Abstract
Little is known about the amount of Motivational Interviewing (MI) needed to reduce risky sexual behavior among People Living with HIV/AIDS (PLWHA) or the roles self-efficacy and motivation to practice safer sex play. Among 183 PLWHA who received safer sex MI and were surveyed every 4 months over a 12 month period, we used hierarchical negative binomial regression models to examine the association between amount of counseling time and sexual risk behavior. We performed mediation analysis to evaluate whether changes in self-efficacy and motivation explained this association. This study found that as MI time and number of provided sessions increased, participants’ sexual risk behavior decreased. The effect of MI time and number of sessions on sexual behavior was mediated by self-efficacy but not by motivation to practice safer sex.
Keywords: HIV, Motivational interviewing, Self-efficacy, Motivation, Sexual behavior
Introduction
Between a third (30%) and a half (46%) of sexually transmitted HIV infections in the US are passed on by people who know that they are HIV positive [1]. Up to one-third of HIV-infected people still practice unprotected sex after learning about their sero-positive status [2, 3]. In addition to transmitting the virus to HIV negative partners, unsafe sex can result in co-infection with other sexually transmitted infections, as well as development of super-infection with other HIV strains [4–6]. Many people living with HIV/AIDS (PLWHA), however, face several challenges to practicing safer sex. Understanding how best to assist PLWHA practice safer sex is, therefore, critical to optimizing their health and reducing HIV spread. A meta-analysis of 12 randomized controlled trials of interventions promoting safer sex behavior for PLWHA has demonstrated that behavioral interventions are effective in reducing unprotected sex and decreasing STI acquisition [7]. The review also noted certain features that are associated with successful interventions (e.g. being theory-based, including skills building, lasting more than 3 months), but knowing more about the mechanism of action through which successful programs operate would enable us to target our programs better.
Motivational Interviewing (MI), a counseling style that intends to change behavior by helping clients “explore and resolve ambivalence” [8], is one intervention approach used to reduce risky behaviors of PLWHA [9–13]. Supporting self-efficacy and motivating people to change their behaviors are the main principles underlying MI counseling [8]. Self-efficacy refers to people’s confidence that they can effectively perform a certain behavior under specified conditions [14]. Self-efficacy can be enhanced and, importantly, this enhancement is prospectively related to health behavior change [15]. Motivation refers to the “forces that determine the direction and intensity of the behavior change effort” [16]. According to the information-motivation-behavioral skills model, motivation to reduce AIDS risk is one of the three factors contributing to AIDS risk reduction behavior [17]. Enhancement of self-efficacy and increased motivation to practice safer sex are significant components of several effective behavioral change interventions aimed at reducing unsafe sex [9, 18–21].
Very few HIV prevention studies have conducted mediational analyses of effective interventions [22, 23] to identify intermediate factors that contribute to a reduction in risky sexual behavior of PLWHA. Once identified, however, program designers can target specific intermediate variables to make future risk reduction intervention programs even more effective. While evidence suggests that building self-efficacy for practicing safer sex is one significant pathway through which safer health behavior change takes place [22, 23], this pathway has not been assessed for MI specifically. Moreover, the relationship between amount of MI counseling (dose) and practicing safer sex (effect) has not yet been investigated. Therefore, we sought to assess empirically whether the dose of MI counseling that HIV-infected patients received contributed to their improvement in sexual risk behavior through changes in self-efficacy and motivation to practice safer sex.
Methods
Participants and Procedures
We used data collected as part of SafeTalk, a two-armed, randomized, controlled trial of a safer sex intervention among 490 HIV-infected patients receiving care at one of three clinics in North Carolina. Participants were followed approximately every 4 months for 12 months between July 2006 and May 2009.
SafeTalk was a multi-component, four session MI-based safer sex program. The attention matched control program was a multi-component, four session heart healthy nutrition counseling program. In addition to individual counseling, all participants received a combined CD and workbook series that helped prepare them for each counseling session.
Participants were eligible for the SafeTalk study if they were: (1) HIV-infected; (2) 18 years of age or over; (3) English-speaking; and (4) reported having sex in the past 12 months. Potential participants were excluded if they were: (1) cognitively unable to provide consent; (2) too sick to travel to clinic; (3) former participants in another safer sex MI program; (4) in clinic for their first visit; or (5) intending to leave the clinic within the next 12 months. Recruitment was conducted through pre-screening at the main site and with the help of clinical staff at the other two sites. For eligible patients who were interested in participating, the research assistant obtained informed consent. Additional details on SafeTalk methods are previously published [24].
Although being sexually active in the past 12 months prior to the baseline assessment was an inclusion criterion, some participants did not report any sexual activity throughout the study. We conducted the analyses reported here with the subsample of participants who were both in the intervention arm (n = 248) and reported being sexually active in the last 3 months on at least one assessment point during the study (n = 183) because the outcome pertinent to the study was the incidence of unprotected sex.
Motivational Interviewing Intervention
Masters’ level-trained counselors delivered the SafeTalk program every 4 weeks for 16 weeks. Participants received booster letters individualized to issues raised in each MI session [24]. The duration of each individual MI session was not prescribed by the protocol, but was flexibly determined by counselor and client together. On average, sessions lasted 40 min.
Each MI session was aimed at enhancing motivation and self-efficacy surrounding participants’ chosen target behaviors (e.g. using condoms, reducing substance use, disclosing HIV status). A CD/workbook series of guided exercises helped participants prepare for each MI session. Each session was based on a standard protocol that allowed the sessions to be individually designed to meet each participant’s needs [24]. The SafeTalk MI protocol directed the counselor to explicitly assess a participant’s current relationship status and sexual activities and to provide a menu of topics related to safer sex practices from which each participant could choose personal goals [25]. Most of the MI sessions were delivered face to face. Telephone MI counseling was offered to participants with transportation problems. Among those who received any counseling (n = 148 since some participants randomized to counseling never came to receive it), 14% (n = 21) received some telephone counseling and three percent (n = 4) received only telephone counseling. Of those participants who received any counseling, 95% (n = 141) received all counseling sessions from the same counselor.
