Abstract
Introduction:
Treatment of tobacco use in mental health settings is rare despite high rates of comorbidity. With a focus on early intervention, we evaluated a tobacco treatment intervention among adolescents and young adults recruited from outpatient, school-based, and residential mental health settings and tested for gender differences.
Methods:
Intervention participants received computerized motivational feedback at baseline, 3 months, and 6 months and were offered 12 weeks of cessation counseling and nicotine patches. Usual care participants received a self-help guide and brief cessation advice. We examined 7-day point prevalence abstinence with biochemical confirmation at 3, 6, and 12 months; smoking reduction; and 24-hr quit attempts.
Results:
At baseline, the sample (N = 60, 52% female, mean age = 19.5±2.9 years, 40% non-Hispanic Caucasian) averaged 7±6 cigarettes/day, 62% smoked daily, 38% smoked ≤ 30min of waking, 12% intended to quit in the next month, 47% had a parent who smoked, and 3 of 5 of participants’ closest friends smoked on average. During the 12-month study, 47% of the sample reduced their smoking, 80% quit for 24 hr, and 11%, 13%, and 17% confirmed 7-day point prevalence abstinence at 3-, 6-, and 12-month follow-up, respectively, with no differences by treatment condition (ps > .400). Over time, abstinence was greater among girls (adjusted odds ratio [AOR] = 8.9) than among boys, and abstinence was greater for lighter smokers than heavier smokers (AOR = 4.5) (p < .05). No mental health or other measured variables predicted abstinence.
Conclusions:
Adolescent and young adult smokers with mental health concerns are a challenging group to engage and to effectively treat for tobacco addiction, particularly heavier smokers and boys. Innovative approaches are needed.
Introduction
Tobacco use among adolescents and young adults in the United States remains a significant problem for public health. In 2013, 15% of girls and 16% of boys in the 9th to 12th grades reported tobacco use in the past 30 days, and the prevalence of every-or-some day smoking among young adults aged 18–24 is 20% for men and 15% for women.1,2 Over 90% of smokers start before the age of 18,3 and few (5%–6%) are likely to quit without treatment.4 To significantly alleviate the burden of tobacco-related illness, effective interventions targeted at adolescents and young adults are needed. Encouragingly, quitting before the age of 30 is estimated to prevent over 90% of all harm from smoking.5,6
Stanton and Grimshaw’s7 Cochrane review of tobacco cessation interventions for smokers under age 20 pooled data from 28 controlled trials and identified as promising approaches those based on the transtheoretical model (TTM; pooled risk ratio [RR] of 1.56 at 1 year; 95% CI = 1.21–2.01) or including motivational enhancement (RR of 1.60, 95% CI = 1.28–2.01). Only 3 of the 28 trials tested pharmacological approaches and with limited efficacy. Nicotine replacement therapy (NRT) is not approved by the FDA for use with children or adolescents and cannot be purchased over-the-counter by smokers under age 18 years, though can be prescribed and used by youth under the supervision of a physician. A study with 120 adolescent smokers aged 13–17 found that the nicotine patch, but not the nicotine gum, had a significant effect for prolonging abstinence relative to placebo.8
Adolescent and young adult smokers can be challenging to engage in treatment, as few intend to quit smoking in the near future.9,10 Backinger et al.11 estimated participation among young people in smoking cessation intervention trials is typically between 2% and 10%. Cigarette smoking is illegal for those under 18, and required parental consent for treatment is a barrier. Engagement is particularly challenging among youth with poor academic performance12 and behavioral health concerns, common among smokers.13
Tobacco use in adolescence is associated with a number of mental health disorders including attention deficit, panic disorder, schizophrenia, and major depression.14–17 Youth with mental health problems report greater lifetime and current smoking as well as heavier smoking and tobacco dependence.18–20 Smoking prevalence has been reported as high as 60% among adolescents receiving inpatient psychiatric treatment, with 40% averaging a pack or more per day.21
The documented intersection of tobacco and mental illness has led to calls for recognition of smokers with co-occurring psychiatric disorders as a disparity group in need of national surveillance, research, and treatment.22,23 The 2008 update of the U.S. Clinical Practice Guidelines for tobacco cessation was informed by nearly 8,800 research articles; yet fewer than two-dozen trials have been conducted with smokers with mental illness, of which only one was conducted with adolescents. Brown et al.24 recruited 191 smokers aged 13–17 years from an inpatient psychiatry unit and evaluated a motivational-interviewing intervention combined with NRT patch relative to usual care. Abstinence rates did not differ by condition or gender; however, the intervention was associated with enhanced self-efficacy and more so among boys than girls.
