Abstract
Background
Low birth weight is known to be associated with postnatal growth failure. It is not yet established that both conditions are determinants of psychomotor development. The study investigated whether or not low birth weight leads to delayed psychomotor development of a child, and whether it can be mitigated by adequate postnatal growth.
Methods
A cross-sectional study was conducted in 2002 in 15 rural and 11 urban communities of Sindh province, Pakistan. Assessment of 1234 children less than 3 years of age included Bayley's Scale of Infant Development II, socioeconomic questionnaire and anthropometry; WHO standards were used to calculate z-scores of height-for-age, weight-for-height and weight-for-age. The underlying study hypotheses were tested through multiple regression modelling.
Results
Out of 1219 children, 283 (23.2%) had delayed psychomotor development and 639 (52.4%) were undernourished according to the composite index of anthropometric failure. Strong negative associations with the psychomotor development index were detected between stunting and being underweight, with a larger magnitude of effect for stunting (p<0.001). The strong relationship persisted even when the analysis was restricted to non-malnourished children. The psychomotor index increased by 2.07 points with every unit increase in height-for-age z-score.
Conclusions
The relationship between low birth weight and psychomotor development appears to be mediated largely by postnatal growth and nutritional status. This association suggests that among undernourished children there is significant likelihood of a group that is developmentally delayed. It is important to emphasize developmental needs in programmes that target underprivileged children.
Keywords: Child development, Low birth weight, Nutritional status, Postnatal growth failure, Psychomotor development
Introduction
The overwhelming effects of low birth weight (LBW) and child under-nutrition are increasingly recognized, and consequently improved nutrition is vital to achieve the Millennium Development Goals. Conventionally, a birth weight of less than 2.5 kg is considered LBW.1 About 21 million babies are born with low birth weight: i.e. more than 16% of all births annually. Low birth weight contributes to poor health outcomes, the effects of which are more pronounced in developing countries.2–4 The magnitude of the problem is grave in south Asia where at least every fourth newborn has LBW.3,4
Worldwide, an enormous burden of under-nutrition among children is strongly associated with poor levels of child survival, accounting for 55% of under-5 mortality, and it is estimated that about 25% of the world's children under 5 years suffer from under-nutrition, particularly in African and Asian regions.2,4 Under-nutrition in children is commonly assessed through the measurement of weight and height, and it manifests in three ways: 1) a child can be too short for their age, i.e. stunted; 2) have low weight for their height i.e. wasted; 3) have low weight for their age, leading to being underweight. A child who is underweight can also be stunted, wasted or both.1 Under-nutrition also augments the effects of other childhood diseases such as diarrhea, measles, malaria and other infectious diseases.4
The dire need for more research on the developmental consequences of child nutritional status has been highlighted.4 Studies assessing the relationship between under-nutrition and child development during the early years of life are relatively limited and in particular those focusing on motor development are rare.5 Under-nutrition has been shown to have negative effects on child development, but the scientific evidence establishing a relationship with psychomotor status lacks consistency.6,7 Cheung et al.8 found that anthropometric indicators such as postnatal stunting and wasting were able to predict the age of walking among Pakistani children. Similar findings were reported in research studies from other countries.9 Contrary to those findings, however, no relationship was found between height and motor development in Kenyan infants.10 The WHO Motor Development Study Group has shown a lack of evidence for an association between growth and motor development among healthy children.11 Principally, the available literature is not comprehensive enough to cover all three anthropometric indicators of stunting, wasting and being underweight.12–14 There is only one study which explores the association between the three anthropometric indicators and psychomotor development (PD) but it did not control for any confounding factors.15 In the present study, we attempted to disentangle the relationship between postnatal anthropometric status and PD among LBW children.
The growth and development of a child are assumed to be closely correlated and the relationship between them is assumed to be straightforward: a well-nourished childhood means better child development and academic performance.16 However, several aspects of this association remain unexplored; in particular the importance of identifying the nature of developmental delays resulting from under-nutrition, and of establishing whether sound nutritional practices in the postnatal period can alleviate the harmful effect of poor fetal growth.
All the domains of child development (psychomotor, cognitive, emotional and social abilities) are vitally linked with a continuous cycle of nutrition and input from the social environment. Psychomotor abilities have a pivotal role in achieving the holistic development of well-balanced children during the early phases of life. We have opted for PD as an outcome in this study because it is relatively independent of cultural background during early years of life and its assessment is a robust measure as compared to mental-development during early child development. The conceptual underpinning of this study builds on strong scientific evidence to suggest that variation in children's physical growth is mainly determined by socioeconomic status (SES),17–19 and growth and development are interlinked. We postulate that nutritional status is on the causal pathway between SES and PD; LBW is known to be associated with postnatal growth failure. However, both nutritional status and PD are prevalent in the low SES groups and it is not clearly established whether the associations are independent or are a consequence of SES. There is a dearth of information about underlying mechanisms linking LBW with developmental delays such as social-environmental factors or current nutritional status. Moreover, it is not clear whether the prevailing scientific belief that poor fetal growth leads to irreversible damage as highlighted by the Lancet under-nutrition series, is also valid for PD.20
The 2013 State of World Children report shows that Pakistan has one of the highest rates of LBW (32%) in the world.21 More than 1.5 million children in Pakistan are currently suffering from acute malnutrition, making them susceptible to infectious diseases which may then lead to death. Long-term chronic malnutrition deteriorates both physical and mental development, and nearly half of Pakistan's children are currently chronically malnourished. The 2011 National Nutrition Survey in Pakistan shows that the under-5 prevalence of stunting was 43.7% whereas 15.1% of children are wasted, compared to 41.6% and 14.3%, respectively, in 2001.22 With LBW and under-nutrition being major public health problems, Pakistan therefore provides a suitable developing country setting to examine whether LBW exerts influence on PD and whether postnatal nutritional status can influence this association.
