Abstract
The construction of vascular conduits is a fundamental strategy for surgical repair of damaged and injured vessels resulting from cardiovascular diseases. The current protocol presents an efficient and reproducible strategy in which functional tissue engineered vessel grafts can be generated using partially induced pluripotent stem cell (PiPSC) from human fibroblasts. We designed a decellularized vessel scaffold bioreactor, which closely mimics the matrix protein structure and blood flow that exists within a native vessel, for seeding of PiPSC-endothelial cells or smooth muscle cells prior to grafting into mice. This approach was demonstrated to be advantageous because immune-deficient mice engrafted with the PiPSC-derived grafts presented with markedly increased survival rate 3 weeks after surgery. This protocol represents a valuable tool for regenerative medicine, tissue engineering and potentially patient-specific cell-therapy in the near future.
Keywords: Bioengineering, Issue 97, stem cells, partially induced pluripotent stem cells, tissue engineering, bioreactor, vascular differentiation, vessel graft, mouse models
Introduction
The construction of vascular conduits is a fundamental strategy for surgical repair of damaged and injured vessels resulting from cardiovascular diseases. To date, graft materials used in surgery include biocompatible synthetic polymers (polytetrafluoroethylene [Teflon], expanded polytetrafluoroethylene [ePTFE; Gore-Tex] or polyethylene terephthalate [Dacron]), allografts, autologous tissue (pericardium or saphenous vein) and xenografts1. Whilst artificial grafts (e.g., Gore-Tex and Dacron) are most commonly used, these materials likely cause numerous short- and long-term complications that include stenosis, calcium deposition, thrombo-embolization and infections. Although patients with biological grafts present with decreased thrombo-embolic events, they still encounter limitations such as secondary graft failure and shortened durability owing to calcification degradation2. Therefore, despite significant improvements in surgical techniques over the years, researchers and clinicians are still burdened with the need for identifying the ideal conduit for vascular diseases. More recently, the research field of vascular tissue engineering has generated a concept in which cells are incorporated into biodegradable scaffolds, with the aim of creating a biomimetic environment that epitomizes a functional vessel for successful grafting1. Fundamentally, the success of the vascular constructs depend on three essential components; cells that comprise the scaffold, i.e., an endothelial cell inner layer and a smooth muscle cell layer, a scaffold containing the appropriate extracellular matrix to provide mechanical properties comparable to the native vasculature, and the molecular/cellular signaling that is required for initiating/regulating repair.
Long term graft patency and sustained development of the neo-tissues are highly dependent on effective cell seeding of scaffolds, thereby rendering the decision of cell type of critical importance. Several reports demonstrate the use of mature endothelial and smooth muscle cells from various sources to develop small diameter conduits3-6. Although promising, the lack of sufficient autologous vessels to obtain mature endothelial and smooth muscle cells remain a considerable burden. More recently, stem cells from various sources have been exploited for vascular tissue engineering applications. Indeed, a variety of stem cell types including embryonic stem cells7, induced pluripotent stem cells (iPSCs)8,9, PiPSC10,11, bone marrow-derived mononuclear cells12, mesenchymal stem cells13, endothelial progenitor cells and adult vessel wall-derived stem cell antigen-1 (Sca-1)+ stem/progenitor cells14,15 have all been demonstrated to be capable of differentiation into either functional endothelial or smooth muscle cells in response to defined media and culture conditions. Furthermore, the unlimited self renewal capacity of the stem cells make them better candidates unlike mature endothelial and smooth muscle cells which can only divide for a finite number of times before undergoing growth arrest and senescence.
The selection of scaffold material to generate successful tissue engineered vessel for grafting depends on several factors such as biocompatibility, biomechanical properties, and rate of biodegradation. Fundamentally, materials used to create scaffolds for the grafts should be biodegradable and will not mount unnecessary recipient immune responses. Additionally, it must encompass a suitable porosity and microstructure for cell attachment and subsequent survival. To date, the most common materials used for scaffolds in vascular tissue engineering include polymers of polyglycolic acid, polylactic acid, and poly ε-caprolactone16. More recently, decellularized biological materials have also been applied with some success. Several laboratories have shown that seeding decellularized human, canine or porcine vessels with autologous cells provided a biological graft that resisted clotting and intimal hyperplasia17-19. Other strategies in vascular tissue engineering include extracellular matrix proteins-based vascular grafts e.g., seeding cells in fibrin gel13 and generating cell sheets without scaffold support20, 21.
The current protocol demonstrates the differentiation of human PiPSC into functional endothelial and smooth muscle cells, the generation of a bioreactor consisting of a decellularized vessel scaffold to harbor functional PiPSC-derived vascular cells, and grafting of the tissue engineered vessels into severe combined immunodeficiency (SCID) mice. PiPSC are an optimum cell type to use for tissue engineering of vessel grafts because these cells do not form tumors in mice or raise ethical and allo-immune responses. Furthermore, we have shown that the strategy for generating PiPS-endothelial cells and PiPS-smooth muscle cells is efficient and reproducible10,11. Thereafter, we designed a decellularized vessel for seeding of PiPSC-derived vascular cells to closely mimic the matrix proteins that exists within a native vessel, thus enhancing grafting and survival efficacy. Furthermore, the decellularization of the vessels prior to PiPSC seeding prevents the occurrence of inflammatory responses mounted by immune cell types such as macrophages. More importantly, this protocol does not only represent a methodology to generate promising vascular conduits for translation into humans, but also provides valuable means of studying and understanding the molecular mechanisms that govern vascular tissue regeneration through mouse models.
Protocol
Perform all animal experiments according to protocols approved by the Institutional Committee for Use and Care of Laboratory Animals.
