Abstract
Clinical studies display a wide range of herb use prevalence among racial/ethnic minorities in the United States. We searched databases indexing the literature including CINAHL, EMBASE, Global Health, CAB Abstracts, and Medline. We included studies that reported herbal medicine prevalence among ethnic minorities, African American, Hispanic, or Asian adults living in the United States. Data from 108 included studies found the prevalence of herb use by African Americans was 17 % (range 1–46 %); for Hispanics, 30 % (4–100 %); and for Asians, 30 % (2–73 %). Smaller studies were associated with higher reported herb use (p = 0.03). There was a significant difference (p = 0.01) between regional and national studies with regional studies reporting higher use. While herb usage surveys in racial/ethnic minorities show great variability, indications suggest high prevalence. More research is needed to understand herb use among ethnic/racial minorities, reasons for use, and barriers to disclosure of use to clinicians.
Keywords: Ethnic, Minority, Herb, Medicinal plant
Introduction
Herbs (also called botanicals or herbal medicine) are defined by the National Center for Complementary and Alternative Medicine (NCCAM) as a plant or plant part used for its scent, flavor, and/or therapeutic properties that are used to supplement the diet [1]. In many countries, 70–80 % of the population has used some form of complementary or alternative medicine (CAM) and herbal treatments are the most popular form [2]. Many people believe that because medicines are herbal (natural) they are safe (or carry no risk for harm). However, herbal medicines can cause harmful, adverse reactions if the herbal product is of poor quality, or it is taken inappropriately or in conjunction with other medicines [2]. Moreover, recent clinical studies have highlighted issues of herbal contamination, herbal adulteration, and misidentification of herbal products [3].
Every culture has a set of values and health traditions which is passed down from generation to generation and they have great influence on health behaviors and adherence to health care recommendations. Yet, little is known about how underserved minority groups use herbal traditions in the US and if this is related to cultural practices, regional location, native language, or lack of income (lack of access and no health insurance). Various national surveys estimate that approximately 18 % of the US population uses herbal medicine [4, 5]. In the 2002 National Health Interview Survey (NHIS), an estimated 14 % of African Americans and 17 % of Hispanics used herbal medicine [6]. The 2007 NHIS, reports biologically based therapies (non-vitamin, non-mineral, natural products) rates of 23 % for Non-Hispanic whites, 12 % for Hispanics, 12 % for Non-Hispanic blacks, and 20 % for Asians [5]. Yet, smaller and regional studies have reported rates higher herb use rates among Hispanics, African Americans and Asians [7–10]. It is unknown why there is such a large variation in herb use prevalence among studies of racial/ethnic groups in the United States.
Despite the high utilization of herbs, relatively little is known about disclosure of herb use to healthcare providers. Questions of herbal safety, efficacy, and herb-drug interactions fuel the importance of discussion of herb use. The 2002 NHIS found that disclosure of overall CAM use is low, especially among racial/ethnic minorities [11]. In addition, little is known about herbal and dietary supplement disclosure to health care providers by individuals with chronic conditions. Furthermore, there may be other factors associated with herb disclosure that may be critical for providers to know in order for them to make clinical decisions.
Our systematic review explores the factors that may account for the large variation in prevalence rates in ethnic/racial herb use by examining biomedical peer reviewed literature. We explore different herbal study characteristics, number of subjects, language of study, location of study in the United States, type of study design, types of journals publishing these studies, definition of herb use in the study, and documentation of disclosure rates of herb use. We hypothesize that small, bilingual, regional studies will report higher prevalence rates. Previous smaller studies assessing herb use in regional areas often report higher use of herbs compared to national studies. Regional studies also provide information about trends within cultural groups that may have more than one subgroup. Furthermore, we believe that bilingual studies may allow participants to explain more about their herb use in their primary language, particularly if their first language is not English. We are interested in seeing whether our collective systematic review finds similar results of individual studies.
Methods
Data Collection
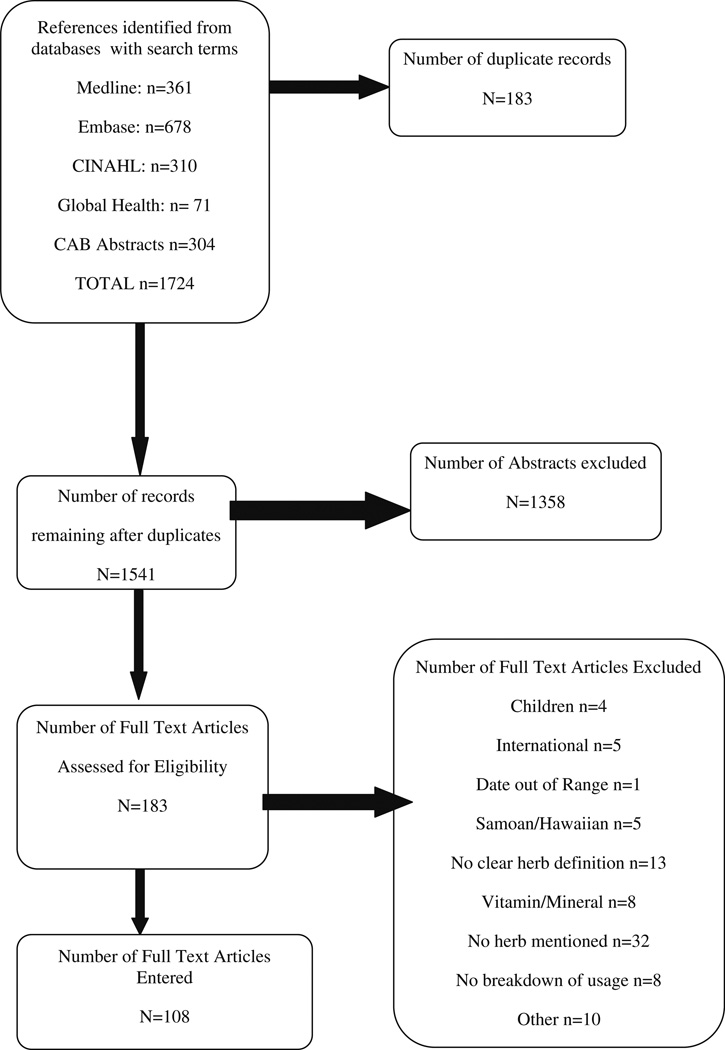
We systematically searched multiple databases including CINAHL, CAB Abstracts, EMBASE, Global Health, and Medline/PubMed (see Fig. 1). We combined the following MeSH and text word terms; dietary supplement, phytotherapy, medicinal plants, Chinese herb, herbal, ayurvedic and combined these with “african americans”[MeSH Terms] OR “Hispanic Americans”[MeSH Terms] OR “asian americans”[MeSH Terms] OR “asian continental ancestry group “[MeSH Terms] OR “american native continental ancestry group”[MeSH Terms] OR “ethnic groups”[MeSH Terms]. Search results were limited to citations published from 1998 until 2010. See Table 1 for an example of a database search in Embase. Additionally, we searched the bibliographies of obtained relevant articles for additional publications that would meet our criteria.
