Abstract
Background
The aim of this study was to investigate the prevalence of hepatitis B, hepatitis C, HIV and syphilis infections in blood donors referred to Tehran Blood Transfusion Center (TBTC), and determine any association between blood groups and blood- borne infections between the years of 2005 and 2011.
Methods
This was a retrospective study conducted at TBTC. All of the donor serum samples were screened for HBV, HCV, HIV and syphilis by using third generation ELISA kits and RPR test. Initial reactive samples were tested in duplicate. Confirmatory tests were performed on all repeatedly reactive donations. Blood group was determined by forward and reverse blood grouping. The results were subjected to chi square analysis for determination of statistical difference between the values among different categories according to SPSS program.
Results
Overall, 2031451 donor serum samples were collected in 2005-2011. Totally, 10451 were positive test for HBV, HCV, HIV and syphilis. The overall seroprevalence of HBV, HCV, HIV, and syphilis was 0.39%, 0.11%, 0.005%, and 0.010%, respectively. Hepatitis B and HIV infections were significantly associated with blood group of donors (P <0.05) ; percentage of HIV Ag/Ab was higher in donors who had blood group “A” and percentage of HBs Ag was lower in donors who had blood group O. There was no significant association between Hepatitis C and syphilis infections with ABO and Rh blood groups (P>0.05).
Conclusion
Compared with neighboring countries and the international standards, prevalence of blood-borne infections is relatively low.
Keywords: HBV, HCV, HIV, Syphilis, ABO Blood groups, Rhesus (Rh), Blood donors
Introduction
The surface of red blood cells contains different polysaccharides and proteins called blood group antigens. Approximately 700 erythrocyte antigens are discovered and part of them that are related to each other described into 33 blood group systems by the International Society of Blood Transfusion (TBTC), of which ABO and Rh groups system are the most important (1-3).
“Blood group antigens plays a vital role in transfusion safety, understanding genetics, inheritance pattern, researching population migration patterns, as well as resolving certain medico-legal issues” (1,4). In modern medicine besides their importance in evolution, their relation to disease and environment is being increasingly important. Some blood groups can act as a receptor and ligand for bacteria, parasites and viruses. “The possible pathogenesis for this susceptibility is that as many organisms that may bind to polysaccharide on cells and soluble blood group antigens may block this binding” (5, 6).
Several studies investigated the association of blood groups with infectious and non-infectious diseases. Among infectious disease, Human immunodeficiency virus (HIV), and Hepatitis virus are of great concern because of their prolonged viraemia and carrier or latent state. They also cause fatal, chronic and life-threatening disorders.
AIDS in human was first reported in 1981 in USA and HIV was first isolated in 1983 (7, 8). HIV has infected more than 33 million people thus far worldwide and infection rates continue to increase (9). Infection with hepatitis B and hepatitis C are also the major health problems worldwide. There are about 2 billion people infected by HBV and among them more than 240 million have chronic (long-term) liver infections (10). It is estimated that 150 million people are chronically infected with HCV and 3 – 4 million are newly infected each year (11). Syphilis is also a systemic disease caused by Treponema pallidum (12). The world health organization (WHO) estimates that 12 million new cases of syphilis occur each year (13). Despite the fact that T. pallidum cannot survive in properly stored blood and the inescapable cost implications of syphilis testing of blood donors particularly in resource-poor settings, it must be noted that the emphasis of blood transfusion should be on two fundamental objectives – safety and protection of human lives. “Syphilis screening of donated blood, no matter what the incidence is in the donor population, has been considered to have value as a ‘lifestyle’ indicator, as individuals exposed to syphilis may also have been exposed to other sexually transmitted diseases”(14).
Several studies have assessed the association of blood groups with blood-borne infections but based on different sample size, test methodology, covered age, social risk factors and geographic conditions, results have been different.
The aim of this study was to investigate the prevalence of hepatitis B, Hepatitis C, HIV and Syphilis infections in blood donors referred to Tehran Blood Transfusion Center, with a population of over 300,000 blood donations per year, and to determine any association between blood groups and blood borne infections during 2005-2011 years.