Study Instruments
Evaluation surveys were administered to study participants at baseline, 4, 8, and 12 month visits using an approximately 40-min audio computer-assisted self-interview (ACASI) in the clinics. ACASIs assessed participants’ demographic and clinical characteristics, psychosocial factors, attitudes and beliefs, characteristics of sexual relationships, and risky sexual behavior.
To assess MI session features, immediately after each MI session counselors recorded the content of that session on standardized recording sheets, the time spent counseling and whether counseling was delivered by phone.
The study procedures were approved by the University of North Carolina at Chapel Hill’s Office for the Protection of Human Research Subjects.
Outcome Variables of Interest
Unprotected Sex Behavior with At-Risk Partner
Unprotected anal or vaginal intercourse with at-risk partner (UAVI-AR) was measured as the number of unprotected acts of vaginal and anal sex with any at-risk (HIV negative or unknown serostatus) partner. Participants were asked a series of questions about the frequency of their sexual behaviors over the past 3 months, and the frequency of condom use, based on the gender and serostatus of their partner(s). The participants entered numerical values to answer the questions. Based on the answers provided to these sexual behavior questions, we calculated the total number of unprotected sex acts with HIV negative and unknown serostatus partners, and summed them for every participant. We treated any item with a value greater than 100 counts as an outlier since the population parameters do not follow the same distribution. Doing so we excluded four outliers on this variable (0.7%).
Unprotected Sex Behavior with Any Type of Partner
Unprotected anal or vaginal intercourse (UAVI) was measured as the number of unprotected acts of vaginal or anal sex with ANY partner. In a manner similar to that of the UAVI-AR variable, we calculated and summed, for each participant, the number of unprotected acts of vaginal and anal sex with HIV positive as well as HIV negative and serostatus unknown partners. We deleted any item with a value greater than 100 counts. Six outliers for this variable were excluded from the analysis (1%).
Independent Variables of Interest
Amount of MI Time (Dose)
Although in planning the study the ideal was for all four counseling sessions to be completed before the 4 month survey, some participants did not stay on schedule and received some of their counseling sessions between the 4 and 8 months surveys (n = 82, 44.8% of total participants). By design, no counseling sessions took place after the 8 months survey. The total amount of counseling time provided to a study participant (dose) was calculated for each participant based on information in the data recording sheets for each session. We first defined two time intervals: (1) time period 1 was the interval between completion of the baseline survey and the 4 month follow-up survey; (2) time period 2 was the interval between completion of the 4 month follow-up survey and the 8 month follow-up survey. Dose per interval was then calculated by summing all of the counseling time participants received during time period 1 and similarly for time period 2. We used this information to cumulate total counseling time received by each time interval.
Number of Counseling Sessions
The total number of counseling sessions provided by counselors to participants was also abstracted from the data recording sheets. Similar to the calculation for the amount of counseling time, the number of counseling sessions per interval was calculated by summing all of the counseling sessions participants received during time period 1 and time period 2. The total number of sessions was cumulative over time.
Mediating Variables of Interest
Self-efficacy to Practice Safer Sex
We measured self-efficacy to practice safer sex using a sixteen-item scale modified from previously validated scales developed by Grimley et al. and Parsons et al. [26, 27]. This scale assessed participants’ confidence in conducting a range of tasks required to practice safer sex (e.g. talk about safer sex with a sexual partner, use a condom correctly, use a condom in potentially tempting situations, and negotiate safer sex with sex partners). Response options on the 11-point scale ranged from zero for “not at all confident” to ten for “completely confident”. A self-efficacy score for each participant was derived by taking the mean of all responses for the 16 items of the scale. A higher score indicated a higher self-efficacy to practice safer sex. We coded a self-efficacy score as missing for our analysis if it had more than four missing values (i.e. more than 25%) on the 16 items. As a result, self-efficacy scores were missing for 22 observations (3.5%). The internal consistency reliability for this scale in the study sample was high (Cronbach’s α 0.92).
Motivation to Practice Safer Sex
To measure motivation to practice safer sex, we used a six-item 4-point scale adapted from the Sex Check study [28]. Response options ranged from 1 = not at all motivated to 4 = totally motivated. Participants expressed their level of motivation over the next 3 months regarding: (1) having safer sex; (2) using a condom every single time they had sex; (3) and telling new partners that they had HIV. Participants were asked the same three questions to assess motivation to practice safer sex for both main and casual partners. Cronbach’s α was 0.71 for the entire scale. A motivation to practice safer sex score for each of the participants was derived by taking the mean of all items of the scale. Similarly to the self-efficacy score, a higher motivation score indicated greater motivation to practice safer sex. We treated a motivation score as missing if it had more than two missing values (i.e. more than 33%) on the six items. As a result, a motivation score was missing for 21 observations (3.4%).
Covariates of Interest
Because MI dose was not randomly assigned, we measured and controlled for potential confounders, which we selected based on an a priori conceptual model of factors informed by the literature and associated with each of the independent and dependent variables of interest.
We assessed demographics, clinical factors, proportion of phone counseling and history of previous participation in safer sex MI. We also assessed binge drinking and cocaine/crack use in the last 3 months (see Table 3).
Table 3.
