Abstract
This paper introduces a scalable “climate health justice” model for assessing and projecting incidence, treatment costs, and sociospatial disparities for diseases with well-documented climate change linkages. The model is designed to employ low-cost secondary data, and it is rooted in a perspective that merges normative environmental justice concerns with theoretical grounding in health inequalities. Since the model employs International Classification of Diseases, Ninth Revision Clinical Modification (ICD-9-CM) disease codes, it is transferable to other contexts, appropriate for use across spatial scales, and suitable for comparative analyses. We demonstrate the utility of the model through analysis of 2008–2010 hospitalization discharge data at state and county levels in Texas (USA). We identified several disease categories (i.e., cardiovascular, gastrointestinal, heat-related, and respiratory) associated with climate change, and then selected corresponding ICD-9 codes with the highest hospitalization counts for further analyses. Selected diseases include ischemic heart disease, diarrhea, heat exhaustion/cramps/stroke/syncope, and asthma. Cardiovascular disease ranked first among the general categories of diseases for age-adjusted hospital admission rate (5286.37 per 100,000). In terms of specific selected diseases (per 100,000 population), asthma ranked first (517.51), followed by ischemic heart disease (195.20), diarrhea (75.35), and heat exhaustion/cramps/stroke/syncope (7.81). Charges associated with the selected diseases over the 3-year period amounted to US$5.6 billion. Blacks were disproportionately burdened by the selected diseases in comparison to non-Hispanic whites, while Hispanics were not. Spatial distributions of the selected disease rates revealed geographic zones of disproportionate risk. Based upon a downscaled regional climate-change projection model, we estimate a >5% increase in the incidence and treatment costs of asthma attributable to climate change between the baseline and 2040–2050 in Texas. Additionally, the inequalities described here will be accentuated, with blacks facing amplified health disparities in the future. These predicted trends raise both intergenerational and distributional climate health justice concerns.
Keywords: Texas, United States, disease mapping, climate change, climate gap, climate health justice, heath disparities, health inequalities, health surveillance
Introduction
The relationship between climate change and health is complex and there remains uncertainty regarding specific health impacts of climate change on human populations (Ebi, Mills, Smith, & Grambsch, 2006; Hajat, O’Connor, & Kosatsky, 2010; McMichael, Woodruff, & Hales, 2006; Portier et al., 2010). Predictive modeling is difficult due to limited availability of data and confounding factors such as individual behavior, human physiology, and social institutions (Brown, Craddock, & Ingram, 2012). Nonetheless, there is scholarly consensus that climate change presents serious risks to human health (Green, Basu, Malig, Broadwin, Kim, et al., 2010; Portier et al., 2010). This understanding stems in part from two decades of retrospective time-series epidemiological studies, which have examined daily changes in weather parameters and associated morbidities and mortality (Turner, Barnett, Connell, & Tong, 2012). For example, researchers have demonstrated that there is a positive relationship between daily increases in temperature and cardiovascular hospital admissions (Ebi et al., 2004; Kovats et al., 2004; 2004; Schwartz et al., 2004), as well as respiratory hospital admissions (Michelozzi et al., 2009; Lin et al., 2009). Overall, a review of the climate change/health literature reveals that cardiovascular, gastrointestinal, heat, respiratory, vector-borne, and water-borne diseases are likely to be associated with climate change (Hales et al., 2003; Portier et al., 2010) (see Table 1).
Table 1.
Climate Change-Relevant Disease Category and Disease Impacts
| Disease Category* | Disease Impacts | References |
|---|---|---|
| Cardiovascular | Cardiovascular diseases hospital admissions increase during extreme heat waves and during peaks in particulate matter. |
Bosello, Roson, & Tol, 2006; Brown, Craddock, & Ingram, 2012; Costello et al., 2009; Hajat, O’Connor, & Kosatsky, 2010; Haines & Patz, 2004; Hales, Edwards, & Kovats, 2003; Harlan & Ruddell, 2011; IPCC, 2007; Portier et al., 2010 |
| Heat | Extreme heat events are a leading cause of weather-related morbidity and mortality in North America. Prolonged heat exposure causes a variety of heat-related diseases, such as heat stroke, heat syncope, and heat exhaustion. |
Costello et al., 2009; Cueto-Garcia, Martinez-Tejeda, & Ostos-Jauregui, 2010; Luber & McGeehin, 2008; Portier et al., 2010 |
| Gastrointestinal | Diarrheal episodes in North America increase because of sewage overflow due to flooding. |
Bosello, Roson, & Tol, 2006; Costello et al., 2009; Haines & Patz, 2004; Hales, Edwards, & Kovats, 2003; Peterson, Zhang, Brunet-India, & Vázquez-Aguirre, 2008; Portier et al., 2010 |
| Respiratory | An increase in respiratory diseases hospital admissions occur during periods of higher temperatures. Respiratory diseases are intensified by peak levels of air pollution due to changes in climate. Longer pollen seasons due to warming climates may also intensify suffering for those with conditions like allergic asthma. |
Bosello, Roson, & Tol, 2006; Comrie, 2007; Costello et al., 2009; Cueto-Garcia et al., 2010; Epstein, 2005; Haines & Patz, 2004; Kovats et al., 2006; Maantay & Becker, 2012; Portier et al., 2010; Shea, Truckner, Weber, & Peden, 2008 |
| Vector-borne | Vector-borne diseases increase due to increased temperatures, which create more suitable habitats for vectors. |
Bosello, Roson, & Tol, 2006; Brownstein, Holford, & Fish, 2005; Costello et al., 2009; Cromley & McLafferty, 2012; Epstein, 2005; Haines & Patz, 2004; Hales, Edwards, & Kovats, 2003; Khasnis & Nettleman, 2005; Portier et al., 2010 |
| Water-borne | Water-borne diseases are associated extreme rainfall events, which are expected to increase under climate change resulting in a contaminated water supply. |
Bosello, Roson, & Tol, 2006; Costello et al., 2009; Epstein, 2005; Haines & Patz, 2004; Hales, Edwards, & Kovats, 2003; Kovats et al., 2006; Portier et al., 2010 |
While important, the climate change/health literature suffers from several limitations. First, most studies examine impacts at a global scale (e.g., McMichael, Woodruff, & Hales, 2006), with far fewer fine-scale spatial analyses (Maantay & Becker, 2012). Second, analyses of social inequalities in the projected health effects of climate change have been largely missing from this literature (see Lin et al., 2012 for an exception). Third, even in the retrospective studies, mortality has been a primary focus as opposed to morbidity outcomes (see Ren & Tong, 2006; Knowlton et al., 2009; Madrigano, Mittleman, Baccarelli, Goldberg, Melly, et al., 2013 as exceptions). Fourth, there are few extant models for assessing and projecting spatial patterns, on a regional scale, of diseases with well-documented climate change linkages (see Lin et al., 2012 for an exception), and none that are sensitive to social disparities in disease outcomes.
The environmental justice and health inequalities literatures provide a basis for beginning to address these limitations. The environmental justice (EJ) literature has documented that poor and racial/ethnic minority groups often face disproportionate exposure to environmental hazards (Brown, 1995; Brulle & Pellow, 2006; Chakraborty, Maantay, & Brender, 2011; Mohai, Pellow, & Roberts 2009). Within that literature, a growing body of work on the “climate gap” is demonstrating that socially marginalized groups face unequal and disproportionate exposure to climate change-related hazards (Grineski et al., 2014; Grineski et al., 2012; Kersten, Morello-Frosch, Pastor, & Ramos, 2012; Morello-Frosch, Pastor, Sadd, Shonkoff, 2009; Pastor, Morello-Frosch, Sadd, & Scoggins, 2010; Shonkoff, Morello-Frosch, Pastor, & Sadd, 2009; Shonkoff, Morello-Frosch, Pastor, & Sadd, 2011). However, few if any scholars have merged normative environmental justice concerns with quantification of health impacts of climate change. This lack of overlap has limited the development of more robust, action-oriented understandings of the unequal health impacts of climate change.
