Abstract
Objective
To examine whether non-psychiatric hospitalizations rates were higher in those with mental disorders.
Method
In a cohort of 15 811 employees, aged 35–50 years in 1989, mental disorder status was defined from 1989 to 2000. Hospitalizations for all-causes, myocardial infarction (MI), stroke, and cancer, were recorded yearly from 2001 to 2011. Negative binomial regression models were used to estimate hospitalization rates over the follow-up.
Results
After controlling for baseline sociodemographic factors, health-related behaviors, self-rated health, and self-reported medical conditions, participants with a mental disorder had significantly higher rates of all-cause hospitalization [incidence rate ratio, IRR = 1.20 (95%, 1.14–1.26)], as well as hospitalization due to MI [IRR = 1.44 (95%, 1.12–1.85)]. For stroke, the IRR did not reach statistical significance [IRR = 1.37 (95%, 0.95–1.99)] and there was no association with cancer [IRR = 1.01 (95%, 0.86–1.19)]. A similar trend was observed when mental disorders groups were considered (no mental disorder, depressive disorder, mental disorders due to psychoactive substance use, other mental disorders, mixed mental disorders, and severe mental disorder).
Conclusion
In this prospective cohort of employees with stable employment as well as universal access to healthcare, we found participants with mental disorders to have higher rates of non-psychiatric hospitalizations.
Keywords: mental disorders, hospitalizations, healthcare, chronic disease, prospective study
Significant outcomes
Individuals with mental disorders had significantly higher rates of all-cause (after excluding those for psychiatric reasons), myocardial infarction and stroke-related hospitalizations compared to those without.
This effect was not observed for cancer-related hospitalizations.
Limitations
Diagnosis of mental disorders was based on medically certified sickness absence episodes rather than structured clinical interviews.
As the GAZEL cohort is not representative of the general population, a healthy worker effect cannot be excluded.
Introduction
Premature mortality among individuals with mental disorders has become a matter of concern (1–3). Research suggests that they have a two- to three-fold increased risk of mortality with some evidence of an increasing mortality gap between persons with mental disorders and the general population (4–6). For example, an American study conducted on data collected from 1997 to 2000 found that individuals with severe mental illness, who were treated in the public healthcare system, had a lower life expectancy of 13 to over 30 years compared to the general population (7).
Excess mortality in individuals with mental disorders is partly, but not only, due to higher suicide rate in this group. Indeed, persons with mental disorders have an increased risk of mortality from physical illnesses, with the commonest cause of mortality being cardiovascular disease, particularly coronary heart disease (CHD) (2, 8–12). Numerous studies have shown that patients with schizophrenia, bipolar disorder, or depression have an increased risk of mortality due to cardiovascular diseases (CVD) (4, 9, 11). The underlying mechanisms are not fully understood; disparities in access or quality of primary health care have been hypothesized as candidate mechanisms for this association (13, 14).
Potentially preventable hospitalizations are increasingly used as measures of access, quality and effectiveness of primary health care (15, 16), as well as indicators of health care disparities (17, 18). Access to timely and appropriate preventive and primary care could prevent or reduce hospitalizations (19). There is consistent evidence showing higher hospitalization rates to be associated with poor access to primary care among vulnerable groups including pediatric populations (20), elderly (21), low-income and uninsured individuals and minorities (22, 23). However, few studies have examined this hypothesis in those with mental disorders, and the extant studies are limited due to their cross-sectional or retrospective design, focus on specific subgroups (schizophrenia) or use of electronic health records with incomplete adjustment for confounding factors (24–27).
Aims of the study
We use data from a large cohort of employees to compare non-psychiatric hospitalization rates between individuals with and without mental disorders, with a focus on hospitalizations for all-causes (excluding psychiatric reasons), myocardial infarction, stroke, and cancer.
Material and methods
Study population
The GAZEL cohort study was established in 1989, further details of this study are available elsewhere (28). Briefly, the target population consisted of employees of the French national gas and electricity company (EDF–GDF) who have civil servant like employment conditions. At baseline, 20 625 volunteers (15 011 men and 5614 women), aged 35–50 years, gave consent to participate in this study. The study design consists of an annual questionnaire used to collect data on health, lifestyle, individual, familial, social, and occupational factors and life events (28). Various sources within EDF–GDF provide additional data on GAZEL participants. The company has an occupational health department, its own medical insurance and a detailed surveillance system that permits extensive follow-up and linkage of health records with exposure characteristics (29). The GAZEL study received approval from the national commission overseeing ethical data collection in France (Commission Nationale de L'Informatique et Libertés).
Measures
Mental disorders
The Health Insurance Department of EDF–GDF established an epidemiological database that records all episodes of sickness absence from work. This database includes medical diagnoses associated with each absence episode, irrespective of length, coded by the occupational physicians according to the International Classification of Diseases (ICD), 9th and 10th Revisions. For this study, we used all medically certified sickness absence episodes of more than 7 days for mental disorder, in accordance with previous analyses in the GAZEL cohort (30–33) and in other cohorts such as the British Whitehall II study (34).
Using an 12-year exposure window (from January 1, 1989 to December 31, 2000), we first created a dichotomized ‘mental disorder’ variable coded as ‘0’ for participants without sickness absence for mental disorder and ‘1’ for those with at least one sickness absence episode for mental disorder. To further explore the association between mental disorders and hospitalizations, we also created a six-category variable: (i) ‘no mental disorder’ group included participants with no sickness absence for mental disorder, (ii) ‘depressive disorder’ group included participants with only sickness absence episode for dysthymic disorder (ICD-9: 300.4), depressive episode (ICD-10: F32), or recurrent depressive disorder (ICD-10: F33), (iii) ‘mental disorders due to psychoactive substance use’ group included participants with only sickness absence episode for alcohol dependence syndrome (ICD-9: 303), non-dependent abuse of drugs (ICD-9: 305), or mental disorders due to use of alcohol (ICD-10: F10), (iv) ‘other mental disorders’ group included participants with only sickness absence episodes for unspecified non-psychotic mental disorder (ICD-9: 300.9), dementia in Alzheimer disease (ICD-10: F00), persistent mood disorders (ICD-10: F34), phobic anxiety, and other anxiety disorders (ICD-10: F40–F41), obsessive–compulsive disorder (ICD-10: F42) or other mental disorder (ICD-10: F99), (v) ‘mixed mental disorders’ group included participants with sickness absence episodes for at least two of the following diagnosis: ‘depressive disorder’, ‘mental disorders due to psychoactive substance use’, ‘other mental disorders’, and ‘mixed anxiety and depressive disorder (ICD-10: F41.2)’, and (vi) ‘severe mental disorder’ group included participants with at least one sickness absence episode for psychoses (ICD-9: 290-299), schizophrenia, or delusional disorder (ICD-10: F20–F29) or maniac episode or bipolar disorder (ICD-10: F30–F31).
