Abstract
A 61-year-old woman who had undergone total hysterectomy 16 years previously exhibited a pelvic tumor on computed tomography (CT). F-18 fluorodeoxyglucose (FDG) combined positron emission tomography (PET)/CT imaging revealed a solitary small focus of increased FDG activity in the pelvis. A gastrointestinal stromal tumor originating in the small intestine or another type of tumor originating in the mesentery (desmoid, schwannoma, or foreign body granuloma) was suspected; therefore, laparoscopic resection was conducted. A white, hard tumor was found to originate from the mesentery of the sigmoid colon and adhered slightly to the small intestine. The tumor was resected with a negative margin, and the pathologic diagnosis was suture granuloma. The possibility of suture granuloma should be kept in mind in cases of tumors with positive PET findings and a history of surgery close to the lesion. However, it is difficult to preoperatively diagnose pelvic tumors using a biopsy. Therefore, considering the possibility of malignancy, it is necessary to achieve complete resection without exposing the tumor.
Key words: Suture granuloma, Laparoscopy, Positron emission tomography (PET)
It is very difficult to diagnose suture granulomas preoperatively. F-18 fluorodeoxyglucose (FDG) combined positron emission tomography (PET)/computed tomography (CT) imaging is often used to differentiate benign from malignant tumors that are difficult to diagnose on other modalities, such as ultrasound (US), CT, and magnetic resonance imaging. However, it is not easy to differentiate tumors associated with inflammation or malignancy using FDG-PET/CT. Suture granulomas are known to be benign; however, false-positive findings were observed on PET/CT in our case. In the literature, there are few reports of suture granulomas showing false-positive findings on PET/CT.1–5 We report here a case in which it was not possible to rule out the potential for malignancy using CT or FDG-PET/CT and the lesion was confirmed to be a suture granuloma based on a pathologic examination following laparoscopic resection.
Case Report
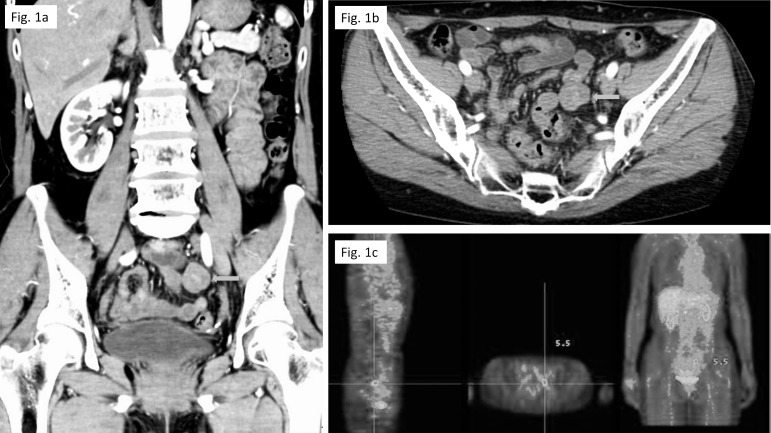
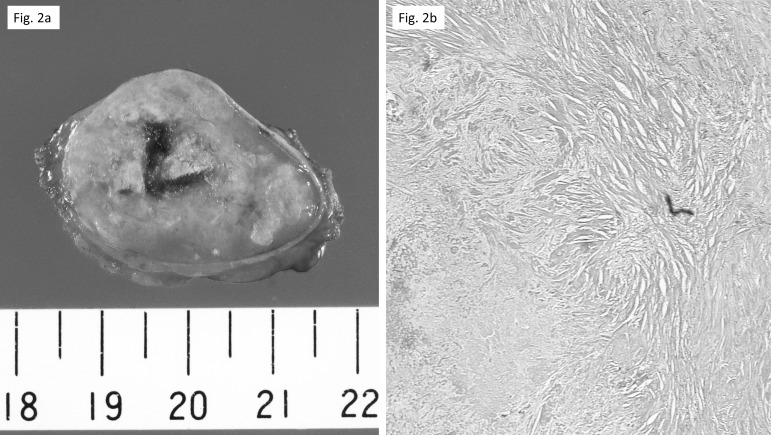
A 61-year-old woman with a history of total hysterectomy for uterine myoma 16 years previously, cesarean delivery 35 years previously, and appendectomy 46 years previously underwent CT because of bloating. The CT scan showed a heterogeneously enhancing tumor measuring 2.3 cm in the left side of the pelvic cavity (Fig. 1a and 1b). FDG-PET/CT imaging subsequently revealed a solitary small focus of increased FDG activity in the pelvis (Fig. 1b and 1c). Tumor markers, including serum carcinoembryonic antigen, CA19-9, and CA-125, were not overexpressed. Colonoscopy was performed and significant findings were not revealed. A diagnosis of gastrointestinal stromal tumor originating in the small intestine or another type of tumor