The adult literature indicates gender differences in the experience of nicotine withdrawal and success with quitting in clinical trials25–28; few studies have reported on gender differences in adolescent smokers. A randomized, placebo-controlled, double-blind trial of the NRT patch for smoking cessation found that adolescent girls experienced similar nicotine withdrawal severity but greater nicotine craving relative to boys.29 A survey study from 1988 to 1992 with 1,430 youth recruited from 24 California and Illinois high schools found that boys and girls were similar with regard to smoking stage of change and perceived likelihood of ever quitting smoking, while boys were somewhat more likely to have tried to quit in the past, and girls reported more circumstances tempting them to smoke, particularly related to affective states and efforts to avoid nicotine withdrawal.10
With a focus on adolescents and young adults with mental health concerns and a goal of early intervention, we sought to extend our team’s efforts with treating tobacco dependence in adults with mental health disorders. Our prior studies tested an intervention package combining computer-assisted TTM-tailored counseling plus NRT with replication of significant treatment effects in clinically depressed outpatients30 and in adults recruited from acute care psychiatric units,31 with comparable treatment effects by gender. For extension to adolescents and young adults, we conducted formative interviews with current smokers aged 13–25 recruited from outpatient mental health settings and their mental health providers.32 Informing treatment adaptations, the youth identified addiction and mood control as reasons for smoking, along with influences from media, parents, and peers. Both clinicians and the youth recommended providers increase their attention to patients’ tobacco use, and they identified mental health clinics as viable settings for treatment delivery.32 Treatment recommendations did not differ by gender.
The primary aims of this randomized controlled clinical trial were to (a) examine the feasibility of recruiting and retaining adolescent and young adult smokers for a cessation trial initiated in mental health settings, (b) examine treatment efficacy relative to usual care, and (c) explore gender differences in treatment outcomes. Given modest success with youth tobacco cessation interventions in the literature, we examined treatment efficacy in terms of traditional abstinence, in relation to heaviness of smoking, and with secondary outcomes of reduced cigarettes per day and 24-hr quit attempts.
Methods
Sample Recruitment, Eligibility, and Randomization
Participants were recruited between April 2008 and June 2010 from 17 mental health settings in the San Francisco Bay Area including an academic-based child and adolescent psychiatric outpatient clinic; a 24-hr service facility with wraparound care serving patients age 13–25; public outpatient, school-based, and residential programs serving Medicaid-eligible youth through age 25; and university student mental health clinics. Recruitment efforts included direct referrals from mental health providers and posted flyers in the clinical settings. Informed consent/assent was obtained from the youth and their parents or clinicians as appropriate (for youth, <18 years of age). For study enrollment, we obtained IRB approval to waive parental consent with clinician sign-off, per the state of California law § 6929(b), which permits the treatment of minors for drug use without parental permission. For use of NRT, however, we required parental permission.
The study procedures were approved by the University of California, San Francisco IRB with permission from the clinical site ethics committees as appropriate. Adolescents and young adults between the ages of 13 and 25 who were receiving mental health treatment at one of the recruitment sites and who reported smoking at least one cigarette in the past month and at least 100 cigarettes in their lifetime were eligible for the study. Those who did not speak English or were currently receiving smoking cessation treatment were excluded. Intention to quit smoking was not required as the treatment was tailored to readiness to quit. We previously reported on sample baseline characteristics, and over half of the sample was not intending to quit in the near future.33 Over the course of the 12-month trial and four assessment points, participants could earn $120 in gift cards for their time and $40 for travel costs.
A total of 110 candidates were screened, of whom 47 were ineligible. Reasons for exclusion were: lifetime cigarettes <100, age >25, lack of contact information, plans to relocate out of area, and lack of a mental health provider or no mental health services being received. Of the remaining 63, 60 agreed to participate in the study and provided informed assent/consent. Following completion of baseline assessments, participants were randomized to either the treatment or control condition using a computer-generated randomization scheme that blocked on tobacco use (daily vs. nondaily) and stage of change (precontemplation, contemplation, or preparation).