1. Preparation of Culture Media
Make culture media for human fibroblast cell line CCL-153: F-12K Medium, 10% fetal bovine serum (FBS) and 100 U/ml penicillin and streptomycin.
Make Reprogramming Media for PiPSC generation: Knockout Dulbecco’s modified eagle’s medium (DMEM) containing 20% Knockout Serum Replacement, 0.1 mM β-mercaptoethanol, 0.1 mM Minimum Essential Medium (MEM) Non-Essential Amino Acids, 10 ng/ml basic Fibroblast Growth Factor 2 (bFGF-2) and 100 U/ml penicillin and streptomycin. Add bFGF-2 freshly each time before using the media.
Make Differentiation Media (DM) to induce smooth muscle cell (SMC) differentiation: α-MEM media containing 10% FBS, 0.1 mM β-mercaptoethanol, 100 U/ml penicillin and streptomycin and 25 ng/ml Platelet Derived Growth Factor (PDGF-ββ).
Make Endothelial Differentiation Media (EC-DM) to induce endothelial cell (EC) differentiation: Endothelial growth media-2 (EGM-2) media containing 50 ng/ml Vascular Endothelial Growth Factor (VEGF) and 100 U/ml penicillin and streptomycin.
2. Reprogramming Human Fibroblasts into Partially-induced Pluripotent Stem Cells (PiPSC)
Culture human fibroblast cell line CCL-153 on 0.04% gelatin solution coated flasks in culture medium.
Passage cells every 3 days at a ratio of 1:6. Use cells before passage 9 for optimal efficiency of PiPSC generation. Cells are ready for transfection upon reaching 80 - 90% confluency.
Linearize polycistronic plasmid pCAG2LMKOSimO containing 4 reprogramming factors octamer-binding transcription factor 4 (OCT4), SOX2, Kruppel-like factor 4 (KLF4) and C-MYC (pCAG-OSKM). Digest 5 µg of plasmid with 5 units of PvuI restriction enzyme for 3 hr at 37 °C. Purify the plasmid with a commercial kit according to manufacturer’s protocol.
Transfect 2 x 106 human fibroblasts with 4 µg of linearized pCAG-OSKM plasmid by electroporation with human dermal fibroblast (NHDF) nucleofection kit according to manufacturer’s protocol. Gently seed transfected cells onto pre- 0.04% gelatin coated T25 flask containing 5 ml of pre-warmed Reprogramming Media.
After 24 hr, change medium with supplements of 25 µg/ml neomycin to select a pure population of transfected cells.
Change medium every other day until day 4. Note: Human fibroblasts become PiPSC after 4 days of reprogramming.
3. Differentiation of PiPSC into Endothelial and Smooth Muscle Cells
Seed PiPSC on collagen IV pre-coated dishes containing DM for 4 days to induce differentiation into SMCs. Change medium every other day until day 4.
Seed PiPSC on collagen IV pre-coated dishes containing endothelial-DM for 6 days to induce differentiation into endothelial cells. Change medium every other day until day 6.
4. Decellularized Aorta Graft Preparation
Note: All solutions and equipment should be sterile.
Sacrifice the mouse by cervical dislocation and fix the mouse in a supine position under dissection microscope.
Cut through the sternum and around the rib cage to open the thoracic cavity. Remove the heart, lungs and esophagus to expose the aorta. Gently remove the peri-aorta fat with forceps.
Cut the aorta from the anterior end with scissors and gently hold the end with blunt forceps. Detach the aorta from the spine column behind by blunt dissection. Carefully close all the branching arteries from the aorta by ligation with a bipolar electrocoagulator and cutting from the far end of the ligation with scissors.
Use a 5 ml syringe to flush the aorta lumen with 3 ml of saline solution containing 100 U of heparin to prevent the formation of blood clots.
Cut the posterior end of the aorta before it branches into the renal. Keeping the integrity of the aorta is very important during the whole procedure.
Flush the aorta lumen with 5 ml of 0.075% sodium dodecyl sulphate (SDS) solution diluted in phosphate buffered saline (PBS).
Soak the thoracic aorta in 0.075% SDS solution in a 10 cm Petri dish. Place the Petri dish on an orbital shaker for 2 hr at 150 rpm at RT.
Flush the aorta lumen with 5 ml of PBS.
Soak the aorta in PBS in a 10 cm Petri dish. Place the Petri dish on the orbital shaker for 2 hr at 150 rpm at RT. Refresh PBS every 20 min.
Flush the aorta lumen with 5 ml of PBS.
Keep decellularized aorta graft in PBS at 4 °C for up to one week.
5. Dual Seeding of PiPSC and Bioreactor Conditioning
Note: All solutions and equipment should be sterile. Perform all operations in a tissue culture hood.
Assemble the bioreactor flow circuit as illustrated in Figure 1. Connect incubation chamber, media reservoir, peristaltic pump and compliance chamber with tubing. Minimal volume of medium needed for circulation is 40 ml.
Pre-condition the decellularized vessel with culture medium by soaking the aorta in DM medium in a 10 cm Petri dish. Place the Petri dish on the orbital shaker for 1 hr at 50 rpm at RT.
Insert 1 cm length Nylon tubes (OD 0.9 mm, ID 0.75 mm) into both ends of the decellularized vessel under microscope. Tie the vessel and the tubes with 8-0 silk sutures.
Assemble the decellularized aorta graft in the incubation chamber by connecting the Nylon tubes with the inlet and outlet ports (1/32” tubing) from the chamber wall. Maintain incubation chamber with 5mls of medium each time.