Materials and methods
Study setting and participants
A cross-sectional study was conducted from May to November 2002 in the province of Sindh in Pakistan. The selected urban and rural communities were those whose health services were provided by two NGOs: Aga Khan Health Services-Pakistan (AKHSP) and the Health and Nutrition Development Society (HANDS). The communities were operationally defined by these NGOs as urban and rural neighborhoods where the primary health care facility such as local health centre or health-post is managed by them. These NGOs collaborated in the study by facilitating the development of a sampling frame and obtaining formal permission from community elders. The field staff of the study approached the communities by contacting their local leaders and visited households to prepare a list of eligible households. All families with children under the age of 3 years were included from 26 communities: 15 rural (613 children) and 11 urban (621 children). In cases of more than one eligible child aged ≤3 years in a household, a single child was randomly selected by flipping a coin. Exclusion criteria were: twins, adopted, physically handicapped, resident in the communities for less than 6 months or refused informed consent by adult caregivers. From a population of 33 934, a total of 1234 eligible children were identified and assessed in their home setting. More details are available from a previous analysis.23
Psychomotor and anthropometric assessment
Bayley's Scale of Infant Development II (BSID II) was used to provide a standard measure of psychomotor performance. This yields a normalized, standardized score termed the PD index.24 All children were weighed and measured by study teams consisting of field workers, an assessor and a helper, according to the standard procedures recommended by the WHO.25 The results were compared with WHO growth standards25 and expressed in terms of z-scores. Two different methods were used to measure weight and height depending on the child's ability to stand or their age, i.e. a length measuring board and infant weighing scales for children aged <18 months, and a stadiometer and bathroom weighing scales for children aged >18 months. Globally stunting, wasting and being underweight were defined as height-for-age (HAZ), weight-for-height (WHZ) and weight-for-age (WAZ) having more than two standard deviations (z-scores) below the median of the WHO growth reference, respectively.
The proportions of the values that were missing or biologically implausible were used to ensure the assessment quality of the anthropometric measurements. WHO Anthro 2005 software (Geneva, Switzerland) flagged records (outliers) for each indicator based on fixed exclusion range criteria: if more than 1.5% of the anthropometric index records were flagged then the quality of the data set was considered as uncertain. The quality of our dataset was good; only 17 (1.37%) WHZ, 9 (0.72%) HAZ and 1(0.08%) WAZ records were flagged and were excluded; analysis was performed on a sample of 1219 children.
Analyses of birth weight were based on 652 (53.5%) children with birth records available at HANDS and AKHSP health facilities. Children with a birth weight below 2.5 kg (LBW) were considered as group 1. Study participants having a birth weight >2.5 kg were further divided into three additional groups as follows. Group 2: birth weight 2.50–2.99 kg; group 3: birth weight 3.00–2.29 kg; group 4: birth weight >3.30 kg.
Sociodemographic information
Background information on SES and demographics was by interviewing primary care givers (e.g. mothers) through detailed questionnaires. Based on information obtained a socioeconomic index (SE index) was created using principal component analysis technique (Supplementary information) and was used to control for the socioeconomic status in the analysis.
Study personnel and quality control measures
Clinical psychologists, community health nurses, sociologists and physicians comprised the 10-member field team. A field supervisor was responsible for quality assurance measures for the data collection. All-inclusive conceptual and practical training on study instruments was given to field staff for 4 weeks in both clinical and community settings until good intra- and inter-observer correlations were achieved. With the exception of specific quality control measures for the respective study instruments, general measures included regular refresher trainings, guidance and monitoring of the teams by cross checks in the field and observation of interviews by the study investigators and supervisor.
Statistical analysis
The analysis was carried out in four stages: 1) The prevalence of under-nutrition according to each indicator was calculated with respect to gender and age. A Composite Index of Anthropometric Failure (CIAF) was formed with children categorized into seven groups: stunted, wasted and under-weight; stunted and under-weight; wasted and under-weight; stunted only; wasted only; under-weight only; well-nourished.26 The category of ‘stunted and wasted’ was omitted as it is anthropometrically impossible and as such a child would always be under-weight. 2) Multiple linear regression was used to examine the relationship between PD index and the following factors: stunting, underweight, wasting and CIAF; each was controlled for a) age and gender, and b) age, gender and SE index, with the p-value for trend calculated where appropriate. 3) Analyses were repeated among the subgroup of healthy children, henceforth defined as those having all anthropometric indices with z-scores greater than –2; a proportion of these children were mildly malnourished (z-scores greater than –2 to 0) but they were retained in the healthy subgroups because clinically they do not require any active treatment. 4) The impact of LBW upon growth and with psychomotor development was examined using multiple regression analysis including adjustments for current anthropometric status, age, gender and SE index. A p-value of 0.05 was considered significant in all our analysis.
