Abstract
Background. The aim of this pilot study was to evaluate intranasal buserelin for luteal phase support and compare its efficacy with standard vaginal progesterone in IVF/ICSI antagonist cycles. Methods. This is a prospective, randomized, open, parallel group study. Forty patients underwent ovarian hyperstimulation with human menopausal gonadotropin under pituitary inhibition with gonadotropin-releasing hormone antagonist, while ovulation trigger and luteal support were achieved using intranasal GnRH agonist (group A). Twenty patients had their cycle downregulated with buserelin and stimulated with hMG, while ovulation trigger was achieved using 10,000 IU human chorionic gonadotropin with luteal support by intravaginal progesterone (group B). Results. No difference was observed in estradiol levels. Progesterone levels on day 5 were significantly lower in group A. However, significantly higher levels of luteinizing hormone were observed in group A during the entire luteal phase. Pregnancy rates (31.4% versus 22.2%), implantation rates (22% versus 15.4%), and clinical pregnancy rates (25.7% versus 16.7%) were not statistically different between groups, although a trend towards higher rates was observed in group A. No luteal phase lasting less than 10 days was recorded in either group. Conclusion. Intranasal administration of buserelin is effective for providing luteal phase support in IVF/ICSI antagonist protocols.
1. Introduction
Cycles resulting from controlled ovarian hyperstimulation (COH), when downregulated with gonadotropin-releasing hormone (GnRH) agonist or GnRH antagonist, commonly result in luteal phase deficiency [1, 2]. This phenomenon is characterized by low progesterone levels, delayed endometrial secretory transformation, and a shortened luteal phase of less than ten days [3], resulting in reduced embryo implantation, lower pregnancy rates, and increased miscarriage rates. For this reason, luteal phase support is a common practice in IVF treatments, as it significantly improves embryo implantation, pregnancy, and delivery rates [2].
Vaginal progesterone with or without estradiol and intramuscular human chorionic gonadotropin (hCG) are the current regimens used for luteal phase support. Since hCG administration is associated with the risk of ovarian hyperstimulation syndrome (OHSS), progesterone is the preferred choice [4].
It was reported that GnRH agonists administered during the luteal phase in addition to standard luteal phase support improved pregnancy rates in IVF-stimulated cycles [5–14], but the mechanism of this apparently beneficial effect is poorly understood. GnRH agonists may support the corpus luteum by stimulating the secretion of luteinizing hormone (LH) by pituitary gonadotroph cells, by acting directly on the endometrium through locally expressed receptors, or by their direct effect on the embryo [6, 7].
The question as to whether GnRH agonist alone is able to efficiently support the luteal phase nevertheless remains.
We previously reported that, in patients undergoing COH, intranasal (IN) administration of buserelin for 15 days is able to trigger final follicular maturation and has a marked, dose-related effect on the luteal phase [15]. This observation led to the conclusion that the optimal dose of buserelin for luteal support in an antagonist protocol is 100 μg 3 times per day.
To further analyze the potential benefits of this new protocol, our study objective was to assess the efficacy of luteal phase GnRH agonist administration in cycles where ovulation was triggered by GnRH agonist and compare it with a standard protocol using hCG to trigger ovulation, followed by intravaginal progesterone as luteal support. To the best of our knowledge, this is the first randomized controlled trial using GnRH agonist as the only luteal phase support.
2. Materials and Methods
2.1. Study Design and Patient Randomization
In order to study the effect of IN administration of GnRH agonist to trigger and support the luteal phase, we initiated a single-center, prospective, randomized, open, parallel group study. We were looking to compare this method in patients undergoing IVF/ICSI after stimulation of multiple follicular development with human menopausal gonadotropin (hMG). Inclusion criteria were the age between 18 and 39 and BMI ≥ 18 but ≤35, while exclusion criteria were a history of poor response, systemic disease (diabetes, severe migraine, hepatic, renal, or cardiovascular disease, and corticodependent asthma), and ovarian cysts ≥11 mm.
Computer-generated randomization was applied (2/1; group A/B). Treatment allocation instructions were placed in individually sealed envelopes to be opened at the center in chronological order on the day of signing the informed consent form.
In study group A, GnRH agonist (buserelin) was administered IN to trigger final follicular maturation and support the luteal phase. In control group B, hCG was administered to trigger final follicular maturation and vaginal progesterone to support the luteal phase.
The primary end-point was the comparison of pregnancy rates between the two groups.
The study protocol and informed consent form were approved by the institution's ethics committee.
2.2. Ovarian Stimulation Protocol and Treatment Groups
Sixty patients with infertility factors indicating IVF or ICSI were enrolled in this study, as shown in Figure 1.
Figure 1.
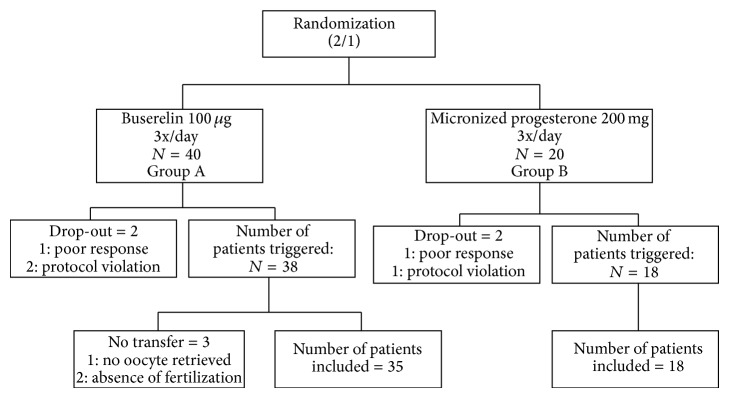
Randomization and allocation of patients to the two groups. In group A, ovulation was triggered with buserelin and the luteal phase was also supported by buserelin. In group B, ovulation was triggered with hCG and the luteal phase was supported with vaginal micronized progesterone.
In study group A, 40 patients underwent COH using hMG (Menopur, Ferring, Brussels, Belgium) at a dose ranging from 150 to 450 IU daily. When the leading follicle reached a mean diameter of 14 mm, daily administration of 0.25 mg GnRH antagonist (Orgalutran; MSD, Brussels, Belgium) was initiated every evening up to the day before ovulation trigger.
