Abstract
Purpose/Objectives
To test the effectiveness of an interdisciplinary cancer support team (CST) on caregiver satisfaction with end-of-life (EOL) care for family members with advanced cancer.
Design
Quasi-experimental pre- and post-test tandem design.
Setting
Outpatient clinics of a comprehensive cancer center in urban Cleveland, OH.
Sample
106 family caregivers.
Methods
Participants were enrolled into the control or CST group. Caregiver mood state and social support were measured at enrollment as well as at 3, 9, and 15 months, and satisfaction with EOL care was measured eight weeks after the patient's death.
Main Research Variables
Caregiver mood state, social support, and satisfaction with EOL care.
Findings
The intervention made no statistically significant contribution to caregiver mood state or perception of social support. The intervention group reported higher satisfaction with overall EOL care as well as five specific areas of EOL satisfaction (i.e., pain relief, information about managing pain, speed in treating symptoms, information regarding side effects, and coordination of care).
Conclusions
The CST yielded improved EOL satisfaction.
Implications for Nursing
Although the emotional impact of an impending loss of a loved one may not change with the provision of support, perception that a loved one was well cared for in the terminal phase of illness may have long-range benefits through the grieving process. Investigation of the long-range effects of satisfaction with EOL care on the grieving process is warranted.
Keywords: family caregivers, end of life, cancer
The importance of attending to family needs as an integral part of quality cancer care has been recognized (American Cancer Society, 2014; National Cancer Institute, 2014). An increase in reports of intervention trials to support families has occurred, particularly when a family member has advanced cancer (Northouse, Katapodi, Song, Zhang, & Mood, 2010). The needs of family caregivers have been described as including emotional support or education and practical help in performing tasks of caregiving. Because the care of patients with cancer has increasingly moved to the home, families are taxed with demands for providing physical care, medication administration, and symptom monitoring (Glajchen, 2004). All of those needs have been noted to increase at the end of life (EOL) (Cameron, Franche, Cheung, & Stewart, 2002; Kim & Given, 2008).
Although the quality of care for patients with cancer at EOL has become a major focus of research and quality improvement initiatives, far less attention has been paid to the experience, needs, and satisfaction of family caregivers in the final phase of illness. A number of studies have been performed with mixed samples of families of patients with and without cancer, which have provided some important insights (Steinhauser et al., 2000; Teno, Casey, Welch, & Edgman-Levitan, 2001). Among the items consistently rated as important at EOL by a large sample of seriously ill patients, bereaved family members, and healthcare providers were pain and symptom management and preparation for death (Steinhauser et al., 2000). Others have identified five domains of EOL care that defined quality: physical comfort, control of decisions, relieving family members of the burden of being the constant advocate, education of family members to instill confidence in caring for the loved one, and emotional support of the family (Teno et al., 2001).
The study of effective interventions for family caregivers of people with cancer at EOL is complicated by the recognized influence of situational and individual psychodynamic factors. Presence of social resources and subjective appraisal of stress have been identified as significant predictors of caregiver depression and life satisfaction (Haley, LaMonde, Han, Burton & Schon-wetter, 2003), and stress appraisal and coping resources have been identified as key mediating variables influencing caregiver outcomes (Northouse, 2005).
The investigation reported in the current article is part of a larger study conducted to test the effect of integrating an interdisciplinary cancer support team (CST) into the routine care of patients with advanced lung, gastrointestinal (GI), or gynecologic (GYN) cancer. The primary aims of that study were patient centered (i.e., quality of life and quality of care at EOL); however, the intervention was designed to include assessment and support of family caregivers. The inclusion of family caregivers gave the authors the opportunity to examine family outcomes (e.g., satisfaction with care at EOL) and the possible influence of mood state and social support on family satisfaction. The purpose of the current article is to report the results of providing an interdisciplinary comprehensive support program to the families of patients with advanced cancer in the last phase of life.
Methods
Setting and Population
The parent study, testing the effect of an interdisciplinary CST, was conducted at two outpatient clinics of Seidman Cancer Center in Cleveland, OH from 2008–2012. Consistent with Donabedian's (1988) framework using structure, process, and outcome, the purpose of the project was to alter the structure of the care delivery system to modify care processes and achieve improved outcomes. The overall sample is described in another article (Daly, Douglas, Gunzler, & Lipson, 2013). In the parent study, 610 patients were enrolled, and 214 (35%) died during the study period. A subsample (i.e., patients who died and their caregivers) of the parent study is included in the analyses described here. Of those who died, 106 had caregivers who participated in the parent study.