originating in the mesentery (desmoid, schwannoma, or foreign body granuloma) was suspected; therefore, laparoscopic resection was conducted. A white, hard tumor measuring approximately 3 cm was found to originate in the mesentery of the sigmoid colon and adhered slightly to the small intestine. The tumor was successfully resected without cutting into the tumor tissue (Fig. 2a). A histopathologic examination revealed a suture fragment in the center of the tumor with necrotic tissue and bleeding around the fragment. A large number of atypical multinucleated giant cells were found around the foreign body (Fig. 2b). The lesion was therefore thought to be a mass of nodular fibrosis because of the presence of the suture fragment and encapsulated fat necrosis. The final pathologic diagnosis was a suture granuloma. The patient's postoperative course was uneventful, and she was discharged 6 days after surgery.
Fig. 1.
(a and b) CT showed a heterogeneously enhancing tumor measuring 2.3 cm in the left side of the pelvic cavity close to the small intestine (arrow). (c) FDG-PET/CT revealed a solitary small focus of increased FDG activity in the pelvis. The maximum standardized uptake value (SUV) at the focus was 5.5.
Fig. 2.
(a and b) The cut surface of the tumor, measuring 30 × 22 × 25 mm, was pale gray and solid. The histopathologic examination revealed a suture fragment at the center of the tumor, and necrotic tissue with bleeding around the fragment. A large number of atypical multinucleated giant cells were found around the foreign body. The lesion was therefore thought to be a mass of nodular fibrosis because of the presence of the suture fragment and encapsulated fat necrosis.
Discussion
Foreign body materials that induce foreign body reactions include nonabsorbable sutures, surgical sponges, Teflon, and activated charcoal.2,6–9 In such cases, lesions related to the suture are called suture granulomas. The initial reaction of the tissue is a reflection of the amount of injury inflicted by the passage of the needle and sutures. After the initial reaction subsides, the second step occurs in which the suture material causes a specific inflammatory reaction. Nonabsorbable sutures are encapsulated by a rim of connective tissue, whereas histiocytes, giant cells, and lymphocytes are found near the suture line. These findings are most marked with silk and cotton compared with other materials.10
Previous studies have reported that nonabsorption thread is a more frequent cause of suture granulomas than absorption thread.11,12 Moreover, suture granulomas that develop following absorption thread suturing tend to heal after simple drainage within 1 week, whereas those that develop following nonabsorption thread suturing require a longer period of time to heal, necessitating removal of the infected suture materials.11 Therefore, using absorption thread is beneficial for preventing unnecessary surgery.
