Abstract
The formation of a bezoar is a relatively infrequent disorder that affects the gastrointestinal system. Bezoars are mainly classified into four types depending on the material constituting the indigestible mass of the bezoar: phytobezoars, trichobezoars, pharmacobezoars, and lactobezoars. Gastric bezoars often cause ulcerative lesions in the stomach and subsequent bleeding, whereas small intestinal bezoars present with small bowel obstruction and ileus. A number of articles have emphasized the usefulness of Coca-Cola® administration for the dissolution of phytobezoars. However, persimmon phytobezoars may be resistant to such dissolution treatment because of their harder consistency compared to other types of phytobezoars. Better understanding of the etiology and epidemiology of each type of bezoar will facilitate prompt diagnosis and management. Here we provide an overview of the prevalence, classification, predisposing factors, and manifestations of bezoars. Diagnosis and management strategies are also discussed, reviewing mainly our own case series. Recent progress in basic research regarding persimmon phytobezoars is also briefly reviewed.
Keywords: Bezoars, Gastrointestinal endoscopy, Persimmon phytobezoar, Trichobezoar, Endoscopic removal, Gastric ulcer, Ileus
Core tip: Among the gastrointestinal bezoars, phytobezoars, which consist of indigestible plant materials, are the most common. An administration of Coca-Cola® is believed to be the primary choice for phytobezoar treatment because it is safe, inexpensive, and effective. However, persimmon phytobezoars (diospyrobezoars) are often resistant to Coca-Cola® dissolution and may require different treatment. Endoscopic fragmentation or surgical removal should be applied in urgent cases, such as those manifesting gastrointestinal bleeding and/or ileus, and in patients with refractory bezoars.
INTRODUCTION
A bezoar is an indigestible conglomeration trapped in the gastrointestinal tract. This indigestible mass can be formed by a variety of materials that were intentionally or accidentally ingested. Representative substances forming bezoars include plant materials such as fibers, skins and seeds of vegetables and fruits (i.e., phytobezoars), ingested hair (i.e., trichobezoars), medications (i.e., pharmacobezoars), and milk protein in milk-fed infants (i.e., lactobezoars)[1]. Bezoars can be formed and found in any part of the gastrointestinal tract, but the stomach is the most common. Once the diagnosis of bezoar is made, the bezoar is generally dissolved or removed because it can cause gastric outlet obstruction, ileus, ulcerations due to pressure necrosis, and subsequent gastrointestinal bleeding. Here we review relevant clinical studies, case reports and basic research findings, using mainly our recent studies[2-4], for a better understanding of the etiology and epidemiology of this disease entity.
PREVALENCE
Bezoars of the gastrointestinal tract are a relatively rare disease entity, with a variable incidence among studies[5]. In 1978, Kadian et al[6] reported that they found six cases of gastric bezoars in a four-year period during which time 1400 gastroscopies were done (0.43% of the gastroscopies). In 1987, Ahn et al[7] reported a similar incidence of 0.43% (14/3247 esophagogastroduodenoscopy examinations) over a seven-year period. More recently, Mihai et al[8] noted that there were 49 cases of gastric bezoars over a period of 20 years (0.068% of all endoscopies).
Although the majority of bezoars are found in the stomach, bezoars sometimes move from the stomach into the small intestine, or they can be primarily formed in the small intestine. Such small intestinal bezoars occasionally cause small bowel obstruction and ileus. Yakan et al[9] reviewed 432 cases of small bowel obstruction treated within 10 years; of these, 14 (3.2%) cases were caused by phytobezoars. In a meta-analysis by Ghosheh et al[10] reviewing 19 reported studies published from 1994 to 2005, laparoscopy was attempted in 1061 patients presenting with acute small bowel obstruction, and bezoars represented the 5th most common cause, accounting for 0.8%[11].
Overall, bezoars can be found in the stomach in less than 0.5% of individuals undergoing esophagogastroduodenoscopy examinations and in the small intestine in 0.4%-4.8% of all cases presenting with intestinal obstruction[9-13]. However, the prevalence of bezoars likely varies among ethnic groups and geographic locations, since the occurrence rate of phytobezoar, the most common type of bezoar, is mostly reflected by food cultures. For example, multiple cases of persimmon phytobezoar (diospyrobezoar) have been reported in regions where the residents frequently consume fresh persimmon fruits and dried persimmons, such as South Korea, Japan, Israel, Spain, Turkey, and Southeastern United States[3,14-19].
BEZOAR CLASSIFICATION
Phytobezoar
Among the four types of bezoars, phytobezoars are the most common[20]. Celery, pumpkins, grape skins, prunes, raisins and, in particular, persimmons are representative causatives of phytobezoars[14]. Some of these foods contain high amount of cellulose, hemicellulose, lignin, and tannins (leucoanthocyanins and catechins), and these nondigestible food materials are the main components of phytobezoars[1,21,22]. Persimmon phytobezoars, i.e., diospyrobezoars, are formed after a frequent consumption of persimmons (Figure 1). The skin of unripe persimmons contains high concentrations of the persimmon tannin. Upon reaction with stomach acid, persimmon tannin is believed to polymerize and form a conglomerate in which cellulose, hemicelluloses, and various proteins are accumulated[20,23]. For example, Holloway et al[21] investigated the plant fiber content in a gastric phytobezoar by using the acid and neutral detergent method. The gastric phytobezoar was composed of approx, 11% cellulose, 5% hemicellulose, and 2% lignin. In a thin-layer chromatography analysis, phytobezoar tissue contained only polymerized tannins, without tannin monomers. Maki et al[24] succeeded in generating an artificial mass in vitro that mimicked a phytobezoar by using persimmon skin pieces, hydrochloric acid, and high-molecular-weight organic polymers. In light of the basic research findings, we speculate that persimmon tannin plays a vital role in the formation of phytobezoars acting as cementing agents that hold undigestible plant fibers together. However, the precise mechanism of the emergence of a phytobezoar is still unknown.
Figure 1.