When patients met the criteria for ovulation trigger (at least 3 follicles >17 mm), they received 200 μg of IN buserelin (Suprefact; Aventis, Brussels, Belgium), followed by 100 μg IN buserelin three times a day for luteal support starting the next day, as previously published by our team [15]. This was continued for a maximum of 16 days until the day of the pregnancy test, whether or not it proved positive.
In control group B, 20 patients had a cycle downregulated with GnRH agonist and stimulated with hMG at a dose ranging from 150 to 450 IU daily. When they met the criteria for ovulation trigger (at least 3 follicles >17 mm), they were given 10,000 IU subcutaneous hCG (Pregnyl; MSD, Brussels, Belgium), followed by 200 mg vaginal progesterone three times a day (Utrogestan; Goodlife pharma, Lelystad, Netherlands), starting on the day of oocyte pick-up for luteal support. Progesterone was administered up to day 16 (day of the pregnancy test). If the pregnancy test proved positive, progesterone administration was continued up to week 12 of pregnancy, which is a common practice in our center.
Pregnancy was diagnosed by measuring serum hCG levels on day 14 of the luteal phase (day of first hCG/buserelin administration = D0). A pregnancy test was considered positive if an increase in serum hCG was observed after a first test showing at least >10 mIU/mL. The implantation rate was calculated as the number of gestational sacs divided by the number of transferred embryos.
Clinical pregnancy was defined as the presence of an intrauterine gestational sac with a positive heartbeat visualized by vaginal ultrasound.
The duration of the luteal phase was calculated from day 1 (the first day after ovulation trigger) up to the day before menstruation commenced.
IVF laboratory culture conditions were the same as those previously described [15].
All embryos were transferred on day 3.
2.3. Hormone Assays
Serum estradiol, serum progesterone, and serum LH concentrations were monitored on D0 (day of ovulation trigger), D2, D5, D9, and D14. Hormone levels were determined with commercially available kits routinely used in our accredited clinical center's central laboratory. Estradiol, progesterone, and LH were assayed using the Elecsys 2010 system (Roche Diagnostics GmbH, 68298 Mannheim, Germany). The E2 intra-assay coefficient of variation (CV) was <6% and the interassay CV was <6%; the P4 intra-assay CV was <3% and the interassay CV was <6%; the LH intra-assay CV was <2% and the interassay CV was <5%. Serum hCG was assayed using the Beckman-Coulter system (Anablis, Namur, Belgium), yielding an intra-assay CV of <2% for a value <5 mIU/mL and an interassay CV of <12%.
2.4. Statistical Analysis
Descriptive quantitative statistics (mean and SD) were calculated for demographic and ovarian stimulation status parameters, IVF/ICSI and embryo transfer parameters, and luteal phase duration. Comparison between groups was done using the student t-test. P < 0.05 was considered statistically significant.
3. Results
Sixty patients were randomized at a ratio of 2/1 (group A/group B). Five patients dropped out of group A and two from group B, leaving 53 patients eligible for analysis. Patient groups did not differ in their basic demographic characteristics, and COH parameters were also comparable (Table 1).
Table 1.
Patient demographics and stimulation parameters (mean ± SD).
| Group A (buserelin 3x/day) n = 35 |
Group B (micronized progesterone 3x/day) n = 18 |
P | |
|---|---|---|---|
| Age (years) | 32 ± 4.4 | 33 ± 4.5 | NS |
| Range | 2 ± 1.1 | 2 ± 1.3 | NS |
| HMG (IU) | 2526 ± 988 | 2614 ± 1077 | NS |
| Day of trigger (=D0) | 12.7 ± 2.7 | 12.9 ± 2.6 | NS |
| Estradiol D0 (pg/mL) | 2960 ± 1068 | 2929 ± 1439 | NS |
| Progesterone D0 (ng/mL) | 0.9 ± 0.4 | 1 ± 0.4 | NS |
| Endometrial thickness D0 (mm) | 9.8 ± 2.1 | 9.0 ± 3.0 | NS |
The mean number of retrieved oocytes, cleaved embryos, and transferred embryos did not show any statistical difference. Embryo transfer was performed in both groups, with a mean number of 1.4 embryos per transfer (Table 2). Furthermore, the mean number of good quality embryos was similar in both groups.
Table 2.
IVF/ICSI cycle outcomes (mean ± SD).
| Group A (buserelin 3x/day) n = 35 |
Group B (micronized progesterone 3x/day) n = 18 |
P | |
|---|---|---|---|
| Retrieved oocytes (n) | 10.1 ± 4.1 | 10.7 ± 5.9 | NS |
| Cleaved embryos (n) | 5.8 ± 2.7 | 6.0 ± 3.2 | NS |
| Transferred embryos (n) | 1.4 ± 0.5 | 1.4 ± 0.5 | NS |
| Pregnancy rate/transfer | 11/35 31.4% |
4/18 22.2% |
NS |
| Clinical pregnancy rate | 9/35 25.7% |
3/18 16.7% |
NS |
| Implantation rate | 11/50 22% |
4/26 15.4% |
NS |
In group A, 11 positive pregnancy tests were recorded during the study. Nine pregnancies were confirmed as clinical pregnancies, 7 of which were singleton and 2 were twin pregnancies. One pregnancy ended in miscarriage at 9 weeks and one was terminated because of spina bifida and another for severe preeclampsia. Eight healthy babies were born after 37 weeks of pregnancy.
In group B, 4 positive pregnancy tests were recorded during the study. Three pregnancies were confirmed as clinical pregnancies, 2 of which were singleton and one was a twin pregnancy. Four healthy babies were born after 37 weeks of pregnancy.
While similar numbers of retrieved oocytes and transferred embryos were found between groups, patients in group A showed a tendency towards a higher pregnancy rate (31.4% versus 22.2%), implantation rate (22% versus 15.4%), and clinical pregnancy rate (25.7% versus 16.7%), despite the fact there is no statistically significant difference (Table 2).
Endometrial thickness on D9 of the luteal phase was also similar in both groups (10.7 ± 3 mm versus 10.5 ± 4.4 mm).
