Abstract
AIM: To summarize the clinical characteristics of Crohn’s disease (CD) patients who underwent surgery in China.
METHODS: We searched four main Chinese electronic databases: CBM, VIP, CNKI, and Wanfang (from January 1990 to October 2013). Then, we selected and carefully read 97 studies and extracted the surgical data for CD. We found that 1858 patients with CD underwent surgery between 1961 and 2012. The patients were stratified into two groups according to the year of surgery: 1961-2000 and 2000-2012. The clinical characteristics of these CD cases were compared between the two groups.
RESULTS: The mean age at the time of surgery was 38.13 years. The most common locations of disease were the small intestine (40.84%), the colon (33.60%) and the ileocolon (23.09%). The primary indications for surgery were intestinal obstruction or stricture (23.84%), failure of drug therapy (14.80%), acute abdominal disease (13.46%), abdominal mass (10.93%), intestinal fistulae (9.90%), intestinal perforation (8.45%), perianal disease (6.73%), gastrointestinal bleeding (4.79%), and abdominal abscess (4.04%). The rate of diagnosis of CD before surgery was low (34.78%), and the misdiagnosis rate was 20.49%. The predominant surgical procedure for CD was bowel resection (69.54%). The rate of surgical complications was 20.34%, and the primary complications of surgery were infection (39.44%) and intestinal fistulae (26.09%). The relapse rate after surgery was 27.71%. For the periods of 1961-2000 and 2000-2013, the rates of both misdiagnosis before surgery and surgery related-death decreased (34.90% vs 12.10%, P < 0.001, and 23.53% vs 5.26%, P < 0.001, respectively).
CONCLUSION: The rates of surgical complications and misdiagnosis were higher, whereas the rate of CD-associated tumor and the relapse rate were lower in China than in West countries.
Keywords: Crohn’s disease, Surgery, Surgical indications, Surgical complications, Surgical recurrence
Core tip: There has been no study of the clinical characteristics of a large population of Chinese Crohn’s disease (CD) patients requiring surgery. Based on a literature review, we summarize the clinical characteristics of 1858 patients with CD who underwent surgery in China. The clinical characteristics were generally similar to those reported in the West. However, the rates of surgical complications and misdiagnosis in China were higher than those in Western countries, whereas the rate of CD complicated by tumors and the relapse rate were lower. Further analysis revealed that the surgical outcomes improved during the period examined.
INTRODUCTION
Crohn’s disease (CD) is a non-specific chronic inflammatory bowel disease (IBD) that is characterized by non-caseating granulomas that occur in the gastrointestinal tract. This disease is chronic, incurable, and prone to relapse. As lifestyles continue to move toward a more Western style, the incidence and prevalence of CD in China have been increasing[1,2], and as a result, this disease continues to attract the attention of researchers and clinical physicians. Approximately 75%-80% of patients require surgical resection at some point in their lives after a diagnosis of CD[3]. However, surgery cannot cure this disease completely, and postoperative recurrence (POR) remains a significant problem in patients with CD. Therefore, we should carefully weigh the benefits and drawbacks prior to surgery. Many studies have been conducted that involve the clinical analysis of surgery in patients with CD from different hospitals in China. However, no multicenter or large observational studies have been published on the clinical characteristics of patients with CD who require surgery in China. To analyze and summarize the surgical clinical characteristics of patients with CD across China, we searched four major Chinese databases for related literature, performed a statistical analysis and compiled a summary.
MATERIALS AND METHODS
To summarize the clinical characteristics of patients with CD who underwent surgery in China, we performed a comprehensive search within four main Chinese electronic databases (from January 1990 to October 2013): CBM, VIP, CNKI, and Wanfang. The following key words were used: “CD”, “IBD”, “surgery”, “operation” and “surgical complications”. The literature search identified 512 journal articles. All reviews, letters to the editor, clinical guidelines, commentaries, and editorials were excluded. Controlled clinical trials, observational studies, and case-controlled studies were included. Based on an examination of the available full-text articles, those which contained information about “surgical indications for surgery”, “surgical procedures” and “the final certain diagnosis of CD” were included, whereas those which included duplicated cases or did not contain the above information were excluded. Finally, 97 articles that involved surgery for patients with CD were included. Then, we read each article carefully and extracted the following information: “the years in which the patient was studied’’, “gender”, “age”, “disease locations” (the Montreal classification of CD[4]), “surgical indications ”, “the diagnosis before surgery”, “surgical procedures”, “surgical complications” and “follow-up outcome”. We extracted these data to analyze and summarize the characteristics of the patients with CD who underwent surgery. To ensure the credibility of the data, data that were unclassified or uncertain were excluded, and only defined data were retained for further analysis. Moreover, data from 1858 cases of CD (surgery period of 1961-2012) in 97 articles were collected by two different researchers (Figure 1).
Figure 1.
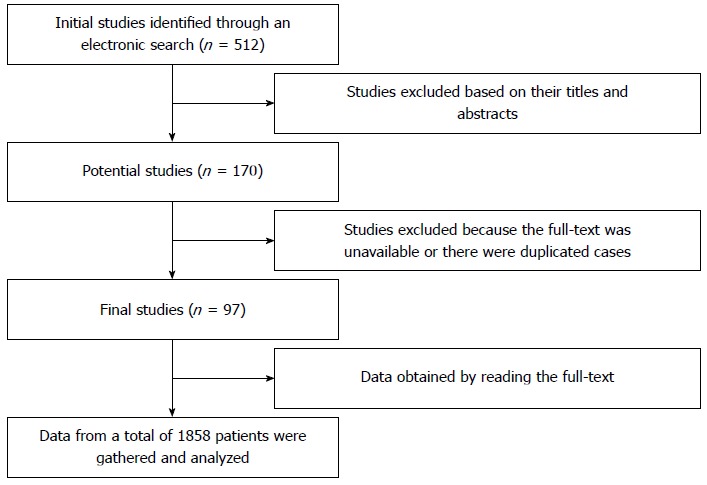
Flow chart of the studies included in the case analyses.