Hospitalizations
Each year from 2001, participants of the GAZEL cohort were asked to respond to the following questions ‘Over the past 12 months, have you been hospitalized?’ and ‘If so, what are the reason and the date of hospitalization?’. Hospitalizations for all-cause (excluding psychiatric reasons), myocardial infarction (MI), stroke, and cancer were recorded yearly from 2001 to 2011. For each individual, we computed the number of each type of hospitalization over the 10 year follow-up.
Baseline covariates
Age, sex, and occupational position were obtained from the employer's human resources files. Education (university degree, higher secondary school, or lower than higher secondary school), income (high/intermediate or low), and marital status (married/cohabiting or other) were used as measures of sociodemographic factors. Alcohol consumption and smoking were self-reported. Alcohol consumption, as drinks per week, was categorized as none, moderate (1–20 for men, 1–13 for women), or heavy consumption (>21 for men, >14 for women). Smoking was categorized as: never-smokers, ex-smokers and current smokers. Self-rated health (good or suboptimum) was assessed using a standard question: ‘How would you judge the state of your general health?’. A checklist was used to determine the following somatic diseases: respiratory diseases (recurrent respiratory infections, chronic bronchitis, asthma…) CVD (hypertension, angina, MI…), and endocrine and metabolic diseases (diabetes, hypercholesterolemia, gout…). Participants were asked whether they had a medical diagnosis over the past 12 months for these conditions and to indicate whether they received treatment for them. For each condition, we created three categories: no, treated, and untreated.
Statistical analyses
Differences in baseline characteristics of the participants as a function of the presence of any mental disorder over the follow-up period were assessed using a chi-square test. Differences in baseline characteristics of participants as a function of the number hospitalizations from all-causes were assessed using one-way anova. Three serially adjusted negative binomial regression models (35) were used to estimate all-cause and cause-specific hospitalization rates as a function of mental disorders. In model 1, incidence rate ratios (IRRs) were adjusted for sociodemographic factors (age, sex, marital status, occupational grade, educational and income levels). Model 2 was additionally adjusted for smoking and alcohol intake. Finally, IRRs in model 3 were further adjusted for self-rated health and somatic diseases. Similar analyses were undertaken to estimate hospitalization rates over the follow-up using categories of mental disorders. As sex and age interactions terms did not affect results, we combined men and women, and age groups in the analyses. All tests were two-sided and P values were considered significant at the 0.05 level. All statistical analyses were conducted using stata (version 12; Stata Corp, College Station, TX, USA).
Results
Baseline characteristics of the 15 811 participants included in the analyses with complete data on all 12 covariates are presented in Table 1. Among these participants, 2199 (13.9%) had received at least one diagnosis for mental disorder over the 1989 to 2000 period. Among them, 54.3% (n = 1194) had a diagnosis for depressive disorder, 11.5% (n = 252) had a diagnosis of ‘mental disorders due to psychoactive substance use’, 7.5% (n = 166) had a diagnosis of ‘other mental disorders’, 24.6% (n = 541) had a diagnosis for ‘mixed mental disorders’, and 2.1% (n = 46) a diagnostic for ‘severe mental disorder’. Participants with a diagnosis of mental disorder were more likely to be female, young, not married/cohabiting, have a lower occupational position, to have lower income and educational levels, smokers, and alcohol abstainers (all P < 0.001). They were also more likely to have poor self-rated health and to have higher rates of (treated and untreated) respiratory, cardiovascular, endocrine, and metabolic diseases (all P ≤ 0.003).
Table 1.
Baseline characteristics as a function of mental disorder status
| Variables | N total (N = 15 811) | Any mental disorder (1989–2000) |
||
|---|---|---|---|---|
| No (N = 13 612) | Yes (N = 2199) | P value | ||
| Sex | ||||
| Men | 11 699 (74.0) | 10 709 (78.7) | 990 (45.0) | <0.001 |
| Women | 4112 (26.0) | 2903 (21.3) | 1209 (55.0) | |
| Age group (years) | ||||
| ≤40 | 3402 (21.5) | 2673 (19.6) | 729 (33.2) | <0.001 |
| 41–45 | 7835 (49.6) | 6827 (50.2) | 1008 (45.8) | |
| 46–50 | 4574 (28.9) | 4112 (30.2) | 462 (21.0) | |
| Marital status | ||||
| Married/cohabiting | 14 164 (89.6) | 12 352 (90.7) | 1812 (82.4) | <0.001 |
| Other | 1647 (10.4) | 1260 (9.3) | 387 (17.6) | |
| Occupational grade | ||||
| Low | 2442 (15.4) | 1838 (13.5) | 604 (27.5) | <0.001 |
| Middle | 9220 (58.3) | 7857 (57.7) | 1363 (62.0) | |
| High | 4149 (26.2) | 3917 (28.8) | 232 (10.6) | |
| Income level | ||||
| Intermediate/high | 9294 (58.8) | 8100 (59.5) | 1194 (54.3) | <0.001 |
| Low | 6517 (41.2) | 5512 (40.5) | 1005 (45.7) | |
| Education | ||||
| University degrees | 3197 (20.2) | 2923 (21.5) | 274 (12.5) | <0.001 |
