Abstract
Purpose
To present normative values of mean sleep duration from adolescence through young adulthood (ages 13–32), prevalence of short (<6 hours) and long (>10 hours) sleep durations, and differences in each by sex and race/ethnicity.
Methods
Mean sleep duration and prevalence of extremely short and long sleep were estimated using data from the US National Longitudinal Study of Adolescent Health, Waves 1–4 (N = 15,701).
Results
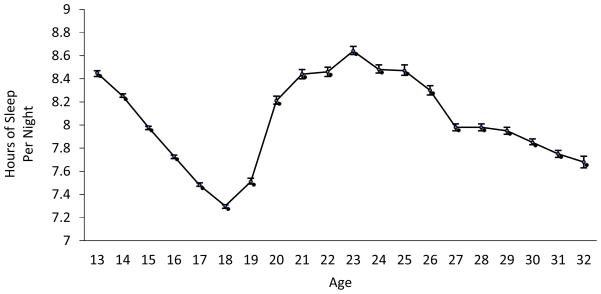
Sleep duration showed age-related trends, with decreases across the adolescent period from 8.5 hours per night at age 13 to 7.3 hours at age 18, an increase through the emerging adulthood period to 8.5 hours at age 22, and a gradual decline across early adulthood to 7.7 hours at age 32. Prevalence of extremely long and short sleep followed similar developmental trends. Adolescent girls reported lower mean sleep duration than boys, but women reported longer average sleep duration than men from age 19 onward. Short sleep duration was most common among African Americans at all ages. Long sleep was most common among African Americans in adolescence and emerging adulthood and among Hispanics in early adulthood.
Conclusions
Sleep duration is developmentally patterned from adolescence through early adulthood. Mean and extreme sleep durations vary systematically by sex and race/ethnicity as well as age. These normative data on sleep duration will inform studies of the role of sleep in the etiology of a wide range of health conditions affecting adolescents and young adults.
Keywords: Sleep, adolescence, young adulthood, norms
Introduction
Sleep is essential for mental and physical health and well-being (1,2). Abnormal sleep duration—too much or too little sleep—is implicated in a wide range of physical and mental health conditions, including diabetes, hypertension, hypercholesterolemia, obesity, depression, substance use, and all-cause mortality (1,3–9). There is reason to expect that sleep duration should vary by developmental period from adolescence through young adulthood. Documented biological mechanisms such as adolescent sleep phase delay and social and contextual factors such as early school start times during adolescence and transition into adulthood roles during emerging and early adulthood provide reasons to expect that sleep duration is developmentally patterned during these periods (10,11). However, no nationally representative data spanning adolescence through early adulthood have been reported. Understanding normative developmental shifts in sleep duration will help to further specify the role of sleep in the etiology of the many health conditions in which it has been implicated.
The life period spanning adolescence through early adulthood is marked by numerous biological and social developments. It encompasses three developmental periods: adolescence, emerging adulthood, and early adulthood, each of which is characterized by a distinct combination of biological, contextual, and social influences. Definitions of the age range covered by each of these developmental periods vary. For purposes of the current study, adolescence refers to participants age 13–18, emerging adulthood refers to ages 19–22, and early adulthood refers to ages 23–32. There is a well-documented decline in average sleep duration across the adolescent period (12–14), a matter of significant concern given that the biological need for sleep does not decrease in adolescence (15). Rather, the decline in sleep duration is driven by constraints imposed by competing biological and social factors. With pubertal onset comes phase delay, a biologically driven shift that results in adolescents staying awake later at night (12,15,16). Coupled with early school start times that require early wake times, this leads to a decline in nightly hours of sleep during adolescence.
It is not clear whether sleep time continues to decline after adolescence, in the emerging adulthood period that begins around age 19, following typical graduation from secondary school. Roles and responsibilities in emerging adulthood are varied; some individuals enter college, while others enter the working world or move into family formation (17). Compared to adolescence, emerging adulthood is a time when individuals exercise greater ability to choose their own context and accommodate their own sleep schedule without the constraint of early wake times generally enforced by high schools. This may result in increased sleep duration during emerging adulthood. In contrast, early adulthood is typically characterized by the onset of adulthood roles, such as full-time work, marriage, and parenthood, each of which places time and energy demands and may result in diminished sleep duration.