Fig. 1.
Search strategy
Table 1.
Search strategy in EMBASE database utilizing Embase.com interface
| Last updated 7/22/2010 Total citations downloaded 678 | |
| #1 ‘plant medicinal product’/exp OR ‘medicinal plant’/exp OR ‘herbaceous agent’/exp OR ‘herbal medicine’/exp OR ‘phytotherapy’/exp OR ‘ayurvedic drug’/exp OR ‘chinese herb’/exp OR ‘plant product’/exp |
1,033,248 |
| #2 ‘african american’/exp OR ‘asian american’/exp OR ‘american indian’/exp OR ‘native american medicine’/exp OR ‘hispanic’/exp OR (‘ethnic and racial groups’/exp AND ‘united states’/exp) |
64,844 |
| #3 #1 AND #2 | 1,769 |
| #4 #1 AND #2 AND ([adult]/lim OR [aged]/lim) AND [humans]/lim AND [english]/lim AND [1-1-1990]/sd |
762 |
| #5 ‘pregnancy’/exp | 512,837 |
| #4 NOT #5 | 740 |
| #7 #4 NOT #5 AND ([controlled clinical trial]/lim OR [randomized controlled trial]/lim) |
62 |
| #8 #6 NOT #7 | 678 |
We included surveys with subjects above the age of 18 that had publication dates between 1998 and 2010. Study design ranged from face to face interview, group interview survey delivered by interviewer, telephone interview, self-reported survey, and other. Studies were included if the prevalence of herb use among subjects was reported. Dissertations, meeting abstracts, non-English publications, and studies outside the United States were excluded. We chose to limit our searches biomedical peer reviewed literature so we could demonstrate the methodological flaws in surveys administered to patients of diverse racial and ethnic backgrounds.
Each study was extracted systematically by two authors independently (NB, PG, AF, JW). A third author (PG, JW, NB) adjudicated if there was disagreement in data extraction. Outcomes collected included: study population characteristics, size of study, definition of herb, documentation of disclosure rate of herb use, number of ethnic groups in the study, language of study (English, bilingual, or multiple languages); location of study in the United States, type of study design, reasons for herb usage, health conditions of subjects, and type of publication. Education, insurance status and income were categorized as documented or not documented.
Analysis
We primarily used descriptive statistics using (SAS™ software Version 9.1 Cary, NC: SAS Institute). Table 2 summarizes the study characteristics. Averages of herb prevalence within ethnic/minority groups were calculated by adding studies which included greater than 1 % African Americans (n = 32); Hispanics (n = 41); Asians (n = 22) and Non-Hispanic whites (n = 35); and dividing by the number of studies.
Table 2.
Characteristics of all studies compared to those with greater than 50 % ethnic group representation
| Category | All studies N = 108 (%) |
>50% African American N= 10 |
>50% Hispanic N= 19 |
>50% Asian N = 4 |
>50% Non-Hispanic White N=49 |
|---|---|---|---|---|---|
| Number racial/ethnic groups | |||||
| More than one group | 84 (78) | 7 (70) | 7 (37) | 0 | 48 (98) |
| One group | 18 (17) | 3 (30) | 12 (63) | 4 (100) | 1(2) |
| Not documented | 6(5) | ||||
| Size of study (N) | |||||
| 1–150 | 21 (19) | 4(40) | 8 (42) | 2(50) | 5(10) |
| 151–500 | 35 (32) | 4(40) | 7 (37) | 1(25) | 14 (29) |
| 501–1,000 | 10(9) | 0 | 2(11) | 1(25) | 5(10) |
| 1,001–10,000 | 23 (21) | 2(20) | 1(5) | 0 | 12 (25) |
| >10,001 | 14 (13) | 0 | 0 | 0 | 10 (20) |
| No documentation | 5(5) | 1(5) | 0 | 3(6) | |
| Language used in study | |||||
| English | 61 (56) | 9(90) | 0 | 1(25) | 35 (71) |
| Bilingual | 27 (25) | 0 | 19 (100) | 2(50) | 3(6) |
| >2 languages | 6(6) | 0 | 0 | 0 | 1(2) |
| Not documented | 14 (13) | 1(10) | 0 | 1(25) | 10 (20) |
| Location of study in the U.S. | |||||
| North East | 10(9) | 2(20) | 1(5) | 2(50) | 3(6) |
| Midwest | 13 (12) | 2(11) | 9(18) | ||
| South | 11 (10) | 4(40) | 2(11) | 4(8) | |
| West | 31 (29) | 13 (68) | 1(25) | 11 (22) | |
| National | 39 (36) | 3 (30) | 1(5) | 1(25) | 21 (43) |
| No documentation | 4(4) | 1(10) | 1(2) | ||
| Type of study design | |||||
| Primary data collection | 75 (69) | 8 (80) | 17 (89) | 3(75) | 31 (63) |
| Secondary database analysis | 32 (30) | 2(20) | 2(11) | 1(25) | 18 (37) |
| Not specified | 1(1) | ||||
| Type of publication | |||||
| Biomedical Medicine Journal | 42 (39) | 6(60) | 7 (37) | 1(25) | 22 (46) |
| CAM journal | 27 (25) | 1(10) | 4(21) | 2(50) | 10 (20) |
| Pharmacy journal | 14 (13) | 3(16) | 7(14) | ||
| Nursing journal | 7(6) | 2(20) | 3(16) | 2(4) | |
| Other* | 18 (17) | 1(10) | 2(10) | 1(25) | 8(16) |
| Definition of herb | |||||
| Herbal supplement | 32 (30) | 2(20) | 6(31) | 17 (35) | |
| Herbal medicine | 13 (12) | 3(16) | 1(25) | 4(8) | |
| Herbal remedy | 11 (10) | 3(16) | 1(25) | 5(10) | |
| Medicinal plant | 16 (15) | 2(20) | 2(11) | 8(16) | |
| Dietary supplement | 6(6) | 1(10) | 1(25) | 3(6) | |
| Biologically based product | 11 (10) | 1(10) | 6(12) | ||
| Not specified | 5(5) | 4(8) | |||
| Other** | 14 (13) | 4(40) | 5(26) | 1(25) | 2(4) |
| Documented Disclosure Rates | |||||
| 0–30 % | 10 (37) | 4(21) | 1(25) | 4(8) | |
| 31–40 % | 7(26) | 1(10) | 4(8) | ||
| >41 % | 10 (37) | 1(5) | 7(14) | ||