Adult patients with newly diagnosed stage III or IV lung, GI, or GYN cancer were screened for eligibility (n = 9,362) during the study period. Of those, 1,233 met eligibility criteria, which also included Eastern Cooperative Oncology Group (ECOG) scores of less than or equal to 3, capacity to provide informed consent, and intention to receive treatment at the cancer center. Patients with stage IIB pancreatic cancer were also considered eligible because their prognoses were similar to stage III lung cancer. Eligible patients were approached at their first or second appointment by a research assistant (RA); the study was explained, and written informed consent was obtained.
Design
The current study used a pre- and post-test design. The control period occurred prior to implementation of the CST, and the experimental period occurred after implementation of the CST. For the first nine months of the study, no intervention was provided, and all participants who were enrolled were in the control group. Data collection occurred at enrollment as well as at 3, 9, and 15 months. When the last control participant was enrolled after 10 months of enrolling participants to the control group, the intervention was introduced at the study site. At that point, all participants subsequently enrolled were experimental participants. Data collection for those participants followed the same pattern as for the control participants; data were collected at enrollment as well as at 3, 9, and 15 months after study enrollment. The protocol, including the consent procedure, was approved by the study site's institutional review board.
Control Group
Patients and caregivers in the control group received support and care coordination from their usual oncology team, including nurses, doctors, advanced practice nurses, and social workers, during active treatment and follow-up. Patients in the control group had access to support services depending on the assessment of need by the primary oncology team. Services were not protocol-driven and were provided independently by each person rather than as a team. No minimum amount of contact with any of the providers was prescribed, no defined focus existed for care planning, discussion of advance directives, or support measures for patients and families.
Intervention Group With Cancer Support Team
Patients and caregivers in the intervention group received support and care coordination from the interdisciplinary CST consistently, integrated in the routine care provided to patients with advanced lung, GI, and GYN cancers. Services were provided in conjunction with active treatment, which included radiation, chemotherapy, and/or surgery. The support service consisted of eight components: (a) baseline assessment of symptoms, distress, and social and spiritual concerns of the patient and primary family caregiver; (b) summary of a plan for supportive services entered in the medical record; (c) ongoing provision of symptom management, education, and psychosocial and spiritual support according to patient need; (d) introduction of advanced care planning discussions as early as possible; (e) a minimum of monthly contacts with the patient in the clinic during treatment or by phone if the patient had no clinic appointments; (f) daily availability to the patient and family caregiver by phone for questions or concerns; (g) regular (monthly or quarterly) meetings with each oncologist on the relevant disease teams to review and coordinate care plans for his or her patients; and (h) referral to and coordination with community providers (e.g., home care, palliative care, hospice) when appropriate.
A member of the CST met each patient and family caregiver on the first or second clinic appointment, explained the purpose of the team (to provide supportive services as an adjunct to their cancer treatment), obtained a detailed history, and performed the baseline assessment. Patients and family caregivers subsequently met and had access to all members of the CST, but the focus and amount of services provided over time (e.g., help with financial concerns, intensive symptom management, spiritual counseling) was determined by patient and caregiver need and varied among patients and over time for individual patients. At minimum, meetings with a member of the CST occurred monthly. Patients and caregivers were encouraged to contact team members at any time with questions. The team reviewed all new patients after admission and met weekly as a team to review active patients and coordinate care plans throughout the 15-month study period, or until the patient died or was transferred to hospice.
Procedures and Measures
Following consent, the RA interviewed the patient and caregiver in the clinic to obtain demographic information and clinical information as well as health-related quality of life (HRQOL), comorbidity, mood state, and social support. For patients, HRQOL was measured using the Functional Assessment of Cancer Therapy–General (FACT-G) tool. This tool has established reliability (α = 0.89) and validity (r = 0.77), with higher scores reflecting better HRQOL (Cella et al., 1995; Schipper, Clinch, McMurray, & Levitt, 1984). Patient comorbidity was measured using the Charlson Comorbidity Index, a tool with established reliability (r = 0.8–0.84) and validity (r = 0.71) (Chaudhry, Jin, & Meltzer; 2005; Mulrow, Gerety, Cornell, Lawrence, & Kanten, 1994). The measures were used for descriptive purposes.
