Abstract
To evaluate whether, in a sample of patients radically treated for colorectal carcinoma, the preoperative determination of the carcinoembryonic antigen (p-CEA) may have a prognostic value and constitute an independent risk factor in relation to disease-free survival. The preoperative CEA seems to be related both to the staging of colorectal neoplasia and to the patient's prognosis, although this—to date—has not been conclusively demonstrated and is still a matter of intense debate in the scientific community. This is a retrospective analysis of prospectively collected data. A total of 395 patients were radically treated for colorectal carcinoma. The preoperative CEA was statistically compared with the 2010 American Joint Committee on Cancer (AJCC) staging, the T and N parameters, and grading. All parameters recorded in our database were tested for an association with disease-free survival (DFS). Only factors significantly associated (P < 0.05) with the DFS were used to build multivariate stepwise forward logistic regression models to establish their independent predictors. A statistically significant relationship was found between p-CEA and tumor staging (P < 0.001), T (P < 0.001) and N parameters (P = 0.006). In a multivariate analysis, the independent prognostic factors found were: p-CEA, stages N1 and N2 according to AJCC, and G3 grading (grade). A statistically significant difference (P < 0.001) was evident between the DFS of patients with normal and high p-CEA levels. Preoperative CEA makes a pre-operative selection possible of those patients for whom it is likely to be able to predict a more advanced staging.
Key words: Colorectal carcinoma, Preoperative carcinoembryonic antigen, Disease-free survival, Independent prognostic factor
In the world today, more than 1 million cases of patients with colorectal neoplasia are identified each year. Forty percent of these will have a poor prognosis for which targeted therapeutic strategies could most likely be more effective.1–3 For this reason, finding prognostic factors that are early, reliable, and related to the extent of the tumor is of the utmost importance. Among these, the most that are considered even to this day are T and N parameters.1,2,4,5 Less relied upon, however, is the M parameter, which is often understaged due to inadequate pretreatment diagnostic methods.6 However, these parameters, which are available to us only after surgery, do not represent the gold standard. In fact, the prognosis of patients with the same staging is often various and that the need to continually implement ever-changing variables in an already excessively fragmented staging is still present.2,4,7–9
Recently, in light of these needs, great attention has been paid to the study of molecular and genetic markers. At present, these markers still have not found a regular application due to the complexity of their determination, the difficulty of standardization and, last but not least, the low cost-benefit ratio.1,3,4,9,10
With this in mind, in our opinion, the carcinoembryonic antigen (CEA) maintains its position, as for over 30 years it has continued to be the most widely used marker11 and whose validity, with regard to colorectal follow-up, has been sanctioned by leading organizations such as the American Society of Clinical Oncology (ASCO)12 and the European Group on Tumor Markers.13 Moreover, as Herrera14 and Wanebo15 had already reported by the end of the ‘70s, the preoperative determination of the CEA (p-CEA) seems to be related both to the staging of colorectal neoplasia and to the patient's prognosis. However, to date, none of this has been conclusively demonstrated and is still a matter of intense debate both in prestigious scientific journals4,7,11,16–21 as well as in different guidelines.22
The American Society of Clinical Oncology itself, if on the one hand suggests using the determination of the CEA in the preoperative staging thus justifying a worse prognosis when increased,12 on the other, does not validate using the p-CEA in the determination of an adjuvant or neo-adjuvant therapeutic strategy.23
Regarding this issue, we believe it still pertinent to evaluate whether in a sample of patients radically treated for colorectal carcinoma, the determination of the p-CEA may have a prognostic value and constitute an independent risk factor in relation to disease-free survival (DFS).
Methods
This is a retrospective analysis of prospectively collected data from a single department.
We evaluated 395 patients operated on for colorectal adenocarcinoma from January 1, 2000, to December 31, 2009, at the Department of Surgical Sciences, Organ Transplantation and Advanced Technologies at the University of Catania.
All the patients included had undergone radical surgical resection (primary tumor resection and regional lymphadenectomy) performed by surgeons of the same school.
Among the patients who were excluded were those who did not undergo determination of the p-CEA, those whose data were not sufficient for a correct pathological staging, and those with initially metastatic disease. Likewise, those with emergencies (intestinal obstruction or perforation), those with synchronous malignancies in different staging, those who had undergone neo-adjuvant radio-chemotherapy, and those with impaired hepatic and/or kidney function were not included in our evaluation.
The determination of the p-CEA levels has always been performed in our laboratory through the electrochemiluminescence (ECL), using Roche Diagnostics reagents and a commercial analyzer (Elecsys 2010; Roche Diagnostics, Basel, Switzerland). The cutoff value was 5 ng/mL, in agreement with what had been reported in other experiences.10,24
The samples used to determine the p-CEA levels were obtained from peripheral venous blood drawn in the days immediately prior to surgery after obtaining consent from the patient.
Patients already classified according to Astler-Coller were restaged according to the Seventh Edition of TNM Staging System of the American Joint Committee on Cancer (AJCC) in 2010.25 After surgery, all patients were advised to undergo a planned follow-up that included quarterly checks until the third postoperative year, bi-annual checks until the fifth year, and annual checks until the tenth year according to a previously published protocol.26 Only 4.05% (16/395) of patients decided not to undergo such a follow-up ab initio. The purpose of the follow-up was to determine DFS (i.e., the time elapsed between radical surgery and locoregional relapse and/or distant metastases).
The follow-ups were assessed up to December 31, 2012.
In our group of patients, we evaluated: p-CEA versus tumor staging according to the AJCC 2010 (stage 0–I, stage II, stage III); p-CEA versus T (T1, T2, T3, T4) and N parameters (N0, N1a+b; N2a+b) of the tumor; and p-CEA versus degree of differentiation (well differentiated + moderately differentiated versus undifferentiated) of the tumor.