| Not documented | 81 | 9(90) | 14 (74) | 3(75) | 34 (69) |
| Health conditions | |||||
| Healthy/general health | 65 (60) | 5 (50) | 10 (53) | 4 (100) | 30 (61) |
| HIV | 7(6) | 4(40) | 2(11) | ||
| Diabetes | 7(6) | 5(26) | |||
| Cancer | 10(9) | 1(10) | 7(14) | ||
| Other*** | 19 (18) | 2(11) | 12 (25) | ||
| Reasons of herb use | |||||
| Overall Health Promotion | 17 (16) | 5 (50) | 3(16) | 10 (20) | |
| Treatment for an ailment | 54 (50) | 4(40) | 13 (68) | 3(75) | 20 (41) |
| Other**** | 12(11) | 1(25) | 7(14) | ||
| Not specified | 25 (23) | 1(10) | 3(16) | 12 (24) | |
| Education reported | |||||
| Yes | 95 (88) | 9(90) | 18 (95) | 4 (100) | 45 (92) |
| No | 13 (12) | 1(10) | 1(5) | 4(8) | |
| Income reported | |||||
| Yes | 69 (64) | 9(90) | 10 (53) | 2(50) | 33 (67) |
| No | 39 (36) | 1(10) | 9(47) | 2(50) | 16 (33) |
| Insurance reported | |||||
| Yes | 42 (39) | 5 (50) | 5(26) | 3(75) | 18 (37) |
| Not documented | 66 (61) | 5 (50) | 14 (74) | 1(25) | 31 (63) |
Public health journals, dental journals, and women’s health journals
Subject used own definition, CAM product, and home remedy
Glaucoma, arthritis, hypertension, depression, and menopause
Personal beliefs regarding herbs and conventional medications, and financial reasons
To assess for significant factors associated with studies with higher rates of herb use we use Chi square tests. Prevalence of herb use was categorized into four categories: prevalence of 0–20, 21–19, and >50 %, and not reported. Size of study was categorized them into less than 500 subjects and greater than 500 subjects. Language was categorized according to English or other; location of study was separated into regional or national survey. Type of publication was categorized as CAM journal or non-CAM journal.
Results
Figure 1 portrays the flow of our search and selection process. Our initial database searches resulted in a total of 1,724 studies. After removing the duplicates, we were left with 1,541 studies. Next, 1,358 were excluded based on our inclusion criteria, leaving us with a total of N = 183. We screened and excluded articles that involved children (n = 4), were international (n = 4), had a date that was out of range (n = 1), included Samoan or Hawaiian participants (n = 5), described vitamins and minerals (n = 8), did not mention an herb (n = 32), had no breakdown of usage (n = 8), and other reasons, such as dissertations (n = 2), clinical trials (n = 3), qualitative papers (n = 2), or safety papers (n = 3). We identified 108 studies that met our inclusion criteria.
Among included studies (N = 108), the prevalence of African Americans’ herb use ranged from 1 to 46 % with an average of 17.4 %. Herb use by Hispanics, ranged from 4 to 100 % with an average of 30 % and herb use by Asians ranged from 2 to 73 % with an average of 30 %. Table 2 highlights the studies with greater than 50 % representation of a particular racial/ethnic group. Eighty-four studies included more than one ethnic group. There was wide variation in study size from 19 % with 1–150 subjects, 32 % with 151–500 subjects, 9 % with 501–1,000 subjects, 21 % with 1,001–10,000 and 13 % with >10,001 subjects. Of the 33 studies with more than 50 % ethnic group representation, 26 (78 %) had samples sizes less than 500 subjects. Among all the studies, smaller studies were associated with higher reported herb use (p = 0.03).
Fifty six percent of all studies utilized English as the primary language, 27 (25 %) were bilingual (English/Spanish or English/Asian language) and 6 (6 %) studies were multilingual. There was no association between language of study and herb use (p = 0.15). All studies with more than 50 % Hispanic representation were bilingual. Eighty three percent of studies did not document the birthplace of the study subjects. Therefore, we were not able to determine if the subjects were first generation, second, or third generations living in the United States.
We categorized study location according to region: North East (9 %), Midwest (12 %), South (10 %), West (29 %), National (36 %). Four percent did not document location of study. There was a significant difference in herb use by region. Regional studies found greater herb use compared to national studies (p = 0.01). Among the predominantly African American studies (n = 10), 40 % were conducted in the South. Of the predominantly Hispanic studies (n = 19), 68 % were conducted in the West. Two of the four predominantly Asian studies were conducted in the Northeastern region of the U.S.
There were over 20 different types of definitions of “herb” described by researchers in their questions to subjects. Examples of definitions included dietary supplement, herbal remedy, botanical supplement, biologically based supplement, and medications derived from plants and herbs (see Table 2). Disclosure of herb use to a health care professional was measured in 27 (25 %) studies and only 7 of these studies occurred in predominately racial/ethnically diverse subjects. The range of disclosure rates for these studies was 7–65 % with an average of 36 %.
