Abstract
Endoscopic retrograde cholangiopancreatography (ERCP) is a state of the art diagnostic and therapeutic procedure for various pancreatic and biliary problems. In spite of the well-established safety of the procedure, there is still a risk of complications such as pancreatitis, cholangitis, bleeding and perforation. Air leak syndrome has rarely been reported in association with ERCP and the optimal management of this serious condition can be difficult to establish. Our group successfully managed a case of air leak syndrome following ERCP which was caused by a 3cm Stapfer type I perforation in the posterolateral aspect of the second part of the duodenum and was repaired surgically. Hereby, we describe the presentation and subsequent therapeutic approach.
Keywords: Air leak syndrome, Endoscopic retrograde cholangiopancreatography, Complication, Perforation, Stapfer
Core tip: Diagnosis and management of air leak syndrome following endoscopic retrograde cholangiopancreatography (ERCP) can be challenging, complex and may be delayed because clinical findings can resemble those of pancreatitis. Moreover, ERCP-related perforation, as seen in our case hereby presented, is uncommon but has a high mortality rate. Stapfer et al classified ERCP-related perforations into four major groups. Hereby, we present a case with a Stapfer I type ERCP-related perforation which was successfully repaired surgically.
TO THE EDITOR
Endoscopic retrograde cholangiopancreatography (ERCP) is a state of the art diagnostic and therapeutic procedure for various pancreatic and biliary problems. In spite of the well-established safety of the procedure, there is still a risk of complications such as pancreatitis, cholangitis, bleeding and perforation. The incidence of major complications ranges from 5.4% to 23.0% and the overall mortality rate ranges from 0.1% to 1%[1]. On the other hand, delay in the diagnosis and intervention following duodenal perforation leads to significantly higher mortality (8%-23%) as a result of sepsis and multi-organ failure[2].
A 53-year-old female patient was admitted for an elective biliary stent replacement which had been placed in another center three months earlier for a benign common biliary duct obstruction. The patient underwent ERCP. The previously placed stent was removed with a snare and replaced with an 8.5 French 11 cm stent. Immediately after the completion of the procedure, the patient developed severe abdominal pain and vomiting. Physical exam revealed subcutaneous emphysema of the neck that extended up to the eye and the patient also had moderate abdominal distention with signs of peritoneal irritation. Complete blood count revealed leukocytosis (white blood cell count 16600/μL). Chest and abdominal X-rays demonstrated subcutaneous emphysema and retroperitoneal free air. A computed tomography scan with oral contrast of the thorax, abdomen and pelvis revealed diffuse subcutaneous emphysema, pneumomediastinum, pneumoretroperitoneum and pneumoperitoneum. There was no extravasation of oral contrast into the thorax and abdomen (Figure 1A and B). She was immediately started on broad spectrum antibiotics and after surgical consultation was promptly operated on after fluid resuscitation. A 3cm perforation in the posterolateral aspect of the second part of the duodenum was identified and repaired (Figure 1C). Intraoperative findings revealed retroperitoneal bile leakage. Debridement and drainage of the right retroperitoneal area was performed. Tube thoracostomy was also performed on the left side for a small pneumothorax. The postoperative course was uneventful.
Figure 1.
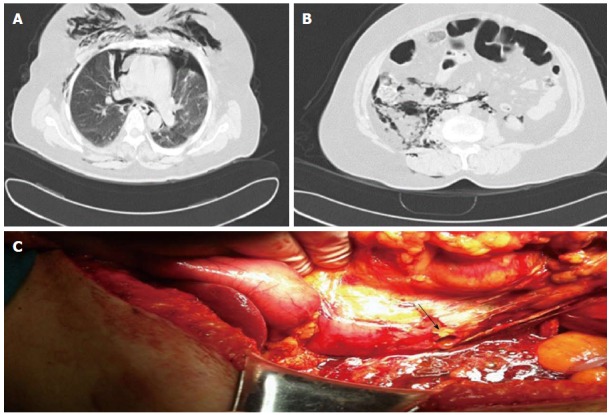
Abdominal computed tomography and posterolateral wall duodenal perforation. A: Abdominal computed tomography (CT) scan showing intra- and retroperitoneal free air. Transverse section of CT abdomen showing pneumoperitoneum and pneumoretroperitoneum; B: Transverse section of CT abdomen showing pneumoperitoneum and pneumoretroperitoneum; C: Posterolateral wall duodenal perforation. The patient underwent exploration five hours following perforation and the defect was managed with primary closure.