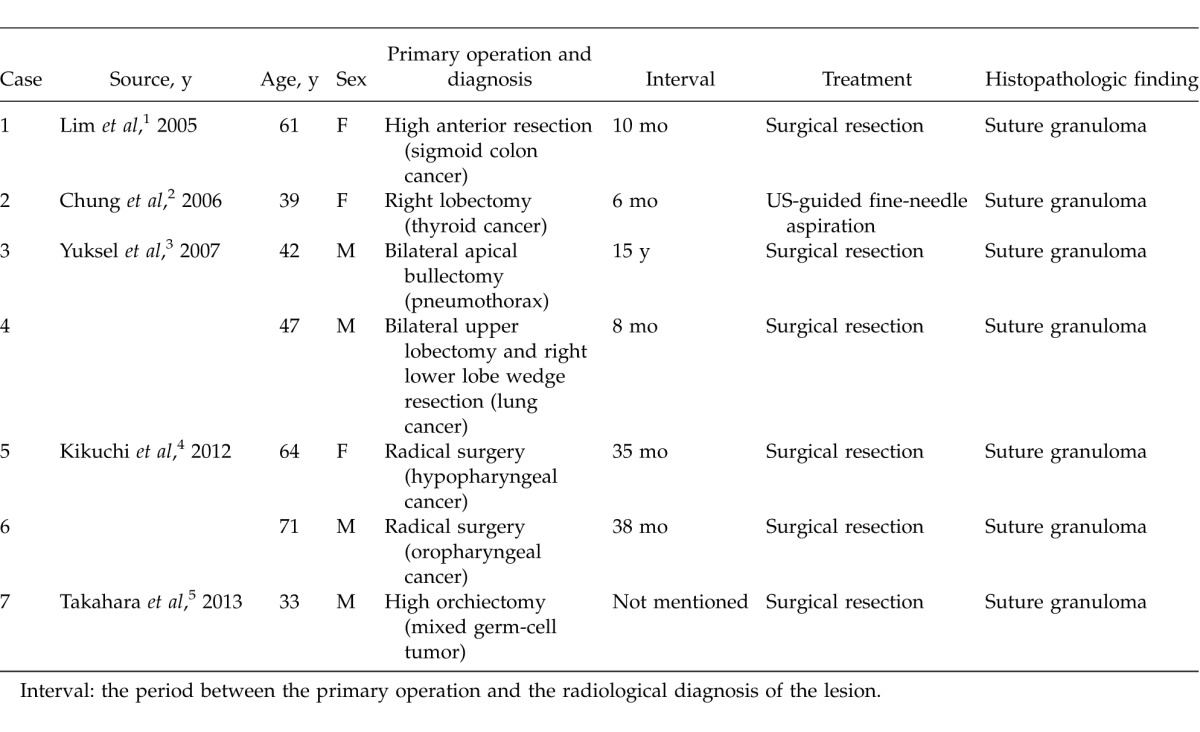
Various modalities are used to diagnose suture granulomas, including US, CT, magnetic resonance imaging, and PET. Although US-guided fine-needle aspiration biopsies are the most useful tool for determining the presence or absence of malignancy,2 in cases of intra-abdominal suture granulomas (not abdominal wall or subcutaneous suture granulomas), it is often difficult to perform aspiration and the lesion must be diagnosed using imaging modalities. In particular, in recent years, PET has been shown to be useful for detecting the presence or absence of malignancy in the field of oncology. On the other hand, a limitation of PET is the detection of false-positive results—for example, in cases of inflammation.13 Based on a literature search of PubMed (using the key words “suture granuloma” and “PET”), 7 cases (5 publications) of suture granulomas associated with false-positive findings on FDG-PET after surgery have been published (Table 1).1–5 Six of these cases occurred after surgery for malignancy, with a time interval between the primary operation and the radiologic diagnosis of the lesion of 6 months to 15 years (median, 10 months). In only 1 case was US-guided fine-needle aspiration performed and follow-up selected in a patient with a diagnosis of suture granuloma; surgical resection was performed in the other cases. In all 7 cases, the diagnoses of suture granulomas could not be made preoperatively. Therefore, it can be said that FDG-PET/CT is not essential for the diagnosis. If malignancy cannot be ruled out with diagnostic imaging and clinical course, an excisional biopsy should be considered.
Table 1.
Previous case reports of suture granuloma with false-positive findings on PET/CT
Although the present patient had no history of malignancy, FDG-PET/CT was positive and it was difficult to perform fine-needle aspiration. Therefore, surgical resection was selected in order to obtain a therapeutic diagnosis. Keeping in mind the potential for malignancy, an excisional biopsy with a negative margin was subsequently performed. There is a single previous report of an intra-abdominal suture granuloma with false-positive findings on FDG-PET/CT1; however, the present case is the first reported case to be treated with laparoscopic resection.