Social scientists have long recognized that patterns of disease and death are shaped by social, economic, political, and cultural factors. Decades of health inequalities studies have demonstrated that persons of lower socioeconomic status (SES) and racial/ethnic minority status tend to have greater morbidity (Nazroo, 2003). These groups suffer from poorer health due to lower levels of education, higher rates of unemployment, less rewarding jobs, reduced access to medical care, and less actual and perceived control over life circumstances (Mirowsky, Ross, & Reynolds, 2000). Those with lower SES and racial/ethnic minorities have also been shown to be more sensitive to environmental exposures, like day-to-day variations in air pollution, than their more affluent and white non-Hispanic counterparts (Clougherty, 2011; Gwynn & Thurston, 2001; Hackbarth, Romley, & Goldman, 2011; O’Neil et al., 2003). Given this body of knowledge, it is surprising that social inequalities have been so underemphasized within the climate change health effects literature.
This paper introduces a scalable “climate health justice” model that addresses these limitations. This model is informed by the retrospective time-series literature on weather parameter/health relationships in that we are able to identify diseases likely to be impacted by warming temperatures. Rooted in a perspective that merges normative environmental justice concerns with theoretical grounding in health inequalities, the model is designed to support the use of low-cost secondary data for assessing and projecting incidence, treatment costs, and sociospatial disparities for diseases with well-documented climate change linkages. Since the model employs International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes, it is transferable to other contexts, appropriate for use across a range of spatial scales, and suitable for comparative analyses of climate health justice.
We demonstrate the utility of the model through analysis of 2008–2010 hospitalization discharge data at state and county levels in Texas (USA). To preview the analysis, we first identified several disease categories with well-established climate change linkages, and then selected corresponding ICD-9-CM disease codes with the highest hospitalization counts for further analyses. Next, we employed direct age-adjustment protocols to “control” for the effect of age (Friis & Sellers, 2014) because age structures in Texas vary significantly between counties based partly on differences in racial/ethnic composition, and because the diseases analyzed do not impact all age groups the same (e.g. ischemic heart disease is a disease of older age while asthma is more prevalent among children). We then employed the Wilcoxon signed-rank test and relative risk ratios to quantify impacts of the diseases in terms of hospital admissions and sociospatial disparities, and we used hospitalization discharge data to calculate direct dollar charges. Finally, we estimated future incidence, treatment costs, and injustices for social sub-groups for the time period of 2040–2050 using a climate change health impact projection from the available literature. The research questions we address are presented below.
Research Question 1. What are the numbers of hospitalization cases for climate change-relevant diseases in Texas from 2008–2010?
Research Question 2. What is the economic impact, based on hospitalization dollar charges, for climate change-relevant diseases in Texas from 2008–2010?
Research Question 3. What are the social and spatial distributional patterns of climate change-related diseases in Texas from 2008–2010? Are these diseases equally distributed across social groups and spatially across counties? If not, what specific social and spatial disparities in climate change-relevant diseases exist?
Research Question 4. What are predictions in terms of the incidence, treatment costs, and social disparities for hospitalizations due to asthma (a key climate change-related disease) for the time period of 2040–2050?
We acknowledge the complexity of the relationship between climate change and health. Our goal is not to present a model for quantifying the proportion of health impacts directly attributable to climate change. Instead, we offer a scalable climate health justice model for quantifying current and future impact of diseases that have been clearly established in the literature as linked to climate change, which can provide a basis for systematically clarifying and reducing the scope, costs, and uneven sociospatial effects of climate change on population health.
Methods
Data Source and Selected Diseases
The study area is Texas, a state with a population of 25,145,561 (US Census Bureau, 2010). While Texas covers 261,233 square miles (Texas Counties: Land Area, Texas Association of Counties, 2010), 89% of the population resides within metropolitan statistical areas (MSAs) that comprise only 25% of the state’s land area (US Census Bureau, 2010). Our analysis utilizes 2008–2010 state and county-level hospital admissions data reported in the Texas Hospital Inpatient Discharge Public Use Data File (PUDF). While we recognize that hospital admissions data only partially measure overall population morbidity (Kovats et al., 2006), they provide the most comprehensive information on patterns of diseases currently available statewide. The PUDF data were prepared by the Texas Health Care Information Council (THCIC). This patient-level dataset includes age; race; ethnicity; diagnosis codes (using the International Classification of Diseases, Ninth Revision, Clinical Modification or ICD-9-CM classification system) for primary, secondary and tertiary diseases; county of residence; payment source (e.g., insurance type); and financial charges associated with admission (among other variables) on a case-by-case basis.
To create the dataset, we first conducted a comprehensive review of the literature to identify disease categories (cardiovascular, gastrointestinal, heat, respiratory, vector-borne, and water-borne) that have well-documented links with climate change (Basu, 2009; Bosello, Roson, and Tol, 2006; Costello et al., 2009; Epstein, 2005; Haines & Patz, 2004; Hales et al., 2003; Portier et al., 2010). Then, we reviewed all ICD-9-CM codes in each category, removing those that were obviously due to factors unrelated to climate change (e.g., smoking, drug use, or occupation). For example, the respiratory disease “pneumonopathy” (ICD-9 code 504), which can occur during the cotton manufacturing process, was removed (ICD9Data.com, 2012). This produced a list of disease codes by category (see Table 2).
Table 2.
Specific Conditions Included in Each Category of Climate Change-Relevant Diseases Based on ICD-9-CM Codes
| Category | ICD-9-CM Code |
|---|---|
| Cardiovascular diseases | 306.2, 402, 402.0, 402.1, 402.9, 405, 405.0, 405.1, 405.9, 429.2, 429, 429.0, 429.1, 429.9, 414, 414.0, 414.2, 414.8, 414.9, 410, 410.0, 410.1, 410.2, 410.3, 410.4, 410.5, 410.6, 410.7, 410.8, 410.9 |
| Gastrointestinal disease | 787.91 |
| Heat-related diseases | 705.1, 992.0, 992.1, 992.2, 992.3, 992.4, 992.5 |
| Respiratory diseases | 416, 416.8, 416.9, 466, 466.0, 466.1, 466.11, 466.19, 491, 493, 493.0, 493.00, 493.01, 493.02, 493.1, 493.10, 493.11, 493.12, 493.2, 493.20, 493.21, 493.22, 493.8, 493.82, 493.9, 493.90, 493.91, 493.92, 514, 518.4 |
| Vector-borne diseases | 061, 066.4, 066.40, 066.41, 066.42, 066.49, 079.81, 084, 084.0, 084.1, 084.2, 084.3, 084.5, 084.9, 088.81 |
| Water-borne diseases | 001, 001.9, 007.4, 007.9, 009.2, 009.3, 564.5 |
The inclusion criterion for the study was being admitted to a hospital for one of the diseases in the six categories during the three-year study period (2008–2010; see Table 2). A patient was counted as having a disease if it was the principal, secondary, or tertiary diagnosis. We selected from three diagnoses because a patient may exhibit a variety of symptoms associated with multiple conditions upon hospital admittance. The inclusion of three diagnoses captures the multiple dimensions of morbidity that may affect the health status of an individual upon admission (e.g. an underlying chronic condition, as well as a heat-related diagnosis).
While the literature suggests that climate change-relevant diseases fall within six disease categories (i.e., cardiovascular, gastrointestinal, heat, respiratory, vector-borne, and water-borne), we eliminated vector-borne and water-borne diseases due to nearly zero counts of hospitalizations in Texas during 2008–2010. Even though there were relatively low counts of heat-related diseases, we included that category because there is a relatively high degree of certainty about their increased occurrence due to elevated temperatures associated with climate change (Brown et al., 2012). Thus, we report the incidence and economic burden of heat diseases in answer to research questions 1 and 2 but, due to small counts, we do not disaggregate heat disease data for analysis and spatial representation at the county level as per research question 3, nor do we project heat diseases into the future as per research question 4.
Of the 254 counties in the state of Texas, there were cases for 251 or 99% of the counties for cardiovascular diseases (3 non-reporting), 243 or 96% of the counties for gastrointestinal diseases (11 non-reporting), 169 or 67% counties for heat diseases (85 non-reporting), and 252 or 99% counties for respiratory diseases (2 non-reporting). Counties are non-reporting or “exempt” when they have a population less than 35,000, have only a military hospital, or are located in a non-urban county (based on US Census definitions) with a population of more than 35,000 but with fewer than 100 licensed hospital beds (Texas Health Care Information Council, 2010). Even with the exclusion of sparsely populated/rural (non-reporting) counties, the PUDF dataset represents 99.99% of the Texas population. We used the “total charges” field to assess all charges related to the hospitalization (as per research question 2), which includes costs covered and not covered by insurance providers, and all expenses due to indigent admissions.