Conditions
Treatment
The two-staged treatment approach combined a motivational engagement program for all intervention participants followed by a cessation program for intervention participants who expressed intention to quit. Stage 1 consisted of a TTM-tailored computer-assisted intervention completed at baseline and repeated at months 3 and 6 with brief counseling. The intervention assessed key TTM constructs (stage of change, decisional balance, self-efficacy, processes of change) and provided feedback that was normative (comparing to others in the same stage of change) and ipsative (comparing to the participants’ earlier responses). Based on findings in our formative work with youth, we adapted the computer-assisted intervention images and tailored feedback to better reflect young people’s life demands and experiences (e.g., reference to school, parents, peers, clubs/sports). Stage 2 provided six sessions over 12 weeks of cognitive-behavioral treatment (CBT)-oriented individual cessation counseling with an adolescent tobacco treatment manual developed by Brown et al.24 that attended to peer relationships, family influences, and the co-use of alcohol and illicit drugs. With the counseling, 12 weeks of NRT patch was available from the study for those who smoked five or more cigarettes daily, had parental consent, and no medical contra-indications determined via consultation with the study physician. Participants could initiate the Stage 2 cessation program at any time through the first 9 months of their study enrollment.
Usual Care
Participants randomized to the usual care condition received a quit smoking self-help brochure and brief advice to quit.
Measures
Descriptive Measures
Demographic measures included age, gender, years of education, race/ethnicity, and residence, coded as living at home with parents or other. To avoid possible stigma and labeling of the youth, psychiatric disorder diagnoses were not assessed or recorded. Instead, mental health measures were behavioral or treatment oriented and included: (a) the number of mental health service visits in the past month (i.e., medication management, individual therapy, group therapy, case management); (b) lifetime history of psychiatric hospitalization; (c) lifetime trauma-exposure, assessed as physical injury to self or other or threat to one’s own life or another’s combined with the experience of feeling helpless or terrified; (d) the Behavior Assessment System for Children (BASC-2), completed by participants under 18 years of age, with scales reflecting internalizing problems, inattention/hyperactivity, school problems, emotional symptoms, and personal adjustment; and (e) the Behavior and Symptom Identification Scale (BASIS-24), completed by participants 18 and over, with subscales of depression and functioning, interpersonal relationships, psychosis, substance abuse, and emotional lability. To allow for analyses across age groups, scale scores for the BASC-2 internalizing scale and the BASIS-24 depression scale were standardized (i.e., z-scores) and combined. Additionally, we examined responses to single items on the BASC-2 and BASIS-24 that assessed seeing or hearing things that others do not. Substance use measures were (a) days of alcohol and drug use in the past month, (b) receipt of treatment for alcohol or drug use in the past month (i.e., outpatient, inpatient, self-help), and (c) lifetime history of drug overdose. “Tobacco Measures” included smoking history (age of first smoking, other tobacco use); prior quit attempts; money spent on tobacco; time to first cigarette in the morning (<30min); heaviness of smoking (based on median split of the sample on baseline cigarettes per day, divided at less than seven cigarettes per day or seven or more cigarettes per day); Smoking Stage of Change34 categorized as precontemplation (no intention to quit within the next 6 months), contemplation (intention to quit within the next 6 months), preparation (intention to quit in the next 30 days with a past year 24-hr quit attempt), action (quit for less than 6 months), and maintenance (quit for 6 months or more); Thoughts About Abstinence Scale35 with 10-point rating scales of participants’ desire to quit, expectations for success with quitting, and perceived difficulty of preventing relapse and a fourth item assessing smoking goal; peer smoking, assessed as the number of participants’ five closest friends who smoke; and parental smoking.
Outcome Measures
The primary outcome was 7-day point prevalence abstinence assessed at 3-, 6-, and 12-month follow-up. Participants who reported no tobacco use, not even a puff, in the past 7 days, provided a breath sample evaluated with a Bedfont smokerlyzer with carbon monoxide readings of ≤10 ppm confirming abstinence at months 3 and 6 and a saliva sample with cotinine levels of <15ng/ml confirming abstinence at month 12, when study-provided NRT should have ended. Secondary outcomes were measured changes in thoughts about abstinence, reductions in cigarettes per day assessed for the past 7 days at baseline and each follow-up, and the likelihood of a 24-hr quit attempt over the 12-month trial.