The reasons for herb usage were diverse but fell into: treatment for an ailment (n = 54), overall health promotion (n = 17), other (personal belief, attitudes about medications, or familial usage) (n = 12), and not specified (n = 25). Subjects in 60 % of the studies were considered generally healthy. There were few studies that look at subjects with chronic conditions (HIV related diseases, Cancer, Diabetes). When a medical condition was mentioned, participants reported using herbs to treat symptoms of menopause, cancer, arthritis, HIV related diseases, and diabetes. Eighteen studies reported who had recommended the herbs to the individuals. The most common sources were family and friends, with a few referencing a physician recommendation. Furthermore, 50 % of studies also reported other CAM (i.e. acupuncture, massage, yoga) use in their surveys.
Table 3 provides greater detail on the studies where more than 50 % of subjects were from a specific racial or ethnic minority group. Among the studies where African Americans represented more than 50 % of the subjects, 12 % (n = 4) had 99 or 100 % male subjects, while 9 % (n = 3) were 100 % female. Studies that were predominantly Hispanic had higher percentages of female subjects. Eleven of the 19 (58 %) studies had less than 40 % representation by males.
Table 3.
Studies with greater than 50 % ethnic group representation
| References | Total % of minority group |
Total sample size % male region Design of study |
Herb definition | Results |
|---|---|---|---|---|
| Studies with more than 50 % of subjects African American (AA) | ||||
| Brown et al. [21] |
100 % AA | N = 4,256 40 % male National study Interview survey |
Biologically based therapy | Prevalence of herb use = 20 % |
| Jones et al. [22] |
100 % AA | N= 14 100 % male South-Virginia Face to face interview |
Root or Folk Medicine | 36 % believed herbs helped 21 % believed herbs didn’t help 43 % unsure if herbs helped |
| Weinrich et al. [23] |
100 % AA | N= 198 100 % male South Self-report survey |
Nutritional Supplement | Prevalence of herb use = 7 % |
| Yoon et al. [9] | 100 % AA | N = 57 0 % male South-Florida Face to face interview |
Non Vitamin, Non mineral Supplements with parts of plants Herbal product |
Prevalence of herb use = 33 % Herbs described: aloe, garlic (26 %), gingko (16 %) |
| Owen-Smith et al. [24] |
85 % AA | N = 366 0 % male South-Alabama and Georgia Self-reported survey |
Herbal or Natural Immunity boosters |
Herbs described: garlic, ginseng, also included algae, mushrooms, and Chinese herbs |
| Milan et al. [25] |
69 % AA | N = 93 52 % male Northeast-New York Face to face interview |
Dietary Supplement | Herbs described: ginseng (18 %), green tea (42 %), and soy |
| Tsang et al. [8] | 56 % AA | N= 106 44 % male Northeast-Massachusetts Self-report survey |
Botanical and Herb | Prevalence of herb use = 27 % Prevalence of herb use Among African Americans = 35 % Herbs described: garlic (12 %), ginseng, gingko, St. John’s wort |
| Uzzo et al. [26] |
56 % AA | N = 333 100 % male National study Interview Survey |
Herbal Supplement | Herbs described: garlic, ginseng, gingko, saw palmetto, St. John’s wort, flaxseed, olive leaf (also included fish oil, cod liver oil, bee pollen) |
| Liu et al. [27] | 54 % AA | N = 1,745 0 % male Multiple sites—Illinois, California, Washington D.C. and New York Face to face interview |
CAM Medications | Herbs described: garlic, gingko, saw palmetto, St. John’s wort, Echinacea |
| Risa et al. [28] | 51 % AA | N= 118 99 % male National study Interview Survey |
Healing therapies involving physical consumption of oral agents |
Prevalence of herb use = 10 % Herbs described: ginseng, gingko St. John’s wort |
| Studies with more than 50 % of subjects Hispanic | ||||
| Gomez-Beloz and Chavez [29] |
100 % Hispanic |
N = 26 17 % male Midwest-Illinois Interview Survey |
Herbs-fresh or dried, not processed |
Prevalence of herb use = 100 % (subjects visited botanical store) |
| Hatcher and Whittemore [30] |
100 % Hispanic |
Unknown sample size 3 % male National Unknown study type |
Herbal treatments | Herbs described: aloe, prickly pear cactus |
| Hunt et al. [31] | 100 % Hispanic |
N = 43 Unknown % male West-Texas Face to face interview |
Treatment other than diet, exercise, and medication |
Prevalence of herb use = 9 % Herbs described: aloe (31 %), loquat leaves |
| Jernewall et al. [32] |
100 % Hispanic |
N= 152 100 % male Northeast Self-reported Survey |
Plant based CAM | Prevalence of herb use = 40 % |
| Jezewski and Poss [33] |
100 % Hispanic |
N = 22 18 % male West-Texas Face to face interview |
Herbal remedy | Herbs described: aloe, herbal tea, nopal, milkberry, trumpet tree, bricklebrush |
| Loera et al. [34] |
100 % Hispanic |
N = 2,734 43 % male West Face to face interview |
Herbs | Prevalence of herb use = 9 % Herbs described: chamomile (24 %), garlic (2 %), ginseng (2 %), peppermint (13 %), also included oregano, cinnamon, and wormwood |
| Mikhali et al. [18] |
100 % Hispanic |
N= 179 32 % male West-California Self -Report Survey |
Subject used own definition | Prevalence of herb use = 57 % Herbs described: aloe (14 %), chamomile (29 %), ginseng, peppermint (35 %), cactus, rue, cat’s claw |
| Ortiz and Clauson [35] |
100 % Hispanic |
N= 142 32 % male South-Florida Interview Survey |
Extracts and prep from raw herbs, fruit, grass |
Prevalence of herb use = 75 % Herbs described: aloe (45 %), chamomile (59 %), garlic (32 %), ginger (30 %), ginseng (26 %), valerian, also include linden, star anise |
| Poss et al. [36] | 100 % Hispanic |
N = 22 18 % male West-Texas Interview Survey |
Home remedy | Herbs described: aloe, eucalyptus, cornsilk, herbal tea, nopal |
| Rivera et al. [13] |
100 % Hispanic |
N= 115 59 % male West-Texas Face to face interview |
Herbal product | Prevalence of herb use = 62 % Herbs described: aloe (6 %), chamomile (14 %) garlic (6 %), ginseng (2 %), Echinacea (1 %), peppermint (6 %), also included lime, oregano, cinnamon, wormwood, eucalyptus |
