The impact of pain does not end when a painful experience is over. Children’s pain memories play a powerful role in their pain experiences [9; 22] and may be a mechanism underlying the persistence of pain [13]. Pain memories are vulnerable to distortion and this malleability has implications for future pain [37; 24]. Therefore, identification of predictors of children’s pain memories may inform effective intervention and prevention of maladaptive future responses to painful events.
The Pediatric Fear-Avoidance Model of Chronic Pain [1] posits that parent cognitive-affective factors and behaviors interact with those of the child to influence pain. Parents who perceive a high degree of threat upon observing their child in pain are more likely to experience distress and behave in ways that signal threat to and evoke fear in their child [15; 6], thereby exacerbating child pain and fear-avoidance [1]. It is likely that this affective process also influences parents’ own cognitions about their child’s pain [24]. Parents’ memories of child pain may be an important and modifiable cognitive factor underlying children’s pain experiences, influencing parent-child interactions about pain and children’s cognitions and behaviors.
In addition to children’s general tendency to perceive threat and experience anxiety [33; 23; 24], children’s and parents’ catastrophizing about child pain have been posited as factors influencing pain memory development [24]. In particular, specific aspects (i.e., individual subscales) of parent and child pain catastrophizing (i.e., parent rumination and helplessness; child magnification) have been found to differentially influence other cognitive biases among children (selective attention; [36]), highlighting the importance of examining catastrophizing as a multidimensional construct in this context.
Children’s catastrophic thinking about pain increases the threat value of pain and contributes to attentional biases [24], which may lead to heightened pain perception and subsequently, more distressing pain memories. Parents’ catastrophic thinking may also negatively influence the child’s pain experience which may, in turn, lead parents to develop more distressing memories about their child’s pain. Indeed, child pain is a powerful communicative signal of threat to high catastrophizing parents, influencing their attention [7], inducing self-oriented distress [16; 6], and instigating attempts to control and avoid child pain [6; 5]. Although parent and child catastrophizing have been associated with persistent post-surgical pain [29; 27; 12], this is the first longitudinal study to examine children’s and parents’ pain catastrophizing prior to major surgery and its relationship to pain memory development.
We hypothesized that high baseline child and parent catastrophizing about child pain would be associated with children’s and parents’ recall of high levels of child pain intensity and pain-related emotional distress two to four months after surgery. Moreover, we hypothesized that these relationships would be mediated through the child’s pain experience in the acute recovery phase following surgery. Given the dearth of research in this area, we did not make specific hypotheses regarding the differential influence of individual pain catastrophizing subscales on memory. Given limited longitudinal data on the reciprocal relationships between children’s and parents’ pain-related cognitions and emotions, relationships between parent and child catastrophizing and children’s and parents’ memories of pain, respectively, were also explored.
Method
Participants and Setting
Sixty children and their parents enrolled in a longitudinal study examining predictors of post-surgical pain were eligible for participation in the current study. These 60 children and their parents were enrolled in person or by telephone from 110 eligible children identified from surgery schedules over a 21-month period. Children were eligible if they were between the ages of 10–18 years and undergoing either spinal fusion or pectus repair surgeries. Spinal fusion and pectus repair were chosen based on prior literature showing that children undergoing these surgeries are at risk for experiencing acute and persistent post-surgical pain [17; 38; 29; 27; 34; 10].
Participants were excluded from the study if they did not speak English and/or if the child had a serious comorbid health condition (e.g. cancer, diabetes) or had undergone prior major surgery. Of the 60 participants enrolled in the larger study, 57 were contacted to take part in the memory study given that three participants had been enrolled in the larger study prior to receiving IRB approval for the current study. Two children did not complete assessment measures at included time points, one dropped out of the study, and five could not be reached for the memory interview within the time window required for participation (i.e., between two to four months after surgery).
Participants therefore included 49 children and adolescents (32 girls, 17 boys; Mage = 14.70 years, SD = 1.98, Range = 10–18 years) undergoing major surgery and their parents (89.4% mothers). Children were undergoing surgery for either spinal fusion (n=40) or pectus repair (n=9). The average surgery duration was 5 hours, 2 minutes (SD=1 hour, 28 minutes). The majority of children were white (91.5%) and most participants (61.7%) reported an average family income of more than $70 000.
Ethical approval for this study was obtained from the research center’s institutional research board (IRB).
Procedure
During the week immediately prior to surgery, participants completed an at-home assessment, which was mailed to them. The child completed a daily electronic pain diary, and the child and parent completed the pain catastrophizing measures and pain questionnaires (described below). All pre-surgery study materials were collected in- person on the day of surgery. Participants were mailed the post-surgical assessment two weeks following surgery, which they completed in their homes. This assessment consisted of the child and parent Pain Questionnaires as well as a daily electronic pain diary for children to complete. Participants mailed these study materials back after completing the assessment. Participants received gift cards to a local retail store ($10.00 USD for parents, $20.00 USD for children) after completing the baseline and two week post-surgery assessments.
Approximately 2.5 months following surgery (M = 76.80 days, SD = 15.39 days, Range = 52–110 days), a researcher contacted parents and children over the telephone to conduct the memory interviews. Previous memory research has used time frames ranging from one week to one year [2; 9]. Parents and children completed the memory interviews out of earshot of each other so as to not bias their recall. The memory assessment followed a similar protocol to that used with children and adolescents examining children’s memory for venipuncture [25] and cold pressor pain [2; 22; 23]. Prior to answering the four memory questions, children and parents were asked to first recall when they/their child were at home in the first few weeks following surgery. They were then asked to rate the levels of pain intensity and pain-related emotional distress that they remembered that they/their child experienced during that time using the same pain scales administered at the post-surgery assessment time point.
Measures
Demographics
Information on race/ethnicity and family household annual income was obtained via parent report on a demographic questionnaire. Child age and sex were obtained from children’s medical records.
