Abstract
The propensity for chronic wounds in humans increases with ageing, disease conditions such as diabetes and impaired cardiovascular function, and unrelieved pressure due to immobility. Animal models have been developed that attempt to mimic these conditions for the purpose of furthering our understanding of the complexity of chronic wounds. The model described herein is a rat ischemic skin flap model that permits a prolonged reduction of blood flow resulting in wounds that become ischemic and resemble a chronic wound phenotype (reduced vascularization, increased inflammation and delayed wound closure). It consists of a bipedicled dorsal flap with 2 ischemic wounds placed centrally and 2 non-ischemic wounds lateral to the flap as controls. A novel addition to this ischemic skin flap model is the placement of a silicone sheet beneath the flap that functions as a barrier and a splint to prevent revascularization and reduce contraction as the wounds heal. Despite the debate of using rats for wound healing studies due to their quite distinct anatomic and physiologic differences compared to humans (i.e., the presence of a panniculus carnosus muscle, short life-span, increased number of hair follicles, and their ability to heal infected wounds) the modifications employed in this model make it a valuable alternative to previously developed ischemic skin flap models.
Keywords: Medicine, Issue 98, Wound Healing, ischemia, rat, animal model, chronic wounds, laser Doppler, bipedicled flap
Introduction
Effective drug development and other wound healing therapeutics require appropriate in vivo models, despite known problems in translating findings in animal models to human therapies1. What follows is a description of a detailed protocol for the use of a rat model of ischemic skin wound healing to investigate mechanisms that further the understanding of pathological wound healing. The rat species, often employed due to its wide availability, size and docile nature is used for wound healing studies as it is large enough to provide a suitable skin area for incisional and excisional wounding, imaging and tissue collection2. However it should be taken into careful consideration that the skin of a rat and a human are different anatomically, with rats being referred to as loose-skinned animals. This distinct characteristic allows for wound contraction, rather than epithelialization to contribute significantly to the closing of rat skin wounds2. Additionally, the presence of a subcutaneous panniculus carnosus muscle in rats, contributes to healing by both contraction and collagen formation3,4. These very important anatomical distinctions were considered in the development of the rat ischemic skin wound model and specific modifications were implemented to decrease wound contraction and reduce the influence of the panniculus carnosus muscle5.
In diabetic foot ulcers, venous leg ulcers, and pressure ulcers, healing is delayed and these wounds are considered chronic. The wounds are characterized by excessive inflammation, which prevents the wound from progressing to the next phases of wound repair6. One of the main factors in the development of a chronic wound is localized tissue ischemia (reduced blood flow)5 contributing to the inability to clear inflammation. At the time during which this model was being developed and validated (in 2003-4), there were no standardized animal models that could provide enough tissue to test induction of angiogenesis in the wound bed, a key stage during normal wound healing and the motivation for developing this model5. That said, the model presented here is a modification of the ischemic wound model originally described by Schwartz et al.7 and subsequently used in modified form by Chen et al.8
In the modified ischemic wound model, changes have been made to circumvent the above mentioned anatomical characteristics of the rat that lead to healing by contraction rather than epithelialization: (1) Two full-thickness excisional wounds are created within a bipedicled dorsal skin flap and the panniculus carnosus muscle is removed from the wound bed by dissecting just above the muscle fascia. (2) The flap itself has more narrow dimensions, ensuring that blood supply is random and the wounds located at the midpoint of the flap are ischemic. (3) A silicone sheet is inserted beneath the flap, preventing readherence and reperfusion of the flap from underlying tissue. Wound contraction is limited (not eliminated) by anchoring or suturing the flap to the silicone sheet5.
The model has recently been used in studies ranging from hyperbaric oxygen effects on ischemic wound healing9,10 to ischemic wound healing in young versus aged rats11 and has proven to be a reliable model of prolonged tissue ischemia. The dimensions of the bipedicled flap have also been adapted to different rat strains, including Sprague Dawley (11 cm long by 2 cm wide) and F344 rats (10.5 cm long by 3.0-3.5 cm wide) and other species, including swine12 and mice13,14 . This video utilizes the F344 inbred rat strain in the demonstration of the ischemic skin wound model.