| Rivera et al. [14] |
100 % Hispanic |
N = 474 West-Texas Face to face interview |
Herbal product | Prevalence of herb use = 71 % in HIV + patients, 79 % in non- HIV patients Herbs described: aloe (8 %), chamomile (14 %), garlic (6 %), ginger (1 %), ginseng (10 %), gingko (10 %), St. John’s wort (13 %), Echinacea (14 %), peppermint (7 %), also included cinnamon, wormwood, eucalyptus, camphor, parsley |
| Shapiro et al. [37] |
100 % Hispanic |
N = 82 24 % male West-California Self-report survey |
Something available in supplement form |
Prevalence of herb use = 78 % Herbs described: aloe, chamomile, garlic, peppermint, cascara sagrada, flaxseed |
| White et al. [38] |
100 % Hispanic |
N= 164 Unknown % male West-California Interview Survey |
Herbal tea or plant based product | Prevalence of herb use = 94 % |
| Zenk et al. [10] |
100 % Hispanic |
N = 30 0 % male Midwest-Illinois Interview Survey |
Crude drugs of vegetable origin used for treatment |
Prevalence of herb use = 47 % Herbs described: aloe (6 %), chamomile (10 %), garlic (6 %), ginseng (3 %), St. John’s wort (3 %), also included dong quai, mullein, cactus, cornsilk, anise, parsley, herbal tea |
| Rivera et al. [15] |
89% Hispanic |
N = 500 West-Texas 64 % male Face to face interview |
Herbal Product | Prevalence of herb use = 68 % Herbs described: aloe (9 %), chamomile (13 %), garlic (7 %), ginseng (2 %), gingko (2 %), Echinacea (1 %), peppermint (7 %), also included oregano, cinnamon, mullein, cactus, wormwood, eucalyptus, camphor |
| Burge and Albright [39] |
80% Hispanic |
N = 575 26 % male West-Texas Interview Survey |
Herbal Remedy | Prevalence of herb use = 24 % Herbs described: aloe, chamomile, garlic, gingko, St. John’s wort |
| Lundy et al. [40] |
75 % Hispanic |
N = 516 42 % male West-Arizona Self-report survey |
Special herbs | Prevalence of herb use among Hispanics = 35 % Prevalence of herb use among Non-Hispanic Whites in study = 25 % |
| Sleath et al. [41] |
71 % Hispanic |
N= 141 35 % male West-Texas Other study design |
Herbal or non-prescriptive medications |
Prevalence of herb use = 17 % |
| Sleath et al. [42] |
64% Hispanic |
N = 205 36 % male West-New Mexico Face to face interview |
Herbal medicine therapy | Prevalence of herb use = 16 % |
| Studies with more than 50 % of subjects Asian | ||||
| Fang and Schinke [43] |
100 % Asian |
N= 153 34 % male Northeast-New York |
Chinese herbal medicine | Prevalence of herb use = 43 % |
| Kim and Chan [44] |
100 % Asian | Self-report survey N= 143 53 % male National |
Herbal treatment | Prevalence of herb use = 62 % |
| Satow et al. [45] |
100 % Asian | Self-report survey N = 64 35 % male Northeast-New York Face to face interview |
Nutritional or herbal products | Prevalence of herb use = 59 % |
| Wade et al. [46] |
100 % Asian | N = 1,021 0 % male West-California Telephone Interview |
Medicinal herb | No prevalence reported |
Many studies asked about specific herbs. The ten herbs used most frequently asked about were garlic supplements (n = 55 studies, the subjects reported an overall prevalence range 1–65 %, average 14.4 %), ginseng (n = 52, prevalence range 1–34 %, average 11.3 %), gingko biloba (n = 43 prevalence range 1–44 %, average 12.4 %), St. John’s wort (n = 39, prevalence range 1–37 %, average 8.5 %), Echinacea (n = 32, prevalence range 1–70 %, average 17.5 %), chamomile (n = 25, prevalence range 1–59 %, average 18.2 %), aloe (n = 24, prevalence range 1–55 %, average 22.3 %), ginger supplements (n = 22, prevalence range 1–34 %, average 9.7 %), saw palmetto (n = 21, prevalence range 1–20 %, average 5.5 %), and peppermint (n = 18, prevalence range 1–35 %, average 10.8 %).
There were regional and ethnic/racial differences found in the types of herbs reported. Studies that had predominantly Hispanic subjects reported using lime, oregano, cinnamon, cactus, wormwood, cascara sagrada, and corn-silk. African American studies reported using soy, flax seed, herbal tea, eucalyptus, and cod liver oil. Study subjects also reported using black cohosh, green tea, dong quai, evening primrose, eucalyptus, licorice, milk thistle, comfrey, parsley, camphor, fever few, hawthorne, mullen, anise, yohimbe, sage, and witch hazel. These herbs were either asked about or used much less frequently than the ten herbs listed above.
Discussion
There are mixed reports in the literature of the prevalence of herb use among racial/ethnic minorities in the United States. This is the first systematic review to explore factors associated with the specific herbs used and their prevalence among various ethnic/racial minorities. The 2007 NHIS, reports “natural products” rates of 12 % for Hispanics, 12 % for African Americans, and 20 % for Asians [5]. We reported similar average rates for African Americans (17 %) but higher rates in Hispanics studies (30 %) and Asians studies (30 %). As we hypothesized, smaller sample size and study location had a significant influence on the rate of herb use among racial/ethnic minorities. Compared to non-Hispanic white subjects, ethnic minorities have lower rates of disclosure to health care providers [11]. Finally, the reasons for herb usage included: treatment for an ailment, overall health promotion and personal belief, attitudes about medications, or familial usage. However, the majority of these studies have been done in healthy adults, leaving a gap in the literature in herb use in chronically ill ethnic/minorities.
Our purpose was to search biomedical literature to note the variability in reported prevalences of herb use among ethnic minorities. We concluded that many studies report results using census bureau categories for race and ethnicity thus losing cultural subgroups depending on how the survey was administered. Some larger studies use national samples but provided less detail about herbs use. Smaller studies provide more qualitative data but are limited in their generalizability.