Ethical considerations
For obtaining informed consent of the study participants, initial contact was made with the community leaders with the aid of NGOs. The study aims, objectives and significance were explained to them in order to seek approval for contacting residents in the community. Individual informed consent was then obtained from the primary care-givers (mothers). As most of the study participants were illiterate their verbal informed consent was considered sufficient. In the event that a child was found to be sick at the time of data collection, the visit was rescheduled and guidance was provided for seeking appropriate medical care. Identification of any significant deficiency in growth and developmental status was followed by provision of advice to seek professional care and support. Members of the field teams were also trained to respond to queries from the care-givers that were related to child nutritional and psychosocial well-being at the end of the assessment session. All identifying information was removed during data analysis and no identifying information was provided in the dissemination of the results.
Results
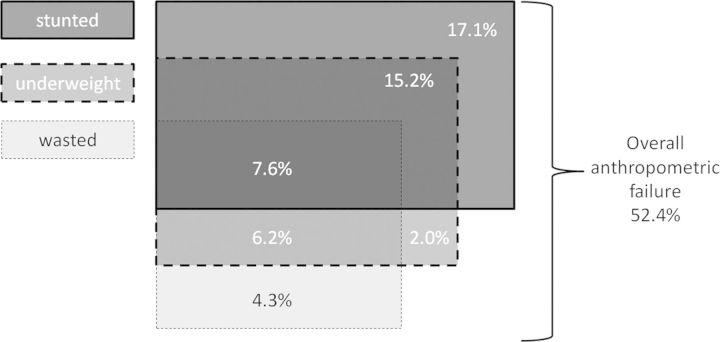
The percentage distribution of combinations of different types of under-nutrition based on CIAF is shown in Figure 1. Overall, 52.4% (639/1219) of the study children were under-nourished and among them 7.6% (93/1219) were concurrently stunted, under-weight and wasted. The combination of stunting and underweight was found in 15.2%, (185/1219), and wasting and underweight -only in 6.2% (75/1219), while 17.1% (208/1219) of children were stunted-only. Overall 39.9% (486/1219) of the children were stunted in the first 3 years of life, 30.9% (377/1219) were underweight and 18.1% (221/1219) were wasted. The results on prevalence of under-nutrition by age and gender showed that girls had better growth indicators compared to boys except for wasting (Supplementary Figure 1). The difference between male and female stunting was about 7% (p=0.012). Different age patterns were seen for the different indicators. In general, stunting rates increased with age (p<0.001), as one would expect owing to the cumulative nature of the stunting phenomenon. No trend with respect to age was observed for being underweight (p=0.553). In contrast, rates of wasting decreased with age (p<0.001).
Figure 1.
Composite index of anthropometric failure (CIAF): percentage distribution of combinations of different types of undernutrition.
The relationship between under-nutrition and PD
Table 1 shows that under-nourished children on average had lower PD indices, and the difference was statistically significant for all anthropometric indicators: e.g. age, gender and SE index. Adjusted mean psychomotor scores for stunted children were about seven points lower than those of children with normal linear growth. Table 2 shows the link between the PD index and combination of three types of under-nutrition, as defined by the CIAF. Psychomotor status was decreased by 10.6 units when a child was under-nourished on all three indicators as compared to a well-nourished child. It is important to note that only stunting containing under-nutrition groups of CIAF are significantly associated with lower PD index scores.
Table 1.
Relationship between under-nutrition and psychomotor development index
| Mean PDI (SD)a | Adjusted mean difference (95% CI)a | p-value | Adjusted mean difference (95% CI)b | p-value | ||
|---|---|---|---|---|---|---|
| Stunted | Yes | 90.63 (16.18) | −8.89 (−10.77, −7.01) | 0.000 | −6.89 (−8.77, −5.01) | 0.000 |
| No | 99.53 (16.11) | |||||
| Underweight | Yes | 90.74 (16.77) | −8.65 (−10.59, −6.70) | 0.000 | −6.47 (−8.44, −4.50) | 0.000 |
| No | 98.80 (16.50) | |||||
| Wasted | Yes | 93.07 (16.52) | −3.55 (−5.96, −1.14) | 0.040 | −1.71 (−4.05, 0.64) | NS |
| No | 96.62 (16.43) | |||||
| Any under-nutrition | Yes | 92.18 (16.92) | −7.66 (−9.47, −5.85) | 0.000 | −5.39 (−7.23, −3.55) | 0.000 |
| No | 100.15 (15.24) | |||||
NS: not significant; PDI: psychomotor development index.
Adjusted for age and gender.
Adjusted for age, gender and socioeconomic (SE) index.
Table 2.