Approval for all animal procedures presented below was obtained from the University of South Florida’s Animal Care Committee (IACUC) and abide by all requirements of the Animal Welfare Act and the Guide for Care and Use of Laboratory Animals.
Protocol
NOTE: Approval for all animal procedures presented below was obtained from the University of South Florida’s Animal Care Committee (IACUC) and abide by all requirements of the Animal Welfare Act and the Guide for Care and Use of Laboratory Animals.
1. Preparation of Silicone Sheets and Surgical Instruments
Precut strips (10.5 cm x 3.0 cm) of non-reinforced 0.01 thickness, medical grade silicone sheeting and sterilize using an autoclave.
Clean and sterilize suitable surgical instruments (scissors, forceps and drapes or towels to create a sterile field during surgery).
2. Experimental Animals
Use adult male or female rats weighing in range from 250-350 g obtained from a commercial breeder. If aged rats are utilized, they should be ≥350 g in order to ensure better survival post-surgery. Prior to the start of any experiments acclimate all animals for at least 7 days under standard conditions of a 12 hr light-dark cycle with food and water ad libitum.
3. Anesthesia, Pre-operative Analgesia and Operative Preparation
Induce general anesthesia by using isoflurane at 3%-4% via an induction chamber and maintain (via use of a nose cone) at 1%-2% with O2 during skin preparation and surgery. Monitor the depth of anesthesia by observation of the rate and depth of respiration, interdigital pinch or palpebral blink reflex. NOTE: At this time, a vet ointment can be placed on the eyes to prevent dryness while the animal is under anesthesia.
In a location remote from the sterile surgical area, place the rat in the prone position and shave the dorsum with clippers from the base of the neck down approximately 11 cm. Stencil with permanent marker, the outline for the 3.0 cm x 10.5 cm flap (see Figure 1A).
Move the rat to a clean, designated surgical area equipped with an approved heating pad and sterile surgical drapes or towels. Inject 5 mg/kg Ketoprofen subcutaneously prior to the first surgical incisions for pain management. Additional fluids (saline) can be given (up to 5 cc) subcutaneously as needed.
Prepare the skin further by swabbing first with 70% isopropyl alcohol and second with 0.2% chlorhexidine, then apply sterile drapes to create a sterile field. 10% povidone-iodine (Betadine) can also be used. NOTE: An antibiotic (ampicillin at 15 mg/kg) can be administered subcutaneously, but if good aseptic techniques are used it is not required.
4. Creating Excisional Wounds and Bipedicled Flap
Using a sterile, disposable 6 mm biopsy punch tool, create two circular “ischemic” wounds in the center of the designated flap area (Figure 1B). The depth of the wound should be down to (not through) the underlying fascia of the panniculus carnosus muscle (Figure 1B inset).
Using forceps lift the skin in the middle of the wound outline created by the punch biopsy and then use iris scissors (with curved tips) to excise the circular piece of tissue (including the panniculus carnosus muscle). The result will be a full-thickness wound with the fascia as the base of the wound. NOTE: The excised tissue (wound plugs) can be snap frozen in liquid nitrogen or fixed in 10% buffered-formalin O/N for later processing as control, normal skin.
Create a bipedicled flap by making incisions with a sterile scalpel on each side of the ischemic wounds along the pre-drawn lines (Figure 1C) that are 10.5 cm in length and 3.0 cm apart. The depth of the incisions should be down to the paraspinous muscles. Using iris scissors, separate the panniculus carnosus fascia from the paraspinous muscles, being careful to keep the fascia intact as the “base” of the 6 mm punches (Figure 1D).
Take 1 sterile pre-cut silicone sheet and place it in between the panniculus carnosus fascia and the paraspinous muscles (Figure 1E) ensuring that the sheet does not buckle or fold. Using black, non-absorbable sutures (size 4.0) close both incisions by anchoring the silicone sheet to the skin with at least 8 interrupted stitches on each side, along the length of the flap (Figure 1F and 1G).
Using a sterile, disposable biopsy punch tool, create two internal control “non-ischemic” wounds (down to the anterior fascia of the panniculus carnosus muscle) 1 cm lateral to the ischemic wounds on either side of the flap (Figure 1G).