| Higher secondary school | 9306 (58.9) | 7956 (58.4) | 1350 (61.4) | |
| Lower than higher secondary school | 3308 (20.9) | 2733 (20.1) | 575 (26.1) | |
| Smoking | ||||
| Smokers | 4191 (26.5) | 3492 (25.7) | 699 (31.8) | <0.001 |
| Non-smokers | 6952 (44.0) | 5890 (43.3) | 1062 (48.3) | |
| Ex-smokers | 4668 (29.5) | 4230 (31.1) | 438 (19.9) | |
| Alcohol use | ||||
| None | 387 (2.4) | 270 (2.0) | 117 (5.3) | <0.001 |
| Moderate | 14 024 (88.7) | 12 110 (89.0) | 1914 (87.0) | |
| Heavy | 1400 (8.9) | 1232 (9.1) | 168 (7.6) | |
| Self-rated health | ||||
| Good | 13 908 (88.0) | 12 175 (89.4) | 1733 (78.8) | <0.001 |
| Suboptimum | 1903 (12.0) | 1437 (10.6) | 466 (21.2) | |
| Respiratory diseases | ||||
| No | 12 006 (75.9) | 10 431 (76.6) | 1575 (71.6) | <0.001 |
| Yes, treated | 624 (3.9) | 530 (3.9) | 94 (4.3) | |
| Yes, untreated | 3181 (20.1) | 2651 (19.5) | 530 (24.1) | |
| Cardiovascular diseases | ||||
| No | 11 044 (69.9) | 9567 (70.3) | 1477 (67.2) | 0.003 |
| Yes, treated | 1346 (8.5) | 1123 (8.3) | 223 (10.1) | |
| Yes, untreated | 3421 (21.6) | 2922 (21.5) | 499 (22.7) | |
| Endocrine and metabolic disease | ||||
| No | 15 216 (96.2) | 13 130 (96.5) | 2086 (94.9) | <0.001 |
| Yes, treated | 304 (1.9) | 256 (1.9) | 48 (2.2) | |
| Yes, untreated | 291 (1.8) | 226 (1.7) | 65 (3.0) | |
Table 2 presents differences in participants’ baseline characteristics as a function of the number hospitalizations (excluding those for psychiatric reasons). Men, older participants, those from higher occupational position, ex-smokers, those with poor self-rated health, and higher rates of (treated and untreated) respiratory, cardiovascular, endocrine, and metabolic diseases had higher number of hospitalizations from all-causes (all P < 0.001). Compared to participants included in this study, those who have been excluded were likely to be women, younger, from lower occupational grade, and less likely to be married and/or cohabiting (all <0.001).
Table 2.
Baseline characteristics as a function of all-cause hospitalizations (excluding psychiatric reasons)
| Variables | No (N = 15 811) | All-cause hospitalizations (2001–2011) |
|
|---|---|---|---|
| Mean (SD) | P value | ||
| Sex | |||
| Men | 11 699 (74.0) | 1.33 (1.45) | <0.001 |
| Women | 4112 (26.0) | 1.18 (1.33) | |
| Age group (years) | |||
| ≤40 | 3402 (21.5) | 1.08 (1.32) | <0.001 |
| 41–45 | 7835 (49.6) | 1.27 (1.40) | |
| 46–50 | 4574 (28.9) | 1.49 (1.51) | |
| Marital status | |||
| Married/cohabiting | 14 164 (89.6) | 1.29 (1.42) | 0.671 |
| Other | 1647 (10.4) | 1.27 (1.41) | |
| Occupational grade | |||
| Low | 2442 (15.4) | 1.19 (1.37) | <0.001 |
| Middle | 9220 (58.3) | 1.29 (1.42) | |
| High | 4149 (26.2) | 1.36 (1.44) | |
| Income level | |||
| Intermediate/high | 9294 (58.8) | 1.30 (1.43) | 0.098 |
| Low | 6517 (41.2) | 1.27 (1.42) | |
| Education | |||
| University degrees | 3197 (20.2) | 1.31 (1.47) | 0.882 |
| Higher secondary school | 9306 (58.9) | 1.28 (1.41) | |
| Lower than higher secondary school | 3308 (20.9) | 1.30 (1.42) | |
| Smoking | |||
| Smokers | 4191 (26.5) | 1.30 (1.46) | <0.001 |
| Non-smokers | 6952 (44.0) | 1.22 (1.38) | |
| Ex-smokers | 4668 (29.5) | 1.38 (1.44) | |
| Alcohol use | |||
| None | 387 (2.4) | 1.38 (1.57) | 0.317 |
| Moderate | 14 024 (88.7) | 1.28 (1.41) | |
| Heavy | 1400 (8.9) | 1.35 (1.48) | |
| Self-rated health | |||
| Good | 13 908 (88.0) | 1.26 (1.38) | <0.001 |
| Suboptimum | 1903 (12.0) | 1.55 (1.65) | |
| Respiratory diseases | |||
| No | 12 006 (75.9) | 1.27 (1.40) | <0.001 |
| Yes, treated | 624 (3.9) | 1.49 (1.51) | |
| Yes, untreated | 3181 (20.1) | 1.35 (1.48) | |
| Cardiovascular diseases | |||
| No | 11 044 (69.9) | 1.23 (1.37) | <0.001 |
| Yes, treated | 1346 (8.5) | 1.51 (1.62) | |
| Yes, untreated | 3421 (21.6) | 1.41 (1.47) | |
| Endocrine and metabolic disease | |||
| No | 15 216 (96.2) | 1.27 (1.41) | <0.001 |
| Yes, treated | 304 (1.9) | 1.86 (1.87) | |
| Yes, untreated | 291 (1.8) | 1.61 (1.58) | |
| Any mental disorders (1989–2000) | |||
| No | 13 612 (86.1) | 1.28 (1.41) | 0.018 |
| Yes | 2199 (13.9) | 1.37 (1.49) | |
Mental disorders and all-cause hospitalizations
Figure1 shows that after adjustment for sociodemographic factors (model 1), participants with mental disorders had significantly higher rate of all-cause hospitalizations [IRR = 1.25 (95%, 1.19–1.32)] when compared to those without mental disorders. This association was only slightly reduced after adjustment for smoking and alcohol intake in model 2 [IRR = 1.24 (95%, 1.18–1.31)] and self-rated health and reported medical conditions in model 3 (IRR = 1.20 (95%, 1.14–1.26)]. A similar pattern was observed when diagnostic categories of mental disorders were considered. Compared to those without mental disorder, participants with depressive disorder [IRR = 1.24 (95%, 1.16–1.32)], mental disorders due to psychoactive substance use [IRR = 1.24 (95%, 1.09–1.41)], other mental disorders [IRR = 1.26 (95%, 1.07–1.49)], and mixed mental disorders [IRR = 1.28 (95%, 1.17–1.41)] had significantly higher rates of all-cause hospitalizations in model 1. These associations remained robust to adjustment for health-related behaviors (model 2) and self-rated health, and somatic diseases (model 3).