Trypsinize PiPSC by adding pre-warmed trypsin to cover the culture dish and gently rock the dish 10 times. Discard the trypsin and leave the dish in incubator for 2 - 3 min. Add pre-warmed culture medium in the dish and mix the medium with the cells.
Count cell number using a hemocytometer. Centrifuge two aliquots of cell suspensions containing 5 x 105 cells each for 5 min at 300 x g. Aspirate the supernatant completely.
After aspirating the supernatant completely, resuspend 1 pellet of the PiPS cell pellets in 50 µl of DM. Inject this cell suspension into the decellularized vessel lumen.
Then, resuspend the other PiPS cell pellet in 100 µl of Matrigel. Carefully pipette the mixture onto the decellularized aorta graft.
Wait for 10 - 15 min until the mixture turns into a gel-like state and evenly wraps around the vessel external surface. Fill the incubation chamber with DM.
Place the whole bioreactor setting in a 5% CO2 incubator at 37 °C. Manually rotate the decellularized graft 90° around the longitudinal axis every half an hour in the first 2 hr.
Keep static culture for 12 hr to enable cell adhesion.
Deliver DM through the lumen by the peristaltic pump to induce smooth muscle cell differentiation. Start initial flow rate at 5 ml/min and stepwise increase to 20 ml/min over 24 hr.
Keep the circulating medium flow rate at 20 ml/min for 24 hr.
Stop the medium flow and move the bioreactor setting out of the incubator.
Re-seed the lumen of the graft with PiPSC. Trypsinize, count and centrifuge 1 x 106 PiPSC as in steps 5.5 - 5.6. Resuspend the cells in 50 µl of EGM-2 medium containing 50 ng/ml VEGF. Inject the cell mixture into the lumen of the graft.
Change the medium in the incubation chamber and whole circulation to EGM-2 medium containing 50 ng/ml VEGF to induce endothelial differentiation.
Move the bioreactor setting back to the incubator. Manually rotate the graft 90° every 30 min in the first 2 hr and then keep a static culture for 12 hr.
Start circulating flow from 5 ml/min and stepwise increase to 35 ml/min. Keep the flow rate at 35 ml/min for 5 days. Change circulating and chamber medium every other day.
Harvest the engineered graft for further grafting to mouse.
6. Grafting of Double-seeded PiPSC Graft into Mice
Use NOD.CB17-Prkdcscid/NcrCrl male mice as vessel graft recipients. Always ensure that the mice are about 10 weeks old, weigh approximately 25 - 35 g, and are in good health conditions.
- Anesthetize recipient mouse by administering a combination of Hypnorm (25 mg/kg) and Hypnovel (25 mg/kg) intraperitoneally. Apply petrolatum ophthalmic ointment on eyes to prevent dryness while under anesthesia. Confirm efficient anesthetization by ensuring that mice have relaxed muscles and are breathing steadily.
- Fix the mouse in a supine position with its neck shaved and extended. Administer atropine sulfate (1.7 mg/kg) in combination with the anaesthetics to ensure that the mouse respiratory tract remains clear.
Prepare a midline incision from the mandible to sternum of the mouse. Under a dissecting microscope with 5- to 10-fold amplification, lift the right salivary glands laterally and remove the right cleidomastoid muscle to expose the right common carotid artery.
Gently remove attached tissues to mobilize the right common carotid artery from the distal end toward the proximal end. Ligate the middle portion of the common carotid artery twice with an 8-0 silk suture and dissect between the two ties.
Pass through a cuff made of autoclavable nylon tube in each vessel end and fix each end with microhemostat clamps.
- Remove suture tie on one end and apply a drop of heparin (100 U/ml). Immediately after, invert the distal end of the artery to cover the whole cuff body and fix the inverted vessel with an 8-0 silk suture to the cuff.
- Repeat the same procedure to the other portion of the artery. Flush artery with saline solution to remove blood clots.
Implant a decellularized vessel graft between two ends of the carotid artery by sliding the decellularized vessel ends of the over the artery cuffs and fixing it with 8-0 silk sutures. Remove vascular clamps from either ends before evaluating the pulsation of the graft.
Place the right salivary gland back to its original position. Close the skin on the surgical location with an interrupted suture using a 6-0 polyglactin suture.
Consistently observe vital signs of mouse after the procedure is completed, until it resumes consciousness. Sacrifice recipient mice by cervical dislocation and harvest vessel grafts either 24 hr or 3 weeks later for further analysis.
Representative Results
The successful generation of PiPSC was confirmed 4 days after nucleofecting human fibroblasts with a linearized pCAG2LMKOSimO plasmid carrying 4 transcription factors, OCT4, SOX2, KLF4 and c-MYC (OSKM). PiPSC displayed a markedly distinct phenotype when compared to fibroblasts (Figure 2A) and expressed the 4 reprogramming factors at mRNA (Figure 2B) and protein (Figure 2C) levels10. The efficacy of a PiPSC-based vascular graft is highly dependent on the ability of the PiPSC to differentiate into both endothelial and smooth muscle lineages. It is therefore critical to confirm these properties of PiPSC in vitro by differentiating the cells in defined media before utilizing them to generate vessel grafts. Figure 3 shows the capacity of PiPSC to differentiate into functional endothelial cells at both gene (Figure 3A) and protein (Figure 3B-D) levels, based on endothelial-specific markers10. Similarly, PiPSC are also able to differentiate into the smooth muscle lineage in response to specific media (Figure 3E-H)11.