Materials and Methods
This was a retrospective study conducted at TBTC. All blood donors who eligible to donated blood from 2005 to 2011 were reviewed. Donors who selected by the medical screening based on standard criteria for blood donation, participate into this study. 2031451 donors were eligible to donate blood. The volunteer donors constituted 100% of total blood donors. All of the eligible donor serum samples were screened for HBV, HCV, HIV and syphilis. Hepatitis B surface Antigen (HBS Ag), HIV (Ag/Ab) and HCV Ab screened using third generation ELISA kits. Serum from all donors was tested for the presence of Treponemal antibodies using Rapid Plasma Reagin test (RPR). Initial reactive samples were tested in duplicate. Repeatedly reactive results were considered sero-positive for their infections. Confirmatory tests were performed on all repeatedly reactive donations using the following tests: HBC Ab and HBS Ag confirmatory assay for HBS Ag positive samples, HCV RIBA for HCV Ab positive samples, HIV Western Blot for HIV Ag/Ab positive samples and FTA-ABS for RPR positive samples.
Blood group was determined by forward blood grouping (cell grouping) and reverse blood grouping (serum grouping) by test tube agglutination method. Final blood group is confirmed only if both cell type and back type are identical. Rh negative blood groups were confirmed by antiglobulin technique. All weak D (DU) groups were considered as Rh positive.
Data on the prevalence of blood-borne infections and the frequency of blood groups of donors was collected from MAK database (software with functionality to the blood banking and blood transfusion Centers that used in TBTC). Statistical analysis was carried out using SPSS software. Chi-square test was performed for Qualitative comparison. P value less than 0.05 was considered statistically significant.
Results
Over a period of six years (March 2005 to March2011) a total of 2,031,451 donations were collected with an average of 338,575 donations per year. 1,892,835(93.2%) of them were male and 138,616(6.8%) were female. After excluding of Blood group discrepancies, blood group of 2,028,086 donors was determined. Blood group O+ with frequency of 665,943 (32.8%) was commonest and Oh - with frequency of 1 donor (0.00004%) was least frequent among blood donors (Fig. 1). the prevalence of Rh positive and Rh negative was, 89.3% and 10.7%, respectively.
Fig. 1.
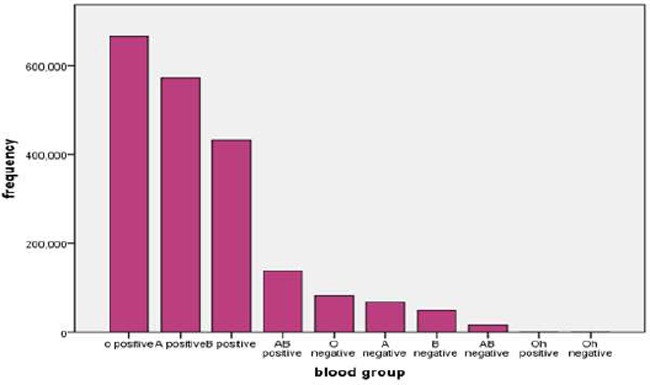
Frequency of blood groups among blood donors referred to Tehran Blood Transfusion Center during 2005-2011
Out of the total blood donors results were positive for one or more infectious disease tests (HBV, HCV, HIV and syphilis) in 10476 donors, 9918 (95%) were males and 558 (5%) were females with male to female ratio of 17.7:1. Mean age of blood donors with positive test results was 38± 10.5 years. The overall prevalence of HBS Ag, anti-HCV, HIV Ag/Ab, and syphilis antibody were 0.39%, 0.11%, 0.005%, and 0.010%, respectively (Table 1).
Table 1.
Frequency of Hepatitis B, Hepatitis C, HIV and Syphilis among blood donors by Year
| Year | Number Of donors | HBV positive | HCV positive | HIV positive | Syphilis positive | ||||
|---|---|---|---|---|---|---|---|---|---|
| Count | % | Count | % | Count | % | Count | % | ||
| 2005-2006 | 303951 | 1745 | 0.57 | 342 | 0.11 | 13 | 0.004 | 23 | 0.008 |
| 2006-2007 | 314203 | 1425 | 0.45 | 328 | 0.10 | 10 | 0.003 | 12 | 0.004 |
| 2007-2008 | 351215 | 1475 | 0.42 | 497 | 0.14 | 22 | 0.006 | 52 | 0.015 |
| 2008-2009 | 351901 | 1236 | 0.35 | 404 | 0.11 | 20 | 0.006 | 82 | 0.023 |
| 2009-2010 | 341260 | 1038 | 0.30 | 358 | 0.10 | 13 | 0.004 | 24 | 0.007 |
| 2010-2011 | 368921 | 932 | 0.25 | 351 | 0.09 | 30 | 0.008 | 19 | 0.005 |
| total | 2031451 | 7851 | 0.39 | 2280 | 0.11 | 108 | 0.005 | 212 | 0.010 |
*The difference between these numbers with the numbers of Table 1 is due to Discrepancy cases (Table 2)
Table 2.
