Abstract
The aim of this study was to present our 20-year experience regarding primary hyperparathyroidism (PHPT). PHPT patients who underwent parathyroidectomy in our clinic were reviewed retrospectively. There were 190 PHPT patients, of whom 137 were asymptomatic (72%). The mean serum calcium at the time of diagnosis was 11.9 ± 2.2 mg/dL. The mean parathyroid hormone (PTH) level was 467 ± 78 pg/mL. Ultrasonography (USG) identified all abnormal glands accurately (82.6%) and Technetium-99m sestamibi scintigraphy (MIBI) was used in 89.4% of the patients and magnetic resonance imaging (MRI) in 61%. The common use of USG and MIBI detected 92% of the lesions. Bilateral neck exploration (BNE) was performed in 12.2% of the patients and focused unilateral neck exploration (FUNE) in the remaining 87.8%. Surgical intervention was unsuccessful in 1 patient (0.5%). The conversion ratio from FUNE to BNE was 5.2%. The mean operation time and mean hospital stay decreased significantly in patients with FUNE. Pathologic examination revealed single adenoma in 93% of the patients. New imaging techniques result in the conversion of surgical treatments of PHPT. FUNE in parathyroidectomy performed by an experienced surgeon may provide successful treatment rates.
Key words: Primary hyperparathyroidism, Focused surgical neck exploration, Developing country
Primary hyperparathyroidism (PHPT) is defined as hypercalcemia with an excessive, uncontrolled parathyroid hormone (PTH) secretion by 1 or more parathyroid glands in the absence of secondary or tertiary factors. In some cases, normocalcemia can be present with osteopenia and vitamin-D deficiency, and normal PTH can occur with high markers of bone formation and bone resorption. The prevalence varies between 1 or 2 people out of 1000 in the USA and the incidence varies between 27 and 30 people out of 100,000 per year, according to the population and research methods.1–3
The first parathyroidectomy was performed in 1924 by Mandl with the exploration of 4 parathyroid glands and excision of an enlarged single parathyroid adenoma.4 This operation was followed by the discovery of parathormone and the development of many measurement methods of PTH.5 In the last 30 years, the wide use of the multichannel autoanalyzer; use of USG, MIBI, computed tomography (CT), and MRI for the diagnosis of PHPT; and new surgical methods and techniques for the surgical treatment of PHPT have resulted in easier diagnosis of the disease, correct localization of pathologic lesions, and different surgical approaches.1,5–17
The aim of this study was to present our 20-year-experience with 190 patients diagnosed with PHPT, their clinical features, diagnostic methods, surgical treatment and pathology, and review of the literature.
Materials and Methods
A retrospective and descriptive study of patients with PHPT undergoing parathyroidectomy in the Department of Surgery, Karadeniz Technical University Farabi Hospital between January 1993 and January 2013 was carried out. Patients with recurrent primary hyperparathyroidism, and secondary and tertiary hyperparathyroidism were excluded. The local ethics committee confirmed that formal approval was not required for this retrospective audit of practice.
All patients with PHPT were referred to surgery from our Endocrinology and Metabolism Department in the same hospital. All related medical data including demographic data, clinical presentations, comorbidities, localizations of abnormal parathyroid glands, operations and their findings, and pathology and complications were reviewed. Demographic data consisted of age, sex, and other diagnoses.
Data on blood chemistry included preoperative and postoperative serum calcium, phosphate, alkaline phosphatase, creatinine, and intact PTH. Postoperative blood chemistry continued to be collected for 12 months. Imaging modalities for localization and their accuracy when comparing surgical findings were noted. USG was performed by 2 academically-experienced radiologists with a General Electric Logic 7 device (12 MHz, General Electric, Wauwatosa, Wisconsin). MIBI scintigraphy was performed before the operation; however, it could not be performed on the same day as the operation, since our hospital lacked the facility to use gamma probe with radioisotope sestamibi during the operation.
PHPT was defined biochemically before the surgery as the presence of hypercalcemia; hypophosphate; and inappropriately high, normal, or elevated plasma intact PTH levels. Serum calcium concentration was corrected for serum albumin. A blood sample was collected in the morning between 8:00 and 9:00 am after an overnight fasting in order to avoid differences in diurnal variation, especially in hormonal parameters. Total serum calcium, serum phosphate, serum creatinine, and blood glucose were measured by an automated electrochemiluminescence system (Roche Modular Analytics P-D, Roche Diagnostics GmbH, and D- 68298 Mannheim, Germany). The concentration of intact PTH in the plasma was determined using a commercial 2-side chemiluminescent, enzyme-labeled immunometric assay (Immulite 2000 PTH, DPC, Los Angeles, California). Intra-assay and inter-assay coefficients of variation were 4.3% (at 258 pg/mL) and 8.8% (at 387 pg/mL), respectively. The detection limit was 3 to 2500 pg/mL (0.3–263 pmol/L). Normal ranges of biochemical parameters were 8.5–10.5 mg/dL for serum calcium, 2.7 to 4.5 mg/dL for serum phosphate, 0.5 to 1.2 mg/dL for serum creatinine, and 12 to 69 pg/mL for plasma intact PTH concentration.