Whole aorta decellularization was achieved by treatment with SDS, an anionic detergent that lyses cells and solubilizes cytoplasmic components. After 2 hr of treatment, the decellularized aorta appeared as a translucent acellular scaffold when compared to a freshly harvested aorta (Figure 4A-B)22. Histological evaluation in Figure 4C-F illustrates the absence of nuclei or cytoplasmic staining in decellularized vessels, but not in the normal mouse aorta. Following double seeding of PiPSC-derived endothelial and smooth muscle cells within decellularized aortas, the engineered vascular grafts display endothelial and smooth muscle cell properties respectively. Hematoxylin and eosin (HE) staining of the double-seeded grafts revealed an architecture similar to that of native vessels (Figure 4G) with multiple layers of smooth muscle cells and a monolayer of endothelial cells as confirmed by positive staining for smooth muscle-22α (SM22), smooth muscle-α actin (SMA), CD31 and CD144 markers respectively (Figure 4H-M)11.
To confirm the patency of the tissue engineered vessels in vivo, the double seeded PiPSC-derived vessels were grafted into mice - both normal mouse and decellularized arteries were used as controls. Subsequent analysis showed that while mice grafted with decellularized vessels presented with markedly higher mortality rates as early as day 1, PiPSC vessel grafts conferred a survival rate of 60% 3 weeks after transplantation (Figure 5A)11. Additionally, 3 week old PiPSC-derived grafts were fully characterized for the presence of human PiPSC-derived endothelial and smooth muscle cells and host macrophage infiltration (Figure 5B and Table 1)11. Taken together, results indicate that PiPSC have the capacity to differentiate into both vascular lineages and are potent for generating functional tissue-engineered vessels that can substitute native vessels in vivo.
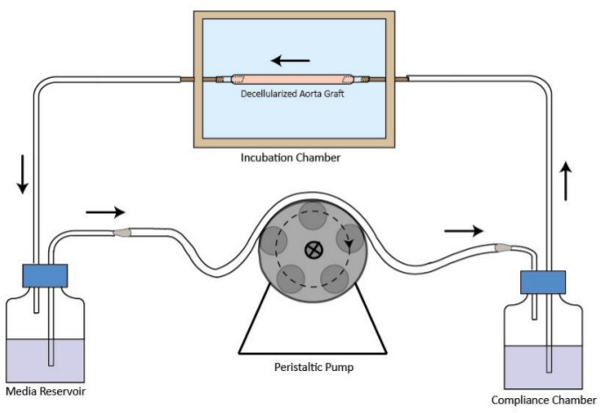 Figure 1. Schematic representation of the decellularized graft bioreactor flow circuit. The decellularized vessel graft is assembled in the incubation chamber. A peristaltic pump is at the upstream of the incubation chamber to provide stable medium perfusion flow. The media reservoir is at the downstream of the incubation chamber. The compliance chamber is to improve the flow regime. The flow direction is indicated by arrows. Please click here to view a larger version of this figure.
Figure 1. Schematic representation of the decellularized graft bioreactor flow circuit. The decellularized vessel graft is assembled in the incubation chamber. A peristaltic pump is at the upstream of the incubation chamber to provide stable medium perfusion flow. The media reservoir is at the downstream of the incubation chamber. The compliance chamber is to improve the flow regime. The flow direction is indicated by arrows. Please click here to view a larger version of this figure.
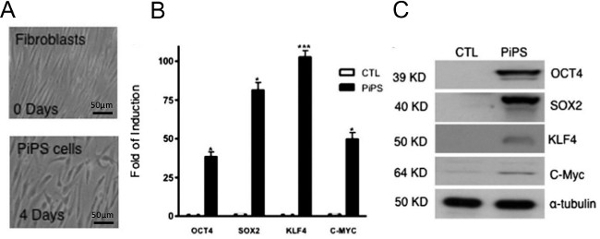 Figure 2. Generation of PiPSC from human fibroblasts. Human fibroblasts were nucleofected with either four reprogramming genes (OCT4, SOX2, KLF4 and C-MYC) or an empty vector (control). (A) Phase contrast pictures show the morphology of PiPS after 4 days. PiPSC expressed all four transcription factors, both at mRNA (B) and protein (C) levels. Scale bar for images shown are 50 µm and data are means ± SEM (n = 3); *P < 0.05, ***P < 0.001. This figure has been modified from Margariti, A. et al.10
Please click here to view a larger version of this figure.
Figure 2. Generation of PiPSC from human fibroblasts. Human fibroblasts were nucleofected with either four reprogramming genes (OCT4, SOX2, KLF4 and C-MYC) or an empty vector (control). (A) Phase contrast pictures show the morphology of PiPS after 4 days. PiPSC expressed all four transcription factors, both at mRNA (B) and protein (C) levels. Scale bar for images shown are 50 µm and data are means ± SEM (n = 3); *P < 0.05, ***P < 0.001. This figure has been modified from Margariti, A. et al.10
Please click here to view a larger version of this figure.