Sample size is one variable that was highly predictive of ethnic representation. The 2002 and 2007 NHIS, administered also in Spanish had an overrepresentation of African Americans and Hispanics in the sample. These surveys focused more on the popular, top selling herbs and asked less about culturally influenced herbs. It can be difficult to obtain herb use information from under-represented populations in national studies since there is such diversity in language of participants (i.e. Asian languages) and diversity in the use of traditional medicine such as herbal medicine that exist within larger communities.
The smaller studies with greater ethnic representation typically had less than 500 subjects and many had less than 50 subjects. The smaller studies often gave specific information about herbs used, sometimes providing specifics about how subjects obtained the herbs and/or prepared the herbs. While these small studies were culturally rich and provided valuable qualitative insight into herb use trends, their small sample size limits external generalizability.
Little is known about how low health literacy, immigration and acculturation affect herb use. Interestingly, self-report of herb use can be influenced by the language and birthplace of subjects. Su et al. [12] studied the acculturation of recent immigrants and the use of CAM. Reported rates of CAM use, including herb use by recent immigrants can be influenced by length of stay in the United States and language of survey. Only 17 % of studies documented birthplace of study subjects, therefore we are unable to assess how long study subjects have been in and whether there are any changes in herb use following entrance into the United States.
Prevalence of herb use is heavily influenced by geographic location, particularly for areas near Mexico [13–15]. Herbal use may be influenced by ethnic groups in a particular region. Regional studies reported higher percentages of herb use compared with the national studies. Health professionals in regions where herb use is common must be particularly vigilant in inquiring about herb use prior to procedures and before prescribing medications that might interact with herbal remedies.
In the United States, many different terms and phrases are used to describe plant based medicine (e.g., herbal medicine, herb, medicinal plant, dietary supplement). In our review we recorded over 20 different phrases used to ask subjects about herb use, categorizing them into 8 categories. The definition and term used is important when inquiring about herbal use as subjects may use different terms depending on their culture, level of health literacy, and regional colloquialisms. In order to gain a comprehensive perspective of herb use in the U.S., studies need to use appropriate and understandable definitions of “plant based medicine” which are understandable to participants from all cultures.
Although we hypothesized that bilingual studies would report higher herb use, in our review we found that among all surveys, there was no association between language of survey and higher reported herb use (p = 0.15). Thus, more research is needed to determine the qualities of an herbal prevalence study that make it understandable and appropriate for the subject to correctly answer. Understanding culturally appropriate definitions of herb use would decrease measurement error in herb use recall studies.
Importantly, we found significant ethnic variations in herb use disclosure rates. Hispanic and Asian Americans are much less likely to disclose their herb use [6, 16–18]. Our findings are particularly striking given that the survey respondents participated in English or Spanish. As has been mentioned in previous work [11], we suspect that more vulnerable members of these communities, including those with limited English proficiency or recent immigrants, may be even less likely to discuss herb use with their health care providers. New immigrants face multiple barriers to receiving adequate healthcare—including cost, communication, and insurance—which may result in medical encounters that do not facilitate disclosure of herb use [19].
Reasons for herb use varied widely, with some studies describing herb use for a particular ailment or to prevent a specific disease, and others revealing that subjects took herbs because of personal beliefs. Many individuals took herbs to relieve symptoms of conditions such as cancer, menopause, diabetes, arthritis, and HIV related diseases. The diversity in the medical issues of study participants demonstrates that practitioners of all disciplines and health care fields can consider herbs for their patients.
There are several limitations to our study. First, we did not include anthropological literature as we wanted to examine peer reviewed biomedical literature to highlight the limitations of surveys often administered to patients of diverse racial and ethnic backgrounds. Research on this topic is growing, however. While we did not include anthropological databases in the search strategy and only included the continental U.S, and excluded U.S. territories (e.g. Puerto Rico, U.S. Virgin Islands), in the last 4 years, 54 studies were published using our search strategy. Another limitation is the lack of distinction of each unique culture. For example many studies aggregated racial and ethnic groups such as Hispanics and did not look at individual groups such Mexican-Americans and Puerto Ricans living in the United States. We are reporting the variation in reported prevalence of herb use as well as highlighting the need to define herbs in culturally relevant terms when surveying or reporting herb use among a population. We hope to influence large, national survey designers to take into account the variation in cultural groups.
The prevalence data reveals great variation in reported herb use. There are thousands of medicinal plants used by various cultures and healing traditions in the United States. We report on a trend where smaller regional studies asked about more specific questions about culturally specific plants. Larger studies asked more about top selling and popular trends in herbal medicine that are more likely to be use by Non-Hispanic whites. Future research is needed to examine both biomedical and anthropological literature for studies on herb use among individual cultural subgroups.
In conclusion, there remain gaps in the literature about herb use among ethnic minorities in the United States. The individual, smaller sample studies are helpful in characterizing a regional ethnic group. National surveys have the power of large sample size and randomization but must be mindful of cultural differences in herb use and issues unique to underserved subjects (chronic illness, lack of access to health care, low health literacy, and health care disparities). In order to reach the most diverse sample of people, questions must reflect specific herbs that are prevalent in all cultural subpopulations.
Finally, lack of herb use disclosure to providers, particularly for self-care practices among minority populations, represents a serious challenge in medical encounter communications. Efforts to improve disclosure of herb use should be aimed at improving patient-physician communication across racial/ethnic groups. [20].
Clinicians are urged to ask about patients’ herb use and to offer evidence-based guidance about the risks and benefits of such therapies. It is necessary for clinicians to understand the prevalence of herb use in the US when caring for all patients as there can be great variation from patient to patient.
Contributor Information
Paula Gardiner, Email: paula.gardiner@bmc.org, Department of Family Medicine, Boston Medical Center, 1 Boston Medical Center Place, Dowling 5 South, Boston, MA, 02118, USA.
Julia Whelan, Countway Library of Medicine, Harvard Medical School, Boston, MA, USA.
Laura F. White, Department of Bio statistics, Boston University School of Public, Health, Boston, MA, USA
Amanda C. Filippelli, Department of Family Medicine, Boston Medical Center, 1 Boston Medical Center Place, Dowling 5 South, Boston, MA, 02118, USA
Nazleen Bharmal, Department of Medicine, University of California Los Angeles, Los Angeles, CA, USA.
