Abstract
Introduction
The indications for a total pancreatectomy (TP), its peri-operative management, provision of pancreatic surgical services and medical treatment of the inherent exo- and endocrine deficient states have all changed considerably over recent decades. The effects of these upon the incidence, indications for and outcomes of TP are unclear. Patients undergoing TP at a single institution over a quarter of a century were reviewed to try to address these issues.
Methods
Data on patients who underwent elective (el-) and emergency TP (em-TP) between 1987 and 2013 were reviewed. Patient demographics, indications, intra-operative details, peri-operative management and long-term outcomes were analysed. Absolute numbers of TP were reported relative to partial pancreatectomy rates.
Results
In total, 136 patients underwent TP [98 (72.1%) el-TP; 38 (27.9%) em-TP]. There was a significant change in indication for el-TP with it increasingly performed for (an intraductal papillary mucinous neoplasm (IPMN) and renal cell metastases whereas there was a decrease in the number of el-TP performed for chronic pancreatitis (P = 0.025). The relative rates of el-TP, however, did not change significantly across the study period (P = 0.225). The median length of stay after el-TP decreased from 19 days pre-1997 to 12 days post-1997 (P = 0.009). The relative use of em-TP declined by 0.28 percentage points per year [P = 0.018; 95% confidence interval (CI): 0.04–0.41].
Conclusions
The indications for el-TP have changed; it is being performed more frequently although the proportion relative to other pancreatic resections has not changed. A decrease in the rate of em-TP is likely to reflect improved peri-operative management of a pancreatic fistula and its complications after a pancreaticoduodenectomy.
Introduction
Enthusiasm for a total pancreatectomy (TP) has varied with time. Early interest in elective TP (el-TP) as a potential solution to the high rates of tumour recurrence after a partial pancreatectomy waned with a clearer understanding of the tumour biology of pancreatic adenocarcinoma.1 More recently, however, interest in el-TP has been replaced by alternative indications for the procedure, with increasing recognition of multifocal parenchymal diseases including intraductal papillary mucinous neoplasms (IPMNs), multifocal renal cell metastases, multifocal neuroendocrine tumours (NET) and inherited neoplastic diseases, including multiple endocrine neoplasia (MEN)1, prompting clinicians to re-evaluate the role of el-TP.2,3 A further indication for TP is in the emergency setting (em-TP), where a completion pancreatectomy can be performed as a method of sepsis control in cases of a post-operative pancreatic fistula (POPF) after a partial pancreatectomy. Improvements in cross-sectional radiology and the ability to perform percutaneous drainage of intra-abdominal collections, however, have provided alternative methods of sepsis control in this setting.
The post operative exo- and endocrine deficient states have always tempered enthusiasm for TP. The diabetic state has been considered so severe it has been termed ‘brittle diabetes’. However, in recent years, improvements in insulin regimens and specialist nurse-led diabetic care have dramatically improved diabetic outcomes post TP.4–8 There is now debate over the actual severity of the diabetic state, with several groups reporting equivalent HbA1c levels between type 1 diabetics and TP patients.4–8
The development of high-quality enzyme replacement formulations has also improved morbidity from exocrine insufficiency.
Given the changing indications for elective surgery, an evolution in the understanding of POPF and sepsis control and medical management of the inherent exo- and endocrine deficient states after TP, the present study aimed to review indications and trends in both el-TP and em-TP at a single institution with a dedicated pancreatic surgical service over a quarter of a century.
Patients and methods
This study considers two distinct scenarios, el-TP and em-TP. Both indications are considered in this study to contrast potential enthusiasm for differing indications for TP within the same institution over a prolonged period to review trends in managing various pancreatic diseases and complications.
Data collection
All patients undergoing a partial or total pancreatic resection [TP, distal pancreatectomy (DP) and pancreaticoduodenectomy (PD)] between January 1987 and December 2013 were identified from a prospectively maintained institutional database. El-TP included single-stage planned elective or single-stage unplanned elective TP where an intra-operative decision to perform TP and not a partial pancreatectomy was made. Patients who had previously undergone a partial pancreatectomy with a subsequent elective completion pancreatectomy were also included in the el-TP group. Em-TP was defined as a completion pancreatectomy performed after a previous partial pancreatectomy in order to control or treat sepsis. The rates of partial pancreatic resection were observed and compared with the rates of el-TP and em-TP to understand changes in the proportion of these operations over time.