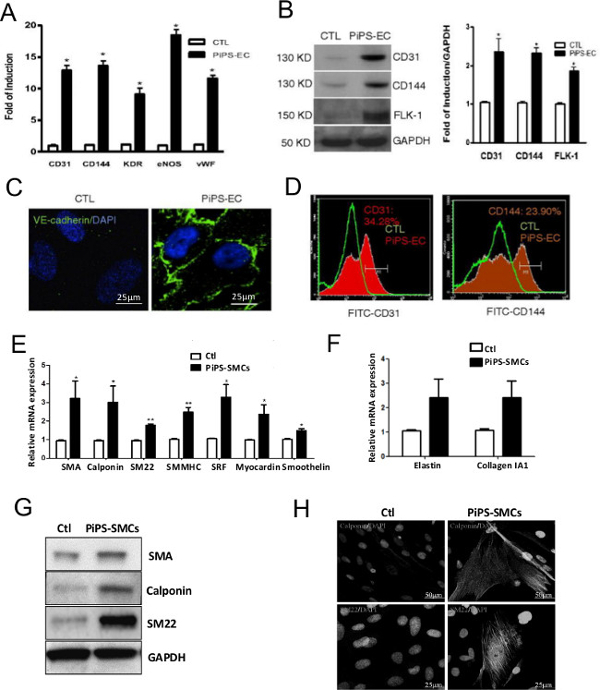 Figure 3. PiPSC can differentiate into both endothelial and smooth muscle cells. PiPSC or control cells were differentiated into endothelial cells . (A) In comparison to control cells, PiPSC-derived endothelial cells expressed endothelial-specific markers such as CD31, CD144, kinase insert domain receptor (KDR), endothelial nitric oxide synthase (eNOS) and von willebrand factor (vWF) at the mRNA level. (B) This was confirmed at the protein level using western blot analysis. (C) Immunofluorescence staining indicated positive staining of CD144 (VE-cadherin) in PiPSC-endothelial, but not control cells. (D) Flow cytometric analysis confirmed PiPSC-endothelial cell expression of CD31 and CD144. Collagen IV-seeded PiPSC (or control cells) were also differentiated into smooth muscle cells. (E,F) Contrary to control cells, PiPSC-derived smooth muscle cells expressed smooth muscle-specific markers at the gene level, including SMA, calponin, SM22, smooth muscle myosin heavy chain II (SMMHC), serum response factor (SRF), myocardin, smoothelin, elastin and collagen 1A1. (G) The expression levels of SMA, calponin and SM22 in PiPSC-derived cells were confirmed using western blot analysis. (H) Immunofluorescence staining using confocal microscopy showed a typical smooth muscle marker staining for calponin and SM22. Data represent means ± SEM (n = 3); *P < 0.05, **P < 0.01, ***P < 0.001. Scale bar for images shown are 25 µm or 50 µm . These figures have been modified from Margariti, A. et al.10 and Karamariti, E. et al.11
Please click here to view a larger version of this figure.
Figure 3. PiPSC can differentiate into both endothelial and smooth muscle cells. PiPSC or control cells were differentiated into endothelial cells . (A) In comparison to control cells, PiPSC-derived endothelial cells expressed endothelial-specific markers such as CD31, CD144, kinase insert domain receptor (KDR), endothelial nitric oxide synthase (eNOS) and von willebrand factor (vWF) at the mRNA level. (B) This was confirmed at the protein level using western blot analysis. (C) Immunofluorescence staining indicated positive staining of CD144 (VE-cadherin) in PiPSC-endothelial, but not control cells. (D) Flow cytometric analysis confirmed PiPSC-endothelial cell expression of CD31 and CD144. Collagen IV-seeded PiPSC (or control cells) were also differentiated into smooth muscle cells. (E,F) Contrary to control cells, PiPSC-derived smooth muscle cells expressed smooth muscle-specific markers at the gene level, including SMA, calponin, SM22, smooth muscle myosin heavy chain II (SMMHC), serum response factor (SRF), myocardin, smoothelin, elastin and collagen 1A1. (G) The expression levels of SMA, calponin and SM22 in PiPSC-derived cells were confirmed using western blot analysis. (H) Immunofluorescence staining using confocal microscopy showed a typical smooth muscle marker staining for calponin and SM22. Data represent means ± SEM (n = 3); *P < 0.05, **P < 0.01, ***P < 0.001. Scale bar for images shown are 25 µm or 50 µm . These figures have been modified from Margariti, A. et al.10 and Karamariti, E. et al.11
Please click here to view a larger version of this figure.
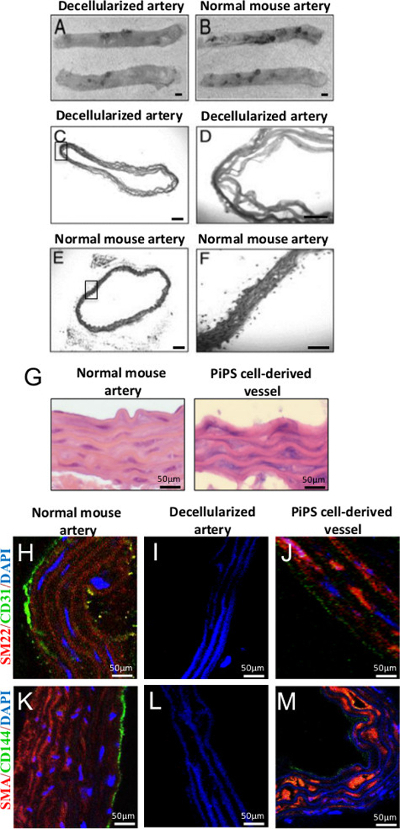 Figure 4. Generation of double-seeded PiPSC-derived tissue engineered vascular grafts. (A,B) Decellularization of mouse thoracic aorta preserved its structure and still resembled that of a normal vessel, original magnification 2X. (C-F) HE staining of decellularized aorta confirmed successful decellularization and complete removal of cells when compared to controls, original magnification: 50X or 200X. (G) HE staining of PiPSC-derived endothelial and smooth muscle cells double-seeded vessels revealed an architecture that was similar to a native vessel. (J,M) Double-seeded PiPSC tissue engineered vessels stained positive for endothelial (CD31 and CD144) and smooth muscle cells (SM22 and SMA) markers unlike decellularized vessel grafts. (H,K) The concomitant expression of vascular markers as well as the characteristic morphology and localization of PiPSC-derived endothelial and smooth muscle cells within medial and intimal areas was comparable to native vessels. Scale bar for images shown are 50 µm. These figures have been modified from Tsai, T. et al. 22 and Karamariti, E. et al.11
Please click here to view a larger version of this figure.