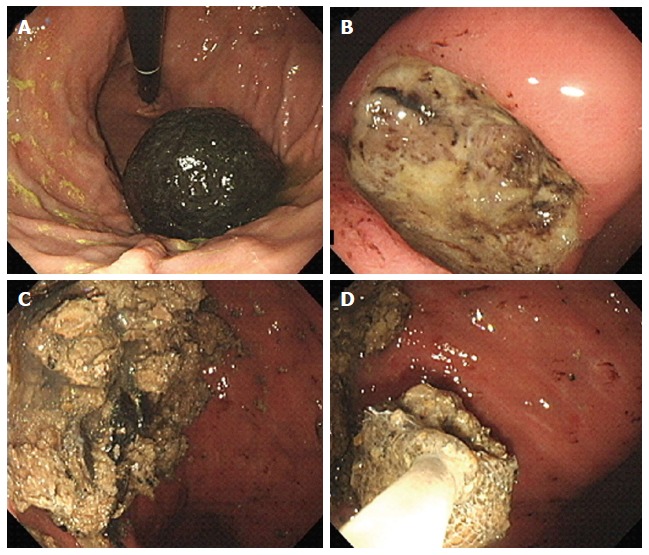
Endoscopic images of a persimmon phytobezoar. A: A large, black bezoar is seen in the gastric fundus; B: A peptic ulcer is also observed in the gastric angle; C: Fragmentation of the bezoar was performed by endoscopy forceps and polypectomy snares; D: The fragments were removed by a retrieval net device and used in the subsequent in vitro analysis.
Trichobezoar
A trichobezoar is a hair ball trapped in the gastrointestinal tract, mainly in the stomach. Trichobezoar is a rare condition, nearly always diagnosed in young females[25-30]. Psychiatric comorbidities that involve strong urges to pull out one’s own hair (trichotillomania) and eat it (trichophagia) are observed in these patients. Due to its enzyme-resistant properties and smooth, slippery surface, human hair cannot be digested and it can be stagnant in the gastrointestinal system. Consequently, eaten hairs retain and accumulate between the gastric mucosal folds and finally lead to the formation of a hair ball together with food and mucus[25]. In some cases, the hair ball extends from the stomach into the small intestines and colon. This condition is named Rapunzel syndrome, which was first described by Vaughan et al[31] in 1968[32].
Pharmacobezoar
Pharmacobezoars are an uncommon complication caused by conglomerations of medications or medication vehicles in the gastrointestinal tract. Bulk-forming laxatives, e.g., perdium and psyllium, and guar gum appear to contribute to the formation of pharmacobezoars because of their hygroscopic properties and bulk-forming nature[1,33-37]. Extended-release drug products are other candidate causatives for bezoars[38-40]. The development of time-release technology enabled drug tablets/capsules to be slowly dissolved and gradually release active ingredients of the medication. Extended-release drugs, e.g., nifedipine and verapamil, are coated with cellulose acetate, a synthetic chemical compound derived from the plant substance cellulose. Cellulose acetate may aggregate and lead to bezoar formation in the gastrointestinal tract. Enteric coatings, which use a polymer barrier to stabilize drug tablets at the highly acidic pH found in the stomach, are dissolved at a less acidic pH in the small intestine. Because of the insolubility of the carrying vehicle of enteric-coated medications, e.g., aspirin, they can also be responsible for bezoar formation[39].
Lactobezoar
A lactobezoar is an undigested mass composed of milk and mucus components[41]. In clear contrast to the other types of bezoars, virtually all patients affected with a lactobezoar are milk-fed infants. The pathogenesis is likely multifactorial and includes both exogenous risk factors (i.e., the composition of synthetic milk, medications lowering gastric motility and secretion, and methodologies of feeding) and endogenous risk factors (i.e., dehydration, premature birth, and the subsequent insufficient activity and capacity of the digestive tract)[42-44]. Heinz-Erian et al[42] reviewed 96 published cases since the first report in 1959 and noted that most cases were published in the period 1975-1985, whereas only 26 cases have been reported since 1986. The reasons for the infrequency of lactobezoar cases in recent years have not been revealed, but the improvement of synthetic milk composition and advances in premature infant management have probably affected the prevalence.
Other types of bezoar
Varieties of substances other than those responsible for the aforementioned four types of bezoars (i.e., plant materials, hair, medications, and artificial milk) have been reported as a source of bezoars. Such bizarre materials include plastic[45], metals[46], parasitic worms (ascaris)[47], and even toilet paper[48]. Theoretically, all indigestible food materials and foreign bodies can cause a mass formation together with mucus and semi-digested foodstuffs.
STRUCTURE OF PERSIMMON PHYTOBEZOAR
Compared with other phytobezoars, persimmon phytobezoars are more difficult to dissolve or break up into small pieces due to their hard consistency. In addition, persimmon phytobezoars usually have a black or darkish-brown color (Figure 1). We recently investigated persimmon phytobezoar fragments by microscopy, transmission electron microscopy, energy dispersive X-ray spectroscopy, and infrared spectroscopy and revealed the unique structure and components that cause the characteristic hard consistency and dark color[2]. In this section, we briefly introduce our analysis regarding the microstructure of persimmon phytobezoar fragments.
First, the bezoar fragments were analyzed by scanning electron microscopy (SEM). The SEM analysis revealed a high-density, continuous layer approx. 20- to 50-µm thick that formed the exterior of the phytobezoar. Close-up observation revealed that aggregated microgranules constituted the exterior surface. These microgranules were stuck together and created an almost seamless structure with a few slits. In contrast, the density of the inner part of the persimmon phytobezoar was low. The inner part consisted of sheet-like structures with curved or wavy shapes. The wiggly arrangement of the sheet-like structures resulted in unoccupied areas existed between the sheets. These microscopic features indicate that the persimmon phytobezoar’s resistance to mechanical and chemical forces was rendered by almost seamless, dense layers of the exterior surface.
Secondly, to investigate the chemical components that constitute the surface structure and the inner part of the persimmon phytobezoar, we performed an infrared spectroscopy analysis. The surface layer and the inner part of the persimmon phytobezoar were manually segmented with a surgical knife. Both parts were air-dried and analyzed by infrared spectroscopy. The spectra obtained from the surface and the inner parts of the persimmon phytobezoar were quite similar to that of persimmon juice. The persimmon juice was extracted from green, unripe persimmon fruits that contained plenty of tannin. This juice can be commercially purchased in Japan as a natural dyestuff and as a coating material for fabric, paper, and wood. The striking resemblance of spectra between the persimmon juice and the phytobezoar fragments indicates that a quite high concentration of persimmon tannin exists in a phytobezoar. It also suggests the importance of persimmon tannin in the pathogenesis of phytobezoars.