Mean psychomotor development index by three types of undernutrition, composite index of anthropometric failure
| CIAF | % (n) | Mean PDI (SD) | Mean difference (95% CI) | p-value | Adjusted mean difference (95% CI)b | p-value |
|---|---|---|---|---|---|---|
| Stunted+underweight+wasted | 7.6 (93) | 86.40 (17.68) | −13.49 (−16.95, −10.03) | 0.000 | −10.61 (−14.06, −7.15) | 0.000 |
| Stunted+underweight | 15.2 (185) | 88.02 (17.61 | −11.71 (−14.34, −9.08) | 0.000 | −9.14 (−11.79, −6.48) | 0.000 |
| Stunted only | 17.1 (208) | 94.05 (15.36) | −5.31 (−7.86, −2.77) | 0.000 | −3.85 (−6.36, −1.35) | 0.003 |
| Underweight+wasted | 6.2 (75) | 97.89 (16.0) | −2.58 (−6.38, 1.22) | NS | −0.78 (−4.52, 2.96) | NS |
| Underweight only | 2.0 (24) | 93.92 (13.91) | −7.17 (−13.63, −0.71) | 0.030 | −4.91 (−11.24, 1.42) | NS |
| Wasted only | 4.3 (53) | 100.62 (14.61) | 2.29 (−5.25, 3.74) | NS | 0.80 (−3.59, 5.19) | NS |
| Well nourished | 47.7 (581) | 100.15 (15.24) | NA | NA | NA | NA |
CIAF: composite index of anthropometric failure; NA: not applicable; NS: not significant; PD: psychomotor development; PDI: psychomotor development index.
Adjusted for age and gender.
Adjusted for age, gender and socioeconomic (SE) index.
The relationship between healthy children and PD
By limiting the analysis to the subgroup of 581 healthy children (Table 3), a statistically significant association was observed between the physical growth and PD for each anthropometric index, e.g. the psychomotor status of children increased by 2.07 points with every increase in a height-for-age z-score.
Table 3.
Relationship between psychomotor development (PD) index and anthropometric status among healthy children (n=581)
| Adjusted mean difference/increment in z-score (95% CI)a | p-value | |
|---|---|---|
| HAZ | 2.07 (0.82, 3.32) | 0.001 |
| WAZ | 3.15 (1.72, 4.58) | 0.000 |
| WHZ | 1.80 (0.52, 3.09) | 0.006 |
HAZ: height-for-age z-score; WAZ: weight-for-age z-score; WHZ: weight-for-height z-score.
Adjusted for age, gender and socioeconomic (SE) index.
The relationship between LBW, postnatal under-nutrition and PD
The relationship between birth weight and current nutritional status is explored in Table 4. LBW children had 2–3 point lower mean psychomotor scores if they were under-nourished on any of the given anthropometric indicators. The same was true when birth weight groupings were used, suggesting that birth weight is a strong predictor of growth failure in the first 3 years of life even when controlled for age, gender and SES.
Table 4.
Relationship between birth weight and anthropometric status (n=647)
| Birth weight |
n (%) | Stunted OR (95% CI) | p-value | Underweight OR (95% CI) | p-value | Wasted OR (95% CI) | p-value | |
|---|---|---|---|---|---|---|---|---|
| LBWa | Yes | 86 (13.2) | 2.43 (1.51, 3.91) | 0.000 | 3.23 (1.99, 5.23) | 0.000 | 1.67 (0.92, 3.02) | NS |
| No | 566 (86.8) | 1 | NA | 1 | NA | 1 | NA | |
| Birth weight groupsa | 1 (<2.50 kg) | 86 (13.2) | 3.52 (1.99, 6.23) | 0.000 | 4.56 (2.47, 8.39) | 0.000 | 2.43 (1.13,5.22) | 0.022 |
| 2 (2.50–2.99 kg) | 179 (27.5) | 1.64 (1.01, 2.66) | 0.045 | 1.44 (0.81,2.55) | NS | 1.61 (0.81, 3.18) | NS | |
| 3 (3.00–2.29 kg) | 216 (33.1) | 1.72 (1.08, 2.72) | 0.022 | 1.75 (1.02, 3.00) | 0.041 | 1.70 (0.88, 3.27) | NS | |
| 4 (≥3.30 kg) | 171 (26.2) | 1 | NA | 1 | NA | 1 | NA | |
| p-value for trenda | 0.000 | 0.000 | 0.041 | |||||
| LBWb | Yes | 86 (13.2) | 2.39 (1.45,3.95) | 0.001 | 3.30 (1.97,5.51) | 0.000 | 1.60 (0.88, 2.92) | NS |
| No | 566 (86.8) | 1 | NA | 1 | NA | 1 | NA | |
| Birth weight groupsb | 1 (<2.50 kg) | 86 (13.2) | 3.01 (1.65, 5.46) | 0.000 | 3.87 (2.03, 7.35) | 0.000 | 2.16 (1.01, 4.68) | 0.050 |
| 2 (2.50–2.99 kg) | 179 (27.5) | 1.54 (0.92,2.55) | NS | 1.29 (0.71, 2.35) | NS | 1.52 (0.76, 3.02) | NS | |
| 3 (3.00–2.29 kg) | 216 (33.1) | 1.25 (0.76, 2.04) | NS | 1.21 (0.68, 2.14) | NS | 1.46 (0.75, 2.85) | NS | |
| 4 (≥3.30 kg) | 171 (26.2) | 1 | NA | 1 | NA | 1 | NA | |
| p-value for trendb | 0.000 | 0.000 | NS | |||||
LBW: low birth weight; NA: not applicable; NS: not significant; SE: socioeconomic.