Statistical Analysis
Descriptive statistics on baseline measures were run to describe the sample with differences by gender tested with t-tests and chi-square. To examine treatment efficacy, we ran a generalized estimating equation (GEE) model with the logit link function (PROC GENMOD in SAS version 9.2; SAS Institute) and tested abstinence versus smoking status at the 3- through 18-month follow-ups by condition (intervention vs. control). The model accounted for dependence of responses within individuals attributable to repeated measures and allowed us to derive effect estimates from all available data. To examine gender differences, we ran a second model with independent variables of condition, gender (boys vs. girls), mental health measures of interest, and tobacco-related variables found to differ by gender at baseline. Secondary outcomes were tested with chi-square (quit attempt) and t-test (smoking reduction, change in thoughts about abstinence).
Results
Sample Characteristics
Baseline descriptive statistics for the full sample have been reported previously,33 and there was no difference in measured variables by treatment group. All participants were receiving mental health treatment, and 12% were in concurrent treatment for drugs or alcohol. Most participants (83%) reported experiencing or witnessing injury or threat to their own or another’s life, and 63% of the sample reported trauma reactions of terror or helplessness. A majority (62%) reported prior hospitalization for mental illness.
Table 1 presents sample characteristics by gender. Boys and girls were similar on all measured variables with the exception of peer smoking and use of other tobacco products. Boys reported more of their close friends smoked and also were more likely to report prior use of other tobacco products. In order of frequency of report, these were cigars, cigarillos, blunts, smokeless tobacco, hookah, pipes, and e-cigarettes. On the continuous mental health measures, the youth under age 18 (n = 8 boys and 9 girls) did not significantly differ by gender on any of the BASC subscales with mean t-score values by gender within 1 SD and all group comparison p values >.240. For the youth 18 and over (n = 21 young men and 20 young women), there was no difference by gender on any of the BASIS-24 scales with all group comparison p values >.160. Further, boys and girls did not significantly differ in prior history of a psychiatric hospitalization, past month drug or alcohol treatment, trauma exposure, hearing or seeing things that others do not, or on an index of depression/internalizing problems (i.e., a z-score transformation combination of the BASC and BASIS-24 scales), though on all of these measures, girls had scores suggestive of greater severity and treatment engagement relative to boys.
Table 1.
Demographic, Mental Health, and Tobacco Characteristics by Gender
| Boys | Girls | |
|---|---|---|
| n = 29 | n = 31 | |
| Age (years) | 19.7 (3.0) | 19.3 (2.9) |
| Race/ethnicity | ||
| Caucasian | 41.4% | 38.7% |
| Hispanic | 24.1% | 9.7% |
| African American | 6.9% | 9.7% |
| Asian American | 10.3% | 3.2% |
| Multiracial/other | 17.3% | 38.7% |
| Education (years) | 11.2 (3.1) | 11.9 (2.1) |
| Past month no. of days with mental health visits | 8.5 (8.9) | 8.5 (8.0) |
| Lifetime psychiatric hospitalization | 51.7% | 71.0% |
| Trauma exposed | 58.6% | 67.7% |
| Depression/internalizing scale z-score | −0.23 (.96) | 0.21 (.96) |
| Hears or sees things others do not | 13.8% | 27.6% |
| Past month substance use | ||
| Alcohol | 58.6% | 58.1% |
| Marijuana | 51.7% | 32.3% |
| Other illicit drug | 17.2% | 25.8% |
| Past 30 days treated for alcohol or drugs | 6.9% | 16.7% |
| History of drug overdose | 13.8% | 35.5% |
| Age first tried smoking (year) | 12.9 (3.2) | 13.7 (2.6) |
| Years smoking regularly | 4.0 (2.6) | 3.1 (1.7) |
| Daily smoker | 51.7% | 48.4% |
| Cigarettes/day | 8.2 (5.7) | 6.2 (5.8) |
| $ spent past month on tobacco (median, IQR) | $30 (10, 60) | $25 (10, 64) |
| Use of tobacco products other than cigarettes* | 62.1% | 19.4% |
| Smoke within 30min of waking | 34.5% | 41.9% |
| Smoking stage of change | 55.2% | 48.4% |
| Precontemplation | 27.6% | 45.2% |
| Contemplation | 17.2% | 6.5% |
| Preparation | ||
| Past-year 24-hr quit attempt | 48.3% | 60.0% |
| Thoughts about abstinence | ||
| Desire to quit | 5.8 (2.5) | 4.5 (2.7) |
| Perceived success with quitting | 4.9 (2.8) | 4.3 (2.4) |
| Anticipated difficulty staying quit | 6.9 (2.9) | 6.5 (2.3) |
| No goal to quit | 27.6% | 19.4% |
| Parent smokes | 48.3% | 44.8% |
| Home is smoke-free | 41.4% | 58.1% |
| 3 or more of 5 closest friends smoke* | 75.9% | 48.4% |
IQR = interquartile range.