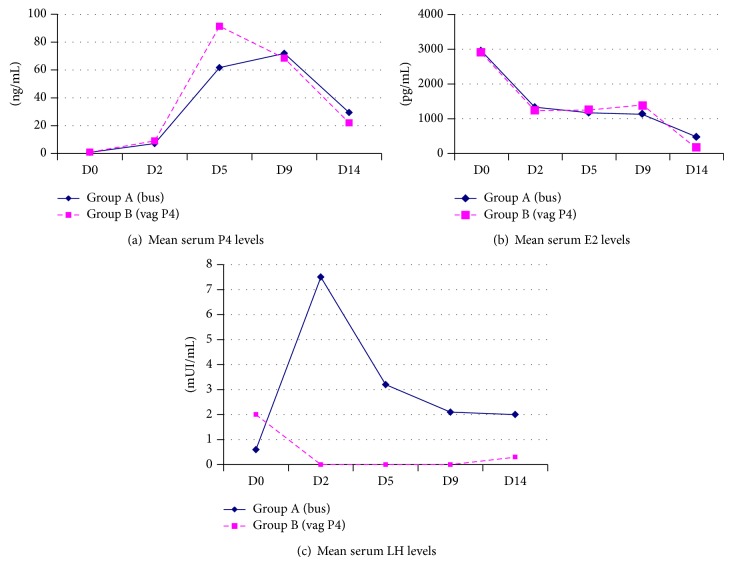
Hormone levels during the luteal phase are shown in Figure 2. The progesterone profile during the luteal phase was similar in both groups, except on D5, where it was significantly higher (P < 0.05) in group B (91.4 ± 38.8 ng/mL) than in group A (61.7 ± 36.9 ng/mL) (Figure 2(a)). Estradiol levels were comparable during the entire luteal phase (Figure 2(b)). By contrast, mean serum LH levels were significantly higher throughout the luteal phase in group A than in group B (where serum LH levels were below the limit of detection (<0.1 IU/L) in most samples taken between D2 and D9) (Figure 2(c)).
Figure 2.
Hormone levels during the luteal phase on D0 (day of ovulation trigger), D2, D5, D9, and D14. (a) Mean progesterone levels. (b) Mean estradiol levels. (c) Mean LH levels.
The duration of the luteal phase assessed in patients who did not become pregnant ranged between 11 and 21 days in group A (mean 13.8 ± 2.3) and between 11 and 19 days in group B (mean 14.7 ± 2.7). No luteal phase lasting less than 10 days was recorded in either group.
Buserelin treatment was well tolerated by all patients. There was no further drop-out, and no significant adverse events were reported in terms of local or systemic tolerance. No OHSS requiring hospitalization was recorded.
4. Discussion
During the menstrual cycle, a normal luteal phase is required for embryo implantation and evolution of pregnancy. The luteal phase is the result of intermittent stimulation of the corpus luteum by pituitary LH. During the luteal phase, pituitary LH pulses are of low frequency, leading to extended episodes of progesterone secretion at a rate of 3–5 per 24 hours [20]. Luteal phase deficiency is a common feature of cycles resulting from COH [21] including GnRH antagonist-treated cycles [22–24]. It is characterized by premature regression of the corpus luteum, leading to a shortened luteal phase (<10 days), low serum progesterone levels, and delayed secretory transformation of the endometrium [25]. Consequences of luteal phase deficiency are reduced embryo implantation rates, lower pregnancy rates, and increased miscarriage rates when pregnancy is established [2]. Besides standard luteal phase support with progesterone, various other methods have also been studied, including use of low-dose hCG [26–30], hCG according to ovarian response to stimulation [31], recombinant LH [32], and intensive progesterone and estradiol administration [33–35]. Because inadvertent administration of GnRH agonist does not appear to compromise pregnancy outcome [36], a number of studies have also investigated the potential benefits of using GnRH agonist for luteal phase support in IVF/ICSI cycles (Tables 3 and 4). The findings are somewhat contradictory, however, with studies identifying a positive [5, 7, 9, 10, 13], absent [12, 14, 16], or negative [17, 19] impact on outcome in long agonist stimulation protocols. Although the number of studies investigating antagonist protocols is smaller, a similar positive influence on implantation and pregnancy rates has been reported in most of these [7, 11, 13, 15]. Protocols of GnRH agonist administration vary, with intermittent single, double, or multiple doses or continuous administration during the luteal phase. It is noteworthy that all studies use GnRH agonist in combination with other luteal phase support methods previously mentioned. No comparison can therefore be made between our results and those in the reported literature. In our previous dose-finding study on the use of GnRH agonist for luteal support, we demonstrated that buserelin is able to induce final follicular maturation, trigger ovulation, and support alone the luteal phase when administered at the appropriate dose [15].
Table 3.
Main characteristics of trials on the use of a single injection of GnRH agonist for luteal phase support.
