Abstract
Endoscopically placed biliary stents are a well-established procedure for the treatment of benign and malignant causes of obstructive jaundice. A plastic stent is usually inserted in patients with obstructive jaundice due to pancreatic cancer as a short-term procedure. Stent migration has been reported as a complication, although in most cases the stent will pass through or remain in the bowel lumen for a period of time. In rare cases, the stent may cause sigmoid perforation and pelvic abscess formation, especially in patients with sigmoid diverticulae or abdominal adhesions due to previous surgery. We present a patient with sigmoid perforation and pelvic abscess due to distal migration of a biliary stent placed to decompress a pancreatic head carcinoma.
Background
This is a rare case with important learning points for healthcare staff.
Case presentation
A man presented to the A&E department in shock, with blood pressure of 60/40; he was cold, clammy and sweating, and had a temperature of 36.2°C. His abdomen showed signs of generalised peritonitis. He exhibited guarding and tenderness all over his abdomen and was most tender in the left iliac fossa. After resuscitation with IV fluids, he produced 100 mL of dark urine. Fourteen months prior to this presentation, he had been diagnosed with advanced carcinoma of the head of pancreas with liver metastases and, following endoscopic insertion of a plastic biliary stent as short-term management, had received palliative chemotherapy. He required insertion of a second stent 10 months later due to stent migration, demonstrated on CT scan. A follow-up endoscopic retrograde cholangiopancreatography 6 months following stent replacement, 4 weeks prior to this presentation, however, failed to demonstrate a stent in the common bile duct. No further investigations were undertaken at that point. Three days before his presentation to A&E, the patient reported abdominal pain and constipation, and was given laxative treatment by his oncologist. No further investigations were performed on the patient by the oncology team.
On admission, the patient’s white cell count was 15.6×103/mL, his C reactive protein level was 99 mg/L and his liver function tests were deranged. There was no evidence of perforation on the erect chest radiograph, but CT of the abdomen demonstrated perforation of the sigmoid colon with an associated pelvic abscess (figure 1). The patient was treated by surgical resection of the perforated sigmoid and Hartman’s procedure was performed after drainage of the abscess cavity and extensive washing out of the peritoneal cavity with warm saline (figure 2). Intraoperatively, there was some reactive peritoneal fluid (suppurative in the pelvis and around the sigmoid, with pelvic abscess and adhesions between small bowel and sigmoid). The stent perforated the sigmoid through a diverticulum in the lateral aspect. A laparoscopy was not performed because of extensive pelvic inflammatory adhesions and primary repair was not an option because of the contamination. The patient spent 5 days in intensive treatment unit and then deteriorated and died due to multiorgan failure.
Figure 1.
Axial CT image showing stent penetrating the sigmoid colon with a surrounding inflammatory collection.
Figure 2.
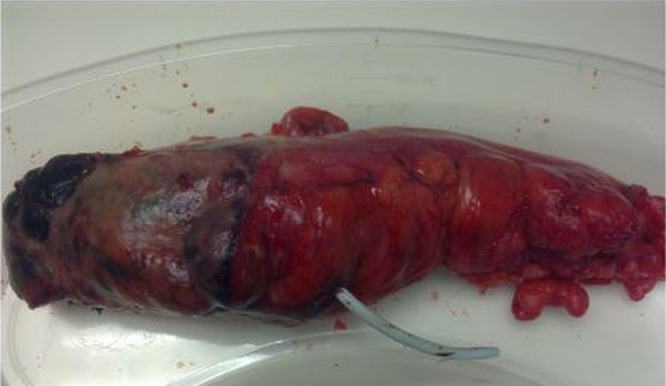
Resection specimen of sigmoid colon with perforating biliary stent.
Discussion
Endoscopic placement of biliary stents for benign and malignant disease was first described in 1980 by Soehendra and Reynder-Frederix, and is a well-established and effective procedure.1 2 Endoscopic biliary drainage for the palliation of malignant common bile duct obstruction is effective in greater than 80% of cases and has lower associated morbidity than surgery.3 4
Dislocation and migration of biliary stents proximally and distally in the gastrointestinal tract is uncommon (6%), and generally cause no major problems. Displaced stents usually pass in the faeces or remain in the bowel, with no overt symptoms.1 2 5 Migration is more common with plastic stents than with metallic stents.6 Endoscopic retrieval is often possible and surgical intervention is rarely necessary.7 8 The most common site of stent migration and associated complications is the duodenum, due to its proximity to the biliary tree and the retroperitoneal fixation of this intestinal segment. Complications in the rest of the small intestine or the colon are rare.9–11
Several complications of stent migration have been reported and can be classified into three categories as penetration, intestinal perforation and obstruction. Other organs are usually unaffected.7 8 Most foreign bodies pass through the intestine without major problems and neither the size nor the shape of the stent predicts the likelihood of successful conservative management. Patients with diverticular disease, hernia or intra-abdominal adhesions, however, are at higher risk of stent-related problems, as intestinal wall thickness and increased resistance during bowel movement can produce localised complications.12 13
Penetration requires adherence between the perforated organs, and does not induce intra-abdominal contamination, but eventually causes fistulae (ie, enteroenteric or biliocolic,14 colovaginal15 or colovesical).16 Stent migration has been associated with benign strictures and ampullary stenosis, while proximal stent migration has been associated with malignant strictures.5
In case of intestinal perforation, surgical stent removal and drainage of the consequential intra-abdominal or retroperitoneal abscess is mandatory. A pelvic abscess and colovesical or colocutaneous fistula are typical consequences.11 A case of necrotising fasciitis due to colonic perforation has also been reported.17 A recent review of the literature includes 11 cases of colonic perforation due to biliary stent migration with straight plastic endoprostheses.11
Learning points.