Adjusted for age and gender.
Adjusted for age, gender and SE index.
Table 5 shows that on average LBW children had four point lower mean psychomotor scores compared to normal birth weight children. This difference remained even after adjustment for age, gender and SE index (p=0.051). Interestingly, the influence of birth weight on PD was considerably reduced and became statistically non-significant when stunting, being under-weight and wasting were added to the model (p=0.309). The same was true when we used birth weight grouping; no statistically significant trend was observed when adjusting for socioeconomic and current nutritional status. Hence, it appears that the association between PD index and LBW was largely mediated by postnatal growth.
Table 5.
Relationship between birth weight and psychomotor development (PD) index (n=647)
| Birth weight |
n (%) | Mean PDI (SD) | Adjusted mean difference (95% CI)a | p-value | Adjusted mean difference (95% CI)b | p-value | Adjusted mean difference (95% CI)c | p-value | |
|---|---|---|---|---|---|---|---|---|---|
| LBW | Yes | 86 (13.2) | 94.13 (18.13) | −4.21 (−7.88, −0.56) | 0.024 | −3.41 (−6.83, 0.02) | 0.051 | −1.82 (−5.33, 1.69) | NS |
| No | 566 (86.8) | 98.47 (15.84) | NA | NA | NA | NA | NA | NA | |
| Birth weight groups | 1 (<2.50 kg) | 86 (13.2) | 94.50 (1.76) | −6.08 (−10.28, −1.88) | 0.005 | −3.59 (−7.56, 0.38) | NS | −1.80 (−5.86, 2.26) | NS |
| 2 (2.50–2.99 kg) | 179 (27.5) | 98.60 (1.21) | −1.81 (−5.23, 1.61) | NS | −0.64 (−3.86, 2.57) | NS | −0.14 (−3.36, 3.08) | NS | |
| 3 (3.00–2.29 kg) | 216 (33.1) | 97.16 (1.20) | −3.16 (−6.42, 0.11) | 0.058 | −0.33 (−3.45, 2.79) | NS | −0.14 (−3.25, 2.97) | NS | |
| 4 (≥3.30 kg) | 171 (26.2) | 100.06 (1.25) | NA | NA | NA | NA | NA | NA | |
| p-value for trend | 0.022 | NS | NS | ||||||
LBW: low birth weight; NA; not applicable; NS: not significant; PDI; psychomotor development index.
Adjusted for age and gender.
Adjusted for age, gender and socioeconomic (SE) index.
Adjusted for age, gender, SE index, stunted, underweight and wasted.
Discussion
Overview
Our previous study incorporated a framework of fundamental directions of the relationship between psychomotor status, sensory stimulation and under nutrition.27 This current study highlights that nutritional status is a key factor for child development and delineates several fundamental conclusions. The findings substantiate existing scientific literature that SES is strongly associated with child under-nutrition. The relationship between child nutritional status and development appears to be multi-dimensional: adequacy of nutrition and levels of under-nutrition both strongly influence PD, and psychomotor delay is further exacerbated with the failure of a number of anthropometric indicators. Lower birth weight is strongly associated with the poor growth of the child within the first 3 years of life, however its association with PD appears to be largely mediated through its impact on postnatal growth.
Overall, more than half of the children investigated in this study were found to be under-nourished. The rates of under-nutrition are comparable with Pakistan's demographic health survey as well as the 2007 UNICEF survey28 and other regional surveys, adding to the validity of the study findings. Our findings are consistent with the existing literature in terms of gender and age differences in nutritional status in developing countries, and also support the evidence of socioeconomic inequality in the nutritional status of children.29–31
Growth and PD
Although PD of a child is considered to be strongly influenced by the nutritional status,9–15 this has never been systematically assessed. We have attempted to explore this association in three dimensions. Firstly, significantly poorer psychomotor status was found among both stunted and under-weight children, suggesting an effect of either chronic or non-specific nutritional fluctuations. The possible mechanism could be due to childhood under-nutrition resulting in a decrease in work performance due to suboptimal development of muscle and neuronal coordination.32 There is a general consensus that under-nutrition, especially being under-weight, is associated with childhood morbidities.33–35 However, scientific evidence of similar types of associations for developmental morbidities is very limited.36,37
Secondly, the impact of overall under-nutrition on PD was assessed by using an aggregate measure of under-nutrition, CIAF, as suggested by Svedberg.26 The conventional solitary anthropometric indicators have an overlapping nature: a child is likely to have a growth deficit on more than one indicator in real life scenarios. CIAF helps to identify the different groups of vulnerable children due to under-nutrition or those who are in a state of anthropometric failure. We found that children suffering from all three anthropometric indicators simultaneously have the lowest mean PD index scores. Furthermore, stunting or its combination with any other anthropometric indicator was significantly associated with PD index. To the best of our knowledge this is the first attempt to assess the influence of CIAF on child development.