The aim of the current paper is to examine whether the well-established decline in sleep time during adolescence continues or reverses in emerging and early adulthood. This is a crucial area of inquiry. If declines in sleep duration previously noted in adolescence continue for a prolonged period into adulthood, this could lead to the development of physical and mental health conditions known to be associated with abnormal sleep duration. We expected that sleep duration would be patterned according to developmental phase—adolescence, emerging adulthood, and early adulthood. Specifically, we hypothesized that sleep duration would decrease in adolescence, increase in emerging adulthood, and decrease somewhat in early adulthood. Normative data are needed to characterize age-related variation in sleep duration and provide a basis for additional research on the precursors and consequences of normal and abnormal sleep duration during this life period.
In addition to mean sleep duration, it is important to consider developmental trends in the prevalence of extreme long and short sleep duration. In adults, accumulating evidence suggests that short and long sleep duration, generally defined as sleeping fewer than 6 or more than 9 hours per night, is associated with negative health outcomes such as obesity, diabetes, and hypertension (4,6,7) and increased risk of mortality (4). Short sleep in particular appears to precede disease onset, while long sleep may also be a consequence of disease. Several studies report that racial and ethnic minorities, particularly African Americans, are disproportionately represented among those reporting extremely long and short sleep duration (18,19). The majority of research on prevalence of short and long sleep duration has focused on middle aged and older populations; establishing prevalence of short and long sleep durations earlier in life is necessary for understanding their lifespan distributions.
Methods
Study sample
This study presents normative values of self-reported sleep duration from adolescence through young adulthood using nationally representative data from the National Longitudinal Study of Adolescent Health (Add Health) (20). In the first wave of Add Health data collection, a subsample of 20,745 adolescents in 7th through 12th grades were selected from a larger school-based sample of 90,118 to participate in in-depth home interviews and to be followed longitudinally in three additional waves. Wave 1 occurred in 1994–1995; longitudinal follow-ups occurred in 1996, 2001–2002, and 2007–2008. Across the four waves, participants’ ages ranged from 11–34 years. The present sample includes data reported at each wave by the 15,701 participants from the Wave 1 home interview subsample who were retained through Wave 4 (49.2% female, 57% White, 16.6% African American, 18.7% Hispanic, and 7.7% other race/ethnicity).
Data were weighted using Add Health Wave 4 grand sample weights, which account for sample attrition and retain the national representativeness of the original Wave 1 sample. 80.3% of Wave 1 sample participated in Wave 4. Using Wave 1 responses, estimated bias in Wave 4 responses due to sample attrition was calculated, and Wave 4 weights were generated to correct for this bias (21). Restricting the age range to 13 through 32 years, the ages at which sample sizes were large enough to provide robust estimates, and deleting impossible values less than 0 or more than 24 hours of sleep per day resulted in a total of 14,799 individuals. Over the course of the four sample waves, these 14,799 individuals provided a total of 52,080 observations on sleep duration, which comprised the final analysis sample. All study procedures were approved by the Institutional Review Board of the University of Wisconsin, Madison.
Measures
Sleep duration
In Waves 1 and 2, participants were asked, “How many hours of sleep do you usually get?” with responses in whole hours. In Waves 3 and 4, participants were asked about amount of sleep via four items: “On days when you go to work, school, or similar activities, what time do you usually wake up?”; “What time do you usually go to sleep the night (or day) before?”; “On days you don’t have to get up at a certain time, what time do you usually get up?”; “On those days, what time do you usually go to sleep the night or day before?”. The first two items were intended to assess weekdays, and the latter two were intended to assess weekends. Hours of sleep per night on weekdays and weekends were calculated, and a weighted average was computed, weighting the weekday items at 5/7 and the weekend items at 2/7. In accordance with previous research and with developmentally appropriate recommendations for optimal sleep duration (12,19,22–26), short and long sleep were defined as sleeping less than 6 or more than 10 hours, respectively.
Demographic characteristics
Participant age at each interview date was calculated and rounded to the nearest year. Participant sex, race, and ethnicity were self-reported at Wave 1. For purposes of the current report, four mutually exclusive racial/ethnic categories were created: (non-Hispanic) White, (non-Hispanic) African American, Hispanic, and (non-Hispanic) other race/ethnicity.
Statistical analysis
Mean sleep duration at each age was calculated using IBM SPSS version 20. Add Health Wave 4 grand sample weights were applied in all analyses. JoinPoint software (27) was used to test whether sleep duration patterned by developmental phase as expected. JoinPoint identifies inflection points at which the slope of a trend line changes significantly, identifying the smallest number of partitions, such that adding another partition does not significantly improve the model fit according to permutation tests and Bayesian Information Criteria comparison. Sex and race differences in mean sleep duration within each age group were tested using pairwise t-tests. Sex and race differences in prevalence of short and long sleep within each age group were tested using pairwise Chi Square tests. Due to high probability of statistical significance given large sample size, significance was tested using χ = .001 for all comparisons.