Patients were selected for parathyroidectomy based on symptoms and according to guidelines for surgical intervention in asymptomatic PHPT cases. Preoperative planning included preoperative calcemia (normal range, 8.5–10.2 mg/dL) and PTH levels (normal range, 11–69 pg/mL).10 Surgical approach, preoperative imaging preference, postoperative complications, conversion rate, number of identified abnormal glands, operation time, length of stay, and persistence and recurrence of hypercalcemia were noted. All patients had preoperative and postoperative vocal cord assessment. All patients underwent surgery under general anesthesia. All operations were performed through small cervical transverse incisions by 2 surgeons (E. Alhan, A. Cinel). The operation began with a unilateral neck operation according to localization studies. If a pathologic gland could not be identified in the first surgical side or in patients with negative USG and MIBI, bilateral neck exploration was used. Preoperative frozen sections were also used routinely to identify parathyroid tissue and differentiate it from nonparathyroid tissue with good accuracy.18 Examinations of the frozen sections were carried out by pathologists, who specialized in endocrine disease. Rapid PTH measurements could not be used. The patients stayed at least overnight and were discharged once their calcium level was stable or normal. It is our institutional policy to check calcium levels at least on day 1 and in the sixth week, and in the sixth and 12th month postoperatively. Persistent hypercalcemia was defined as recurrent presence of high calcium within 6 months of operation.
Data were analyzed using statistical package SPSS 13.01 for Windows (SPSS, Chicago, Illinois, and serial number 9069728). For the parametric distribution of values, Student t-test was used to compare the mean values of 2 or more groups. For the nonparametric variables, the Mann-Whitney U test was used to compare the median values of the response variable. The results were given mean ± standard derivation and they were considered significant at a P value of less than 0.05.
Results
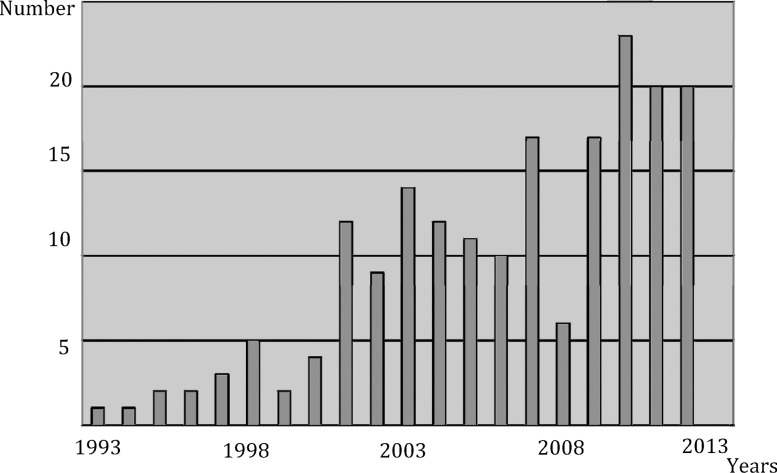
One hundred and ninety cases of PHPT undergoing parathyroidectomy in Farabi Hospital between January 1993 and January 2013 were analyzed in this study (Fig. 1). Ages ranged from 29 to 81 years with the mean age of 54 ± 13 years and a female-to-male ratio of 2.5:1. The majority of patients were between 50 and 60 years of age. There was no mortality in this study.
Fig. 1.
The distribution of the cases according to the years.
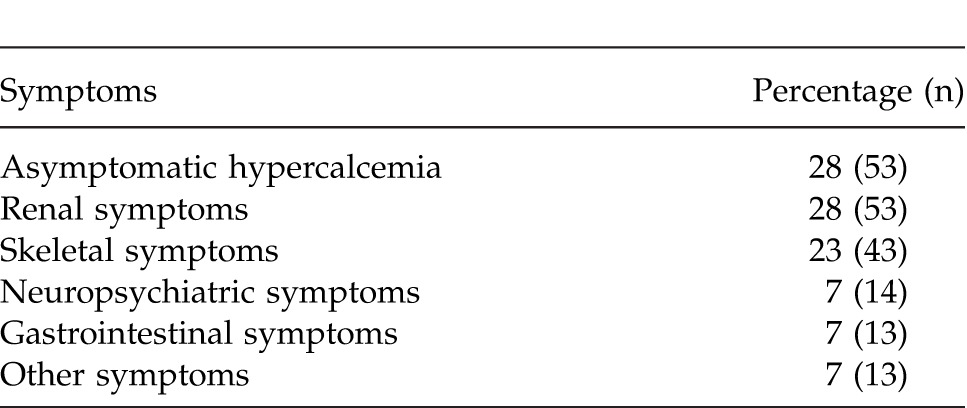
In this study, there were 53 asymptomatic patients (28%) at the time of diagnosis. The majority of 137 patients (72%) presented with various symptoms. The most common clinical features were found in the renal system in 53 patients (28%, Table 1). The skeletal system was affected in 43 patients (23%), gastrointestinal system in 13 (7%), neuropsychiatric system in 14 (13%) and other systems in 13 patients (12%). Preoperative ultrasonography (USG) in our study identified all abnormal glands accurately (82.6%), whereas MIBI and MRI showed an accuracy of 89.4% and 61%, respectively. The common use of USG and MIBI detected 92% of the pathologic lesions.