The incidence of ERCP-related perforation is low and yet mortality has been reported in up to 20% of patients[3]. ERCP-related perforations generally present as perforations to the retroperitoneal region. Such retroperitoneal perforations presenting with limited signs of peritoneal irritation can be managed conservatively. Stapfer et al[3] classified ERCP-related perforations into 4 types according to anatomic and mechanical properties and the severity of injury: Type I, lateral or medial duodenal wall; type II, perivaterian injury; type III, bile or pancreatic duct injury; and type IV, presence of retroperitoneal air alone without a true perforation. Ten to forty-three percent of type II perforations require surgical repair, whereas Type III and IV perforations usually resolve spontaneously. Our case was a Stapfer type I ERCP-related perforation. In some cases, as in our patient, air can dissect through fascial planes into potential neighboring spaces. Subcutaneous emphysema after an ERCP is a rare but well-recognized complication[4,5]. We presume that in our patient prolonged air insufflation caused air to dissect through the retroperitoneum and peritoneal cavity into the pleural space, mediastinum and subcutaneous tissue of neck, face and intramuscular and fascial planes around the right hip joint. Another probable mechanism is the entry of air along the perineural and perivascular sheaths into the mediastinum[6]. Apart from these mechanisms, it should also be kept in mind that in cases of large neoplastic hepatic masses, rupture of intrahepatic bile ducts and pneumobilia risk during ERCP leading to pneumoperitoneum is increased due to increased friability of neoplastic tissue[7].
In conclusion, ERCP-related perforation is uncommon but has a high mortality rate. Diagnosis may be delayed because clinical findings can resemble those of pancreatitis. Surgical indications in such cases are acute peritoneal irritation signs with or without sepsis and large contrast extravasation into the abdomen.
Footnotes
Conflict-of-interest: The authors declare no conflicting interests related to this paper.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: July 23, 2014
First decision: October 14, 2014
Article in press: February 13, 2015
P- Reviewer: Liberal R S- Editor: Yu J L- Editor: Roemmele A E- Editor: Wang CH
References
- 1.Masci E, Toti G, Mariani A, Curioni S, Lomazzi A, Dinelli M, Minoli G, Crosta C, Comin U, Fertitta A, et al. Complications of diagnostic and therapeutic ERCP: a prospective multicenter study. Am J Gastroenterol. 2001;96:417–423. doi: 10.1111/j.1572-0241.2001.03594.x. [DOI] [PubMed] [Google Scholar]
- 2.Avgerinos DV, Llaguna OH, Lo AY, Voli J, Leitman IM. Management of endoscopic retrograde cholangiopancreatography: related duodenal perforations. Surg Endosc. 2009;23:833–838. doi: 10.1007/s00464-008-0157-9. [DOI] [PubMed] [Google Scholar]
- 3.Stapfer M, Selby RR, Stain SC, Katkhouda N, Parekh D, Jabbour N, Garry D. Management of duodenal perforation after endoscopic retrograde cholangiopancreatography and sphincterotomy. Ann Surg. 2000;232:191–198. doi: 10.1097/00000658-200008000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Doerr RJ, Kulaylat MN, Booth FV, Corasanti J. Barotrauma complicating duodenal perforation during ERCP. Surg Endosc. 1996;10:349–351. doi: 10.1007/BF00187390. [DOI] [PubMed] [Google Scholar]
- 5.Mosler P, Fogel EL. Massive subcutaneous emphysema after attempted endoscopic retrograde cholangiopancreatography in a patient with a history of bariatric gastric bypass surgery. Endoscopy. 2007;39 Suppl 1:E155. doi: 10.1055/s-2006-925181. [DOI] [PubMed] [Google Scholar]
- 6.Alexiou K, Sakellaridis T, Sikalias N, Karanikas I, Economou N, Antsaklis G. Subcutaneous emphysema, pneumomediastinum and pneumoperitoneum after unsuccessful ERCP: a case report. Cases J. 2009;2:120. doi: 10.1186/1757-1626-2-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Assimakopoulos SF, Thomopoulos KC, Giali S, Triantos C, Siagris D, Gogos C. A rare etiology of post-endoscopic retrograde cholangiopancreatography pneumoperitoneum. World J Gastroenterol. 2008;14:2917–2919. doi: 10.3748/wjg.14.2917. [DOI] [PMC free article] [PubMed] [Google Scholar]