Daily electronic pain diary
Children completed an electronic diary for seven days in which they rated their pain intensity each day. Children started the daily electronic diary monitoring one week prior to surgery (pre-surgery assessment) and again two weeks post-surgery (two week follow-up assessment). Pain intensity was rated at the end of the day (in the evening) using an 11-point numerical rating scale (NRS) (anchors: 0 = no pain, 10 = worst pain). Numerical ratings scales are a valid and reliable tool to assess pain intensity and are recommended for assessment of pain intensity for acute pediatric postsurgical pain in youth [28]. Prospectively captured pain scores minimize recall biases. For the purposes of analyses, average pain scores were computed for pain intensity ratings obtained during each recording period. The average pain score assessed two weeks post-surgery served as the primary sensory measure of experienced pain.
Pain Questionnaire – Child
This self-report measure includes seven items assessing pain frequency, location, duration, intensity, emotional distress, and interference. For the purposes of the present study, we utilized the item assessing pain- related emotional distress. This item is rated on a five point Likert scale assessing how much aches or pain bothered or upset the child during the last seven days (anchors: 1 = not at all, 5 = very much) [21]. The Pain Questionnaire has demonstrated adequate validity in children for rating pain-related emotional distress [31]. Child-report of pain- related emotional distress served as the primary affective measure of experienced pain.
Pain Questionnaire – Parent
The parent version of the Pain Questionnaire contains identical questions as the child version but is instead based on parent proxy report. For the purposes of the present study, we utilized two items assessing parent proxy ratings of child pain-related emotional distress and pain intensity. Pain-related emotional distress was rated using a five point Likert scale assessing how much aches or pains bothered or upset the child during the past seven days (anchors: 1 = not at all, 5 = very much [21]). Parental perception of their child’s pain intensity was rated using an 11- point numerical rating scale (NRS; anchors: 0=no pain, 10=worst pain).
Pain Catastrophizing Scale – Child and Parent versions (PCS-C and PCS-P)
The PCS-C is a 13-item self-report measure that assesses children’s catastrophic thoughts and feelings about their pain [11]. The PCS-P is a 13-item self-report measure that assesses catastrophic thoughts and feelings that parents may have when their child experiences pain [15]. Items on both the PCS-C and PCS-P are rated on a five point Likert scale yielding a total score and three subscale scores: rumination, magnification, and helplessness. On the PCS-C, children rate the extent to which they experience each thought or feeling when they are in pain (“When I have pain I feel I can’t go on”). On the PCS-P, parents rate the extent to which they experience each thought or feeling when their child is in pain (“When my child is in pain, I feel I can’t go on like this much longer”). Lower scores indicate less rumination, magnification or helplessness about child pain. The PCS-C and PCS-P have been found to have good validity and reliability in youth with pain [11] and their parents [15], respectively.
As previously mentioned, PCS-P rumination (i.e., perseveration of thoughts pertaining to suffering and avoidance) and helplessness (i.e., tendency to perceive oneself as being helpless in the face of pain) subscales and PCS-C magnification (i.e., exaggerating negative consequences of pain) subscales have been shown to influence children’s attentional biases for pain [36]. This supports its role as a multidimensional construct and underscores the importance of examining individual subscales in examinations of cognitive biases for pain, which informed our analytic plan.
Memory
At two to four months following surgery, a memory interview was conducted with parents and children. They were each asked to remember the levels of sensory (pain intensity) and affective (pain-related emotional distress) pain that children experienced two weeks following surgery. The four questions were directly adapted from the NRS and Likert scales administered in the electronic pain diary and the parent and child versions of the Pain Questionnaire. Memories for pain intensity and pain-related emotional distress were elicited due to the multidimensional nature of pain memories [26] and the importance of examining these aspects of recall separately due to different relationships with aspects of the child’s pain experience [22]. Prior to answering each memory question, children and parents were first asked to remember when the child was at home in the first few weeks following surgery. Then, they were asked to rate the average level of pain intensity that they remembered that they/their child experienced during that time using the same 11-point NRS. Similarly, they were asked to rate the average level of pain-related emotional distress that they remembered that they/their child experienced during that time using the same five point Likert scales. Telephone interviews for research on children’s memory for cold pressor, venipuncture, and in hospital pain have been effectively conducted with children and adolescents of similar ages [18; 40; 25; 22; 23].
Data Analysis
Analyses were conducted using the Statistical Package for the Social Sciences (SPSS) version 19.0. Descriptive, correlational, regression, and mediation analyses were conducted using two-tailed hypothesis testing.
Differences between parents and children on key variables were assessed using t- tests. Bivariate Pearson correlations were conducted between the key variables to justify their inclusion in regression models [14; 22]. In order to be entered in the regression models, child and parent pain catastrophizing subscales had to be significantly related to an aspect of pain memories. Chi square and t-tests were conducted to determine whether there were differences in key variables as a function of child sex and age. Similar to the approach taken by Gedney and Logan [13] and Noel and colleagues [21], hierarchical linear regression modeling was used to test pain catastrophizing (magnification, rumination, helplessness subscales) as a predictor of children’s and parents’ sensory (pain intensity) and affective (pain-related emotional distress) memories. Models examining the influence of parent catastrophizing on pain memories included child catastrophizing (total score) as a covariate. Likewise, models examining the influence of child catastrophizing on pain memories included parent catastrophizing (total score) as a covariate. In addition, all regression models controlled for two-week post-surgery pain ratings (pertaining to the specific memory question examined).