We then performed a univariate analysis between DFS and the factors that we thought could be of influence, such as the age and sex of the patient, the p-CEA, p-CEA >5 ng/mL, CEA >5 ng/mL at the first postoperative control at 3 months, staging according to the AJCC 2010, the T parameter according to the AJCC 2010, the N parameter according to the AJCC 2010, the degree of differentiation of the tumor (G1+2, G3), the number of lymph nodes sampled by the pathologist, the number of lymph nodes less than or >12 and finally whether patients were undergoing chemotherapy or not. Then we performed a multivariate analysis of the factors that reached statistical significance on univariate analysis to identify independent predictors of DFS.
Once these were identified, we then evaluated the overall DFS, the DFS in patients with normal p-CEA versus patients with high p-CEA and DFS of patients in whom the CEA fell within normal limits after surgery versus those patients in which the CEA levels were high on the first postoperative check-up (3 months).
Statistical analysis was performed using commercial software (SPSS for Windows, version 15.0, SPSS, Inc, Chicago, Illinois). Data were checked for normality before a statistical analysis with the Kolmogorov-Smirnov test. Continuous variables are presented as mean ± SD if normally distributed, otherwise as a median and interquartile range. Categorical variables are presented as absolute numbers and/or percentages.
Normally distributed continuous variables were compared using the unpaired t-test, whereas the Mann-Whitney U test was used for those variables that were not normally distributed. Categorical variables were analyzed using either the χ2 test or Fischer's exact test, where appropriate.
All parameters recorded in our database were tested for the relationship with DFS with a binary logistic regression analysis. To avoid overfitting, only factors being significantly associated (P < 0.05) with the main outcome were used to build multivariate stepwise forward logistic regression models to establish their independent predictors. To avoid multicollinearity, variables affected by mathematical coupling were separately entered into different models. In cases of intercorrelation, the best single independent variable was chosen.
Disease-free survival in different subgroups of patients was assessed with the Kaplan-Meier survival analysis. Comparison between groups was evaluated with the log-rank test.
For all statistical tests, a P value <0.05 was considered significant.
Results
The average age of the 395 patients was 68 (interquartile range, 61–74 years); 223 were male (56.46%) and 172 were female (43.54%).
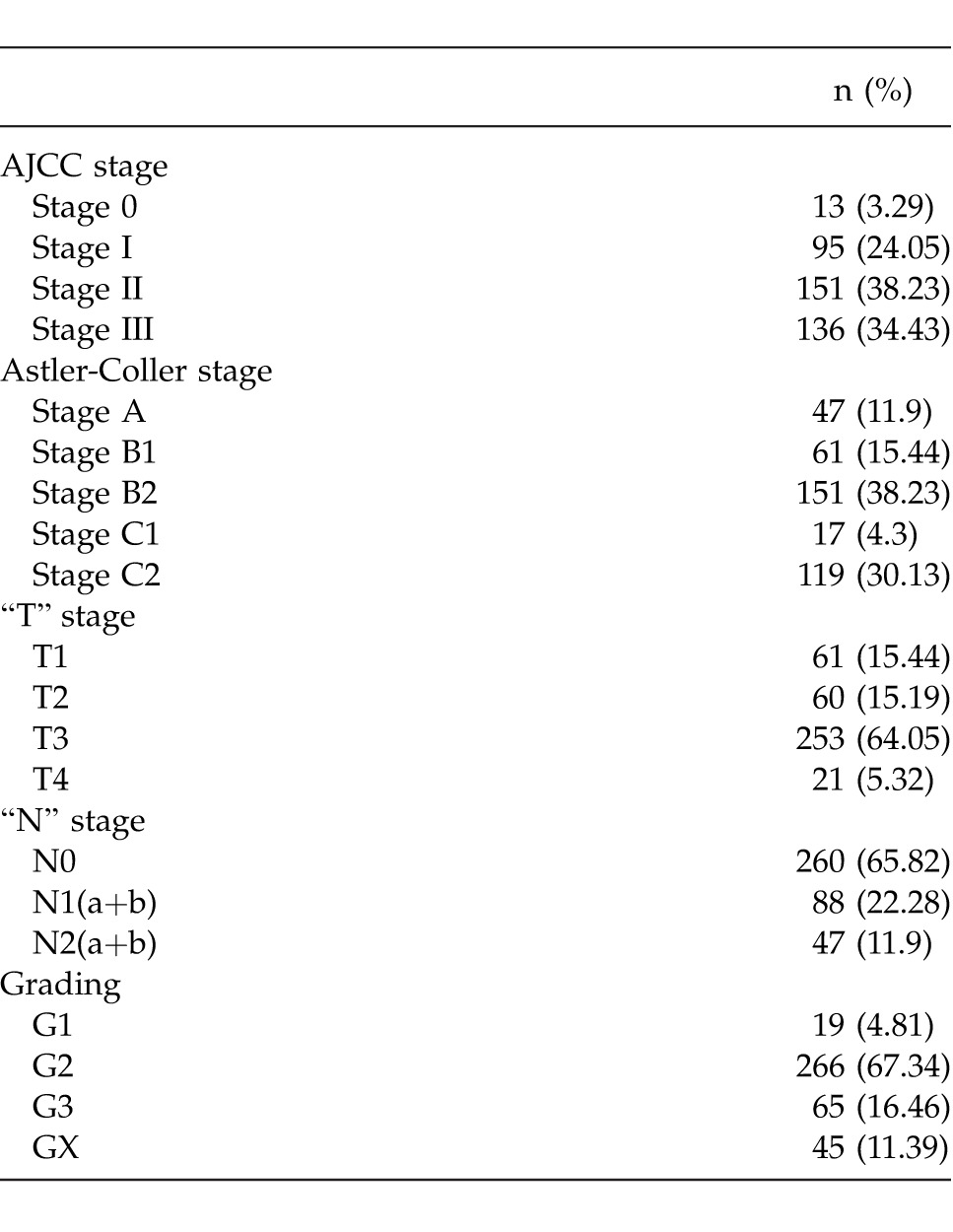
Colorectal adenocarcinoma was located in 29.11% (115/395) in the ascending colon included the right colic flexure, 2.03% in the transverse colon (8/395); 28.61% (113/395) in the descending colon included the left colic flexure and the sigmoid colon; 36.96% (146/395) in the rectum. In 3.29% (13/395), the neoplasia was synchronous but with the same staging. Table 1 shows the staging of the patients according to the AJCC 2010 classification, Astler-Coller, T and N parameters, and lastly the degree of differentiation.