We used the disease categories to characterize the baseline burden of climate change-related diseases in terms of the number of hospital admissions and cost in each category (research questions 1-2). Then, to better support the inferential analyses related to social and spatial disparities, we selected the ICD-9-CM codes with the most numerous case counts (across primary, secondary and tertiary codes) within each disease category as our selected diseases of focus. An ICD-9-CM code is defined as having a three digit category code, and may have a fourth digit that specifies a subcategory, and a fifth digit that indicates a sub-classification. The selected diseases are: ischemic heart disease (ICD-9-CM 414-414.9) (Portier et al., 2010); diarrheal disease (ICD-9-CM 787.91) (Rosenthal, 2010); heat diseases, including heat exhaustion, heat cramps, heat stroke, and heat syncope, herein ‘heat ECSS’ (ICD-9-CM 992-992.5) (Brown et al., 2012); and asthma (493-493.92) (Tagaris et al., 2009). All of these selected diseases have well-documented empirical links to climate change in the extant literature.
Age-Adjustment
We used the direct method to create separate age-adjusted hospital admission rates per 100,000 people for each of the selected diseases by six social groups: (1) all people, (2) black, (3) Hispanic, (4) white non-Hispanic, (5) uninsured, and (6) insured. The justification for selecting these social groupings is provided in the next section. The age-adjustment was done at the state and county-level (except heat-related, which was age-adjusted only at the state-level as we did not conduct county-level analysis due to small counts), and for each of the six groups, using age-stratum data.
The 2010 Decennial Census was the source of age-stratum data for all people and it was used to calculate the state and county-level admission rates. The ACS 2006–2010 (5-year estimates) was the only available data source for black, Hispanic and white non-Hispanic populations by age, and so it was used to calculate the state and county-level rates. A 5-year ACS estimate was not available for the insured and uninsured variable, so we used the ACS 2008–2010 3-year estimate instead to calculate the rates at the state and county-level. Because the ACS does not report data for every county for each social group (to assure anonymity of respondents in counties with small counts), we eliminated counties without data; this corresponds to 19 counties for analyses using the black sub-group, 1 for analyses using the Hispanic sub-group, and 135 for analyses using the insured/uninsured sub-groups. Also, we eliminated counties that had less than 25 cases for each selected disease per social group because small health event occurrences will produce a large amount of random variation (Curtin & Klein, 1995).
To age-adjust using the direct method, we applied observed age-stratum disease rates for the population of interest (Texas counties and the State of Texas) to the reference population, i.e., the 2000 US Standard Population. Use of the 2000 Standard Population for age-adjustment is recommended by the National Center for Health Statistics’ age-adjustment guidelines (Friis & Sellers, 2014). Within that, we selected weight distribution #3 because the age distribution structure aligned with the US Census Bureau Decennial Census and American Community Survey (ACS) groupings (see Table 3). Direct age-adjustment was accomplished by multiplying the age-stratum rates of disease for the population of interest by the corresponding age-stratum weights for the 2000 US Standard Population. The weighted rates are then summed across the age-stratum groups to calculate the overall age-adjusted rate (Szklo & Nieto, 2014).
Table 3.
Age-adjusted Weighting, Distribution #31
| All ages | 1.000000 |
|---|---|
| Under 18 years | 0.257736 |
| 18-44 years | 0.393797 |
| 45-54 years | 0.134834 |
| 55 -64 years | 0.087247 |
| 65-74 years | 0.066037 |
| 75 years and over | 0.060349 |
Based upon 2000 projected population (Klein & Schoenborn, 2001).
Age-adjustment enabled us to remove effects based on varying population structures at the state- and county-levels and allowed us to compare selected diseases across geographic areas, i.e. county-to-county (Rushton, 2003). While our study did not compare Texas to other US states, it is possible to do so because we age-adjusted to the 2000 US Standard Population. Crude disease rate comparisons are not appropriate because diseases can have a disproportionate impact on the old and/or young and areas may have a large aging population or a high birth rate, resulting in over and/or under representation of disease rates. For example, ischemic heart disease disproportionately affects the elderly (Ang, 2013) and asthma has a higher prevalence among children than adults (Moorman et al., 2012). In essence, population age-adjustment controls for the potentially confounding effects of varying age structures across geographic units of analysis.
Social Sub-group Variables
Race/ethnicity and insurance status were examined. In terms of race/ethnicity, each patient was designated as black (of Hispanic or non-Hispanic origin), Hispanic (of any race), or white non-Hispanic based on information provided in the PUDF. These three groupings were selected to match population level estimates provided by the American Community Survey (ACS), which is the most accurate data source in the US for the calculation of disease rates including county-level age-adjusted rates by race/ethnicity. The ACS does not report an exclusive black non-Hispanic variable by age. While the hospitalization data would permit the calculation of mutually exclusive disease rates for black non-Hispanics and Hispanics, we needed to align our race/ethnicity categories with those available from the ACS for the purposes of age-adjustment. Our categorization means that there is slight overlap between black and Hispanic (i.e., black is not mutually exclusive of Hispanic, but both are exclusive of non-Hispanic white). The overlap is quite small due to the demographics of the Hispanic population in Texas: black Hispanics (of all ages) represent only 3.11% of the total black population and 0.98% of the total Hispanic population in Texas (US Census Bureau, 2010).
Each patient was also categorized as insured or uninsured. Because PUDF data do not include income variables, lacking health insurance was used as a marker of social vulnerability. Those lacking insurance include immigrants without access to public programs such as Medicaid or Medicare, the working poor who make too much to qualify for public programs but not enough to afford private health insurance, and employees of small businesses who either do not have access to insurance through their employer or cannot afford the premiums (Grineski & McDonald, 2011; O’Neil & O’Neil, 2009). Insured include cases covered by the categories of private insurance, Medicare, Medicaid, or insurance from other government programs (e.g., military). The uninsured category is mutually exclusive of the insured, which is the reference category in the analyses. The categories of black, Hispanic, and the uninsured are associated with social vulnerability to climate change, as these sub-groups are likely to be disproportionately impacted by climate change-related exposures (Reid et al., 2009; Shonkoff, et al., 2011).
Model Projections
In order to estimate the future incidence, treatment costs, and disparities for social subgroups (research question 4), we considered the time period 2040–2050 for asthma only. We used 2040-2050 because substantial climatic changes are expected with relative certainty by that time period, yet it is also proximate enough to support reasonable predictions regarding human health impacts. We selected asthma because it is associated with weather parameters influenced by climate change (Kinney, 2008); a temperature/hospitalization relationship has been established for it based on a previous study (Lin et al., 2012); it has the highest incidence rate among our selected diseases; and it is illustrative of a climate health injustice, i.e., blacks are disproportionately burdened with asthma.
Projected temperature data for Texas were obtained from a downscaled regional climate-change projection model (RCPM) that utilized multi-model ensembles (Nielsen-Gammon, 2011). The RCPM was developed using the International Panel of Climate Change (IPCC) A1B scenario and a Texas centric 10-grid-cell computation (see Nielsen-Gammon, 2011). The IPCC defines the A1B scenario as a future world with very rapid economic growth and a global population that peaks in mid-century, and then experiences a decline. It is marked with the rapid introduction of new and more efficient technologies, which do not rely too heavily on one particular energy source (Intergovernmental Panel on Climate Change, 2007). Assuming A1B conditions, the RCPM predicts a 2.2°C temperature increase for Texas by 2040-2050 relative to the baseline of a simulated 1980-1999 mean (Nielsen-Gammon, 2011).