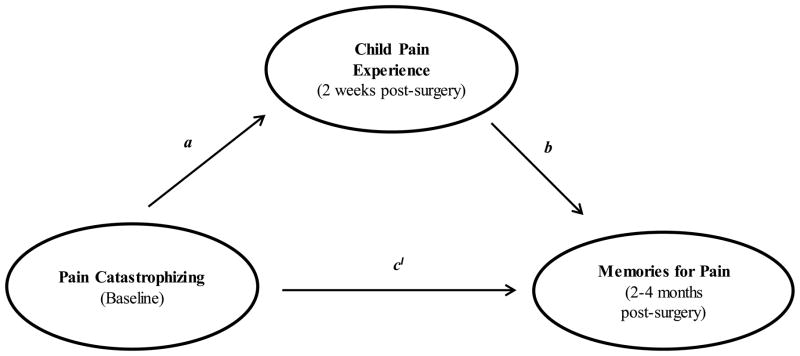
An additional aim of the study was to test whether the child’s pain experience two weeks post-surgery would mediate the associations between parent and child pain catastrophizing and their memories for pain. To test for mediation, the various effects and their corresponding weights were examined (Figure 1). The total effect of pain catastrophizing on pain memories (weight c) was comprised of a direct effect of pain catastrophizing on pain memories (weight c1), and an indirect effect of pain catastrophizing on pain memories through the mediator, children’s pain reported two weeks following surgery (weight ab). Weight a represents the effect of pain catastrophizing on child pain and weight b corresponds to the effect of child pain on pain memories partialling out the effect of pain catastrophizing [6]. A direct effect does not need to be significant to test for mediation; rather, the indirect effect is of primary importance in establishing mediation. As such, mediation models were tested even if pain catastrophizing was not significantly related to pain memories. For a mediation model to be tested, pain catastrophizing had to be related to an aspect of the child’s pain experience two weeks post-surgery (i.e., pain intensity or pain-related emotional distress; path a). Likewise, experienced pain (pain intensity or pain-related emotional distress) had to be related to an aspect of subsequent pain memories (path b). When mediated effects exist in the absence of a significant direct effect, mediation is referred to as indirect-only mediation [36].
Figure 1.
Graphic depiction of the hypothesized mediation model.
To test the indirect effect, the Preacher and Hayes [31] bootstrapping macro was used to test for the significance of indirect effects while controlling for child or parent catastrophizing (depending on whether parent or child catastrophizing, respectively, was tested in the mediation model). The bootstrapping method of testing the significance of the indirect effect is preferred over more traditional methods (e.g., the Sobel test) because it does not assume normality and reduces the chance of Type II errors by limiting the number of parameter estimates and maximizing power with small samples [31]. These analyses produced 1) empirical approximations of the product of the estimated coefficients’ sampling distribution in the direct path, 2) percentile based bootstrap confidence intervals, and 3) bootstrap measures of standard errors using 5000 resamples with replacement from the data [31]. The presence of a significant indirect effect is indicated when zero is not contained between the upper and lower limits of the confidence interval suggesting with 95% confidence that the indirect effect is not zero.
Results
Descriptive Statistics
Descriptive data for all included parent and child measures obtained at baseline, two weeks post-surgery, and during the memory interview are shown in Table 1. As would be expected, children’s postsurgical pain at the two-week follow-up assessment was higher than their baseline pain intensity reported the week before surgery (t (89) = 2.78, p < .01). Parents and children reported similar levels of pain catastrophizing (p’s > .05). There were no differences between parents’ and children’s ratings of pain intensity or pain-related emotional distress two weeks following surgery or their subsequent memories for pain-related emotional distress (p’s > .05). However, children recalled higher levels of pain intensity (t (95) = 2.58, p < .05) as compared to parents. There were no significant differences in any of the catastrophizing or memory variables as a function of child sex or age (p’s > .05).
Table 1.
Descriptive data for key child and parent variables across time points.
| Variable; Time points | Child-report M (SD) Observed Range |
Parent-report M (SD) Observed Range |
|---|---|---|
| Child pain catastrophizing (PCS-C), magnification subscale; baseline | 1.93 (2.11) 0.00–7.00 |
- |
| Child pain catastrophizing (PCS-C), rumination subscale; baseline | 6.69 (3.47) 0.00–12.19 |
- |
| Child pain catastrophizing (PCS-C), helplessness subscale; baseline | 3.70 (3.81) 0.00–13.40 |
|
| Child pain catastrophizing (PCS-C) total score; baseline | 12.32 (8.17) 0.00–32.59 |
- |
| Parent catastrophizing about child pain (PCS-P), magnification subscale; baseline | - | 2.63 (2.65) 0.00–9.00 |
| Parent catastrophizing about child pain (PCS-P), rumination subscale; baseline | - | 8.13 (4.36) 0.00–16.00 |
| Parent catastrophizing about child pain (PCS-P), helplessness subscale; baseline | 4.25 (4.54) 0.00–18.00 |
|
| Parent catastrophizing about child pain (PCS-P), total score; baseline | - | 15.00 (10.42) 0.00–41.00 |
| Pain intensity (NRS); baseline | 2.39 (2.33) 0.00–9.00 |
- |
| Pain-related emotional distress (NRS); baseline | 2.37 (0.82) 1.00–5.00 |
2.33 (0.82) 1.00–4.00 |
| Pain intensity (NRS); two weeks following surgery | 3.70 (2.13) 0.00–8.25 |
3.17 (1.76) 0.00–7.00 |
| Pain-related emotional distress (NRS); two weeks following surgery | 2.47 (0.87) 1.00–4.00 |
2.59 (0.96) 1.00–5.00 |
| Recalled pain intensity (NRS); two to four months following surgery | 5.33 (1.98) 2.00–9.00 |
4.35 (1.79) 2.00–9.00 |
| Recalled pain–related emotional distress (NRS); two to four months following surgery | 2.88 (0.79) 2.00–5.00 |
3.04 (0.93) 2.00–5.00 |
Correlational Analyses
Results of the correlational analyses are shown in Table 2. Greater parental catastrophizing about their child’s pain at baseline by magnifying the threat value of pain (magnification) and feeling helpless upon witnessing their child in pain (helplessness) was associated with children remembering experiencing more pain-related emotional distress two weeks following surgery (r = .42, p < .01; r = .35, p < .05, respectively). Similarly, higher parental magnification of pain was associated with parents remembering more pain-related child emotional distress in the weeks following surgery (r = .29, p < .05). Higher parental perseveration on the threatening details of the child’s pain experience (rumination) was associated with parental memories of higher child pain intensity (r = .34, p < .05). Parent rumination was also the only aspect of pain catastrophizing that was related to children’s pain intensity two weeks following surgery (r = .34, p < .05). Child helplessness was the only aspect of pain catastrophizing that was related to children’s pain-related emotional distress two weeks after surgery (r = .36, p < .05).
Table 2.