Fig 1.
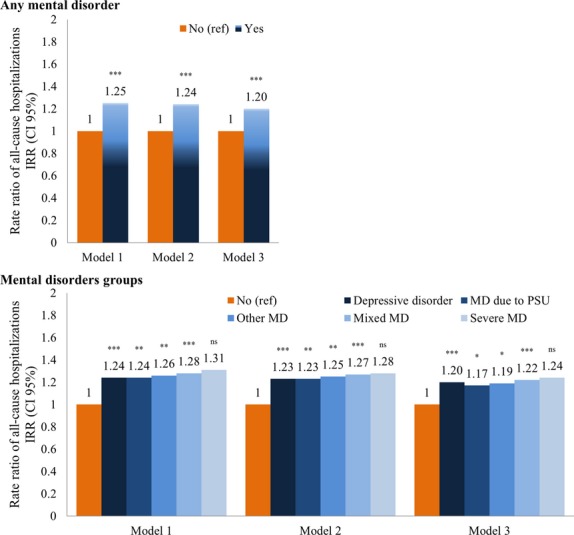
Mental disorders and all-cause hospitalizations (excluding psychiatric reason). *P < 0.05; **P < 0.01; ***P < 0.001; nsnon-significant. MD, mental disorder; PSU, psychoactive substance use. Model 1: incidence rate ratio (IRR) adjusted on sex, age group, marital status, occupational grade, income level, and education. Model 2: IRR model 1 adjusted on smoking and alcohol use. Model 3: IRR model 2 adjusted on self-related health and somatic diseases.
Mental disorders and myocardial infarction hospitalizations
Figure2 shows MI hospitalization rates over the follow-up as a function of the presence of mental disorder. In model 1, participants with any mental disorder had significantly higher rate of hospitalizations for MI [IRR = 1.63 (95%, 1.27–2.10)] compared to those without mental disorders. Additional adjustment for health-related behaviors in model 2 [IRR = 1.54 (95%, 1.20–1.97)] and self-rated health and medical conditions in model 3 [IRR = 1.44 (95%, 1.12–1.85)] did not affect this association. When diagnostic categories were taken into account, only participants with depressive disorder [IRR = 1.42 (95%, 1.02–1.99)] and those with mixed mental disorders [IRR = 2.20 (95%, 1.39–3.49)] had significantly higher rates of hospitalizations for MI. In fully adjusted models (model 3), hospitalization rates for MI remained significantly higher only among participants with mixed mental disorders [IRR = 1.93 (95%, 1.22–3.05)].
Fig 2.
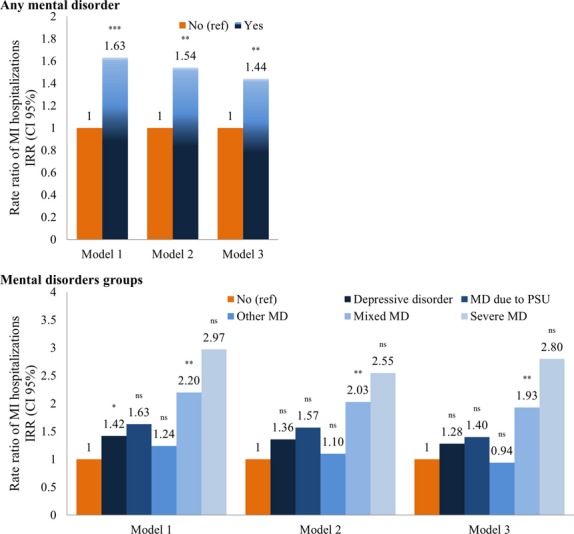
Mental disorders and myocardial infarction (MI) hospitalizations. *P < 0.05; **P < 0.01; ***P < 0.001; nsnon-significant. MD, mental disorder; PSU, psychoactive substance use. Model 1: incidence rate ratio (IRR) adjusted on sex, age group, marital status, occupational grade, income level, and education. Model 2: IRR model 1 adjusted on smoking and alcohol use. Model 3: IRR model 2 adjusted on self-related health and somatic diseases.
Mental disorders and stroke hospitalizations
Figure3 shows hospitalization rates for stroke over the follow-up as a function of the presence of mental disorder. In model 1, participants with mental disorder had significantly higher rate of stroke hospitalizations [IRR = 1.48 (95%, 1.03–2.13)] but adjustment for health-related behaviors [IRR = 1.43 (95%, 0.99–2.07)], self-rated health, and medical conditions [IRR = 1.37 (95%, 0.95–1.99)] reduced the magnitude of this association and rendered it non-significant at P = 0.05. When diagnostic categories were considered, there was no significant difference of stroke hospitalizations rates between participants with mental disorders and those without.
Fig 3.
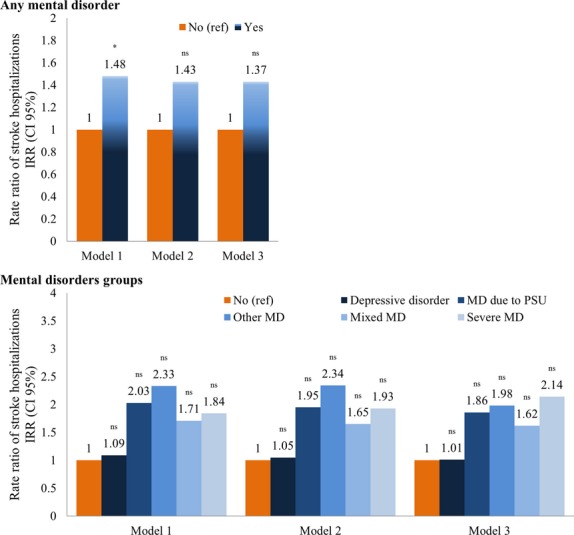
Mental disorders and stroke hospitalizations. *P < 0.05; **P < 0.01; ***P < 0.001; nsnon-significant. MD, mental disorder; PSU, psychoactive substance use. Model 1: incidence rate ratio (IRR) adjusted on sex, age group, marital status, occupational grade, income level, and education. Model 2: IRR model 1 adjusted on smoking and alcohol use. Model 3: IRR model 2 adjusted on self-related health and somatic diseases
Mental disorders and cancer hospitalizations
Figure4 displays hospitalization rates for cancer over the follow-up as a function of the presence of mental disorder. In model 1 adjusted for sociodemographic characteristics, there was no difference in cancer hospitalization rates between participants with mental disorders and those without [IRR = 1.07 (95%, 0.91–1.25)]. This remained unchanged in models adjusted for covariates. Similar results were obtained using diagnostic categories for the adjusted models.