Results
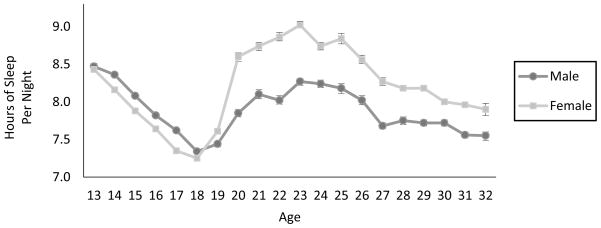
Average sleep duration decreased across adolescence from a high of 8.5 hours of sleep per night at age 13 to a low of 7.3 hours at age 18. Sleep duration then increased during the emerging adulthood period, through age 22, to 8.5 hours, and declined in early adulthood, to 7.7 hours at age 32 (Table 1 and Figure 1). Males slept significantly longer than females in adolescence (7.8 versus 7.6 hours, respectively). Females slept longer than males during emerging adulthood (8.4 hours per night for females and 7.8 hours per night for males) and during early adulthood (8.4 hours per night for females and 7.9 hours per night for males).
Table 1.
Mean sleep duration and prevalence of short and long sleep duration by age
| Age | N | Sleep Duration M (SD) | Sleep < 6 hours/night % | Sleep > 10 hours/night % |
|---|---|---|---|---|
| Total | 52,080 | 7.9 (1.9) | 1.1 | 2.9 |
| 13 | 1129 | 8.5 (1.3) | 1.1 | 4.5 |
| 14 | 2870 | 8.3 (1.3) | 1.5 | 4.0 |
| 15 | 3888 | 8.0 (1.3) | 2.7 | 2.8 |
| 16 | 4858 | 7.7 (1.4) | 4.7 | 2.9 |
| 17 | 5288 | 7.5 (1.4) | 6.2 | 2.1 |
| 18 | 5101 | 7.3 (1.5) | 8.5 | 1.6 |
| 19 | 2691 | 7.5 (1.7) | 9.0 | 5.0 |
| 20 | 1828 | 8.2 (2.2) | 7.6 | 15.0 |
| 21 | 1778 | 8.4 (2.4) | 8.8 | 20.1 |
| 22 | 2178 | 8.5 (2.6) | 9.9 | 23.6 |
| 23 | 2277 | 8.6 (2.3) | 6.4 | 25.0 |
| 24 | 2211 | 8.5 (2.2) | 8.3 | 23.0 |
| 25 | 1482 | 8.5 (2.5) | 8.4 | 25.3 |
| 26 | 1476 | 8.3 (2.1) | 6.1 | 14.1 |
| 27 | 1845 | 8.0 (1.9) | 9.1 | 8.9 |
| 28 | 2314 | 8.0 (2.1) | 9.7 | 7.1 |
| 29 | 2815 | 8.0 (2.0) | 8.7 | 8.0 |
| 30 | 2746 | 7.9 (2.1) | 11.2 | 8.2 |
| 31 | 2489 | 7.8 (2.0) | 10.2 | 5.9 |
| 32 | 816 | 7.7 (1.9) | 11.1 | 5.6 |
Figure 1.
Mean sleep duration per night, ages 13–32. Error bars represent 95% confidence intervals. Individuals contributed multiple observations over the four waves of the study.
The percentage of individuals reporting short sleep duration, fewer than 6 hours per night, increased from 1.1% to 8.5% in adolescence, ranged from 7.6%–9.9% in emerging adulthood, and generally increased across early adulthood to 11.1% at age 32. Likewise, the percentage of individuals reporting long sleep duration, longer than 10 hours per night, decreased across adolescence, from 4.5% at age 13 to 1.6% at age 18, increased in emerging adulthood to 23.6% at age 22, then subsequently decreased across the early adulthood period to 5.6% by age 32.
The JoinPoint analysis of average sleep duration revealed two significant inflection points, an increase beginning at age 18 and a decrease beginning at age 22. Therefore, sleep was patterned according to developmental phase—adolescence, emerging adulthood, and early adulthood—as expected. This result is analogous to a significant cubic trend in traditional regression analysis, with interpretability improved by the identification of specific inflection points.