Beyond A1B scenario assumptions, the RCPM temperature model assumes people will not reduce their greenhouse emissions output to levels that would reduce the model estimates and that there will not be other natural events that impact temperature (Nielsen-Gammon, 2011). Population and sub-group populations were held constant (see Lin et al., 2012), which means that we assume that population age structures for each of the sub-groups examined will remain the same in the future; this allows us to isolate the effects of climate change on health without complicating the associations with variable population parameters. We also assume that no significant human adaptations to temperature increases will occur in the intervening time period. In terms of the effect on hospital admissions due to increase in temperature, we used a conservative approach and applied the low-end range of Lin et al.’s (2012) log-linear empirical estimation, in which a 1°C increase in temperature will result in a 2.1% same-day increase in admissions for respiratory diseases, after adjusting other covariates. Based on this empirically-estimated temperature/hospitalization relationship, we assume that a Texas statewide increase of 2.2°C (from the baseline) will result in a 5.12% increase in asthma hospital admission rates by 2040-2050.
Analysis Strategy
To answer research question 1, we present age-adjusted rates of hospital admissions for the cardiovascular, gastrointestinal, heat, and respiratory disease categories and for the selected diseases, which include ischemic heart disease, diarrhea, heat ECSS, and asthma for the state as a whole. To address research question 2, we sum total hospitalization dollar charges and calculate mean dollar charges for the disease categories and the selected diseases.
Addressing research question 3 involves four analyses using the selected disease data. First, we used the Wilcoxon signed-rank test to determine if there were social disparities (between black/white non-Hispanic, Hispanic/white non-Hispanic, and uninsured/insured) in hospitalizations for the age-adjusted selected diseases at the county level. We used this non-parametric test because the data were not normally distributed.
Second, we use relative risk ratios (RR) to explore if there were disparities between age-adjusted social groups (same three comparisons as above) by selected disease at the county-level. SPSS version 21.0 was used for these statistical tests. The RR results for asthma are also mapped since asthma had the most counties with complete data. The RR results for ischemic heart disease and diarrhea were not mapped because the number of included counties was insufficient to support meaningful spatial representation. Third, to explore spatial distributions of age-adjusted hospital admissions for all people for the selected diseases, we create maps showing counties with low (<-1 standard deviation below the mean), moderate (≥-1 and ≤1 standard dev. from the mean), and high (>1 standard deviation above the mean) rates.
To address research question 4, we apply the estimated 5.12% increase in asthma hospitalization rates by 2040 – 2050 (Lin et al., 2012) to our 2008-2010 asthma statistics: asthma hospital admissions cases per 100,000, the total and mean hospital charges for asthma hospital admissions, and the age-adjusted hospitalization rates for asthma by social sub-groups. Social sub-groups include blacks, Hispanics, white non-Hispanics, and individuals admitted with and without medical insurance (i.e. insured and uninsured persons). Future projection was performed at the state-level.
Results
In answer to research question 1, the rates for the disease categories and selected diseases are presented in Table 4. Cardiovascular disease ranked first among the categories of diseases examined in terms of age-adjusted rates at the state level, and asthma had the highest rate out of the selected diseases for hospital admissions per 100,000 people.
Table 4.
Hospital Admission Cases per Disease per 100,000 Population at the State-Level
| Disease Category | p/100,000 | Selected Disease | p/100,000 |
|---|---|---|---|
| Cardiovascular | 5268.37 | Ischemic heart disease | 195.20 |
| Gastrointestinal | 75.35 | Diarrhea | 75.35 |
| Heat | 13.71 | Heat ECSS | 7.81 |
| Respiratory | 1237.97 | Asthma | 517.51 |
| Vector-borne | 0.00 | N/A | |
| Water-borne | 0.40 | N/A |
In response to research question 2, total and mean charge summaries are presented in Table 5. Cardiovascular disease was the most costly disease category for hospital admissions, with nearly six times the total dollar charges than the second most costly category, respiratory disease. Asthma and ischemic heart disease were the most costly of the selected diseases. Although ischemic heart disease had more than $1.5 billion less in total charges than asthma, its mean hospital charges were more than $10,000 greater per patient.
Table 5.
Hospital Charges by Disease Category and Selected Disease, 2008 - 2010 at the State-Level
| Disease Category | Total Charges | Mean Charges | SD |
|---|---|---|---|
| Cardiovascular | 53348045592 | 40270 | 668365 |
| Gastrointestinal | 385477208 | 20345 | 23578 |
| Heat | 81480523 | 23631 | 50082 |
| Respiratory | 8917064693 | 28645 | 156529 |
| Selected Disease | |||
| Ischemic Heart Disease | 1824315434 | 37168 | 49447 |
| Diarrhea | 385477208 | 20345 | 23577 |
| Heat ECSS | 45226859 | 23027 | 47832 |
| Asthma | 3416051022 | 26251 | 232361 |
Total, mean, and standard deviation are in US dollars
For the first analysis addressing research question 3, blacks had the highest age-adjusted hospital admission rates for ischemic heart disease, asthma, and heat ECSS, while white non-Hispanic was the top social sub-group for diarrhea (see Table 6). Hispanics had the lowest age-adjusted hospitalizations for all of the selected diseases. The insured had higher rates of age-adjusted hospital admissions for ischemic heart disease, diarrhea, and asthma than the uninsured, but the uninsured had a higher rate than the insured for heat ECSS.
Table 6.
Age-adjusted Disease Rates at the State-Level by Selected Disease by Social Sub-Groups for Hospital Admissions, 2008 -2010*
| IHD1 | Diarrhea | Asthma | Heat ECSS | |
|---|---|---|---|---|
| Social Sub-Groups | ||||
| Black | 195.62 | 67.77 | 935.02 | 11.05 |
| Hispanic | 182.15 | 60.16 | 401.18 | 5.70 |
| White non-Hispanic | 191.42 | 80.76 | 455.71 | 6.93 |
| Insured | 235.80 | 89.42 | 579.13 | 7.40 |
| Uninsured | 147.59 | 37.85 | 322.48 | 20.18 |
Disease rates are per 100,000 population and presented by age-adjusted rate.
Ischemic Heart Disease
For the second analysis addressing research question 3 (see Table 7), the Wilcoxon signed-rank test (two-tailed) for ischemic heart disease at the county-level revealed that the age-adjusted mean was higher (p = .01) for blacks than white non-Hispanics and for uninsured as compared to insured (p = .02). There was no significant difference between the mean ischemic heart disease hospitalization rates for Hispanics versus white non-Hispanics at the county level. However, for diarrhea, white non-Hispanics had a higher age-adjusted county-level mean (p = .02) than Hispanics. In contrast to the result for ischemic heart disease, the county mean diarrhea rate for the insured was higher (p = .05) than it was for the uninsured. All three county-level comparisons were significant for asthma with blacks having higher mean rates than white non-Hispanics, white non-Hispanics having higher mean rates than Hispanics, and the insured having higher mean rates than the uninsured. (p = .01 for all three).
Table 7.