Fig 4.
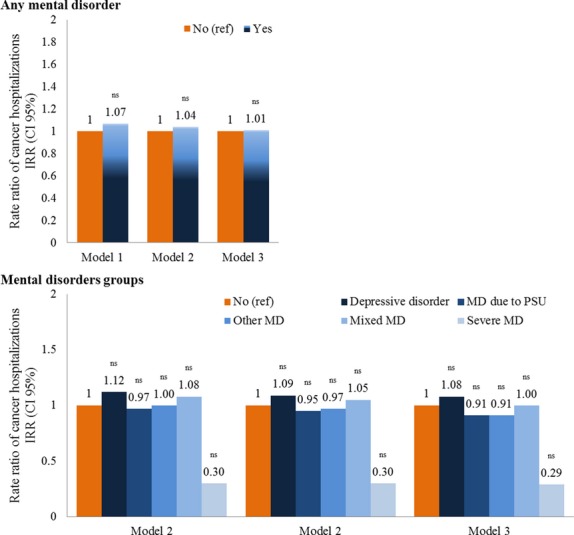
Mental disorders and cancer hospitalizations. *P < 0.05; **P < 0.01; ***P < 0.001; nsnon-significant. MD, mental disorder; PSU, psychoactive substance use. Model 1: incidence rate ratio (IRR) adjusted on sex, age group, marital status, occupational grade, income level, and education. Model 2: IRR model 1 adjusted on smoking and alcohol use. Model 3: IRR model 2 adjusted on self-related health and somatic diseases.
Sensitivity analyses
To test the robustness of our findings, we conducted further analyses. First, we stratified our analyses by retirement status. The results of the fully adjusted models reveal retirement status not to confound or modify associations, although associations were stronger in non-retired participants. Among both non-retired [IRR = 1.24 (95%, 1.14–1.34)] and retired [IRR = 1.16 (95%, 1.08–1.24)] participants, a diagnosis for mental disorders was associated with higher rates of all-cause hospitalizations. The corresponding figures for MI hospitalizations were IRR = 1.78 (95%, 1.15–2.74) and IRR = 1.27 (95%, 0.93–1.73), for stroke hospitalizations IRR = 1.54 (95%, 0.84–2.81) and IRR = 1.27 (95%, 0.79–2.03), and for cancer hospitalizations IRR = 1.02 (95%, 0.80–1.31) and IRR = 0.98 (95%, 0.79–1.22). Second, as we used an 12-year exposure window to assess mental disorders, we divided the observation period into two (1989–1993 and 1994–2000), to determine whether associations differed according to the period to which the diagnosis of mental disorders was attributed. The results for both periods were similar to those reported in our main analyses.
Discussion
Summary of findings
Using a large occupational cohort of over 15 000 participants, we examined whether rates of non-psychiatric hospitalization vary between individuals with and without mental disorders. After adjustment for sociodemographic factors, we found that those with a mental disorder had significantly higher rates of all-cause (after excluding those for psychiatric reasons) and cardiovascular (MI, stroke) but not cancer-related hospitalizations. In fully adjusted models, only associations with all-cause and MI hospitalizations remained statistically significant. A similar trend was observed when specific psychiatric diagnostic categories were considered, but the magnitude of the associations was much stronger, particularly for MI and stroke hospitalizations.
Results in the context of the literature
To the best of our knowledge, this is the first large observational study to examine the prospective association between the presence of a mental disorder and hospitalizations for multiple causes. Four previous studies have examined the association between mental disorders in general (25, 26) or a specific mental disorder such as schizophrenia (24, 27) and hospitalizations. In contrast to our well-characterized cohort study, previous studies were based on administrative databases, which limited their ability to examine the effects of potential confounders such as education, occupational position, and health-related behaviors. We were also able to track hospitalizations over 10 years, thus minimizing chance findings. Nonetheless, our results are in accordance with findings from previous studies. The first study that included a large sample of hospitalized in-patient cases, using discharge data from New York State Hospital, found persons with mental disorders over two times (adjusted odds ratio, AOR = 2.30) more likely to be hospitalized for ambulatory care sensitive medical conditions (preventable conditions) (25). In addition, all major mental disorders including schizophrenia, major depression, and bipolar disorder were found to have two to four times higher risk of hospitalizations. The second study using a 5-year follow-up from Taiwan on 2503 patients with schizophrenia and 20 024 matched controls (24) showed schizophrenics to have a 3.26-fold higher risk of hospitalization in a setting with universal health coverage. The third study was a retrospective population-based cohort of more than 400 000 patients with mental disorders and 290 000 controls in Western Australia (26). Using linked data from electoral roll registrations, mental health registry records and hospital discharges, the results showed that patients with any mental disorder were two times more likely to experience a potentially preventable hospitalization with the associations being stronger for more severe mental disorders such as alcohol and drugs disorders, affective psychoses and other psychoses and schizophrenia. Finally, a retrospective cross-sectional American study (27) on adults aged 18–64 showed that schizophrenia was associated with higher hospitalization rates.