Table 1.
The distribution of the symptoms according to the system
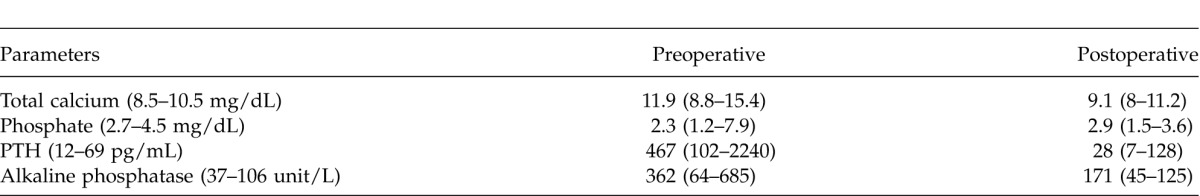
In this study, the mean serum calcium at the time of diagnosis was 11.9 ± 2.2 mg/dL, (range, 8.8–15.2; Table 2). Mean parathyroid hormone level was 467 ± 78 pg/mL (range, 102–2240 pg/mL). Elevated alkaline phosphatase was shown in 157 patients (83%) with the mean of 383 u/L ± 92 (range, 64–685 u/L).
Table 2.
Blood chemistry in pre- and postoperative period
In the present study, preoperative USG identified all abnormal glands accurately at a rate of 82.6%, while MIBI identified at 89.4% and MRI at 61%. The common use of USG and MIBI detected 92% of the pathologic lesions. MIBI showed correct localization in 18 cases with USG negative (9.4%) and USG identified abnormal glands in 5 cases with MIBI negative (2%). USG was used in a limited number of cases (2%) during the preoperative period.
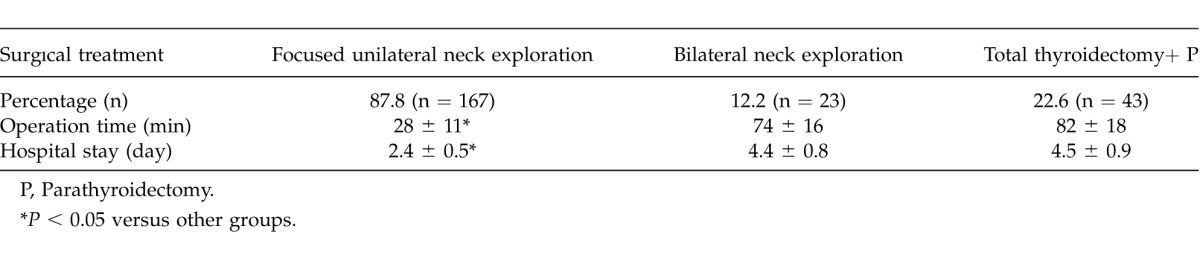
All patients had standard collar incision with bilateral neck exploration or unilateral neck exploration. Parathyroid gland was identified and the pathology was confirmed by frozen section examination. Bilateral neck exploration was performed in 23 patients (12.2%; Table 3). Focused unilateral neck exploration was performed for the remaining of the patients (87.8%). Surgical intervention in 1 patient was unsuccessful (0.5%). Forty-three patients (22.6%) undergoing parathyroidectomy also had a concomitant thyroid pathology and total thyroidectomy was performed on those patients. The conversion ratio from focused unilateral neck exploration to bilateral exploration was 5.2% and all of these patients were examined preoperatively with USG and MIBI. Transient recurrent nerve paralyses occurred in 2 patients with bilateral neck exploration due to parathyroid adenoma or hyperplasia. The mean operation time was 28 ± 11 minutes (P < 0.05; Table 3) for focused unilateral neck exploration, 74 ± 16 minutes for bilateral neck exploration, and 82 ± 18 minutes for parathyroidectomy and total thyroidectomy.
Table 3.