Age-Adjusted per 100,000 by Selected Disease by Social Sub-Groups at the County-Level, 2008 -2010
| Ischemic Heart Disease | Diarrhea | Asthma | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Social Sub-Groups Variable | N | Mean | SD | Wilcoxon1 | N | Mean | SD | Wilcoxon1 | N | Mean | SD | Wilcoxon1 |
| White non-Hispanic | 27 | 212.00 | 67.23 | 13 | 80.18 | 21.63 | 76 | 536.53 | 220.71 | |||
| Black | 27 | 259.38 | 124.54 | .01** | 13 | 83.32 | 30.51 | .75 | 76 | 1237.29 | 847.87 | .01** |
| White non-Hispanic | 49 | 918.71 | 3678.75 | 28 | 189.52 | 484.49 | 77 | 998.49 | 2390.14 | |||
| Hispanic | 49 | 366.87 | 1008.11 | .50 | 28 | 158.99 | 432.82 | .02* | 77 | 624.71 | 1072.49 | .01** |
| Insured | 31 | 257.93 | 74.87 | 11 | 90.19 | 18.87 | 68 | 660.97 | 241.72 | |||
| Uninsured | 31 | 261.35 | 377.34 | .02* | 11 | 54.44 | 59.69 | .05* | 68 | 427.45 | 362.07 | .01** |
Wilcoxon signed-rank test (two-tailed)
N = Number of Counties with at least 25 cases per disease per social group
Mean statistically significant at .01 and
Mean statistically significant < .05
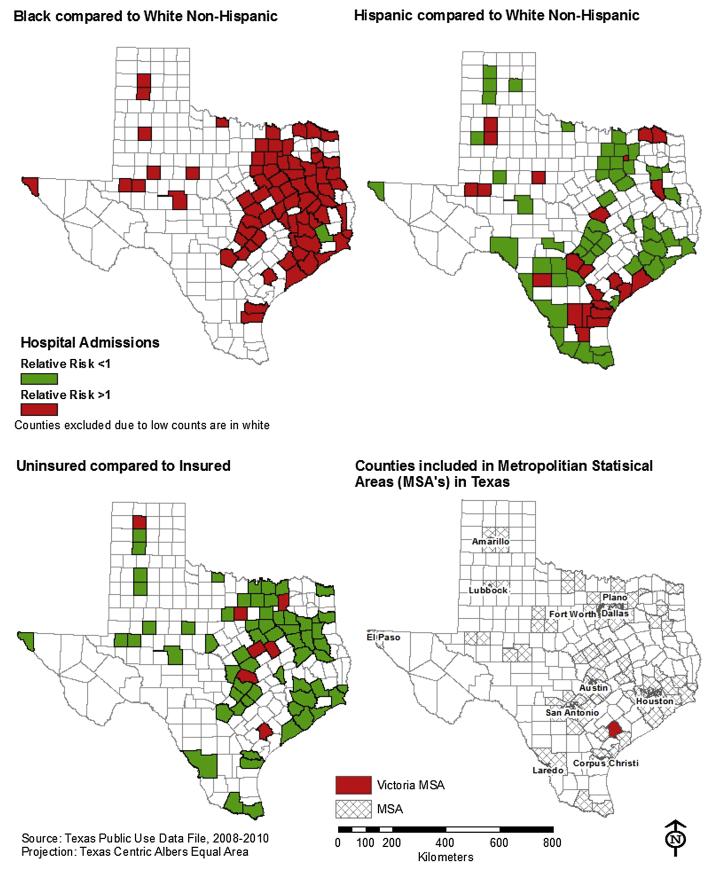
The relative risk ratio (RR) analysis for hospital admissions at the county-level by selected diseases also addressed research question 3 (see supplementary file A).
For ischemic heart disease, 74% of the counties under study (20 out of 27) had a RR above 1 for blacks compared to white non-Hispanics indicating that blacks were at increased risk in the majority of Texas counties as compared to white non-Hispanics. The same disparities were not clearly evident for Hispanics; the percentage of counties with RR above 1 was less for the Hispanic vs. white non-Hispanic comparison (54%, 27 out of 50 counties). Interestingly, the percentage of counties with RR above 1 for the uninsured as compared the insured was 23% (7 out of 30), which indicates that the insured are more prone to be hospitalized due to ischemic heart disease across approximately three-quarters of Texas counties. The same trends across the three comparisons observed for ischemic heart disease, wherein black populations experience greater risks relative to white non-Hispanics in the majority of Texas counties while Hispanics do not, and the insured exhibit increased odds of hospitalization relative to the uninsured, were also found for diarrhea and asthma hospitalizations (see supplementary file A). In the case of asthma, it is notable that 99% of 76 counties under study had a RR above 1 for black compared to white non-Hispanic indicating this racial disparity in asthma hospitalizations is present in nearly every county across the state.
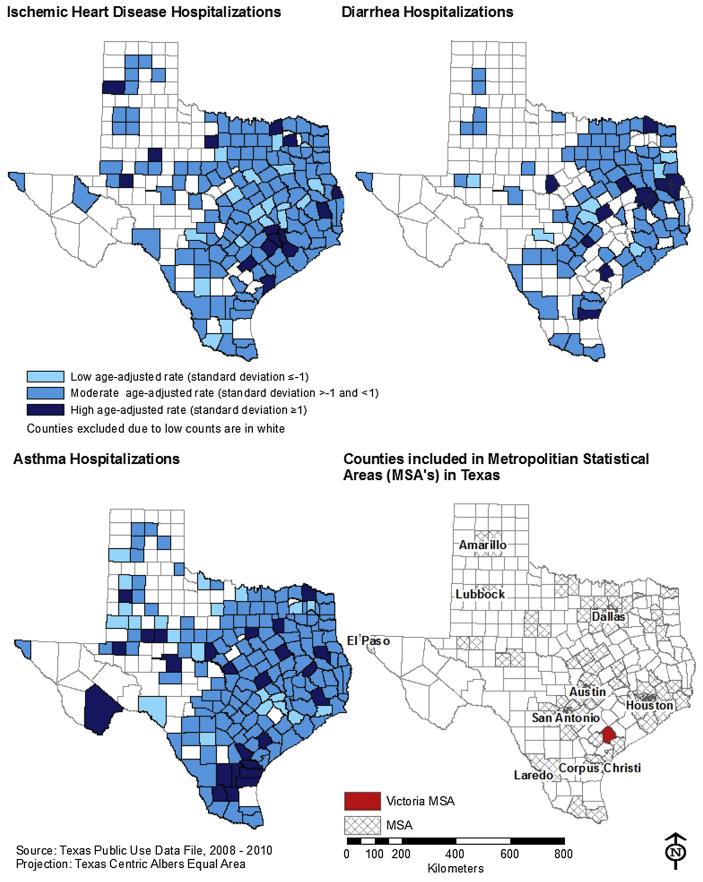
Maps showing the Texas counties with high rates of the selected diseases (the fourth and final analysis for research question 3) are presented in Figure 2. The maps display age-adjusted disease rates based on three classes of standard deviation values: low (<-1), moderate (≥-1 to ≤1), or high (>1). In terms of ischemic heart disease, 9% (15 out of 159) of the counties had high rates (i.e., age-adjusted admission rate that is greater than one standard deviation above the Texas county mean), while 12% (12 out of 98), and 14% (25 of 177) of counties had high rates for diarrhea, and asthma, respectively.
Figure 2.
To address research question 4, estimated 2040–2050 hospital admissions, treatment costs, and social sub-groups rates for asthma are presented in Table 7. While the relationships remained the same to present day findings, the magnitudes of the incidence of disease, economic burden, and health disparities are amplified in response to temperature increases.
Discussion
This analysis of 2008 – 2010 hospitalization discharge data at state and county levels in Texas (USA) demonstrated the utility of our climate health justice model. Note that the intent of the model is not to support claims about the proportion of health effects (hospital admissions) or economic costs (dollar charges) that are directly attributable to climate change. Instead, our purpose has been to quantify the current impact of these diseases and project future impacts under climate change, demonstrating how this model can be used to assess climate health (in)justice.
Model Applications
The model can be tailored to meet assessment needs in a variety of ways. We illustrated its utility at the US county and state levels, but it could be used at finer and coarser scales, for example, for neighborhood proxy geographic units or even countries and world regions. The use of an international disease coding system (ICD-9-CM or ICD-10-CM) and a standard age-adjustment protocol allows for comparability across different scales and between geographic locations. The model can be applied for non-comparative purposes and researchers have the flexibility to focus on a variety of climate change-associated diseases (see Table 1 and 2). While hospitalization data have limitations (e.g. a lack of information on socioeconomic status and indirect economic impacts), they are relatively accessible in many countries, making them ideal for comparative purposes. While our analyses did not include a focus on indirect economic impacts (e.g. those associated with missed days of work or reduced spending), it would not be beyond the scope of the model, since such economic impacts can be projected.
Emergency room (ER) records also use ICD codes to classify patients, making them easily employable in the model, and they are available in some US states. Their inclusion would allow for consideration of less serious cases of the illnesses (see Table 2) not requiring hospital admission. In the US, hospitalization and ER data are often available from state health departments at the individual level. These data include home address, which allows patients’ locations to be geocoded and then analyzed as individuals or aggregated to coarser geographic scale of interest. Other health data sources could be utilized, such as national health surveys and mortality statistics with geographic information about respondents. The health data source selected by the analyst will determine the sorts of health conditions that can be examined. For example, hospitalization data were not a good choice for vector- and water-borne diseases in Texas, but they were ideal for examining ischemic heart disease.