Interpretation of the findings
Preventable hospitalizations in general and for chronic medical conditions in particular are increasingly used as a measure of access to health care (19) with the hypothesis that timely and appropriate preventive and primary care should reduce hospitalizations. Thus, the association we observed could be interpreted to suggest that participants with mental disorders do not have adequate access to preventive and primary care. However, our results are based on a cohort with access to universal healthcare and do not support this hypothesis. Indeed, participants in the GAZEL cohort have civil servant status and benefit from job security. In addition, an extensive human resources system allows for a complete follow-up of all workers. Finally, the company had its own Occupational Health and Social Security system with approximately 300 physicians responsible for workers’ health surveillance. These peculiarities fit with several suggestions that have been put forward to reduce the increased mortality of patients with mental disorders in the general population. Our results and the setting in which they have been obtained suggest that this might not be enough and that it is the ‘quality’ rather than access to healthcare that matters, particularly in settings like France where there is access to universal healthcare. Contextual factors are bound to influence health care provision but our basic finding of higher hospitalization in those with mental disorders is unlikely to be shaped by them. It has been suggested that one plausible reason for somatic health disparities observed between individuals with mental disorders could be because of their inability to adequately communicate and express their health concerns and symptoms (36). An alternative explanation could be that healthcare providers may focus on mental health issues, neglecting other health concerns (37). For instance, it has been repeatedly shown that patients with mental disorders benefit from less adequate healthcare regarding cardiovascular risk diseases (38). The present results thus suggest that clinicians should pay extra attention to physical health issues and risk factors when taking care of patients with mental disorders. Another explanation lies in the poorer health profile of individuals with mental disorders, in terms of smoking (39), poor diet (40), physical inactivity (41, 42), obesity (43, 44), diabetes (45), and negligence in treatment options (46). In addition, psychotropic drugs may worsen many of these risk factors. In our analyses, hospitalizations rates remained higher in participants with mental disorders even after adjustment for sociodemographic variables, behavioral risk factors, and medical conditions. Higher hospitalization rates for cardiovascular but not cancer morbidity have been reported previously (14, 47, 48, 38) and require further investigation.
Limitations
Our findings should be interpreted in light of several limitations. First, diagnosis of mental disorders was not based on structured clinical interviews. Although several studies, including those conducted in the GAZEL cohort, have demonstrated the validity of these diagnoses to predict health outcomes (12, 31, 33), misclassification bias cannot be ruled out. Second, although the GAZEL cohort covers all regions of France and a wide socioeconomic range, it is not representative of the general population. GAZEL participants have been shown to be in better health than the source population from which the cohort has been derived (49). Thus, the associations we have observed in the present study might underestimate the relationship between mental disorders and hospitalizations. Finally, hospitalizations were self-reported and although there is good concordance (between 90% and 100% for cancer and cardiovascular disease for example) between self-report of hospitalizations and medical records (50–52), recall bias may still possible.
Despite these limitations, this study makes a unique contribution, as it is the first large prospective population-based study to estimate hospitalization rates for somatic diseases as a function of mental disorders over an extended follow-up period. The fact that our findings were based on an occupational cohort where employees had job security, stable income as well as an occupational health, and social security system in charge of their health surveillance strongly suggests that inadequate preventive and/or medical care or poor self-care rather than limited access to care might partly explain our finding. Clustering of other risk factors as well as pathophysiological processes due to mental disorders in those with mental disorders is another possible explanation. Our findings raise important questions about the need of integration or cooperation between general medical and mental healthcare to support prevention, early diagnosis, treatment, and management of health among individuals with mental disorders. Mental health services and professionals should be implicated and have an important role to play in the management of medical health problems of their patients.
Acknowledgments
The authors thank the French national gas and electricity company ‘Electricité de France-Gaz de France’ (EDF–GDF), especially the ‘Service Général de Médecine de Contrôle’, and the ‘Caisse centrale d'action sociale du personnel des industries électrique et gazière’. The GAZEL Cohort Study was funded by EDF–GDF and INSERM, and received grants from the ‘Cohortes Santé TGIR Program’, ‘Agence nationale de la recherche’ (ANR) and ‘Agence française de sécurité sanitaire de l'environnement et du travail’ (AFSSET). We also thank the ‘Cohortes’ team of the UMS INSERM 011-Versailles St-Quentin University responsible for the GAZEL database management. This study benefited from a multi-institutional grant [Direction Générale de la Santé (DGS), Mission recherché de la Direction de la Recherche, des Etudes, de l'Evaluation et des Statistiques (MiRe-DRESS), Caisse Nationale d'Assurance Maladie des Travailleurs Salariés (CNAMTS), Régime des Indépendants (RSI), Caisse Nationale de Solidarité pour l'Autonomie (CNSA), Institut National de Prévention et D'Education pour la Santé (INPES)] received within the framework of the IReSP call for projects in 2011 (IReSP 2011 A11228LS).
Declaration of interest
None of the authors have conflict of interest in relation to this study to report. Cédric Lemogne has accepted paid speaking engagements in industry-sponsored symposia from Astra Zeneca, Lundbeck, and Servier. Silla M. Consoli has accepted paid speaking engagements in industry-sponsored symposia from Astra Zeneca, Euthérapie, Lilly, Lundbek, Merck Sharp Dohme, and Pfizer.