*p ≤ .05 for test of difference by gender.
Treatment Engagement and Retention
All treatment participants completed Stage 1, receiving TTM-tailored computer-assisted individual counseling. Five of 28 participants (18%) entered Stage 2; all five were males, with four completing all six CBT sessions and three receiving study-provided NRT. At baseline, relative to the other intervention participants, the five males who entered CBT cessation counseling reported two-fold greater cigarette consumption: M = 12.7 (SD = 6.0) versus M = 5.6 (SD = 4.5), F (1,30) = 9.39, p = .005; had a greater desire to quit: M = 7.6 (SD = 1.1) versus M = 4.0 (SD = 2.3), F (1,30) = 11.66, p = .002; were less likely to be in precontemplation: 0% versus 62%, χ2 = 6.36, p = .018; and had more past year quit attempts: M = 3.4, SD = 3.8 versus M = 1.1 (SD = 1.8), F (1, 30) = 4.58, p = .041. Follow-up rates for treatment and usual care participants were 93% and 94% at 3 months, 89% and 87% at 6 months, and 86% and 90% at 12 months and did not differ by gender.
Change in Smoking Overtime by Condition
Nearly half the sample (47%) reduced cigarettes per day from baseline with 20% reducing by 50% or greater; 80% made a 24-hr quit attempt; and 11%, 13%, and 17% reported 7-day point prevalence abstinence at 3-, 6-, and 12-month follow-up, respectively (10%, 12%, and 15% if assume those lost to follow-up were smoking). None of the tobacco outcomes differed by treatment group (all p values >0.400).
Predictors of Smoking Outcomes
Two variables predicted tobacco abstinence at 12-month follow-up independent of treatment condition in the GEE model: gender (adjusted odds ratio [AOR] = 8.9, 95% CI = 1.8, 44.4) and heaviness of smoking (AOR = 4.5, 95% CI = 1.0, 21.0). Use of other tobacco products (p = .722), number of close friends who smoke (p = .086), hearing voices (p = .760), depression/internalizing symptoms (p = .655), trauma exposure (p = .693), residing at home (p = .933), and condition (p = .477) were not significant factors in the GEE model, and their entry did not influence the strength of associations of gender and heaviness of smoking with abstinence. Figure 1a and b shows the abstinence rates overtime by gender and heaviness of smoking coding missing as missing and missing as smoking. Gender and heaviness of smoking differences were not apparent until the 6- and 12-month follow-ups, suggesting that boys initially tried to quit at 3 months but then struggled. Girls who smoked less than seven cigarettes per day had the greatest likelihood of quitting; girls who were heavier smokers looked similar to boys until the 12-month follow-up when none of the boys reported abstinence. Additionally, though not a significant variable in the GEE model, we observed that all nine participants who were quit at 12 months resided in their parents’ home.
Figure 1.
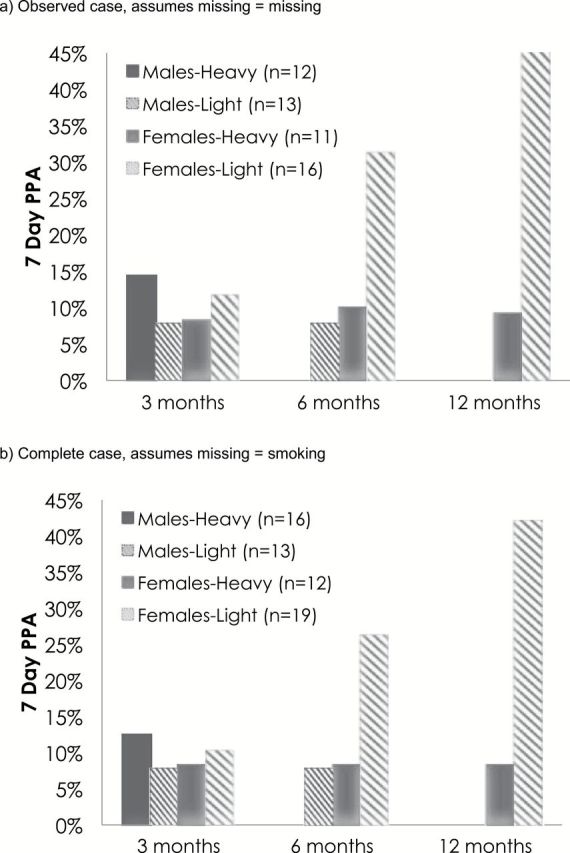
Abstinence over time by gender and heaviness of smoking.