| Trial | Study design | Stimulation protocol | Ovulation trigger | Luteal phase support | Day of ET | Implantation rate (study group/control group) | (Ong/Clin) Pregnancy rate (study group/control group) | ||
|---|---|---|---|---|---|---|---|---|---|
| Study group GnRH-a |
Control group | Other concomitant medications (all patients) |
|||||||
| Tesarik et al. [7] | RCT | GnRH-a long GnRH-antag |
250 µg r-hCG |
n: 150 GnRH-a long n: 150 GnRH-antag 0.1 mg/triptorelin Single injection D6 after OPU |
n: 150 GnRH-a long n: 150 GnRH-antag Placebo |
Vaginal micronized progesterone (400 mg/d) + estradiol valerate (4 mg/d) + r-hCG (250 µg; single dose on d of ET) | Day 3 | GnRH-a long: 29.8% 18.2% (P < 0.05) GnRH-antag: 27.1% 17.4% (P < 0.05) |
GnRH-a long: Ong PR/Tf: 46.8% 38.0% (NS) GnRH-antag: Ong PR/Tf: 44.8% 31.9% (P < 0.05) |
|
| |||||||||
| Ata et al. [16] | RCT | GnRH-a long | 10.000 IU u-hCG |
n: 285 0.1 mg/triptorelin Single injection D6 after OPU |
n: 285 Placebo |
Vaginal micronized progesterone gel (90 mg/d) | Day 3 | 21.1% 20.1% (NS) |
Ong PR: 31.2% 29.5% (NS) |
|
| |||||||||
| Isik et al. [11] | RCT | GnRH-antag | 10.000 IU u-hCG or 250 µg r-hCG |
n: 74 0.5 mg/leuprolide Single injection D6 after OPU |
n: 80 No placebo |
Vaginal micronized progesterone (600 mg/d) + hCG (single dose) | Day 3 | 26.5% 9.3% (P < 0.0001) |
Clin PR: 40.5% 20.0% (P < 0.01) |
|
| |||||||||
| Razieh et al. [10] | RCT | GnRH-a long | 10.000 IU u-hCG |
n: 90 0.1 mg/triptorelin Single injection D5 or D6 after OPU |
n: 90 Placebo |
Vaginal micronized progesterone (800 mg/d) | Days 2-3 | 12.3% 7.3% (P < 0.05) |
Clin PR: 25.5% 10.0% (P < 0.05) |
|
| |||||||||
| Ata and Urman [17] | RCT | GnRH-antag | 10.000 IU u-hCG |
n: 38 0.1 mg/triptorelin Single injection D6 after OPU |
n: 52 Placebo |
Vaginal micronized progesterone gel (90 mg/d) | Day 3 | 14.12% 27.27% (P < 0.05) |
Ong PR: 18.4% 42.31% (P < 0.05) |
|
| |||||||||
| Kung et al. [13] | Retrospective study | GnRH-a long GnRH-antag |
500 µg r-hCG |
n: 147 0.1 mg/triptorelin Single injection D6 after OPU |
n: 93 No GnRH-a |
Vaginal micronized progesterone gel (90 mg/d) or i.m. progesterone (25–50 mg/d) |
Days 3–5 | 24.5% 17.0% (P < 0.05) |
Clin PR: 49.0% 33.3% (P < 0.05) |
|
| |||||||||
| Yıldız et al. [14] | RCT | GnRH-a long | 10.000 IU u-hCG |
n: 100 1 mg/leuprolide acetate Single injection D6 after OPU |
n: 95 No placebo |
Vaginal micronized progesterone (600 mg/d) + 17β estradiol (4 mg/d) | Day 3 | 20.7% 13.3% (NS) |
Ong PR: 36.0% 27.4% (NS) |
Table 4.
Main characteristics of trials on the use of multiple doses of GnRH agonist for luteal phase support.
| Trial |
Study design |
Stimulation protocol | Ovulation trigger | Luteal phase support | Day of ET | Implantation rate (study group/control group) | (Ong/Clin) Pregnancy rate (study group/control group) | ||
|---|---|---|---|---|---|---|---|---|---|
| Study group GnRH-a |
Control group | Other concomitant medications (all patients) |
|||||||
| Fujii et al. [5] | RCT | GnRH-a long | 5.000 IU u-hCG |
n: 161 Continuous 600 µg/d IN buserelin twice daily during the luteal phase until D14 after OPU |
n: 158 No placebo |
Dydrogesterone for 14 days (10 mg/d) + i.m. hCG on the day of ET (2.500 IU) | Days 2-3 | 28.5% 19.6% (P < 0.05) |
Clin PR: 44.5% 34.3% (NS) |
|
| |||||||||
| Pirard et al. [15] |
RCT (dose finding study) | GnRH-antag | IN buserelin (study groups) 10.000 u-hCG (control group) |
IN buserelin during the luteal phase until D14 after OPU 1 every 2 d (n: 2) 1/d (n: 3) 2/d (n: 6) 3/d (n: 6) |
n: 6 Vaginal micronized progesterone (600 mg/d) |
No other drug (for study groups) | Day 3 | NA | NA |
|
| |||||||||
| Hugues et al. [18] | ESHRE abstract | GnRH-antag | 250 µg r-hCG |
n: 25 0.1 mg/triptorelin Two injections (D3 and D6 after OPU) |
n: 22 No placebo |
Vaginal micronized progesterone (400 mg/day) | Day 3 | NA | NA |
|
| |||||||||
| Isikoglu et al. [19] | RCT | GnRH-a long | 10.000 IU u-hCG |
n: 90 Continuous 0.25 mg/d leuprolide acetate during the luteal phase until 14 days after OPU |
n: 91 No placebo |
i.m. progesterone (50 g/day) | NA | 35.6% 35.3% (NS) |
Clin PR: 50.0% 52.32% (NS) |
|
| |||||||||
| Qublah et al. [9] | RCT | GnRH-a long | 10.000 IU u-hCG |
n: 60 0.1 mg/triptorelin Three injections (D of OPU, D3, and D6 after OPU) |
n: 60 Placebo |
Vaginal progesterone (pessaries: cyclogest) | Day 3 | 21.4% 7.3% (P < 0.01) |
PR: 36.6% 13.3% (P < 0.01) |
|
| |||||||||
| Inamdar and Majumdar [12] | RCT | GnRH-a long | 250 µg r-hCG |
n: 213 1 mg/leuprolide acetate Three injections (D6, D7, and D8 after OPU) |
n: 213 No placebo |
Vaginal progesterone (400 mg twice daily) alternating with i.m. natural micronized progesterone (100 mg) starting from the day of OPU | Day 2 | 17.57% 17.07% (NS) |
Ong PR: 27.69% 26.29% (NS) |
|
| |||||||||
| Yıldız et al. [14] |
RCT | GnRH-a long | 10.000 IU u-hCG |
n: 84 1 mg/leuprolide acetate Two injections D6 and D9 after OPU |
n: 95 No placebo |
Vaginal micronized progesterone (600 mg/d) + 17β estradiol (4 mg/d) | Day 3 | 25.8% 13.3% (NS) |
Ong PR: 42.9% 27.4% (NS) |
d: day; ET: embryo transfer; GnRH-a: GnRH agonist; GnRH-antag: GnRH antagonist; IU: international unit; n: number of cycles; OPU: oocyte pick-up; r: recombinant; u: urinary; PR: pregnancy rate; Clin PR: clinical pregnancy rate; Ong PR: ongoing pregnancy rate; NA: not available; NS: not significant.