The model can be expanded to include any relevant axis of social marginality, such as gender or occupation, depending on relevance in the study area and data availability. In Texas, black and Hispanic were important racial/ethnic categories for which data were available, but elsewhere, other racial/ethnic groups may be more applicable (e.g., Native American, if one was studying the state of New Mexico). Analysts may also be limited to some degree by the availability of population data for use in age-adjustments. In our case, the 5-year ACS estimates were the best available data for the age-adjustments, but use of this data source meant that two of the social groups we examined were not mutually exclusive. The seriousness of such data issues needs to be evaluated on a case-by-case basis; for our purposes, the slight overlap of Hispanic and black had a limited impact on the analysis, results, and conclusions. Incorporating socio-demographic data beyond what is available in hospital records is also advisable to permit more robust analyses of health inequalities.
The modest health impact projection steps employed in the Texas application above illustrate that it is possible to estimate future disease rates, economic costs, and inequalities using the model, based on the integration of data on projected climate parameter changes and known weather parameter/health relationships derived from empirical analyses. The analyst will be restricted by preexisting knowledge of weather parameter/health relationships and projections. In our case, asthma was the best choice to demonstrate the utility of the model (e.g., we did not find a reliable figure for the expected increase in excess cases of diarrhea hospitalization due to climate change in the literature). While this is a limitation of our case study, it is not a limitation of the general model. In implementing our asthma projection, we used estimated increase from Lin et al. (2012), as they actually perform a climate change respiratory health impact projection analysis. Even though the projection is based on an analysis of New York, it is the best climate change-respiratory health impact projection analogue currently available in the literature. The absence of information on empirically-based projected weather parameter/health relationships for specific climate change-related diseases in particular regions of interest should direct future analysts to determine those relationships based upon public health need. We recommend that analysts seek to identify downscaled climate models that permit finer-scale analyses and incorporate population projections for socio-demographic changes in age structures. These improvements would allow for better identification of geographic areas likely to be disproportionately burdened in the future and for the prediction of changing trends in disparities between social groups.
Relevance of the Texas Application
Our analyses can inform policy discussions of the possible future health impacts of climate change in Texas and other similar contexts, which indicates the potential utility of our climate health justice model for addressing health impacts and inequalities. Hospital admissions for climate change-relevant diseases in Texas during the study period were associated with $62.7 billion in charges, which equaled 5% of the Texas GDP in 2010. This figure does not account for all costs, since it excludes healthcare accessed in clinics, urgent care centers, emergency rooms, and indirect impacts, such as lost economic productivity. In terms of social inequalities, blacks were disproportionally burdened while Hispanics had the lowest rates for all of the selected diseases. These Hispanic findings align with the social health inequalities literature documenting a “Hispanic Health Paradox”, which refers to a contradiction in that Hispanics in the US enjoy better health compared to other minorities despite their relatively low socioeconomic status (Collins, Jimenez, & Grineski , 2013; Markides & Coreil, 1986; Morales, Lara, Kington, Valdez, & Escarce, 2002). The difference in disease risk between Hispanics and blacks demonstrates the importance of considering these sub-groups separately, as opposed to pooling them into one “minority” group, as is sometimes done. More generally, the marked difference in disease risk between Texas’ two largest racial/ethnic minority groups highlights the importance of operationalizing regionally-relevant social categories for successful model implementation. The insurance status results demonstrate the complicated relationships between insurance status, wealth, and severity of disease. We found that those with insurance were more likely to be hospitalized for non-life threatening climate change-related diseases, as opposed to those without insurance, and conversely, that hospitalization rates for life threatening diseases were highest among the uninsured. It is likely that concerns about cost are driving this pattern with the uninsured using the hospital only as a last resort for serious illnesses. Finally, the Victoria MSA emerged as a locale that warrants future research and programmatic intervention due to its high risk for all selected diseases.
Conclusion
Our model extends from the well-established literatures on weather parameter/health relationships and climate change projections, and merges a normative emphasis on unequal impacts associated with climate change with health inequalities scholarship. It demonstrates four contributions to climate change health literature. First, it introduces a model that can be used to inform understandings of climate health justice. Second, it addresses the relative neglect of a social inequalities perspective in the current health impacts of climate change literature by focusing analytical attention on the differential social impacts of diseases associated with climate change. Third, it can project future climate health injustices in a technically-sound manner using projected weather parameter/health relationships found in the literature. Fourth, it demonstrates how tools that are relatively low-cost, readily available, and easy to implement by scholars and practitioners alike can be utilized to implement a geographic approach to understanding disparate health impacts associated with climate change. The model can be adopted in future studies by academic analysts or public health practitioners and can help inform the development of public health intervention strategies to reduce health disparities.
From the normative perspective that underpins our climate health justice model, intervention strategies should be designed with the goals of ameliorating injustices through the reduction of social and spatial health disparities. For example, public health interventions in Texas should prioritize addressing the disproportionate impacts experienced by black residents and geographical groups of people at disparately high risk, such as residents of the Victoria MSA. If interventions are not targeted to address the climate health injustices burdening these groups of Texans now, the health inequalities they experience will deepen in the coming decades.
Supplementary Material
Figure 1.
Table 8.
2008-2010 Compared to Projected 2040-2050 Hospital Admissions, Treatment Costs, and Social Sub-Groups Disease Rates for Asthma at the State-Level
| 2008-2010 | 2040-2050 | |
|---|---|---|
| Incidence1 | 517.51 | 544.01 |
| Total Charges2 | $3,416,051,022 | $3,590,952,834 |
| Mean Charges2 | $26,251 | $27,595 |
| Social Sub-Groups Asthma Rates3 | ||
| Black | 935.02 | 982.89 |
| Hispanic | 401.18 | 421.72 |
| White non-Hispanic | 455.71 | 479.04 |
| Insured | 579.13 | 608.78 |
| Uninsured | 322.48 | 338.99 |
Incidence is per 100,000 at the State-Level, and population is held constant.
Charges are treatment costs and are in un-adjusted US dollars.
Disease rates are age-adjusted per 100,000 population, and population is held constant.