Table 1.
Classification according to AJCC stage, Astler-Collers stage, “T” and “N” stage according AJCC and grading (395 patients)
The average number of sampled lymph nodes was 15.39 (0–77); for 57.22% (226 patients), it was ≥12; for 42.78% (169 patients), it was <12.
The average p-CEA levels were 7.51 ng/mL (0–157.6 ng/mL). In 27.34% of the patients (108/395), the p-CEA levels exceeded the normal range (≤5 ng/mL) reaching an average value of 21.53 ng/mL (5.2–157.6 ng/mL).
In 86.5% (90/104) of the patients, the postoperative CEA levels during the first post-surgery checkup (3 months) were within normal range; meanwhile, in the remaining 14 patients (13.5%) the 3-month levels were high (average value 26.85 ng/mL; range, 6.6–141.5 ng/mL).
Table 2 shows the correlation between the p-CEA and the AJCC staging.
Table 2.
Relationship between p-CEA and AJCC 2010 stage (395 patients)
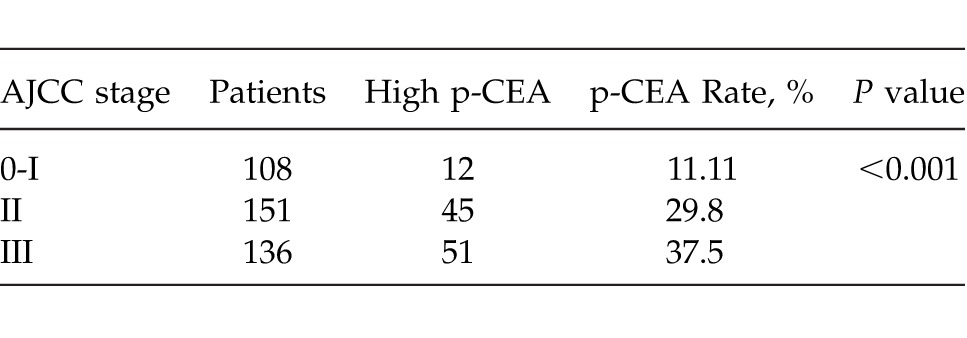
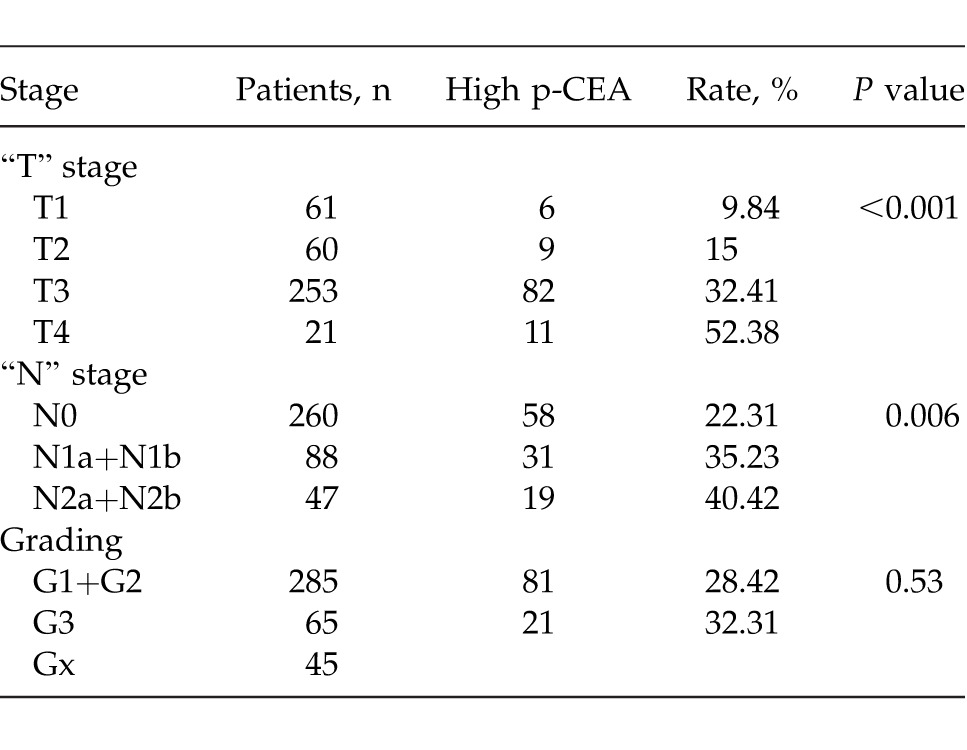
Table 3 shows the correlation between the p-CEA and T and N parameters and grading.
Table 3.
Relationship between p-CEA and “T” stage and “N” stage according AJCC 2010 and grading (395 patients)
Among the patients who had undergone adjuvant chemotherapy, 58.82% (80/136) were at stage III, 35.76% (54/152) were at stage II and only 5.26% (5/95) were at stage I. Reasons why the treatment was not performed were: favorable staging, patient refusal, advanced age, presence of comorbidities.
Table 4 shows the factors that on a univariate analysis had a statistically significant correlation with DFS.
Table 4.