Surgical treatment, operation time, and hospital stay of the patients
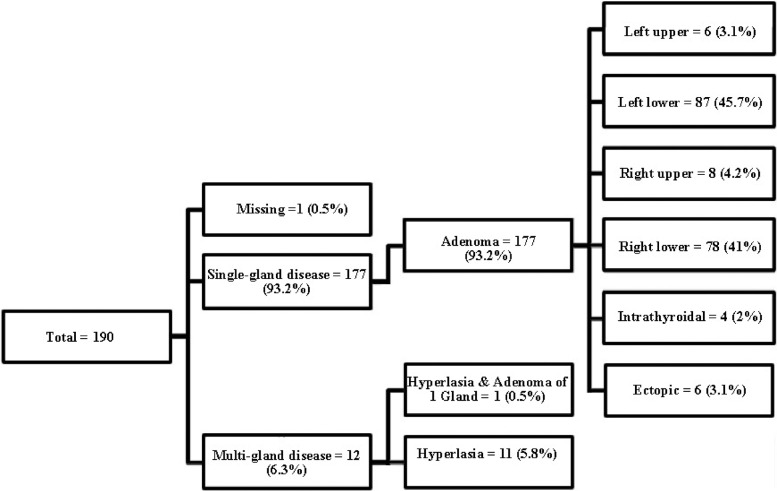
Pathologic examination revealed single adenoma in 93% of the patients (n = 177, 10 ± 2 mm; Fig. 2) and hyperplasia in 7% (n = 12). The most common thyroid pathology in patients with thyroidectomy was multinodular goiter (n = 41). Two patients also had a papillary thyroid carcinoma (1%). Adenomatous disease occurred most frequently in the inferior parathyroid glands (n = 165, 86.7%; Fig. 2) and most commonly on the left side (n = 93, 48.89%). Four of the single-gland adenomas were intrathyroidal and 6 had an ectopic location (upper mediastinum, carotid sheath). In cases with hyperplasia, MIBI did not indicate the localization of the pathologic lesion. The mean diameter of the pathologic lesion after surgical excision was found to be 10 ± 2mm. There was no difference between the diameter of pathologic lesion found by USG and the pathologic examination. Statistical analysis of frozen section examinations revealed 100% sensitivity, 69.2% specificity, 97.8% positive predictive value, and 100% negative predictive value.
Fig. 2.
Parathyroid pathology and localizations of adenoma.
The mean hospital stay was 2.4 ± 0.5 days for patients with unilateral neck exploration (P < 0.05; Table 3), 4.4 ± 0.8 days for patients with bilateral neck exploration, and 4.5 ± 0.9 days for patients with total thyroidectomy.
On the postoperative course, 23 patients (12%) had severe and prolonged hypocalcaemia, known as hungry bone syndrome (HBS). These patients were treated with oral calcium and vitamin D. Mean follow-up period was 8.4 ± 4.6 years (ranging from 9 months to 19 years). The follow-up rates were 80% after 1 year, 72% after 5 years, 53% after 10 years, and 41% after 19 years. None of these patients had persistent PHPT. Of the 34 patients unavailable for 5-year follow-up, 18 died, and 16 refused further investigation. Sixteen patients had decreased serum ionized calcium levels in 1-year follow-up and 9 patients in 5-year follow-up. The mean age of the hypocalcemic patients was 64 ± 11 years being significantly higher when compared to the overall mean age of this series (54 ± 13 years) and 75% of those patients had skeletal symptoms. The mean diameter of the pathologic lesions in patients with hypocalcaemia was 24 ± 3 mm, which was significantly greater when compared to the mean of overall series. Nine patients with long-time hypocalcaemia underwent subtotal parathyroidectomy or total thyroidectomy. No other long-term complications were recorded.
Discussion
PHPT is the most common cause of hypercalcemia in outpatients.19 It mostly affects females over 50 years of age.20 The demographic findings in our study (mean age: 54 ± 13 years and a female: male ratio of 2.5) were similar to the literature results.20 PHPT is traditionally known with multiple somatic signs and symptoms of many systems, including the skeletal system (bone pain, osteitis fibrosa cystica, pathologic fracture, and proximal muscle weakness), renal system (recurrent nephrolithiasis, renal failure), and nervous system (psychosis, alteration of consciousness).20 The wide use of multichannel autoanalyzers in many developed countries in the 1970s resulted in the early diagnosis of PHPT in asymptomatic state with minor symptoms.21 We started to use autoanalyzers in the beginning of the year 2000 and our cases have increased since, as shown in Fig. 1.
Symptomatic PHPT cases in eastern countries vary between 90% and 95%, and in western countries between 5% and 12%.1,15,16,20,22,23 In our study, the symptomatic cases were 72% (Table 1). The location of our country between the eastern and western countries explains this result. A similar finding for PTH level was observed. Intact PTH level in western studies is 100–120 pg/mL, and in the eastern series, over 600 pg/mL, which was also shown in our study with 467 pg/mL (Table 2).15,16,22,23 The renal and the skeletal systems were affected in most patients (Table 1). The remaining cases involved the gastrointestinal system, the neuropsychiatric system, and others, which is similar to the recent literature.2,10,16,20–23
All patients with PHPT were referred to surgery from our Endocrinology and Metabolism Department in the same hospital, where we are working as a team with the Endocrinology Department for the treatment of PHPT. Surgical indications are based on symptoms and according to guidelines for surgical intervention in asymptomatic PHPT cases, such as serum calcium > 1.0 mg/dL (0.25 mmol/L) above normal, creatinine clearance reduced to < 60 mL/min, T-score < −2.5 at any site and/or previous fragility fracture, and age < 50 years.10 Sosa et al have reported in the USA that a large divergence in surgical practice exists due to the widespread failure to apply international guidelines and experienced surgeons keen to operate on several asymptomatic or minimally-symptomatic patients with no insignificant mortality.24