Models to test mediation in the relationship between the MI time and sexual risk behavior (N = 600)
| Outcome | Predictors | Univariate model
|
Multivariate Model
|
|||||
|---|---|---|---|---|---|---|---|---|
| β (SE) unadjusted | t | P | β (SE) adjusted | t | P | 1-eβ | ||
| Mediation by self-efficacy | ||||||||
| MI counseling time—Self-efficacyd—UAVI-AR | ||||||||
| UAVI-AR | MI counseling time | −0.0082 (0.0051) | −1.62 | 0.1052 | −0.0135 (0.0041) | −3.26 | 0.0011 | 1.3 |
| Self-efficacya,d | MI counseling time | 0.0032 (0.0008) | 4.03 | <0.0001 | 0.0025 (0.0008) | 3.18 | 0.0015 | |
| UAVI-AR | Self-efficacyd | −0.3613 (0.1393) | −2.59 | 0.0095 | −0.7418 (0.0929) | −7.99 | <0.0001 | 52.4 |
| MI counseling time | −0.0090 (0.0042) | −2.16 | 0.0306 | −0.0128 (0.0034) | −3.81 | 0.0001 | 1.3 | |
| ab productc | −0.0012 (0.0007) | −1.75 | 0.0403 | |||||
| Number of MI sessions—self-efficacyd—UAVI-AR | ||||||||
| UAVI-AR | Number of MI sessions | −0.6674 (0.1133) | −5.89 | <0.0001 | −0.8386 (0.1192) | −7.04 | <0.0001 | 56.8 |
| Self-efficacya,d | Number of MI sessions | 0.1432 (0.0331) | 4.33 | <0.0001 | 0.1236 (0.0365) | 3.39 | 0.0007 | |
| UAVI-AR | Self-efficacyd | −0.2549 (0.1470) | −1.73 | 0.0830 | −0.3984 | 0.0609 | <0.0001 | 32.9 |
| Number of MI sessions | −0.6259 (0.1281) | −4.88 | <0.0001 | −0.5527 (0.0716) | −7.72 | <0.0001 | 42.5 | |
| ab productd | −0.0561 (0.0293) | −1.91 | 0.0278 | |||||
| MI counseling time—Self-efficacyd—UAVI | ||||||||
| UAVI | MI counseling time | −0.0087 (0.0036) | −2.43 | 0.0152 | −0.008 (0.0023) | −3.50 | 0.0005 | 0.8 |
| Self-efficacya,d | MI counseling time | 0.0032 (0.0008) | 4.03 | <0.0001 | 0.0025 (0.0008) | 3.18 | 0.0015 | |
| UAVI | Self-efficacyd | −0.4030 (0.0862) | −4.67 | <0.0001 | −0.494 (0.0798) | −6.19 | <0.0001 | 39 |
| MI counseling time | −0.0096 (0.0028) | −3.42 | 0.0006 | −0.0093 (0.0023) | −3.96 | <0.0001 | 0.9 | |
| ab productc | −0.0007 (0.0004) | −1.64 | 0.0505 | |||||
| Number of MI sessions—self-efficacyd—UAVI | ||||||||
| UAVI | Number of MI sessions | −0.6189 (0.0883) | −7.01 | <0.0001 | −0.6512 (0.0724) | −9.00 | <0.0001 | 47.9 |
| Self-efficacya,d | Number of MI sessions | 0.1432 (0.0331) | 4.33 | <0.0001 | 0.1236 (0.0365) | 3.39 | 0.0007 | |
| UAVI | Self-efficacyd | −0.3077 (0.0884) | −3.48 | 0.0005 | −0.4298 (0.0705) | −6.10 | <0.0001 | 34.9 |
| Number of MI sessions | −0.5875 (0.0964) | −6.09 | <0.0001 | −0.5867 (0.0811) | −7.23 | <0.0001 | 44.4 | |
| ab productc | −0.0363 (0.0189) | −1.92 | 0.0275 | |||||
| Mediation by motivation | ||||||||
| MI counseling time—motivationd—UAVI-AR | ||||||||
| UAVI-AR | MI counseling time | −0.0082 (0.0051) | −1.62 | 0.1052 | −0.0135 (0.0041) | −3.26 | 0.0011 | 1.3 |
| Motivationb,d | MI counseling time | −0.0001 (0.0003) | −0.26 | 0.7962 | −0.0002 (0.0003) | −0.58 | 0.5638 | |
| UAVI-AR | Motivationd | −0.1289 (0.2831) | −0.46 | 0.6490 | −1.4411 (0.2762) | −5.22 | <0.0001 | 76.3 |
| MI counseling time | −0.0087 (0.0053) | −1.63 | 0.1034 | −0.0148 (0.0043) | −3.42 | 0.0006 | 1.5 | |
| Number of MI sessions—motivationd—UAVI-AR | ||||||||
| UAVI-AR | Number of MI sessions | −0.6674 (0.1133) | −5.89 | <0.0001 | −0.8386 (0.1192) | −7.04 | <0.0001 | 56.8 |
| Motivationb,d | Number of MI sessions | −0.0100 (0.0116) | −0.86 | 0.3878 | −0.0133 (0.0125) | −1.07 | 0.2867 | |
| UAVI-AR | Motivationd | −0.2831 (0.2394) | −1.18 | 0.2369 | −1.3743 (0.2616) | −5.25 | <0.0001 | 74.7 |
| Number of MI sessions | −0.7003 (0.1114) | −6.29 | <0.0001 | −0.903 (0.1728) | −5.23 | <0.0001 | 59.5 | |
| MI counseling time—motivationd—UAVI | ||||||||
| UAVI | MI counseling time | −0.0087 (0.0036) | −2.43 | 0.0152 | −0.008 (0.0023) | −3.50 | 0.0005 | 0.8 |
| Motivationb,d | MI counseling time | −0.0001 (0.0003) | −0.26 | 0.7962 | −0.0002 (0.0003) | −0.58 | 0.5638 | |
| UAVI | Motivationd | −0.9759 (0.2205) | −4.43 | <0.0001 | −1.1465 (0.211) | −5.43 | <0.0001 | 68.2 |
| MI counseling time | −0.0095 (0.0033) | −2.91 | 0.0036 | −0.009 (0.0023) | −3.93 | <0.0001 | 0.9 | |
| Number of MI sessions—Motivationd—UAVI | ||||||||
| UAVI | Number of MI sessions | −0.6189 (0.0883) | −7.01 | <0.0001 | −0.6512 (0.0724) | −9.00 | <0.0001 | 47.9 |
| Motivationb,d | Number of MI sessions | −0.0100 (0.0116) | −0.86 | 0.3878 | −0.0133 (0.0125) | −1.07 | 0.2867 | |
| UAVI | Motivationd | −0.8937 (0.1942) | −4.60 | <0.0001 | −0.921 (0.2328) | −3.96 | <0.0001 | 60.2 |
| Number of MI sessions | −0.6617 (0.0845) | −7.83 | <0.0001 | −0.6358 (0.0787) | −8.08 | <0.0001 | 47 | |
Controlling for age, educational attainment, having a main partner, sexual identity, date of HIV diagnosis, having an undetectable HIV viral load, clinic site, counselor, proportion of counseling sessions done by telephone, history of previous enrollment in a study providing MI counseling, binge drinking in the last 3 months, cocaine/crack use in the last 3 months
UAVI unprotected anal or vaginal intercourse with any partner, UAVI-AR unprotected anal or vaginal intercourse with at-risk partner
Controlling for all variables listed in point 1 above and motivation to practice safer sex
Controlling for all variables listed in point 1 above and self-efficacy to practice safer sex
Obtained from bootstrapping of 1,000 samples with replacement; P value shows one tailed P value of a z test
To practice safer sex
Analysis
Descriptive Analyses
We conducted a descriptive analysis of the study cohort, examined self-efficacy, motivation to practice safer sex, UAVI-AR and UAVI at each of the four survey assessments. In an attrition analysis, we examined characteristics of study participants lost to follow-up by conducting multivariate logistic regression with participants being present or not at 12 month follow-up as the dependent variable and baseline demographic and sexual behavior variables as well as counselor identity as potential predictor variables.