Although two conferences that focused on the diagnosis and the therapeutic effects of IBD in China were convened in 1978 and 1993, the first guidelines regarding therapy for CD in China were not established until 2000. The patients who were included in this review were stratified into two groups according to the year of surgery: 1961-2000 (Group A) and 2000-2012 (Group B). Those articles which included an interval before and after the year 2000 were excluded. Among the remaining 72 articles, 28 contained information about the surgery of 447 CD cases in Group A, and 44 contained information about the surgery of 620 CD cases in Group B. Moreover, the data were summarized by two different researchers, as mentioned above.
Statistical analysis
Statistical Package for Social Science (SPSS 19.0) software was used for statistical analyses. The mean ± SD was calculated for continuous numerical variables. The numbers and percentages were calculated for categorical variables. The χ2 test or Fisher’s exact test (if the expected number of cases was less than 5) was applied to compare the categorical variables. A P-value less than 0.05 was considered to be significant.
RESULTS
Study information and patient characteristics
The articles (from January 1990 to October 2013) contained data from 1858 patients with CD who underwent surgery between 1961 and 2012. These cases were obtained from various cities of the 24 provinces or municipalities in China (Figure 2). According to the different regions in China, 45.59% of the cases were from Eastern China, followed by Southern China (19.16%), Northern China (18.62%), Central China (13.56%) and Western China (3.07%). No data were obtained from patients in Hainan, Inner Mongolia, Tibet, Shaanxi, Ningxia, Qinghai or Xinjiang.
Figure 2.
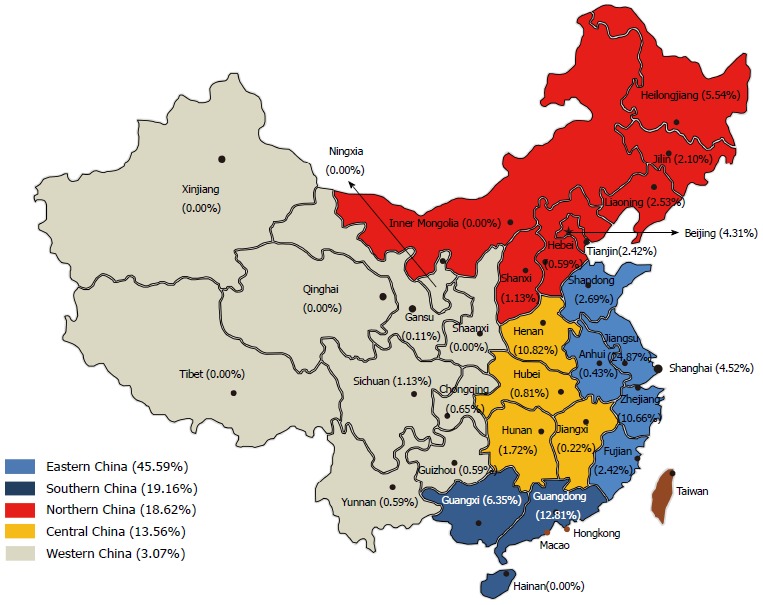
Crohn’s disease cases from a variety of provinces and municipalities.
Among the 1858 cases of CD, 1080 (58.13%) were male. The gender ratio (male/female) was 1.39. The mean age was 38.13 years (range, 0.5 to 84 years). No record of disease location was found for approximately one-third of the patients [602 (32.4%)]. According to the Montreal classification[4], of the remaining 1256 patients, most experienced this disease in the small intestine [L1, 513 (40.84%)], colon [L2, 422 (33.60%)], or small intestine and colon (ileocolon) [L3, 290 (23.09%)] at the time of diagnosis. Fewer than 3% had CD in other locations, such as the upper gastrointestinal tract [L4, 23 (1.83%)]; colon and upper gastrointestinal tract [L2 + L4, 3 (0.24%)]; or small intestine, colon and upper gastrointestinal tract [L3 + L4, 5 (0.40%)]. Among the 1858 cases of CD, 1.18% (22/1858) had comorbidities that included intestinal tumors, such as adenocarcinoma (18 cases), lymphoma (1 case) and atypical dysplasia (3 cases).
Surgical indications
Among the 1858 patients, the primary indications for surgery were intestinal obstruction or stricture (23.84%), peritonitis or other acute abdominal disease (not including obstruction or intestinal perforation) (13.46%), abdominal mass (10.93%), intestinal fistulae (9.90%), intestinal perforation (8.45%), perianal disease (6.73%), gastrointestinal bleeding (4.79%), abdominal abscess (4.04%), and intestinal adhesion (2.69%) (Table 1). Among the 184 cases of intestinal fistulae, internal fistulae, external fistulae, vaginal fistulae, vesical fistulae and other unclassified fistulae were observed in 33.70%, 24.46%, 2.71%, 8.15% and 31.52% of patients, respectively. With respect to these fistulae, one case had external fistulae and vesical fistulae simultaneously. Perianal disease including perianal abscess (17.60%), perianal fistulae (48.80%), perianal fissure (3.20%), perianal ulcer (1.60%), perianal fistulae and fissure (8.00%), and perianal fistulae and ulcer (4.00%), and other unclassified perianal diseases (16.80%) were also present.
Table 1.