Figure 4. Generation of double-seeded PiPSC-derived tissue engineered vascular grafts. (A,B) Decellularization of mouse thoracic aorta preserved its structure and still resembled that of a normal vessel, original magnification 2X. (C-F) HE staining of decellularized aorta confirmed successful decellularization and complete removal of cells when compared to controls, original magnification: 50X or 200X. (G) HE staining of PiPSC-derived endothelial and smooth muscle cells double-seeded vessels revealed an architecture that was similar to a native vessel. (J,M) Double-seeded PiPSC tissue engineered vessels stained positive for endothelial (CD31 and CD144) and smooth muscle cells (SM22 and SMA) markers unlike decellularized vessel grafts. (H,K) The concomitant expression of vascular markers as well as the characteristic morphology and localization of PiPSC-derived endothelial and smooth muscle cells within medial and intimal areas was comparable to native vessels. Scale bar for images shown are 50 µm. These figures have been modified from Tsai, T. et al. 22 and Karamariti, E. et al.11
Please click here to view a larger version of this figure.
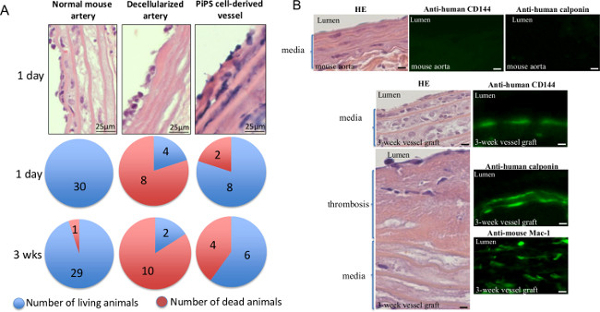 Figure 5. Double-seeded PiPSC-derived tissue engineered vascular grafts are patent for substituting native vessels in vivo. PiPSC-derived vessels were grafted into the carotid artery of severe combined immunodeficiency (SCID) mice, normal mouse and decellularized arteries were used as controls. (A) Analysis of mice grafted with PiPSC-derived vessels showed 60% survival rate 3 weeks post surgery, whereas mice grafted with decellularized vessels presented with markedly higher mortality rates and lower survival (20%). Data represent means (n = 10). (B) The tissue-engineered vessels were also harvested 3 weeks after grafting and subjected to HE (left panels) or immunofluorescence staining (right panels) for the presence of human CD144 and calponin or mouse CD11b/CD18 (Mac-1); quantification of staining is summarized in Table 1. Original magnification for images shown are 400X unless stated. This figure has been modified from Karamariti, E. et al.11
Please click here to view a larger version of this figure.
Figure 5. Double-seeded PiPSC-derived tissue engineered vascular grafts are patent for substituting native vessels in vivo. PiPSC-derived vessels were grafted into the carotid artery of severe combined immunodeficiency (SCID) mice, normal mouse and decellularized arteries were used as controls. (A) Analysis of mice grafted with PiPSC-derived vessels showed 60% survival rate 3 weeks post surgery, whereas mice grafted with decellularized vessels presented with markedly higher mortality rates and lower survival (20%). Data represent means (n = 10). (B) The tissue-engineered vessels were also harvested 3 weeks after grafting and subjected to HE (left panels) or immunofluorescence staining (right panels) for the presence of human CD144 and calponin or mouse CD11b/CD18 (Mac-1); quantification of staining is summarized in Table 1. Original magnification for images shown are 400X unless stated. This figure has been modified from Karamariti, E. et al.11
Please click here to view a larger version of this figure.
| Positive cells Field (40X) | Engineered-vessel before grafting | Engineered-vessel graft (3 weeks) |
| calponin | 72 ± 9 | 22 ± 11* |
| CD144 | 20 ± 8 | 5 ± 6* |
| Mac-1 | 0 | 71 ± 11* |
Table 1. Characterization of tissue-engineered vessels 3 weeks after grafting. The number of PiPSC-derived endothelial and smooth muscle cells and host macrophages was quantified following immunofluorescence staining with human calponin, human CD144 and mouse Mac-1 respectively. Data represents mean ± SEM (n = 6); *P < 0.05, significant difference from tissue-engineered vessels before grafting. This table has been modified from Karamariti, E. et al.11
Discussion
The current protocol indicates a sound, fast, simple, efficient and reproducible strategy in which functional tissue engineered vessels can be generated using PiPSC from human fibroblasts. This technique represents a valuable tool for regenerative medicine, tissue engineering and potentially patient-specific cell therapy in the near future. Critical steps to ensure the efficacy of the protocol include the preparation of PiPSC, preparation of sterile and fully decellularized aortic grafts, successful seeding and differentiation of PiPSC in the scaffolds and maintaining sterility of aortic grafts in the vascular bioreactor.