Acknowledgments
This research was supported by the Southwest Consortium for Environmental Research (SCERP), the Environmental Protection Agency (EPA), the National Institute on Minority Health and Health Disparities (NIMHD), the National Science Foundation (NSF), and the National Aeronautics and Space Administration (NASA). The authors would like to thank participants of the XVth International Medical Geography Symposium for their initial feedback of this research. We would also like to acknowledge the anonymous reviewers who provided very constructive feedback on the original draft of the manuscript. The content is solely the responsibility of the authors and does not necessarily represent the official views of the SCERP, EPA, NIMHD, NSF, or NASA.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ang R. Surveillance report: cardiovascular disease in Texas 2012. Texas Department of State Health Services; [Accessed 06.26.2012]. 2013. Available at http://www.dshs.state.tx.us/wellness/data.shtm. [Google Scholar]
- Basu R. High ambient temperature and mortality: a review of epidemiologic studies from 2001 to 2008. Environmental Health. 2009;8:40. doi: 10.1186/1476-069X-8-40. doi:10.1186/1476-069X-8-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basu R, Ostro BD. A multicounty analysis identifying the populations vulnerable to mortality associated with high ambient temperature in California. American Journal of Epidemiology. 2008;168(6):632–637. doi: 10.1093/aje/kwn170. [DOI] [PubMed] [Google Scholar]
- Bosello F, Roson R, Tol RSJ. Economy-wide estimates of the implications of climate change: human health. Ecological Economics. 2006;58(3):579–591. [Google Scholar]
- Brown P. Race, class and environmental health: a review and systematization of the literature. Environmental Research. 1995;69(1):15–30. doi: 10.1006/enrs.1995.1021. [DOI] [PubMed] [Google Scholar]
- Brown T, Craddock S, Ingram A. Critical interventions in global health: governmentality, risk, and assemblage. Annals of the Association of American Geographers. 2012;102(5):1182–1189. [Google Scholar]
- Brownstein JS, Holford TR, Fish D. Effect of climate change on Lyme disease risk in North America. EcoHealth. 2005;2(1):38–46. doi: 10.1007/s10393-004-0139-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brulle RJ, Pellow DN. Environmental justice: human health and environmental inequalities. Annual Review of Public Health. 2006;27:103–124. doi: 10.1146/annurev.publhealth.27.021405.102124. [DOI] [PubMed] [Google Scholar]
- Chakraborty J, Maantay J, Brender JD. Disproportionate proximity to environmental health hazards: methods, models, and measurement. American Journal of Public Health. 2011;101(S1):S27–S36. doi: 10.2105/AJPH.2010.300109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clougherty JE. A growing role for gender analysis in air pollution epidemiology. Ciencia & Saude Coletiva. 2011;16(4):2221–2238. doi: 10.1590/s1413-81232011000400021. [DOI] [PubMed] [Google Scholar]
- Collins TW, Jimenez AM, Grineski SE. Hispanic health disparities after a flood disaster: results of a population-based survey of individuals experiencing home site damage in El Paso (Texas, USA) Journal of Immigrant and Minority Health. 2013;15(2):415–426. doi: 10.1007/s10903-012-9626-2. [DOI] [PubMed] [Google Scholar]
- Comrie A. Climate change and human health. Geography Compass. 2007;1(3):325–339. [Google Scholar]
- Costello A, Abbas M, Allen A, Ball S, Bell S, Bellamy R, et al. Managing the health effects of climate change. Lancet. 2009;373:1693–1733. doi: 10.1016/S0140-6736(09)60935-1. [DOI] [PubMed] [Google Scholar]
- Cromley EK, McLafferty SL. GIS and Public Health. The Guilford Press; New York, New York: 2012. [Google Scholar]
- Cueto-Garcia RO, Martinez-Tejeda A, Ostos-Jauregui E. Heat waves and heat days in an arid city in the northwest of Mexico: current trends and in climate change scenarios. International Journal of Biometeorology. 2010;54(4):335–345. doi: 10.1007/s00484-009-0283-7. [DOI] [PubMed] [Google Scholar]
- Curtin LR, Klein RJ. Direct standardization (age-adjusted death rates) National Center for Health Statistics; [Accessed 31.05.2011]. 1995. Available at http://www.cdc.gov/nchs/data/statnt/statnt06rv.pdf. [PubMed] [Google Scholar]
- Ebi KL, Exuzides KA, Lau E, Kelsh M, Barnston A. Weather changes associated with hospitalizations for cardiovascular diseases and stroke in California, 1983-1998. International Journal of Biometeorology. 2004;49(1):48–58. doi: 10.1007/s00484-004-0207-5. [DOI] [PubMed] [Google Scholar]
- Ebi KL, Mills DM, Smith JB, Grambsch A. Climate change and human health impacts in the United States: an update on the results of the U.S. national assessment. Environmental Health Perspectives. 2006;114(9):1318–1324. doi: 10.1289/ehp.8880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein PR. Climate change and human health. The New England Journal of Medicine. 2005;353(14):1433–1436. doi: 10.1056/NEJMp058079. [DOI] [PubMed] [Google Scholar]
- Friis RH, Sellers TA. Epidemiology for Public Practice. Jones & Bartlett Learning; Burlington, MA: 2014. [Google Scholar]
- Green RS, Basu R, Malig B, Broadwin R, Kim JJ, Ostro B. The effect of temperature on hospital admissions in nine California counties. International Journal of Public Health. 2010;55(2):113–121. doi: 10.1007/s00038-009-0076-0. [DOI] [PubMed] [Google Scholar]
- Grineski SE, Collins TW, Ford P, Fitzgerald R, Aldouri R, Velazquez-Angulo G, et al. Climate change and environmental injustice in a bi-national context. Applied Geography. 2012;33(1):25–35. [Google Scholar]
- Grineski SE, Collins TW, McDonald Y, Aboarbog F, Eldeb A, Aldouri R, et al. [Accessed 01.10.13];Double exposure and the climate gap: changing demographics and extreme heat in Ciudad Juárez, Mexico. Local Environment. 2014 doi: 10.1080/13549839.2013.839644. Available at http://www.tandfonline.com/doi/abs/10.1080/13549839.2013.839644#.Uv2jMfldWPY. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grineski SE, McDonald YJ. Mapping the uninsured using secondary data: an environmental justice application in Dallas. Population and Environment. 2011;32(4):376–387. [Google Scholar]
- Gwynn RC, Thurston GD. The burden of air pollution: impacts among racial minorities. Environmental Health Perspectives. 2001;109:501–506. doi: 10.1289/ehp.01109s4501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hackbarth AD, Romley JA, Goldman DP. Racial and ethnic disparities in hospital care resulting from air pollution in excess of federal standards. Social Science & Medicine. 2011;73(8):1163–1168. doi: 10.1016/j.socscimed.2011.08.008. [DOI] [PubMed] [Google Scholar]
- Haines A, Patz J. Health effects of climate change. Journal of American Medical Association. 2004;291(1):99–103. doi: 10.1001/jama.291.1.99. [DOI] [PubMed] [Google Scholar]
- Hajat S, O’Connor M, Kosatsky T. Health effects of hot weather: from awareness of risk factors to effective health protection. Lancet. 2010;375:856–863. doi: 10.1016/S0140-6736(09)61711-6. [DOI] [PubMed] [Google Scholar]
- Hales S, Edwards SJ, Kovats RS. Impacts on health and climate extremes. In: McMichael AJ, Campbell-Lendrum D, Corvalan CF, Ebi KL, Githeko AK, Schrega JD, Woodward A, editors. Climate change and human health: risks and responses. World Health Organization; Malta: 2003. pp. 79–102. [Google Scholar]
- Harlan SL, Ruddell DM. Climate change and health in cities: impacts of heat and air pollution and potential co-benefits from mitigation and adaptation. Current Opinion in Environmental Sustainability. 2011;3(3):126–134. [Google Scholar]
- ICD9Data [Accessed 28.01.2012];ICD-9-CM diagnosis code 504. 2008 Available at http://www.icd9data.com/2008/Volume1/460-519/500-508/504/504.htm.
- Intergovernmental Panel on Climate Change (IPCC) Climate change 2007: impacts, adaptation and vulnerability. Contribution of working group II to the fourth assessment report of the intergovernmental panel on climate change. Cambridge University Press; Cambridge, UK: 2007. [Google Scholar]
- Kersten E, Morello-Frosch R, Pastor M, Ramos M. Facing the climate gap: how environmental justice communities are leading the way to a more sustainable and equitable California. Program for Environmental and Regional Equity. University of Southern California; [Accessed 21.06.13]. 2012. Available at http://dornsife.usc.edu/assets/sites/242/docs/FacingTheClimateGap_web.pdf. [Google Scholar]
- Khasnis AA, Nettleman MD. Global warming and infectious disease. Archives of Medical Research. 2005;36(6):689–696. doi: 10.1016/j.arcmed.2005.03.041. [DOI] [PubMed] [Google Scholar]
- Kinney PL. Climate change, air quality, and human health. American Journal of Preventive Medicine. 2008;35(5):459–467. doi: 10.1016/j.amepre.2008.08.025. [DOI] [PubMed] [Google Scholar]
- Klein RJ, Schoenborn CA. Age-adjustment using the 2000 projected U.S. population. National Center for Health Statistics; [Accessed 31.05.2011]. 2001. Available at http://www.cdc.gov/nchs/data/statnt/statnt20.pdf. [PubMed] [Google Scholar]