Data on patient demographics, indications for surgery, pathology, peri-operative complications and long-term outcomes were retrieved from the database for all TP patients. Data accuracy was confirmed by retrospective review of patient records.
Follow-up of patients consisted of clinical review every 4–6 months for 2 years with at least an annual follow-up until 5 years. Follow-up aimed to assess evidence of tumour recurrence and survival. Sequelae of endocrine insufficiency and post-operative quality of life have been reported elsewhere.9
Statistical analysis
The relationships between pre-surgical factors, and the outcomes of overall survival, complication rates and lengths of hospital stay were assessed separately for patients undergoing el- and em-TP.
Survival analysis was performed using Kaplan–Meier survival curves, with Log-Rank significance tests. Complication rates were compared across factors using Fisher's exact test. As the distribution of lengths of hospital stay was highly skewed, a non-parametric approach to analysis was employed. The Mann–Whitney and Kruskal–Wallis tests were used, depending on the number of groups be compared, and data were summarized using medians and quartiles.
The trends over time in frequency and relative rates of pancreatic resection were then compared using linear regression models. The year number was included as the independent variable, and either the number of operations, or relative proportion of operations entered as the dependent variable. When working with proportions, the denominator was set as a weighting variable, in order to give greater influence to percentages based on a greater number of patients. The resulting coefficients represented the year-on-year increase in operations or the percentage point change in proportions, respectively.
All analyses were performed using IBM SPSS 19 (IBM Corp., Armonk, NY, USA), with P < 0.05 indicative of statistical significance. A medical statistician (J.H.) provided advice on study design and with data analysis.
Results
Study population
Some 1609 pancreatic resections were performed comprising of 1232 PD (76.5%), 241 DP (15.0%) and 136 TP (8.4%). Of the TP group 98 were el-TP (72.1%) and 38 em-TP (27.9%).
Elective TP
In total, 80 (82%) patients underwent a single-stage planned el-TP, 11 (11%) a single-stage unplanned el-TP, and a 7 (7%) elective completion pancreatectomy. An intra-operative decision was made to convert from a PD to a TP in 11 patients owing to evidence of tumour deposits (macroscopic or microscopic) beyond the neck of the pancreas (6), need for extensive venous reconstruction (3), inadvertent arterial damage (1), or findings of a soft pancreas deemed unsuitable for anastomosis (1).
The median age of patients undergoing el-TP was 63 years (range 18–84) and 53/98 (54.1%) were male. El-TP was performed for adenocarcinoma (45; 46%), NET (8; 8%), chronic pancreatitis (18; 18%), trauma (1; 1%), IPMN (12; 12%), renal cell metastases (10; 10%), benign lesions (3; 3%) and other malignant lesions (1; 1%).
The median follow-up was 8.4 years, and at last follow-up, 61 (62.2%) patients had died. Post-operative mortality did not change significantly over time (P = 0.763). A total of 12 patients (KM estimate 12.5%) died within 90 days of surgery owing to abdominal sepsis (4), pneumonia (4), myocardial infarction (1), intracerebral haemorrhage (1), hypoglycaemic cerebral injury (1) and Clostridium difficile colitis (1).
The median length of stay was 13 days [interquartile range (IQR) 9–39 days] and decreased over time from 19 days pre-1997 to 12 days post-2006 (P = 0.009). Post-operative complications occurred in 45/98 (46.0%) patients. Complication rates were not significantly associated with pathology (P = 0.084), patient demographics (gender: P = 1.000, age: P = 0.135) or year of surgery (P = 0.851). The commonest complication was pulmonary sepsis (14; 14%), others included post-operative haemorrhage (5; 5%), biliary obstruction (1; 1%), bile leak (1; 1%) and thrombosis of a reconstructed portal vein in one patient from three who underwent venous reconstruction.