In terms of thoughts about abstinence, girls increased in desire to quit (mean = 2.0, SD = 3.3) more than boys (mean = 0.3, SD = 2.8) from baseline to 12 months (p = .033, F (1,59) = 4.78). Gender differences on expected success with quitting were not significant (p = .115) but were in the direction of greater increase for girls compared to boys. Baseline heaviness of smoking was unrelated to thoughts about abstinence, mental health indices, and exposure to parent and peer smoking (all p > .40).
Discussion
Adolescent and young adult smokers with mental illness are a challenging group to engage and effectively treat for tobacco dependence. Intention to quit was not a requirement for participation in this trial, and despite tripling our number of recruitment sites and doubling the study incentive, enrollment was lower than hoped. The intervention effect was not significant; however, the 12-month quit rate among girls and lighter smokers was comparable to cessation rates reported in other studies with adolescents without mental illness.7 Abstinence from smoking among girls increased over time, which is consistent with motivational approaches targeting smokers not initially ready to quit. In contrast, abstinence among boys was comparable to girls at 3 months, but then declined at 6 months, and by 12 months all had returned to smoking. The finding of greater abstinence among youth smoking less cigarettes at baseline may be due to an easier time with quitting due to lower nicotine dependence; may reflect greater environmental or social controls; or reduction efforts in anticipation of quitting.
The lack of a significant intervention effect is consistent with findings from a randomized clinical trial of adolescent smokers aged 13–17 years recruited from inpatient psychiatry and randomized to brief advice or a motivational-interviewing intervention combined with NRT patch; 7-day point prevalence abstinence was 10% with brief advice and 14% for the intervention.24 The two-stage treatment approach employed in the current study provided motivational engagement to all intervention participants, followed by a CBT-based cessation program for only those participants who expressed intention to quit. Due to low readiness to quit smoking among adolescent and young adult smokers in mental health settings, fewer than 20% of intervention participants entered Stage 2, with only four participants completing all six CBT sessions and three receiving study-provided NRT. Notably, the five participants who entered CBT treatment were all boys; they reported desire and intention to quit but also were challenged by heavier smoking and a recent history of unsuccessful quit attempts. Previous randomized clinical trials of adolescents24 and adults30,31 with psychiatric problems have not found significant gender differences in abstinence rates. The lower abstinence rates and less expected success with quitting over time among boys versus girls in the current study, however, suggests innovative, and perhaps gender-specific, cessation treatments are needed to engage and retain adolescent and young adult smokers in the long-term process of quitting smoking.
There were few gender differences in the measured demographic, mental health, and tobacco use variables to explain the gender differences in abstinence. Notably, boys reported more of their close friends smoke and they were more likely to report ever use of other forms of tobacco, including cigarillos, hookah, and blunts. Less commonly reported at the time this study was conducted were e-cigarettes. Neither of these gender group differences was related to abstinence status and neither reduced the strength of the association between gender and abstinence. The finding that all nine girls who were quit at 12 months were residing at home with their parents is interesting and suggestive of a supportive parental effect.
Study limitations include the small sample size due to challenges with engaging young smokers into a smoking intervention study. That said, the recruited sample was diverse with respect to age and race/ethnicity and was balanced on gender allowing for group comparisons. Further, study retention was strong and did not differ by condition or gender. Future research is needed to determine ways to optimally engage young smokers into cessation programs and with larger sample sizes to identify the determinants of gender differences.
Funding
This work was supported by the National Institute on Drug Abuse (#K23 DA018691 and #P50 DA09253).