Thirdly, to compare the elemental composition of the surface and the inner part of the phytobezoar, we used S4800 scanning electron microscopy and energy dispersive X-ray spectroscopy (EDX) (EDAX Genesis APEX2 system, Ametek, Paoli, PA). The net intensity of each element was measured at five different points on the surface and the inner part, respectively. We analyzed the spectrum of the EDX results using Genesys software (Ametek). The amount of each element was quantified by the standardless EDAX ZAF quantification method. As a result, higher amounts of sulphur and iron were detected in the surface layer compared to the inner part (Table 1). We speculate that the iron deposition and resulting compound, iron(III) tannate, are responsible for the black color of the persimmon phytobezoar surface. In our study, yttrium, aluminum, and osmium were detected in the persimmon phytobezoar, in addition to the major elements such as carbon, oxygen, sodium and sulfur. Generally, edible plants have yttrium at a concentration of 20-100 ppm[49]. The seeds of woody plants have high amounts, up to 700 ppm. Aluminum is also contained in foods and food additives. Osmium was probably contaminated during the process of sample preparation for the SEM analysis, because it was used as a fixing agent.
Table 1.
Net intensity of elements determined by energy-dispersive X-ray spectroscopy in a persimmon phytobezoar
| Surface layer | Inner part | P value | |
| C | 52.91 ± 13.88 | 62.30 ± 15.77 | 0.35 |
| O | 22.42 ± 5.95 | 43.71 ± 14.56 | < 0.05 |
| Na | 12.77 ± 5.09 | 21.24 ± 6.26 | < 0.05 |
| Al | 9.98 ± 2.55 | 13.01 ± 2.64 | 0.1 |
| Y | 160.62 ± 29.73 | 209.37 ± 38.48 | 0.06 |
| S | 16.96 ± 3.22 | 5.27 ± 1.95 | < 0.01 |
| Fe | 9.88 ± 1.69 | 2.02 ± 1.17 | < 0.01 |
| Os | 45.02 ± 3.96 | 60.35 ± 6.26 | < 0.01 |
For comparisons, statistical analyses were performed by t tests. C: Carbon; O: Oxygen; Na: Sodium; Al: Aluminum; Y: Yttrium; S: Sulfur; Fe: Iron; Os: Osmium.
A limitation associated with our study is that the phytobezoar examined was obtained from a single patient. Since the structure of phytobezoars presumably varies among patients, an analysis of the ultrastructure would ideally include phytobezoars extracted from several different patients. Another subject of great interest is the structure and components of other types of bezoars (i.e., trichobezoars, pharmacobezoars, and lactobezoars). Although the formation of bezoars is a relatively infrequent disorder, further in vitro investigations could provide findings that contribute to the management of phytobezoars.
PATIENT SUSCEPTIBILITY
Bezoars are believed to form as a complication of delayed gastric emptying. Predisposed risk factors include prior gastric surgery such as partial gastrectomy, vagotomy and pyloroplasty, peptic ulcer disease, chronic gastritis, Crohn’s disease, carcinoma of the gastrointestinal tract, dehydration and hypothyroidism[46,50]. These conditions lead to reduced gastric acidity, gastric stasis, loss of pyloric function, and/or pyloric stenosis. Elderly individuals and diabetic patients with neuropathy or myotonic dystrophy have impaired gastric motility[1,12,51,52].
In our previous study, we reviewed 19 Japanese patients with gastrointestinal bezoars and presented their clinical characteristics[3]. To date, we have collected an additional 12 cases. A summary of the 31 cases (13 males and 18 females) is shown in Table 2. In accord with previous studies, the histories of our patient series included diabetes mellitus (n = 3, 9.7%) and surgery of the gastrointestinal tract (n = 11, 35.5%). Notably, except for the 10-year-old patient with a trichobezoar, all patients were 61 years of age or older. Consequently, the potential development of bezoars in elderly individuals and patients with underlying disease that causes poor gastric motility should be borne in mind by clinicians.
Table 2.
Clinical characteristics of bezoar patients
| n (%) | |
| Total | 31 |
| Female | 18 (58.1) |
| Median age (yr, range) | 74 (10-93) |
| Past histories | |
| Diabetes mellitus | 3 (9.7) |
| Surgery of gastrointestinal tract | 11 (35.5) |
| Symptoms | |
| Pain | 11 (35.5) |
| Bloody or tarry stool | 5 (16.1) |
| Abdominal fullness | 5 (16.1) |
| Discomfort | 5 (16.1) |
| Anemia | 4 (12.9) |
| Difficulty of swallowing | 3 (9.7) |
| Hematemesis | 3 (9.7) |
| Nausea | 3 (9.7) |
| Anorexia | 1 (3.2) |
| Faint | 1 (3.2) |
| None | 3 (9.7) |
| Bezoar location | |
| Stomach | 29 (93.5) |
| Small intestine | 2 (6.5) |
| Diagnosis modality | |
| Esophagogastroduodenoscopy | 23 (74.2) |
| Computed tomography | 8 (25.8) |
| Complications of bezoar | |
| Gastric ulcer | 201 (64.5) |
| Ileus | 31 (9.7) |
| Reflux esophagitis | 1 (3.2) |
| Acute gastric mucosal lesions | 1 (3.2) |
| Duodenal ulcer | 1 (3.2) |
| None | 6 (19.4) |
One patient presented with both gastric ulcer and ileus.
MANIFESTATIONS AND DIAGNOSIS
Bezoars can be asymptomatic or present with a variety of gastrointestinal symptoms. In our series of 31 patients with gastrointestinal bezoars, pain (n = 11), bloody or tarry stool (n = 5), abdominal fullness (n = 5), discomfort (n = 5), anemia (n = 4), difficulty swallowing (n = 3), hematemesis (n = 3), nausea (n = 3), anorexia (n = 1), and fainting (n = 1) were observed as initial presentations (Table 2). In contrast, bezoars were coincidentally found in asymptomatic patients (n = 5) by esophagogastroduodenoscopy or computed tomography (CT) scans performed during a health check-up or follow-up of other diseases. Symptoms related to gastrointestinal bleeding such as hematemesis, bloody or tarry stool, anemia, and fainting are the result of the development of ulceration in the gastric mucosa due to pressure necrosis induced by the bezoar[1]. As shown in Table 2, gastric ulcers were observed in 20 of the 31 patients (64.5%) by esophagogastroduodenoscopy. Lee et al[53] also documented a high rate of gastric ulcers as a complication of bezoars (41.2%, 7/17 cases). Obstruction of the gastrointestinal tract is another vital manifestation caused by bezoars, particularly by small intestinal bezoars.
Endoscopic examinations play the most important role in the detection of gastric bezoars, as well as in the treatment of this disease. A phytobezoar is typically observed in the gastric fundus as a single mass, but it can be multiple. The color is diverse depending on the materials constituting the phytobezoar, ranging from beige, tan, ocher, yellow green, to black[3]. As described above, the black color of persimmon phytobezoar’s surface is probably imparted by iron(III) tannate (Figure 1A)[2].