References
- 1.Harris EC, Barraclough B. Excess mortality of mental disorder. Br J Psychiatry. 1998;173:11–53. doi: 10.1192/bjp.173.1.11. [DOI] [PubMed] [Google Scholar]
- 2.Brown S, Inskip H, Barraclough B. Causes of the excess mortality of schizophrenia. Br J Psychiatry. 2000;177:212–217. doi: 10.1192/bjp.177.3.212. [DOI] [PubMed] [Google Scholar]
- 3.Fagiolini A, Goracci A. The effects of undertreated chronic medical illnesses in patients with severe mental disorders. J Clin Psychiatry. 2009;70(Suppl. 3):22–29. doi: 10.4088/JCP.7075su1c.04. [DOI] [PubMed] [Google Scholar]
- 4.Saha S, Chant D, McGrath J. A systematic review of mortality in schizophrenia: is the differential mortality gap worsening over time? Arch Gen Psychiatry. 2007;64:1123–1131. doi: 10.1001/archpsyc.64.10.1123. [DOI] [PubMed] [Google Scholar]
- 5.Amaddeo F, Barbui C, Perini G, Biggeri A, Tansella M. Avoidable mortality of psychiatric patients in an area with a community-based system of mental health care. Acta Psychiatr Scand. 2007;115:320–325. doi: 10.1111/j.1600-0447.2006.00894.x. [DOI] [PubMed] [Google Scholar]
- 6.Hoang U, Goldacre MJ, Stewart R. Avoidable mortality in people with schizophrenia or bipolar disorder in England. Acta Psychiatr Scand. 2013;127:195–201. doi: 10.1111/acps.12045. [DOI] [PubMed] [Google Scholar]
- 7.Colton CW, Manderscheid RW. Congruencies in increased mortality rates, years of potential life lost, and causes of death among public mental health clients in eight states. Prev Chronic Dis. 2006;3:A42. [PMC free article] [PubMed] [Google Scholar]
- 8.Newcomer JW, Hennekens CH. Severe mental illness and risk of cardiovascular disease. JAMA. 2007;298:1794–1796. doi: 10.1001/jama.298.15.1794. [DOI] [PubMed] [Google Scholar]
- 9.Lawrence DM, Holman CDAJ, Jablensky AV, Hobbs MST. Death rate from ischaemic heart disease in Western Australian psychiatric patients 1980–1998. Br J Psychiatry. 2003;182:31–36. doi: 10.1192/bjp.182.1.31. [DOI] [PubMed] [Google Scholar]
- 10.Hennekens CH, Hennekens AR, Hollar D, Casey DE. Schizophrenia and increased risks of cardiovascular disease. Am Heart J. 2005;150:1115–1121. doi: 10.1016/j.ahj.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 11.Osborn DPJ, Levy G, Nazareth I, Petersen I, Islam A, King MB. Relative risk of cardiovascular and cancer mortality in people with severe mental illness from the United Kingdom's General Practice Research Database. Arch Gen Psychiatry. 2007;64:242–249. doi: 10.1001/archpsyc.64.2.242. [DOI] [PubMed] [Google Scholar]
- 12.Lemogne C, Nabi H, Melchior M, et al. Mortality associated with depression as compared with other severe mental disorders: a 20-year follow-up study of the GAZEL cohort. J Psychiatr Res. 2013;47:851–857. doi: 10.1016/j.jpsychires.2013.03.015. [DOI] [PubMed] [Google Scholar]
- 13.de Hert M, Correll CU, Bobes J, et al. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry. 2011;10:52–77. doi: 10.1002/j.2051-5545.2011.tb00014.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de Hert M, Dekker JM, Wood D, Kahl KG, Holt RIG, Möller HJ. Cardiovascular disease and diabetes in people with severe mental illness position statement from the European Psychiatric Association (EPA), supported by the European Association for the Study of Diabetes (EASD) and the European Society of Cardiology (ESC) Eur Psychiatry. 2009;24:412–424. doi: 10.1016/j.eurpsy.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 15.Brown AD, Goldacre MJ, Hicks N, et al. Hospitalization for ambulatory care-sensitive conditions: a method for comparative access and quality studies using routinely collected statistics. Can J Public Health. 2001;92:155–159. doi: 10.1007/BF03404951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bindman AB, Grumbach K, Osmond D, et al. Preventable hospitalizations and access to health care. JAMA. 1995;274:305–311. [PubMed] [Google Scholar]
- 17.Pappas G, Hadden WC, Kozak LJ, Fisher GF. Potentially avoidable hospitalizations: inequalities in rates between US socioeconomic groups. Am J Public Health. 1997;87:811–816. doi: 10.2105/ajph.87.5.811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weissman JS, Gatsonis C, Epstein AM. Rates of avoidable hospitalization by insurance status in Massachusetts and Maryland. JAMA. 1992;268:2388–2394. [PubMed] [Google Scholar]
- 19.Billings J, Zeitel L, Lukomnik J, Carey TS, Blank AE, Newman L. Impact of socioeconomic status on hospital use in New York City. Health Aff (Millwood) 1993;12:162–173. doi: 10.1377/hlthaff.12.1.162. [DOI] [PubMed] [Google Scholar]
- 20.Parker JD, Schoendorf KC. Variation in hospital discharges for ambulatory care-sensitive conditions among children. Pediatrics. 2000;106:942–948. [PubMed] [Google Scholar]
- 21.Parchman ML, Culler SD. Preventable hospitalizations in primary care shortage areas. An analysis of vulnerable Medicare beneficiaries. Arch Fam Med. 1999;8:487–491. doi: 10.1001/archfami.8.6.487. [DOI] [PubMed] [Google Scholar]
- 22.Blustein J, Hanson K, Shea S. Preventable hospitalizations and socioeconomic status. Health Aff (Millwood) 1998;17:177–189. doi: 10.1377/hlthaff.17.2.177. [DOI] [PubMed] [Google Scholar]
- 23.Roos LL, Walld R, Uhanova J, Bond R. Physician visits, hospitalizations, and socioeconomic status: ambulatory care sensitive conditions in a Canadian setting. Health Serv Res. 2005;40:1167–1185. doi: 10.1111/j.1475-6773.2005.00407.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lin H-C, Huang C-C, Chen S-F, Chen Y-H. Increased risk of avoidable hospitalization among patients with schizophrenia. Can J Psychiatry. 2011;56:171–178. doi: 10.1177/070674371105600307. [DOI] [PubMed] [Google Scholar]
- 25.Li Y, Glance LG, Cai X, Mukamel DB. Mental illness and hospitalization for ambulatory care sensitive medical conditions. Med Care. 2008;46:1249–1256. doi: 10.1097/MLR.0b013e31817e188c. [DOI] [PubMed] [Google Scholar]
- 26.Mai Q, Holman CDAJ, Sanfilippo FM, Emery JD. The impact of mental illness on potentially preventable hospitalisations: a population-based cohort study. BMC Psychiatry. 2011;11:163. doi: 10.1186/1471-244X-11-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cahoon EK, McGinty EE, Ford DE, Daumit GL. Schizophrenia and potentially preventable hospitalizations in the United States: a retrospective cross-sectional study. BMC Psychiatry. 2013;13:37. doi: 10.1186/1471-244X-13-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Goldberg M, Leclerc A, Bonenfant S, et al. Cohort profile: the GAZEL Cohort Study. Int J Epidemiol. 2007;36:32–39. doi: 10.1093/ije/dyl247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goldberg M, Chastang JF, Zins M, Niedhammer I, Leclerc A. Health problems were the strongest predictors of attrition during follow-up of the GAZEL cohort. J Clin Epidemiol. 2006;59:1213–1221. doi: 10.1016/j.jclinepi.2006.02.020. [DOI] [PubMed] [Google Scholar]