Ted J. Kaptchuk, Division of General Medicine and Primary Care, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA, USA
References
- 1.National Center for Complementary and Alternative Medicine. Herbs at a Glance. 2010:2011. [Google Scholar]
- 2.World Health Organization. Traditional Medicine. 2008:2011. [Google Scholar]
- 3.Saper RB, Kales SN, Paquin J, Burns MJ, Eisenberg DM, Davis RB, Phillips RS. Heavy metal content of ayurvedic herbal medicine products. JAMA. 2004;292:2868–2873. doi: 10.1001/jama.292.23.2868. [DOI] [PubMed] [Google Scholar]
- 4.Gardiner P, Graham R, Legedza AT, Ahn AC, Eisenberg DM, Phillips RS. Factors associated with herbal therapy use by adults in the United States. Altern Ther Health Med. 2007;13:22–29. [PubMed] [Google Scholar]
- 5.Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Rep. 2008;12:1–23. [PubMed] [Google Scholar]
- 6.Graham RE, Ahn AC, Davis RB, O’Connor BB, Eisenberg DM, Phillips RS. Use of complementary and alternative medical therapies among racial and ethnic minority adults: results from the 2002 National Health Interview Survey. J Natl Med Assoc. 2005;97:535–545. [PMC free article] [PubMed] [Google Scholar]
- 7.Tam KK, Gadbury-Amyot CC, Cobb CM, Williams KB. Differences between herbal and nonherbal users in dental practice. J DentHyg. 2006;80:10. [PubMed] [Google Scholar]
- 8.Tsang S, Pycz L, Herbold N. Dietary supplement use among physically active multiethnic adults. Top Clin Nutr. 2007;22:246–257. [Google Scholar]
- 9.Yoon SL, Home CH, Adams C. Herbal product use by African American older women. Clin Nurs Res. 2004;13:271–288. doi: 10.1177/1054773804267877. [DOI] [PubMed] [Google Scholar]
- 10.Zenk SN, Shaver JL, Peragallo N, Fox P, Chavez N. Use of herbal therapies among midlife Mexican women. Health Care Women Int. 2001;22:585–597. doi: 10.1080/07399330127197. [DOI] [PubMed] [Google Scholar]
- 11.Mehta DH, Gardiner PM, Phillips RS, McCarthy EP. Herbal and dietary supplement disclosure to health care providers by individuals with chronic conditions. J Altern Complement Med. 2008;14:1263–1269. doi: 10.1089/acm.2008.0290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Su D, Li L, Pagan JA. Acculturation and the use of complementary and alternative medicine. Soc Sci Med. 2008;66:439–453. doi: 10.1016/j.socscimed.2007.08.023. [DOI] [PubMed] [Google Scholar]
- 13.Rivera JO, Chaudhuri K, Gonzalez-Stuart A, Tyroch A, Chaudhuri S. Herbal product use by Hispanic surgical patients. Am Surg. 2005;71:71–76. [PubMed] [Google Scholar]
- 14.Rivera JO, Gonzalez-Stuart A, Ortiz M, Rodriguez JC, Anaya JP, Meza A. Herbal product use in non-HIV and HIV-positive Hispanic patients. J Natl Med Assoc. 2005;97:1686–1691. [PMC free article] [PubMed] [Google Scholar]
- 15.Rivera JO, Ortiz M, Gonzalez-Stuart A, Hughes H. Bi-national evaluation of herbal product use on the United States/Mexico border. J Herb Pharmacother. 2007;7:91–106. doi: 10.1080/15228940802142621. [DOI] [PubMed] [Google Scholar]
- 16.Busse JW, Heaton G, Wu P, Wilson KR, Mills EJ. Disclosure of natural product use to primary care physicians: a cross-sectional survey of naturopathic clinic attendees. Mayo Clin Proc. 2005;80:616–623. doi: 10.4065/80.5.616. [DOI] [PubMed] [Google Scholar]
- 17.Kuo GM, Hawley ST, Weiss LT, Balkrishnan R, Volk RJ. Factors associated with herbal use among urban multiethnic primary care patients: a cross-sectional survey. BMC Complement Altern Med. 2004;4:18. doi: 10.1186/1472-6882-4-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mikhail N, Wali S, Ziment I. Use of alternative medicine among Hispanics. J Altern Complement Med. 2004;10:851–859. doi: 10.1089/acm.2004.10.851. [DOI] [PubMed] [Google Scholar]
- 19.Ahn AC, Ngo-Metzger Q, Legedza AT, Massagli MP, Clarridge BR, Phillips RS. Complementary and alternative medical therapy use among Chinese and Vietnamese Americans: prevalence, associated factors, and effects of patient-clinician communication. Am J Public Health. 2006;96:647–653. doi: 10.2105/AJPH.2004.048496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kronenberg F, Cushman LF, Wade CM, Kalmuss D, Chao MT. Race/ethnicity and women’s use of complementary and alternative medicine in the United States: results of a national survey. Am J Public Health. 2006;96:1236–1242. doi: 10.2105/AJPH.2004.047688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brown CM, Barner JC, Richards KM, Bohman TM. Patterns of complementary and alternative medicine use in African Americans. J Altern Complement Med. 2007;13:751–758. doi: 10.1089/acm.2006.6392. [DOI] [PubMed] [Google Scholar]
- 22.Jones RA, Taylor AG, Bourguignon C, Steeves R, Fraser G, Lippert M, Theodorescu D, Mathews H, Kilbridge KL. Complementary and alternative medicine modality use and beliefs among African American prostate cancer survivors. Oncol Nurs Forum. 2007;34:359–364. doi: 10.1188/07.ONF.359-364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weinrich SP, Hudson Priest J, Moyad MA, Weinrich MC. Intake of selected nutritional supplements by African-American men. Urology. 2004;64:1094–1097. doi: 10.1016/j.urology.2004.08.020. [DOI] [PubMed] [Google Scholar]
- 24.Owen-Smith A, Diclemente R, Wingood G. Complementary and alternative medicine use decreases adherence to HAART in HIV-positive women. AIDS Care. 2007;19:589–593. doi: 10.1080/09540120701203279. [DOI] [PubMed] [Google Scholar]
