Abstract
Our case report describes a previously healthy 34-year-old male who develops a descending mediastinitis as a complication of an Epstein-Barr virus (EBV) infection. The mediastinitis was suspected to have developed by a breakthrough of a peritonsillar abscess through the space between the alar and prevertebral space.
CASE REPORT
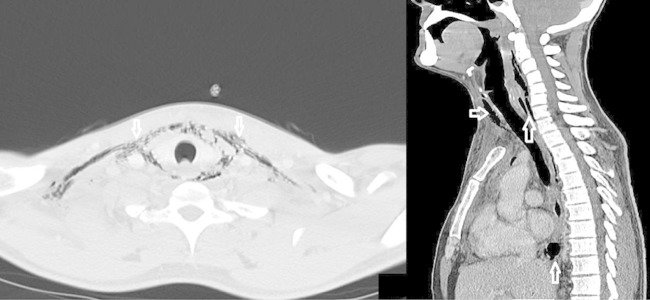
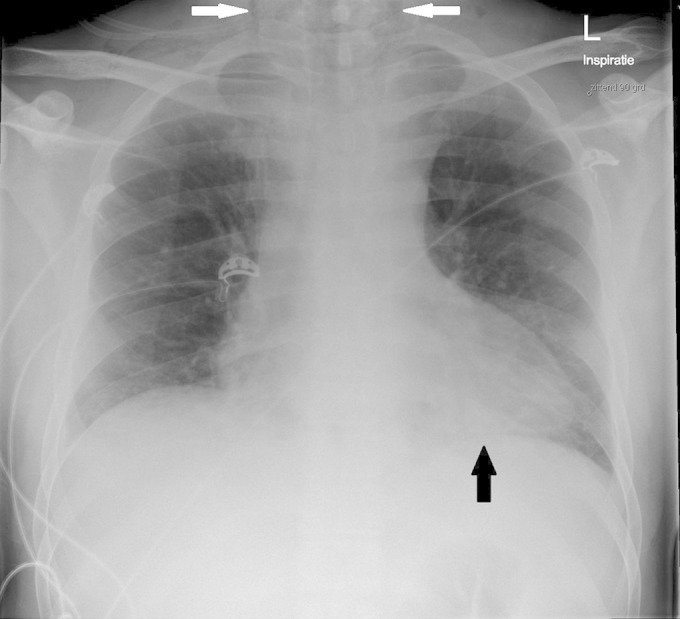
The patient in our case report was a previously healthy 34-year-old male, who was referred to our emergency department by his general practitioner. He presented with complaints of fever and a sore throat for 2 to 3 weeks and was diagnosed with a primary Epstein-Barr virus (EBV) infection (positive IgM anti-viral capsid antigen [anti-VCA], positive IgG anti-VCA, and negative anti-Epstein-Barr virus nuclear antigen). Because of new onset of pain in his upper abdomen and dysphagia, he consulted his general practitioner again. His family later reported that the patient had a painful swelling in his neck, which disappeared shortly before presentation in the emergency room. On physical examination, he had a relatively low blood pressure (116/82 mm Hg), tachycardia (140 beats per minute [bpm]), and a high respiratory rate (35 to 40/min). At inspection, the tonsils were enlarged with white exudate. His throat was swollen and painful at palpation, but no erythema was seen. During pulmonary investigation, pleural rubs were heard, and the abdominal survey revealed a painful upper abdomen. Laboratory investigations showed leukocytosis (13.6 ×109/liter), elevated C-reactive protein (399 mg/liter), and elevated liver enzymes (aspartate transaminase [AST], 174 U/liter; alanine aminotransferase [ALT], 287 U/liter). Blood smear showed atypical lymphocytes and granulocytes with vacuoles, both compatible with an infection with EBV, cytomegalovirus (CMV), or toxoplasmosis. The chest X-ray showed a minor infiltrate (black arrow) and cervical and mediastinal emphysema (white arrows) (Fig. 1). Blood cultures were drawn, the patient was started on amoxicillin-clavulanic acid, and the intensive care unit was consulted. A computed tomography (CT) scan of the thorax and of the neck showed cervical and mediastinal emphysema (hollow white arrows), cellulitis, mediastinitis, and a peritonsillar abscess (Fig. 2). The mediastinal emphysema could have arisen from either an infection by a gas-producing bacterium (fasciïtis necroticans) or from a perforating defect in the trachea or esophagus. The preliminary diagnosis was descending mediastinitis as a complication of a peritonsillar abscess. Because of respiratory distress, the patient was intubated and admitted to the intensive care unit. Gentamicin, metronidazole, and clindamycin were added to the antibiotic regimen. The patient was transferred to a university hospital for evaluation for thoracic surgery. Treatment with broad-spectrum antibiotics was continued, and intravenous (i.v.) Ig was administered for a short period to treat a putative toxic shock syndrome. After 48 h, the i.v. Ig was stopped. Furthermore, the patient underwent extensive surgery, consisting of debridement of the neck and mediastinum. Pleuritic empyema and multiple abscesses were drained. Staphylococcus aureus and Streptococcus salivarius grew in a preoperative deep tonsil culture. Fusobacterium necrophorum was cultured from a deep wound site in the neck. The antibiotic regimen was switched to a combination of penicillin, flucloxacillin, and metronidazole. After a 60-day period in the hospital, including 26 days in intensive care, the patient was discharged to a rehabilitation center.
