We read with interest the report by Mediratta et al. (1), which concluded that an intercommissural or middle-of-the-annulus position is desired to minimize device-related tricuspid regurgitation (TR) post-implantation of right ventricle (RV) pacemaker and implantable cardioverter-defibrillator (ICD) leads. In their methodology, the RV lead location is determined by 3-dimensional (3D) transthoracic echocardiography (TTE) and the severity of TR, only by 2-dimensional (2D) color Doppler evaluation. Finally, they suggested that 3D TTE should be routinely used during intraprocedural lead placement. Several important issues, especially factors related to assessment of the severity of TR in this retrospective study, need to be clarified.
Although not considered by Mediratta et al. (1), causes of TR other than lead placement may be critical. TR may be due to either intrinsic valvular disease/dysfunction (leaflet, chord, or papillary muscle) or tricuspid annulus enlargement. For patients with cardiac devices, the most frequent change in RV morphology is dilation due to chronic elevation of left heart filling pressures and subsequent development of pulmonary hypertension. When pulmonary artery systolic pressure (PASP) exceeds 40 mm Hg, the incidence of TR approaches 90% (2). Due to lack of focus during retrospective analysis on etiological factors and time interval dependence between device implantation and 3D TTE study, one could question whether TR is caused by underlying heart disease or lead location. In their Figures 1 and 4 (1), moderate-to-severe RV dysfunction was apparent in an example of septal impingement by a device lead, whereas a normal/smaller RV chamber was shown in their example (Figure 5) (1) of a well-positioned lead. There must be other factors involved; otherwise, what would explain the greater baseline severity of TR in the lead impingement group as shown in their Figure 6 (1)? Paired comparison data for the subgroup patients with 2D TTE before and after implantation (n = 53) should have been shown separately.
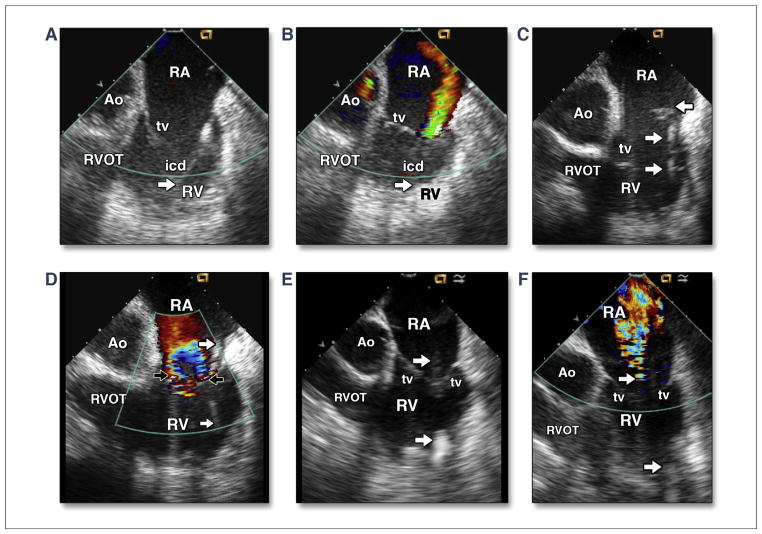
FIGURE 1. Intracardiac Echocardiographic Images of Intracardiac Device Lead and Tricuspid Regurgitant Severity With Different Etiologies.
Intracardiac echocardiographic imaging with the transducer placed in the right atrium in 3 patients. The first patient had severe left ventricular (LV) dysfunction (left ventricular ejection fraction [LVEF] = 20%), normal right ventricular (RV) size, and pulmonary artery systolic pressure (PASP) estimated at 55 mm Hg, an implantable cardioverter defibrillator (ICD) lead (arrow) placed at the RV anterolateral wall with impingement of the posterior leaflet (A), and moderately eccentric tricuspid regurgitation (TR) with color Doppler imaging (CDI) (B). The second patient had moderate LV dysfunction (LVEF = 35%); enlarged RV and tricuspid annulus; PASP of 51 mm Hg; an ICD lead (rightward arrows) placed at the RV apex; multiple small thrombi (leftward arrow) attached at the lead (C); and severely centralized TR with CDI, which shows that the lead (arrows) is slightly impinging the posterior leaflet (D). The third patient had arrhythmogenic RV cardiomyopathy, enlarged RV and tricuspid annulus, PASP of 33 mm Hg, LVEF = 30%, a centralized location of ICD lead (arrows) placed at the RV apex (E), and moderately to severely centralized TR with CDI (F). Ao = aortic root; RA = right atrium; RVOT = RV outflow tract; tv = tricuspid valve.
With routine clinical application of intracardiac echocardiography (ICE), RV anatomy and function (3) and many of the valvular etiologies of TR can be identified and assessed in real time. Real-time ICE imaging has superior capability to image the course of the device lead from the right atrium to the RV. The device-lead location and route passing through the annulus can be imaged. TR induced by intracardiac device-lead impingement and its severity can be accurately assessed (Figures 1A and 1B). However, independent of lead position, moderate-to-severe and mainly centralized TR can be commonly detected in an enlarged and dysfunctional RV, secondary to left ventricular (LV) dysfunction/heart failure (Figures 1C and 1D) or due to arrhythmogenic RV cardiomyopathy (Figures 1E and 1F) with recurrent ventricular tachyarrhythmia. It is strange that this paper found no difference in TR severity in ICD versus pacemaker lead implantation. Our clinical observations with ICE imaging may indicate that ICD leads with more thickness and rigidity have higher events of TR than standard pacing leads, as others have reported previously (4).
Iatrogenic lead–related TR is an important clinical problem, and the investigators should be congratulated for reporting a relatively large number of cases with 2D and 3D TTE imaging. However, their results do not consider other important causes for TR and certainly did not demonstrate convincingly how real-time 3D TTE would consistently facilitate lead placement.
References
- 1.Mediratta A, Addetia K, Yamat M, et al. 3D echocardiographic location of implantable device leads and mechanism of associated tricuspid regurgitation. J Am Coll Cardiol Img. 2014;7:337–47. doi: 10.1016/j.jcmg.2013.11.007. [DOI] [PubMed] [Google Scholar]
- 2.Yock PB, Popp RL. Noninvasive estimation of right ventricular systolic pressure by Doppler ultrasound in patients with tricuspid regurgitation. Circulation. 1984;70:657–62. doi: 10.1161/01.cir.70.4.657. [DOI] [PubMed] [Google Scholar]
- 3.Ren JF, Callans DJ, Marchlinski FE. A simplified quantitative evaluation of right ventricular anatomy and function by intracardiac echocardiography. J Am Coll Cardiol HF. 2014;2:198–9. doi: 10.1016/j.jchf.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 4.Kim JB, Spevack DM, Tunick PA, et al. The effect of transvenous pacemaker and implantable cardioverter defibrillator lead placement on tricuspid valve function: an observational study. J Am Soc Echocardiogr. 2008;21:284–7. doi: 10.1016/j.echo.2007.05.022. [DOI] [PubMed] [Google Scholar]