Univariate analysis (variables correlated in a statistically significant way to the DFS)
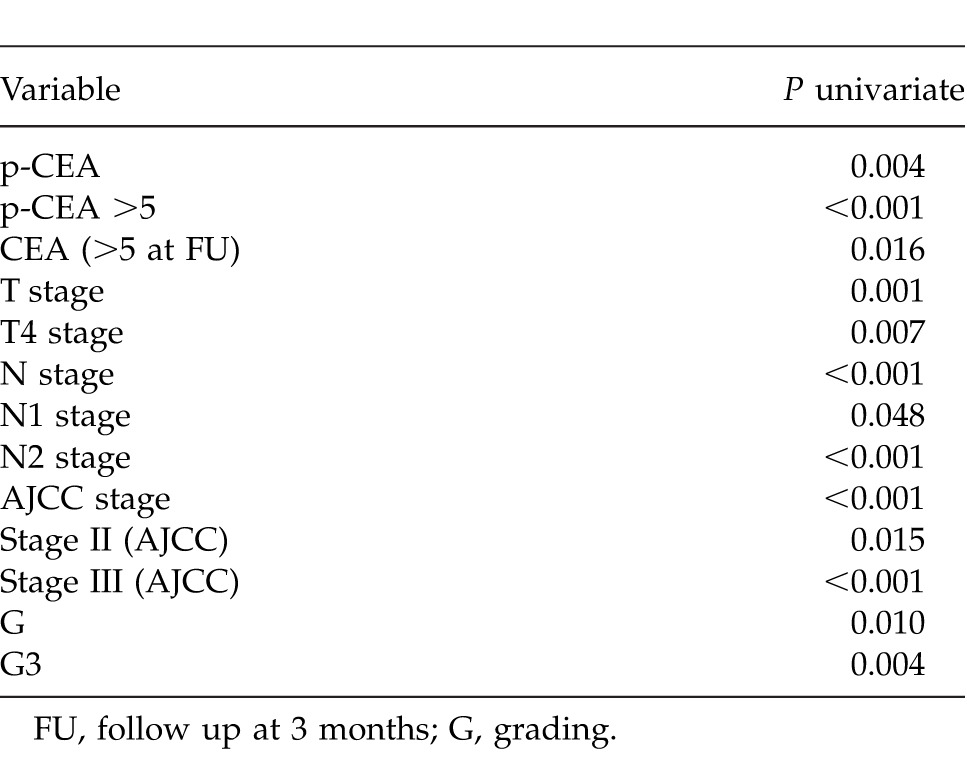
Table 5 shows independent predictor factors of DFS in a multivariate analysis.
Table 5.
Multivariate analysis between independent predictors of DFS in univariate analysis.
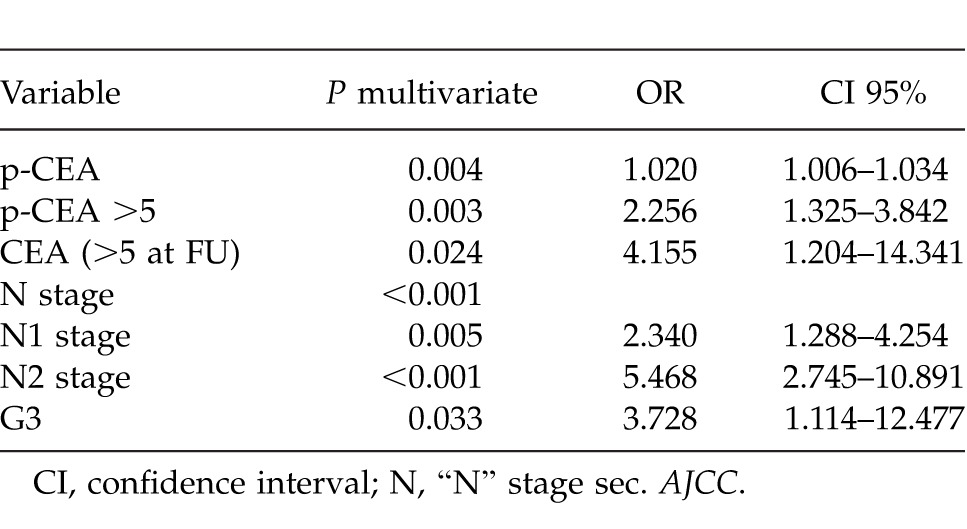
In particular, preoperative CEA concentrations gave a 2% incremental risk of recurrence of malignancy per each unit increase (OR 1.020, P = 0.004), whereas preoperative CEA concentrations >5 ng/mL gave a 2.256-fold absolute risk (P = 0.003).
Preoperative N staging was also a risk factor, especially in stage N2 and N3. On the other hand, only a G3 grading was independently correlated to the recurrence of malignancy.
Furthermore, the presence of still elevated CEA concentrations >5 ng/mL after surgery was an independent predictor factor of recurrence, with an OR of 4.155 (P = 0.024).
Out of 395 patients, 379 had agreed upon the postoperative follow-up.
The median follow-up of the 379 patients was 61 months (interquartile range, 23–106 months). Figure 1 shows overall DFS of the 379 patients undergoing follow-up.
Fig. 1.
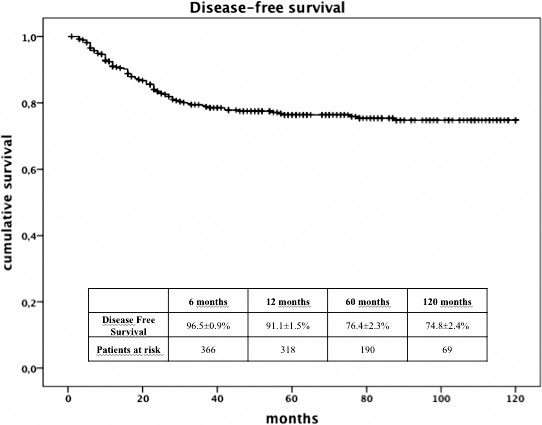
Overall disease-free survival.