Thirdly, we found a strong association between nutritional status and PD among healthy children suggesting that the effects of growth on childhood development are not limited to those with severe levels of malnutrition. Persistent marginally insufficient food intake is known to reduce physical performance before there is a substantial observable deficit in growth.38 Here it is important to note that gross motor milestones developed by WHO have shown no relationship with the nutritional status of the child.11 This finding might be linked to certain conceptual and analytical issues in development of these milestones e.g. PD is a continuous process comprising both gross and fine motor outcomes, whereas it comprised only six gross motor milestones in the WHO study. In addition, the method for generating motor standards was based on ‘windows of achievement’, defined as the time of attainment of a specific milestone bounded by the 1st and 99th percentile in months, rather than the conventional percentile curves. As a result, achievement of a specific milestone at a later month within a normal ‘window of achievement’ has a limited predictive value for a successful or failed motor outcome, as demonstrated by another study of child development in healthy populations.39
Birth weight, growth and PD
There is a strong body of evidence that prenatal (intrauterine) growth is a strong predictor of postnatal growth and consequently of an intergenerational vicious cycle of poor growth.3 In our analysis, lower birth weight was associated with lower psychomotor scores when controlled for age, gender and SES. However, when current nutritional status was added into the model, the association between birth weight and PD disappeared indicating that adequate postnatal nutrition can ameliorate the harmful effect of low birth weight.
Epidemiological literature on the influence of birth weight on psychomotor status is limited. A review identified seven eligible studies but was unable to draw any conclusions due to inconsistent definitions and assessment methodologies.14 A study conducted in Brazil demonstrated that LBW children have a PD index score 9.9 points lower at 12 months of age (p<0.001),40 while in our study LBW children aged under 3 years scored 4.3 points lower (p<0.001). Both studies have the same direction of association but the magnitude of the effect is different. This could be partially explained by the fact that in the Brazilian study the reference group was >3 kg, larger than the conventional cut-off of 2.5 kg which we used: this might have resulted in an inflated magnitude of effect. However, current nutritional status of a child is an important factor which can influence the association between the LBW and psychomotor status.
Limitations
Anthropometric indicators represent protein energy malnutrition. Micronutrient deficiency is another important determinant of child survival, growth and development. This aspect of under-nutrition assessment requires an enormous amount of resources and that was beyond the scope of this study.
Information about birth weight was available for only 53.5% of the sample. Primarily it represented a group of children whose mother received antenatal care and delivered either in hospital or a maternity home, and overall they had better SES as assessed in a separate analysis. This might have resulted in underestimation of association as a relatively vulnerable group was excluded from the analysis due to lack of data.
Due to the cross-sectional nature of this study, concurrent assessment of physical growth and psychomotor status raises the issue of reverse causality. However under-nutrition is more likely to be a potent determinant of physical growth and physical performance (motor development) as compared to the influence of physical performance on physical growth and under-nutrition. This is theoretically possible in extreme cases of physical activity/stress when the routine nutritional intake is primarily used to maintain bodily functions at the expense of growth.
Implications for policy and future research
This study emphasizes the fact that under-nutrition is a facet of poverty. Due to the strong association with SES, the levels of a child's growth and development can potentially be good indicators of the quality of life in a community. Furthermore, any assessment of nutritional status based on a single anthropometric indicator will underestimate the under-nutrition status of children; therefore, it is important to consider multiple indicators simultaneously to adequately describe growth status.
Anthropometric assessment is a well-recognized and widely practised strategy at population level to identify the needs of undernourished groups.34 In practice, such needs are limited to provision of nutrients and treatment for infections. However, it is important to consider the developmental needs of undernourished children in public health programmes that target improved child survival.
The practical implication of a lack of association between birth weight and PD due to mediation of its influence by postnatal growth suggests that efforts to improve child growth status can potentially ameliorate any harmful influences of antenatal growth on PD. Research efforts are required to further understand the underlying mechanisms of under-nutrition in child development morbidities, through properly designed longitudinal studies, in order to provide more comprehensive evidence for corrective public health initiatives in child health.
Supplementary data
Supplementary data are available at Transactions Online (http://trstmh.oxfordjournals.org/).
Acknowledgments
Authors' contributions: BIA conceived the study, designed the protocol and implemented the study. SAR and BRK contributed to interpretation of results. All authors critically revised the manuscript for intellectual content. All authors also read and approved the final manuscript. BIA is the guarantor of the paper.
Acknowledgments: Support for this study was provided by the Department of Child and Adolescent Health and Development, World Health Organization.
Funding: The study was funded through a cooperative agreement with the Bill and Melinda Gates Foundation and the US National Institute of Child Health and Human Development (NICHD) Global Network for Women's and Children's Health Research [HD40607-04 and HD40636-06] as part of a Fogarty Fellowship to BIA and also by the University Research Council of the Aga Khan University, Karachi, Pakistan [Grant ID: 021F410X9].
Competing interests: None declared.
Ethical approval: For institutional approval, the study protocol was submitted to the Ethics Review Committee of the Aga Khan University in Karachi, Pakistan and was approved [148-CHS/ERC-02]. Further approval was also obtained from National Institute of Health in US and the Ethics Committee of London School of Hygiene and Tropical Medicine in UK [reference number 3055].