CT scanning is useful to detect both gastric and small intestinal bezoars. Phytobezoars are visualized by CT scan as an ovoid or round occupational mass in the gastrointestinal tract with air bubbles retained inside and a mottled appearance[54,55]. A CT scan is particularly valuable in patients requiring the surgical removal of small intestinal bezoars, not only because it demonstrates the obstructed site of the intestines; it also enables the visualization of multiple bezoars[19].
TREATMENT OF BEZOARS
Overview
The currently available treatment options for a gastric phytobezoar include dissolution of the bezoar by Coca-Cola®, removal by endoscopic devices, laparotomy, and laparoscopic surgery. It should be noted that persimmon phytobezoars are often resistant to chemical dissolution because of their hard consistency, and they are thus usually removed endoscopically or surgically[53,55].
Intestinal bezoars are generally removed by a surgical procedure, since patients with this type of bezoar often present with intestinal obstruction and ileus.
Coca-Cola
The first successful treatment achieved with Coca-Cola® lavage was reported in 2002 by Ladas et al[56]. In a recent review by Ladas et al[56], they summarized 24 publications including 46 patients and noted that Coca-Cola® administration resulted in phytobezoar resolution in 91.3% of the cases, either as a sole treatment or in combination with an endoscopic procedure[20]. The protocol for Coca-Cola® administration has varied among authors[53]. Ladas et al[56] performed gastric lavage via nasogastric tubes with 3000 mL of Coca-Cola® administered over 12 h. Hayashi et al[57] reported that the peroral intake of 500-1000 mL/d of Coca-Cola® for 3 wk resulted in a decrease in size and softened structure of the phytobezoar. Mihai et al[8] described 12 patients treated with 4800 mL of Coca-Cola® ingestion over 12 h (100 mL every 15 min); complete dissolution of the bezoar was observed in 5 patients (42%), and fragmentation of the bezoar was found in 5 patients (42%). In the latest review, Ladas et al[20] recommended gastric lavage with 3000 mL of Coca-Cola® for 12 h, or drinking 3000 mL of Coca-Cola® over 12 h. The adequate dose and timing of Coca-Cola® administration should be investigated, because no standard protocol for bezoar treatment has been established to date.
In our recent paper, we investigated persimmon phytobezoar dissolubility by Coca-Cola® in vitro[4]. A gastric persimmon phytobezoar was fragmented by endoscopy forceps and polypectomy snares (Figure 1C) and extracted with a retrieval net device (Figures 1D and 2A). A fragment and hydrochloric acid-potassium chloride buffer (pH 2.0) was put into each of several tubes. Double-distilled water, Coca-Cola®, Coca-Cola Zero®, a digestive enzyme supplement containing cellulase, or papain supplement was added to the tube. After a 12-h incubation, the contents of the tubes were gently decanted into 100-mm polystyrene dishes, and photographs of these dishes were taken. Representative images of each group at post-incubation are shown in Figures 2B-2F. The particles of broken bezoar were fewest in the control (Figure 2B).
Figure 2.
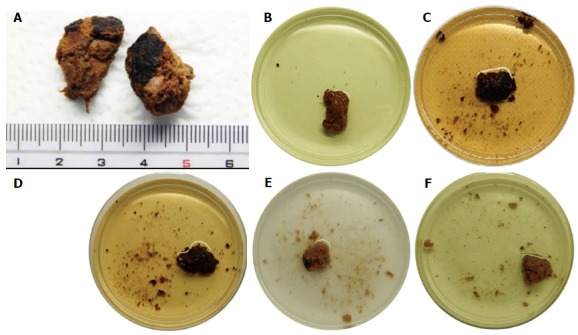
Photographs of the in vitro experiment. A: Endoscopically extracted fragments of the gastric bezoar were used; B: Representative photographs of the bezoar fragments incubated at 37 °C with gentle swirling for 12 h with double-distilled water; C: Bezoar fragments after incubation with Coca-Cola®; D: Bezoar fragments after incubation with Coca-Cola Zero®; E: Bezoar fragments after incubation with a digestive enzymes supplement including cellulase; F: Bezoar fragments after incubation with papain. The bezoar fragments were clearly more softened and more fragmented after 12-h incubation with Coca-Cola® or Coca-Cola Zero® than with the other agents.
By contrast, more particles of the broken bezoar were observed after incubation with Coca-Cola® (Figure 2C) or Coca-Cola Zero® (Figure 2D), even compared to cellulase (Figure 2E) or papain (Figure 2F). Next, the undissolved bezoar fragments were extracted, and their weights were measured after 30 min of air-drying and compared the values with the weight at pre-incubation. The phytolytic activities of the solvents are summarized in Figure 3. Bezoar fragments showed significantly better dissolubility in Coca-Cola Zero® (16.1% ± 0.4%) than in water (7.0% ± 5.3%) (P < 0.05, t test). The dissolubility in Coca-Cola® (18.5% ± 5.8%) was also higher than that in cellulase (10.1 ± 4.5%), papain (9.5% ± 6.5%), and water, though the difference between Coca-Cola® and water was not significant (P = 0.06) due to the relatively large standard deviation. Overall, our study obtained the first evidence of the comparative benefits of Coca-Cola® beverages. In addition, Coca-Cola® and Coca-Cola Zero® showed equal phytolytic activities in vitro.
Figure 3.

The dissolubility of bezoar fragments. The mean dissolubility of bezoar fragments was highest by Coca-Cola®, but the difference between Coca-Cola® and water was not significant (P = 0.06) due to the relatively large standard deviation. NS: Not significant. aP < 0.05.
Although the mechanism has not been fully elucidated, it has been speculated that some ingredients in Coca-Cola® play a key role in bezoar dissolution. Such hypotheses include enhanced bezoar digestion by the mucolytic effect of sodium bicarbonate and/or by the acidifying effect of carbonic acid and phosphoric acid. Destruction of the bezoar may also be assisted by the carbon dioxide bubbles, which penetrate into the bezoar through the microscopic pores on its surface[5,20,56,58,59]. Diet Coke®, Coca-Cola Light®, and Coca-Cola Zero® all contain these ingredients. Since the clinical success of bezoar dissolution by Diet Coke®, Coca-Cola Light®, and Coca-Cola Zero® was documented in previous reports, several authors have speculated that these sugar-free beverages have the same effect of bezoar dissolution as the regular version of Coca-Cola®[5,60]. Although our study was conducted using the phytobezoar obtained from a single patient, the results confirmed this speculation, revealing almost equal bezoar dissolubility between Coca-Cola® and Coca-Cola Zero®. A future study should determine whether or not other carbonated beverages such as Pepsi-Cola® and carbonated water have the same lytic action against phytobezoars.