Effect of the Amount of MI on Sexual Risk Behavior
Separate analyses were done for “amount of counseling time” and “number of sessions,” respectively, to see their effects on UAVI-AR and UAVI. Because both outcome variables (UAVI-AR and UAVI) were count variables, we conducted negative binomial regression analysis. We used the PROC GENMOD procedure in SAS 9.2. (SAS Institute, Cary, NC) since observations for a cohort over time were correlated within each study participant. Negative binomial regression was chosen because, unlike Poisson regression, it does not make an assumption about equality of mean and variance. A two-level model was used in which units in the first (lower) level were study assessments (baseline, 4 months follow-up, 8 months follow-up and 12 months follow-up) which were nested within the units in the second (upper) level (study participants). The statistical analysis included all data collected for each study participant at each of the assessments regardless of a participant’s intervention exposure. The model estimated the difference in the logs of expected counts for one unit change in a predictor variable holding other variables constant in the model.
Mediation Analysis
We analyzed lower level mediation since all main variables in our analysis were lower level variables. The upper level was a person and the lower level was a survey assessment. The model tested whether the treatment influenced the mediator which, in turn, affected the outcome. The same mediation analysis (Fig. 1) was implemented for each of the predictors, for each of the proposed mediating variables and for each of the two outcomes (UAVI-AR, UAVI). In each case, three equations were used to assess the mediation effect:
| (1) |
| (2) |
| (3) |
where f was a log link function, Y is sexual risk behavior (UAVI or UAVI-AR), X was dose of MI at each given time point (“amount of time” or “number of sessions”), M was the value of the mediator (self-efficacy or motivation to practice safer sex). First, we analyzed the relationship between the predictor and the outcome in Eq. 1. Next, we tested the association between the predictor and the potential mediator in Eq. 2. Last, we estimated the effect of the predictor on the outcome adjusting for a potential mediator in Eq. 3. All potential confounders (described in the “covariates of interest” section above) were included in each of the equations.
Fig. 1.
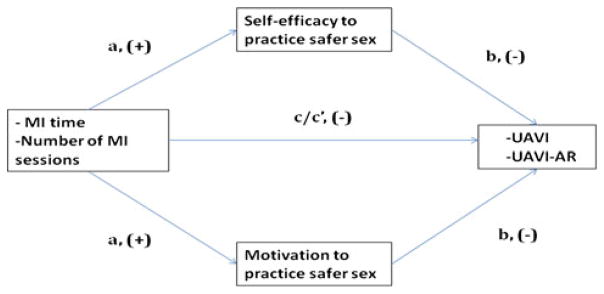
Mediation analysis
The causal step method of Baron and Kenny (1986) has low power to detect mediated effects [29], since the relationship between X and Y variables may be non-significant when the predictor is distal to the outcome [30] or, in the case of inconsistent mediation, when two or more indirect paths operate in opposite directions [31, 32]. Therefore, even though we tested the relationship between X and Y, we took a product of coefficients approach to assess mediation. The product of two estimated coefficients, ab (named βa and βb above), gave us the mediated effect. To test for its significance, we used a bootstrapping method to create confidence intervals for indirect effects [33] since the Sobel test does not take into account non-normality of the distribution of the ab product [33]. MacKinnon et al. [34] found that type-I error was more accurate and statistical power was greater when significance tests for the mediated effect were based on the distribution of the product. Finally, we calculated the percent of the total effect that was mediated using the ab/(c′ + ab) measure because it did not require standardizing coefficients to equate the scale across negative binomial regression models [33].
For continuous outcomes in Eq. 2, we conducted linear regression analyses for longitudinal data using the PROC GENMOD procedure in SAS 9.2. (SAS Institute, Cary, NC) since observations for a cohort over time were correlated within each study participant. For count outcomes in Eq. 3, we conducted negative binomial regression analysis using the PROC GENMOD procedure in SAS 9.2. Since observation time varied across participants, we used the offset option in the model statement to obtain unbiased regression estimates.
Results
Study Cohort Characteristics and Participation Rates
The sample of 183 study participants consisted of 63 men who had sex with men (MSM), 51 men who had sex with women (MSW) and 67 women who had sex with men (WSM). Participants had a mean age of 42 years (SD = 9.58), 74% were African Americans, 62% were male, 23% had less than a high school education, 60% earned less than $10,000/year. On average, participants were diagnosed with HIV for 9 years (SD = 6.1). At baseline, one half (52%) reported undetectable viral loads, and about 80% were on antiretroviral therapy. About a fourth reported crack or cocaine use, and 44% reported binge drinking in the 3 months before the baseline survey (Table 1).
Table 1.