Correlations among the key variables.
| N = 49 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. PCS-C (magnification) | 1.00 | .54** | .71** | .23 | .10 | .26 | .12 | .13 | −.24 | .24 | −.17 | .15 | −.24 | .06 |
| 2. PCS-C (rumination) | 1.00 | .63** | .23 | .28 | .19 | .06 | .34* | .02 | .18 | −.03 | .02 | −.05 | .05 | |
| 3. PCS-C (helplessness) | 1.00 | .21 | .24 | .35* | .51** | .55*** | .07 | .36* | −.01 | .23 | .02 | .16 | ||
| 4. PCS-P (magnification) | 1.00 | .63** | .83** | .17 | .20 | .22 | .18 | .11 | .42** | .25 | .29* | |||
| 5. PCS-P (rumination) | 1.00 | .69** | .18 | .28 | .34* | .16 | .05 | .24 | .34* | .22 | ||||
| 6. PCS-P (helplessness) | 1.00 | .31* | .26 | .23 | .23 | .04 | .35* | .15 | .25 | |||||
| 7. Pain intensity baseline (child report) | 1.00 | .59*** | .52*** | .22 | .29 | .28 | .21 | .20 | ||||||
| 8. Pain-related emotional distress baseline (child report) | 1.00 | .51** | .48** | .19 | .25 | .33* | .32* | |||||||
| 9. Pain intensity two weeks post-surgery (child report) | 1.00 | .50** | .68** | .34* | .50** | .35* | ||||||||
| 10. Pain-related emotional distress two weeks post-surgery (child report) | 1.00 | .48** | .39** | .34* | .36* | |||||||||
| 11. Child memory of pain intensity | 1.00 | .37* | .36* | .32* | ||||||||||
| 12. Child memory of emotional distress | 1.00 | .34* | .62** | |||||||||||
| 13. Parent memory of pain intensity | 1.00 | .58** | ||||||||||||
| 14. Parent memory of emotional distress | 1.00 |
Note:
p < .05,
p < .01
Contrary to our hypotheses, child catastrophizing was not related to any aspects of children’s or parents’ recall or their pain two weeks following surgery; therefore, it was not included in any of the regression models except as a covariate (PCS-C total score) when examining relationships between parent catastrophizing and recall. However, given that child helplessness was related to pain-related emotional distress, indirect only mediation models were tested with this particular PCS-C subscale.
Children’s two-week post-surgery pain intensity and pain-related emotional distress were related to all aspects of children’s and parents’ pain memories (p’s < .05). Children’s report of baseline pain intensity was not related to any aspect of children’s or parents’ pain memories. Children’s report of baseline pain-related emotional distress was related to parents’ subsequent recall of child post-operative pain intensity and pain- related emotional distress (r = .33, p < .05; r = .32, p < .05, respectively); therefore, baseline emotional distress was controlled for in the respective regression analyses.
Hierarchical Regression Analyses
The results of the regression analyses are shown in Table 3. Hierarchical regression analyses were conducted to examine the contribution of pain catastrophizing to children’s and parents’ memories for pain. Based on correlational analyses, four regressions were conducted, two for the prediction of children’s pain memories and two for the prediction of parents’ pain memories.
Table 3.
Hierarchical regression analysis explaining children’s and parents’ pain memories.
| Criterion Variable | Step | Predictor | Beta | ΔR2 | Cumulative R2 |
|---|---|---|---|---|---|
|
| |||||
| Children’s memory of pain-related emotional distress | 1 | PCS-C (total) | .054 | .003 | .003 |
| 2 | Experienced post-operative pain-related emotional distress (child report) | .360 | .121* | .124 | |
| 3 | PCS-P (magnification) | .491 | .220** | .344 | |
|
| |||||
| Children’s memory of pain-related emotional distress | 1 | PCS-C (total) | .054 | .003 | .003 |
| 2 | Experienced post-operative pain-related emotional distress (child report) | .360 | .121* | .124 | |
| 3 | PCS-P (helplessness) | .256 | .058 | .182 | |
|
| |||||
| Parents’ memory of child pain intensity | 1 | PCS-C (total), Baseline pain-related emotional distress (child report) | −.251, .446 | .166* | .166 |
| 2 | Experienced child post-operative pain intensity (parent report) | .445 | .134* | .300 | |
| 3 | PCS-P (rumination) | .294 | .077* | .378 | |
|
| |||||
| Parents’ memory of child pain-related emotional distress | 1 | PCS-C (total), Baseline pain-related emotional distress (child report) | −.157, .364 | .108 | .108 |
| 2 | Experienced post-operative child pain-related emotional distress (parent report) | .584 | .257*** | .365 | |
| 3 | PCS-P (magnification) | .268 | .058 | .423 | |
Note:
p < .05,
p < .01,
p < .001
Children’s Pain Memories
After controlling for child pain catastrophizing total scores and experienced pain-related emotional distress, parent catatastrophizing about child pain (magnification) accounted for a significant portion of variance in children’s affective pain memories. This suggests that parents’ levels of pain catastrophizing at baseline influenced children’s memories of their post-surgical pain experience as being more emotionally distressing. As expected, experienced pain-related emotional distress two weeks post-surgery was also a unique predictor of children’s recalled pain-related emotional distress. Collectively, this model accounted for 34% of the variance in children’s affective pain memories with parent catastrophizing uniquely accounting for 22% of the variance. Conversely, parental catastrophizing about child pain (helplessness) did not predict children’s memories of emotional distress, over and above their initial ratings of emotional distress two weeks post-surgery.
Parents’ Pain Memories
After controlling for child pain catastrophizing total scores, child report of baseline pain-related emotional distress, and parents’ ratings of child post-operative pain intensity, parent catastrophizing about child pain (rumination) accounted for a significant portion of variance in parents’ memories of child pain intensity. As expected, child report of baseline emotional distress and parent’s initial ratings of child post-operative pain intensity were also significantly related to their subsequent recall. Collectively, this model accounted for approximately 38% of the variance in parents’ pain memories with parent catastrophizing uniquely accounting for 8% of the variance. Parent magnification was not a significant predictor of parents’ affective pain memories, over and above their initial proxy ratings of child distress and the other covariates.