Average nightly sleep duration differed significantly by sex and race/ethnicity within each of the three developmental periods (Table 2 and Figure 2). Female adolescents slept slightly less, 10 minutes per night, than males, but women slept 37 minutes longer per night than men in emerging adulthood and 30 minutes longer than men in early adulthood. The largest sex differences occurred at ages 22 and 23, when women slept 50 and 45 minutes, respectively, longer than men. Mean sleep duration also varied significantly by race/ethnicity. Across the three developmental periods, White and Hispanic individuals consistently reported the longest sleep duration, while African Americans and individuals of other race/ethnicity generally reported the shortest sleep durations. Racial and ethnic differences in sleep duration were relatively smaller than sex differences. In adolescence, the largest difference in sleep duration was between White and African American adolescents; White adolescents slept on average 14 minutes longer per night than African American adolescents. In emerging adulthood, White adults slept about 11 minutes longer than adults of other race/ethnicity, who reported the least amount of sleep in that age group. In early adulthood, Whites again reported the most sleep, 8.1 hours per night, about 13 minutes longer per night than African American adults.
Table 2.
Mean sleep duration per night, by sex and race/ethnicity
| Adolescence (Ages 13–18) | Emerging Adulthood (Ages 19–22) | Early Adulthood (Ages 23–32) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| n | M | 95% CI | n | M | 95% CI | n | M | 95% CI | |
| Total | 23,134 | 7.71 | 7.70–7.72 | 8,475 | 8.12 | 8.10–8.13 | 20,469 | 8.10 | 8.09–8.11 |
| Sex | |||||||||
| Male | 10,636 | 7.79 | 7.78–7.80a | 3,929 | 7.81 | 7.78–7.83a | 9,646 | 7.86 | 7.85–7.88a |
| Female | 12,498 | 7.63 | 7.62–7.64a | 4,546 | 8.43 | 8.40–8.45a | 10,823 | 8.36 | 8.34–8.37a |
| Race/Ethnicity | |||||||||
| White | 12,500 | 7.78 | 7.77–7.79a,b,c | 4,638 | 8.17 | 8.15–8.20a,b | 10,783 | 8.10 | 8.08–8.11a,b,c |
| African American | 5,031 | 7.54 | 7.52–7.55a,d | 1,846 | 8.10 | 8.06–8.15 | 4,318 | 7.89 | 7.87–7.92a,d |
| Hispanic | 3,560 | 7.72 | 7.70–7.73b,d,e | 1,269 | 8.01 | 7.97–8.05a | 3,391 | 8.38 | 8.35–8.40b,d,e |
| Other | 2,043 | 7.55 | 7.53–7.58c,e | 722 | 7.98 | 7.92–8.04b | 1,977 | 7.93 | 7.89–7.96c,e |
Significant sex or race/ethnicity differences in mean sleep duration within age group (adolescence, emerging adulthood, and early adulthood). Groups with matching superscripts differed significantly, p < .001.
Figure 2.
Mean sleep duration per night, ages 13–32, by sex. Error bars represent 95% confidence intervals.
Prevalence of short and long sleep varied significantly by sex (Table 3). Adolescent girls were more likely than boys to sleep less than 6 hours per night and equally likely to sleep longer than 10 hours per night. In emerging and early adulthood, these patterns reversed; women were less likely to sleep shorter than 6 hours per night and more likely to sleep longer than 10 hours per night compared to men in both emerging and early adulthood.
Table 3.
Prevalence of short and long sleep by sex and race/ethnicity
| Adolescence (ages 13–18) | Emerging Adulthood (ages 19–22) | Early Adulthood (ages 23–32) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % <6 hours |
95% CI | % >10 hours |
95%CI | n | % <6 hours |
95% CI | % >10 hours |
95% CI | n | % <6 hours |
95% CI | % >10 hours |
95% CI | |
| Total | 23,134 | 5.00 | 4.90–5.10 | 2.60 | 2.54–2.69 | 8,475 | 8.93 | 8.71–9.15 | 15.39 | 15.10–15.67 | 20,471 | 8.94 | 8.80–9.08 | 12.77 | 12.61–12.93 |
| Sex | |||||||||||||||
| Male | 10,636 | 4.18 | 4.05–4.31a | 2.57 | 2.46–2.67 | 3,929 | 10.71 | 10.37–11.05a | 9.99 | 9.66–10.31a | 9,646 | 10.62 | 10.41–10.83a | 10.18 | 9.98–10.39a |
| Female | 12,498 | 5.81 | 5.66–5.96a | 2.67 | 2.57–2.77 | 4,546 | 7.13 | 6.85–7.42a | 20.84 | 20.39–21.29a | 10,823 | 7.20 | 7.02–7.38a | 15.47 | 15.22–15.73a |
| Race/Ethnicity | |||||||||||||||
| White | 12,500 | 3.98 | 3.86–4.10a,b,c | 2.58 | 2.48–2.68a,b,c | 4,638 | 8.13 | 7.85–8.42a,b | 15.47 | 15.10–15.85a,b,c | 10,783 | 7.50 | 7.33–7.67a,b,c | 11.39 | 11.19–11.60a,b |
| African American | 5,031 | 8.60 | 8.28–8.91a,d,e | 3.53 | 3.32–3.74a,d,e | 1,846 | 11.75 | 11.14–12.35a,c | 17.85 | 17.13–18.57a,d,e | 4,318 | 14.04 | 13.62–14.47a,d,e | 13.08 | 12.67–13.49a,c,d |
| Hispanic | 3,560 | 4.55 | 4.32–4.77b,d,f | 2.13 | 1.98–2.29b,d | 1,269 | 8.07 | 7.58–8.56c,d | 14.17 | 13.54–14.79b,d,f | 3,391 | 8.60 | 8.29–8.92b,d,f | 17.49 | 17.06–17.92b,c,e |
| Other | 2,043 | 6.04 | 5.65–6.43c,e,f | 2.12 | 1.88–2.35c,e | 722 | 10.65 | 9.78–11.51b,d | 12.27 | 11.35–13.18c,e,f | 1,977 | 9.93 | 9.41–10.45c,e,f | 10.68 | 10.14–11.22d,e |
Significant sex or race/ethnicity differences in prevalence of short or long sleep duration within age group (adolescence, emerging adulthood, and early adulthood). Groups with matching superscripts differed significantly, p < .001.