In the last 30 years, new imaging and diagnostic methods for the localization of the pathologic lesion of the PHPT have resulted in the change of surgical approach of the PHPT and the confirmation of surgical therapy. These new imaging and diagnostic methods include USG, MIBI scintigraphy, MRI, MIBI scintigraphy with the use of CT, and intraoperative adjuncts, such as a gamma probe with radioisotope sestamibi, intraoperative rapid PTH measurements, and the use of methylene blue or frozen section.5–17
USG is a cheap, adequate, and noninvasive modality. Sensitivity of USG is associated with the user, the size and localization of the adenoma and concomitant thyroid disorder.6,7,15,16,25 In our study, USG detected 82.6% of the parathyroid lesions. In the literature, the accuracy of USG has been reported to range between 72 and 89%.6 High accuracy of USG obtained in our study can be explained with its implementation by an experienced radiologist and the good quality of the USG device. A recent meta-analysis by Cheung et al has reported a sensitivity of 93.2%.26
There are multiple scintigraphic techniques for the evaluation of PHPT, such as dual-phase scintigraphy using a single radiopharmaceutical (99mTc MIBI) or dual-isotope subtraction scintigraphy using 99mTc MIBI and 99mTc–pertechnetate. In addition, tomographic imaging with SPECT or SPECT/CT increases the sensitivity of this investigation.7 MIBI scintigraphy is a widely-popular modality.12,14 The size of lesions and concomitant thyroid disease decrease the sensitivity of MIBI similar to USG.7,10,12,14 In this study, the sensitivity of MIBI was found to be 89.4% alone. MIBI is more sensitive than USG in the literature similar to our results.7,10,12,14 Recent large series using SPECT have shown sensitivities for the detection of solitary adenomas in the range of 68 to 95%.6 The meta-analysis of Ruda et al included 96 studies where MIBI scintigraphy was used between 1995 and 2003 for the evaluation of PHPT and obtained the sensitivity of MIBI as 88%.27 The use of SPECT/CT with MIBI increases the sensitivity up to 95–98%.6,7,12
Combined USG and MIBI use for the preoperative evaluation of PHPT increases the sensitivity than either technique alone.6 Lumachi et al have reported preoperative USG and MIBI findings in patients with PHPT proven solitary adenomas and found a combined sensitivity of 95% versus 80% for USG and 87% for scintigraphy alone.28 These results are similar to our results. In cases with parathyroid hyperplasia, MIBI is more helpful than USG.6,7,28
Adenomatous disease occurred most frequently in the inferior parathyroid glands [n = 165 (86.7 %); Fig. 2] and most commonly on the left side [n = 93 (48.89%)]. Four of the single-gland adenomas were intrathyroidal and 6 were atypical location (upper mediastinum, carotid sheath). McVeigh et al have found results similar to our study in the inferior gland; however, their results have been observed most commonly on the right side contrary to our study.11
The aim of parathyroid surgery is the biochemical cure of PHPT. Traditionally, the standard surgical intervention for most patients with PHPT is bilateral neck exploration, usually under general anesthesia.9,10,29 Bilateral exploration provides visual observation based on estimations of the gland size to distinguish single adenoma from multiglandular disease. However, with increased experience, improved imaging modalities, and the use of adjuncts such as intraoperative PTH monitoring (IOPTH), minimally-invasive parathyroidectomy (MIP) or focused unilateral parathyroid exploration are emerging as the procedure of choice.6,10,11,13,15,16 Focused unilateral parathyroid exploration leads to reduced postoperative pain and lower incidence of hypocalcaemia from ischemia of other glands with smaller incision and less dissection, less operation time, hospital stay, and patient cost.30–35
In this study, focused unilateral parathyroid exploration was performed with small cervical incision under general anesthesia. One recurrence and 2 transient unilateral recurrent nerve paralyses were found, achieving a success rate of 99.52%. All operations were performed by 2 experienced surgeons (E. Alhan and A. Cinel). The confirmation of the diagnosis was made by frozen-section examination—not IOPTH measurement, the use of the gamma probe with radioisotope sestamibi, or methylene blue injection.10–18 We found a mean operation time of 28 ± 11 minutes for focused unilateral exploration and 74 ± 14 minutes for bilateral exploration. The difference was significant between the 2 groups (P < 0.05). Wong et al have reported that the mean operative time for unilateral exploration with minimal invasive surgery is 42.38 [standard deviation (SD): 12.31] minutes and the mean operative time for bilateral exploration is 76.43 (SD: 16.51) minutes.15 On the other hand, Teksöz et al have shown that mean time for unilateral exploration with local anesthesia and IOPTH measurement was 15.09 ± 6:38 minutes.30 One of the limitations