Frequency of Hepatitis B, Hepatitis C, HIV and Syphilis positivity according to blood group types 2005-2011
| Blood Group | Donors (n) | HBV positive | HCV positive | HIV positive | Syphilis positive |
|---|---|---|---|---|---|
| n(%) | n(%) | n(%) | n(%) | ||
| O positive | 665943 | 2396(0.36) | 705(0.11) | 28(0.004) | 61(0.009) |
| A positive | 572999 | 2322(0.40) | 686(0.12) | 40(0.007) | 55(0.009) |
| B positive | 433472 | 1766(0.41) | 510(0.12) | 14(0.003) | 61(0.014) |
| AB positive | 138444 | 575(0.42) | 148(0.11) | 9(0.006) | 15(0.011) |
| Oh positive | 17 | - | - | - | - |
| O negative | 82423 | 311(0.38) | 99(0.12) | 4(0.005) | 7(0.008) |
| A negative | 68379 | 231(0.34) | 65(0.09) | 8(0.011) | 8(0.012) |
| B negative | 50325 | 186(0.37) | 46(0.09) | 4(0.008) | 4(0.008) |
| AB negative | 16083 | 52(0.32) | 14(0.09) | - | - |
| Oh negative | 1 | - | - | - | - |
| Total | 2028086 | 7839(0.39) | 2273(0.11) | 107(0.005) | 211(0.010) |
| Discrepancy cases | 3344 | 12 | 7 | 1 | 1 |
| Total | 2031430 | 7851 | 2280 | 108 | 12 |
Table 2 shows the group wise distribution of Hepatitis B, Hepatitis C, HIV and syphilis. The prevalence of Hepatitis B, Hepatitis C, HIV and syphilis according to Rh status is given in Table 3.
Table 3.
Frequency of Hepatitis B, Hepatitis C, HIV and syphilis positivity according to Rh status 2005-2011
| Blood Group | NO. of Donors | HBV positive | HCV positive | HIV positive | Syphilis positive |
|---|---|---|---|---|---|
| n(%) | n(%) | n(%) | n(%) | ||
| Rh D positive | 1810875 | 7059(0.39) | 2049(0.11) | 91(0.005) | 192(0.011) |
| Rh D negative | 217211 | 780(0.36) | 224(0.10) | 16(0.007) | 19(0.009) |
| Total | 2028086 | 7839*(0.39) | 2273*(0.11) | 107*(0.005) | 211*(0.010) |
In HBV positive donors, a significant association between blood groups (P =0.001, X2=31.902) and Rh status (P=0.029, X2 =4.752) was observed. Percentage of HBS Ag was found to be lower in donors who has blood group “O” and was higher among Rh positive donors.
In HIV positive donors, a significant association between “A” blood group and HIV infection was observed (P =0.032, X2=15.346), but there was no significant association between HIV infection and Rh status (P =0.156, X2=2.015).
In HCV positive donors, there was no Significant association between Hepatitis C infection and ABO blood groups system (P =0.104,X2=11.887) or Rh status (P =0.187, X2=1.741)
In syphilis positive donors, There was no significant association between syphilis infection and ABO blood groups (P =0.229, X2= 9.345) or Rh status (P =0.423, X2 =0.642)
Discussion
After the discovery of blood groups, numerous studies on associations of blood groups and various diseases were performed. Identifying the prognostic and associating factors, which predict the condition of the disease and its response to the treatment, can play an important role in determining the therapeutic strategies.
This study demonstrated that blood group O+ was commonest and Oh - was least frequent among blood donors. This is in agreement with the studies that performed on blood donors (15) and population of Tehran Province (16).
In the current study, the overall prevalence of hepatitis b, hepatitis C, HIV and syphilis infections was 0.39%, 0.11%, 0.005%, and 0.010 %, respectively. Compared with neighboring countries and the international standards this level of prevalence is relatively low (17-25).
The prevalence of all infections was lower among females, maybe females made a smaller section of blood donors in Iran, (only 6% of Iranian blood donors) (26) because they were found to be anemic and did not fulfill the required fitness criteria or maybe, as mentioned in many studies, women were reported as a healthier source of blood in the community (27).
In our study, HBV prevalence among blood donors showed a downward trend over the period of six years. It seems that, vaccination against HBV among all of neonates since 1992 and selected groups such as health care workers, pregnant women, families of HBs Ag positive donors, multi-transfused patients and their families, progress in the recruitment of a safer donor population, confidential unit exclusion (CUE) applying, computerized data registry of blood donors, increase public knowledge about blood-borne infections and routes of transmission, may also have contributed to the observed decline (28).