Summary of the surgical indications n (%)
| Surgical indication | Cases |
| Intestinal obstruction or stricture | 443 (23.84) |
| Peritonitis or other acute abdominal disease | 250 (13.46) |
| Abdominal mass | 203 (10.93) |
| Intestinal fistulae1 | 184 (9.90) |
| Internal fistulae | 62 (3.34) |
| External fistulae | 45 (2.42) |
| Vaginal fistulae | 5 (0.27) |
| Vesical fistulae | 15 (0.81) |
| Other unclassified fistulae | 58 (3.12) |
| Intestinal perforation | 157 (8.45) |
| Perianal disease2 | 125 (6.73) |
| Perianal abscess | 22 (1.18) |
| Perianal fistulae | 61 (3.28) |
| Perianal fissure | 4 (0.22) |
| Perianal ulcer | 2 (0.11) |
| Perianal fistulae and fissure | 10 (0.54) |
| Perianal fistulae and ulcer | 5 (0.27) |
| Other unclassified perianal disease | 21 (1.13) |
| Gastrointestinal bleeding | 89 (4.79) |
| Abdominal abscess | 75 (4.04) |
| Intestinal adhesion | 50 (2.69) |
| Failure of drug therapy | 275 (14.80) |
| Pyloric obstruction | 4 (0.22) |
| Colic intussusception | 3 (0.16) |
The percentage of each type of fistulae in 1858 cases;
The percentage of each perianal disease in 1858 cases.
Another primary indication for surgery was failure of drug therapy (14.80%). Other reasons for surgery, such as pyloric obstruction (0.22%) and colic intussusception (0.16%), were less frequent.
These articles contained data on 83.26% (1547/1858) of patients with regard to specific information about the diagnosis of CD prior to surgery. Before surgery, only 538 (34.78%) patients were diagnosed with CD, 692 (44.73%) patients had an uncertain diagnosis, and 317 (20.49%) patients were misdiagnosed. Prior to surgery, in the group of misdiagnosed patients, 49.21% were diagnosed with appendicitis, 29.02% with an intestinal tumor, 11.36% with intestinal tuberculosis, and 10.41% with ulcerative colitis.
Surgical procedures
The most common type of surgical procedure was bowel resection (69.54%), which included colonic resection (24.27%), ileal resection (22.60%), ileocolonic resection (10.23%), upper gastrointestinal resection (0.54%) and other unclassified types of bowel resection (11.89%) (Table 2). Other surgeries included operation for perianal disease (4.84%), ileostomy or colostomy (4.09%), operation for fistulae or perforations (3.01%), abdominal exploration (2.10%), small intestinal colon short circuit (1.29%), drainage of an abdominal abscess (0.59%), stricturoplasty (0.48%), intestinal adhesion release (0.48%), and operation for a complicated tumor (0.22%). Moreover, only 33 (1.78%) patients who underwent laparoscopic surgery were recorded in our results. Of the 451 patients who received colonic resection, right hemicolectomy (50.78%), ileocecal resection (21.95%), left hemicolectomy (9.97%), rectal resection (2.44%), transverse colonic resection (1.55%), total proctocolectomy (1.11%), or another type of unclassified partial colectomy (12.20%) was performed.
Table 2.
Summary of the surgical procedures n (%)
| Surgical procedure | Cases |
| Ileal resection | 420 (22.60) |
| Colonic resection | 451 (24.27) |
| Total proctocolectomy | 5 (0.27) |
| Partial colectomy | 446 (24.00) |
| Right hemicolectomy | 229 (12.33) |
| Ileocecal resection | 99 (5.33) |
| Left hemicolectomy | 45 (2.42) |
| Rectal resection | 11 (0.59) |
| Transverse colonic resection | 7 (0.38) |
| Other colonic resection (unclassified) | 55 (2.96) |
| Ileocolonic resection | 190 (10.23) |
| Other unclassified bowel resection | 221 (11.89) |
| Upper gastrointestinal resection | 10 (0.54) |
| Operation for perianal disease | 90 (4.84) |
| Ileostomy or colostomy | 76 (4.09) |
| Operation for fistulae or perforations | 56 (3.01) |
| Drainage of an abdominal abscess | 11 (0.59) |
| Abdominal exploration | 39 (2.10) |
| Small intestinal colon short circuit | 24 (1.29) |
| Stricturoplasty | 9 (0.48) |
| Intestinal adhesion release | 9 (0.48) |
| Operation for a complicated tumor | 4 (0.22) |
| Other or unclassified surgery | 223 (12.00) |
Although rare, some patients underwent more than one surgical procedure simultaneously.
Surgical complications
These articles contained information on 1583 patients who experienced surgical complications (surgery-related complications in a short period of time). A total of 20.34% of patients experienced surgical complications (Table 3). Infection (39.44%) was the primary surgical complication, which included incision infection (27.33%), abdominal infection (5.28%), and infection in other location (6.83%). Other complications included intestinal fistulae (26.09%), surgery-related death (18.63%), stricture or obstruction (12.11%), intestinal adhesion (3.42%), abdominal abscess (4.35%), gastrointestinal bleeding (4.04%), stress ulcer (2.80%), liquefied fat at the incision site (1.24%), short bowel syndrome (0.93%), gastrointestinal perforation (0.62%), and incisional fissure (0.62%).
Table 3.
Surgical complications of 322 cases n (%)
| Surgical complication | Cases |
| Infection | 127 (39.44) |
| Incision infection | 88 (27.33) |
| Abdominal infection | 17 (5.28) |
| Other infection | 22 (6.83) |
| Intestinal fistula | 84 (26.09) |
| Death | 60 (18.63) |
| Stricture or stenosis | 39 (12.11) |
| Intestinal adhesion | 11 (3.42) |
| Abdominal abscess | 14 (4.35) |
| Gastrointestinal bleeding | 13 (4.04) |
| Stress ulcer | 9 (2.80) |
| Incision fat liquefied | 4 (1.24) |
| Short bowel syndrome | 3 (0.93) |
| Gastrointestinal perforation | 2 (0.62) |
| Incision fissure | 2 (0.62) |
| Others or unclassified | 25 (7.76) |
The patients may have experienced more than one complication simultaneously.