Luteal phase support after COH is even more important when triggering with GnRH agonists. Previous randomized controlled trials [37, 38] found that the use of GnRH agonist to trigger ovulation was associated with negative clinical results, namely, low implantation and clinical pregnancy rates and high rates of early pregnancy loss, presumably related to luteal phase insufficiency despite standard supplementation with progesterone and estradiol [27]. Only intensive progesterone and estradiol support [33–35] and hCG [26–31] or recombinant LH [32] were able to normalize the luteal phase after GnRH agonist administration for ovulation trigger. Finally, in a very recent Cochrane review, Youssef et al. [39] reported that, in women undergoing fresh autologous IVF/ICSI cycles, GnRH agonists were associated with a lower ongoing pregnancy rate than that obtained with hCG (OR = 0.70; 95% CI: 0.54 to 0.91). However, the effect was dependent on the type of luteal support provided. The higher pregnancy rate in the hCG trigger group applied only to the GnRH agonist trigger group that received luteal support without LH activity (OR = 0.36, 95% CI: 0.21 to 0.62) [39].
Studies showing that implantation rates remain normal in oocyte recipients and frozen-thawed cycles with embryos issuing from protocols with GnRH agonist trigger [40, 41] confirm that a deficient luteal phase is the main problem leading to reduced outcomes.
In our study, similar outcome parameters were obtained when GnRH agonist was used to trigger ovulation, demonstrating that GnRH agonist (IN buserelin) is able to adequately support the luteal phase. Indeed, the implantation potential of our embryos did not appear to be hampered compared to the standard protocol using hCG for ovulation trigger and vaginal progesterone as luteal support. Furthermore, an additional study conducted in our department, in which hCG was used to trigger ovulation and GnRH agonist (without any other supplementation) to support the luteal phase, found similar pregnancy rates (data not shown) and hence corroborates the current study.
The beneficial effect of GnRH agonist during the luteal phase may be linked to its impact on the embryo or a direct or indirect effect on the endometrium. Indeed, GnRH receptors have been shown to be present in preimplantation human embryos in the luteal phase at both the mRNA and protein levels [42, 43], and different observations support the hypothesis that GnRH agonist exerts a direct beneficial effect on embryos [6, 7]. Animal experiments suggest that GnRH agonists can enhance the in vitro development of embryos [42, 44–46]. In addition, GnRH agonists appear to have a regulatory impact on the synthesis and secretion of hCG by preimplanted embryos and the placenta [7, 47, 48].
Direct action on uterine tissue may also be responsible for the effects of GnRH agonists in the luteal phase. The presence of a GnRH receptor showing a dynamic pattern (more intense in the luteal phase) was demonstrated in human endometrium, both in the epithelium and stroma, providing evidence that GnRH may play a key role as a molecular autocrine-paracrine regulator in embryonic-endometrial interactions during early implantation [49–51].
The corpus luteum is another possible GnRH agonist target, though it is questionable whether such action would occur through the secretion of pituitary hormones or by direct action in the ovary [52]. In cycles with GnRH antagonists, it is speculated that the stimulation of corpus luteum activity by GnRH agonist may result from the stimulation of LH secretion, given that, despite the blockade, the pituitary gland remains responsive to GnRH or GnRH agonist [11].
In our study, we found completely different LH profiles during the luteal phase between the two groups, with significantly higher LH levels when GnRH agonist was administered for luteal support. Although preliminary, our data suggest that maintaining LH secretion throughout the luteal phase by repeated administration of GnRH agonist could overcome the drawbacks of GnRH agonist-induced final follicular maturation followed by standard luteal support.
Besides LH-mediated stimulation of steroid production by the corpus luteum, LH activity could also have an impact on the endometrium through LH receptors expressed in the endometrium [53–55] or by promoting expression and secretion of relaxin [56], angiogenic and growth factors, and cytokines involved in implantation [57].
In conclusion, our study confirms that GnRH agonist is able to trigger ovulation and support the luteal phase in antagonist IVF cycles, showing comparable efficacy to the standard protocol. Furthermore, this new approach has several advantages over other forms of luteal support in terms of convenience for the patient, because nasal administration is easily done anywhere, is not painful, and does not require the help of a nurse. Since GnRH agonist was the only drug administered for luteal support, compared to other protocols that add GnRH agonist to their classic luteal support, this new protocol can contribute to more patient-friendly ART.
However, although all babies born in this study were in good health, our data need to be corroborated by larger series, and caution should still be exercised concerning the condition and state of health of children issuing from this protocol.
Acknowledgments
The authors are grateful to Mira Hryniuk, B.A., for reviewing the English language of the paper. The authors thank Laurence Beausaert, their data manager, Catherine Rousseau, their head nurse, Dominique Demylle, the biologist in charge of the IVF laboratory, and their teams for their contribution to this study.