Despite the number of reports describing a successful treatment outcome of phytobezoars, however, persimmon phytobezoars may not be dissolved by Coca-Cola® beverages alone because of their hard consistency. For example, Lee et al[53] reported that complete dissolution by Coca-Cola® administration was observed in 4/6 patients (66.7%) with non-persimmon phytobezoars, whereas Coca-Cola® was completely ineffective in all 11 patients with persimmon phytobezoars (0%) in whom this method was attempted. For such phytobezoars that are resistant to chemical dissolution, endoscopic fragmentation and removal in combination with or without Coca-Cola® dissolution is generally effective[55].
Papain
Papain, an enzyme extracted from the Carica papaya plant, has been used as an alternative enzymatic therapy for bezoars. Generally, papain rapidly hydrolyzes a variety of proteins based on the proteolytic activity. Several authors have described bezoar dissolution by the oral administration of Adolph’s Meat Tenderizer or gastric lavage with the tenderizing agent[61]. However, papain is no longer included in Adolph’s Meat Tenderizer, because the manufacturer changed the chief ingredient from papain to bromelain, which is another proteolytic enzyme contained in pineapples. Papain is currently used in other products for tenderizing meat, in clarifying beer, and in biochemical research involving the analysis of proteins. Papain is thus still commercially available, but physicians should keep in mind that adverse events such as gastric ulceration and esophageal perforation following papain therapy have been documented[62,63].
In our previous study, papain powders were extracted from a capsule of dietary supplement, but the bezoar dissolubility in papain was not significantly higher than that in water (Figures 2 and 3)[4]. The insufficient dissolubility of bezoars in papain is contradictory to the previous successful clinical outcomes. We speculate that this might be due to the small dose size of the active enzymes in a dietary supplement capsule. An excess doses of papain supplement may be effective for the dissolution of bezoars, but it is impractical in a clinical setting because the maximum dose of papain for safe ingestion have not been elucidated.
Cellulase
Cellulase has been widely used for phytobezoar treatment, since vegetables and fruits contain large amounts of cellulose. The enhancement of phytobezoar digestion by cellulase may originate in its degradation activity against cellulose by cleaving the glycosidic bond. A successful outcome of bezoar treatment with tablet-form gastroenterase (containing pepsin, pancreatic enzyme concentrate, cellulase, and dehydrocholic acid) was described in the 1970s[64,65]. However, these tablets have been discontinued. Additionally, in many countries, cellulase is not readily available for ingestion as a commercial product, or even as a medication under prescription[60]. For example, in the United States, cellulase is only available as a dietary supplement in combination with other digestive enzymes. In our previous study, however, one capsule of cellulase supplement was not effective for the lysis of bezoar fragments (Figures 2 and 3)[4].
Endoscopic removal
Endoscopic fragmentation has often been applied for gastric bezoars. Various types of endoscopy devices including biopsy forceps, alligator forceps, a polypectomy snare, a basket catheter, an argon plasma coagulation device and an electrohydraulic lithotripsy device have been used for fragmentation[3]. Kurt et al[66] recently reported the first patient with a gastric bezoar successfully treated with a bezoaratom, an oval polyfilament snare device specifically designed for the treatment of bezoars. Endoscopic spraying or the endoscopic injection of Coca-Cola® into bezoars probably assists fragmentation via lytic activity for gastrointestinal bezoars[20,67]. It should be noted that persimmon phytobezoars may require multiple sessions of endoscopic treatment to be completely broken down because of the hard consistency[3].
Trichobezoars are resistant to enzymatic degradation and pharmacotherapy. Endoscopic fragmentation is generally ineffective due to the high density of the hair conglomerate. In a review of the 40 reported trichobezoar cases, endoscopic removal was successful in only two of the cases; the other cases required laparotomy or laparoscopic surgery[35]. In our experience, however, we achieved fragmentation of trichobezoar in one patient by using an electrosurgical knife[3]. Electrosurgical knives developed for endoscopic submucosal dissection may thus be useful for treating trichobezoars.
Surgical removal
Surgical removal is inevitable for cases presenting with ileus or patients with refractory bezoars. Bezoars were traditionally managed by open surgical retrieval (laparotomy). Recent papers emphasized the importance of a minimally invasive surgical approach by laparoscopy in the management of gastrointestinal bezoars[54,68-70]. Intraoperative endoscopic removal has also been reported[71].
Other treatment strategies
In some patients, the administration of prokinetic agents was reportedly effective in resolving the gastric bezoar[3]. As described above, a reduction in the evacuation of indigestible foods due to insufficient gastric motor activity can lead to bezoar formation. Prokinetic agents such as itopride, mosapride, and metoclopramide may improve gastric emptying and facilitate the break-down of a bezoar by enhancing contractions of the gastrointestinal tract and increasing their frequency, if the bezoar is soft enough to be digested with gastrointestinal peristalsis.
Spontaneous disappearance of a bezoar under the absence of specific treatment was also observed in some patients[3,6]. The etiology of the bezoars and the mechanisms underlying how the bezoars were digested in these patients remain to be determined. However, careful follow-up without any specific treatment is a possible option in the management of bezoar patients, if they are in stable condition[6].
CONCLUSION
We reviewed the prevalence, classification, structure, predisposing factors, manifestations, diagnosis, and treatment strategies of gastrointestinal bezoars. Endoscopy and CT play key roles in the detection and management of bezoars. The administration of Coca-Cola® is currently the primary choice for phytobezoar treatment because it is safe, inexpensive, and effective. Endoscopic fragmentation or surgical removal should be applied in urgent cases, such as those manifesting gastrointestinal bleeding and/or ileus, and patients with refractory bezoars.
ACKNOWLEDGMENTS
We thank the following individuals for their important contributions to the identification of patient medical records: Dr. Shouichi Tanaka and Dr. Daisuke Tanioka, (Iwakuni Clinical Center); Dr. Junji Shiode (Okayama Saiseikai General Hospital); Dr. Motowo Mizuno (Hiroshima City Hospital); Dr. Ryuta Takenaka (Tsuyama Central Hospital); Dr. Tatsuya Toyokawa (Fukuyama Medical Center); Dr. Yuko Okamoto (Ibara City Hospital); Dr. Yoshinari Kawai and Dr. Toshihiro Murata, (Onomichi Municipal Hospital); Electron microscopy analyses were performed by Mr. Haruo Urata and Ms. Masumi Furutani, (Central Research Laboratory, Okayama University Medical School).