Short sleep duration was most common among African Americans and least common among Whites and Hispanics in all three developmental periods (Table 3). Long sleep duration was most common among African Americans in adolescence and emerging adulthood and among Hispanics in early adulthood and least common among the other race/ethnicity group in all developmental periods.
Discussion
Age differences in sleep duration
The current study revealed developmental patterning of average nightly sleep duration and of prevalence of short and long sleep duration by age, as well as substantial differences by sex and race/ethnicity within age groups. Analyses revealed two significant inflection points in sleep duration trends by age. Following a decrease in sleep duration across adolescence, ages 13–18, there was a steep increase beginning at age 19. The second inflection point occurred at age 22, which marked the beginning of gradual decreases in sleep duration through age 32. These results provide clear evidence that sleep is patterned by developmental stage. The reported decrease in sleep duration in adolescence is consistent with a number of previous studies documenting decreases in sleep duration across adolescence (10–16). We also found previously unreported developmental trends extending into emerging and early adulthood, an increase in sleep duration following the typical transition out of high school, beginning at age 19 and a decrease in sleep duration beginning at age 22 and continuing throughout early adulthood.
Sleep duration is determined by both biological and social factors. The developmental trends in mean and extreme sleep duration reported here are likely attributable to a coalescence of biological and social forces that lead to declining sleep during adolescence, including sleep phase delay and early school start times. The marked upturn in emerging adulthood may be driven by context-the freedom to “sleep in” later as a result of no longer being required to wake early for high school. Gradual decreases in average sleep duration in early adulthood potentially reflect an accumulation of adulthood roles and responsibilities such as full time work, marriage, and parenthood. Additional research probing the associations of adulthood roles and responsibilities with sleep duration is warranted.
The National Sleep Foundation recommends that adolescents should sleep 9 hours per night, and adults should sleep 7–8 hours per night (22,23). Our results extend in a national, population-based US sample what has been observed in previous studies: On average, American adolescents get significantly less than the recommended amount of sleep (11,12,28). Insufficient sleep in adolescence is associated with primary determinants of morbidity and mortality, including depression, suicidality, motor vehicle accident, alcohol and marijuana use, obesity, and pre-diabetic insulin sensitivity (8,8,25,29,30). Our results raise alarm that widespread insufficient sleep among American adolescents may lead to increasing prevalence of chronic disease in adulthood. One important question for future research will be whether insufficient sleep experienced in adolescence has a negative impact on adulthood health, independent of early adulthood sleep duration.
Our results regarding emerging and early adults are more positive: On average, individuals ages 19–32 reported sleeping just over eight hours per night, which corresponds well to the National Sleep Foundation recommendations. However, a substantial portion of emerging and early adults reported sleeping less than 6 hours per night (8.9% of emerging adults and 8.9% of early adults) or longer than 10 hours per night (15.4% of emerging adults and 12.8% of early adults). Recent research has demonstrated prospective associations of short and long sleep during adolescence and early adulthood with increased risk of diabetes, hypertension, high cholesterol, and all-cause mortality in later adulthood (3–6). Thus, although the emerging and early adults report sufficient sleep on average, those who experience short and long sleep may be at heightened risk for a range of serious health conditions.