Long-term outcome
The included articles contained follow-up data for 1415 (76.16%) out of 1858 patients. The rate of follow-up was 87.99% (1245/1415). The average follow-up time was 6.5 years (range, 1 mo-20 years). The rate of remission was 72.29% (900/1245), and the relapse rate after surgery, including 47 cases of death, was 27.71% (345/1245). Among the patients who experienced a relapse, 27.83% (96/345) required a second surgery, whereas some required a third [3.48% (12/345)] or fourth [0.58% (2/345)] surgery.
Comparison between group A (1961-2000) and group B (2000-2012)
The clinical characteristics of the patients with CD who underwent surgery in China over the entire interval from 1961 to 2012 were summarized above. These cases were categorized into two groups: Group A (1961-2000) and Group B (2000-2012). Of these 1858 patients, 1067 from 72 articles were included in a comparison of the clinical characteristics of the patients with CD between Group A (447 cases, 28 articles) and Group B (620 cases, 44 articles) (Table 4). In Group A, 71.05% of the patients underwent surgery during the period of 1990-2000.
Table 4.
Summary of the clinical characteristics of Groups A and B n (%)
| Surgery characteristics | Group A (n = 447) | Group B (n = 620) | P value |
| Gender ratio (male/female) | 262/185 | 375/245 | 0.539 |
| Mean age | 38.46 | 37.78 | - |
| Disease location1 | < 0.001 | ||
| L1 | 166 (53.21) | 126 (29.37) | < 0.001 |
| L2 | 82 (26.28) | 111 (25.87) | 0.901 |
| L3 | 54 (17.31) | 179 (41.72) | < 0.001 |
| Upper gastrointestinal disorder involvement | 10 (3.21) | 13 (3.03) | 0.892 |
| Surgical indication | < 0.001 | ||
| Intestinal obstruction or stricture | 92 (20.58) | 205 (33.06) | < 0.001 |
| Abdominal mass | 44 (9.84) | 36 (5.81) | 0.013 |
| Perianal disease | 0 (0.00) | 97 (15.65) | < 0.001 |
| Intestinal fistulae | 7 (1.57) | 68 (10.97) | < 0.001 |
| Intestinal adhesion | 0 (0.00) | 12 (1.94) | 0.003 |
| Gastrointestinal bleeding | 2 (0.45) | 26 (4.19) | < 0.001 |
| Abdominal abscess | 11 (2.46) | 30 (4.84) | 0.046 |
| Intestinal perforation | 22 (4.92) | 46 (7.42) | 0.099 |
| Peritonitis or other acute abdominal diseases | 21 (4.70) | 17 (2.74) | 0.089 |
| Failure of drug therapy | 248 (55.48) | 83 (13.39) | < 0.001 |
| Diagnosis of CD before surgery | < 0.001 | ||
| Certain | 137 (30.65) | 194 (31.29) | 0.689 |
| Misdiagnosis2 | 156 (34.90) | 75 (12.10) | < 0.001 |
| Intestinal tuberculosis | 22 (14.10) | 2 (2.67) | 0.008 |
| UC | 8 (5.13) | 6 (8.00) | 0.574 |
| Tumor | 49 (31.41) | 23 (30.67) | 0.909 |
| Acute appendicitis | 77 (49.36) | 44 (58.67) | 0.185 |
| Uncertain | 154 (34.45) | 351 (56.61) | < 0.001 |
| Surgical procedure | |||
| Bowel resection | 312 (69.80) | 430 (69.35) | 0.876 |
| Colonic resection | 83 (18.57) | 105 (16.94) | - |
| Ileal resection | 65 (14.54) | 175 (28.23) | - |
| Ileocolonic resection | 40 (8.95) | 105 (16.94) | - |
| Upper gastrointestinal resection | 8 (1.79) | 1 (0.16) | - |
| Unclassified bowel resection | 126 (28.19) | 44 (7.10) | - |
| Operation for perianal disease | 0 (0.00) | 81 (13.06) | < 0.001 |
| Ileostomy or colostomy | 6 (1.34) | 27 (4.35) | 0.005 |
| Stricturoplasty | 1 (0.22) | 8 (1.29) | 0.123 |
| Complication of surgery3 | 68 (18.94) | 133 (24.23) | 0.061 |
| Infection | 21 (30.88) | 60 (45.11) | 0.052 |
| Stricture or stenosis | 14 (20.59) | 24 (18.05) | 0.663 |
| Death | 16 (23.53) | 7 (5.26) | 0.708 |
| Intestinal fistulae | 9 (13.24) | 28 (21.05) | < 0.001 |
| Abdominal abscess | 5 (7.35) | 5 (3.76) | 0.176 |
| Surgical relapse rate4 | 115 (31.59) | 126 (28.64) | 0.362 |
| Surgery after relapse | 38 (33.04) | 34 (26.98) | 0.305 |
There were 312 cases and 429 cases for which the disease location was reported in Groups A and B, respectively;
Misdiagnosis was retrospectively analyzed furtherly;
There were 359 cases and 549 cases in Groups A and B, respectively, who experienced surgical complications; the distribution of these complications was further analyzed;
There were 364 cases and 440 cases in Group A and B, respectively, which contained follow-up data. P < 0.05 was considered to be significant. L1: Small intestine; L2: Colon; L3: Small intestine and colon; UC: Ulcerative colitis.