Emergency TP
In total, 38 patients underwent em-TP after a prior pancreaticoduodenectomy. The median age was 63 years (range 17–81), and 25 patients were male and 13 female. A total of 20 patients died within 90 days of the operation (KM estimate 47.4%), and there was no significant change in survival over time (P = 0.537).
The median length of stay after em-TP was 27 days (IQR 13–48) and this did not vary significantly across the study period (P = 0.443). Post-operative complications occurred in 30/38 patients although this rate reflects morbidity incurred from the prior pancreaticoduodenectomy which necessitated the em-TP.
The year of surgery and underlying pathology were not found to be significantly associated with 90-day survival, complication rates or length of stay after univariate analysis. However, older patients were shown to have significantly lower survival rates (P = 0.025), higher complication rates (P = 0.042) and longer inpatient stays (P = 0.018).
Comparison of outcomes after elective and emergency TP
Patients undergoing em-TP were more likely to suffer complications (46% versus 79%) (P = 0.001) and have a longer hospital stay [27 (IQR: 13–48) versus 13 (9–19) days, P < 0.001] than el-TP patients. Emergency TP patients also had significantly shorter survival (P = 0.003), with a Kaplan–Meier estimated 5-year survival of 15.5%, compared with 36.7% in el-TP.
Changes in trends of TP over time
Absolute annual numbers of TP (elective and emergency) increased steadily across the study period, by a mean of 0.28 per year (95% CI: 0.16–0.41, P < 0.001) (Fig. 1a). The number of partial pancreatic resections also increased, and at a faster rate of 4.3 per year (95% CI: 3.5–5.0, P < 0.001). The rise in total TP was predominantly due to the increase in the number of elective patients of 0.25 per year (95% CI: 0.14–0.35, P < 0.001) (Fig. 1b). The number of emergency procedures performed annually did not change significantly over the period (coefficient: 0.04 per year, 95% CI: −0.02–0.01, P = 0.227).
Figure 1.
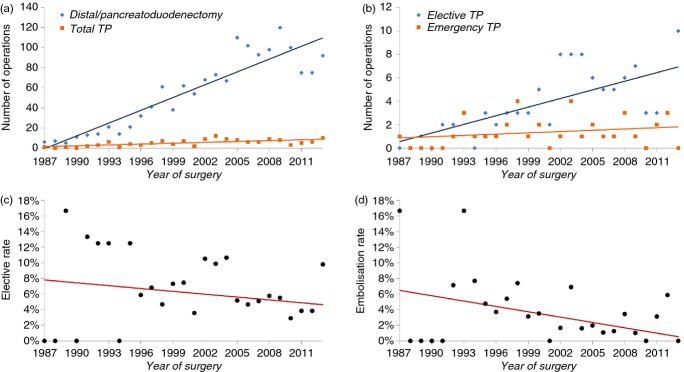
(a) Annual numbers of pancreatic resections. The total of total pancreatectomies (TP) includes both elective and emergency cases. (b) Annual numbers of elective and emergency TP. (c) Elective TP as a proportion of partial resections [pancreatoduodenectomy/ distal pancreatectomy (DP)]. (d) Emergency CP as a proportion of pancreatoduodenectomy
Figure 1c illustrates that the rate of el-TP as a proportion of partial pancreatic resections showed no significant trend across the study period (P = 0.225). However, em-TP, as a proportion of PD (Fig. 1d) demonstrated a significant decline (P = 0.018). This was equivalent to a reduction of 0.28 percentage points per year (95% CI: 0.04–0.41).
The surgical drainage rate was found to have significantly declined over the period of the study (P = 0.002), with a reduction of 0.4 percentage points per year (95% CI: 0.2–0.7) (Fig. 2a). Radiological drainage and embolization rates were negligible for the majority of the study period (Fig. 2b,c). Hence, the analysis was split into two eras: 1987–2004 and 2005–2013. From 2005 onwards, both rates were found to increase significantly, by 2.0 percentage points per year (95% CI: 0.8–3.1, P = 0.003) for radiological drainage, and 0.8 percentage points per year (95% CI: 0.2–1.5, P = 0.013) for embolization.
Figure 2.