References
- 1.Ohlsson A, Shah P. Determinants and prevention of low birth weight: a synopsis of the evidence. Alberta, Canada: Institute of Health Economics; 2008. http://www.ihe.ca/documents/IHE%20Report%20LowBirthWeight%20final.pdf. [accessed 9 September 2014] [Google Scholar]
- 2.Pelletier DL, Frongillo EA, Schroeder DG, Habicht JP. The effects of malnutrition on child mortality in developing countries. Bull World Health Organ. 1995;73:443–8. [PMC free article] [PubMed] [Google Scholar]
- 3.Ramakrishnan U. Nutrition and low birth weight: from research to practice. Am J Clin Nutr. 2004;79:17–21. doi: 10.1093/ajcn/79.1.17. [DOI] [PubMed] [Google Scholar]
- 4.Black RE, Allen LH, Bhutta ZA, et al. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. 2008;371:243–60. doi: 10.1016/S0140-6736(07)61690-0. [DOI] [PubMed] [Google Scholar]
- 5.Grantham-McGregor S, Cheung YB, Cueto S, et al. Developmental potential in the first 5 years for children in developing countries. Lancet. 2007;369:60–70. doi: 10.1016/S0140-6736(07)60032-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pollitt E, Jahari A, Walka HA. A developmental view of the effects of an energy and micronutrient supplement in undernourished children in Indonesia. Eur J Clin Nutr. 2000;54:S107–13. doi: 10.1038/sj.ejcn.1601012. [DOI] [PubMed] [Google Scholar]
- 7.Grantham-McGregor S. The relationship between developmental level and different types of malnutrition in children. Hum Nutr Clin Nutr. 1982;36:319–20. [PubMed] [Google Scholar]
- 8.Cheung YB, Yip PS, Karlberg JP. Fetal growth, early postnatal growth and motor development in Pakistani infants. Int J Epidemiol. 2001;30:66–72. doi: 10.1093/ije/30.1.66. [DOI] [PubMed] [Google Scholar]
- 9.Siegel EH, Stoltzfus RJ, Kariger PK, et al. Growth indices, anemia, and diet independently predict motor milestone acquisition of infants in south central Nepal. J Nutr. 2005;135:2840–4. doi: 10.1093/jn/135.12.2840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bhargava A. Modeling the effects of maternal nutritional status and socioeconomic variables on the anthropometric and psychological indicators of Kenyan infants from age 0–6 months. Am J Phys Anthropol. 2000;111:89–104. doi: 10.1002/(SICI)1096-8644(200001)111:1<89::AID-AJPA6>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 11.WHO Multicentre Growth Reference Study Group. WHO Motor Development Study: windows of achievement for six gross motor development milestones. Acta Paediatr Suppl. 2006;450:86–95. doi: 10.1111/j.1651-2227.2006.tb02379.x. [DOI] [PubMed] [Google Scholar]
- 12.Pollitt E, Oh S-Y. Early supplementary feeding, child development, and health policy. Food and Nutr. Bull. 1994;15:208–14. http://archive.unu.edu/unupress/food/8F153e/8F153E0c.htm. [accessed 12 September 2014] [Google Scholar]
- 13.Hoorweg J, Stanfield JP. The effects of protein energy malnutrition in early childhood on intellectual and motor abilities in later childhood and adolescence. Dev Med Child Neurol. 1976;18:330–50. doi: 10.1111/j.1469-8749.1976.tb03656.x. [DOI] [PubMed] [Google Scholar]
- 14.Grantham-McGregor SM, Fernald LC, Sethuraman K. Effects of health and nutrition on cognitive and behavioural development in children in the first three years of life, part 1: low birthweight, breastfeeding, and protein-energy malnutrition. Food and Nutr. Bull. 1999;20:53–75. http://archive.unu.edu/unupress/food/fnb20-1.pdf. [accessed 12 September 2014]. [Google Scholar]
- 15.Powell CA, Walker SP, Himes JH, et al. Relationships between physical growth, mental development and nutritional supplementation in stunted children: the Jamaican study. Acta Paediatr. 1995;84:22–9. doi: 10.1111/j.1651-2227.1995.tb13479.x. [DOI] [PubMed] [Google Scholar]
- 16.Pollitt E, Gorman KS, Engle PL, et al. Early supplementary feeding and cognition: effects over two decades. Monogr Soc Res Child Dev. 1993;58:1–99. [PubMed] [Google Scholar]
- 17.Bhandari N, Bahl R, Taneja S, et al. Growth performance of affluent Indian children is similar to that in developed countries. Bull World Health Organ. 2002;80:189–95. [PMC free article] [PubMed] [Google Scholar]
- 18.Owusu WB, Lartey A, de Onis M, et al. Factors associated with unconstrained growth among affluent Ghanaian children. Acta Paediatr. 2004;93:1115–9. doi: 10.1111/j.1651-2227.2004.tb02726.x. [DOI] [PubMed] [Google Scholar]
- 19.Som S, Pal M, Bhattacharya B, et al. Socioeconomic differentials in nutritional status of children in the states of West Bengal and Assam, India. J Biosoc Sci. 2006;38:625–42. doi: 10.1017/S0021932005026921. [DOI] [PubMed] [Google Scholar]