Place a ruler below the wounds and take digital photos for wound measurement purposes (see Figure 3A). At this time, blood flow (perfusion) can be monitored by use of laser Doppler or other manipulations (topical drug placement) performed.
Apply an approved liquid adhesive both cranial and caudal to the wounds and a transparent film dressing to keep the wound environment moist and clean (sterile). An additional dressing may be placed at the caudal end of the flap to prevent the animal from removing the most caudal sutures.
5. Post-operative Procedures
Place animals in cages (singly housed) equipped with shallow feeders so as to prevent the surgical site from rubbing against the feeder. Animals should not be left unattended or returned to the company of other animals until they regain sufficient consciousness to maintain sternal recumbency and exhibit purposeful movement. Heating mats should be placed under half of the cage for up to 2 days during recovery.
To manage pain post-operatively, administer Ketoprofen (5 mg/kg) subcutaneously to animals the following morning and 1x per day for up to 48 hr post-surgery. Animals should also be monitored daily for prolonged signs of pain, weight loss or surgical site infections.
6. Subsequent Wound Measurements and Dressing Changes
Measure ischemic and non-ischemic wounds frequently under general anesthesia using isoflurane at 3%-4% via an induction chamber and maintained (via a nose cone) at 1%-2% with O2 as in step 3.1.
Remove the dressing gently as to not pull the adhesive from the skin. At this time additional digital photos are taken for wound measurements, topical treatments re-applied, laser Doppler imaging (LDI) or other manipulations performed to suit the investigator’s needs.
Apply adhesive and a clean dressing and allow the animal to recover as in step 5.1.
7. Wound Collection and Euthanasia
Harvest ischemic and non-ischemic wounds (on days the investigator deems appropriate) while the animal is under general anesthesia using isoflurane at 3%-4% via an induction chamber and maintained (via a nose cone) at 1%-2% with O2 as in step 3.1.
Using a scalpel, make a square shaped excision around the wound to include some healthy tissue around the wound. Place the excision into a 1.5 ml snap cap tube and snap freeze in liquid nitrogen (store at -80 °C) for future molecular analysis or incubate in 10% buffered formalin O/N at RT for histological processing. NOTE: The wound excisions can also be cut in half to provide more samples for analysis.
After wound tissue removal, euthanize the animal using the approved method of CO2 inhalation.
Representative Results
The rat ischemic wound healing model protocol should take approximately 20 min per animal if performed efficiently. Prior to application of a dressing the model should appear as represented in Figure 1G. It will be important to verify that the bipedicled flap and wounds therein are ischemic. Subcutaneous oxygen tension (PscO2) at the level of the wounds has been measured during validation of this model5 by placing a polarographic electrode in the subcutaneous tissue between the two ischemic wounds. PscO2 values were in the critically ischemic range (20-40 mmHg). Since the development of this model the use of LDI has increasingly been used to measure blood perfusion and this technique will give adequate information about the ischemic state of the bipedicled flap.
Briefly, the LDI technique is based on the emission of a beam of laser light carried by a fiber-optic probe. The measuring depth depends on the tissue properties and wavelength of the laser light. In normal skin, an instrument with a probe with standard fiber separation (0.25 mm) and a 780 nm wavelength laser, measuring depth will be on the order of 0.5-1 mm. A representative Doppler image (left) for a dorsal bipedicled flap showing both a perfused area (left of the suture line) and the non-perfused area (right of the suture line) is shown in Figure 2.
In addition to measuring subcutaneous oxygen tension, one can also use probes or common biochemical markers to establish that the wounds in the flap are ischemic. PECAM-1 or CD31 normally found on vascular endothelial cells is a marker for new vessel formation in the wounds. Various markers for reactive oxygen species, found to be elevated in ischemic wounds, are available commercially often as fluorescent-tagged antibodies or superoxide indicators such as dihydroethidium (DHE).
