Abstract
Hemobilia is an uncommon presentation of biliary tract or pancreatic disease. The investigation and management of this clinical problem is challenging. We report on a case of biliary tract hemorrhage from an otherwise asymptomatic right lobe biliary cystadenocarcinoma and review the literature on this unusual presentation. Hemobilia from primary or secondary liver tumors is not frequently reported in the literature. Hemobilia in this setting is usually observed in association with an obvious liver mass or abnormal liver function tests. This is a report of a case of hemobilia as the primary presentation of a small right lobe cystadenocarcinoma. Literature on the incidence and treatment of hemobilia associated with liver tumors has been reviewed. Hemobilia is investigated and definitively treated with angiography. In our case, initial imaging was equivocal and the lesion was only demonstrated after rebleeding, requiring a second angiogram. Surgical resection of the mass was required for definitive control of bleeding. This case illustrates the difficulties of investigating and treating hemobilia caused by primary or secondary liver tumors. Cystadenocarcinoma of the liver is not a common tumor, and biliary tract hemorrhage as the primary presentation of this tumor in the absence of a significant mass or abnormal liver function tests has not been previously described.
Key words: Biliary cystadenocarcinoma, Hemobilia, Gastrointestinal tract bleeding, Liver resection
Hemobilia is defined as bleeding into the biliary tract from a fistula between the splanchnic vasculature and an intra- or extra-hepatic biliary duct. Iatrogenic injuries from percutaneous biliary tract instrumentation and trauma are the most common causes. Hemobilia as the initial presentation of primary or secondary liver tumors is unusual and poses significant diagnostic and therapeutic challenges.1
Case Report
A 69-year-old male presented with a symptomatic anemia and hemoglobin of 6.7g/dL. Upper and lower gastrointestinal tract endoscopy were negative. Bleeding from the ampulla of vater was observed at the small bowel endoscopy. An endoscopic retrograde cholangiogram performed shortly thereafter revealed the presence of clot-like material within the common bile duct. An abdominal magnetic resonance imaging (MRI) scan performed without liver specific contrast was negative for any hepatic masses.
Visceral angiography did not demonstrate an obvious source. Embolization of the gastroduodenal artery and its principal branches was performed, which controlled the bleed temporarily. The patient was admitted 1 month later with further bleeding. Repeat angiography demonstrated an area of hypervascularity in the right posterior liver lobe, approximately 4 cm in maximal diameter (Fig. 1). This area, suggestive of a tumor mass, was promptly embolized. Postembolization MRI confirmed the presence of a hypoenhancing mass. A computed tomography (CT) scan-guided biopsy of the mass was not diagnostic.
Fig. 1.
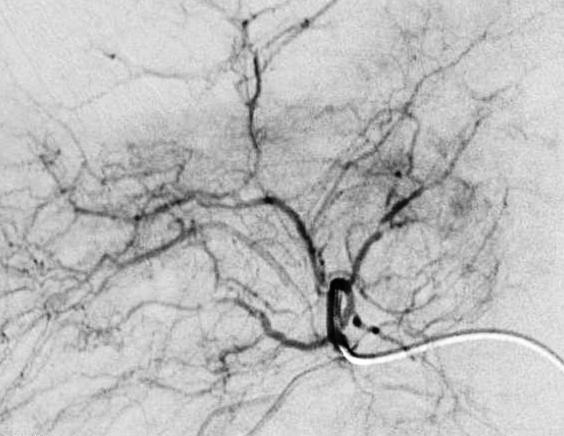
Angiogram showing splaying of right posterior segmental arterial branches, suggesting a mass.
A surgical evaluation was sought after the patient was readmitted with bleeding requiring blood transfusion 2 months later. A liver-specific MRI was repeated and confirmed the presence of a nonenhancing, 3-cm mass in the posterior right lobe with evidence of postembolization change (Fig. 2). The patient did not have cirrhosis and his alpha-fetoprotein and liver function tests were not elevated. No extra hepatic disease was noted. The patient underwent a right hepatectomy. Pathology of the specimen revealed a biliary cyst adenocarcinoma, 3 cm in maximal diameter, with clear resection margins.
Fig. 2.