- 20.Victora CG, Adair L, Fall C, et al. Maternal and child undernutrition: consequences for adult health and human capital. Lancet. 2008;371:340–57. doi: 10.1016/S0140-6736(07)61692-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.United Nations Children's Fund and World Health Organization. New York: UNICEF; 2013. State of World Children 2013. http://www.unicef.org/guyana/SOWC_Report_2013.pdf. [Accessed 12 September 2014] [Google Scholar]
- 22.Pakistan National Nutrition Survey. Pakistan: UNICEF; 2011. Aga Khan University, Pakistan Medical Research Council, Ministy of Health Pakistan. https://pak.humanitarianresponse.info/system/files/documents/files/Pakistan_NNS_Version%2027.7.June%202012.pdf. [accessed 26 July 2014]. [Google Scholar]
- 23.Avan BI, Kirkwood B. Role of neighbourhoods in child growth and development: does ‘place’ matter? Soc Sci Med. 2010;71:102–09. doi: 10.1016/j.socscimed.2010.02.039. [DOI] [PubMed] [Google Scholar]
- 24.Bayley N. San Antonio: Harcourt Brace; 1993. Bayley scales of infant development II Manual. [Google Scholar]
- 25.WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr Suppl. 2006;450:76–85. doi: 10.1111/j.1651-2227.2006.tb02378.x. [DOI] [PubMed] [Google Scholar]
- 26.Svedberg P. Oxford: Oxford University Press; 2000. Poverty and Undernutrition: Theory, Measurement, and Policy. [Google Scholar]
- 27.Avan BI, Raza SA, Kirkwood BR. A community-based study of early childhood sensory stimulation in home environment associated with growth and psychomotor development in Pakistan. Int J Public Health. 2014;59:779–88. doi: 10.1007/s00038-013-0525-7. [DOI] [PubMed] [Google Scholar]
- 28.UNICEF. (2007) UNICEF Country Statistics: Pakistan. New York, USA; United Nations Children's Emergency Fund; 2007. http://www.unicef.org/infobycountry/pakistan.html. [accessed 13 August 2007] [Google Scholar]
- 29.Reed BA, Habicht JP, Niameogo C. The effects of maternal education on child nutritional status depend on socio-environmental conditions. Int J Epidemiol. 1996;25:585–92. doi: 10.1093/ije/25.3.585. [DOI] [PubMed] [Google Scholar]
- 30.Frongillo EA, Jr, de Onis M, Hanson KM. Socioeconomic and demographic factors are associated with worldwide patterns of stunting and wasting of children. J Nutr. 1997;127:2302–9. doi: 10.1093/jn/127.12.2302. [DOI] [PubMed] [Google Scholar]
- 31.Shen T, Habicht JP, Chang Y. Effect of economic reforms on child growth in urban and rural areas of China. N Engl J Med. 1996;335:400–6. doi: 10.1056/NEJM199608083350606. [DOI] [PubMed] [Google Scholar]
- 32.Udani PM. Protein energy malnutrition (PEM), brain and various facets of child development. Indian J Pediatr. 1992;59:165–86. doi: 10.1007/BF02759978. [DOI] [PubMed] [Google Scholar]
- 33.de Onis M, Onyango A, Borghi E, et al. Worldwide implementation of the WHO Child Growth Standards. Public Health Nutr. 2012;15:1603–10. doi: 10.1017/S136898001200105X. [DOI] [PubMed] [Google Scholar]
- 34.Black RE, Victora CG, Walker SP, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382:427–51. doi: 10.1016/S0140-6736(13)60937-X. [DOI] [PubMed] [Google Scholar]
- 35.Black RE, Allen LH, Bhutta ZA, et al. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. 2008;371:243–60. doi: 10.1016/S0140-6736(07)61690-0. [DOI] [PubMed] [Google Scholar]
- 36.Spurr GB. Physical activity and energy expenditure in undernutrition. Prog Food Nutr Sci. 1990;14:139–92. [PubMed] [Google Scholar]
- 37.Spurr GB, Reina JC, Dahners HW, Barac-Nieto M. Marginal malnutrition in school-aged Colombian boys: functional consequences in maximum exercise. Am J Clin Nutr. 1983;37:834–47. doi: 10.1093/ajcn/37.5.834. [DOI] [PubMed] [Google Scholar]
- 38.Viteri FE, Torun B, Immink MD, Flores R. Marginal malnutrition and working capacity. Prog Clin Biol Res. 1981;77:277–83. [PubMed] [Google Scholar]
- 39.Darrah J, Hodge M, Magill-Evans J, Kembhavi G. Stability of serial assessments of motor and communication abilities in typically developing infants–implications for screening. Early Hum Dev. 2003;72:97–110. doi: 10.1016/s0378-3782(03)00027-6. [DOI] [PubMed] [Google Scholar]
- 40.Grantham-McGregor SM, Lira PI, Ashworth A, et al. The development of low birth weight term infants and the effects of the environment in northeast Brazil. J Pediatr. 1998;132:661–6. doi: 10.1016/s0022-3476(98)70357-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.