Outcome variables used in this study were the Profile of Mood States (POMS), Medical Outcomes Study Social Support Survey (MOS-SS), and Family Satisfaction With End-of-Life Care (FAMCARE). Caregiver mood state was measured using POMS, where higher scores indicate a higher degree of mood disturbance. This tool has established reliability (α = 0.88–0.94) and moderate discriminant validity (McNair, Lorr, & Droppleman, 1971). The total POMS score captures the mood states of anger, depression, fatigue, tension, and vigor.
Caregiver social support was measured using MOS-SS, with higher scores reflecting more perceived social support. This tool has established reliability (α = 0.93) and validity (factor loadings greater than 0.6) (Mahmud, Awang, & Mohamed, 2004).
Satisfaction with care received at EOL was measured using FAMCARE, which measures the degree to which family members are satisfied with the health care received by the patient and family with respect to four components of care (i.e., information giving, availability of care, psychological care, and physical patient care), with higher scores reflecting more satisfaction with EOL care. The tool has established reliability (α = 0.93) and criterion validity (McCusker Scale of 0.8 and 0.77) (Aoun, Bird, Kristjanson, & Currow, 2010). Postenrollment data collection points were at 3, 9, and 15 months. A monthly phone call was made by the RA to determine patient status (i.e., survival and location) and resource use (i.e., initiation of home care, placement in a nursing facility, or initiation of hospice services). If a patient died during the 15-month time period, which was the sample used for the current study, the RA scheduled a telephone interview eight weeks after the patient's death for the purpose of administering FAMCARE (Daly, Douglas, O'Toole, et al., 2010).
Data Analysis
All analyses were performed using SPSS®, version 20.0. Univariate comparisons of demographic and clinical characteristics of patients and caregivers were performed using one-way analysis of variance (ANOVA) for continuous variables, and chi-square for categorical variables. Hospice length of stay was highly skewed and exhibited kurtosis, and the Mann-Whitney U test was employed and reported. Multiple linear regression analysis was used to examine the impact of group on key outcome variables after controlling for influential variables. Repeated measures ANOVA was conducted to examine changes in POMS and MOS-SS over time. Covariates included variables that were statistically significant in comparison with experimental and control groups (e.g., caregiver gender), as well as variables that were shown to influence burden associated with EOL decision making (e.g., caregiver race) (Braun, Beyth, Ford, & McCullough, 2008; Jenkins, Lapelle, Zapka, & Kurent, 2005; Waters, 2001).
The key outcome variables examined were caregiver mood (POMS), social support (MOS-SS), and the 13 postdeath satisfaction items included in FAMCARE. FAMCARE has 20 items, 7 of which ask about EOL care for patients who died in the hospital. Only eight of the patients included in the analyses died in a hospital setting. Therefore, the sum of the 13 items that applied to EOL care regardless of location of death was used. For all analyses, a two-sided p value of less than 0.05 was considered to be statistically significant.
Results
Sample Characteristics
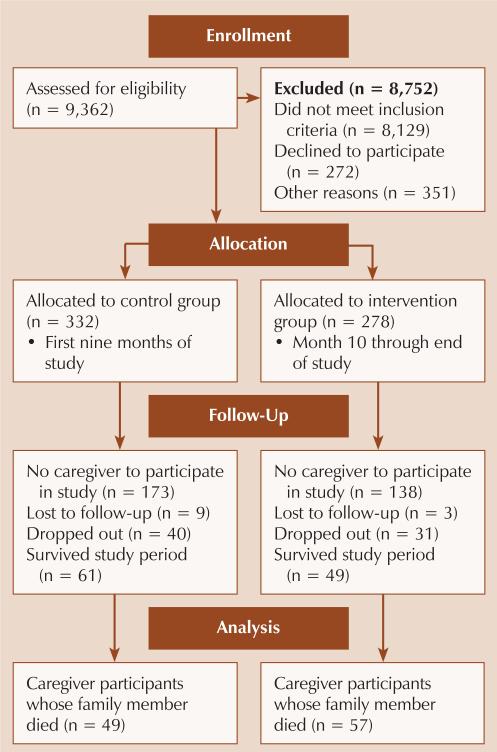
A convenience sample of 610 were enrolled and consented to participate in the study (see Figure 1). The control group included 332 patients, and 278 patients were placed into the experimental group. Of those who died, 106 (17%) had caregivers who participated in the parent study (49 control, 57 experimental). The 106 patients who died and had caregivers comprised the study sample for the current study.