Figure 2 shows a comparison between the DFS of patients with normal p-CEA levels (274 patients) and the DFS of patients with high p-CEA levels (105 patients) who had undergone follow-up. When patients were divided into two groups according to preoperative CEA concentrations, patients with preoperative CEA >5 ng/ml showed a significantly lower DFS (P < 0.001; Fig. 2).
Fig. 2.
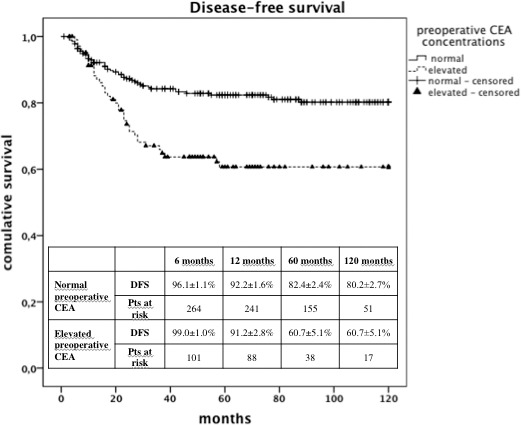
Disease-free survival: patients with normal p-CEA versus patients with p-CEA >5 ng/mL.
Figure 3 shows the comparison between the DFS of patients with high p-CEA levels which fell within normal in the first postoperative scheduled visit (91 patients) and the DFS of patients with high p-CEA levels which did not fall within normal in the first postoperative scheduled visit (14 patients). When patients with preoperative CEA >5 ng/mL were considered, a significantly better DFS was observed in those patients who had normalized CEA concentrations postoperatively (P < 0.001; Fig 3).
Fig. 3.
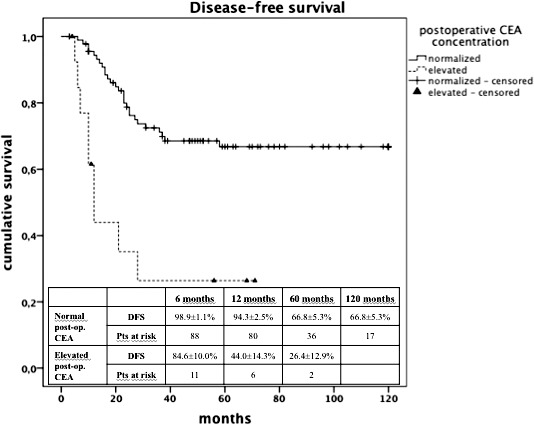
Disease-free survival: patients with normal postoperative CEA versus patients with high postoperative CEA (3 months).
Discussion
“Carcinoembryonic antigen is the most widely used tumor marker in patients with colorectal cancer.”11 These observations, which were made as recently as 2013 and which still seem surprising after 30 years, are certainly not due to the lack of testing new molecular, genetic, or humoral markers, but to the fact that these are not reliable, simple, nor cost effective as the CEA could be. In recent years, we are not the only ones1,3,4,6,7,10,11,16,18,19,27–29 who believe that the determination of the p-CEA has a prognostic value in identifying, preoperatively, the group of patients who most likely will show recurrences. In fact, p-CEA is able to identify both patients whose understaging results from occult metastasis and those who are carriers of histologically advanced or more aggressive neoplasms.
Identifying these individuals would not be mere speculation, but would allow one to pinpoint those patients who, even with a less advanced staging, would further benefit from a more aggressive treatment. Even Fong,30 albeit in a more specific field, includes the p-CEA in the 5 necessary parameters for the prognostic classification of those patients undergoing hepatic resection for metastatic colorectal cancer. This approach finds its biological basis in the fact that the carcinoembryonic antigen appears to have a role both in fostering the uncontrolled growth of the tumor and in facilitating its invasion and metastasis.10,20,31 However, not all seem to agree with such an approach nor have they become aware of one, if it is true that the determination of p-CEA in a patient with colorectal neoplasia varies in literature between 45 and 88%.22,31
In our sample, only 27.34% of the patients with colorectal cancer showed high p-CEA levels. This finding has allowed us to confirm that the determination of the p-CEA cannot serve as a means of screening. Even from a review of the literature, an increase of the preoperative marker is recorded in only a third of patients suffering from this cancer. This seems to be due to the fact that, although over 90% of colorectal cancers produce the antigen, this is catabolized in its first passage through the liver.5,9,11 For this reason, we have excluded all patients with clinical and instrumental evidence of liver disease from our research.
In our experience, as also reported by other authors,6,19,20,32,33 the determination of p-CEA is statistically significantly related to both the AJCC 2010 staging used to restage our patients (P < 0.001; Table 2) and the T and N histological parameters (P < 0.001 and P = 0.006, respectively; Table 3). This would allow for a selection of that group of patients for whom a more probable advanced histological staging can already be preoperatively expected, and thus it would enable us to setup, already intra-operatively, those medical treatments justified only in such circumstances. Intraportal chemotherapy, for example, does not seem to give significant results when applied indiscriminately to all patients treated for colorectal neoplastic disease. It does, however, seem to be most useful when selectively applied to patients with worse prognoses.34 In this field,8,10,11,20,24 some authors add a further element reporting conflicting information in the literature with regard to the increase in p-CEA levels which could forecast a worse prognosis in more advanced stages (Dukes' C or TNM stage III), according to some authors, or in less advanced ones (Dukes' B or TNM stage II) according to others.