- 30.Vahtera J, Westerlund H, Ferrie JE, et al. All-cause and diagnosis-specific sickness absence as a predictor of sustained suboptimal health: a 14-year follow-up in the GAZEL cohort. J Epidemiol Community Health. 2010;64:311–317. doi: 10.1136/jech.2008.083923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ferrie JE, Vahtera J, Kivimäki M, et al. Diagnosis-specific sickness absence and all-cause mortality in the GAZEL study. J Epidemiol Community Health. 2009;63:50–55. doi: 10.1136/jech.2008.074369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Allonier C, Chevalier A, Zins M, et al. Anxiety or depressive disorders and risk of ischaemic heart disease among French power company employees. Int J Epidemiol. 2004;33:779–786. doi: 10.1093/ije/dyh077. [DOI] [PubMed] [Google Scholar]
- 33.Melchior M, Ferrie JE, Alexanderson K, et al. Does sickness absence due to psychiatric disorder predict cause-specific mortality? A 16-year follow-up of the GAZEL occupational cohort study. Am J Epidemiol. 2010;172:700–707. doi: 10.1093/aje/kwq186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Head J, Ferrie JE, Alexanderson K, et al. Diagnosis-specific sickness absence as a predictor of mortality: the Whitehall II prospective cohort study. BMJ. 2008;337:a1469. doi: 10.1136/bmj.a1469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lawless JF. Negative binomial and mixed Poisson regression. Can J Stat. 1987;15:209–225. [Google Scholar]
- 36.Bjorkenstam E, Ljung R, Burstrom B, Mittendorfer-Rutz E, Hallgvist J, Weitoft GR. Quality of medical care and excess mortality in psychiatric patients – a nationwide register-based study in Sweden. BMJ Open. 2012;2:e000778. doi: 10.1136/bmjopen-2011-000778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kopp M, Fleischhacker WW, Sturz K, Ruedl G, Kumnig M, Rumpold G. Poor health behaviour and reduced quality of life of people treated with psychotropic drugs. Hum Psychopharmacol. 2011;26:161–167. doi: 10.1002/hup.1190. [DOI] [PubMed] [Google Scholar]
- 38.Mitchell AJ, Lawrence D. Revascularisation and mortality rates following acute coronary syndromes in people with severe mental illness: comparative meta-analysis. Br J Psychiatry. 2011;198:434–441. doi: 10.1192/bjp.bp.109.076950. [DOI] [PubMed] [Google Scholar]
- 39.de Leon J, Tracy J, McCann E, McGrory A, Diaz FJ. Schizophrenia and tobacco smoking: a replication study in another US psychiatric hospital. Schizophr Res. 2002;56:55–65. doi: 10.1016/s0920-9964(01)00192-x. [DOI] [PubMed] [Google Scholar]
- 40.le Port A, Gueguen A, Kesse-Guyot E, et al. Association between dietary patterns and depressive symptoms over time: a 10-year follow-up study of the GAZEL cohort. PLoS ONE. 2012;7:e51593. doi: 10.1371/journal.pone.0051593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ströhle A, Höfler M, Pfister H, et al. Physical activity and prevalence and incidence of mental disorders in adolescents and young adults. Psychol Med. 2007;37:1657–1666. doi: 10.1017/S003329170700089X. [DOI] [PubMed] [Google Scholar]
- 42.Azevedo Da Silva M, Singh-Manoux A, Brunner EJ, et al. Bidirectional association between physical activity and symptoms of anxiety and depression: the Whitehall II study. Eur J Epidemiol. 2012;27:537–546. doi: 10.1007/s10654-012-9692-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Limosin F, Gasquet I, Leguay D, Azorin JM, Rouillon F. Body mass index and prevalence of obesity in a French cohort of patients with schizophrenia. Acta Psychiatr Scand. 2008;118:19–25. doi: 10.1111/j.1600-0447.2008.01208.x. [DOI] [PubMed] [Google Scholar]
- 44.Kivimäki M, Lawlor DA, Singh-Manoux A, et al. Common mental disorder and obesity: insight from four repeat measures over 19 years: prospective Whitehall II cohort study. BMJ. 2009;339:b3765. doi: 10.1136/bmj.b3765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McIntyre RS, Konarski JZ, Misener VL, Kennedy SH. Bipolar disorder and diabetes mellitus: epidemiology, etiology, and treatment implications. Ann Clin Psychiatry. 2005;17:83–93. doi: 10.1080/10401230590932380. [DOI] [PubMed] [Google Scholar]
- 46.Forsythe AB, Griffiths B, Reiff S. Comparison of utilization of medical services by alcoholics and non-alcoholics. Am J Public Health. 1982;72:600–602. doi: 10.2105/ajph.72.6.600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kisely S, Crowe E, Lawrence D. Cancer-related mortality in people with mental illness. JAMA Psychiatry. 2013;70:209–217. doi: 10.1001/jamapsychiatry.2013.278. [DOI] [PubMed] [Google Scholar]
- 48.Dalton SO, Mellemkjaer L, Thomassen L, Mortensen PB, Johansen C. Risk for cancer in a cohort of patients hospitalized for schizophrenia in Denmark, 1969–1993. Schizophr Res. 2005;75:315–324. doi: 10.1016/j.schres.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 49.Goldberg M, Chastang JF, Leclerc A, et al. Socioeconomic, demographic, occupational, and health factors associated with participation in a long-term epidemiologic survey: a prospective study of the French GAZEL cohort and its target population. Am J Epidemiol. 2001;154:373–384. doi: 10.1093/aje/154.4.373. [DOI] [PubMed] [Google Scholar]
- 50.Kehoe R, Wu SY, Leske MC, Chylack LT., Jr Comparing self-reported and physician-reported medical history. Am J Epidemiol. 1994;139:813–818. doi: 10.1093/oxfordjournals.aje.a117078. [DOI] [PubMed] [Google Scholar]
- 51.Haapanen N, Miilunpalo S, Pasanen M, Oja P, Vuori I. Agreement between questionnaire data and medical records of chronic diseases in middle-aged and elderly Finnish men and women. Am J Epidemiol. 1997;145:762–769. doi: 10.1093/aje/145.8.762. [DOI] [PubMed] [Google Scholar]
- 52.Rahman A, Gibney L, Person SD, et al. Validity of self-reports of reasons for hospitalization by young adults and risk factors for discordance with medical records: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Am J Epidemiol. 2005;162:491–498. doi: 10.1093/aje/kwi215. [DOI] [PubMed] [Google Scholar]