- 25.Milan FB, Arnsten JH, Klein RS, Schoenbaum EE, Moskaleva G, Buono D, Webber MP. Use of complementary and alternative medicine in innercity persons with or at risk for HIV infection. AIDS Patient Care STDS. 2008;22:811–816. doi: 10.1089/apc.2007.0159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Uzzo RG, Brown JG, Horwitz EM, Hanlon A, Mazzoni S, Konski A, Greenberg RE, Pollack A, Kolenko V, Watkins-Bruner D. Prevalence and patterns of self-initiated nutritional supplementation in men at high risk of prostate cancer. BJU Int. 2004;93:955–9560. doi: 10.1111/j.1464-410X.2004.04759.x. [DOI] [PubMed] [Google Scholar]
- 27.Liu C, Yang Y, Gange SJ, Weber K, Sharp GB, Wilson TE, Levine A, Robison E, Goparaju L, Gandhi M, Merenstein D. Disclosure of complementary and alternative medicine use to health care providers among HIV-infected women. AIDS Patient Care STDS. 2009;23:965–971. doi: 10.1089/apc.2009.0134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Risa KJ, Nepon L, Justis JC, Panwalker A, Berman SM, Cinti S, Wagener MM, Singh N. Alternative therapy use in HIV-infected patients receiving highly active antiretroviral therapy. Int J STD AIDS. 2002;13:706–713. doi: 10.1258/095646202760326471. [DOI] [PubMed] [Google Scholar]
- 29.Gomez-Beloz A, Chavez N. The botanica as a culturally appropriate health care option for Latinos. J Altern Complement Med. 2001;7:537–546. doi: 10.1089/10755530152639765. [DOI] [PubMed] [Google Scholar]
- 30.Hatcher E, Whittemore R. Hispanic adults’ beliefs about type 2 diabetes: clinical implications. J Am Acad Nurse Pract. 2007;19:536–545. doi: 10.1111/j.1745-7599.2007.00255.x. [DOI] [PubMed] [Google Scholar]
- 31.Hunt LM, Arar NH, Akana LLHerbs, prayer insulin. Use of medical and alternative treatments by a group of Mexican American diabetes patients. J Fam Pract. 2000;49:216–223. [PubMed] [Google Scholar]
- 32.Jernewall N, Zea MC, Reisen CA, Poppen PJ. Complementary and alternative medicine and adherence to care among HIV-positive Latino gay and bisexual men. AIDS Care. 2005;17:601–609. doi: 10.1080/09540120512331314295. [DOI] [PubMed] [Google Scholar]
- 33.Jezewski MA, Poss J. Mexican Americans’ explanatory model of type 2 diabetes. West J Nurs Res. 2002;24:840–858. doi: 10.1177/019394502237695. discussion 858-67. [DOI] [PubMed] [Google Scholar]
- 34.Loera JA, Black SA, Markides KS, Espino DV, Goodwin JS. The use of herbal medicine by older Mexican Americans. J Gerontol A Biol Sci Med Sci. 2001;56:M714–M718. doi: 10.1093/gerona/56.11.m714. [DOI] [PubMed] [Google Scholar]
- 35.Ortiz BI, Clauson KA. Use of herbs and herbal products by Hispanics in south Florida. J Am Pharm Assoc. 2003;2006(46):161–167. doi: 10.1331/154434506776180649. [DOI] [PubMed] [Google Scholar]
- 36.Poss JE, Jezewski MA, Stuart AG. Home remedies for type 2 diabetes used by Mexican Americans in El Paso, Texas. Clin Nurs Res. 2003;12:304–323. doi: 10.1177/1054773803256872. [DOI] [PubMed] [Google Scholar]
- 37.Shapiro K, Gong WC. Use of herbal products for diabetes by Latinos. J Am Pharm Assoc (Wash) 2002;42:278–279. doi: 10.1331/108658002763508542. [DOI] [PubMed] [Google Scholar]
- 38.White B, Knox L, Zepeda M, Mull D, Nunez F. Impact of immigration on complementary and alternative medicine use in Hispanic patients. J Am Board Fam Med. 2009;22:337–338. doi: 10.3122/jabfm.2009.03.080210. [DOI] [PubMed] [Google Scholar]
- 39.Burge SK, Albright TL. Residency Research Network of South Texas (RRNeST): use of complementary and alternative medicine among family practice patients in south Texas. Am J Public Health. 2002;92:1614–1616. doi: 10.2105/ajph.92.10.1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lundy MB, Morgan LL, Rhoads KVL, Bay RC. Hispanic and anglo patients’ reported use of alternative medicine in the medical clinic context. Complementary Health Pract Rev. 2001;6:205–217. [Google Scholar]
- 41.Sleath BL, Williams JW., Jr Hispanic ethnicity, language, and depression: physician-patient communication and patient use of alternative treatments. Int J Psychiatry Med. 2004;34:235–246. doi: 10.2190/VQU1-QYWT-XW6Y-4M14. [DOI] [PubMed] [Google Scholar]
- 42.Sleath B, Rubin RH, Campbell W, Gwyther L, Clark T. Ethnicity and physician-older patient communication about alternative therapies. J Altern Complement Med. 2001;7:329–335. doi: 10.1089/107555301750463206. [DOI] [PubMed] [Google Scholar]
- 43.Fang L, Schinke SP. Complementary alternative medicine use among Chinese Americans: findings from a community mental health service population. Psychiatr Serv. 2007;58:402–404. doi: 10.1176/ps.2007.58.3.402. [DOI] [PubMed] [Google Scholar]
- 44.Kim J, Chan MM. Factors influencing preferences for alternative medicine by Korean Americans. Am J Chin Med. 2004;32:321–329. doi: 10.1142/S0192415X04001977. [DOI] [PubMed] [Google Scholar]
- 45.Satow YE, Kumar PD, Burke A, Inciardi JF. Exploring the prevalence of ayurveda use among Asian Indians. J Altern Complement Med. 2008;14:1249–1253. doi: 10.1089/acm.2008.0106. [DOI] [PubMed] [Google Scholar]
- 46.Wade C, Chao MT, Kronenberg F. Medical pluralism of Chinese women living in the United States. J Immigr Minor Health. 2007;9:255–267. doi: 10.1007/s10903-007-9038-x. [DOI] [PubMed] [Google Scholar]