It is difficult to safely perform a biopsy in cases of suture granulomas in the abdominal cavity. Furthermore, false-positive findings on FDG-PET may be obtained because of the presence of inflammation. Therefore, it is necessary to treat such lesions as malignant. On the other hand, anatomic identification can be difficult because of adhesion in patients with a history of abdominal surgery. Although laparoscopic resection is a minimally invasive and ideal procedure in such cases, safe resection with a negative margin is essential, bearing in mind the potential for malignancy.
References
- 1.Lim JW, Tang CL, Keng GH. False positive F-18 fluorodeoxyglucose combined PET/CT scans from suture granuloma and chronic inflammation: report of two cases and review of literature. Ann Acad Med Singapore. 2005;34(7):457–460. [PubMed] [Google Scholar]
- 2.Chung YE, Kim EK, Kim MJ, Yun M, Hong SW. Suture granuloma mimicking recurrent thyroid carcinoma on ultrasonography. Yonsei Med J. 2006;47(5):748–751. doi: 10.3349/ymj.2006.47.5.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yuksel M, Akgul AG, Evman S, Batirel HF. Suture and stapler granulomas: a word of caution. Eur J Cardiothorac Surg. 2007;31(3):563–565. doi: 10.1016/j.ejcts.2006.11.056. [DOI] [PubMed] [Google Scholar]
- 4.Kikuchi M, Nakamoto Y, Shinohara S, Fujiwara K, Tona Y, Yamazaki H, et al. Suture granuloma showing false-positive finding on PET/CT after head and neck cancer surgery. Auris Nasus Larynx. 2012;39(1):94–97. doi: 10.1016/j.anl.2011.04.012. [DOI] [PubMed] [Google Scholar]
- 5.Takahara K, Kakinoki H, Ikoma S, Udo K, Tobu S, Satoh Y, et al. Suture granuloma showing false-positive findings on FDG-PET. Case Rep Urol. 2013;2013:472642. doi: 10.1155/2013/472642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Poyanli A, Bilge O, Kapran Y, Guven K. Case report: foreign body granuloma mimicking liver metastasis. Br J Radiol. 2005;78(932):752–754. doi: 10.1259/bjr/65834078. [DOI] [PubMed] [Google Scholar]
- 7.Kim YK, Park HS. Foreign body granuloma of activated charcoal. Abdom Imaging. 2008;33(1):94–97. doi: 10.1007/s00261-007-9180-x. [DOI] [PubMed] [Google Scholar]
- 8.Yeretsian RA, Blodgett TM, Branstetter BF, 4th, Roberts MM, Meltzer CC. Teflon-induced granuloma: a false-positive finding with PET resolved with combined PET and CT. AJNR Am J Neuroradiol. 2003;24(6):1164–1166. [PMC free article] [PubMed] [Google Scholar]
- 9.Ghersin E, Keidar Z, Brook OR, Amendola MA, Engel A. A new pitfall on abdominal PET/CT: a retained surgical sponge. J Comput Assist Tomogr. 2004;28(6):839–841. doi: 10.1097/00004728-200411000-00019. [DOI] [PubMed] [Google Scholar]
- 10.Postlethwait RW, Willigan DA, Ulin AW. Human tissue reaction to sutures. Ann Surg. 1975;181(2):144–150. doi: 10.1097/00000658-197502000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Iwase K, Higaki J, Tanaka Y, Kondoh H, Yoshikawa M, Kamiike W. Running closure of clean and contaminated abdominal wounds using a synthetic monofilament absorbable looped suture. Surg Today. 1999;29(9):874–879. doi: 10.1007/BF02482778. [DOI] [PubMed] [Google Scholar]
- 12.Nagar H. Stitch granulomas following inguinal herniotomy: a 10-year review. J Pediatr Surg. 1993;28(11):1505–1507. doi: 10.1016/0022-3468(93)90442-n. [DOI] [PubMed] [Google Scholar]
- 13.Strauss LG. Positron emission tomography: current role for diagnosis and therapy monitoring in oncology. Oncologist. 1997;2(6):381–388. [PubMed] [Google Scholar]