To initiate the successful generation of tissue-engineered grafts, it is of utmost importance to ensure that the preparation of PiPSC is carried out effectively. The protocol has successfully 'reprogrammed' a human fibroblast cell line into PiPSC via nucleofection with a pCAG2LMKOSimO OSKM plasmid. The survival of fibroblasts after nucleofection relies on several key points such as the use of high quality OSKM plasmids, plasmids of concentrations ranging between 500 - 1,000 ng/µl, avoid delays in seeding of fibroblasts immediately after nucleofection as cells are particularly sensitive following the introduction of relatively large plasmids and finally the addition of FGF-2 which is crucial and should be added into freshly prepared media just before use. Additionally, we found that it was crucial to use cells of up to passage 9 to avoid replicative senescence, to ensure efficient 'reprogramming' into PiPSC and subsequent differentiation into endothelial and smooth muscle cells. The purity of PiPSC can be improved by selection of the nucleofected cells with neomycin. The pCAG2LMKOSimO plasmid has a neomycin resistant gene and thus the addition of neomycin in a range of 25 µg/ml one day after the nucleofection for 3 days will result in the selection of a pure population of PiPSC. To engineer an efficient PiPSC vessel for grafting into mice, we considered the integrity and sterility of the decellularized aortas to be of highest priority. To maintain integrity of the aortas before and after decellularization, it was necessary to constantly apply manual dexterity whilst handling the vessels, as they were relatively fragile and considerably diminutive in size. The efficient removal of perivascular tissue and sealing of branching arteries using a bipolar electro-coagulator was critical to ensure subsequent competent cell seeding and to avoid leakage of media. At any point, we ensured that all materials and apparatus used to generate the bioreactor (i.e., forceps, tubes, bottles, chambers, scissors, adaptors and connectors) were autoclavable, thus reducing risks of bacterial contamination and failure of vascular grafts prior to surgery.
Whilst the current protocol holds promising clinical applications in cardiovascular diseases, there are a few limitations which should be improved in the near future to further enhance the methodology. Thus far, the OSKM transcription factors were introduced into human fibroblasts via nucleofection. While this technique is relatively simple and straightforward, it also resulted in variable transfection efficiencies at different experimental times. Notably, this inconsistency may be overcome by introducing an additional step of the aforementioned neomycin selection. Similarly, one could consider the introduction of the four factors into human fibroblasts using lentivirus integration, which may potentially increase the efficiency of 'reprogramming' and enhance the survival of cells following infection. In terms of the bioreactor, we found that complete decellularization of aortas can be achieved using 0.075% SDS. Although this technique was considered to be optimal for cell removal as compared to other detergents (e.g., Triton X-100), it may however cause potential alterations within the ultra-structures of the extracellular matrix proteins23. This phenomenon therefore warrants more efficient decellularization strategies to minimize disruption of the associated extracellular matrix proteins. Additionally, we also considered that the diameter and wall thickness of decellularized aortas vary between mice, depending on their age, strain and background, and thus cause potential differences in the speed of flow and shear stress within bioreactors and the distribution of PiPSC following PiPSC seeding. All this remains to be clarified.
This protocol herein described the generation of functional tissue engineered grafts using PiPSC that hold a promising potential for future clinical applications in stem cell therapy for cardiovascular disease. This process which utilizes the direct reprogramming from one somatic lineage (fibroblasts) to another (either endothelial or smooth muscle cells) by skipping pluripotency may be a way to obtain safe and suitable cells of interest. Indeed, several protocols have been published to describe the generation of stem cell lines from human embryos, iPS cells and adult stem cells24-26, all of which however still raise concerning issues with regards to their use in clinic. It is now known that PiPSC do not develop teratomas in SCID mice, thus eliminating the concern of tumor formation. Furthermore, the cells take a significantly shorter time to generate, culture and differentiate10,11, and have been shown to generate successful and functional tissue engineered vessels grafts that are comparable to native aortas. Therefore, PiPSC present as a promising cell source for treatment of patients using personalized cell therapy because fibroblasts (e.g., from skin) can be derived from a specific individual. The decellularised vessel system in this protocol provides a more biomimetic model that provides seeded cells with an extracellular matrix protein that is more representative to that of a native aorta11. These key points are critical for ensuring the survival, differentiation and functionality of the seeded cells and tissue engineered vessels thereafter. Recent study by Sumitran-Holgersson and colleagues demonstrated a successful repopulation of a previously decellularized illiac vein graft from a deceased person prior to engraftment27, thus postulating a translational value of the current protocol into humans in the near future. Furthermore, the decellularized vessel grafts may represent a good model in which the role and behavior of other vascular cell types that also contribute to tissue-engineered grafts can be assessed. This model system in mice could provide a powerful tool for future drug screening and also in elucidating the cellular and molecular mechanisms involved in vascular stem cell biology. Taken together, the current protocol holds promising value for its application in vascular tissue engineering and a breakthrough in personalized medicine.
Disclosures
The authors have no conflicting financial interests.
Acknowledgments
This work was supported by The British Heart Foundation and The Oak Foundation.