of the present study was the absence of the facility of IOPTH measurements and the use of gamma probe with radioisotope sestamibi in our hospital during the operation; however, frozen section examination in all cases and intraoperative USG examination in 2% of the patients (in limited cases) could be performed. The operation time could be reduced with the use of IOPTH measurement and local anesthesia in the future. However, our surgical intervention with focused parathyroid exploration led to less hospital stay and indirectly low hospital cost, similar to the literature.31–35 On the other hand, the high positive predictive value (97.8%) after the frozen section examination performed by specialized 2 pathologists increased the surgical success in our study.18
The cure rates of bilateral neck exploration and MIP are similar. Although there are few randomized trials comparing minimally-invasive parathyroidectomy with traditional bilateral approach, cure rates appear to be similar when the procedures are performed by experienced endocrine surgeons.9,32–38 Udelsman et al have reported that the overall success rate for the entire group was 98%, and there were no significant differences in cure rates between traditional (97%) and minimally-invasive (99%) techniques. The overall complication rates were also similar, but minimally-invasive surgery was associated with a 50% reduction in operating time, a seven-fold reduction in length of hospital stay, and a mean cost savings of $2693 per case with an experienced surgeon.33
Pathologic examination in our study showed single adenoma in 93% of the patients and hyperplasia in 7%. One patient had 3 adenomas. No parathyroid carcinoma was observed. Histopathologic distribution of the cases was similar to the literature results.9–11,15,16,31
Before parathyroid surgery, concomitant thyroid pathology must be investigated. Goiter is endemic in our region in Turkey. Total thyroidectomy was performed in 43 patients (22.6%) during parathyroidectomy. Papillary carcinoma of the thyroid was found in 2 patients as described in the literature.39
Hypocalcaemia, known as HBS, was observed during the postoperative course in 23 patients (12%). Large PHPT case series suggest that the syndrome develops postoperatively in up to 13% of patients.40 Recent case series from Asia have reported much higher prevalence rates of 24 to 87%, whereas a case series from Saudi Arabia documented a prevalence rate of only 4%.40 Risk factors for the development of HBS are old age at time of surgery, increased high alkaline phosphatase level, radiologic bone disease before surgery, great volume and weight of resected pathologic parathyroid gland, increased levels of osteocalcin, and extent of surgery.40 Increased diameter of the resected pathologic lesion, old age, more skeletal symptoms, and increased alkaline phosphatase level in our study support that suggestion.
Calcium supplement in patients with hypocalcaemia at the postoperative period depend on serum calcium, PTH, and vitamin D3 level. Should permanent hypoparathyroidism occur, calcium and vitamin D3 supplementations continue for a lifetime. In patients with transient hypocalcaemia and with vitamin D3 insufficiency, calcium and vitamin D3 were given until this condition was healed.8,10 Our geographic location in Turkey is northeast and people cannot receive sufficient sunlight exposure to maintain adequate vitamin D3 level due to the mainly cloudy weather. Thus, for the treatment of postoperative hypocalcaemia, vitamin D3 supplementation was preferred in addition to calcium.
Despite the advances in preoperative imaging, regional anesthetic techniques, and the availability of new operative techniques and intraoperative parathyroid hormone (PTH) monitoring, in a small percentage of patients either persistent or recurrent PHPT develops. Persistent PHPT occurs when hypercalcemia develops within 6 months of initial operation. When hypercalcemia develops after a normocalcemic period of 6 months, it is defined as recurrent disease.10 There was 1 persistent PHPT (0.5%) and no recurrent diseases in our study. This ratio varies in the literature between 0.2% and 2%.9,10,15,17 Several causes of recurrent disease include errors of differential diagnosis of PHPT, low follow-up rate, and surgeon inexperience.10 The low recurrent disease in our study may be explained by low follow-up rate and surgeon experience.
Our follow-up rate was low when compared to the developed countries.9 It may be explained with the differences of socioeconomic and sociocultural levels of our country.
Focused surgical exploration (unilateral neck exploration) in parathyroidectomy with new imaging techniques and its implementation by an experienced surgeon resulted in adequate treatment success rate, decreased operation time, hospital stay, and hospital cost.
References
- 1.Wermers RA, Khosla S, Atkinson EJ. Incidence of primary hyperparathyroidism in Rochester, Minnesota, 1993–2001: an update on the changing epidemiology of the disease. J Bone Miner Res. 2006;21(1):171–177. doi: 10.1359/JBMR.050910. [DOI] [PubMed] [Google Scholar]