Overall, the prevalence of HCV decreased in six years however, fluctuated during the period under study, peaking in 2007. Such variation could be as a result of a combination of several factors including a change in screening reagent used, actual changes in population risks, changes in basic population which donor recruitment was done from that, or effectiveness of prospective donor screening measures (29). But it should be noted that people who may have been infected in the past years may identify in this year.
HIV and RPR trends were shown a similar pattern, but RPR confirmed rates over the time were shown more rapid than HIV confirm results. It is essential to watch HIV after observing the raising pattern of syphilis due to changes in high risk behaviors in the community. It should be noted that the results of our study does not necessarily reflect the results of community because population of blood donors are predefined groups and most of them are in the sexually active age group.
So far, in several studies the association of specific blood groups to certain diseases has been investigated. Prevalence of cardiovascular disease, ischemic heart disease, venous thrombosis, atherosclerosis, squamous cell carcinoma and basal cell carcinoma is higher in individuals with non-O blood groups (30-34). B antigen links with increased risk of ovarian cancer and diabetes mellitus (6, 35). Prevalence of gastric cancer, pancreatic cancer and salivary gland tumors is higher in “A” blood group (36-38). “O” blood group individuals are known to have a higher risk of cholera, gastro-intestinal infection with E. coli, peptic ulcer, duodenal ulcer, chronic myelocytic leukemia, acute lymphocytic leukemia and thalassemia (39-44). HTLV-1, cervical carcinoma and pulmonary tuberculosis have reported to be more common in persons with blood group “AB” (45-47). On the other hand, some studies demonstrated association of specific blood groups and resistance to certain infections for example blood groups “O” and “B” are associated with resistance to small pox (48), blood group “Pk” is associated with resistance to HIV-1 (49) and the absence of the Duffy blood group is associated with resistance to Plasmodium vivax (6).
In the present study, a significant association between HBV with ABO and Rh blood groups was observed. This is comparable with previous findings (50), but it differs with other studies (51–54). Our results show that the presence of “O” blood group may significantly decrease the risk of hepatitis B and the distribution of Rh in HBV infected individuals was higher between Rh positive donors. In similar finding that performed on patients with hepatitis B in the hemodialysis center (55), blood group “O” was more frequent among people with HBV, but in their study it was not significant association between O blood group and HBV (56). In another study, higher frequency of blood group ‘‘B” in HBV infected patients was reported but there was no significant correlation between HBV infection and blood groups (51). In one study about patients with chronic hepatitis B, individuals with blood group “A” compared with other blood groups had higher serum bilirubin level, prothrombin time and higher risk of Hepato-cellular carcinoma and significant association was found between the presence of HBe Ag and blood groups (57). Meo et al. showed a significant association between hepatitis B and secretor status (58).
We did not find any association between sero-positivity of HCV and ABO/Rh antigens. This is in concurrence with previous reports (59). However, in some studies, with less population, a significant association between blood groups and hepatitis C was reported (60-61). In a systematic review on 14 papers there was no significant association between four types of blood groups and HCV infection (62). In a study on patients with chronic hepatitis C infection, it was observed that non-O blood group was associated with increased severity of fibrosis (63).
In the present study, there was a significant association between HIV infection and blood groups. Blood group ‘‘A” was the commonest blood group in HIV infected patients and percentage of HIV (Ag/Ab) was lower in donors who has blood group “B”. The similar results were reported by Amidu, et al. (64). In one study patients who were HIV sero-positive, “O positive” was the most prevalent blood group and “AB negative” blood group was the least prevalent (65). In Nigeria in pregnant women, the prevalence of blood group “O positive” was higher than in the general population (66). Farhud et al. showed a significant decrease of “B” blood group in anti-HIV positive individuals (67).
A study in UK showed that ABO histo-blood group sugars were detected on the viral envelope protein, gp120. Thus incorporation of ABO antigens by HIV-1 may affect transmission of virus between individuals of discordant blood groups by interaction with host natural antibody and complement (68). We found no significant association between syphilis infection and blood groups in this study, similar to previous finding (52). In other study there was no association between syphilis and blood groups (69). In our study the prevalence of hepatitis B, hepatitis C, HIV, and syphilis infections was higher in subjects with RhD+, one reason for this, is the higher prevalence of RhD+ in the population of blood donors.