Endoscopic insertion of biliary stents is a good procedure for short-term and long-term decompression of the biliary system. Stent migration is a rare but important complication, as it may result in life-threatening conditions, particularly in patients with comorbid intestinal pathologies such as herniae, diverticular disease or abdominal adhesions, who are at increased risk of intestinal perforation. R Diller recommended that a migrated biliary stent should be removed immediately irrespective of whether it is symptomatic.18
Stent migration is an important differential diagnosis in any patient with a biliary stent presenting with abdominal pain or sepsis. Plain abdominal radiographs should be routinely performed if stent migration is suspected and as a follow-up tool.
The European Society of Gastrointestinal Endoscopy (ESGE) guidelines for the indications and choice of biliary stent should also be followed. Plastic stents must not be used as long-term management for biliary obstruction.
Footnotes
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Soehendra N, Reynders-Frederix V. Palliative bile duct drainage: a new endoscopic method of introducing a transpapillary drain. Endoscopy 1980;12:8–11. 10.1055/s-2007-1021702 [DOI] [PubMed] [Google Scholar]
- 2.Konstantinidis C, Varsos P, Kympouris S et al. Migrated biliary plastic stent causing double sigmoid colon perforation. J Surg Case Rep 2014;2014:pii: rju134 10.1093/jscr/rju134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dumonceau J-M, Tringali A, Blero D et al. , European Society of Gastrointestinal Endoscopy. Biliary stenting: indications, choice of stents and results: European Society of Gastrointestinal Endoscopy (ESGE) clinical guideline. Endoscopy 2012;44:277–98. 10.1055/s-0031-1291633 [DOI] [PubMed] [Google Scholar]
- 4.Jafferbhoy SF, Scriven P, Bannister J et al. Endoscopic management of migrated biliary stent causing sigmoid perforation. BMJ Case Rep 2011;2011:pii: bcr0420114078 10.1136/bcr.04.2011.4078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Akimboye F, Lloyd T, Hobson S et al. Migration of endoscopic biliary stent and small bowel perforation within an incisional hernia. Surg Laparosc Endosc Percutan Tech 2006;16:39–40. 10.1097/01.sle.0000202198.74569.5a [DOI] [PubMed] [Google Scholar]
- 6.Arhan M, Odemis B, Parlak E et al. Migration of biliary plastic stents: experience of a tertiary center. Surg Endosc. 2009;23:769–75. 10.1007/s00464-008-0067-x [DOI] [PubMed] [Google Scholar]
- 7.Jendersen MB, Svendsen LB. proximal displacement of biliary stent with distal perforation and impaction in the pancreas. Endoscopy 2001;33:195 10.1055/s-2001-11920 [DOI] [PubMed] [Google Scholar]
- 8.Liebich-Bartholain L, Kleinau U, Elsbernd H et al. Biliary pneumonitis after proximal stent migration. Gastroentist Endosc 2001;54:382–4. 10.1067/mge.2001.113646 [DOI] [PubMed] [Google Scholar]
- 9.Baty V, Denis B, Bigard MA et al. Sigmoid diverticular perforation related to the migration of a polyethelene endoprosthesis. Endoscopy 1996;28:781 10.1055/s-2007-1005606 [DOI] [PubMed] [Google Scholar]
- 10.Storkson RH, Edwin B, Reiersten O et al. Gut perforation caused by biliary endoprosthesis. Endoscopy 2000;32:87–9. 10.1055/s-2000-87 [DOI] [PubMed] [Google Scholar]
- 11.Namder T, Raffel AM, Topp SA et al. Complications and treatment of migrated biliary endoprosthesis: a review of literature. World J Gasrtoentrol 2007;13:5397–9. 10.3748/wjg.v13.i40.5397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Klein U, Weiss F, Wittkugel O. Migration of a biliary Tannenbaum stent with perforation of sigmoid diverticulum. Rofo 2001;173:1057 10.1055/s-2001-18306 [DOI] [PubMed] [Google Scholar]
- 13.Ruffolo TA, Lehman GA, Sherman S et al. Biliary stent migration with colonic diverticular impaction. Gastrointest Endosc 1992;38:81–3. 10.1016/S0016-5107(92)70342-3 [DOI] [PubMed] [Google Scholar]
- 14.Fiori E, Mazzoni G, Galati G et al. Unusual breakage of a plastic biliary endoprosthesis causing an enterocuaneous fistula. Surg Endosc 2002;16:870 10.1007/s004640042021 [DOI] [PubMed] [Google Scholar]
- 15.Blacke AM, Monga N, Dunn EM. Biliary stent causing colovaginal fistula: case report. JSLS 2004;8:73–5. [PMC free article] [PubMed] [Google Scholar]
- 16.Wilhelm A, Larger C, Zoeller G et al. complex colovesical fistula: a severe complication caused by biliary stent migration. Gastrointest Endosc 2003; 57:124–6. 10.1067/mge.2003.71 [DOI] [PubMed] [Google Scholar]
- 17.Marsman JW, Hoedemaker HP. Necrotizing fasciitis: a fatal complication of migrated biliary stent. Australas Radiol 1996;40:80–3. 10.1111/j.1440-1673.1996.tb00398.x [DOI] [PubMed] [Google Scholar]
- 18.Diller R, Senninger N, Kautz G et al. stent migration necessitating surgical intervention. Surg Endosc 2003;17:1803–7. 10.1007/s00464-002-9163-5 [DOI] [PubMed] [Google Scholar]