- 2.Mundy GR, Cove DH, Fisken R. Primary hyperparathyroidism: changes in the pattern of clinical presentation. Lancet. 1980;315(8182):1317–1320. doi: 10.1016/s0140-6736(80)91783-3. [DOI] [PubMed] [Google Scholar]
- 3.Melton LJ., III The epidemiology of primary hyperparathyroidism in North America. J Bone Miner Res. 2002;17(2):12–17. [PubMed] [Google Scholar]
- 4.Mandl F. Hyperparathyroidism. A review of historical developments and the present state of knowledge on the subject. Surgery. 1947;21(3):394–440. [PubMed] [Google Scholar]
- 5.Taniguchi M, Tanaka M, Hamano T, Nakanishi S. Comparison between whole and intact parathyroid hormone assays. Ther Apher Dial. 2011;15(1):42–49. doi: 10.1111/j.1744-9987.2011.00926.x. [DOI] [PubMed] [Google Scholar]
- 6.Johnson NA, Tublin ME, Ogilvie JB. Parathyroid imaging: technique and role in the preoperative evaluation of primary hyperparathyroidism. AJR. 2007;188(16):1706–1715. doi: 10.2214/AJR.06.0938. [DOI] [PubMed] [Google Scholar]
- 7.Patel CN, Salahudeen HM, Lansdown M, Scarbrook AF. Clinical utility of ultrasound and 99mTc sestamibi SPECT/CT for preoperative localization of parathyroid adenoma in patients with primary hyperparathyroidism. Clin Radiol. 2010;65(4):278–287. doi: 10.1016/j.crad.2009.12.005. [DOI] [PubMed] [Google Scholar]
- 8.Pyram R, Mahajan G, Gliwa A. Primary hyperparathyroidism: skeletal and non-skeletal effects, diagnosis and management. Maturitas. 2011;70(3):246–255. doi: 10.1016/j.maturitas.2011.07.021. [DOI] [PubMed] [Google Scholar]
- 9.Westerdahl J, Bergenfelz A. Unilateral versus bilateral neck exploration for primary hyperparathyroidism, five-year follow-up of a randomized controlled trial. Ann Surg. 2007;246(6):976–981. doi: 10.1097/SLA.0b013e31815c3ffd. [DOI] [PubMed] [Google Scholar]
- 10.Udelsman BV, Udelsman R. Surgery in primary hyperparathyroidism: extensive personal experience. J Clin Densitom. 2013;16(1):54–59. doi: 10.1016/j.jocd.2012.11.007. [DOI] [PubMed] [Google Scholar]
- 11.McVeigh T, Lowery AJ, Quill DS, Kerin MJ. Changing practices in the surgical management of hyperparathyroidism - A 10-year review. Surgeon. 2012;10(6):314–320. doi: 10.1016/j.surge.2011.10.005. [DOI] [PubMed] [Google Scholar]
- 12.Burke JF, Naraharisetty K, Schneider DF, Sippel RS, Chen H. Early-phase technetium-99m sestamibi scintigraphy can improve preoperative localization in primary hyperparathyroidism. Am J Surg. 2013;205(3):269–273. doi: 10.1016/j.amjsurg.2013.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen H, Pruhs Z, Starling JR, Mack E. Intraoperative parathyroid hormone testing improves cure rates in patients undergoing minimally invasive parathyroidectomy. Surgery. 2005;138(4):583–590. doi: 10.1016/j.surg.2005.06.046. [DOI] [PubMed] [Google Scholar]
- 14.Dy BM, Richards ML, Vazquez BJ, Thompson GB, Farley DR, Grant CS. Primary hyperparathyroidism and negative Tc99 sestamibi imaging: to operate or not? Ann Surg Oncol. 2012;19(7):2272–2278. doi: 10.1245/s10434-012-2325-3. [DOI] [PubMed] [Google Scholar]
- 15.Wong W, Foo FJ, Lau MI, Sarin A, Kiruparan P. Simplified minimally invasive parathyroidectomy: a series of 100 cases and review of the literature. Ann R Coll Surg Engl. 2011;93(4):290–293. doi: 10.1308/003588411X571836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Paravastu SCV, Chadwick DR. Parathyroidectomy in a district general hospital: outcomes and evolution in the era of minimally invasive surgery. Int J Surg. 2012;10(7):373–377. doi: 10.1016/j.ijsu.2012.05.021. [DOI] [PubMed] [Google Scholar]
- 17.Schneider DF, Mazeh H, Sippel RS, Chen H. Is minimally invasive parathyroidectomy associated with greater recurrence compared to bilateral exploration? Analysis of more than 1,000 cases. Surgery. 2012;152(6):1008–1015. doi: 10.1016/j.surg.2012.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Westra WH, Pritchett DD, Udelsman R. Intraoperative confirmation of parathyroid tissue during parathyroid exploration: a retrospective evaluation of the frozen section. Am J Surg Pathol. 1998;22(5):538–544. doi: 10.1097/00000478-199805000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Khan A, Bilezikian J. Primary hyperparathyroidism: pathophysiology and impact on bone. CMAJ. 2000;163(2):184–187. [PMC free article] [PubMed] [Google Scholar]
- 20.Khan AA, Bilezikian JP, Potts JT., Jr The diagnosis and management of asymptomatic primary hyperparathyroidism revisited. J Clin Endocrinol Metab. 2009;94(2):333–334. doi: 10.1210/jc.2008-1757. [DOI] [PubMed] [Google Scholar]
- 21.Kaplan EL, Yashiro T, Salti G. Primary hyperparathyroidism in the 1990s: choice of surgical procedures for this disease. Ann Surg. 1992;215(4):300–317. doi: 10.1097/00000658-199204000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fraser WD. Hyperparathyroidism. Lancet. 2009;374(9684):145–158. doi: 10.1016/S0140-6736(09)60507-9. [DOI] [PubMed] [Google Scholar]