The mechanism between blood type and infections remained undefined, which may be related to red cell immune adherence function among persons with different blood types (70). As the Swedish researchers investigated cell surface–expressed Pk in HIV infection and concluded that Pk expression strongly influences susceptibility to HIV-1 infection, which implicates Pk as a new endogenous cell-surface factor that may provide protection against HIV-1 infection and showed that Individuals with high Pk levels exhibited a greater natural resistance to HIV infection, (49) ABO and Rh blood groups polymorphisms may be involved in viral transmission.
This study also justifies the statement that “in any country, as the proportion of the population with infectious diseases, such as HIV and hepatitis, increase the proportion of the population who are eligible to donate blood falls (71).
Conclusion
From the above data it is evident that blood group type of an individual does have some biological role in case of hepatitis B and HIV infections. Further studies regard in association of HBV and HIV infections with blood groups in different communities and even in national level is necessary to get more knowledge about this aspect.
Ethical considerations
Ethical issues (Including plagiarism, Informed Consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc) have been completely observed by the authors.
Acknowledgements
The authors would like to thank all of coworkers in TBTC. The authors declare that there is no conflict of interests.
References
- Anonymous (2012). Table of blood group systems. International Society of Blood Transfusion (ISBT). Available from: www.ibgrl.blo-od.co.uk/isbt.
- Garratty G, Dziik W, Issitt PD, Lublin DM, Reid ME, Zelinski T (2000). Terminology for blood group antigens and genes – Historical origins and guideline in the new millennium. Transfusion, 40: 477–89. [DOI] [PubMed] [Google Scholar]
- Mollison PL (1994). The genetic basis of Rh blood group system. Transfusion, 34: 539–41. [DOI] [PubMed] [Google Scholar]
- Lease MEE, Bazuaye GN (2008). Distribution of ABO and Rh-D blood groups in the Benin area of Niger-Delta: Implication for regional blood transfusion. Asian J Transfus Sci, 2(1): 3–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerald L, Douglas M (2000). Principles and practice of infectious disease. 5th Ed Churchill, pp.: 1–39. [Google Scholar]
- Ahmad J, Taj AS, Rahim A, Shah A, Rehman M (2004). Frequency of Hepatitis B and Hepatitis C in healthy blood donors of NWFP: a single center experience. J Postgrad Med Inst, 18(3): 343–52. [Google Scholar]
- Gottlieb MS, Schroff R, Schanker HM, Schanker HM, Weisman JD, Thim Fan DP, Wolf RA, Saxon A (1981). Pneumocystis carinii pneumonia and mucosal candidiasis in previously healthy homosexual men: evidence of a new acquired cellular immunodeficiency. N Eng J Med, 305: 1425–1431. [DOI] [PubMed] [Google Scholar]
- Weller IVD, Comlon CP, Peto TEA.HIV infection and AIDS, Oxford Textbook of Medicine on CD-ROM Version 1.0: pp.: 10–29. [Google Scholar]
- Branch DR (2010). Blood groups and susceptibility to virus infection: new developments. Curr Opin Hematol, 17: 558–564. [DOI] [PubMed] [Google Scholar]
- Anonymous (2012). Hepatitis B fact sheet number 204. World Health Organization. Available from: www.who.int/mediacentre/factsheets/fs204/en.
- Anonymous (2012). Hepatitis C Fact sheet number 164. World Health Organization, Available from : www.who.int/mediacentre/factsheets/fs164/en.