Baseline descriptive characteristics of the study sample (N = 183)
| N | % | |
|---|---|---|
| Demographics | ||
| Age [N, Mean (SD)] | 182 | 41.9 (9.58) |
| Ethnicity | ||
| African American | 136 | 73.73 |
| White | 31 | 17.03 |
| Other | 15 | 8.24 |
| Education | ||
| Less than high school | 42 | 22.95 |
| High school | 63 | 34.43 |
| More than high school | 78 | 42.62 |
| Income | ||
| $10,000 or less | 104 | 59.43 |
| $10,001–40,000 | 58 | 33.14 |
| More than $40,000 | 13 | 7.43 |
| Gender | ||
| Female | 68 | 37.2 |
| Male | 114 | 62.3 |
| Transgender (Female to Male) | 1 | 0.5 |
| Sexual orientation | ||
| Men having sex with men | 63 | 34.81 |
| Men having sex with women | 51 | 28.18 |
| Women having sex with men | 67 | 37.02 |
| Clinical characteristics | ||
| Duration of diagnosis (N, Mean (SD)) | 181 | 9.18(6.09) |
| CD4 count <200 | 24 | 14.46 |
| Viral load | ||
| Undetectable | 95 | 51.91 |
| Detectable | 66 | 36.07 |
| Unaware | 22 | 12.02 |
| Currently on HAART | 148 | 80.87 |
| Behavioral characteristics | ||
| Substance use in past 3 months | ||
| Binge drinking | 80 | 44.2 |
| Cocaine/crack use | 44 | 25.00 |
| Sexual behavior past 3 months | ||
| Had main sex partner | 110 | 62.15 |
| Sexually active | 139 | 75.96 |
| Had UAVI-AR | 31 | 17.42 |
| Had UAVI | 56 | 31.46 |
In the study sample, 19% (n = 35) of the participants did not show up to receive any MI counseling, 6.5% (n = 12) received 1 counseling session, 6.5% (n = 12) received 2 counseling sessions, 9% (n = 17) received 3 counseling sessions and 59% (n = 107) received 4 counseling sessions.
The 183 participants completed 600 surveys. Of the 183 enrolled at baseline, 154 (84%) were retained at 4-month follow-up, 142 (78%) at 8 month follow-up, and 121 (66%) at 12 month follow-up. We did not have many missing observations on outcome variables of interest. Out of 600 observations, only 10 had missing data on UAVI and 10 were missing on UAVI-AR.
The logistic regression analysis showed that participants’ absence at the last follow-up was associated with reporting having unprotected sex with any partner (OR = 3.93, P = 0.01), being more motivated to practice safer sex (OR = 2.35, P = 0.02) at baseline and being an MSM compared to WSM (OR = 2.76, P = 0.02). Participants who had taken part previously in another safer sex MI program were more likely to stay in this study than participants who had not (OR = 9.4, P = 0.04). We found no other differences between those who were and were not absent at the last follow-up.
Means of Self-Efficacy and Motivation to Practice Safer Sex at Each Time Point
Table 2 presents the means of self-efficacy and motivation to practice safer sex for each of the four study assessments. As can be seen from the table, on average, self-efficacy increased whereas motivation to practice safer sex decreased over time.
Table 2.
Level of mediators and outcome variables over time
| Baseline mean (SD) | 4-Months mean (SD) | 8-Months mean (SD) | 12-Months mean (SD) | |
|---|---|---|---|---|
| n = 183 | n = 154 | n = 142 | n = 121 | |
| Self-efficacy to practice | ||||
| Safer sex | 8.22 (1.88) | 8.56 (1.72) | 8.6 (1.68) | 8.76 (1.61) |
| Motivation to practice | ||||
| Safer sex | 3.32 (0.54) | 3.26 (0.61) | 3.22 (0.59) | 3.24 (0.6) |
| n = 172 | n = 152 | n = 140 | n = 120 | |
| UAVI count | 2.99 (8.53) | 2.28 (7.71) | 1.51 (4.0) | 2.02 (10.0) |
| UAVI-AR count | 1.34 (6.03) | 0.79 (4.7) | 0.48 (1.65) | 0.19 (1.02) |
| UAVI proportion% | 31.46 | 23.03 | 25.71 | 17.5 |
| UAVI-AR proportion% | 17.42 | 9.21 | 14.29 | 6.67 |
Means and Proportion of UAVI-AR and UAVI at Each Time Point
Table 2 shows the mean number of acts of UAVI-AR and UAVI as well as the proportion of participants engaged in UAVI-AR and UAVI at each study assessment. Both UAVI-AR and UAVI counts decreased from baseline to 4, 8 and 12 month follow-ups. The proportion of participants engaged in UAVI-AR and UAVI also decreased from baseline to 4 months, then increased slightly from 4 month values at 8 months but continued to decline from 8 to 12 months.
Effect of the Dose and Number of Counseling Sessions on Sexual Risk Behavior
Table 3 shows that the difference in the logs of expected counts for both UAVI-AR and UAVI decreased significantly as the dose of counseling increased. Thus, with 10 min increase in counseling time, UAVI-AR and UAVI rates decreased by 13 and 8% respectively. Similarly, the difference in the logs of expected counts for both UAVI-AR and UAVI decreased significantly as the number of counseling sessions increased. Thus, with one unit increase in number of sessions, UAVI-AR and UAVI rates decreased by 57 and 48% respectively.
Mediation Analysis
Effect of the Amount of MI on Self-Efficacy and Motivation to Practice Safer Sex (a Coefficient)
Overall, self-efficacy to practice safer sex increased as the number of counseling sessions (b = 0.1236, SE = 0.0365, t = 3.39, P = 0.0007) and number of minutes of counseling (b = 0.0025, SE = 0.0008, t = 3.18, P = 0.0015) increased (Table 3). Although motivation was positively associated with self-efficacy (correlation coefficient = 0.4527, P <0.0001), there was no association between the amount of MI and motivation to practice safer sex.
Effect of Self-Efficacy and Motivation to Practice Safer Sex on Sexual Risk Behavior (b Coefficient)
Both self-efficacy and motivation to practice safer sex were negatively associated with UAVI-AR and UAVI. The difference in the logs of expected counts for unprotected sexual intercourse decreased as self-efficacy and motivation to practice safer sex increased (Table 3). A one unit increase in self-efficacy score was associated with a 52 and 39% decrease in UAVI-AR and UAVI rates respectively. A one unit increase in motivation scores was associated with a 76 and 68% decrease in UAVI-AR and UAVI rates respectively.
Mediation Effects
Significant mediation effects of self-efficacy to practice safer sex occurred in the relationships between dose and UAVI-AR, dose and UAVI, number of sessions and UAVI-AR, number of sessions and UAVI (Table 3). Self-efficacy to practice safer sex accounted for approximately 11% of the total effect of counseling dose on UAVI-AR, [0.0022 × 0.7418/(0.0022 × 0.7418 + 0.0128)]. The total effect of dose on UAVI accounted for by self-efficacy to practice safer sex was also equal to 11%. The proportion of total effect of number of sessions on UAVI-AR and UAVI mediated by self-efficacy to practice safer sex equaled seven percent.