Footnotes
Conflict-of-interest: The authors declare that there are no conflicts of interest.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: September 6, 2014
First decision: September 28, 2014
Article in press: January 20, 2015
P- Reviewer: Grunewald B, Koulaouzidis A, Kamberoglou D S- Editor: Gong XM L- Editor: A E- Editor: Wu HL
References
- 1.Sanders MK. Bezoars: from mystical charms to medical and nutritional management. Pract Gastroenterol. 2004;18:37–50. [Google Scholar]
- 2.Iwamuro M, Urata H, Furutani M, Kawai Y, Shiraha H, Takaki A, Okada H, Yamamoto K. Ultrastructural analysis of a gastric persimmon phytobezoar. Clin Res Hepatol Gastroenterol. 2014;38:e85–e87. doi: 10.1016/j.clinre.2013.11.005. [DOI] [PubMed] [Google Scholar]
- 3.Iwamuro M, Tanaka S, Shiode J, Imagawa A, Mizuno M, Fujiki S, Toyokawa T, Okamoto Y, Murata T, Kawai Y, et al. Clinical characteristics and treatment outcomes of nineteen Japanese patients with gastrointestinal bezoars. Intern Med. 2014;53:1099–1105. doi: 10.2169/internalmedicine.53.2114. [DOI] [PubMed] [Google Scholar]
- 4.Iwamuro M, Kawai Y, Shiraha H, Takaki A, Okada H, Yamamoto K. In vitro analysis of gastric phytobezoar dissolubility by coca-cola, coca-cola zero, cellulase, and papain. J Clin Gastroenterol. 2014;48:190–191. doi: 10.1097/MCG.0b013e3182a39116. [DOI] [PubMed] [Google Scholar]
- 5.Ertuğrul G, Coşkun M, Sevinç M, Ertuğrul F, Toydemir T. Treatment of gastric phytobezoars with Coca-Cola given via oral route: a case report. Int J Gen Med. 2012;5:157–161. doi: 10.2147/IJGM.S29453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kadian RS, Rose JF, Mann NS. Gastric bezoars--spontaneous resolution. Am J Gastroenterol. 1978;70:79–82. [PubMed] [Google Scholar]
- 7.Ahn YH, Maturu P, Steinheber FU, Goldman JM. Association of diabetes mellitus with gastric bezoar formation. Arch Intern Med. 1987;147:527–528. [PubMed] [Google Scholar]
- 8.Mihai C, Mihai B, Drug V, Cijevschi Prelipcean C. Gastric bezoars--diagnostic and therapeutic challenges. J Gastrointestin Liver Dis. 2013;22:111. [PubMed] [Google Scholar]
- 9.Yakan S, Sirinocak A, Telciler KE, Tekeli MT, Deneçli AG. A rare cause of acute abdomen: small bowel obstruction due to phytobezoar. Ulus Travma Acil Cerrahi Derg. 2010;16:459–463. [PubMed] [Google Scholar]
- 10.Ghosheh B, Salameh JR. Laparoscopic approach to acute small bowel obstruction: review of 1061 cases. Surg Endosc. 2007;21:1945–1949. doi: 10.1007/s00464-007-9575-3. [DOI] [PubMed] [Google Scholar]
- 11.de Toledo AP, Rodrigues FH, Rodrigues MR, Sato DT, Nonose R, Nascimento EF, Martinez CA. Diospyrobezoar as a cause of small bowel obstruction. Case Rep Gastroenterol. 2012;6:596–603. doi: 10.1159/000343161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cifuentes Tebar J, Robles Campos R, Parrilla Paricio P, Lujan Mompean JA, Escamilla C, Liron Ruiz R, Pellicer Franco EM. Gastric surgery and bezoars. Dig Dis Sci. 1992;37:1694–1696. doi: 10.1007/BF01299861. [DOI] [PubMed] [Google Scholar]
- 13.Acar T, Tuncal S, Aydin R. An unusual cause of gastrointestinal obstruction: bezoar. N Z Med J. 2003;116:U422. [PubMed] [Google Scholar]
- 14.Moffat JH, Fraser WP. Gastric Bezoar. Can Med Assoc J. 1962;87:813–814. [PMC free article] [PubMed] [Google Scholar]
- 15.Park SE, Ahn JY, Jung HY, Na S, Park SJ, Lim H, Choi KS, Lee JH, Kim do H, Choi KD, et al. Clinical outcomes associated with treatment modalities for gastrointestinal bezoars. Gut Liver. 2014;8:400–407. doi: 10.5009/gnl.2014.8.4.400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gayà J, Barranco L, Llompart A, Reyes J, Obrador A. Persimmon bezoars: a successful combined therapy. Gastrointest Endosc. 2002;55:581–583. doi: 10.1067/mge.2002.122332. [DOI] [PubMed] [Google Scholar]
- 17.Moriel EZ, Ayalon A, Eid A, Rachmilewitz D, Krausz MM, Durst AL. An unusually high incidence of gastrointestinal obstruction by persimmon bezoars in Israeli patients after ulcer surgery. Gastroenterology. 1983;84:752–755. [PubMed] [Google Scholar]
- 18.Granot E, Fich A, Ayalon A, Manny J, Winograd I, Schwartz J, Rachmilewitz D. An epidemic of persimmon bezoars in Israel. Isr J Med Sci. 1984;20:167–169. [PubMed] [Google Scholar]
- 19.Altintoprak F, Degirmenci B, Dikicier E, Cakmak G, Kivilcim T, Akbulut G, Dilek ON, Gunduz Y. CT findings of patients with small bowel obstruction due to bezoar: a descriptive study. ScientificWorldJournal. 2013;2013:298392. doi: 10.1155/2013/298392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ladas SD, Kamberoglou D, Karamanolis G, Vlachogiannakos J, Zouboulis-Vafiadis I. Systematic review: Coca-Cola can effectively dissolve gastric phytobezoars as a first-line treatment. Aliment Pharmacol Ther. 2013;37:169–173. doi: 10.1111/apt.12141. [DOI] [PubMed] [Google Scholar]
- 21.Holloway WD, Lee SP, Nicholson GI. The composition and dissolution of phytobezoars. Arch Pathol Lab Med. 1980;104:159–161. [PubMed] [Google Scholar]
- 22.Matsuo T, Ito S. The chemical structure of kaki-tannin from immature fruit of the persimmon. Agric Biol Chem. 1978;126:421–424. [Google Scholar]