Oddly despite a correlation between p-CEA and staging, and T and N parameters of the cancer such correlation was not recorded for the grading. In our records, indeed, the impact of patients with high p-CEA levels is almost similar among both the patients with undifferentiated tumors and those with well-differentiated or moderately differentiated tumors (P = 0.53; Table 3), although the poorly differentiated tumor (G3) is an independent prognostic factor for DFS (Table 5). While there are some authors in literature who agree with this figure,20,24 others refuse to accept it.1
Some authors20 recently report that the idea of the p-CEA being an independent prognostic factor for DFS is controversial. The study of our data shows that if univariate analysis (Table 4) has pointed out 13 factors as being associated with DFS when studied in a multivariate model (Table 5), only the p-CEA >5 ng/mL, the presence of metastatic lymph nodes, and the low degree of differentiation were independent variables. Among these, the risk of relapse possible with a p-CEA >5 ng/mL is similar to the risk of relapse in patients with N1 stage according to AJCC classification, which are the ones with up to 3 neoplastic lymph-nodes at the postoperative histological exam. With regard to the p-CEA and the multivariate analysis, other authors5,8,20,27,35 report similar results.
In light of these data on the p-CEA, we could calculate a significantly lower DFS (P < 0.001) for patients who had a preoperative increase of CEA over 5 ng/mL compared with those with p-CEA within normal range (Fig. 2).
Many authors4,5,9,19,22,32 have reported that the lack of return of the CEA to normal range after radical surgical resection, given the short half-life marker, is an index of both inadequate resection leading to early recurrence or presence of mostly hepatic occult metastases. In our study, we recorded that in 13.5% of the cases, a percentage noticeably lower than that reported by other authors,32 the p-CEA did not fall within normal range after 3 months after a surgery judged as radical. The disease-free surgery in these patients was statistically significantly worse (P < 0.001) compared with the patients who registered instead of postoperative tumor marker normalization (Fig. 3). Moreover, a multivariate analysis shows (Table 5) that the risk of relapse related to CEA which remains high in postoperative cases is only slightly lower than that of patients staged N2 according to the AJCC classification, who have at least 4 histologically malignant nodes.
It must be considered that, in our series, with regard to the N parameter, the number of sampled lymph nodes in 42.78% of the cases was lower than 12. This number, though in the context of an issue still unresolved,36 has been considered the minimum for a correct staging of the tumor. Currently data similar to ours has been reported in literature if it is true that in the US reports published between 2005 and 2010 revealed that lymphadenectomy was still considered inadequate in 48 to 63% of cases.37,38 Similarly in Germany in 2009, the Dutch Surgical Colorectal Audit39 reported that in 73% of colon cancers and 58% of rectum cancers, the number of lymph nodes examined was ≤10.
Lastly in England, Johnson40 and Mitchell41 have recently pointed out that the limit of 12 nodes was not reached between 33 and 50% of colorectal cancer cases. In view of these data, we deem it reasonable to say that the value of p-CEA acquires further importance.
This study could supposedly carry a limitation in the fact that smoking was not considered a variable that could affect the value of the CEA. It must be said, however, that most of the mentioned authors1,3–5,9,10,19,21,24,27,29,32,35 do not consider this variable in their clinical cases and that the only author20 referring to it claim it has no impact on the CEA levels.
A second bias could be the quantity of case studies that might seem too widespread. However, we have been able to create a homogenous and single-center study group, surgically treated by the same team and checked throughout a long follow-up, always scheduled with the same timing and diagnostic modalities.
If on the one hand, Goldstein42 said: “no studies have shown benefit from specific treatment planning based solely on preoperative CEA measurement,” the ASCO,43 on the other hand, suggests an adjuvant treatment for stage II patients radically treated for colorectal cancer only with “high risk.” We believe that our data on p-CEA, along with data from other previously mentioned authors, can help in the stratification of patients with high risk of relapse, even independently from an advanced staging,5,6,29,44 who can benefit most from both intra- or postoperative adjuvant therapies and tighter controls.
Acknowledgments
The authors alone are responsible for the content and writing of the paper.
References
- 1.Mehrkhani F, Nasiri S, Donboli K, Meysamie A, Hedayat A. Prognostic factors in survival of colorectal cancer patients after surgery. Colorectal Dis. 2009;11(2):157–161. doi: 10.1111/j.1463-1318.2008.01556.x. [DOI] [PubMed] [Google Scholar]
- 2.Weiser MR, Landmann RG, Kattan MW, Gonen M, Shia J, Chou J, et al. Individualized prediction of colon cancer recurrence using a nomogram. J Clin Oncol. 2008;26(3):380–385. doi: 10.1200/JCO.2007.14.1291. [DOI] [PubMed] [Google Scholar]