Wound area measurements to track wound closure may be represented in a variety of ways. Commonly, wound area is quantified from digital images of the wounds over the time course of healing11 using a formula such as (6 mm punch biopsy area = (π) r2 = 3.14 x 9 = 28.26 mm2 at day 0) with data presented as percentage of initial wound area or wound surface area on a particular day can be quantified as in Gould et al.5 For the purposes of this demonstration, wound closure progression is represented as percent of initial wound area over a time course of 28 days. Using the free software ImageJ, a digital picture is opened and the scale is set using 10 mm on the ruler in the image (Figure 3A). A line drawn 10 mm in length equates to a pixel count (inset in Figure 3A) which can be converted into a unit of choice, in this case (mm). Next, the circumference of the wound is traced on the image (Figure 3B) and once the measure command is given, the area is presented in mm (inset in Figure 3B). Data can then be presented as percentage of initial wound area on the y-axis and days on the x-axis (Figure 3C).
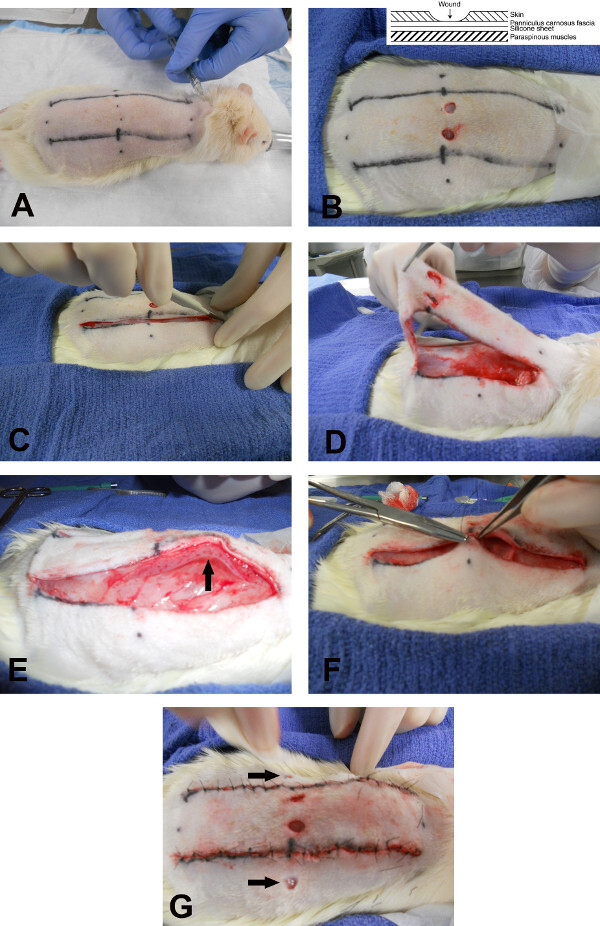 Figure 1. Photographs depicting steps during surgery to create ischemic wounds, the bipedicled flap, and non-ischemic wounds. (A) Pre-surgical hair removal and skin preparation of an anesthetized rat receiving a pre-surgical dose of analgesic (Ketoprofen) subcutaneously for pain management. (B and inset) Ischemic wounds are created inside the 2 incision markers by utilizing a sterile punch biopsy tool. (C) Incisions are made along the marked lines down to the paraspinous muscle and (D) the bipedicled flap is raised to show the separation of the flap (with the panniculus carnosus fascia intact) from the muscle layer below. (E) A sheet of sterile silicone (black arrow) is placed between the fascia of the panniculus carnosus and the paraspinous muscle. (F) Black, non-absorbable sutures (size 4.0) close both incisions by anchoring the silicone sheet to the skin with multiple interrupted stitches along the length of the flap (G). Two non-ischemic wounds (black arrows) are created using a sterile punch biopsy tool lateral to the bipedicled flap on both sides. Please click here to view a larger version of this figure.