No significant difference was observed in the gender ratio between the two groups. These articles provided the disease locations for 312 and 429 cases in Groups A and B, respectively. Over time, the number of patients with disease in the small intestine decreased (from 53.21% to 29.37%, P < 0.001); however, the number of patients with disease in the ileocolon increased (from 17.31% to 42.72%, P < 0.001). No significant difference was found with respect to the proportion of patients with disease in the colon or the upper gastrointestinal tract. The indications for surgery varied throughout the years. The percentage of patients with intestinal obstruction or stricture, perianal disease, intestinal fistulae, intestinal adhesion, gastrointestinal bleeding or abdominal abscess increased, whereas the percentage of patients with an abdominal mass or who experienced failure of drug therapy decreased (P < 0.05). Failure of drug therapy decreased dramatically from 55.48% to 13.39%. The rate of misdiagnosis decreased from 34.90% to 12.10% (P < 0.001). The need for ileostomy or colostomy and for surgery for perianal disease was increased in Group B (P < 0.05). Of the surgical procedures, no laparoscopic surgeries were performed on the patients in Group A, but 33 laparoscopic surgeries were performed on the patients in Group B (not shown in Table 4). The rate of surgery-related death decreased from 23.53% to 5.26% (P < 0.001). Infection remained the primary complication observed in the two groups (30.88% vs 45.11%, P = 0.052).
DISCUSSION
Although the surgical management of CD has changed considerably during the last decade as a result of developments in medical therapy, most patients still eventually require surgical intervention. The gastroenterologist and surgeon should understand the value or clinical characteristics of surgery so that the best therapy can be offered at the optimal time. This paper is the first literature review of patients with CD who underwent surgery in China. We summarized the major clinical characteristics of 1858 patients with CD who underwent surgery in China, with the hope that this analysis can help physicians and surgeons in clinical practice. Bernell et al[5] reported that the cumulative rate of intestinal resection in 1936 patients was 44%, 61%, and 71% at 1, 5, and 10 years after diagnosis, respectively, whereas the overall rate of surgery was 73.6%; in another systematic review, the rate of intestinal resection was 16.3%, 33.3%, and 46.6% at 1, 5, and 10 years after diagnosis, respectively[6]. In South China, the intestinal resection rate was reported to be 16.6%, 35.4%, 53%, and 94.5% at 1, 5, 10, and 30 years, respectively, after the onset of the disease[7]. Although the rate of surgery after CD diagnosis varies slightly among these studies, many CD patients will undergo surgery during their lifetime.
Because we searched our primary electronic databases, we did not include the data on the patients who underwent surgery in Hong Kong, Macao or Taiwan. These data were obtained from 24 of the 31 (77.42%) Chinese provinces and municipalities. More surgeries for CD were reported in Eastern and Southern China than in other regions of China. An increased number of inhabitants and the greater development of these areas may explain the higher prevalence and incidence of CD in these regions. The data derived from these articles are assumed to generally reflect the clinical characteristics of patients with CD who underwent surgery in China.
In our study, the gender ratio (male/female) was 1.39. Male patients have a slightly higher risk for surgery. Gao et al[7] also reported that male gender is associated with an increased risk for primary surgery in their study of 323 patients with CD from South China. However, a study of 289 consecutive Japanese patients with CD found that females have a higher risk for surgery[8]. Other studies reported no difference in the risk of surgery between males and females[9,10]. The mean age was 38.13 years in our study. Whereas in the Western countries, the mean age was reported to be 32 years[5] and 28.7 years[11]. The average age of surgery from most reports in Western countries is lower than in our study. This may be related to the relatively late onset of CD in Chinese patients[12]. In our study, the primary disease location was the small intestine (L1, 40.84%). The occurrence of disease in the upper gastrointestinal tract (L4, L1 + L4, L2 + L4 or L3 + L4) was less than 3% in our study. Basilisco et al[13] reported that an increased risk of surgery was found in ileal and ileocolonic CD, whereas another study demonstrated an increased risk of surgery with ileocolonic disease[14]. The frequency of synchronous tumors was 1.18% in patients with CD, which is lower than previous reports that suggested the frequency is 4% to 11%[15].
Most studies reported that the general indications for surgery for patients with CD are based on an evaluation of several factors, such as the failure of medical treatment, complications due to the disease or to pharmacological therapy, development of dysplasia or cancer and growth retardation. The reasons for failed medical therapy can vary from medication noncompliance to a lack of treatment response[16,17]. The indications for surgery were assessed by studies from Olmsted County (1935-75, 1970-2004)[9,18] and Stockholm County (1955-94)[5]. Through an update of the Olmsted County data[9], the main indications for surgery were found to be obstruction or medical therapy failure in 24% of cases; perforation or abscess each in 10%; fistulizing disease in 8%; intestinal cancer in 4%; and severe perianal disease, bleeding or severe pain, each in 3%. In our study, the indications for surgery included intestinal obstruction or stricture (23.84%), acute abdominal disease (13.46%), abdominal mass (10.93%), intestinal fistulae (9.90%), intestinal perforation (8.45%), and perianal disease (6.73%).
Another main reason for surgery was failure of drug therapy (14.80%). These data indicated that intractability to medical treatment that necessitates surgery remains frequent in CD. Concerning the surgical characteristics, failure of drug therapy was not specifically listed in most of these articles. We performed a literature search of the four electronic databases mentioned above using the terms “infliximab (IFX)” and “CD” and found that this therapy was initially used to treat CD in China in 2007. This finding suggested that failure of drug therapy in these cases primarily involved 5-ASA, corticosteroids, immunosuppressant and, infrequently, IFX.