- 3.Peng JJ, Cai SJ, Lu HF, Cai GX, Lian P, Guan ZQ, et al. Predicting prognosis of rectal cancer patients with total mesorectal excision using molecular markers. World J Gastroenterol. 2007;13(21):3009–3015. doi: 10.3748/wjg.v13.i21.3009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee WS, Baek JH, Kim KK, Park YH. The prognostic significant of percentage drop in serum CEA post curative resection for colon cancer. Surg Oncol. 2012;21(1):45–51. doi: 10.1016/j.suronc.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 5.Ogata Y, Murakami H, Sasatomi T, Ishibashi N, Mori S, Ushijima M, et al. Elevated preoperative serum carcinoembrionic antigen level may be an effective indicator for needing adjuvant chemotherapy after potentially curative resection of stage II colon cancer. J Surg Oncol. 2009;99(1):65–70. doi: 10.1002/jso.21161. [DOI] [PubMed] [Google Scholar]
- 6.El-Awady S, Lithy R, Morshed M, Khafagy W, Abd Monem H, Waleed O, et al. Utility of serum preoperative carcinoembryonic antigen in colorectal cancer patients. Hepatogastroenterology. 2009;56(90):361–366. [PubMed] [Google Scholar]
- 7.Chen L, Jiang B, Wang Z, Liu M, Yang H, Xing J, et al. Combined preoperative CEA and CD44v6 improves prognostic value in patients with stage I and stage II colorectal cancer. Clin Transl Oncol. 2014;16(3):285–292. doi: 10.1007/s12094-013-1069-2. [DOI] [PubMed] [Google Scholar]
- 8.Jeon BG, Shin R, Chung JK, Jung IM, Heo SC. Individualized cutoff value of the preoperative carcinoembryonic antigen level is necessary for optimal use as a prognostic marker. Ann Coloproctol. 2013;29(3):106–114. doi: 10.3393/ac.2013.29.3.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim JY, Kim NK, Sohn SK, Kim YW, Kim KJ, Hur H, et al. Prognostic value of postoperative CEA clearance in rectal cancer patients with high preoperative CEA levels. Ann Surg Oncol. 2009;16(10):2771–2778. doi: 10.1245/s10434-009-0651-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Szynglarewicz B, Matkowski R, Forgacz J, Pudelko M, Smorag Z, Dryl J, et al. Clinical factors in prediction of prognosis after anterior resection with total mesorectal excision for carcinoma of the rectum. Oncol Rep. 2007;17(2):471–475. [PubMed] [Google Scholar]
- 11.Huh JW, Kim CH, Lim SW, Kim HR, Kim YJ. Factors predicting long-term survival in colorectal cancer patients with a normal preoperative serum level of carcinoembryonic antigen. J Cancer Res Clin Oncol. 2013;139(9):1449–1455. doi: 10.1007/s00432-013-1459-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Compton C, Fenoglio-Preiser CM, Pettigrew N, Fielding LP. American Joint Committee on Cancer Prognostic Factors Consensus Conference: Colorectal Working Group. Cancer. 2000;88(7):1739–1757. doi: 10.1002/(sici)1097-0142(20000401)88:7<1739::aid-cncr30>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 13.Duffy MJ, van Dalen A, Haglund C, Hansson L, Holinski-Feder E, Klapdor R, et al. Tumour markers in colorectal cancer: European Group on Tumour Markers (EGTM) guidelines for clinical use. Eur J Cancer. 2007;43(9):1348–1360. doi: 10.1016/j.ejca.2007.03.021. [DOI] [PubMed] [Google Scholar]
- 14.Herrera MA, Chu TM, Holyoke ED. Carcinoembryonic antigen (CEA) as a prognostic and monitoring test in clinically complete resection of colorectal carcinoma. Ann Surg. 1976;183(1):5–9. doi: 10.1097/00000658-197601000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wanebo HJ, Rao B, Pinsky CM, Hoffman RG, Stearns M, Schwartz MK, et al. Preoperative carcinoembryonic antigen level as a prognostic indicator in colorectal cancer. N Engl J Med. 1978;299(9):448–451. doi: 10.1056/NEJM197808312990904. [DOI] [PubMed] [Google Scholar]
- 16.Jeon BG, Shin R, Chung JK, Jung IM, Heo SC. Individualized cutoff value of the preoperative carcinoembryonic antigen level is necessary for optimal use as a prognostic marker. Ann Coloproctol. 2013;29(3):106–114. doi: 10.3393/ac.2013.29.3.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Keum MA, Lim SB, Kim SA, Yoon YS, Kim CW, Yu CS, et al. Clinicopathologic factors affecting recurrence after curative surgery for stage I colorectal cancer. J Korean Soc Coloproctol. 2012;28(1):49–55. doi: 10.3393/jksc.2012.28.1.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Basbug M, Arikanoglu Z, Bulbuller N, Cetinkaya Z, Aygen E, Akbulut S, et al. Prognostic value of preoperative CEA and CA 19-9 levels in patients with colorectal cancer. Hepatogastroenterology. 2011;58(106):400–405. [PubMed] [Google Scholar]
- 19.Søreide K, Søreide JA, Kørner H. Prognostic role of carcinoembryonic antigen is influenced by microsatellite instability genotype and stage in locally advanced colorectal cancers. World J Surg. 2011;35(4):888–894. doi: 10.1007/s00268-011-0979-9. [DOI] [PubMed] [Google Scholar]
- 20.Huh JW, Oh BR, Kim HR, Kim YJ. Preoperative carcinoembryonic antigen level as an independent prognostic factor in potentially curative colon cancer. J Surg Oncol. 2010;101(5):396–400. doi: 10.1002/jso.21495. [DOI] [PubMed] [Google Scholar]
- 21.Hatano S, Ishida H, Ishibashi K, Kumamoto K, Haga N, Miura I. Identification of risk factors for recurrence in high-risk stage II colon cancer. Int Surg. 2013;98(2):114–121. doi: 10.9738/CC131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kosmider S, Stella DL, Field K, Moore M, Ananda S, Oakman C, et al. Preoperative investigations for metastatic staging of colon and rectal cancer across multiple centres–what is current practice? Colorectal Dis. 2009;11(6):592–600. doi: 10.1111/j.1463-1318.2008.01614.x. [DOI] [PubMed] [Google Scholar]