Figure 1.
Participant Flow Diagram
The average age of caregivers was 57.1 years (SD = 13.4), with the majority being female and Caucasian (see Table 1). A majority of caregivers were the spouses of patients, were employed, and provided more than 20 hours per week of caregiving to the patient. No statistically significant differences existed between caregiver groups at baseline, with the exception of gender.
Table 1.
Comparison of Caregiver Demographic Variables Between Experimental and Control Group Caregivers (N = 106)
| Control (n = 49) |
Experimental (n = 57) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Variable | X̄ | SD | 95% CI | X̄ | SD | 95% CI | F | p |
| Age (years) | 58.6 | 14.5 | [54.4, 62.8] | 55.6 | 12.4 | [57.5, 59.1] | 1.1 | 0.29 |
| POMS | 15.6 | 21.1 | [8.9, 22.3] | 14.9 | 19.9 | [8.7, 21.1] | 0.002 | 0.88 |
| MOS-SS | 62.9 | 23.9 | [55.7, 70.2] | 65.9 | 21.1 | [58.8, 71.9] | 0.4 | 0.53 |
| FAMCARE | 77.8 | 20.1 | [71.1, 84.4] | 81.4 | 12.5 | [77.6, 85.2] | 1 | 0.33 |
| Variable | n | n | χ 2 | p |
|---|---|---|---|---|
| Gender | 9.5 | 0.002 | ||
| Female | 28 | 48 | ||
| Male | 21 | 9 | ||
| Ethnicity | ||||
| Caucasian | 44 | 48 | 0.7 | 0.39 |
| Other | 5 | 9 | ||
| Relationship to patient | 2.9 | 0.23 | ||
| Spouse | 37 | 36 | ||
| Child | 7 | 10 | ||
| Other | 3 | 9 | ||
| Missing data | 2 | 2 | ||
| Married | 42 | 45 | 0.8 | 0.37 |
| Employed | 20 | 35 | 2.5 | 0.11 |
| Lived with patient | 40 | 41 | 1.3 | 0.25 |
| Greater than 20 hours per week of caregiving | 22 | 26 | 0.1 | 0.8 |
CI—confidence interval; FAMCARE—Family Satisfaction With End-of-Life Care; MOS-SS—Medical Outcomes Study-Social Support Survey; POMS—Profile of Mood States
The average age of patients was 62.9 years (SD = 10.6) with a slight majority being female and a larger majority being Caucasian. Almost three-quarters of the patients had stage IV cancer, including GI, lung, and GYN. At study enrollment, most had an ECOG status of 0 or 1 as well as a living will and durable power of attorney. A majority of patients died in hospice service, and very few died in a hospital setting. Participants in the intervention group were more likely to have lung cancer (p = 0.02) and have a living will (p = 0.03) when compared to the control group (see Table 2).
Table 2.
Comparison of Patient Demographic Variables Between Experimental and Control Group Patients (N = 106)
| Control (n = 49) |
Experimental (n = 57) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Variable | X̄ | SD | 95% CI | X̄ | SD | 95% CI | F | p |
| Age (years) | 63 | 9 | [60.4, 65.6] | 62.7 | 11.8 | [59.7, 65.9] | 0.1 | 0.91 |
| CCI | 0.5 | 1 | [0.2, 0.8] | 0.8 | 1.2 | [0.5, 1.1] | 1.3 | 0.26 |
| FACT-G | 73.6 | 18.3 | [68, 79.2] | 74.6 | 14.7 | [70.4, 78.8] | 0.9 | 0.77 |
| MOS-SS | 75.6 | 12.8 | [71.7, 79.5] | 77.4 | 10.3 | [74.4, 80.4] | 0.6 | 0.46 |
| Hospice stay (days) | 28.9 | 26.7 | [18.4, 39.5] | 40.2 | 57.7 | [22.8, 57.5] | –0.4 | 0.69 |
| Variable | n | n | χ 2 | p |
|---|---|---|---|---|
| Gender | ||||
| Female | 30 | 24 | 3.9 | 0.05 |
| Male | 19 | 33 | ||
| Ethnicity | ||||
| Caucasian | 44 | 48 | 0.7 | 0.39 |
| Other | 5 | 9 | ||
| Cancer type | ||||
| GI | 18 | 28 | ||
| Lung | 18 | 25 | ||
| GYN | 13 | 4 | ||
| Has stage IV cancer | 32 | 45 | 1.6 | 0.21 |
| Went to hospice | 34 | 51 | 2.4 | 0.12 |
| Received palliative care | 8 | 15 | 0.8 | 0.37 |
| Has living will | 20 | 35 | 5 | 0.03 |
| Has DPOA | 21 | 34 | 3.4 | 0.07 |
CCI—Charlson Comorbidity Index; CI—confidence interval; DPOA—durable power of attorney; FACT-G—Functional Assessment of Cancer Therapy-General; GI—gastrointestinal; GYN—gynecologic; MOS-SS—Medical Outcomes Study-Social Support Survey
Mood State and Social Support