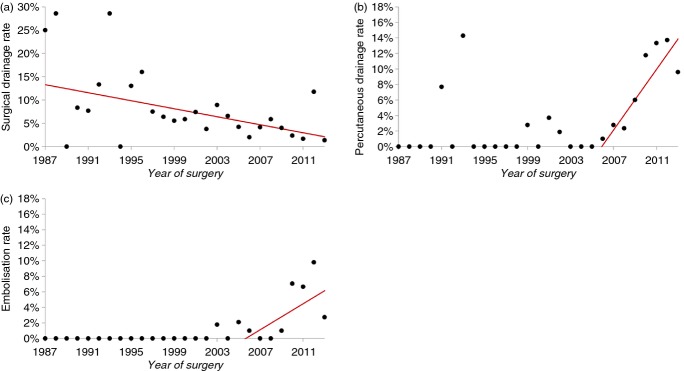
(a) Annual rates of (a) surgical drainage, (b) percutaneous drainage and (c) embolization relative to the number of patients undergoing a pancreaticoduodenectomy across the study period
The underlying pathology amongst patients undergoing TP changed significantly across the study period (P = 0.025) with an increase in el-TP performed pre-1997 and post-2006, respectively, for IPMN, NET and renal cell metastases and a decrease in chronic pancreatitis (Fig. 3).
Figure 3.
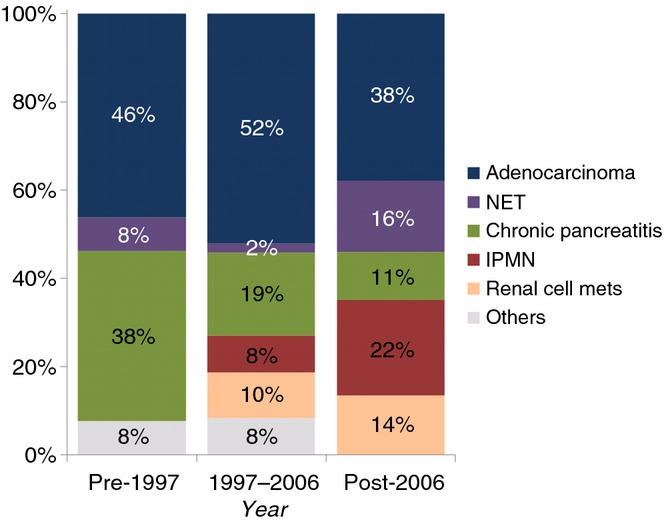
Trends in indications for elective total pancreatectomy (TP). The distribution of pathology changed significantly across the study period P = 0.025 (Fisher's Exact test)
Discussion
This study reports trends in indications and outcomes for patients undergoing el- or em-TP at a single centre with a dedicated pancreatic surgical team over a quarter of a century. El-TP increased in absolute terms across the study period although did not change significantly, relative to partial pancreatectomy rates. A marked change was observed in indications for el-TP owing to increased recognition of multi-focal parenchymal diseases including IPMN, NET and renal cell metastases, and a decline in the role of el-TP in chronic pancreatitis.
International consensus guidelines for the management of IPMN recommend resection for main duct disease with clearance of all high-grade dysplasia (HGD).10 As main duct IPMN may be associated with extensive multifocal HGD, the role of el-TP in this setting is increasingly recognized. The decision to perform el-TP may be made pre-operatively based on imaging (EUS, MRI, CT), or intra-operatively in patients with positive margins on frozen section. In the present study, the existence of main duct IPMN accounted for 22% of el-TP performed since 2007, a significant increase on previous years (Fig. 3).
Murphy et al. reported increasing nationwide utilization of el-TP in the US between 1998 and 2006.11 Although trends in indications were not reported, the authors concluded the rise in el-TP was a consequence of increased diagnosis of diffuse neoplastic diseases, particularly IPMN, and improved peri-operative outcomes.
Early post-operative morbidity after el-TP remains high. In the present study, 46% of patients developed a complication after el-TP. This is consistent with rates of 32% to 54% reported elsewhere.1,5,7,12,13 Ninety-day mortality across the study period was 12.5% which is comparable to a US national audit of el-TP, which reported an in-hospital mortality of 8.5% between 1998 and 2006. The 90-day mortality since 2006 in the present study was 8.8%.