Conflict of Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
References
- 1.Macklon N. S., Fauser B. C. Impact of ovarian hyperstimulation on the luteal phase. Journal of reproduction and fertility. Supplement. 2000;55:101–108. [PubMed] [Google Scholar]
- 2.Pritts E. A., Atwood A. K. Luteal phase support in infertility treatment: a meta-analysis of the randomized trials. Human Reproduction. 2002;17(9):2287–2299. doi: 10.1093/humrep/17.9.2287. [DOI] [PubMed] [Google Scholar]
- 3.Smitz J., Camus M., Devroey P., Bollen N., Tournaye H., van Steirteghem A. C. The influence of inadvertent intranasal buserelin administration in early pregnancy. Human Reproduction. 1991;6(2):290–293. doi: 10.1093/oxfordjournals.humrep.a137324. [DOI] [PubMed] [Google Scholar]
- 4.van der Linden M., Buckingham K., Farquhar C., Kremer J. A., Metwally M. Luteal phase support for assisted reproduction cycles. Cochrane Database of Systematic Reviews. 2011;(10) doi: 10.1002/14651858.CD009154.pub2.CD009154 [DOI] [PubMed] [Google Scholar]
- 5.Fujii S., Sato S., Fukui A., Kimura H., Kasai G., Saito Y. Continuous administration of gonadotrophin-releasing hormone agonist during the luteal phase in IVF. Human Reproduction. 2001;16(8):1671–1675. doi: 10.1093/humrep/16.8.1671. [DOI] [PubMed] [Google Scholar]
- 6.Tesarik J., Hazout A., Mendoza C. Enhancement of embryo developmental potential by a single administration of GnRH agonist at the time of implantation. Human Reproduction. 2004;19(5):1176–1180. doi: 10.1093/humrep/deh235. [DOI] [PubMed] [Google Scholar]
- 7.Tesarik J., Hazout A., Mendoza-Tesarik R., Mendoza N., Mendoza C. Beneficial effect of luteal-phase GnRH agonist administration on embryo implantation after ICSI in both GnRH agonist- and antagonist-treated ovarian stimulation cycles. Human Reproduction. 2006;21(10):2572–2579. doi: 10.1093/humrep/del173. [DOI] [PubMed] [Google Scholar]
- 8.Lambalk C. B., Homburg R. GnRH agonist for luteal support in IVF? Setting the balance between enthusiasm and caution. Human Reproduction. 2006;21(10):2580–2582. doi: 10.1093/humrep/del321. [DOI] [PubMed] [Google Scholar]
- 9.Qublah H., Amarin Z., Al-Quda M., et al. Luteal phase support with GnRH-a improves implantation and pregnancy rates in IVF cycles with endometrium of ≤7 mm on day of egg retrieval. Human Fertility (Camb) 2008;11(1):43–47. doi: 10.1080/14647270701704768. [DOI] [PubMed] [Google Scholar]
- 10.Razieh D. F., Maryam A. R., Nasim T. Beneficial effect of luteal-phase gonadotropin-releasing hormone agonist administration on implantation rate after intracytoplasmic sperm injection. Taiwanese Journal of Obstetrics and Gynecology. 2009;48(3):245–248. doi: 10.1016/s1028-4559(09)60297-7. [DOI] [PubMed] [Google Scholar]
- 11.Isik A. Z., Caglar G. S., Sozen E., et al. Single-dose GnRH agonist administration in the luteal phase of GnRH antagonist cycles: a prospective randomized study. Reproductive BioMedicine Online. 2009;19(4):472–477. doi: 10.1016/j.rbmo.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 12.Inamdar D. B., Majumdar A. Evaluation of the impact of gonadotropin-releasing hormone agonist as an adjuvant in luteal-phase support on IVF outcome. Journal of Human Reproductive Sciences. 2012;5(3):279–284. doi: 10.4103/0974-1208.106341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kung H. F., Chen M. J., Guua H. F., et al. Luteal phase support with decapeptyl improves pregnancy outcomes in intracytoplasmic sperm injection with higher basal follicle-stimulating hormone or lower mature oocytes. Journal of the Chinese Medical Association. 2014;77(10):524–530. doi: 10.1016/j.jcma.2014.07.001. [DOI] [PubMed] [Google Scholar]
- 14.Yıldız G. A., Şükür Y. E., Ateş C., Aytaç R. The addition of gonadotrophin releasing hormone agonist to routine luteal phase support in intracytoplasmic sperm injection and embryo transfer cycles: a randomized clinical trial. European Journal of Obstetrics & Gynecology and Reproductive Biology. 2014;182:66–70. doi: 10.1016/j.ejogrb.2014.08.026. [DOI] [PubMed] [Google Scholar]
- 15.Pirard C., Donnez J., Loumaye E. GnRH agonist as luteal phase support in assisted reproduction technique cycles: results of a pilot study. Human Reproduction. 2006;21(7):1894–1900. doi: 10.1093/humrep/del072. [DOI] [PubMed] [Google Scholar]
- 16.Ata B., Yakin K., Balaban B., Urman B. GnRH agonist protocol administration in the luteal phase in ICSI-ET cycles stimulated with the long GnRH agonist protocol: a randomized, controlled double blind study. Human Reproduction. 2008;23(3):668–673. doi: 10.1093/humrep/dem421. [DOI] [PubMed] [Google Scholar]
- 17.Ata B., Urman B. Single dose GnRH agonist administration in the luteal phase of assisted reproduction cycles: is the effect dependent on the type of GnRH analogue used for pituitary suppression? Reproductive BioMedicine Online. 2010;20(1):165–166. doi: 10.1016/j.rbmo.2009.10.022. [DOI] [PubMed] [Google Scholar]
- 18.Hugues JN., Cedrin-Durnerin I., Bsandig B., et al. Administration of gonadotropin-releasing hormone agonist during the luteal phase of GnRH-antagonist IVF cycles. Human Reproduction. 2006;21(article i3) [Google Scholar]
- 19.Isikoglu M., Ozgur K., Oehninger S. Extension of GnRH agonist through the luteal phase to improve the outcome of intracytoplasmic sperm injection. Journal of Reproductive Medicine for the Obstetrician and Gynecologist. 2007;52(7):639–644. [PubMed] [Google Scholar]
- 20.Yen S. S., Jaffe R. B., editors. Reproductive Endocrinology. Philadelphia, Pa, USA: WB Saunders; 1991. [Google Scholar]