References
- Kurobe H, Maxfield MW, Breuer CK, Shinoka T. Concise Review: Tissue-Engineered Vascular Grafts for Cardiac Surgery: Past, Present, and Future. Stem Cells Transl Med. 2012;1(7):566–571. doi: 10.5966/sctm.2012-0044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jonas RA, Freed MD, Mayer JE., Jr Long-term follow-up of patients with synthetic right heart conduits. Circulation. 1985;72:II77–II83. [PubMed] [Google Scholar]
- Heureux N, et al. Technology insight: the evolution of tissue-engineered vascular grafts-from research to clinical practice. Nat Clin Pract Cardiovasc Med. 2007;4:389–395. doi: 10.1038/ncpcardio0930. [DOI] [PubMed] [Google Scholar]
- Zhang WJ, Liu W, Cui L, Cao Y. Tissue engineering of blood vessel. J Cell Mol Med. 2007;11:945–957. doi: 10.1111/j.1582-4934.2007.00099.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cearbhaill ED, et al. Response of mesenchymal stem cells to the biomechanical environment of the endothelium on a flexible tubular silicone substrate. Biomaterials. 2008;29:1610–1619. doi: 10.1016/j.biomaterials.2007.11.042. [DOI] [PubMed] [Google Scholar]
- Gong Z, Niklason LE. Small-diameter human vessel wall engineered from bone marrow-derived mesenchymal stem cells (hMSCs) FASEB J. 2008;22:1635–1648. doi: 10.1096/fj.07-087924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong MM, et al. Over-expression of HSP47 augments mouse embryonic stem cell smooth muscle differentiation and chemotaxis. PLoS One. 2014;9(1):e86118. doi: 10.1371/journal.pone.0086118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park SW, et al. Efficient differentiation of human pluripotent stem cells into functional CD34+ progenitor cells by combined modulation of the MEK/ERK and BMP4 signaling pathways. Blood. 2010;116:5762–5772. doi: 10.1182/blood-2010-04-280719. [DOI] [PubMed] [Google Scholar]
- Samuel R, et al. Generation of functionally competent and durable engineered blood vessels from human induced pluripotent stem cells. Proc Natl Acad Sci USA. 2013;110:12774–12779. doi: 10.1073/pnas.1310675110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margariti A, et al. Reprogramming of fibroblasts into endothelial cells capacble of angiogenesis and reendothelialization in tissue-engineered vessels. Proc Natl Acad Sci USA. 2012;109:13793–13798. doi: 10.1073/pnas.1205526109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karamariti E, et al. Smooth muscle cells differentiated from reprogrammed embryonic lung fibroblasts through DKK3 signaling are potent for tissue engineering of vascular grafts. Circ Res. 2013;112:1433–1443. doi: 10.1161/CIRCRESAHA.111.300415. [DOI] [PubMed] [Google Scholar]
- Udelsman B, et al. Development of an operator-independent method for seeding tissue-engineered vascular grafts. Tissue Eng Part C Methods. 2011;17(7):731–736. doi: 10.1089/ten.tec.2010.0581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cearbhaill ED, Murphy M, Barry F, McHugh PE, Barron V. Behavior of human mesenchymal stem cells in fibrin-based vascular tissue engineering constructs. Ann Biomed Eng. 2010;38(3):649–657. doi: 10.1007/s10439-010-9912-x. [DOI] [PubMed] [Google Scholar]
- Wong MM, et al. Macrophages control vascular stem/progenitor cell plasticity through tumor necrosis factor-α-mediated nuclear factor-κB activation. Arterioscler Thromb Vasc Biol. 2014;34(3):635–643. doi: 10.1161/ATVBAHA.113.302568. [DOI] [PubMed] [Google Scholar]
- Wong MM, et al. Sirolimus stimulates vascular stem/progenitor cell migration and differentiation into smooth muscle cells via epidermal growth factor receptor/extracellular signal-regulated kinase/β-catenin signaling pathway. Arterioscler Thromb Vasc Biol. 2013;33(10):2397–2406. doi: 10.1161/ATVBAHA.113.301595. [DOI] [PubMed] [Google Scholar]
- Lee J, Cuddihy MJ, Kotov NA. Three-dimensional cell culture matrices: State of the art. Tissue Eng Part B Rev. 2008;14:61–86. doi: 10.1089/teb.2007.0150. [DOI] [PubMed] [Google Scholar]
- Hung HS, Hsu SH. Current Advances of stem cell-based approaches to tissue-engineering vascular grafts. OA Tissue Engineering. 2013;1(1):2. [Google Scholar]
- Quint C, et al. Decellularized tissue-engineered blood vessel as an arterial conduit. Proc Natl Acad Sci USA. 2011;108(22):9214–9219. doi: 10.1073/pnas.1019506108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X, Xu Y, Thomas V, Bellis SL, Vohra YK. Engineering an antiplatelet adhesion layer on an electrospun scaffold using porcine endothelial progenitor cells. J Biomed Mater Res A. 2011;97(2):145–151. doi: 10.1002/jbm.a.33040. [DOI] [PubMed] [Google Scholar]
- Hibino N, et al. Evaluation of the use of an induced puripotent stem cell sheet for the construction of tissue-engineered vascular grafts. J Thorac Cardiovasc Surg. 2012;143(3):696–703. doi: 10.1016/j.jtcvs.2011.06.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao J, et al. A novel strategy to engineer small-diameter vascular grafts from marrow-derived mesenchymal stem cells. Artif Organs. 2012;36(1):93–101. doi: 10.1111/j.1525-1594.2011.01231.x. [DOI] [PubMed] [Google Scholar]
- Tsai T, et al. Contribution of stem cells to neointimal formation of decellularized vessel grafts in a novel mouse model. Am J Pathol. 2012;181(1):362–373. doi: 10.1016/j.ajpath.2012.03.021. [DOI] [PubMed] [Google Scholar]
- Kasimir MT, et al. Comparison of different decellularization procedures of porcine heart valves. Int J Artif Organs. 2003;26(5):421–427. doi: 10.1177/039139880302600508. [DOI] [PubMed] [Google Scholar]
- Stephenson E, et al. Derivation and propagation of human embryonic stem cell lines from frozen embryos in an animal product-free environment. Nature Protocols. 2012;7:1366–1381. doi: 10.1038/nprot.2012.080. [DOI] [PubMed] [Google Scholar]
- Takahashi K, Okita K, Nakagawa M, Yamanaka S. Induction of pluripotent stem cells from fibroblast cultures. Nature Protocols. 2007;2:3081–3089. doi: 10.1038/nprot.2007.418. [DOI] [PubMed] [Google Scholar]
- McCall FC, et al. Myocardial infarction and intramyocardial injection models in swine. Nature Protocols. 2012;7:1479–1496. doi: 10.1038/nprot.2012.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olausson M, et al. Transplantation of an allogeneic vein bioengineered with autologous stem cells: a proof-of-concept study. Lancet. 2012;380(9838):230–237. doi: 10.1016/S0140-6736(12)60633-3. [DOI] [PubMed] [Google Scholar]