Sex and race differences in sleep duration
Sleep duration varied significantly by sex and race/ethnicity within each of the three developmental periods examined. Females reported sleeping less than males in adolescence and more in emerging and early adulthood. That women sleep more in adulthood may be good news, considering recent reports of stronger associations between sleep and high cholesterol and with heightened levels of inflammatory markers implicated in coronary heart disease in women versus men (5,31). African Americans and individuals of other race/ethnicity reported lower mean sleep duration than White and Hispanic individuals across the three developmental periods. African Americans were the most likely to report short sleep duration in all three developmental periods, consistent with prior research that has shown high prevalence of extremely long and short sleep in this group across the lifespan (18,19). Long sleep duration was most common among African Americans during adolescence and emerging adulthood and among Hispanics during early adulthood. The high prevalence of short and long sleep among African Americans indicates that sleeping too much or too little may be one mechanism leading to disparities in the occurrence chronic disease among this group later in life (32).
Limitations
This study had several limitations. First, sleep data were self-reported. Although some studies have reported disagreement between objective and subjective reports of sleep duration (33) self-reports of sleep duration have been found to generally correspond well to more objective measures of sleep such as actigraphy (34,35). Given that objective measures of sleep are not currently available in nationally representative samples such as ours and that self-reported sleep duration is a reliable, prospective predictor of mortality and chronic disease (3–6), self reports are valid for the current purposes of establishing normative developmental variation in sleep duration. Second, the items used to measure sleep duration in Waves 1 and 2, when participants reported average daily sleep duration, differed from those used in Waves 3 and 4, when participants reported wake times and bed times on weekdays and weekends. Although identical measurement across waves would have been ideal, changes in measurement across time are a sometimes unavoidable occurrence in longitudinal studies, as measures are improved but therefore changed across the duration of the study. For this same reason, we were unable to report weekday and weekend sleep duration separately, owing to the fact that they were not assessed separately in Waves 1 and 2 of the study, the waves comprising the adolescent portion of our sample. Differential sleep duration on weekdays and weekends, and particularly weekend “catch-up” sleep, has been implicated in a range of negative outcomes, including poor academic performance, obesity, and suicidality among adolescents (36–38). Future studies should assess how the age, sex, and race differences in sleep duration reported here are reflected in weekday versus weekend sleep duration.
Finally, the current data were collected from 1994–2008. This period of time in the U.S. captures the widespread use of mobile phones, computers, and video games. Compared with the present time period, however, it reflects lower utilization of “smartphones” such as the iPhone, which was first released in 2007. Thus, the effects of increased use of smartphones or other new technologies known to interfere with sleep (39) are not fully reflected in these data. Smartphones are currently most common among younger and higher-income individuals (40), and use of this technology could thus be expected to exert particular impact on sleep in these groups.
Conclusions
This is the first study to describe normative age variation in sleep duration from adolescence through early adulthood in a national US sample. Population norms are presented for mean sleep duration as well as the prevalence of short and long sleep from ages 13 through 32, a heterogeneous and formative period of the lifespan. Analyses demonstrated that sleep duration is developmentally patterned from adolescence through early adulthood, with a steep decrease across adolescence, an increase in emerging adulthood, and gradual decreases across early adulthood. Knowledge of developmental trends in average and extreme sleep durations will inform deeper understanding of the role of sleep duration in the development, maintenance, and alteration of many behaviors and physical and mental health conditions in which it is known to be involved. Recent research has begun to illuminate the role of sleep in contributing to the development of diabetes, obesity, heart disease, substance abuse, depression, and other conditions. Understanding the age at which insufficient sleep emerges, in the context of developmental norms presented here, will inform future developmentally targeted studies of risk factors for insufficient sleep and mechanisms by which sleep may catalyze disease. An important direction for future research will be the further characterization of subgroups who deviate from the norms presented here, particularly those with extremely long and short sleep duration, and to characterize the coincident and resultant disease markers that may explain sleep-associated morbidity and mortality.
Implications and Contribution.
This study reveals normative developmental shifts in sleep duration from adolescence through early adulthood. Sleep duration decreases sharply across adolescence, increases somewhat in emerging adulthood, and decreases again across early adulthood. These normative data provide a developmentally informed foundation for studies of sleep’s role in a wide range of health conditions.
Acknowledgments
The authors gratefully acknowledge support from the Robert Wood Johnson Health and Society Scholars program (Maslowsky) and Angela Forgues, BA, for editorial assistance.
Contributor Information
Julie Maslowsky, Robert Wood Johnson Foundation Health and Society Scholars Program, School of Medicine and Public Health, University of Wisconsin-Madison.
Emily Ozer, Division of Community Health and Human Development, School of Public Health, University of California-Berkeley.