- Murray P, Rosenthal K, Kobayashi G, faller M (2002). Medical Microbiology. Mosby company, St. Loius, pp.: 379–380. [Google Scholar]
- Gerbase AC, Rowley JT, Heymann DH, Berkley SF, Piot P (1998). Global prevalence and incidence estimates of selected curable STDs. Sex Transm Infect, 74: S12–S16. [PubMed] [Google Scholar]
- Buseri FI, Muhibi MA, Jeremiah ZA (2009). Sero-epidemiology of transfusion-transmissible infectious diseases among blood donors in Osogbo, south-west Nigeria. Blood Transfus, 7(4): 293–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pourfathollah AA, Oody A, Honarkaran N (2003). Geographical distribution of ABO and Rh (D) blood groups among Iranian blood donors in the year 1361(1982) as compared with that of the year 1380 (2001). Blood Journal, 1(1): 11–19 [in Farsi]. [Google Scholar]
- Farhud DD, Eftekhari A (1994). Blood groups distribution in Iran. Iranian J Publ Health, 23(1): 1–10. [Google Scholar]
- Khedmat H, Alavian SMM, Miri SM, Amini M, Abolghasemi H, Hajibeigi B, Alaeddini F, Fallahian F (2009). Trends in Seroprevalence of Hepatitis B, Hepatitis C, HIV, and Syphilis Infections in Iranian Blood Donors from 2003 to 2005. Hepat Mon, 9(1): 24–28. [Google Scholar]
- Salawu L, Bolarinwa RA, Adegunloye AB, Muraina HA (2010). HBs Ag, anti-HCV, anti-HIV and VDRL in blood donors: Prevalence and trends in the last three and a half years in a tertiary health care facility in Ile-Ife, Nigeria. Int J Med, 2(11): 335–341. [Google Scholar]
- Gupta N, Kumar V, Kaur A (2004). Seroprevalence of HIV, HBV, HCV and syphilis in voluntary blood donors. Indian J Med Sci, 58: 255–257. [PubMed] [Google Scholar]
- El-Hazmi MM (2004). Prevalence of HBV, HCV, HIV-1,2 and HTLV-?/Π infections among blood donors in a teaching hospital in the central region of Saudi Arabia. Saudi Med, 25: 26–33. [PubMed] [Google Scholar]
- Jehangir W, Ali F, Shahnawaz U (2005). Prevalence of Hepatitis B, C and HIV in blood donors of south PUNJAB. Pak J Med Sci, 20(1): 24–8. [Google Scholar]
- Dessie A, Abera B, Wale F (2007). Seroprevalence of major blood-borne infections among blood donors at Felege Hiwot referral hospital, northwest Ethiopia. Ethiop J Health Dev, 21(1): 68–69. [Google Scholar]
- Anonymous (1999). Hepatitis C global prevalence. Weekly Epidemiological Record (WHO). available from: www.who.int/docstore/wer/pdf/1999/wer7449.pdf
- Bhawani Y, Rao P, Sudhakar V (2010). Seroprevalence of transfusion transmissible infections among blood donors in a tertiary care hospital of Andhra Pradesh. Biol Med, 2 (4): 45–48. [Google Scholar]
- Likatavicius G, Hamers FF, Downs AM, Alix J, Nardone A (2007). Trends in HIV prevalence in blood donations in Europe, 1990–2004. AIDS, 21(8): 1011–8. [DOI] [PubMed] [Google Scholar]
- Cheraghali AM (2012). Overview of Blood Transfusion System of Iran: 20022011. Iranian J Publ Health, 41(8): 89–93. [PMC free article] [PubMed] [Google Scholar]
- Javadzadeh Shahshahan H (2007). Why don’t women volunteer to give blood? A study of knowledge, attitude and practice of women about blood donation, Yazd, Iran, 2005. Transfus Med, 17: 451–454. [DOI] [PubMed] [Google Scholar]
- AminiKafi-abad S, Rezvan H, Abolghasemi H (2009). Trends in prevalence of hepatitis B virus infection among Iranian blood donors, 1998–2007. Transfus Med, 19: 189–194. [DOI] [PubMed] [Google Scholar]
- Glynn SA, Kleinman SH, Schreiber GB, Busch MP, Wright DJ, Smith JW, Nass CC, Williams AE (2000). Trends in incidence and prevalence of major transfusion-transmissible viral infections in US blood donors, 1991 to 1996. JAMA, 284: 229–235. [DOI] [PubMed] [Google Scholar]
- Khan MI, Micheal S, Akhtar F, Naveed A, Ahmed A, Qamar R (2009). Association of ABO blood groups with glaucoma in the Pakistani population. Can J Ophthalmol, 44: 582–586. [DOI] [PubMed] [Google Scholar]
- Gill JC, Endres-Brooks J, Bauer PJ, Marks WJ, Montgomery RR (1987). The effect of ABO blood group on the diagnosis of von Willebrand diseases. Blood, 69(6): 1691–1695. [PubMed] [Google Scholar]