- 23.Krausz MM, Moriel EZ, Ayalon A, Pode D, Durst AL. Surgical aspects of gastrointestinal persimmon phytobezoar treatment. Am J Surg. 1986;152:526–530. doi: 10.1016/0002-9610(86)90221-7. [DOI] [PubMed] [Google Scholar]
- 24.Maki T, Suzuki N. Experimental formation of persimmon-bezoar. Tohoku J Exp Med. 1965;86:168–177. doi: 10.1620/tjem.86.168. [DOI] [PubMed] [Google Scholar]
- 25.Gorter RR, Kneepkens CM, Mattens EC, Aronson DC, Heij HA. Management of trichobezoar: case report and literature review. Pediatr Surg Int. 2010;26:457–463. doi: 10.1007/s00383-010-2570-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Diefenbach GJ, Reitman D, Williamson DA. Trichotillomania: a challenge to research and practice. Clin Psychol Rev. 2000;20:289–309. doi: 10.1016/s0272-7358(98)00083-x. [DOI] [PubMed] [Google Scholar]
- 27.Carr JR, Sholevar EH, Baron DA. Trichotillomania and trichobezoar: a clinical practice insight with report of illustrative case. J Am Osteopath Assoc. 2006;106:647–652. [PubMed] [Google Scholar]
- 28.Bouwer C, Stein DJ. Trichobezoars in trichotillomania: case report and literature overview. Psychosom Med. 1998;60:658–660. doi: 10.1097/00006842-199809000-00025. [DOI] [PubMed] [Google Scholar]
- 29.Sehgal VN, Srivastava G. Trichotillomania +/- trichobezoar: revisited. J Eur Acad Dermatol Venereol. 2006;20:911–915. doi: 10.1111/j.1468-3083.2006.01590.x. [DOI] [PubMed] [Google Scholar]
- 30.DeBakey M, Ochsner A. Part 1: Bezoars and concretions. Surgery. 1938;4:934–963. [Google Scholar]
- 31.Vaughan ED, Sawyers JL, Scott HW. The Rapunzel syndrome. An unusual complication of intestinal bezoar. Surgery. 1968;63:339–343. [PubMed] [Google Scholar]
- 32.Naik S, Gupta V, Naik S, Rangole A, Chaudhary AK, Jain P, Sharma AK. Rapunzel syndrome reviewed and redefined. Dig Surg. 2007;24:157–161. doi: 10.1159/000102098. [DOI] [PubMed] [Google Scholar]
- 33.Stack PE, Thomas E. Pharmacobezoar: an evolving new entity. Dig Dis. 1995;13:356–364. doi: 10.1159/000171515. [DOI] [PubMed] [Google Scholar]
- 34.Schneider RP. Perdiem causes esophageal impaction and bezoars. South Med J. 1989;82:1449–1450. doi: 10.1097/00007611-198911000-00032. [DOI] [PubMed] [Google Scholar]
- 35.Frohna WJ. Metamucil bezoar: an unusual cause of small bowel obstruction. Am J Emerg Med. 1992;10:393–395. doi: 10.1016/0735-6757(92)90030-2. [DOI] [PubMed] [Google Scholar]
- 36.Agha FP, Nostrant TT, Fiddian-Green RG. “Giant colonic bezoar”: a medication bezoar due to psyllium seed husks. Am J Gastroenterol. 1984;79:319–321. [PubMed] [Google Scholar]
- 37.Oka A, Ishihara S, Kinoshita Y. An unusual case of a gastric foreign body. Gastroenterology. 2013;145:1206, 1500–1501. doi: 10.1053/j.gastro.2013.08.012. [DOI] [PubMed] [Google Scholar]
- 38.Taylor JR, Streetman DS, Castle SS. Medication bezoars: a literature review and report of a case. Ann Pharmacother. 1998;32:940–946. doi: 10.1345/aph.17420. [DOI] [PubMed] [Google Scholar]
- 39.Stack PE, Patel NR, Young MF, Ferslew KE, Thomas E. Pharmacobezoars--the irony of the antidote: first case report of nifedipine XL bezoar. J Clin Gastroenterol. 1994;19:264–265. doi: 10.1097/00004836-199410000-00020. [DOI] [PubMed] [Google Scholar]
- 40.Chung M, Reitberg DP, Gaffney M, Singleton W. Clinical pharmacokinetics of nifedipine gastrointestinal therapeutic system. A controlled-release formulation of nifedipine. Am J Med. 1987;83:10–14. doi: 10.1016/0002-9343(87)90630-9. [DOI] [PubMed] [Google Scholar]
- 41.Levkoff AH, Gadsden RH, Hennigar GR, Webb CM. Lactobezoar and gastric perforation in a neonate. J Pediatr. 1970;77:875–877. doi: 10.1016/s0022-3476(70)80252-9. [DOI] [PubMed] [Google Scholar]
- 42.Heinz-Erian P, Gassner I, Klein-Franke A, Jud V, Trawoeger R, Niederwanger C, Mueller T, Meister B, Scholl-Buergi S. Gastric lactobezoar - a rare disorder? Orphanet J Rare Dis. 2012;7:3. doi: 10.1186/1750-1172-7-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bos ME, Wijnen RM, de Blaauw I. Gastric pneumatosis and rupture caused by lactobezoar. Pediatr Int. 2013;55:757–760. doi: 10.1111/ped.12164. [DOI] [PubMed] [Google Scholar]
- 44.WOLF RS, BRUCE J. Gastrotomy for lactobezoar in a newborn infant. J Pediatr. 1959;54:811–812. doi: 10.1016/s0022-3476(59)80150-5. [DOI] [PubMed] [Google Scholar]
- 45.Yeh J, Saul T, Gingrich A, Wassermann J. Bezoar. J Emerg Med. 2013;45:615–616. doi: 10.1016/j.jemermed.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 46.Kumar GS, Amar V, Ramesh B, Abbey RK. Bizarre metal bezoar: a case report. Indian J Surg. 2013;75:356–358. doi: 10.1007/s12262-012-0706-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zheng PP, Wang BY, Wang F, Ao R, Wang Y. Esophageal space-occupying lesion caused by Ascaris lumbricoides. World J Gastroenterol. 2012;18:1552–1554. doi: 10.3748/wjg.v18.i13.1552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Goldman RD, Schachter P, Katz M, Bilik R, Avigad I. A bizarre bezoar: case report and review of the literature. Pediatr Surg Int. 1998;14:218–219. doi: 10.1007/s003830050492. [DOI] [PubMed] [Google Scholar]