- 21.Tavaniotou A., Albano C., Smitz J., Devroey P. Impact of ovarian stimulation on corpus luteum function and embryonic implantation. Journal of Reproductive Immunology. 2002;55(1-2):123–130. doi: 10.1016/s0165-0378(01)00134-6. [DOI] [PubMed] [Google Scholar]
- 22.Tavaniotou A., Albano C., Smitz J., Devroey P. Effect of clomiphene citrate on follicular and luteal phase luteinizing hormone concentrations in in vitro fertilization cycles stimulated with gonadotropins and gonadotropin-releasing hormone antagonist. Fertility and Sterility. 2002;77(4):733–737. doi: 10.1016/s0015-0282(01)03265-4. [DOI] [PubMed] [Google Scholar]
- 23.Beckers N. G. M., Macklon N. S., Eijkemans M. J., et al. Nonsupplemented luteal phase characteristics after the administration of recombinant human chorionic gonadotropin, recombinant luteinizing hormone, or gonadotropin-releasing hormone (GnRH) agonist to induce final oocyte maturation in in vitro fertilization patients after ovarian stimulation with recombinant follicle-stimulating hormone and gnrh antagonist cotreatment. The Journal of Clinical Endocrinology & Metabolism. 2003;88(9):4186–4192. doi: 10.1210/jc.2002-021953. [DOI] [PubMed] [Google Scholar]
- 24.Albano C., Smitz J., Tournaye H., Riethmüller-Winzen H., Van Steirteghem A., Devroey P. Luteal phase and clinical outcome after human menopausal gonadotrophin/gonadotrophin releasing hormone antagonist treatment for ovarian stimulation in in-vitro fertilization/intracytoplasmic sperm injection cycles. Human Reproduction. 1999;14(6):1426–1430. doi: 10.1093/humrep/14.6.1426. [DOI] [PubMed] [Google Scholar]
- 25.Smitz J., Bourgain C., van Waesberghe L., Camus M., Devroey P., van Steirteghem A. C. A prospective randomized study on oestradiol valerate supplementation in addition to intravaginal micronized progesterone in buserelin and HMG induced superovulation. Human Reproduction. 1993;8(1):40–45. doi: 10.1093/oxfordjournals.humrep.a137871. [DOI] [PubMed] [Google Scholar]
- 26.Humaidan P., Bredkjær H. E., Westergaard L. G., Andersen C. Y. 1,500 IU human chorionic gonadotropin administered at oocyte retrieval rescues the luteal phase when gonadotropin-releasing hormone agonist is used for ovulation induction: a prospective, randomized, controlled study. Fertility and Sterility. 2010;93(3):847–854. doi: 10.1016/j.fertnstert.2008.12.042. [DOI] [PubMed] [Google Scholar]
- 27.Castillo J. C., Dolz M., Bienvenido E., Abad L., Casan E. M., Bonilla-Musoles F. Cycles triggered with GnRH agonist: exploring low-dose HCG for luteal support. Reproductive BioMedicine Online. 2010;20(2):175–181. doi: 10.1016/j.rbmo.2009.11.018. [DOI] [PubMed] [Google Scholar]
- 28.Radesic B., Tremellen K. Oocyte maturation employing a GnRH agonist in combination with low-dose hCG luteal rescue minimizes the severity of ovarian hyperstimulation syndrome while maintaining excellent pregnancy rates. Human Reproduction. 2011;26(12):3437–3442. doi: 10.1093/humrep/der333. [DOI] [PubMed] [Google Scholar]
- 29.Kol S., Humaidan P., Itskovitz-Eldor J. GnRH agonist ovulation trigger and hCG-based, progesterone-free luteal support: a proof of concept study. Human Reproduction. 2011;26(10):2874–2877. doi: 10.1093/humrep/der220. [DOI] [PubMed] [Google Scholar]
- 30.Iliodromiti S., Lan V. T. N., Tuong H. M., Tuan P. H., Humaidan P., Nelson S. M. Impact of GnRH agonist triggering and intensive luteal steroid support on live-birth rates and ovarian hyperstimulation syndrome: a retrospective cohort study. Journal of Ovarian Research. 2013;6(1, article 93) doi: 10.1186/1757-2215-6-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Humaidan P., Thomsen L. H., Alsbjerg B. GnRHa trigger and modified luteal support with one bolus of hCG should be used with caution in extreme responder patients. Human Reproduction. 2013;28(9):2593–2594. doi: 10.1093/humrep/det287. [DOI] [PubMed] [Google Scholar]
- 32.Papanikolaou E. G., Verpoest W., Fatemi H., Tarlatzis B., Devroey P., Tournaye H. A novel method of luteal supplementation with recombinant luteinizing hormone when a gonadotropin-releasing hormone agonist is used instead of human chorionic gonadotropin for ovulation triggering: a randomized prospective proof of concept study. Fertility and Sterility. 2011;95(3):1174–1177. doi: 10.1016/j.fertnstert.2010.09.023. [DOI] [PubMed] [Google Scholar]
- 33.Engmann L., DiLuigi A., Schmidt D., Benadiva C., Maier D., Nulsen J. The effect of luteal phase vaginal estradiol supplementation on the success of in vitro fertilization treatment: a prospective randomized study. Fertility and Sterility. 2008;89(3):554–561. doi: 10.1016/j.fertnstert.2007.04.006. [DOI] [PubMed] [Google Scholar]
- 34.Shapiro B. S., Daneshmand S. T., Garner F. C., Aguirre M., Hudson C. Comparison of ‘triggers’ using leuprolide acetate alone or in combination with low-dose human chorionic gonadotropin. Fertility and Sterility. 2011;95(8):2715–2717. doi: 10.1016/j.fertnstert.2011.03.109. [DOI] [PubMed] [Google Scholar]
- 35.Orvieto R. Intensive luteal-phase support with oestradiol and progesterone after GnRH-agonist triggering: does it help? Reproductive BioMedicine Online. 2012;24(6):680–681. doi: 10.1016/j.rbmo.2012.03.005. [DOI] [PubMed] [Google Scholar]
- 36.Balasch J., Martinez F., Jove I., et al. Inadvertent gonadotrophin-releasing hormone agonist (GnRHa) administration in the luteal phase may improve fecundity in in-vitro fertilization patients. Human Reproduction. 1993;8(7):1148–1151. doi: 10.1093/oxfordjournals.humrep.a138210. [DOI] [PubMed] [Google Scholar]
- 37.Humaidan P., Bredkjær H. E., Bungum L., et al. GnRH agonist (buserelin) or hCG for ovulation induction in GnRH antagonist IVF/ICSI cycles: a prospective randomized study. Human Reproduction. 2005;20(5):1213–1220. doi: 10.1093/humrep/deh765. [DOI] [PubMed] [Google Scholar]