Mediation Analyses
The Mediating Role of Child Pain in the Acute Recovery Period in the relationship between Child Catastrophizing and Pain Memories
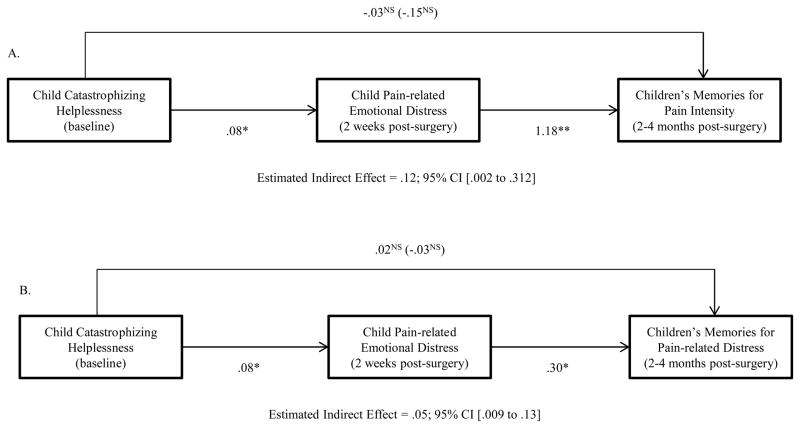
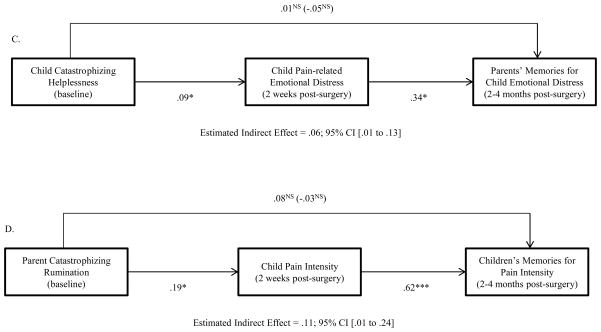
An additional aim was to examine the mediating role of children’s experienced pain after surgery in the relationship between catastrophic thinking and pain memories. Specifically, it was hypothesized that child pain catastrophizing at baseline would influence pain recall at two to four months post-surgery through the child’s pain experience two weeks post-surgery, while controlling for total parent catastrophizing scores. Analyses revealed that the relationship between child catastrophizing (helplessness) and children’s sensory pain memories (recalled pain intensity) was explained by higher levels of experienced emotional distress two weeks post-surgery (95% CI Lower to Upper = .002 to .312; See Figure 2a). Likewise, the relationship between child catastrophizing (helplessness) and children’s affective pain memories (recalled pain-related emotional distress) was explained by higher levels of experienced emotional distress two weeks post-surgery (95% CI Lower to Upper = .009 to .13; See Figure 2b). Children’s pain experience accounted for 26% and 22% of the variance in the relationships between children’s catastrophic thinking and sensory and affective pain memories, respectively. Moreover, children’s catastrophic thinking (helplessness) influenced parents’ affective pain memories through the child’s experience of pain-related emotional distress (95% CI Lower to Upper = .01 to .13; See Figure 2c). Children’s pain accounted for 23% of the variance in the relationship between children’s catastrophic thinking and parents’ affective memories of their child’s pain. Given that there were not direct effects of child pain catastrophizing on children’s or parents’ memories of pain, this type of mediation is termed indirect-only mediation [39].
Figure 2.
A, The association between baseline child pain catastrophizing (helplessness) and children’s memories of pain intensity is mediated by children’s pain-related emotional distress reported two weeks post-surgery.
B, The association between baseline child pain catastrophizing (helplessness) and children’s memories of pain-related emotional distress is mediated by children’s pain- related emotional distress reported two weeks post-surgery.
C, The association between baseline child pain catastrophizing (helplessness) and parents’ memories of their child’s pain-related emotional distress is mediated by children’s pain-related emotional distress reported two weeks post-surgery.
D, The association between baseline parent catastrophizing about child pain (rumination) and children’s memories of pain intensity is mediated by children’s pain intensity reported two weeks post-surgery.
Note: Path coefficients outside parentheses are estimates of the total effect of group status on pain memories, and direct effects between pain catastrophizing to the mediator (reported pain intensity/pain-related emotional distress) and the mediator and memories. Coefficients inside parentheses are results that include the mediator variable with a direct effect on the criterion. Estimated indirect effects and confidence intervals are results from bootstrapping analyses. Mediation analyses examining child catastrophizing (helplessness) controlled for parent catastrophizing about child pain (total score). Analyses examining parent catastrophizing (rumination) controlled for child catastrophizing (total score) *p < .05, **p < .01, ***p < .001.
The Mediating Role of Child Pain in the Acute Recovery Period in the relationship between Parent Catastrophizing and Pain Memories
Additionally, it was hypothesized that parent pain catastrophizing would influence parents’ and children’s pain memories through the child’s pain experience, while controlling for child pain catastrophizing. Analyses revealed that the relationship between parents’ catastrophic thinking (rumination) and children’s memories of pain intensity was explained by higher levels of pain intensity two weeks post-surgery (95% CI Lower to Upper = .01 to .24; See Figure 2d). Children’s pain experience accounted for 42% of the variance in the relationship between parents’ catastrophic thinking and children’s sensory pain memories. Given that there was not a direct effect of parent catastrophic thinking (rumination) on children’s pain memories, this was indirect-only mediation [39]. Analyses examining child pain intensity as a mediator of the relationship between parent rumination and parents’ memories were not significant because the confidence intervals crossed zero (95% CI Lower to Upper = −.03 to .16 and −.01 to .07, respectively).
Discussion
This is the first longitudinal examination of the role of pain catastrophizing in the development of children’s and parents’ memories for pain following pediatric major surgery. Results revealed that parent, but not child, catastrophizing exerts a direct influence on both children’s and parents’ memories of child post-surgical pain, over and above their initial pain reports. Greater parent magnification was associated with children’s recall of higher levels of emotional distress. Similarly, parent rumination was associated with parents remembering that their child experienced greater levels of pain intensity. In addition to the direct effect on parents’ pain memories, higher parent rumination about child pain influenced greater child pain intensity in the acute recovery period, which, in turn, led to children developing more distressing pain memories. Child catastrophizing did not exert a direct effect on children’s and parents’ pain memories; rather, these relationships were indirectly mediated through the affective aspect of the child’s post-operative pain experience. That is, children who perceived themselves as being more helpless in the face of pain prior to surgery experienced greater post- operative emotional distress during the acute recovery period, which, in turn, led to children and parents developing more distressing pain memories two to four months later. These findings show how aspects of child and parent catastrophizing about child pain influence the development of pain memories over time.