To evaluate the impact of the intervention on caregivers’ mood state and sense of social support, the authors conducted multiple linear regression analyses. Controlling for variables that differed between experimental and control groups (e.g., caregiver gender) and shown to relate to mood state and social support (e.g., caregiver race) (Braun et al., 2008; Jenkins et al., 2005; Waters, 2001), the authors then added the intervention variable using coding for the analysis (control = 1, intervention = 2). The last POMS and MOS-SS interviews conducted prior to the patient's death were used as the outcome variables for the analyses. The authors did not obtain POMS and MOS-SS data eight weeks after death because the focus was satisfaction with EOL care, and the authors did not want to add additional burden by lengthening the interview. The models with covariates explained only 2.3% (p = 0.36) of the variance in mood state (POMS) and 2.5% (p = 0.3) of the variance in social support (MOS-SS). The addition of the intervention variable made nonsignificant contributions to social support and mood state.
The authors were also interested in comparing the experience of social support (MOS-SS) and mood state (POMS) over time. Because the intervention had no significant impact on social support or mood state, the authors examined changes over time with the groups combined. Controlling for caregiver gender and race, the authors conducted repeated measures ANOVA using the following time points: enrollment into study (shortly after diagnosis), three months after enrollment, and the last interview time point prior to the patient's death. Although a persistent negative trend was found over time, no significant changes existed in social support or mood state.
Satisfaction With End-of-Life Care
The authors also examined the impact of the intervention on the caregiver's satisfaction with EOL care. Multiple linear regression was used with the FAMCARE 13-item total score as well as the 13 individual item scores considered to be outcome variables. Controlling for caregiver gender and race, the authors added the intervention variable. The addition of the intervention variable made a statistically significant difference for 6 of the 13 individual satisfaction item scores (i.e., pain relief, information about managing pain, speed in treating symptoms, information about side effects, coordination of care, and satisfaction with overall care the last week of life) (see Table 3). However, the overall model with gender, race, and group included was only statistically significant for four variables (i.e., pain relief, speed in treating symptoms, information regarding side effects, and overall satisfaction). In all analyses, higher satisfaction was associated with the intervention group.
Table 3.
Statistically Significant Variables From FAMCARE
| Gender |
Race |
Group |
|
|---|---|---|---|
| FAMCARE Variable | p | p | p |
| Pain relief | 0.01 | 0.43 | 0.01 |
| Information on managing pain | 0.09 | 0.21 | 0.02 |
| Speed in treating symptoms | 0.01 | 0.68 | 0.036 |
| Information on side effects | 0.002 | 0.08 | 0.003 |
| Coordination of care | 0.21 | 0.26 | 0.02 |
| Overall care in last week of life | 0.03 | 0.15 | 0.03 |
FAMCARE—Family Satisfaction With End-of-Life Care
Discussion
The purpose of this study was to assess the impact of a CST on psychological, social support, and satisfaction outcomes for caregivers of patients with advanced cancer who died. Although a greater percentage of caregivers in the intervention group were women when compared to the control group, the authors found that when the effects of gender and race were controlled, no significant differences were found in any of the psychological or social support outcomes. However, when examining individual satisfaction FAMCARE items, six areas were identified where satisfaction was greater for those in the intervention versus control group after controlling for gender and race. Four of those six areas (i.e., pain relief, information about pain relief, speed of treating symptoms, and information related to side effects) fall into key areas identified as important to caregivers at EOL, particularly the need for pain and symptom management.