The severity of post TP diabetes, and existence of ‘brittle diabetes’ as a particularly difficult to control diabetic state, is an area of debate. Emerging evidence questions the existence of ‘brittle diabetes’ after TP. Case-matched analysis of patients who have undergone el-TP with patients who have type 1 diabetes has demonstrated equivalent diabetes-specific outcomes using a diabetes-specific quality of life tool and equivalent episodes of hypoglycaemia, HbA1c values and mortality from diabetic complications. Several recent prospective series have supported these findings.6,7,9,14,15 In spite of these reports, the potential morbidity associated with endocrine deficiency must not be underestimated and specialist diabetic input should be sought in the early post-operative period after TP. Importantly, there are several reports of post TP deaths owing to hypoglycaemia.7,8 In previous studies from this institution no such deaths were reported,9 although more recently 1 patient died 53 days after el-TP from a cardiac arrest precipitated by hypoglycaemia. This patient had suffered several post-operative hypoglycaemic episodes in soite of specialist diabetic input. After TP the onset of diabetes is immediate; the authors presume this develops with more rapidity than the onset in patients with type 1 diabetes. Whether the presumed less rapid onset of diabetes allows patients with type 1 diabetes to adjust to diabetic life and risks of hypoglycaemia more safely than those patients undergoing TP is speculation. What is clear is that patients who undergo TP must have exposure to specialist diabetic team input. Ideally this should begin prior to the procedure when possible.
Outcomes of em-TP were significantly worse than for el-TP and were consistent with other recent series. Muller et al. reported a peri-operative mortality of 39% after em-TP. In addition, the high reported rate of morbidity in the em-TP group in the present study demonstrates the poor outcomes associated with salvage completion pancreatectomy in the setting of severe abdominal sepsis or haemorrhage after a pancreaticoduodenectomy. The significant decline in the use of em-TP relative to a pancreaticoduodenectomy reflects a shift in the management of POPF and post-operative haemorrhage, with radiological drainage and arterial embolization now readily available and preferred to re-laparotomy (Fig. 2).16,17
The present study has several limitations. The prospectively maintained database did not include complete data on patient comorbidity or other measures of pre-operative performance status meaning outcomes could not be analysed with respect to these variables. In addition, long-term sequelae of exocrine dysfunction and the success of enzyme replacement therapy have not been established, although diabetic and quality of life outcomes have been evaluated, and are reported elsewhere.9 Finally, although this study represents a large single-centre cohort, the value of multivariate analysis was restricted by sample size.
Conclusion
The role of em-TP is declining in favour of alternative strategies for the management of POPF and secondary haemorrhage. Whilst the rate of el-TP relative to partial pancreatic resections is relatively static, the indications for el-TP are changing and there is evidence that short- and long-term outcomes are improving. Although post-operative morbidity remains substantial, el-TP should be considered an established treatment option for multifocal neoplastic lesions with an acceptable in-hospital mortality. An understanding of the post-operative exo- and endocrine deficient states is essential and careful patient selection and counselling should be undertaken whenever el-TP is considered.
Conflicts of interest
None declared.