Figure 1. Photographs depicting steps during surgery to create ischemic wounds, the bipedicled flap, and non-ischemic wounds. (A) Pre-surgical hair removal and skin preparation of an anesthetized rat receiving a pre-surgical dose of analgesic (Ketoprofen) subcutaneously for pain management. (B and inset) Ischemic wounds are created inside the 2 incision markers by utilizing a sterile punch biopsy tool. (C) Incisions are made along the marked lines down to the paraspinous muscle and (D) the bipedicled flap is raised to show the separation of the flap (with the panniculus carnosus fascia intact) from the muscle layer below. (E) A sheet of sterile silicone (black arrow) is placed between the fascia of the panniculus carnosus and the paraspinous muscle. (F) Black, non-absorbable sutures (size 4.0) close both incisions by anchoring the silicone sheet to the skin with multiple interrupted stitches along the length of the flap (G). Two non-ischemic wounds (black arrows) are created using a sterile punch biopsy tool lateral to the bipedicled flap on both sides. Please click here to view a larger version of this figure.
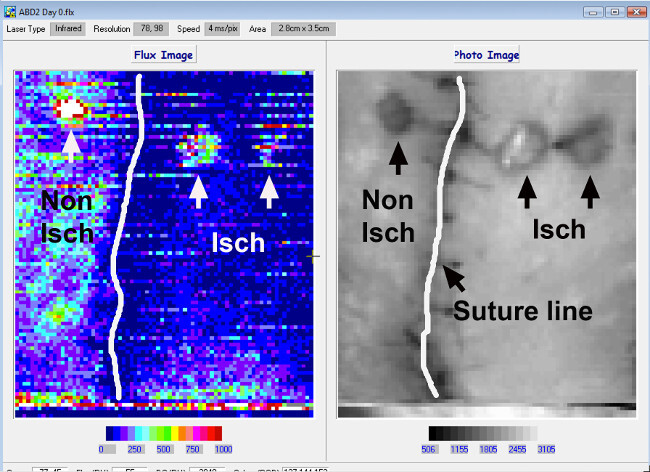 Figure 2. Representative laser Doppler image of blood perfusion post-surgery. The right panel shows a black and white image of 2 ischemic wounds (black arrows) in the middle of the bipedicled flap and 1 non-ischemic wound (single black arrow) lateral to the flap. The suture line has been highlighted in white. The left panel shows the Doppler image of the same area depicted in the right panel. Areas with brighter colors are more perfused than areas with dark blue. This difference in perfusion between the non-ischemic area (left) and the ischemic area (right) is clear and can be followed along the entire length of the suture line. Note that the wounds on both sides appear bright, as blood cells are still present to some degree. Please click here to view a larger version of this figure.
Figure 2. Representative laser Doppler image of blood perfusion post-surgery. The right panel shows a black and white image of 2 ischemic wounds (black arrows) in the middle of the bipedicled flap and 1 non-ischemic wound (single black arrow) lateral to the flap. The suture line has been highlighted in white. The left panel shows the Doppler image of the same area depicted in the right panel. Areas with brighter colors are more perfused than areas with dark blue. This difference in perfusion between the non-ischemic area (left) and the ischemic area (right) is clear and can be followed along the entire length of the suture line. Note that the wounds on both sides appear bright, as blood cells are still present to some degree. Please click here to view a larger version of this figure.
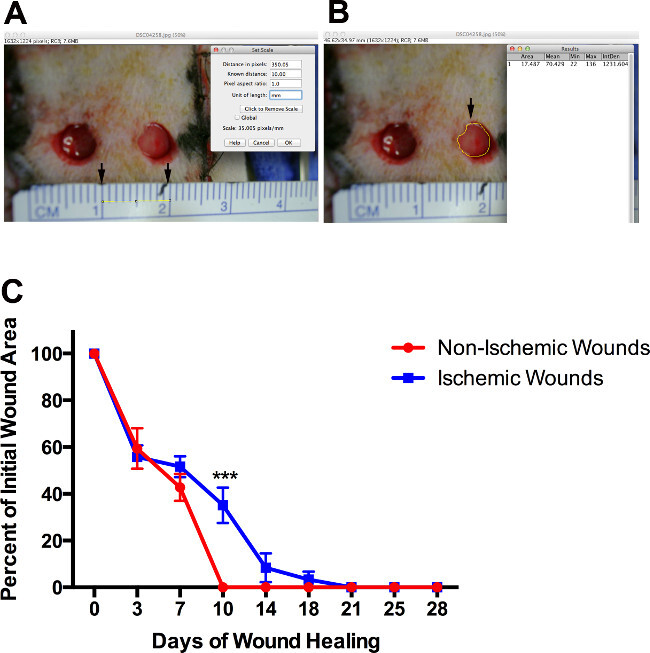 Figure 3. Wound measurement and data representation. (A) Digital photographs depicting wound area measurement using software (ImageJ), conversion of pixels to (mm) (black arrows) and the method to capture an accurate circumference (single black arrow) of the wound (B). Statistical data (mean ± SEM of wound areas on a given day) can then be presented as percentage of initial wound area (day 0) on the y-axis and days on the x-axis (C). The line graph presents data analyzed using a 2-way ANOVA with Sidak’s multiple comparisons test, *** represents significantly higher (P = 0.0004) than non-ischemic at the same time point (day 10), N = 8 wounds per group. Please click here to view a larger version of this figure.