References
- 1.Brand S, Kirov R. Sleep and its importance in adolescence and in common adolescent somatic and psychiatric conditions. Int J Gen Med. 2011;4:425–442. doi: 10.2147/IJGM.S11557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Walker MP. The role of sleep in cognition and emotion. Ann N Y Acad Sci. 2009;1156:168–197. doi: 10.1111/j.1749-6632.2009.04416.x. [DOI] [PubMed] [Google Scholar]
- 3.Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2010;33(5):585–592. doi: 10.1093/sleep/33.5.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gangwisch JE, Heymsfield SB, Boden-Albala B, et al. Sleep duration as a risk factor for diabetes incidence in a large US sample. Sleep. 2007;30(12):1667–1673. doi: 10.1093/sleep/30.12.1667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gangwisch JE, Malaspina D, Babiss LA, et al. Short sleep duration as a risk factor for hypercholesterolemia: Analyses of the National Longitudinal Study of Adolescent Health. Sleep. 2010;33(7):956–961. doi: 10.1093/sleep/33.7.956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gangwisch JE, Feskanich D, Malaspina D, Shen S, Forman JP. Sleep duration and risk for hypertension in women: results from the nurses’ health study. Am J Hypertens. 2013;26(7):903–911. doi: 10.1093/ajh/hpt044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity. 2008;16(3):643–653. doi: 10.1038/oby.2007.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McKnight-Eily LR, Eaton DK, Lowry R, et al. Relationships between hours of sleep and health-risk behaviors in US adolescent students. Prev Med. 2011;53(4–5):271–273. doi: 10.1016/j.ypmed.2011.06.020. [DOI] [PubMed] [Google Scholar]
- 9.Moore M, Kirchner HL, Drotar D, et al. Correlates of adolescent sleep time and variability in sleep time: The role of individual and health related characteristics. Sleep Med. 2011;12(3):239–245. doi: 10.1016/j.sleep.2010.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Crowley SJ, Acebo C, Carskadon MA. Sleep, circadian rhythms, and delayed phase in adolescence. Sleep Med. 2007;8(6):602–612. doi: 10.1016/j.sleep.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 11.Wahlstrom K. Changing times: Findings from the first longitudinal study of later high school start times. NASSP Bulletin. 2002;86(633):3–21. [Google Scholar]
- 12.Leger D, Beck F, Richard J-B, Godeau E. Total sleep time severely drops during adolescence. PLoS ONE. 2012;7(10):e45204. doi: 10.1371/journal.pone.0045204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Olds T, Maher C, Blunden S, Matricciani L. Normative data on the sleep habits of Australian children and adolescents. Sleep. 2010;33(10):1381–1388. doi: 10.1093/sleep/33.10.1381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Williams JA, Zimmerman FJ, Bell JF. Norms and trends of sleep time among US children and adolescents. JAMA Pediatr. 2013;167(1):55–60. doi: 10.1001/jamapediatrics.2013.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carskadon MA. Adolescent sleep patterns: biological, social, and psychological influences. Cambridge University Press; 2002. [Google Scholar]
- 16.Knutson KL. The association between pubertal status and sleep duration and quality among a nationally representative sample of U. S. Adolescents. Am J Hum Biol. 2005;17(4):418–424. doi: 10.1002/ajhb.20405. [DOI] [PubMed] [Google Scholar]
- 17.Furstenberg FF, Kennedy S, McLoyd VC, et al. Growing up is harder to do. Contexts. 2004;3:33–41. [Google Scholar]
- 18.Nunes J, Jean-Louis G, Zizi F, et al. Sleep duration among black and white Americans: Results of the National Health Interview Survey. J Natl Med Assoc. 2008;100(3):317–322. doi: 10.1016/s0027-9684(15)31244-x. [DOI] [PubMed] [Google Scholar]
- 19.Krueger PM, Friedman EM. Sleep duration in the United States: A cross-sectional population-based study. Am J Epidemiol. 2009;169(9):1052–1063. doi: 10.1093/aje/kwp023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Harris KM. The National Longitudinal Study of Adolescent Health (Add Health), Waves I & II, 1994–1996; Wave III, 2001–2002; Wave IV, 2007–2009 [data file and documentation] Chapel Hill, NC: Carolina Population Center, University of North Carolina at Chapel Hill; 2009. [Google Scholar]
- 21.Brownstein N, Kalsbeek WD, Tabor J, et al. [Accessed September 13, 2013];Non-response in Wave IV of the National Longitudinal Study of Adolescent Health. http://www.cpc.unc.edu/projects/addhealth/data/guides/W4_nonresponse.pdf.