Most patients in our study were unable to obtain a definitive diagnosis before surgery. Almost half of the patients were given an uncertain diagnosis, and 20.49% were misdiagnosed before surgery. The major misdiagnoses were acute appendicitis, intestinal tumor, intestinal tuberculosis, and ulcerative colitis. There are many factors that may delay the diagnosis of CD in China, including the relative severity of infectious colitis that can mask CD, inadequate medical and diagnostic facilities, a lack of awareness and sufficient knowledge of CD on the part of the doctors, and the lack of an appropriate follow-up period. In contrast to the West, many infectious intestinal diseases exist in China, which are similar to CD, especially intestinal tuberculosis (ITB). ITB and CD have overlapping symptomatic, physical, radiographic and colonoscopic features[19-21]. Therefore, the diagnosis of CD in China is more difficult.
Several studies that included population-based cohorts evaluated the types of surgery performed for CD[9,18,22,23]. Resection of the colon and/or small bowel comprised approximately two-thirds of the operations in the Olmsted County study (1935-75)[18]. Ileal or ileocecal resection was the main indication for surgery and was performed in 67% and 72.4% of patients, respectively, from the Cardiff (1986-2003)[22] and Olmsted County (1970-2004) studies[9]. This suggests that bowel resection was the primary type of surgery for cases of CD. Our study also showed that 69.54% (1292/1858) of patients underwent bowel resection, including colonic resection (24.27%), ileal resection (22.60%) and ileocolonic resection (10.23%). Stricturoplasty was performed in 7% of patients in Cardiff[22], whereas it was performed in only 0.7% and 0.48% of patients in Olmsted County[9] and in our study, respectively. This may reflect differences in the surgical management of small bowel strictures. Some patients eventually require multiple operations throughout their lifetime and may be at risk for the development of short bowel syndrome and repeat resections. Our study showed that 7.71% of patients required surgery again (a total of 1245 patients) and some required a third (0.96%) or fourth (0.16%) surgery. Among all patients, 0.93% of patients experienced short bowel syndrome. The current practice is to leave the diseased bowel behind and to remove only the part of the bowel that is responsible for the symptoms. Bowel-sparing techniques such as stricturoplasty have been suggested to reduce this risk. Stricturcoplasty is a safe alternative to resection in jejuno-ileal CD, including ileocolonic recurrence[24]. Additionally, most of studies reported that laparoscopic surgery for CD is feasible and safe and is associated with a shorter hospital stay and a better short-term outcome compared with open resection[25-28]. Laparoscopic surgery is preferred for ileocolonic resections. However, insufficient evidence exists for the recommendation of laparoscopic surgery as the first-line technique in more complex cases or in recurrent resections. In these situations, appropriate surgical expertise is a mandatory prerequisite. As surgical technology develops, there may be more patients with CD who undergo laparoscopic surgery.
In our study, a total of 20.34% of patients experienced one or more surgical complications. Surgery-related infection was the most common complication and accounted for 39.44% of all complications. Surgery-related death accounted for 18.63% of all complications. However, Brouquet et al[29] reported that the rate of major complications of surgery was less than 10%, which is lower than what we observed. Additionally, the surgery rate in Western countries is higher than that in China. Doctors and patients in China seemed to be more reluctant to perform and undergo surgery compared with patients and doctors in Western nations. Some gastroenterologists might consider surgery as a last resort. It must be recognized that this belief carries an implicit risk because those patients who ultimately undergo surgery might have a more complicated disease and are likely to be at a higher risk for septic complications. In complicated cases of CD, surgery at an early stage is a valid alternative to other types of medical therapies. According to a study of 207 patients with CD, early surgery prolongs clinical remission compared with surgery that is performed during the course of the disease within 10 years of the disease onset[30]. The complexity and heterogeneity of the disease and the different options for medical or surgical treatment are all so diverse that it is even more important to discuss each case in multidisciplinary clinical conferences. Therefore, close interactions between the gastroenterologist, the surgeon and physicians of other disciplines are needed to determine the best therapy.
The rate of remission was 72.29% and the relapse rate after surgery was 27.71% in our study. Bernell et al[5] observed that postoperative recurrence occurred in 33% and 44% of patients at 5 and 10 years after resection, respectively. Similar to these results, Cullen et al[11] observed that the relapse rate was 35%. The relapse rate was relatively low in our study. The reason for this may be that the follow-up of some patients was relatively short.
Additional information was analyzed for the years before and after 2000. Over time, the percentage of patients who experienced failure of drug therapy that led to surgery, misdiagnosis before surgery, and surgery-related death decreased; in contrast, the percentage of patients who underwent ileostomy or ileocolostomy and operation for perianal disease increased. Furthermore, an increasing trend in the number of patients who underwent stricturoplasty was detected. Laparoscopic surgery has also been increasingly applied to patients with CD. This finding may be because in recent years, the standards of diagnosis, medical therapy, and surgical management may have been developed concurrent with the establishment of further guidelines or consensuses regarding IBD.
Our study has some limitations. First, our results were obtained from an analysis of the literature in China, and some of the data are not properly classified or sorted within the published studies. Second, the length of the follow-up varies in these articles. Third, some data on patients with CD who underwent surgery were not published in China. However, the data we gathered from the selected papers were obtained from various hospitals throughout China. Furthermore, we searched four electronic databases to ensure that most publications were included. Therefore, our results may be representative of the clinical characteristics of patients with CD who underwent surgery in China. Fourth, although the clinical characteristics of patients with CD who underwent surgery between 1961-2000 and 2000-2012 were compared, 791 cases were excluded because they did not undergo surgery within either specific time interval. Fifth, many of the articles were observational studies. Hence, large population-based prospective studies are required to accurately predict the characteristics of surgery for CD to gain a better understanding of the natural history of CD.