The focus of the intervention was to provide early and consistent involvement in symptom management, advanced care planning, and support from the first through the last visit. Given the unique needs of caregivers who are providing EOL care for a loved one, the intervention had the greatest impact on tangible aspects of EOL care (e.g., symptoms, pain relief) that seem to be most related to overall satisfaction. Those in the intervention group were more satisfied with EOL care, but a similar impact on mood state and perceived sense of social support was not found.
Although others have reported significant relationships between social support and depression and satisfaction among caregivers (Haley et al., 2003; Steinhauser et al., 2000; Teno et al., 2001), the authors of the current article found no such relationships. However, caregivers in the intervention group reported higher overall satisfaction with EOL care than those in the control group. Intervention and control group patients and families were cared for by the same physicians, had similar rates of hospice referral, and had similar hospice stays. The finding that the intervention did not significantly increase hospice referral rates is likely related to the very high use of hospice for all patients at EOL at the study site. As reported in the Dartmouth Atlas Report of EOL cancer care, this cancer center averaged an overall referral rate of 71% for all patients with cancer who died from 2003–2007, compared to 62% at comparable cancer centers in Ohio (Goodman et al., 2010). Hospice use at the study site has continued to increase in the intervening years, and the authors were not surprised that all patients in the study sample with known terminal prognoses were routinely referred to hospice without the intervention of the study team.
Because almost all patients in both groups had access to the skilled care of hospice providers in the last two weeks of life, the authors hypothesized that the greater satisfaction with EOL care that was seen in the intervention group was a function of the assessment of caregiver needs and provision of support early and systematically throughout the trajectory of care. As has been well documented, many healthcare providers wait until later in the patient's illness until any attention or support is given to the caregiver (Teno et al., 2001). However, early and consistent assessment and support, even before the caregiver identifies a need, can result in greater caregiver satisfaction with EOL care.
The authors were not able to demonstrate the significant relationship between satisfaction with EOL care and mood state or social support that others have reported (Haley et al., 2003; Teno et al., 2001). A persistent negative trend was found over time in perceived social support and poor mood state, both of which are evident as early as three months postdiagnosis. Because of the relatively short period of time from advanced cancer diagnosis to death, healthcare providers should tend to the support and mood state needs of caregivers in as timely a manner as possible. These caregivers are unique, and more work is needed to gain the necessary insight into the mechanisms that lead to greater satisfaction, social support, and mood state.
Limitations
Several limitations existed in this study. The sample of caregivers represented only half of all possible caregivers. Of the 214 patients who died, only 106 (50%) had a caregiver who participated in the study. Of those, 79 caregivers completed the postdeath interviews. Although selection bias must be taken into account, the impact of such bias on the representative nature of the caregiver sample was not large. The authors compared characteristics of caregivers in the current analysis to those not included in the analysis and found no significant differences in any variables. When comparing patient characteristics, the authors found significant differences in variables that primarily reflected the severity of illness (e.g., FACT-G, stage IV, social support), which were not unexpected because the participants included in the analysis died. Of note, significant differences existed between patients, but not caregivers, based on gender and race, with a larger percentage of those in the analysis being Caucasian but not female, when compared to those who were not included in the analysis. That may reflect the differences, which were not significant, in GYN cancer between the two groups. The study design also had an additional threat because of the potential for history to have an impact, particularly because the control and experimental participants were not enrolled concurrently. To evaluate the potential impact of history, the authors conducted interviews with key personnel in the hospital (e.g., administrators, clinicians) over the study period to track significant events or changes in practice or education that may have affected study results. No issues were identified, but the authors recognize the possibility of history as a potential confounding factor. The power of the test statistics for significant models for FAMCARE items ranged from 0.14–0.72. The study is underpowered and, given the relatively small effect sizes associated with significant models, an estimated sample size of 100–150 would be needed to yield power estimates of at least 0.8 for the analyses with larger effect sizes (Faul, Erdfelder, Buchner, & Lang, 2009; Cohen, 1988). Because of the low power, the probability of not identifying statistically significant relationships is quite high. Therefore, replication with a larger sample size may yield additional significant relationships.
Despite those limitations, caregivers who received early and ongoing assessment of their needs for support reported higher satisfaction and social support scores than those who did not receive the intervention. Although effect sizes for significant results ranged from small to medium, the trend was consistent, indicating a positive impact of the intervention on caregiver satisfaction with EOL care of their loved one and a sense of enhanced social support.