- 22.National Sleep Foundation. [Accessed September 12, 2013];Teens and sleep. http://www.sleepfoundation.org/article/sleep-topics/teens-and-sleep.
- 23.National Sleep Foundation. [Accessed September 12, 2013];How much sleep do adults need? http://www.sleepfoundation.org/article/white-papers/how-much-sleep-do-adults-need.
- 24.Bin YS, Marshall NS, Glozier N. Sleeping at the limits: the changing prevalence of short and long sleep durations in 10 countries. Am J Epidemiol. 2013;177:826–833. doi: 10.1093/aje/kws308. [DOI] [PubMed] [Google Scholar]
- 25.Javaheri S, Storfer-Isser A, Rosen CL, et al. Association of short and long sleep durations with insulin sensitivity in adolescents. J Pediatr. 2011;158:617–623. doi: 10.1016/j.jpeds.2010.09.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pallesen S, Saxvig IW, Molde H, et al. Brief report: behaviorally induced insufficient sleep syndrome in older adolescents: prevalence and correlates. J Adolesc. 2011;34:391–395. doi: 10.1016/j.adolescence.2010.02.005. [DOI] [PubMed] [Google Scholar]
- 27.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19:335–351. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 28.Eaton DK, McKnight-Eily LR, Lowry R, et al. Prevalence of insufficient, borderline, and optimal hours of sleep among high school students – United States, 2007. J Adolesc Health. 2010;46:399–401. doi: 10.1016/j.jadohealth.2009.10.011. [DOI] [PubMed] [Google Scholar]
- 29.Mitchell JA, Rodriguez D, Schmitz KH, et al. Sleep duration and adolescent obesity. Pediatrics. 2013;131(5):1–7. doi: 10.1542/peds.2012-2368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Martiniuk ALC, Senserrick T, Lo S, et al. Sleep-deprived young drivers and the risk for crash: the DRIVE prospective cohort study. JAMA Pediatr. 2013;167:647–655. doi: 10.1001/jamapediatrics.2013.1429. [DOI] [PubMed] [Google Scholar]
- 31.Prather AA, Epel ES, Cohen BE, et al. Gender differences in the prospective associations of self-reported sleep quality with biomarkers of systemic inflammation and coagulation: Findings from the Heart and Soul Study. J Psychiatr Res. 2013;47:1228–1235. doi: 10.1016/j.jpsychires.2013.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Grandner MA, Buxton M, Jackson N, et al. Extreme sleep durations and increased C-reactive protein: Effects of sex and ethnoracial group. Sleep. 2013;36:769–779E. doi: 10.5665/sleep.2646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Arora T, Broglia E, Pushpakumar D, et al. An investigation into the strength of the association and agreement levels between subjective and objective sleep duration in adolescents. PLoS ONE. 2013;8(8):e72406. doi: 10.1371/journal.pone.0072406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tremaine RB, Dorrian J, Blunden S. Subjective and objective sleep in children and adolescents: Measurement, age, and gender differences. Sleep Biol Rhythms. 2010;8(4):229–238. [Google Scholar]
- 35.Wolfson AR, Carskadon MA, Acebo C, et al. Evidence for the validity of a sleep habits survey for adolescents. Sleep. 2003;26(2):213–216. doi: 10.1093/sleep/26.2.213. [DOI] [PubMed] [Google Scholar]
- 36.Lee YJ, Cho S-J, Cho IH, Kim SJ. Insufficient sleep and suicidality in adolescents. Sleep. 2012;35(4):455–460. doi: 10.5665/sleep.1722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Spruyt K, Molfese DL, Gozal D. Sleep duration, sleep regularity, body weight, and metabolic homeostasis in school-aged children. Pediatrics. 2011;127(2):e345–352. doi: 10.1542/peds.2010-0497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kim SJ, Lee YJ, Cho S-J, et al. Relationship between weekend catch-up sleep and poor performance on attention tasks in Korean adolescents. Arch Pediatr Adolesc Med. 2011;165(9):806–812. doi: 10.1001/archpediatrics.2011.128. [DOI] [PubMed] [Google Scholar]
- 39.Chahal H, Fung C, Kuhle S, Veugelers PJ. Availability and night-time use of electronic entertainment and communication devices are associated with short sleep duration and obesity among Canadian children. Pediatr Obes. 2013;8(1):42–51. doi: 10.1111/j.2047-6310.2012.00085.x. [DOI] [PubMed] [Google Scholar]
- 40.Pew Internet and American Life Project. [Accessed September 12, 2013];Two thirds of young adults and those with higher income are smartphone owners. http://www.pewinternet.org/Reports/2012/Smartphone-Update-Sept-2012/Findings.aspx.