The relative strength of these effects suggests that while both child and parent catastrophizing play important roles in pain memory development, parent catastrophizing is most influential to both children’s and parents’ evolving cognitions about child pain. This is consistent with previous research showing that parent as opposed to child factors are most influential to long-term trajectories of pediatric post-surgical pain [27]. Upon observing their child in pain, parents who catastrophize tend to exhibit avoidance and distress [16; 6], engage in protective [19] and pain attending behaviors [7; 4] and show attentional biases related to their child’s pain [35]. The current findings extend this research by showing that parent catastrophizing about child pain also influences children’s and parents’ memories for pain several months following a major painful event. Contrary to our hypotheses, children’s magnification and rumination were not related to pain memory development. It could be that children’s pain catastrophizing at baseline is not stable. While it may be related to pain memories in the initial weeks following surgery, it may not be closely tied to children’s cognitions about pain over longer periods of time. Perhaps anxiety sensitivity, a stable predisposing anxiety variable, is more closely linked to children’s evolving cognitions of pain. Indeed, anxiety sensitivity has been linked to memory biases in experimental pain contexts [23; 22], albeit after shorter periods of time.
To date, research has rarely teased apart specific aspects of pain catastrophizing to examine the relative influences on children’s pain, although recent research revealed that children’s selective attention to pain was differentially impacted by magnification, rumination, and helplessness [36]. Likewise, the present findings suggest that particular cognitive tendencies of magnification and rumination among parents and helplessness among children may be most influential in the development of children’s and parents’ pain memories. It is not surprising that parents’ tendencies to perseverate on, and magnify, the threat value of their child’s pain is directly linked to increasingly negative memories. Memory is susceptible to distortion and each time an event is recalled, whether internally or within a social context, the memory is vulnerable to being re- written [37]. Moreover, there is theoretical and empirical support for the relationship between anxiety and memory biases [3; 24]. If each time the child’s pain experience is recalled, parents magnify its threatening aspects and continue to dwell upon it, increasingly distressing pain memories would be expected to develop. Interestingly, children’s tendency to catastrophize about their own pain (helplessness) was not directly related to their pain memory development; rather, it indirectly led to parents and children recalling higher levels of child pain by first increasing the child’s affective post-surgical pain experience. Helplessness may impede the child’s ability to cope with their pain and serve as a communicative signal to parents of threat, thereby exacerbating the unpleasant nature of pain and leading to increasingly distressing pain memories. Indeed, building efficacy in one’s coping abilities is a central intervention target in memory reframing interventions designed to positively/accurately reframe exaggerations in negative pain memories [8].
The influence of parent and child catastrophizing on pain memories may also be mediated by parent-child interactions about pain. Just as catastrophizing about child pain has been linked to verbal interactions shown to increase attention to pain [7; 4], parents’ and children’s memories may also reflect the verbally-based interactions that they have about pain prior to and following surgery. This may in part explain the indirect relationship between parent rumination and children’s pain memories. Parents who ruminate about their child’s pain may also externalize these cognitions, engaging in frequent discussions about children’s past and current pain experiences wherein they repeatedly emphasize its threatening aspects. This may cue children to also attend to the threatening aspects of their pain, thereby heightening pain perception and leading to increasingly distressing pain memories. In the field of developmental psychology, parent- child narratives have been shown to be powerful predictors of children’s memory development [32]. It is likely that these relationships are dynamic and the influences of parents’ cognitions and emotions on those of children, and vice versa, strengthen and interact over time as these patterns become more established and pain, for some, becomes chronic [1]. The current investigation only captured a limited snapshot of that evolving, reciprocal process. Incorporating observational methods into future research may enhance understanding of the specific parent-child communication processes that are associated with memory development.
The majority of research on factors influencing pain memory development has been in experimental [2; 22; 23] and non-surgical acute pain [18; 25] contexts. It is unknown whether memory for surgical pain is comparable to memory for experimental pain and researchers have called for extension of lab-based work with healthy children to clinical samples of children with medically induced and chronic pain [20]. The results of the current study and other pediatric surgery research suggest that parent emotions and behaviors are important in understanding trajectories of pediatric pain [27] and pain memories. Nevertheless, the role of parents has been largely overlooked in investigations of pain memory development despite their established role in children’s memories for other autobiographical events [32]. We argue that exclusion of parents from investigations on memory for pain is developmentally insensitive and will not propel forward this growing area of inquiry. Future research should examine the potential role of parents’ memories of child pain in influencing language-based interactions about pain, health care interactions, and children’s subsequent pain-related cognitions and behaviors.
This study had limitations. Memory was solely assessed using single item rating scales. Future research should employ a mixture of quantitative and qualitative methods of assessing pain memories to better capture the multidimensional aspects of children’s and parents’ recall. Obtaining free recall, unbiased by imposed language and probed questions would enable assessment of the details of the surgery experience that children and parents spontaneously remember. This might include negative and/or positive aspects and might differ depending on one’s individual characteristics (anxiety, pain/trauma history). Given that pain ratings were prospectively captured over several days, an average pain score was computed and assessed during the memory interviews. Average ratings may not have captured the most salient aspects of the pain memory and therefore, current recall ratings may underestimate the pain experienced and subsequently recalled. Third, our sample size was small and we had adequate power to only detect medium to large effects, which may have influenced our ability to detect relationships. Future research should replicate and expand upon these findings with larger samples of youth undergoing clinical pain experiences.