References
- Karpoff HM, Klimstra DS, Brennan MF, Conlon KC. Results of total pancreatectomy for adenocarcinoma of the pancreas. Arch Surg. 2001;136:44–47. doi: 10.1001/archsurg.136.1.44. [DOI] [PubMed] [Google Scholar]
- Bartsch DK. Familial pancreatic cancer. Br J Surg. 2003;90:386–387. doi: 10.1002/bjs.4127. [DOI] [PubMed] [Google Scholar]
- Stauffer JA, Nguyen JH, Heckman MG, Grewal MS, Dougherty M, Gill KR, et al. Patient outcomes after total pancreatectomy: a single centre contemporary experience. HPB. 2009;11:483–492. doi: 10.1111/j.1477-2574.2009.00077.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casadei R, Monari F, Buscemi S, Laterza M, Ricci C, Rega D, et al. Total pancreatectomy: indications, operative technique, and results: a single centre experience and review of literature. Updat Surg. 2010;62:41–46. doi: 10.1007/s13304-010-0005-z. [DOI] [PubMed] [Google Scholar]
- Muller MW, Friess H, Kleeff J, Dahmen R, Wagner M, Hinz U, et al. Is there still a role for total pancreatectomy? Ann Surg. 2007;246:966–974. doi: 10.1097/SLA.0b013e31815c2ca3. [DOI] [PubMed] [Google Scholar]
- Jethwa P, Sodergren M, Lala A, Webber J, Buckels JA, Bramhall SR, et al. Diabetic control after total pancreatectomy. Dig Liver Dis. 2006;38:415–419. doi: 10.1016/j.dld.2006.01.022. [DOI] [PubMed] [Google Scholar]
- Billings BJ, Christein JD, Harmsen WS, Harrington JR, Chari ST, Que FG, et al. Quality-of-life after total pancreatectomy: is it really that bad on long-term follow-up? J Gastrointest Surg. 2005;9:1059–1066. doi: 10.1016/j.gassur.2005.05.014. ; discussion 1066-7. [DOI] [PubMed] [Google Scholar]
- Barbier L, Jamal W, Dokmak S, Aussilhou B, Corcos O, Ruszniewski P, et al. Impact of total pancreatectomy: short- and long-term assessment. HPB. 2013;15:882–892. doi: 10.1111/hpb.12054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts KJ, Blanco G, Webber J, Marudanayagam R, Sutcliffe RP, Muiesan P, et al. How severe is diabetes after total pancreatectomy? A case-matched analysis. HPB. 2014;16:814–821. doi: 10.1111/hpb.12203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanaka M, Fernandez-del Castillo C, Adsay V, et al. International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology. 2012;12:183–197. doi: 10.1016/j.pan.2012.04.004. [DOI] [PubMed] [Google Scholar]
- Murphy MM, Knaus WJ, 2nd, Ng SC, Hill JS, McPhee JT, Shah SA, et al. Total pancreatectomy: a national study. HPB. 2009;11:476–482. doi: 10.1111/j.1477-2574.2009.00076.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crippa S, Tamburrino D, Partelli S, Salvia R, Germenia S, Bassi C, et al. Total pancreatectomy: indications, different timing, and perioperative and long-term outcomes. Surgery. 2011;149:79–86. doi: 10.1016/j.surg.2010.04.007. [DOI] [PubMed] [Google Scholar]
- Schmidt CM, Glant J, Winter JM, Kennard J, Dixon J, Zhao Q, et al. Total pancreatectomy (R0 resection) improves survival over subtotal pancreatectomy in isolated neck margin positive pancreatic adenocarcinoma. Surgery. 2007;142:572–578. doi: 10.1016/j.surg.2007.07.016. ; discussion 578–80. [DOI] [PubMed] [Google Scholar]
- Muller-Gerbes D, Aymaz S, Dormann A. Diagnostic and therapeutic management of Barrett's esophagus. Dtsch Med Wochenschr. 2011;136:1796–1800. doi: 10.1055/s-0031-1286105. [DOI] [PubMed] [Google Scholar]
- Heidt DG, Burant C, Simeone DM. Total pancreatectomy: indications, operative technique, and postoperative sequelae. J Gastrointest Surg. 2007;11:209–216. doi: 10.1007/s11605-006-0025-7. [DOI] [PubMed] [Google Scholar]
- Haddad LB, Scatton O, Randone B, Andraus W, Massault PP, Dousset B, et al. Pancreatic fistula after pancreaticoduodenectomy: the conservative treatment of choice. HPB. 2009;11:203–209. doi: 10.1111/j.1477-2574.2009.00007.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedrazzoli S, Liessi G, Pasquali C, Ragazzi R, Berselli M, Sperti C. Postoperative pancreatic fistulas: preventing severe complications and reducing reoperation and mortality rate. Ann Surg. 2009;249:97–104. doi: 10.1097/SLA.0b013e31819274fe. [DOI] [PubMed] [Google Scholar]