Since motivation to practice safer sex was not significantly associated with any of the predictors (coefficient a in Eq. 2 above), we cannot conclude that motivation mediates the relationship between dose/number of sessions and UAVI-AR/UAVI.
Discussion
We found that almost 20% of the study participants at baseline reported having unsafe sex with an at-risk partner and more than 30% reported having unsafe sex with a partner of any serostatus. This finding confirms yet again a need for further HIV prevention programs for PLWHA as one important component of a strategy to reduce the HIV epidemic. Furthermore the overall amount of counseling time, whether measured in number of counseling sessions or minutes spent being counseled, was associated with improvements in safer sexual behavior. Self-efficacy, but not motivation to practice safer sex, mediated this relationship.
Our study findings not only contribute to an understanding of how to best deliver HIV counseling to PLWHA, but also provide insight on how to deliver optimal MI counseling in general. To our knowledge, this is the first study that has attempted to examine the effect of MI dose on sexual behaviors of PLWHA and the role that self-efficacy plays in this relationship.
While the optimal dose is still not clear, these findings suggest that, at least for HIV “prevention with positives” programs, increasing the overall amount of counseling time is a key to promoting safer sexual behavior by enhancing self-efficacy to practice safer sex. Previous research has established an association between the duration of MI counseling, the number of encounters clients have with counselors, and the likelihood of achieving an effect [35, 36]. Our study confirms these findings for PLWHA undergoing safer sex counseling. Polcin et al. [37] has speculated that providing more MI counseling may permit the client more time to remain in a pre-contemplation stage and work through any ambivalence he or she may have during the contemplation stage. Our finding suggests that the mechanism by which this effect occurs acts in part via the self-efficacy pathway.
Enhancing self-efficacy has been shown in multiple settings to enhance health behaviors that are linked to health outcomes [13, 18, 38]. On the other hand, few HIV prevention studies have demonstrated that self-efficacy is the mechanism by which the intervention has improved safer sex practices [22, 23]. Our findings add to existing research by establishing a mediating role for self-efficacy in a sample of HIV positive people receiving MI counseling. We may conclude that interventions that focus more on enhancing self-efficacy to practice safer sex might perform better, holding the amount of motivational interviewing time equal. It is important to keep in mind, however, that in this study, clients had continuity of counselors across sessions 95% of the time and this continuity may have contributed to the relationship between dose and behavior change.
We cannot conclude that the counseling time had an effect on participants’ sexual behavior via changes in motivation because we did not find any association between the amount of counseling and motivation to practice safer sex (coefficient a). From the attrition analysis, however, we know that more motivated participants were lost to follow-up. It is possible we may have underestimated the potential effect that the intervention would have had on more motivated groups of participants.
In addition to our main study finding regarding the effects of dose, we found that an increase in motivation as well as an increase in self-efficacy was associated with a decrease in risky sexual behavior (coefficient b). These findings confirm the importance of aiming health behavior interventions at changing both self-efficacy and motivation, but suggest that self-efficacy, but not motivation, enhancement is more influenced by the amount of counseling received.
The use of a longitudinal design with a diverse sample and repeated measures provide us with greater confidence in establishing causality compared to using data from a cross-sectional design, or from a more homogeneous sample, by offering information about the temporality of change and generalizability of the findings. These factors also allow us to address several alternative explanations for the effects we found, such as the existence of omitted variables. The changes we observed occurred over time within an individual, with every person serving as his or her own control [33]. To minimize alternative explanations even further, we included potential confounding variables in the analysis.
We used count measures (i.e. absolute frequency measures) to assess sexual behavior because, compared to categorical measures, counts provide a more informative means to estimate HIV contraction risk [39]. Also, we used a bootstrapping technique to create confidence intervals for indirect effects. This method provides good accuracy for significance tests for the mediated effect [34].
Our study has several limitations. Because of the sensitive and private nature of sexual health and sexual activity, the study used self-reported data from participants rather than observational data. Self-reported data, however, are subject to social desirability and recall biases [40]. These biases were minimized in the study by the use of computer-assisted interviewing techniques [41, 42] and asking questions related to the last 3 month time period rather than the past month [43]. Also, to measure self-efficacy and motivation to practice safer sex, we used scales with good validity and high reliability.
Absence of randomization of counseling time limits our ability to establish a causal relationship between the amount of motivational interviewing received and change in sexual behavior. For example, it is possible that those participants who were more motivated to change their behavior received more counseling time and attended more sessions than participants who were less motivated. In contrast, it is also possible that counselors provided more MI time to participants with higher risk sexual behavior compared to participants with lower sexual risk behavior. It is also possible that, if the quality of counseling had been unequal across counselors, patients may have stayed longer or come back more often with some counselors than with others. However, our attrition analysis revealed no difference by counselor. We did find that participants’ absence at the 12 months follow-up was associated with having more unprotected sex with any partner and having greater motivation to practice safer sex at baseline. Nevertheless, we are still able to establish an association between the amount of counseling and sexual risk behavior for the sample of participants who were less motivated to practice safer sex. This association, however, could be due to the loss of participants reporting any UAVI at baseline.
It is also possible that participants practiced safer sex as a result of being exposed to the survey questions or because of local events (such as health promotion campaigns) happening during the study period. Although only randomization to a condition may address these threats to internal validity, we minimized them by controlling for potential confounding variables in the analysis.
We analyzed the mediation effect of self-efficacy and motivation to practice safer sex because supporting self-efficacy and motivating people to change their behaviors are the two main principles underlying MI counseling. However, these are not the only factors that may explain the effect of counseling on changes in sexual behavior. There are likely other mediating variables that we did not measure. For example, counseling could provide a client with social support which, in turn, could lead to changes in sexual behaviors.
Finally, threats to external validity exist in this study because the study sites were not randomly chosen for the intervention. Therefore, readers should exercise caution in generalizing the study findings beyond the population of HIV positive patients who attended the three study clinic sites or to populations similar to these participants.