In summary, this is the first longitudinal examination of the influence of parent and child catastrophizing on children’s and parents’ pain memory development following surgery. Findings suggest that particular aspects of parents’ catastrophic thinking about child pain (magnification, rumination) prior to surgery directly influences both children’s and parents’ subsequent memories of child pain. Conversely, children’s helplessness indirectly impacts children’s and parents’ pain memories by first influencing the emotional aspect of the child’s post-surgical pain experience, which, in turn, influences memories of greater pain. The long-term impact of post-surgical pain memories on subsequent pain is unknown. However, in surgical contexts, parents’ emotions and cognitions are emerging as most influential in children’s pain trajectories over time [27]. Although many questions remain about the mechanisms driving these relationships, these findings underscore the importance of examining the parent-child relationship over time. Surgery offers a unique opportunity to examine the transition from acute to chronic pain and the modifiable factors underlying this process. Anxiety and pain memories of children and parents are modifiable factors that may serve as critical prevention and treatment targets. Further examination of these constructs within existing models outlining the bidirectional influences of parent-child interactions on child pain [30; 1] will take us closer to reducing the impact of pediatric pain across the lifespan.
Acknowledgments
Dr. Noel is funded by a Post-PhD Fellowship Award from the Canadian Institutes of Health Research and is a trainee member of Pain in Child Health, a Strategic Training Initiative in Health Research of the Canadian Institutes of Health Research. Funding for this research was provided by a grant from Seattle Children’s Center for Clinical and Translational Research Clinical Research Scholars Program awarded to Dr. Rabbitts. Dr. Palermo is supported by NIH K24HD060068.
Footnotes
The authors have no conflicts of interest to disclose.
References
- 1.Asmundson GJ, Noel M, Petter M, Parkerson HA. Pediatric fear-avoidance model of chronic pain: foundation, application and future directions. Pain Res Manag. 2012;17(6):397–405. doi: 10.1155/2012/908061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Badali MA, Pillai RR, Craig KD, Giesbrecht K, Chambers CT. Accuracy of children’s and parents’ memory for a novel pain experience. Pediatric Pain Management. 2000;5:161–168. [Google Scholar]
- 3.Beck AT, Clark DA. An information processing model of anxiety: automatic and strategic processes. Behav Res Ther. 1997;35(1):49–58. doi: 10.1016/s0005-7967(96)00069-1. [DOI] [PubMed] [Google Scholar]
- 4.Caes L, Vervoort T, Devos P, Verlooy J, Benoit Y, Goubert L. Parental distress and catastrophic thoughts about child pain: implications for parental protective behavior in the context of child leukemia-related medical procedures. Clin J Pain. 2014;30(9):787–799. doi: 10.1097/AJP.0000000000000028. [DOI] [PubMed] [Google Scholar]
- 5.Caes L, Vervoort T, Eccleston C, Goubert L. Parents who catastrophize about their child’s pain prioritize attempts to control pain. Pain. 2012;153(8):1695–1701. doi: 10.1016/j.pain.2012.04.028. [DOI] [PubMed] [Google Scholar]
- 6.Caes L, Vervoort T, Eccleston C, Vandenhende M, Goubert L. Parental catastrophizing about child’s pain and its relationship with activity restriction: the mediating role of parental distress. Pain. 2011;152(1):212–222. doi: 10.1016/j.pain.2010.10.037. [DOI] [PubMed] [Google Scholar]
- 7.Caes L, Vervoort T, Trost Z, Goubert L. Impact of parental catastrophizing and contextual threat on parents’ emotional and behavioral responses to their child’s pain. Pain. 2012;153(3):687–695. doi: 10.1016/j.pain.2011.12.007. [DOI] [PubMed] [Google Scholar]
- 8.Chen E, Zeltzer LK, Craske MG, Katz ER. Alteration of memory in the reduction of children’s distress during repeated aversive medical procedures. J Consult Clin Psychol. 1999;67(4):481–490. doi: 10.1037//0022-006x.67.4.481. [DOI] [PubMed] [Google Scholar]
- 9.Chen E, Zeltzer LK, Craske MG, Katz ER. Children’s memories for painful cancer treatment procedures: implications for distress. Child Dev. 2000;71(4):933–947. doi: 10.1111/1467-8624.00200. [DOI] [PubMed] [Google Scholar]
- 10.Connelly M, Fulmer RD, Prohaska J, Anson L, Dryer L, Thomas V, Ariagno JE, Price N, Schwend R. Predictors of postoperative pain trajectories in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2014;39(3):E174–181. doi: 10.1097/BRS.0000000000000099. [DOI] [PubMed] [Google Scholar]
- 11.Crombez G, Bijttebier P, Eccleston C, Mascagni T, Mertens G, Goubert L, Verstraeten K. The child version of the pain catastrophizing scale (PCS-C): a preliminary validation. Pain. 2003;104(3):639–646. doi: 10.1016/S0304-3959(03)00121-0. [DOI] [PubMed] [Google Scholar]
- 12.Esteve R, Marquina-Aponte V, Ramirez-Maestre C. Postoperative pain in children: association between anxiety sensitivity, pain catastrophizing, and female caregivers’ responses to children’s pain. J Pain. 2014;15(2):157–168. e151. doi: 10.1016/j.jpain.2013.10.007. [DOI] [PubMed] [Google Scholar]
- 13.Flor H. New developments in the understanding and management of persistent pain. Curr Opin Psychiatry. 2012;25(2):109–113. doi: 10.1097/YCO.0b013e3283503510. [DOI] [PubMed] [Google Scholar]
- 14.Gedney JJ, Logan H. Pain related recall predicts future pain report. Pain. 2006;121(1–2):69–76. doi: 10.1016/j.pain.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 15.Goubert L, Eccleston C, Vervoort T, Jordan A, Crombez G. Parental catastrophizing about their child’s pain. The parent version of the Pain Catastrophizing Scale (PCS-P): a preliminary validation. Pain. 2006;123(3):254–263. doi: 10.1016/j.pain.2006.02.035. [DOI] [PubMed] [Google Scholar]