- Knowlton K, Rotkin-Ellman M, King G, Margolis HG, Smith D, Solomon G, et al. The 2006 California heat wave: impacts on hospitalizations and emergency department visits. Environmental Health Perspectives. 2009;117(1):61–67. doi: 10.1289/ehp.11594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovats RS, Tirado C, Ebi KL, Hajat S, Edwards S, Kaesbohrer A. Climate, weather, and enteric disease. In: Menne B, Ebi KL, editors. Climate change and adaption strategies for human health. World Health Organization; Darmstadt, Germany: 2006. pp. 269–295. [Google Scholar]
- Lin S, Hsu WH, Van Zutphen AR, Saha S, Luber G, Hwang SA. Excessive heat and respiratory hospitalizations in New York State: estimating current and future public health burden related to climate change. Environmental Health Perspectives. 2012;120(11):1571–1577. doi: 10.1289/ehp.1104728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin S, Luo M, Walker RJ, Liu X, Hwang S-A, Chinery R. Extreme high temperatures and hospital admissions for respiratory and cardiovascular diseases. Epidemiology. 2009;20(5):738–746. doi: 10.1097/EDE.0b013e3181ad5522. [DOI] [PubMed] [Google Scholar]
- Luber G, McGeehin M. Climate change and extreme heat events. American Journal of Preventive Medicine. 2008;35(5):429–435. doi: 10.1016/j.amepre.2008.08.021. [DOI] [PubMed] [Google Scholar]
- Maantay J, Becker S. The health impacts of global climate change: a geographic perspective. Applied Geography. 2012;33:1–3. [Google Scholar]
- Madrigano J, Mittleman MA, Baccarelli A, Goldberg R, Melly S, von Klot S, et al. Temperature, myocardial infarction, and mortality, effect modification by individual-and area-level characteristics. Epidemiology. 2013;24(3):439–445. doi: 10.1097/EDE.0b013e3182878397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markides KS, Coreil J. The health of Hispanics in the southwestern United States: an epidemiologic paradox. Public Health Reports. 1986;101:253–265. [PMC free article] [PubMed] [Google Scholar]
- McMichael AJ, Woodruff RE, Hales S. Climate change and human health: present and future risks. Lancet. 2006;367:859–869. doi: 10.1016/S0140-6736(06)68079-3. [DOI] [PubMed] [Google Scholar]
- Michelozzi P, Accetta G, De Sario M, D’Ippoliti D, Marino C, Baccini M, Perucci CA. High temperature and hospitalizations for cardiovascular and respiratory causes in 12 European cities. American Journal of Respiratory and Critical Care Medicine. 2009;179(5):383–389. doi: 10.1164/rccm.200802-217OC. [DOI] [PubMed] [Google Scholar]
- Mirowsky J, Ross C, Reynolds J. Links between social status and health status. In: Bird C, Conrad P, Fremont A, editors. Handbook of Medical Sociology. 5th edition Prentice-Hall; Upper Saddle River, NJ: 2000. pp. 47–67. [Google Scholar]
- Mohai P, Pellow DN, Roberts JT. Environmental justice. Annual Review of Environment and Resources. 2009;34:405–430. [Google Scholar]
- Moorman JE, Akinbami LJ, Bailey CM, Zahran HS, King ME, Johnson CA, et al. National surveillance of asthma: United States, 2001–2010. 35. Vol. 3. National Center for Health Statistics. Vital Health Stat; [Accessed 06.26. 2012]. 2012. Available at http://www.cdc.gov/nchs/data/series/sr_03/sr03_035.pdf. [PubMed] [Google Scholar]
- Morales LS, Lara M, Kington RS, Valdez RO, Escarce JJ. Socioeconomic, cultural and behavioral factors affecting Hispanic health outcomes. Journal of Health Care for the Poor and Underserved. 2002;13(4):477–503. doi: 10.1177/104920802237532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morello-Frosch R, Pastor M, Sadd J, Shonkoff SB. The climate gap: inequalities in how climate change hurts Americans & how to close the gap. Program for Environmental and Regional Equity. University of Southern California; [Accessed 21.06.13]. 2009. Available at http://dornsife.usc.edu/assets/sites/242/docs/The_Climate_Gap_Full_Report_FINAL.pdf. [Google Scholar]
- Nazroo JY. The structuring of ethnic inequalities in health: economic position, racial discrimination, and racism. American Journal of Public Health. 2003;93(2):277–284. doi: 10.2105/ajph.93.2.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielsen-Gammon JW. The changing climate of Texas. In: Schmandt J, North GR, Clarkson J, editors. The impact of global warming on Texas. University of Texas Press; Austin, TX: 2011. pp. 39–68. [Google Scholar]
- O’Neill MS, Jerrett M, Kawachi L, Levy JL, Cohen AJ, Gouveia N, et al. Health, wealth, and air pollution: advancing theory and methods. Environmental Health Perspectives. 2003;111(16):1861–1870. doi: 10.1289/ehp.6334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Neil JE, O’Neil DM. Who are the uninsured? An analysis of America’s uninsured population, their characteristics and their health. Employment Policies Institute; Washington, DC: [Accessed 24.04.2010]. 2009. Available at http://www.epionline.org/studies/oneill_06-2009.pdf. [Google Scholar]
- Pastor M, Morello-Frosch R, Sadd J, Scoggins J. Minding the climate gap: what’s at stake if California’s climate law isn’t done right and right away. University of Southern California; [Accessed 21.06.13]. 2010. Available at http://dornsife.usc.edu/assets/sites/242/docs/mindingthegap.pdf. [Google Scholar]
- Patz JA, McGeehin MA, Bernard SM, Ebi KL, Epstein PR, Grambsch A, et al. The potential health impacts of climate variability and change for the United States: executive summary of the report of the health sector of the U.S. national assessment. Environmental Health Perspectives. 2000;108(4):367–376. doi: 10.1289/ehp.00108367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson TC, Zhang X, Brunet-India M, Vázquez-Aguirre JL. Changes in North American extremes derived from daily weather data. Journal of Geophysical Research. 2008;113:D07113. doi:10.1029/2007JD009453.D7. [Google Scholar]
- Portier CJ, Thigpen TK, Carter SR, Dilworth CH, Grambsch AE, Gohlke J, et al. A report outlining the research needs on the human health effects of climate change. Environ Health Perspect/National Institute of Environmental Health Sciences; Research Triangle Park, NC: [Accessed 26.6. 2011]. 2010. Available at http://www.niehs.nih.gov/health/assets/docs_a_e/climatereport2010.pdf. [Google Scholar]
- Reid CE, O’Neill MS, Gronlund CJ, Brines SJ, Brown DG, Diez-Roux AV, et al. Mapping community determinants of heat vulnerability. Environmental Health Perspectives. 2009;117(11):1730–1736. doi: 10.1289/ehp.0900683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren C, Tong S. Temperature modifies the health effects of particulate matter in Brisbane, Australia. International Journal of Biometeorology. 2006;51:87–96. doi: 10.1007/s00484-006-0054-7. [DOI] [PubMed] [Google Scholar]
- Rosenthal J. Climate change and the geographic distribution of infectious diseases. EcoHealth. 2009;6(4):489–495. doi: 10.1007/s10393-010-0314-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rushton G. Public health, GIS, and spatial analytic tools. Annual Review of Public Health. 2003;24:43–56. doi: 10.1146/annurev.publhealth.24.012902.140843. [DOI] [PubMed] [Google Scholar]
- Shea KM, Truckner RT, Weber RW, Peden DB. Climate change and allergic disease. The Journal of Allergy and Clinical Immunology. 2008;122(3):443–453. doi: 10.1016/j.jaci.2008.06.032. [DOI] [PubMed] [Google Scholar]
- Shonkoff SB, Morello-Frosch R, Pastor M, Sadd J. Minding the climate gap: environmental health and equity implications of climate change mitigation policies in California. Environmental Justice. 2009;2(4):173–177. [Google Scholar]
- Shonkoff SB, Morello-Frosch R, Pastor M, Sadd J. The climate gap: environmental health and equity implications of climate change and mitigation policies in California – a review of the literature. Climatic Change. 2011;109(1):485–503. [Google Scholar]
- Szklo M, Nieto FJ. Epidemiology: Beyond the Basics. Jones & Bartlett Learning; Burlington, MA: 2014. [Google Scholar]
- Tagaris E, Kuo-Jen L, Delucia AJ, Deck L, Amar P, Russel AG. Potential impact of climate change on air pollution-related human health effects. Environmental Science & Technology. 2009;43:4979–4988. doi: 10.1021/es803650w. [DOI] [PubMed] [Google Scholar]
- Texas Association of Counties [Accessed 07.07.2012];Texas counties: land Area. 2010 Redistricting Data (PL 94-171). Available at http://www.txcip.org/tac/census/morecountyinfo.php?MORE=1005.
- Texas Department of State Health Services [Accessed 07.01.2012];User manual for Texas inpatient public use data file 2010. Available at http://www.dshs.state.tx.us/thcic/hospitals/Inpatientpudf.shtm.
- Turner LR, Barnett AG, Connell D, Tong S. Ambient temperature and cardiorespiratory morbidity: A systematic review and met-analysis. Epidemiology. 2012;23(4):594–604. doi: 10.1097/EDE.0b013e3182572795. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau [Accessed 04.06.2013];2010 Available at http://factfinder2.census.gov.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.