- Wolpin BM, Kraft P, Gross M, Helzlsouer K (2010). Pancreatic cancer risk and ABO blood group alleles: results from the pancreatic cancer cohort consortium. Cancer Res, 70 (3): 1015–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amundadottir L, Kraft P, Stolzenberg-Solomon RZ, Fuchs CS (2010). Genome-wide association study identifies variants in the ABO locus associated with susceptibility to pancreatic cancer. Nat Genet, 41 (9): 986–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fahud DD, Mohebb M, Farhud I, Khavari-khorasani H (1992). ABO and Rh blood in Cardiovascular Disease from Iran. Iranian J Publ Health, 21(1): 1–10. [Google Scholar]
- Gates MA, Wolpin BM, Cramer DW, Hankinson SE, Tworoger SS (2010). ABO blood group and incidence of epithelial ovarian cancer. Int J Cancer, 128 (2): 482–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aird I, Bentall HH, Roberts JA (2011). A relationship between cancer of stomach and the ABO blood groups. Br Med J, 1 (4814): 799–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choo QL, Kuo G, Weiner AJ (1998). Isolation of a DNA clone derived from a blood borne non A, non B viral hepatitis genome. Science, 244(3): 362–4. [DOI] [PubMed] [Google Scholar]
- Pinkston JA, Cole P (1996). ABO blood groups and salivary gland tumors. Cancer Causes Control,7: 572–74 . [DOI] [PubMed] [Google Scholar]
- Harris JB, Khan A, LaRocque RC, Dorer DJ, Chowdhury F, Faruque AS, Sack D, Ryan ET, Qadri F, Calderwood S (2005). Blood group, immunity, and risk of infection with Vibrio cholerae in an area of endemicity. Infect Immun, 73(11): 7422–7427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blackwell CC, Dundas S, James VS (2002). Blood group and susceptibility to disease caused by Escherichia coli O157. J Infect Dis, 185(3): 393–396. [DOI] [PubMed] [Google Scholar]
- Aird I, Bentall HH, Mehigan JA, Roberts JAF (1954). The blood groups in relation to peptic ulceration and carcinoma of the colon, rectum, breast and bronchus. BMJ, 2(4883): 315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke CA, Cowan WK, Edwards JW (1955). The relationship of ABO blood groups to duodenal and gastric ulceration. BMJ, 2(4940): 643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farhud DD, Sadighi H, Andonian L, Safari M (1995). Study of sex ratio, ABO and Rh blood groups distribution in some haematological and lymphatic disease in Iran. Iranian J Publ Health, 24(3): 9–14. [Google Scholar]
- Farhud DD, Sadighi H, Mohammadhasani MR, Samavat A, Zakizadeh R, Yazdani Z (1996). Study of sex, age and blood groups (ABO, Rh) distribution in Thalassemia patients in Iran. Iranian J Publ Health, 25(1): 1–8. [Google Scholar]
- Ayatollahi H, Rafatpanah H, Khayyami ME, Sayyadpour D, Ravarian M, Sadeghian MH, Izadi N, KhabbazKhoob M (2008). Association between ABO and Rhesus blood group systems among confirmed human T lymphotropic virus type 1-infected patients in Northeast Iran. AIDS Res Hum Retroviruses, 24(9): 1155–1158. [DOI] [PubMed] [Google Scholar]
- Tyagi SP, Tyagi GK, Pradhan AC (1967). ABO blood in relation to carcinoma cervix. Ind J Med Sci, 21: 611. [PubMed] [Google Scholar]
- Jains RC (1970). ABO Blood group and Pulmonary tuberculosis. Tubercle, 51: 322–323. [DOI] [PubMed] [Google Scholar]
- Garratty G (2005). Relationship of blood groups to disease: do blood groups antigens have a biological role? Rev Med Inst Mex Senguro Soc, 43 (1): 113–21. [Google Scholar]
- Lund N, Olsson ML, Ramkumar S, Sakac D, Yahalom V, Levene C, Hellberg A, Ma XZ, Binnington B, Jung D, Lingwood CA, Branch DR (2009). The human Pk histo-blood group antigen provides protection against HIV-1 infection. Blood, 113: 4980–4991. [DOI] [PubMed] [Google Scholar]
- Dirisu JO, Alli TO, Adegoke AO, Osazuwa F (2011). A Survey of prevalence of serum antibodies to human immunodeficiency deficiency virus (HIV), hepatitis B virus (HBV) and hepatitis C virus (HCV) among blood donors. N Am J Med Sci, 3(1): 35–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behal R, Jain R, Behal KK, Bhagoliwal A, Aggarwal N, Dhole TN (2008). Seroprevalence and risk factors for hepatitis B virus infection among general population in Northern India. Arq Gastroenterol, 45: 137–40. [DOI] [PubMed] [Google Scholar]