- 38.Kolibianakis E. M., Schultze-Mosgau A., Schroer A., et al. A lower ongoing pregnancy rate can be expected when GnRH agonist is used for triggering final oocyte maturation instead of HCG in patients undergoing IVF with GnRH antagonists. Human Reproduction. 2005;20(10):2887–2892. doi: 10.1093/humrep/dei150. [DOI] [PubMed] [Google Scholar]
- 39.Youssef M. A., Van der Veen F., Al-Inany H. G., et al. Gonadotropin-releasing hormone agonist versus HCG for oocyte triggering in antagonist assisted reproductive technology cycles. Cochrane Database of Systematic Reviews. 2011;(11) doi: 10.1002/14651858.CD008046.pub2.CD008046 [DOI] [PubMed] [Google Scholar]
- 40.Acevedo B., Gomez-Palomares J. L., Ricciarelli E., Hernández E. R. Triggering ovulation with gonadotropin-releasing hormone agonists does not compromise embryo implantation rates. Fertility and Sterility. 2006;86(6):1682–1687. doi: 10.1016/j.fertnstert.2006.05.049. [DOI] [PubMed] [Google Scholar]
- 41.Griesinger G., Kolibianakis E. M., Papanikolaou E. G., et al. Triggering of final oocyte maturation with gonadotropin-releasing hormone agonist or human chorionic gonadotropin. Live birth after frozen-thawed embryo replacement cycles. Fertility and Sterility. 2007;88(3):616–621. doi: 10.1016/j.fertnstert.2006.12.006. [DOI] [PubMed] [Google Scholar]
- 42.Casañ E. M., Raga F., Polan M. L. GnRH mRNA and protein expression in human preimplantation embryos. Molecular Human Reproduction. 1999;5(3):234–239. doi: 10.1093/molehr/5.3.234. [DOI] [PubMed] [Google Scholar]
- 43.Casañ E. M., Raga F., Bonilla-Musoles F., Polan M. L. Human oviductal gonadotropin-releasing hormone: possible implications in fertilization, early embryonic development, and implantation. The Journal of Clinical Endocrinology & Metabolism. 2000;85(4):1377–1381. doi: 10.1210/jc.85.4.1377. [DOI] [PubMed] [Google Scholar]
- 44.Raga F., Casañ E. M., Kruesse J., Wen Y., Bonilla-Musoles F., Polan M. L. The role of gonadotropin-releasing hormone in murine preimplantation embryonic development. Endocrinology. 1999;140(8):3705–3712. doi: 10.1210/endo.140.8.6899. [DOI] [PubMed] [Google Scholar]
- 45.Kawamura K., Fukuda J., Kumagai J., et al. Gonadotropin-releasing hormone I analog acts as an anti-apoptotic factor in mouse blastocysts. Endocrinology. 2005;146(9):4105–4116. doi: 10.1210/en.2004-1646. [DOI] [PubMed] [Google Scholar]
- 46.Nam D. H., Lee S. H., Kim H. S., et al. The role of gonadotropin-releasing hormone (GnRH) and its receptor in development of porcine preimplantation embryos derived from in vitro fertilization. Theriogenology. 2005;63(1):190–201. doi: 10.1016/j.theriogenology.2004.04.004. [DOI] [PubMed] [Google Scholar]
- 47.Lin L.-S., Roberts V. J., Yen S. S. Expression of human gonadotropin-releasing hormone receptor gene in the placenta and its functional relationship to human chorionic gonadotropin secretion. Journal of Clinical Endocrinology and Metabolism. 1995;80(2):580–585. doi: 10.1210/jcem.80.2.7852524. [DOI] [PubMed] [Google Scholar]
- 48.Islami D., Chardonnens D., Campana A., Bischof P. Comparison of the effects of GnRH-I and GnRH-II on HCG synthesis and secretion by first trimester trophoblast. Molecular Human Reproduction. 2001;7(1):3–9. doi: 10.1093/molehr/7.1.3. [DOI] [PubMed] [Google Scholar]
- 49.Raga F., Casañ E. M., Kruessel J. S., et al. Quantitative gonadotropin-releasing hormone gene expression and immunohistochemical localization in human endometrium throughout the menstrual cycle. Biology of Reproduction. 1998;59(3):661–669. doi: 10.1095/biolreprod59.3.661. [DOI] [PubMed] [Google Scholar]
- 50.Shemesh M. Actions of gonadotrophins on the uterus. Reproduction. 2001;121(6):835–842. doi: 10.1530/rep.0.1210835. [DOI] [PubMed] [Google Scholar]
- 51.Klemmt P. A. B., Liu F., Carver J. G., et al. Effects of gonadotrophin releasing hormone analogues on human endometrial stromal cells and embryo invasion in vitro. Human Reproduction. 2009;24(9):2187–2192. doi: 10.1093/humrep/dep181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Oliveira J. B. A., Baruffi R., Petersen C. G., Mauri A. L., Cavagna M., Franco J. G., Jr. Administration of single-dose GnRH agonist in the luteal phase in ICSI cycles: a meta-analysis. Reproductive Biology and Endocrinology. 2010;8, article 107 doi: 10.1186/1477-7827-8-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Stewart E. A. Gonadotropins and the uterus: is there a gonad-independent pathway? Journal of the Society for Gynecologic Investigation. 2001;8(6):319–326. doi: 10.1016/s1071-5576(01)00136-8. [DOI] [PubMed] [Google Scholar]
- 54.Rao C. V., Lei Z. M. Consequences of targeted inactivation of LH receptors. Molecular and Cellular Endocrinology. 2002;187(1-2):57–67. doi: 10.1016/S0303-7207(01)00694-3. [DOI] [PubMed] [Google Scholar]
- 55.Tesarik J., Hazout A., Mendoza C. Luteinizing hormone affects uterine receptivity independently of ovarian function. Reproductive BioMedicine Online. 2003;7(1):59–64. doi: 10.1016/S1472-6483(10)61729-4. [DOI] [PubMed] [Google Scholar]
- 56.Loumaye E., Depreester S., Donnez J., Thomas K. Immunoreactive relaxin surge in the peritoneal fluid of women during the midluteal phase. Fertility and Sterility. 1984;42(6):856–860. doi: 10.1016/s0015-0282(16)48256-7. [DOI] [PubMed] [Google Scholar]
- 57.Licht P., Russu V., Wildt L. On the role of human chorionic gonadotropin (hCG) in the embryo-endometrial microenvironment: Implications for differentiation and implantation. Seminars in Reproductive Medicine. 2001;19(1):37–47. doi: 10.1055/s-2001-13909. [DOI] [PubMed] [Google Scholar]