Conclusions
Our research suggests that MI-based prevention programs for PLWHA need to enhance self-efficacy to practice safer sex to ensure a behavior change, at least in populations similar to the one we studied. If clinicians and specialists developing MI interventions for PLWHA recognized the importance that the amount of time they spend with clients has on improving safer sex behavior, money and time could be saved. In an era of budgetary constraints that includes increasing pressure on clinicians and counselors to limit the time they spend with their patients, our research findings provide evidence that more time spent counseling PLWHA can have a positive impact on patient and public health outcomes.
Acknowledgments
This research was funded by National Institutes of Mental Health under grant R01 MH 69989 and was also supported in part by National Institutes of Health Grants (DK056350) and (P30-AI50410). We thank Catherine Grodensky and Jennifer Groves for their help with data management and data preparation. We thank the SafeTalk staff for their work on the project.
Contributor Information
Zulfiya Chariyeva, Email: zchariyeva@futuresgroup.com, Futures Group, 308 West Rosemary Street, Suite 203A, Chapel Hill, NC 27516, USA.
Carol E. Golin, Department of Health Behavior and Health Education, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, Chapel Hill, USA
Jo Anne Earp, Department of Health Behavior and Health Education, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, Chapel Hill, USA.
Suzanne Maman, Department of Health Behavior and Health Education, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, Chapel Hill, USA.
Chirayath Suchindran, Department of Biostatistics, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, Chapel Hill, USA.
Catherine Zimmer, Department of Sociology, University of North Carolina at Chapel Hill, Chapel Hill, USA.
References
- 1.Marks G, Crepaz N, Janssen RS. Estimating sexual transmission of HIV from persons aware and unaware that they are infected with the virus in the USA. AIDS. 2006;20(10):1447. doi: 10.1097/01.aids.0000233579.79714.8d. [DOI] [PubMed] [Google Scholar]
- 2.Kalichman SC, Rompa D, Cage M, DiFonzo K, Simpson D, Austin J, et al. Effectiveness of an intervention to reduce HIV transmission risks in HIV-positive people. Am J Prev Med. 2001;21(2):84–92. doi: 10.1016/s0749-3797(01)00324-5. [DOI] [PubMed] [Google Scholar]
- 3.Fisher JD, Cornman DH, Osborn CY, Amico KR, Fisher WA, Friedland GA. Clinician-initiated HIV risk reduction intervention for HIV-positive persons: formative research, acceptability, and fidelity of the options project. J Acquir Immune Defic Syndr. 2004;37:S78. doi: 10.1097/01.qai.0000140605.51640.5c. [DOI] [PubMed] [Google Scholar]
- 4.Blackard JT, Cohen DE, Mayer KH. Human immunodeficiency virus superinfection and recombination: current state of knowledge and potential clinical consequences. Clin Infect Dis. 2002;34(8):1108–14. doi: 10.1086/339547. [DOI] [PubMed] [Google Scholar]
- 5.Blackard JT, Mayer KH. HIV superinfection in the era of increased sexual risk-taking. Sex Transm Dis. 2004;31(4):201. doi: 10.1097/01.olq.0000118082.45312.1f. [DOI] [PubMed] [Google Scholar]
- 6.Smith DM, Richman DD, Little SJ. HIV superinfection. J Infect Dis. 2005;192(3):438–44. doi: 10.1086/431682. [DOI] [PubMed] [Google Scholar]
- 7.Crepaz N, Lyles CM, Wolitski RJ, Passin WF, Rama SM, Herbst JH, et al. Do prevention interventions reduce HIV risk behaviours among people living with HIV? A meta-analytic review of controlled trials. AIDS. 2006;20(2):143. doi: 10.1097/01.aids.0000196166.48518.a0. [DOI] [PubMed] [Google Scholar]
- 8.Miller WR, Rollnick S. Motivational interviewing: preparing people to change addictive behavior. New York: Guilford Press; 1991. [Google Scholar]
- 9.Bryan AD, Fisher JD, Fisher WA, Murray DM. Understanding condom use among heroin addicts in methadone maintenance using the information-motivation-behavioral skills model. Subst Use Misuse. 2000;35(4):451–71. doi: 10.3109/10826080009147468. [DOI] [PubMed] [Google Scholar]
- 10.DiIorio C, Resnicow K, McDonnell M, Soet J, McCarty F, Yeager K. Using motivational interviewing to promote adherence to antiretroviral medications: a pilot study. J Assoc Nurses AIDS Care. 2003;14(2):52–62. doi: 10.1177/1055329002250996. [DOI] [PubMed] [Google Scholar]
- 11.Kalichman SC, Kelly JA, Rompa D. Continued high-risk sex among HIV seropositive gay and bisexual men seeking HIV prevention services. Health Psychol. 1997;16(4):369–73. doi: 10.1037//0278-6133.16.4.369. [DOI] [PubMed] [Google Scholar]
- 12.Naar-King S, Wright K, Parsons JT, Frey M, Templin T, Lam P, et al. Healthy choices: motivational enhancement therapy for health risk behaviors in HIV-positive youth. AIDS Educ Prev. 2006;18(1):1–11. doi: 10.1521/aeap.2006.18.1.1. [DOI] [PubMed] [Google Scholar]
- 13.Parsons JT, Golub SA, Rosof E, Holder C. Motivational interviewing and cognitive-behavioral intervention to improve HIV medication adherence among hazardous drinkers: a randomized controlled trial. J Acquir Immune Defic Syndr. 2007;46(4):443. doi: 10.1097/qai.0b013e318158a461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bandura A. Self-efficacy: the exercise of control. New York: Worth Publishers; 1997. [Google Scholar]
- 15.Strecher V, DeVellis ME, Becker M, Rosenstock I. The role of self-efficacy in achieving health behavior change. Health Educ Behav. 1986;1(13):73–92. doi: 10.1177/109019818601300108. [DOI] [PubMed] [Google Scholar]
- 16.Carey MP, Lewis BP. Motivational strategies can enhance HIV risk reduction programs. AIDS Behav. 1999;3(4):269–76. doi: 10.1023/a:1025429216459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychol Bull. 1992;111(3):455–74. doi: 10.1037/0033-2909.111.3.455. [DOI] [PubMed] [Google Scholar]