In conclusion, the clinical characteristics of patients with CD who underwent surgery in China are generally similar to those of Western patients, except for a few differences. As in the West, the predominant surgical procedure for CD was partial bowel resection, and the primary indications for surgery were obstruction or failure of drug therapy. However, the rate of surgical complications and the rate of misdiagnosis in China were higher than those in the West, whereas the rate of CD complicated by tumors and the relapse rate were lower. In the past several years, the standards of diagnosis and therapy have continued to improve in China, resulting in fewer cases of misdiagnosis and surgery-related death. Moreover, additional types of surgery have been applied to patients with CD.
COMMENTS
Background
Surgery still plays a vital role in Crohn’s disease (CD) therapy. Although there were some studies about the clinical characteristics of the surgery in CD patients in varied hospitals in China, no multicenter or large observational studies have been published on the clinical characteristics of patients with CD who require surgery in China.
Research frontiers
Over the decades, more and more studies about Chinese CD patients requiring surgery were reported. However, most of these studies were small or based on single-center experiences. Therefore, it was insufficient to reach complete information about the clinical characteristics of Chinese CD patients who undergo surgery.
Innovations and breakthroughs
The authors summarized the clinical characteristics of the CD patients requiring surgery in China through literature review and obtained surgical information from 24 provinces or municipalities in China. The clinical characteristics were summarized, and compared with those of the West including the gender, the mean age, disease location, surgical indication, surgical procedure, surgical complication, surgical outcome, and the surgical development in recent years.
Applications
Clinicians may get some information about the Chinese specific clinical characteristics of CD patients requiring surgery. Then, they can make treatment decisions better for CD therapy. Large population-based prospective studies are still required to accurately predict the characteristics of surgery for CD to gain a better understanding of the natural history of CD.
Peer-review
This is an interesting study on clinical literature review of the surgery in 1858 CD cases in China.
Footnotes
Supported by Key Technologies Research and Development Program of China, No. 2012BAI06B03; and National Natural Science Foundation of China, No. 81270447.
Conflict-of-interest: Authors declare no conflict of interest.
Data sharing: No additional data are available.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: September 2, 2014
First decision: October 14, 2014
Article in press: January 16, 2015
P- Reviewer: Kanellos I, Tsujikawa T S- Editor: Ma YJ L- Editor: Wang TQ E- Editor: Wang CH
References
- 1.Wang YF, Ouyang Q, Hu RW. Progression of inflammatory bowel disease in China. J Dig Dis. 2010;11:76–82. doi: 10.1111/j.1751-2980.2010.00421.x. [DOI] [PubMed] [Google Scholar]
- 2.Zheng JJ, Zhu XS, Huangfu Z, Shi XH, Guo ZR. Prevalence and incidence rates of Crohn’s disease in mainland China: a meta-analysis of 55 years of research. J Dig Dis. 2010;11:161–166. doi: 10.1111/j.1751-2980.2010.00431.x. [DOI] [PubMed] [Google Scholar]
- 3.Travis SP, Stange EF, Lémann M, Oresland T, Chowers Y, Forbes A, D’Haens G, Kitis G, Cortot A, Prantera C, et al. European evidence based consensus on the diagnosis and management of Crohn’s disease: current management. Gut. 2006;55 Suppl 1:i16–i35. doi: 10.1136/gut.2005.081950b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Satsangi J, Silverberg MS, Vermeire S, Colombel JF. The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut. 2006;55:749–753. doi: 10.1136/gut.2005.082909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bernell O, Lapidus A, Hellers G. Risk factors for surgery and postoperative recurrence in Crohn’s disease. Ann Surg. 2000;231:38–45. doi: 10.1097/00000658-200001000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Frolkis AD, Dykeman J, Negrón ME, Debruyn J, Jette N, Fiest KM, Frolkis T, Barkema HW, Rioux KP, Panaccione R, et al. Risk of surgery for inflammatory bowel diseases has decreased over time: a systematic review and meta-analysis of population-based studies. Gastroenterology. 2013;145:996–1006. doi: 10.1053/j.gastro.2013.07.041. [DOI] [PubMed] [Google Scholar]
- 7.Gao X, Yang RP, Chen MH, Xiao YL, He Y, Chen BL, Hu PJ. Risk factors for surgery and postoperative recurrence: analysis of a south China cohort with Crohn’s disease. Scand J Gastroenterol. 2012;47:1181–1191. doi: 10.3109/00365521.2012.668931. [DOI] [PubMed] [Google Scholar]
- 8.Morimoto N, Kato J, Kuriyama M, Fujimoto T, Nasu J, Miyaike J, Morita T, Okada H, Suzuki S, Shiode J, et al. Risk factors and indications for first surgery in Crohn’s disease patients. Hepatogastroenterology. 2007;54:2011–2016. [PubMed] [Google Scholar]