Figure 3. Wound measurement and data representation. (A) Digital photographs depicting wound area measurement using software (ImageJ), conversion of pixels to (mm) (black arrows) and the method to capture an accurate circumference (single black arrow) of the wound (B). Statistical data (mean ± SEM of wound areas on a given day) can then be presented as percentage of initial wound area (day 0) on the y-axis and days on the x-axis (C). The line graph presents data analyzed using a 2-way ANOVA with Sidak’s multiple comparisons test, *** represents significantly higher (P = 0.0004) than non-ischemic at the same time point (day 10), N = 8 wounds per group. Please click here to view a larger version of this figure.
Discussion
Wound healing in rats has often been the subject of debate due to their ability to heal infected wounds and high rate of interanimal variability5. One of the original goals of the model during its development was to decrease this variation. Modifications to the width of the flap, reducing the number of wounds with specific placement (centered on the flap with consistent cranio-caudal location) and introduction of a silicone sheet has accomplished this goal. Wound healing by contraction has also been reduced and healing by epithelialization, as in humans, is the measured outcome. Adaptation of the model to a different strain of rat, i.e., the F344, has also proven successful and reproduces the degree of ischemia observed using Sprague Dawley rats. Overall the surgical techniques (biopsy, suturing and wound excision) required for this model are easily acquired by most students and technicians with limited surgical experience.
To achieve consistency with this model while performing multiple surgeries, it was found that it is important to create the ischemic wounds prior to elevation of the flap for silicone sheet placement5. Additionally, not punching through the panniculus carnosus fascia is critical to provide a viable wound bed to remain over the silicone. The silicone acts not only to prevent vascular regrowth but also as a “splint” that encourages wound re-epithelialization. The application of the adhesive and dressings to prevent infection and maintain a moist environment for wound healing is also important. Product choice can be what is preferred or used in the researcher’s animal facility. However, it is not uncommon for some of the animals to be able to remove their dressings, no matter what type of adhesive/dressing combination is used.
The bipedicled flap should remain viable throughout a time course of healing which is approximately 28 days, depending on rat strain and other co-morbidities present. Rarely, abscesses can form in the flap (particularly near sutures) and seromas may form under the flap. Fluid can be drained and antibiotics administered if necessary. However, if the flap loses viability and becomes necrotic it is recommended that that animal no longer be used. Wound excision for biochemical analysis does introduce variability due to (1) some normal tissue must be retained for support (2) the choice of tissue homogenization and preparation for isolation of RNA, DNA or protein and (3) inherent interanimal variability5,10,11. One could consider this last point a limitation to the model and it was found that reducing the size of the flap (<2.0 cm) or flap trauma can cause necrosis, indicating that minor variations in factors such as temperature or stress levels, may also lead to biochemically detectable variation between wound samples from one rat to another5.
In summary, this model, with a longitudinal, bipedicled flap ranging from 2.0-3.0 cm in width and a strategically placed silicone sheet, is a reliable model of prolonged tissue ischemia. Once the user is adept at using the techniques to create a consistent ischemic wound, they should be able to adapt it to additional ages and species of rodents (mice included). The excisional wounds can be treated topically, or systemic treatments utilized to further explore the mechanism(s) involved in chronic wound formation, exacerbated inflammatory responses, aberrant angiogenesis and delayed wound closure.