- 23.Locker GY, Hamilton S, Harris J, Jessup JM, Kemeny N, Macdonald JS, et al. ASCO 2006 update of recommendations for the use of tumor markers in gastrointestinal cancer. J Clin Oncol. 2006;24(33):5313–5327. doi: 10.1200/JCO.2006.08.2644. [DOI] [PubMed] [Google Scholar]
- 24.Boonpipattanapong T, Chewatanakornkul S. Preoperative carcinoembryonic antigen and albumin in predicting survival in patients with colon and rectal carcinomas. J Clin Gastroenterol. 2006;40(7):592–595. doi: 10.1097/00004836-200608000-00006. [DOI] [PubMed] [Google Scholar]
- 25.Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A. American Joint Committee On Cancer Staging Manual. 7th ed. New York, NY: Springer; 2010. p. 9. [Google Scholar]
- 26.Li Destri G, Di Cataldo A, Puleo S. Colorectal cancer follow-up: useful or useless? Surg Oncol. 2006;15(1):1–12. doi: 10.1016/j.suronc.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 27.Katoh H, Yamashita K, Kokuba Y, Satoh T, Ozawa H, Hatate K, et al. Diminishing impact of preoperative carcinoembryonic antigen (CEA) in prognosis of Dukes' C colorectal cancer. Anticancer Res. 2008;28((3B)):1933–1941. [PubMed] [Google Scholar]
- 28.Yeh CY, Hsieh PS, Chiang JM, Lai CC, Chen JS, Wang JY, et al. Preoperative carcinoembryonic antigen elevation in colorectal cancer. Hepatogastroenterology. 2011;58(109):1171–1176. doi: 10.5754/hge10564. [DOI] [PubMed] [Google Scholar]
- 29.Quah HM, Chou JF, Gonen M, Shia J, Schrag D, Landmann RG, et al. Identification of patients with high-risk stage II colon cancer for adjuvant therapy. Dis Colon Rectum. 2008;51(5):503–537. doi: 10.1007/s10350-008-9246-z. [DOI] [PubMed] [Google Scholar]
- 30.Fong Y, Fortner J, Sun RL, Brennan MF, Blumgart LH. Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg. 1999;230(3):318–321. doi: 10.1097/00000658-199909000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thirunavukarasu P, Sukumar S, Sathaiah M, Mahan M, Pragatheeshwar KD, Pingpank JF, et al. C-stage in colon cancer: implications of carcinoembryonic antigen biomarker in staging, prognosis, and management. J Natl Cancer Inst. 2011;103(8):689–697. doi: 10.1093/jnci/djr078. [DOI] [PubMed] [Google Scholar]
- 32.Lin JK, Lin CC, Yang SH, Wang HS, Jiang JK, Lan YT, et al. Early postoperative CEA level is a better prognostic indicator than is preoperative CEA level in predicting prognosis of patients with curable colorectal cancer. Int J Colorectal Dis. 2011;26(9):1135–1141. doi: 10.1007/s00384-011-1209-5. [DOI] [PubMed] [Google Scholar]
- 33.Filiz AI, Sucullu I, Kurt Y, Karakas DO, Gulec B, Akin ML. Persistent high postoperative carcinoembryonic antigen in colorectal cancer patients–is it important? Clinics (Sao Paulo) 2009;64(4):287–294. doi: 10.1590/S1807-59322009000400004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li Destri G, Lanteri R, Santangelo M, Torrisi B, Di Cataldo A, Puleo S. Can biliary carcinoembryonic antigen identify colorectal cancer patients with occult hepatic metastases? World J Surg. 2006;30(8):1494–1499. doi: 10.1007/s00268-005-0698-1. [DOI] [PubMed] [Google Scholar]
- 35.Heinzerling JH, Anthony T, Livingston EH, Huerta S. Predictors of distant metastasis and mortality in patients with stage II colorectal cancer. Am Surg. 2007;73(3):230–238. [PubMed] [Google Scholar]
- 36.Li Destri G, Di Carlo I, Scilletta R, Scilletta B, Puleo S. Colorectal cancer and lymph nodes: the obsession with the number 12. World J Gastroenterol. 2014;20(8):1951–1960. doi: 10.3748/wjg.v20.i8.1951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Carriquiry LA. More is not always better. World J Surg. 2011;35(12):2804–2805. doi: 10.1007/s00268-011-1283-4. [DOI] [PubMed] [Google Scholar]
- 38.Nathan H, Shore AD, Anders RA, Wick EC, Gearhart SL, Pawlik TM. Variation in lymph node assessment after colon cancer resection: patient, surgeon, pathologist, or hospital? J Gastrointest Surg. 2011;15(3):471–479. doi: 10.1007/s11605-010-1410-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kuijpers CC, van Slooten HJ, Schreurs WH, Moormann GR, Abtahi MA, Slappendel A, et al. Better retrieval of lymph nodes in colorectal resection specimens by pathologists' assistants. J Clin Pathol. 2013;66(1):18–23. doi: 10.1136/jclinpath-2012-201089. [DOI] [PubMed] [Google Scholar]
- 40.Johnson A, Rees JR, Schwenn M, Riddle B, Verrill C, Celaya MO, et al. Oncology care in rural Northern New England. J Oncol Pract. 2010;6(2):81–89. doi: 10.1200/JOP.200015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mitchell PJ, Ravi S, Grifftiths B, Reid F, Speake D, Midgley C, et al. Multicentre review of lymph node harvest in colorectal cancer: are we understaging colorectal cancer patients? Int J Colorectal Dis. 2009;24(8):915–921. doi: 10.1007/s00384-009-0697-z. [DOI] [PubMed] [Google Scholar]
- 42.Goldstein MJ, Mitchell EP. Carcinoembryonic antigen in the staging and follow-up of patients with colorectal cancer. Cancer Invest. 2005;23(4):338–351. doi: 10.1081/cnv-58878. [DOI] [PubMed] [Google Scholar]
- 43.Benson AB, III, Schrag D, Somerfield MR, Cohen AM, Figueredo AT, Flynn PJ, et al. American society of clinical oncology recommendations on adjuvant chemotherapy for stage II colon cancer. J Clin Oncol. 2004;22(16):3408–3419. doi: 10.1200/JCO.2004.05.063. [DOI] [PubMed] [Google Scholar]
- 44.Uehara M, Manaka D, Baba S, Oji Y, Hirata K, Shimizu M, et al. Prognostic study of preoperative serum levels of CEA and CA 19-9 in colorectal cancer. Gan To Kagaku Ryoho. 2007;34(9):1413–1417. [PubMed] [Google Scholar]