- 18.Dilorio C, Dudley WN, Soet J, Watkins J, Maibach E. A social cognitive-based model for condom use among college students. Nurs Res. 2000;49(4):208. doi: 10.1097/00006199-200007000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Kalichman SC, Nachimson D. Self-efficacy and disclosure of HIV-positive serostatus to sex partners. Health psychol. 1999;18(3):281–7. doi: 10.1037//0278-6133.18.3.281. [DOI] [PubMed] [Google Scholar]
- 20.Fisher JD, Fisher WA, Williams SS, Malloy TE. Empirical tests of an information–motivation–behavioral skills model of AIDS-preventive behavior with gay men and heterosexual university students. Health Psychol. 1994;13(3):238–50. doi: 10.1037//0278-6133.13.3.238. [DOI] [PubMed] [Google Scholar]
- 21.Kalichman S, Malow R, Dévieux J, Stein JA, Piedman F. HIV risk reduction for substance using seriously mentally ill adults: test of the information-motivation-behavior skills (IMB) model. Community Ment Health J. 2005;41(3):277–90. doi: 10.1007/s10597-005-5002-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.NIMH The NIMH Multisite HIV Prevention Trial Group. Social cognitive theory mediators of behavior change in The NIMH Multisite HIV Prevention Trial. Health Psychol. 2001;20:369–76. [PubMed] [Google Scholar]
- 23.O’Leary A, Jemmott LS, Jemmott JB., III Mediation analysis of an effective sexual risk-reduction intervention for women: the importance of self-efficacy. Health Psychol. 2008;27(2):S180–4. doi: 10.1037/0278-6133.27.2(Suppl.).S180. [DOI] [PubMed] [Google Scholar]
- 24.Golin CE, Davis RA, Przybyla SM, Fowler B, Parker S, Earp JA, et al. SafeTalk, a multicomponent, motivational interviewing-based, safer sex counseling program for people living with HIV/AIDS: a qualitative assessment of patients’ views. AIDS Patient Care STDs. 2010;24(4):1073–6. doi: 10.1089/apc.2009.0252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Miller WR, Rollnick S, Moyers TB. Motivational interviewing: professional training videotape series. Albuquerque: The University of New Mexico; 1998. [Google Scholar]
- 26.Grimley DM, Prochaska GE, Prochaska JO, Velicer WF, Galavotti C, Cabral RJ, et al. Cross-validation of measures assessing decisional balance and self-efficacy for condom use. Am J Health Behav. 1996;20(6):406–16. [Google Scholar]
- 27.Parsons JT, Halkitis PN, Bimbi D, Borkowski T. Perceptions of the benefits and costs associated with condom use and unprotected sex among late adolescent college students. J Adolesc. 2000;23(4):377–91. doi: 10.1006/jado.2000.0326. [DOI] [PubMed] [Google Scholar]
- 28.Picciano JF, Roffman RA, Kalichman SC, Rutledge SE, Berghuis JP. A telephone based brief intervention using motivational enhancement to facilitate HIV risk reduction among MSM: a pilot study. AIDS Behav. 2001;5(3):251–62. [Google Scholar]
- 29.MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Ann Rev Psychol. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: New procedures and recommendations. Psychol Methods. 2002;7(4):422–45. [PubMed] [Google Scholar]
- 31.Hayes AF. Beyond baron and kenny: statistical mediation analysis in the new millennium. Commun Monogr. 2009;76(4):408–20. [Google Scholar]
- 32.MacKinnon DP, Krull JL, Lockwood CM. Equivalence of the mediation, confounding and suppression effect. Prev Sci. 2000;1(4):173–81. doi: 10.1023/a:1026595011371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.MacKinnon DP. Introduction to statistical mediation analysis. New York: Lawrence Erlbaum Associates; 2008. [Google Scholar]
- 34.MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods. 2002;7(1):83. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Burke BL, Arkowitz H, Menchola M. The efficacy of motivational interviewing: a meta-analysis of controlled clinical trials. J Consult Clin Psychol. 2003;71(5):843–61. doi: 10.1037/0022-006X.71.5.843. [DOI] [PubMed] [Google Scholar]
- 36.Rubak S, Sandbæk A, Lauritzen T, Christensen B. Motivational interviewing: a systematic review and meta-analysis. Br J Gen Pract. 2005;55(513):305. [PMC free article] [PubMed] [Google Scholar]
- 37.Polcin DL, Galloway GP, Palmer J, Mains W. The case for high-dose motivational enhancement therapy. Subst Use Misuse. 2004;39(2):331–43. doi: 10.1081/ja-120028494. [DOI] [PubMed] [Google Scholar]
- 38.Wolf MS, Davis TC, Osborn CY, Skripkauskas S, Bennett CL, Makoul G. Literacy, self-efficacy, and HIV medication adherence. Patient Educ Couns. 2007;65(2):253–60. doi: 10.1016/j.pec.2006.08.006. [DOI] [PubMed] [Google Scholar]
- 39.Schroder KEE, Carey MP, Vanable PA. Methodological challenges in research on sexual risk behavior: I. Item content, scaling, and data analytical options. Ann Behav Med. 2003;26(2):76–103. doi: 10.1207/s15324796abm2602_02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fisher RJ. Social desirability bias and the validity of indirect questioning. J Consu Res. 1993;20(2):303–15. [Google Scholar]
- 41.Gribble JN, Miller HG, Rogers SM, Turner CF. Interview mode and measurement of sexual behaviors: methodological issues. J Sex Res. 1999;36(1):16–7. doi: 10.1080/00224499909551963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Turner CF, Ku L, Rogers SM, Lindberg LD, Pleck JH, Sonenstein FL. Adolescent sexual behavior, drug use, and violence: increased reporting with computer survey technology. Science. 1998;280(5365):867. doi: 10.1126/science.280.5365.867. [DOI] [PubMed] [Google Scholar]
- 43.Schroder KEE, Carey MP, Vanable PA. Methodological challenges in research on sexual risk behavior: II. Accuracy of self-reports. Ann Behav Med. 2003;26(2):104–23. doi: 10.1207/s15324796abm2602_03. [DOI] [PMC free article] [PubMed] [Google Scholar]