Implications for Nursing
The focus of care in cancer centers should be on the patient, but caregivers also need attention. Unless assessment and inclusion of family caregivers is systematized as part of care routines, as was done by the CST in the current study, opportunities to address caregiver needs will likely be missed. One of the most important practice implications stemming from this study is the value of performing brief but focused assessment of caregiver status early in the care-planning process and periodically throughout care. The pattern documented in the current article of increasing mood disturbance and decreasing social support identified an important target for nursing intervention.
Although the emotional impact of an impending loss of a family member may not change with the provision of social support, perception that one's loved one was well cared for in the final stages of life may have long-range benefits through the grieving process. Additional work must be conducted if healthcare providers are to continue to find effective ways to provide meaningful support for caregivers, support that is not only helpful through the final stages of their loved ones life but in the grief and recovery process, as well.
Knowledge Translation.
The assessment of caregiver needs and the provision of care-giver support early and throughout the trajectory of patient care contributed to increased caregiver satisfaction with endof-life (EOL) care.
Meeting with caregivers early in the provision of the care process and giving them information and support yielded significant and high caregiver satisfaction regarding EOL pain and symptom management.
The intervention, which involved meetings with caregivers and patients, had its greatest impact on caregiver satisfaction with tangible aspects of EOL care.
Acknowledgments
This study was funded, in part, by a grant from the National Institute of Nursing Research and the National Cancer Institute (No. NR018717).
References
- American Cancer Society . What you need to know as a cancer caregiver. Author; Atlanta, GA: 2014. [Google Scholar]
- Aoun S, Bird S, Kristjanson LJ, Currow D. Reliability testing of the FAMCARE-2 scale: Measuring family carer satisfaction with palliative care. Palliative Medicine. 2010;24:674–81. doi: 10.1177/0269216310373166. doi:10.1177/0269216310373166. [DOI] [PubMed] [Google Scholar]
- Braun UK, Beyth RJ, Ford ME, McCullough LB. Voices of African American, Caucasian, and Hispanic surrogates on the burdens of end-of-life decision making. Journal of General Internal Medicine. 2008;23:267–74. doi: 10.1007/s11606-007-0487-7. doi:10.1007/s11606-007-0487-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cameron JI, Franche RL, Cheung AM, Stewart DE. Lifestyle interference and emotional distress in family caregivers of advanced cancer patients. Cancer. 2002;94:521–527. doi: 10.1002/cncr.10212. doi:10.1002/cncr.10212. [DOI] [PubMed] [Google Scholar]
- Cella DF, Bonomi AE, Lloyd SR, Tulsky DS, Kaplan E, Bonomi P. Reliability and validity of the Functional Assessment of Cancer Therapy-Lung (FACT-L) quality of life instrument. Lung Cancer. 1995;12:199–220. doi: 10.1016/0169-5002(95)00450-f. doi:10.1016/0169-5002(95)00450-F. [DOI] [PubMed] [Google Scholar]
- Chaudhry S, Jin L, Meltzer D. Use of a self-report-generated Charlson Comorbidity Index for predicting mortality. Medical Care. 2005;43:607–615. doi: 10.1097/01.mlr.0000163658.65008.ec. doi:10.1097/01.mlr.0000163658.65008.ec. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Routledge; New York, NY: 1988. [Google Scholar]
- Daly BJ, Douglas SL, Gunzler D, Lipson AR. Clinical trial of a supportive care team for patients with advanced cancer. Journal of Pain and Symptom Management. 2013;46:775–784. doi: 10.1016/j.jpainsymman.2012.12.008. doi:10.1016/j.jpainsymman.2012.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daly BJ, Douglas SL, O'Toole E, Gordon NH, Hejal R, Peerless J, Hickman R. Effectiveness trial of an intensive communication structure for families of long-stay ICU patients. Chest. 2010;138:1340–1348. doi: 10.1378/chest.10-0292. doi:10.1378/chest.10-0292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donabedian A. The quality of care. How can it be assessed? JAMA. 1988;260:1743–1748. doi: 10.1001/jama.260.12.1743. [DOI] [PubMed] [Google Scholar]
- Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analysis using G*Power 3.1: Tests for correlation and regression analyses. Behavior Research Methods. 2009;41:1149–1160. doi: 10.3758/BRM.41.4.1149. [DOI] [PubMed] [Google Scholar]
- Glajchen M. The emerging role and needs of family caregivers in cancer care. Journal of Supportive Oncology. 2004;2:145–155. [PubMed] [Google Scholar]
- Goodman DC, Fisher ES, Chang C, Morden NE, Jacobson JO, Murray K, Miesfeldt S. Quality of end-of-life cancer care for Medicare beneficiaries: A report of the Dartmouth Atlas Project. 2010 Retrieved from http://bit.ly/1nxTBKS. [PubMed]
- Haley WE, LaMonde LA, Han B, Burton AM, Schonwetter R. Predictors of depression and life satisfaction among spousal caregivers in hospice: Application of a stress process model. Journal of Palliative Medicine. 2003;6:215–224. doi: 10.1089/109662103764978461. doi:10.1089/109662103764978461. [DOI] [PubMed] [Google Scholar]
- Jenkins C, Lapelle N, Zapka JG, Kurent JE. End-of-life care and African Americans: Voices from the community. Journal of Palliative Medicine. 2005;8:585–592. doi: 10.1089/jpm.2005.8.585. doi:10.1089/jpm.2005.8.585. [DOI] [PubMed] [Google Scholar]
- Kim Y, Given BA. Quality of life of family caregivers of cancer survivors: Across the trajectory of illness. Cancer. 2008;112(Suppl.):2556–2568. doi: 10.1002/cncr.23449. doi:10.1002/cncr.23449. [DOI] [PubMed] [Google Scholar]
- Mahmud WM, Awang A, Mohamed MN. Psychometric evaluation of the Medical Outcome Study (MOS) social support survey among Malay postpartum women in Kedah, north west of Peninsular Malaysia. Malaysian Journal of Medical Sciences. 2004;11:26–33. [PMC free article] [PubMed] [Google Scholar]
- McNair DM, Lorr M, Droppleman LF. Manual for the Profile of Mood States. Educational and Industrial Testing Services; San Diego, CA: 1971. [Google Scholar]
- Mulrow CD, Gerety MB, Cornell JE, Lawrence VA, Kanten DN. The relationship between disease and function and perceived health in very frail elders. Journal of the American Geriatrics Society. 1994;42:374–380. doi: 10.1111/j.1532-5415.1994.tb07484.x. [DOI] [PubMed] [Google Scholar]
- National Cancer Institute Coping with cancer: Supportive and Palliative Care for caregivers, family, and friends. 2014 Retrieved from http://www.cancer.gov/cancertopics/coping/familyfriends.
- Northouse L. Helping families of patients with cancer. Oncology Nursing Forum. 2005;32:743–750. doi: 10.1188/05.onf.743-750. doi:10.1188/12.ONF.500–506. [DOI] [PubMed] [Google Scholar]
- Northouse LL, Katapodi MC, Song L, Zhang L, Mood DW. Interventions with family caregivers of cancer patients: Meta-analysis of randomized trials. CA: A Cancer Journal for Clinicians. 2010;60:317–339. doi: 10.3322/caac.20081. doi:10.3322/caac.20081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schipper H, Clinch J, McMurray A, Levitt M. Measuring the quality of life of cancer patients: The Functional Living Index-Cancer: Development and validation. Journal of Clinical Oncology. 1984;2:472–483. doi: 10.1200/JCO.1984.2.5.472. [DOI] [PubMed] [Google Scholar]
- Steinhauser KE, Christakis NA, Clipp EC, McNeilly M, McIntyre L, Tulsky JA. Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA. 2000;284:2476–2482. doi: 10.1001/jama.284.19.2476. doi:10.1001/jama.284.19.2476. [DOI] [PubMed] [Google Scholar]
- Teno JM, Casey VA, Welch LC, Edgman-Levitan S. Patient-focused, family-centered end-of-life medical care: Views of the guidelines and bereaved family members. Journal of Pain and Symptom Management. 2001;22:738–751. doi: 10.1016/s0885-3924(01)00335-9. doi:10.1016/S0885-3924(01)00335-9. [DOI] [PubMed] [Google Scholar]
- Waters CM. Understanding and supporting African Americans’ perspectives of end-of-life care planning and decision making. Qualitative Health Research. 2001;11:385–398. doi: 10.1177/104973201129119172. doi:10.1177/10497320112 9119172. [DOI] [PubMed] [Google Scholar]