- 49.Daane AH. Yttrium. In: The Encyclopedia of the Chemical Elements, edited by Hampel CA., editors. New York, NY: Reinhold Book Corporation; 1968. [Google Scholar]
- 50.LaFountain J. Could your patient’s bowel obstruction be a bezoar? Todays Surg Nurse. 1999;21:34–37. [PubMed] [Google Scholar]
- 51.Campos RR, Paricio PP, Albasini JLA, Riquelme Riquelme J, Cifuentes Tebar J, Luján Mompeán JA. Gastrointestinal bezoars. Presentation of 60 cases. Dig Surg. 1990;7:39–44. [Google Scholar]
- 52.Simsek Z, Altinbas A, Yuksel I, Yuksel O. Effective treatment with pineapple juice in small bowel obstruction due to phytobezoar in a gastrectomized patient. Dig Endosc. 2011;23:197. doi: 10.1111/j.1443-1661.2010.01059.x. [DOI] [PubMed] [Google Scholar]
- 53.Lee BJ, Park JJ, Chun HJ, Kim JH, Yeon JE, Jeen YT, Kim JS, Byun KS, Lee SW, Choi JH, et al. How good is cola for dissolution of gastric phytobezoars? World J Gastroenterol. 2009;15:2265–2269. doi: 10.3748/wjg.15.2265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sharma D, Srivastava M, Babu R, Anand R, Rohtagi A, Thomas S. Laparoscopic treatment of gastric bezoar. JSLS. 2010;14:263–267. doi: 10.4293/108680810X12785289144566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zhang RL, Yang ZL, Fan BG. Huge gastric disopyrobezoar: a case report and review of literatures. World J Gastroenterol. 2008;14:152–154. doi: 10.3748/wjg.14.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ladas SD, Triantafyllou K, Tzathas C, Tassios P, Rokkas T, Raptis SA. Gastric phytobezoars may be treated by nasogastric Coca-Cola lavage. Eur J Gastroenterol Hepatol. 2002;14:801–803. doi: 10.1097/00042737-200207000-00017. [DOI] [PubMed] [Google Scholar]
- 57.Hayashi K, Ohara H, Naitoh I, Okumura F, Andoh T, Itoh T, Nakazawa T, Joh T. Persimmon bezoar successfully treated by oral intake of Coca-Cola: a case report. Cases J. 2008;1:385. doi: 10.1186/1757-1626-1-385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chung YW, Han DS, Park YK, Son BK, Paik CH, Jeon YC, Sohn JH. Huge gastric diospyrobezoars successfully treated by oral intake and endoscopic injection of Coca-Cola. Dig Liver Dis. 2006;38:515–517. doi: 10.1016/j.dld.2005.10.024. [DOI] [PubMed] [Google Scholar]
- 59.Sanderson I, Ibberson O, Fish EB. Gastric phytobezoar following gastrectomy. Can Med Assoc J. 1971;104:1115 passim. [PMC free article] [PubMed] [Google Scholar]
- 60.Kramer SJ, Pochapin MB. Gastric phytobezoar dissolution with ingestion of diet coke and cellulase. Gastroenterol Hepatol (N Y) 2012;8:770–772. [PMC free article] [PubMed] [Google Scholar]
- 61.Dwivedi AJ, Chahin F, Agrawal S, Patel J, Khalid M, Lakra Y. Gastric phytobezoar: treatment using meat tenderizer. Dig Dis Sci. 2001;46:1013–1015. doi: 10.1023/a:1010701809950. [DOI] [PubMed] [Google Scholar]
- 62.Dugan FA, Lilly JO, McCaffery TD. Dissolution of a phytobezoar with short-term medical management. South Med J. 1972;65:313–316. doi: 10.1097/00007611-197203000-00013. [DOI] [PubMed] [Google Scholar]
- 63.Holsinger JW, Fuson RL, Sealy WC. Esophageal perforation following meat impaction and papain ingestion. JAMA. 1968;204:734–735. [Google Scholar]
- 64.Bruck HM. Letter: Gastric phytobezoar. JAMA. 1975;231:26. doi: 10.1001/jama.231.1.26b. [DOI] [PubMed] [Google Scholar]
- 65.Gold MH, Patteson TE, Green GI. Cellulase bezoar injection: a new endoscopic technique. Gastrointest Endosc. 1976;22:200–202. doi: 10.1016/s0016-5107(76)73753-2. [DOI] [PubMed] [Google Scholar]
- 66.Kurt M, Posul E, Yilmaz B, Korkmaz U. Endoscopic removal of gastric bezoars: an easy technique. Gastrointest Endosc. 2014:In press. doi: 10.1016/j.gie.2014.01.052. [DOI] [PubMed] [Google Scholar]
- 67.Lin CS, Tung CF, Peng YC, Chow WK, Chang CS, Hu WH. Successful treatment with a combination of endoscopic injection and irrigation with coca cola for gastric bezoar-induced gastric outlet obstruction. J Chin Med Assoc. 2008;71:49–52. doi: 10.1016/S1726-4901(08)70073-X. [DOI] [PubMed] [Google Scholar]
- 68.Kannan NL, Singaraju H, Sim SW. Laparoscopic-assisted removal of gastric trichobezoar: a novel technique to reduce operative complications and time. J Pediatr Surg. 2013;48:1826–1827. doi: 10.1016/j.jpedsurg.2013.05.069. [DOI] [PubMed] [Google Scholar]
- 69.Javed A, Agarwal AK. A modified minimally invasive technique for the surgical management of large trichobezoars. J Minim Access Surg. 2013;9:42–44. doi: 10.4103/0972-9941.107142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Nirasawa Y, Mori T, Ito Y, Tanaka H, Seki N, Atomi Y. Laparoscopic removal of a large gastric trichobezoar. J Pediatr Surg. 1998;33:663–665. doi: 10.1016/s0022-3468(98)90342-6. [DOI] [PubMed] [Google Scholar]
- 71.Gong EJ, Jung HY, Kim do H, Lim H, Song KB. Intraoperative endoscopic removal of a duodenal bezoar in a patient with intestinal malrotation. Gastrointest Endosc. 2014;80:346; discussion 347. doi: 10.1016/j.gie.2014.02.028. [DOI] [PubMed] [Google Scholar]