- 9.Peyrin-Biroulet L, Harmsen WS, Tremaine WJ, Zinsmeister AR, Sandborn WJ, Loftus EV. Surgery in a population-based cohort of Crohn’s disease from Olmsted County, Minnesota (1970-2004) Am J Gastroenterol. 2012;107:1693–1701. doi: 10.1038/ajg.2012.298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.De Cruz P, Kamm MA, Prideaux L, Allen PB, Desmond PV. Postoperative recurrent luminal Crohn’s disease: a systematic review. Inflamm Bowel Dis. 2012;18:758–777. doi: 10.1002/ibd.21825. [DOI] [PubMed] [Google Scholar]
- 11.Cullen G, O’toole A, Keegan D, Sheahan K, Hyland JM, O’donoghue DP. Long-term clinical results of ileocecal resection for Crohn’s disease. Inflamm Bowel Dis. 2007;13:1369–1373. doi: 10.1002/ibd.20220. [DOI] [PubMed] [Google Scholar]
- 12.Wang YF, Zhang H, Ouyang Q. Clinical manifestations of inflammatory bowel disease: East and West differences. J Dig Dis. 2007;8:121–127. doi: 10.1111/j.1443-9573.2007.00296.x. [DOI] [PubMed] [Google Scholar]
- 13.Basilisco G, Campanini M, Cesana B, Ranzi T, Bianchi P. Risk factors for first operation in Crohn’s disease. Am J Gastroenterol. 1989;84:749–752. [PubMed] [Google Scholar]
- 14.Farmer RG, Whelan G, Fazio VW. Long-term follow-up of patients with Crohn’s disease. Relationship between the clinical pattern and prognosis. Gastroenterology. 1985;88:1818–1825. doi: 10.1016/0016-5085(85)90006-x. [DOI] [PubMed] [Google Scholar]
- 15.Kiran RP, Khoury W, Church JM, Lavery IC, Fazio VW, Remzi FH. Colorectal cancer complicating inflammatory bowel disease: similarities and differences between Crohn’s and ulcerative colitis based on three decades of experience. Ann Surg. 2010;252:330–335. doi: 10.1097/SLA.0b013e3181e61e69. [DOI] [PubMed] [Google Scholar]
- 16.Lu KC, Hunt SR. Surgical management of Crohn’s disease. Surg Clin North Am. 2013;93:167–185. doi: 10.1016/j.suc.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 17.Shaffer VO, Wexner SD. Surgical management of Crohn’s disease. Langenbecks Arch Surg. 2013;398:13–27. doi: 10.1007/s00423-012-0919-7. [DOI] [PubMed] [Google Scholar]
- 18.Agrez MV, Valente RM, Pierce W, Melton LJ, van Heerden JA, Beart RW. Surgical history of Crohn’s disease in a well-defined population. Mayo Clin Proc. 1982;57:747–752. [PubMed] [Google Scholar]
- 19.Zhou ZY, Luo HS. Differential diagnosis between Crohn’s disease and intestinal tuberculosis in China. Int J Clin Pract. 2006;60:212–214. doi: 10.1111/j.1742-1241.2006.00702.x. [DOI] [PubMed] [Google Scholar]
- 20.Arhan M, Köksal AS, Ozin Y, Kiliç ZM, Tunç B, Ulker A. Colonic tuberculosis or Crohn’s disease? An important differential diagnosis. Acta Gastroenterol Belg. 2013;76:59–61. [PubMed] [Google Scholar]
- 21.Epstein D, Watermeyer G, Kirsch R. Review article: the diagnosis and management of Crohn’s disease in populations with high-risk rates for tuberculosis. Aliment Pharmacol Ther. 2007;25:1373–1388. doi: 10.1111/j.1365-2036.2007.03332.x. [DOI] [PubMed] [Google Scholar]
- 22.Ramadas AV, Gunesh S, Thomas GA, Williams GT, Hawthorne AB. Natural history of Crohn’s disease in a population-based cohort from Cardiff (1986-2003): a study of changes in medical treatment and surgical resection rates. Gut. 2010;59:1200–1206. doi: 10.1136/gut.2009.202101. [DOI] [PubMed] [Google Scholar]
- 23.Hellers G. Crohn’s disease in Stockholm county 1955-1974. A study of epidemiology, results of surgical treatment and long-term prognosis. Acta Chir Scand Suppl. 1979;490:1–84. [PubMed] [Google Scholar]
- 24.Dignass A, Van Assche G, Lindsay JO, Lémann M, Söderholm J, Colombel JF, Danese S, D’Hoore A, Gassull M, Gomollón F, et al. The second European evidence-based Consensus on the diagnosis and management of Crohn’s disease: Current management. J Crohns Colitis. 2010;4:28–62. doi: 10.1016/j.crohns.2009.12.002. [DOI] [PubMed] [Google Scholar]
- 25.Okabayashi K, Hasegawa H, Watanabe M, Nishibori H, Ishii Y, Hibi T, Kitajima M. Indications for laparoscopic surgery for Crohn’s disease using the Vienna Classification. Colorectal Dis. 2007;9:825–829. doi: 10.1111/j.1463-1318.2007.01294.x. [DOI] [PubMed] [Google Scholar]
- 26.Rosman AS, Melis M, Fichera A. Metaanalysis of trials comparing laparoscopic and open surgery for Crohn’s disease. Surg Endosc. 2005;19:1549–1555. doi: 10.1007/s00464-005-0114-9. [DOI] [PubMed] [Google Scholar]
- 27.Polle SW, Wind J, Ubbink DT, Hommes DW, Gouma DJ, Bemelman WA. Short-term outcomes after laparoscopic ileocolic resection for Crohn’s disease. A systematic review. Dig Surg. 2006;23:346–357. doi: 10.1159/000097950. [DOI] [PubMed] [Google Scholar]
- 28.Soop M, Larson DW, Malireddy K, Cima RR, Young-Fadok TM, Dozois EJ. Safety, feasibility, and short-term outcomes of laparoscopically assisted primary ileocolic resection for Crohn’s disease. Surg Endosc. 2009;23:1876–1881. doi: 10.1007/s00464-008-0308-z. [DOI] [PubMed] [Google Scholar]
- 29.Brouquet A, Blanc B, Bretagnol F, Valleur P, Bouhnik Y, Panis Y. Surgery for intestinal Crohn’s disease recurrence. Surgery. 2010;148:936–946. doi: 10.1016/j.surg.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 30.Aratari A, Papi C, Leandro G, Viscido A, Capurso L, Caprilli R. Early versus late surgery for ileo-caecal Crohn’s disease. Aliment Pharmacol Ther. 2007;26:1303–1312. doi: 10.1111/j.1365-2036.2007.03515.x. [DOI] [PubMed] [Google Scholar]