- Emeribe AO, Ejezie GC (1992). ABO blood groups distribution in relation to Hepatitis B surface antigen and the presence of lipoidophil antibodies. East Afr Med J, 69: 146–8. [PubMed] [Google Scholar]
- Das S, Kumar MH (2012). Association of blood group types to hepatitis B and hepatitis C viruses among blood donors. A five years institutional based study. Int J Appl Basic Med Res, 2 (1): 191–195. [Google Scholar]
- Farzadegan H, Harbour C, Ala F (1979). The prevalence of hepatitis B surface antigen and it’s antibody in blood donors and high risk groups in Iran. Vox Sang, 37: 182–6. [DOI] [PubMed] [Google Scholar]
- Lewkonia RM, Finn R (1969). ABO blood distribution in serum hepatitis. BMJ, 3(6) : 168–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emami-Naeini A, Rostami M, Emami-Naeini S (2010). Chronic viral hepatitis and their relation to ABO blood groups and rhesus (Rh) factor. Med Case Stud, 1: 5–7. [Google Scholar]
- Li Q, Yu CH, Yu JH, Liu L, Xie SS (2012). ABO Blood Group and the Risk of Hepatocellular Carcinoma: A Case-Control Study in Patients with Chronic Hepatitis B. PLoS One, 7(1): e29928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meo SA, Assad AA, Sanie FM, Baksh ND, Al-Qahtani A, Shaikh ZA (2010). Transmission of Hepatitis-B Virus Through Salivary Blood Group Antigens in Saliva. J Coll Physicians Surg Pak, 20 (7): 444–448. [PubMed] [Google Scholar]
- Jeremiah ZA, Koate B, Buseri F, Emelike F (2004). Prevalence of antibodies to hepatitis C virus in apparently healthy Port Harcourt blood donors and association with blood groups and other risk indicators. J Infect Dis, 186(6): 1159–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El–Gilany AH, El–Fedawy S (2006). Blood borne infections among student voluntary blood donors in Mansoura University, Egypt. East Mediterr Health J, 12: 742–48. [PubMed] [Google Scholar]
- Luksamijarulkul P, Thammata N, Tiloklurs M (2002). Seroprevalence of Hepatitis B, Hepatitis C and Human Immunodeficiency Virus among blood donors, Phistanulok Regional Blood Centre, Thailand. Southeast Asian J Trop Med Public Health, 33: 272–79. [PubMed] [Google Scholar]
- Gao X, Cui Q, Shi X, SU J, Peng ZH, Chen X, Lei N, Ding K, Wang L, Yu R, Wang N (2011). Prevalence and trend of hepatitis C virus infection among blood donors in Chinese mainland: a systematic review and meta-analysis. BMC Infect Dis, 11: 88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poujol-Robert A, Boelle PY, Wendum D, Poupon R, Robert A (2006). Association between ABO blood group and fibrosis severity in chronic Hepatitis C infection. Dig Dis Sci, 51: 1633–36. [DOI] [PubMed] [Google Scholar]
- Amidu N, Owiredu W, Addai-Mensah A, Alhassan A, Quaye L, Batong B (2010). Seroprevalence and Risk Factors for Human Immunodeficiency Virus, Hepatitis B and C Viruses Infections among Blood Donors at the Bolgatanga Regional Hospital in Bolgatanga, Ghana. J Ghana Sci Ass, 12 (1): 10–15. [Google Scholar]
- Banu A, Ahmed SM, Shastri S (2011). Distribution Of ABO And Rh Blood Groups In HIV Seropositives at an Integrated Counseling And Testing Centre In Karnataka, India. SAARC, 8(2): 42–45. [Google Scholar]
- Nneli RO, Ekpo BO, Ohaeri OC, Egene J (2004). Prevalence of Rh and ABO blood groups in HIV seropositive pregnant women in Enugu, Nigeria. Niger J Physiol Sci, 19(1–2): 7–9. [Google Scholar]
- Farhud DD (1987). ABO and Rh blood groups distribution in Hemophilia and anti HIV positive individuals. Iranian J Publ Health, 16(1): 1–8. [Google Scholar]
- Neil SJ, McKnight A, Gustafsson K, Weiss RA (2004). HIV-1 incorporates ABO histo-blood group antigens that sensitise virions to complement-mediated inactivation. Blood, 11: 42–67. [DOI] [PubMed] [Google Scholar]
- Sathe PV, Toshniwal MH, Gosawi SB (1973). ABO Blood Groups and Sero-positivity For Syphilis in Blood Donors and Antenatal Cases. Indian J Dermatol Venereol Leprol, 39(4): 170–171. [PubMed] [Google Scholar]
- Rui ZL (1998). The relationship of hepatitis C virus infection and blood types explored preliminarily. JZMU, 8: 493. [Google Scholar]
- Richards C, Holland P, Kuramoto K (1991). Prevalence of antibody to hepatitis C virus in a blood donor population. Transfusion, 31(11): 109–13. [DOI] [PubMed] [Google Scholar]


