagnosis of inective endocarditis. Clin Infect Dis. 2000;30:633. doi: 10.1086/313753. doi:10.1086/313753. [DOI] [PubMed] [Google Scholar]
- 14.Chow J, Rayment G, San Miguel S, et al. A randomised controlled trial of buttonhole cannulation for the prevention of fistula access complications. J Renal Care. 2011;37:85–89. doi: 10.1111/j.1755-6686.2011.00211.x. doi:10.1111/j.1755-6686.2011.00211.x. [DOI] [PubMed] [Google Scholar]
- 15.Birchenough E, Moore C, Stevens K, et al. Buttonhole cannulation in adult patients on haemodialysis: an increased risk of infection. Nephrol Nurs J. 2010;37:491–498. [PubMed] [Google Scholar]
- 16.Gray N. The risk of sepsis from buttonhole needling must be appreciated. Nephrol Dial Transplant. 2010;25:2385–2386. doi: 10.1093/ndt/gfq255. doi:10.1093/ndt/gfq255. [DOI] [PubMed] [Google Scholar]
- 17.Nesrallah GE, Cuerdon M, Wong JH, et al. Staphylococcus aureus bacteraemia and buttonhole cannulation: Long term safety and efficacy of Mupirocin prophylaxis. Clin J Am Soc. 2010;5:1047–1053. doi: 10.2215/CJN.00280110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Van Eps CL, Jones M, Ng T, et al. The impact of extended hours home haemodialysis and buttonhole cannulation technique on hospitalization rates for septic events related to dialysis access. Hemodial Int. 2010;14:451–463. doi: 10.1111/j.1542-4758.2010.00463.x. doi:10.1111/j.1542-4758.2010.00463.x. [DOI] [PubMed] [Google Scholar]