- 23.Pradeep PV, Jayashree B, Mishra A, Mishra SK. Systematic review of primary hyperparathyroidism in India: the past, present, and the future trends. Int J Endocrinol. 2011;2011:921814. doi: 10.1155/2011/921814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sosa JA, Powe NR, Levine MA, Udelsman R, Zeiger MA. Profile of a clinical practice: thresholds for surgery and surgical outcomes for patients with primary hyperparathyroidism: a national survey of endocrine surgeons. J Clin Endocrinol Metab. 1998;83(8):2658–2665. doi: 10.1210/jcem.83.8.5006. [DOI] [PubMed] [Google Scholar]
- 25.Erbil Y, Barbaros U, Tukenmez M. Impact of adenoma weight and ectopic location of parathyroid adenoma on localization study results. World J Surg. 2008;32(4):566–571. doi: 10.1007/s00268-007-9389-4. [DOI] [PubMed] [Google Scholar]
- 26.Cheung K, Wang TS, Farrokhyar F, Romon SA, Sosa JA. A meta-analysis of preoperative localization techniques for patients with primary hyperparathyroidism. Ann Surg Oncol. 2012;19(2):577–583. doi: 10.1245/s10434-011-1870-5. [DOI] [PubMed] [Google Scholar]
- 27.Ruda JM, Hollenbeak CS, Stack BC., Jr A systematic review of the diagnosis and treatment of primary hyperparathyroidism from 1995 to 2003. Otolaryngol Head Neck Surg. 2005;132(3):359–372. doi: 10.1016/j.otohns.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 28.Lumachi F, Zucchetta P, Marzola MC, Boccagni P, Angelini F, Buf F, et al. Advantages of combined technetium-99m-sestamibi scintigraphy and high-resolution ultrasonography in parathyroid localization: comparative study in 91 patients with primary hyperparathyroidism. Eur J Endocrinol. 2000;143(6):755–760. doi: 10.1530/eje.0.1430755. [DOI] [PubMed] [Google Scholar]
- 29.Silverberg SJ, Bilezikian JP. Asymptomatic primary hyperparathyroidism: a medical perspective. Surg Clin North Am. 2004;84(3):787–801. doi: 10.1016/j.suc.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 30.Teksoz S, Bukey Y, Ozcan M, Arikan AE, Erbabacan SE, Ozyegin A. Minimal invasive parathyroidectomy with local anesthesia for well-localized primary hyperparathyroidism: “Cerrahpasa experience. Updates Surg. 2013;65(3):217–223. doi: 10.1007/s13304-013-0202-7. [DOI] [PubMed] [Google Scholar]
- 31.Grant CS, Thompson G, Farley D, van Heerden J. Primary hyperparathyroidism surgical management since the introduction of minimally invasive parathyroidectomy: Mayo Clinic experience. Arch Surg. 2005;140:472–478. doi: 10.1001/archsurg.140.5.472. [DOI] [PubMed] [Google Scholar]
- 32.Bergenfelz A, Lindblom P, Tibblin S, Westerdahl J. Unilateral versus bilateral neck exploration for primary hyperparathyroidism: a prospective randomized controlled trial. Ann Surg. 2002;236(5):543–551. doi: 10.1097/00000658-200211000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Udelsman R. Six hundred fifty-six consecutive explorations for primary hyperparathyroidism. Ann Surg. 2002;235(5):665–670. doi: 10.1097/00000658-200205000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Miccoli P, Minuto MN, Massi M, Barellini L, Galleri D, D'Agostino J, et al. Video-assisted minimally invasive parathyroidectomy with median access. Technical changes: case load 1999–2002. Ann Ital Chir. 2003;74(4):407–412. [PubMed] [Google Scholar]
- 35.Russell CF, Dolan SJ, Laird JD. Randomized clinical trial comparing scan-directed unilateral versus bilateral cervical exploration for primary hyperparathyroidism due to solitary adenoma. Br J Surg. 2006;93(4):418–421. doi: 10.1002/bjs.5250. [DOI] [PubMed] [Google Scholar]
- 36.Slepavicius A, Beisa V, Janusonis V, Strupas K. Focused versus conventional parathyroidectomy for primary hyperparathyroidism: a prospective, randomized, blinded trial. Langenbecks Arch Surg. 2008;393(5):659–666. doi: 10.1007/s00423-008-0408-1. [DOI] [PubMed] [Google Scholar]
- 37.Aarum S, Nordenström J, Reihnér E, Zedenius J, Jacopsson H, Danielsson R, et al. Operation for primary hyperparathyroidism: the new versus the old order. A randomised controlled trial of preoperative localisation. Scand J Surg. 2007;96(1):26–30. doi: 10.1177/145749690709600105. [DOI] [PubMed] [Google Scholar]
- 38.Mihai R, Barczynski M, Iacobone M, Sitges-Serra A. Surgical strategy for sporadic primary hyperparathyroidism an evidence-based approach to surgical strategy, patient selection, surgical access, and reoperations. Langenbecks Arch Surg. 2009;394(5):785–798. doi: 10.1007/s00423-009-0529-1. [DOI] [PubMed] [Google Scholar]
- 39.Javadi H, Jallalat S, Semnani S, Mogharrabi M, Riazi A, Nabipour I, et al. Concurrent papillary thyroid cancer and parathyroid adenoma as a rare condition: a case report. Nucl Med Rev East Eur. 2012;15(2):153–155. [PubMed] [Google Scholar]
- 40.Witteveen JE, van Thiel SV, Romijn JA, Hamdy NAT. Hungry bone syndrome: still a challenge in the post-operative management of primary hyperparathyroidism: a systematic review of the literature. Eur J Endocrinol. 2013;168(3):45–53. doi: 10.1530/EJE-12-0528. [DOI] [PubMed] [Google Scholar]