FIG 1.
Chest X-ray showing a minor infiltrate (black arrow) and mediastinal/cervical emphysema (white arrows).
FIG 2.
Two images from CT scan of neck and thorax showing mediastinal/cervical emphysema (hollow white arrows).
Epstein-Barr virus (EBV) is a common disease with a seroprevalence in adulthood of more than 90%. If patients are symptomatic, the most common complaints are fever, sore throat, fatigue, and enlarged lymph nodes. In limited cases, complications can arise, including rupture of the spleen, myocarditis, pancreatitis, acute kidney failure, or neurological disorders (1). In a review of the literature, only two previous case reports were found describing mediastinitis as a complication of an EBV infection (2) (3). In 2002, a case was published by Adrianakis et al. of a 17-year-old female with active EBV infection, who developed mediastinitis after a 3-day period with complaints of a sore throat (3). In this paper, two different mechanisms for the development of mediastinitis are described. Either mechanism can only occur when a peritonsillar abscess is already present. The first mechanism is a breakthrough of the abscess through the space between the alar and prevertebral space and the second is through septic thrombophlebitis (syndrome of Lemierre). In our case, F. necrophorum was cultivated, which is a Gram-negative anaerobic bacillus. This microorganism is part of the normal oropharyngeal flora. It is the most common organism to cause suppurative septic thrombophlebitis, which is called Lemierre's syndrome when found in the jugular vein. CT scans in our case did not show thrombophlebitis, which would lead us to believe that a breakthrough of a peritonsillar abscess between the alar and the prevertebral space was the mechanism that occurred in our patient. The added information that a swelling in the region of the peritonsillar abscess abruptly disappeared seems to confirm this. Another variant of Lemierre's syndrome is suggested in a case report by Matten et al., where a patient with a suspected EBV infection had a nearly complete consolidation of her left lung (4). F. necrophorum was isolated in a blood culture, but the CT scan of the head, neck, and thorax did not show a septic thrombophlebitis or abscess (4).The cases described above show that EBV infection can be complicated by superinfections. Hagelskjaer Kristensen and Prag speculated that a transient decrease in the T cell-mediated immunity caused by EBV infection may predispose to a bacterial superinfection (5). Oral commensals would be the logical microorganisms to cause cases like these (6). In 2014, a case report was published of an 18-year-old woman with a white cell count below 2,000/ml3 and positive IgM/IgG antibodies to EBV (7). She developed Lemierre's syndrome caused by F. necrophorum, with cavernous-sinus thrombophlebitis, carotid artery thromboarteritis, and abcesses of the parotid gland and subperiosteal orbit. If EBV infection leads to immunosuppression, one can speculate that EBV infection could be a step in the pathway that leads to these life-threatening presentations. Descending mediastinitis is a complication of EBV infection, which can take a fulminant course, even in previously healthy young individuals. Early recognition and treatment are vital for a full recovery.
REFERENCES
- 1.Bennett JE, Dolin R, Blaser MJ. 2015. Mandell, Douglas, and Bennett's principles and practices of infectious diseases, 8th ed Churchill Livingstone, Philadelphia, PA. [Google Scholar]
- 2.Kopec SE, Irwin RS, Curtis JM, Umali CB. 1997. Bilateral anaerobic empyemas complicating infectious mononucleosis. Chest 112:833–835. doi: 10.1378/chest.112.3.833. [DOI] [PubMed] [Google Scholar]
- 3.Andrianakis IA, Kotanidou AN, Pitaridis MT, Saroglou GJ, Exarhos DN, Roussos CS, Bellenis IP. 2002. Life-threatening bilateral empyema and mediastinitis complicating infectious mononucleosis. Intensive Care Med 28:663–664. doi: 10.1007/s00134-002-1270-1. [DOI] [PubMed] [Google Scholar]
- 4.Matten EC, Grecu L. 2006. Unilateral empyema as complication of infectious mononucleosis: a pathogenic variant of Lemierre's syndrome. J Clin Microbiol 44:659–661. doi: 10.1128/JCM.44.2.659-661.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hagelskjaer Kristensen L, Prag J. 2000. Human necrobacillosis, with emphasis on Lemierre's syndrome. Clin Infect Dis 31:524–532. doi: 10.1086/313970. [DOI] [PubMed] [Google Scholar]
- 6.Bartlett JG. 1993. Anaerobic bacterial infections of the lung and pleural space. Clin Infect Dis 16:248–255. [DOI] [PubMed] [Google Scholar]
- 7.Olson KR, Freitag SK, Johnson JM, Branda JA. 2014. An 18-year-old woman with fever, pharyngitis and double vision. N Engl J Med 371:2018–2027. doi: 10.1056/NEJMcpc1310001. [DOI] [PubMed] [Google Scholar]