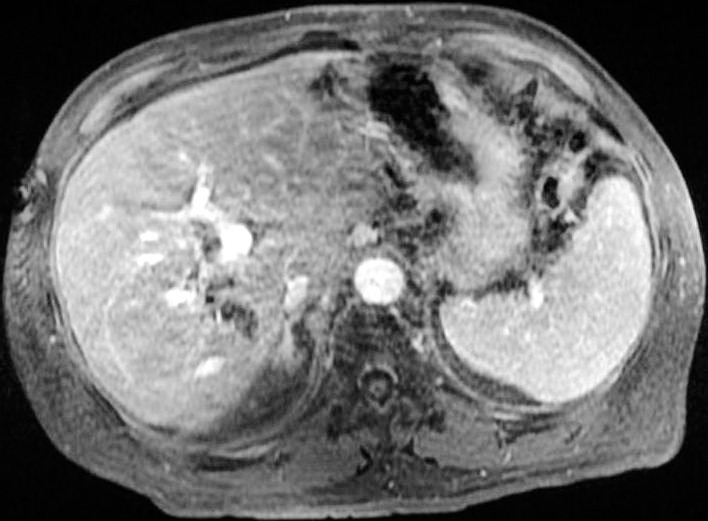
MRI abdomen with eovist, demonstrating a right posterior lobe hypoenhancing mass.
Discussion
Biliary cystic tumors account for fewer than 5% of all intrahepatic cysts of biliary origin. The mean age of presentation is 50 years and many patients are asymptomatic at diagnosis.2 Cystadenomas are usually multilocular and over 80% have a dense mesenchymal stroma composed of spindle cells. The epithelial lining of cystadenocarcinomas is similar but the cells demonstrate atypia, greater mitotic activity, and infiltrative growth.2 The majority of cystadenomas and cystadenocarcinomas arise from the intrahepatic biliary tree, although about 10% of biliary cystic tumors have been reported to originate from extrahepatic bile ducts.5 These tumors are typically slow growing but can range in size from 1.5 to 35 cm.5 A combination of CT, MRI, and ultrasound combined with clinical features may more accurately differentiate complex biliary cysts.5 Biliary cystic tumors are typically multilocular on MRI and demonstrate a homogenous low-intensity T1 signal and a high-intensity T2 signal.5 The most common presenting symptoms are right upper quadrant pain, a palpable mass, or jaundice. Hemorrhage and cyst rupture have been reported in the literature, but are very uncommon.5
Tumors as a primary cause of hemobilia are unusual. In a systematic review of 222 cases of hemobilia over a 3-year period, only 14 cases of tumor related biliary tract bleeding were identified. Hepatocellular carcinoma, cholangiocarcinoma, and metastatic cancer were the liver tumors associated with bleeding in this series. It is not clear, however, whether hemobilia was the primary presenting symptom in this group.3
In reviewing the literature, we identified 1 report of a hepatic papillary cystadenocarcinoma presenting with melena, abnormal liver function tests, and a liver mass on a CT scan.4 Our case uniquely illustrates how a small liver mass that is consistently difficult to identify on imaging can present primarily with biliary tract hemorrhage.
Conclusion
The diagnosis and treatment of hemobilia in the presence of indeterminate abdominal imaging in a patient with no history of liver disease and normal liver function tests can be challenging. As this case demonstrates, small intrahepatic tumors remain an important, but extremely unusual, differential diagnosis. Angiography with embolization remains the principal modality of intervention,3 although, as in our case, more than 1 angiogram may be necessary to identify the source. Although embolization controlled bleeding from the tumor in our case acutely, hepatic resection was eventually required for recurrent symptoms and should be considered in good risk patients who have isolated hepatic lobar trauma or a resectable neoplasm.3
References
- 1.Lech G, Krasnodebski IW. Hemobilia of neoplastic origin. Pol Merkur Lekarski. 2010;29(173):328–330. [PubMed] [Google Scholar]
- 2.Kim HG. Biliary cystic neoplasm: biliary cystadenoma and cystadenocarcinoma. Korean J Gastroenterol. 2006;47(1):5–14. [PubMed] [Google Scholar]
- 3.Green MHA, Duell RM, Johnson CD, Jamieson NV. Haemobilia. Br J Surg. 2001;88(6):773–786. doi: 10.1046/j.1365-2168.2001.01756.x. [DOI] [PubMed] [Google Scholar]
- 4.Alapati R, Ibrahim MA, D'Angelo DM, Malhotra SK, Nensey YM, Salah-Eldin AA, et al. Papillary cystadenocarcinoma of the bile ducts resulting in hemobilia. Am J Gastroenterol. 1989;84(12):1564–1566. [PubMed] [Google Scholar]
- 5.Soares K, Arnaoutakis D, Kamel I, Anders R, Adams R, Bauer T, et al. Cystic neoplasms of the liver: biliary cystadenoma and cystadenocarcinoma. J Am Coll Surg. 2014;218(1):119–128. doi: 10.1016/j.jamcollsurg.2013.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]