Disclosures
The authors have nothing to disclose.
Acknowledgments
The authors would like to acknowledge funding support from the University of South Florida, Department of Surgery (Mack Wu, MD, PhD).
References
- Ansell DM, Holden KA, Hardman MJ. Animal models of wound repair: Are they cutting it. Experimental dermatology. 2012;21(8):581–585. doi: 10.1111/j.1600-0625.2012.01540.x. [DOI] [PubMed] [Google Scholar]
- Dorsett-Martin WA. Rat models of skin wound healing: a review. Wound repair and regeneration : official publication of the Wound Healing Society [and] the European Tissue Repair Society. 2003;12(6):591–599. doi: 10.1111/j.1067-1927.2004.12601.x. [DOI] [PubMed] [Google Scholar]
- Davidson JM. Animal models for wound repair. Arch Dermatol Res. 1998;290(S1-11) doi: 10.1007/pl00007448. [DOI] [PubMed] [Google Scholar]
- Finn G, Magnus SA, Tonny K. Models for use in wound healing research: A survey focusing on in vitro and in vivo adult soft tissue) Wound Repair and Regeneration. 2000;8 doi: 10.1046/j.1524-475x.2000.00083.x. [DOI] [PubMed] [Google Scholar]
- Gould LJ, Leong M, Sonstein J, Wilson S. Optimization and validation of an ischemic wound model. Wound repair and regeneration : official publication of the Wound Healing Society [and] the European Tissue Repair Society. 2004;13(6):576–582. doi: 10.1111/j.1524-475X.2005.00080.x. [DOI] [PubMed] [Google Scholar]
- Loots MA, et al. Differences in cellular infiltrate and extracellular matrix of chronic diabetic and venous ulcers versus acute wounds. The Journal of investigative dermatology. 1998;111(5):850–857. doi: 10.1046/j.1523-1747.1998.00381.x. [DOI] [PubMed] [Google Scholar]
- Schwartz DA, Lindblad WJ, Rees RR. Altered collagen metabolism and delayed healing in a novel model of ischemic wounds. Wound Repair Regen. 1995;3(2):204–212. doi: 10.1046/j.1524-475X.1995.30212.x. [DOI] [PubMed] [Google Scholar]
- Chen C, et al. Molecular and mechanistic validation of delayed healing rat wounds as a model for human chronic wounds. Wound Repair and Regeneration. 1999;7 doi: 10.1046/j.1524-475x.1999.00486.x. [DOI] [PubMed] [Google Scholar]
- Zhang Q, Chang Q, Cox RA, Gong X, Gould LJ. Hyperbaric oxygen attenuates apoptosis and decreases inflammation in an ischemic wound model. The Journal of investigative dermatology. 2008;128(8):2102–2112. doi: 10.1038/jid.2008.53. [DOI] [PubMed] [Google Scholar]
- Zhang Q, Gould LJ. Hyperbaric oxygen reduces matrix metalloproteinases in ischemic wounds through a redox-dependent mechanism. The Journal of investigative dermatology. 2013;134(1):237–246. doi: 10.1038/jid.2013.301. [DOI] [PubMed] [Google Scholar]
- Moor AN, et al. Consequences of age on ischemic wound healing in rats: altered antioxidant activity and delayed wound closure. Age (Dordrecht, Netherlands) 2014;36(2):733–748. doi: 10.1007/s11357-014-9617-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy S, et al. Characterization of a preclinical model of chronic ischemic wound) Physiological genomics. 2009;37(3):211–224. doi: 10.1152/physiolgenomics.90362.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biswas S, et al. Hypoxia inducible microRNA 210 attenuates keratinocyte proliferation and impairs closure in a murine model of ischemic wounds. Proceedings of the National Academy of Sciences of the United States of America. 2010;107(15):6976–6981. doi: 10.1073/pnas.1001653107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winocour S, Vorstenbosch J, Trzeciak A, Lessard L, Philip A. CD109, a novel TGF-beta antagonist, decreases fibrotic responses in a hypoxic wound model. Exp Dermatol. 2014;23(7):475–479. doi: 10.1111/exd.12439. [DOI] [PubMed] [Google Scholar]