- 16.Goubert L, Vervoort T, Sullivan MJ, Verhoeven K, Crombez G. Parental emotional responses to their child’s pain: the role of dispositional empathy and catastrophizing about their child’s pain. J Pain. 2008;9(3):272–279. doi: 10.1016/j.jpain.2007.11.006. [DOI] [PubMed] [Google Scholar]
- 17.Kotzer AM. Factors predicting postoperative pain in children and adolescents following spine fusion. Issues Compr Pediatr Nurs. 2000;23(2):83–102. doi: 10.1080/01460860050121411. [DOI] [PubMed] [Google Scholar]
- 18.Lander J, Hodgins M, Fowler-Kerry S. Children’s pain predictions and memories. Behav Res Ther. 1992;30(2):117–124. doi: 10.1016/0005-7967(92)90134-3. [DOI] [PubMed] [Google Scholar]
- 19.Langer SL, Romano JM, Mancl L, Levy RL. Parental Catastrophizing Partially Mediates the Association between Parent-Reported Child Pain Behavior and Parental Protective Responses. Pain Res Treat. 2014;2014:751097. doi: 10.1155/2014/751097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liossi C, Fitzgerald M. Remember, remember... a child’s pain experience. Pain. 2012;153(8):1543–1544. doi: 10.1016/j.pain.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 21.McGrath PA. Pain in children: Nature, assessment, and treatment. New York: Guilford Press; 1990. [Google Scholar]
- 22.Noel M, Chambers CT, McGrath PJ, Klein RM, Stewart SH. The influence of children’s pain memories on subsequent pain experience. Pain. 2012;153(8):1563–1572. doi: 10.1016/j.pain.2012.02.020. [DOI] [PubMed] [Google Scholar]
- 23.Noel M, Chambers CT, McGrath PJ, Klein RM, Stewart SH. The role of state anxiety in children’s memories for pain. J Pediatr Psychol. 2012;37(5):567–579. doi: 10.1093/jpepsy/jss006. [DOI] [PubMed] [Google Scholar]
- 24.Noel M, Chambers CT, Petter M, McGrath PJ, Klein RM, Stewart SH. Pain is not over when the needle ends: a review and preliminary model of acute pain memory development in childhood. Pain Manag. 2012;2(5):487–497. doi: 10.2217/pmt.12.41. [DOI] [PubMed] [Google Scholar]
- 25.Noel M, McMurtry CM, Chambers CT, McGrath PJ. Children’s memory for painful procedures: the relationship of pain intensity, anxiety, and adult behaviors to subsequent recall. J Pediatr Psychol. 2010;35(6):626–636. doi: 10.1093/jpepsy/jsp096. [DOI] [PubMed] [Google Scholar]
- 26.Ornstein PA, Manning EL, Pelphrey KA. Children’s memory for pain. J Dev Behav Pediatr. 1999;20(4):262–277. doi: 10.1097/00004703-199908000-00009. [DOI] [PubMed] [Google Scholar]
- 27.Page MG, Campbell F, Isaac L, Stinson J, Katz J. Parental risk factors for the development of pediatric acute and chronic postsurgical pain: a longitudinal study. J Pain Res. 2013;6:727–741. doi: 10.2147/JPR.S51055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Page MG, Katz J, Stinson J, Isaac L, Martin-Pichora AL, Campbell F. Validation of the numerical rating scale for pain intensity and unpleasantness in pediatric acute postoperative pain: sensitivity to change over time. J Pain. 2012;13(4):359–369. doi: 10.1016/j.jpain.2011.12.010. [DOI] [PubMed] [Google Scholar]
- 29.Page MG, Stinson J, Campbell F, Isaac L, Katz J. Pain-related psychological correlates of pediatric acute post-surgical pain. J Pain Res. 2012;5:547–558. doi: 10.2147/JPR.S36614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Palermo TM, Chambers CT. Parent and family factors in pediatric chronic pain and disability: An integrative approach. Pain. 2005;119(1–3):1–4. doi: 10.1016/j.pain.2005.10.027. [DOI] [PubMed] [Google Scholar]
- 31.Palermo TM, Valenzuela D, Stork PP. A randomized trial of electronic versus paper pain diaries in children: impact on compliance, accuracy, and acceptability. Pain. 2004;107(3):213–219. doi: 10.1016/j.pain.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 32.Peterson C, Sales JM, Reese M, Fivush R. Parent-child talk and children’s memory for stressful events. Appl Cognitive Psych. 2007;21:1057–1075. [Google Scholar]
- 33.Rocha EM, Marche TA, von Baeyer CL. Anxiety influences children’s memory for procedural pain. Pain Res Manag. 2009;14(3):233–237. doi: 10.1155/2009/535941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sieberg CB, Simons LE, Edelstein MR, DeAngelis MR, Pielech M, Sethna N, Hresko MT. Pain prevalence and trajectories following pediatric spinal fusion surgery. J Pain. 2013;14(12):1694–1702. doi: 10.1016/j.jpain.2013.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vervoort T, Caes L, Crombez G, Koster E, Van Damme S, Dewitte M, Goubert L. Parental catastrophizing about children’s pain and selective attention to varying levels of facial expression of pain in children: a dot-probe study. Pain. 2011;152(8):1751–1757. doi: 10.1016/j.pain.2011.03.015. [DOI] [PubMed] [Google Scholar]
- 36.Vervoort T, Trost Z, Van Ryckeghem DM. Children’s selective attention to pain and avoidance behaviour: the role of child and parental catastrophizing about pain. Pain. 2013;154(10):1979–1988. doi: 10.1016/j.pain.2013.05.052. [DOI] [PubMed] [Google Scholar]
- 37.von Baeyer CL, Marche TA, Rocha EM, Salmon K. Children’s memory for pain: overview and implications for practice. J Pain. 2004;5(5):241–249. doi: 10.1016/j.jpain.2004.05.001. [DOI] [PubMed] [Google Scholar]
- 38.Wong GT, Yuen VM, Chow BF, Irwin MG. Persistent pain in patients following scoliosis surgery. Eur Spine J. 2007;16(10):1551–1556. doi: 10.1007/s00586-007-0361-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhao X, Lynch JG, Chen Q. Reconsidering Baron and Kenny: Myths and truths about mediation analysis. J Consum Res. 2010;37(2):197–206. [Google Scholar]
- 40.Zonneveld LN, McGrath PJ, Reid GJ, Sorbi MJ. Accuracy of children’s pain memories. Pain. 1997;71(3):297–302. doi: 10.1016/s0304-3959(97)03379-4. [DOI] [PubMed] [Google Scholar]