Declaration of Interests
Judith Prochaska has served as an expert witness against the tobacco companies in lawsuits for which she has received fees for the work and has provided consultation to Pfizer, which makes medications for quitting smoking. Sharon Hall has consulted with Gilead and Sleepio. All other contributing authors declare no competing interest.
Acknowledgments
We acknowledge our clinical collaborators Ken Epstein, MSW, Alan Louie, MD, Celia Moreno, MD, and Susan Smiga, MD for the opportunity to work with adolescent and young adult patients at their outpatient sites. We acknowledge Mark Myers, PhD, for providing smoking cessation materials that were incorporated into our manual. We acknowledge Ryan Matlow, MA and Jessica Clifton, MA for their work as research assistants on this project and Carson Benowitz-Fredericks for his help with the literature review.
Data from this paper were presented at a Pre-Conference Workshop at the Society for Research on Nicotine and Tobacco Annual Meeting; February 25, 2015; Philadelphia, Pennsylvania, USA.
References
- 1. Agaku IT, King BA, Dube SR. Current cigarette smoking among adults - United States, 2005-2012. MMWR Morb Mortal Wkly Rep. 2014;63:29–34. [PMC free article] [PubMed] [Google Scholar]
- 2. Kann L, Kinchen S, Shanklin SL, et al. Youth risk behavior surveillance–United States, 2013. MMWR Surveill Summ. 2014;63:1–72. [PubMed] [Google Scholar]
- 3. US Department of Health and Human Services. (1994). Preventing tobacco use among young people: A report of the surgeon general. Atlanta, GA: USDHHS, CDC, Office on Smoking and Health. [Google Scholar]
- 4. Sussman S, Lichtman K, Ritt A, Pallonen UE. Effects of thirty-four adolescent tobacco use cessation and prevention trials on regular users of tobacco products. Subst Use Misuse. 1999;34:1469–1503. [DOI] [PubMed] [Google Scholar]
- 5. Doll R, Peto R, Boreham J, Sutherland I. Mortality in relation to smoking: 50 years’ observations on male British doctors. BMJ. 2004;328:1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pirie K, Peto R, Reeves GK, Green J, Beral V; Million Women Study Collaborators. The 21st century hazards of smoking and benefits of stopping: a prospective study of one million women in the UK. Lancet. 2013;381:133–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Stanton A, Grimshaw GM. Tobacco cessation interventions for young people. Cochrane Database Syst Rev. 2013;4:CD003289. [DOI] [PubMed] [Google Scholar]
- 8. Moolchan ET, Robinson ML, Ernst M, et al. Safety and efficacy of the nicotine patch and gum for the treatment of adolescent tobacco addiction. Pediatrics. 2005;115:e407–e414. [DOI] [PubMed] [Google Scholar]
- 9. Myers MG, MacPherson L. Adolescent reasons for quitting smoking: initial psychometric evaluation. Psychol Addict Behav. 2008;22:129–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sussman S, Dent CW, Nezami E, Stacy AW, Burton D, Flay BR. Reasons for quitting and smoking temptation among adolescent smokers: gender differences. Subst Use Misuse. 1998;33:2703–2720. [DOI] [PubMed] [Google Scholar]
- 11. Backinger CL, Fagan P, Matthews E, Grana R. Adolescent and young adult tobacco prevention and cessation: Current status and future directions. Tob Control. 2003;12(suppl 4):IV46–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Siddiqui O, Flay BR, Hu FB. Factors affecting attrition in a longitudinal smoking prevention study. Prev Med. 1996;25:554–560. [DOI] [PubMed] [Google Scholar]
- 13. Morrison TC, Wahlgren DR, Hovell MF, et al. Tracking and follow-up of 16,915 adolescents: minimizing attrition bias. Control Clin Trials. 1997;18:383–396. [DOI] [PubMed] [Google Scholar]
- 14. Boden JM, Fergusson DM, Horwood LJ. Cigarette smoking and depression: tests of causal linkages using a longitudinal birth cohort. Br J Psychiatry. 2010;196:440–446. [DOI] [PubMed] [Google Scholar]
- 15. Breslau N, Novak SP, Kessler RC. Daily smoking and the subsequent onset of psychiatric disorders. Psychol Med. 2004;34:323–333. [DOI] [PubMed] [Google Scholar]
- 16. Jamal M, Does AJ, Penninx BW, Cuijpers P. Age at smoking onset and the onset of depression and anxiety disorders. Nicotine Tob Res. 2011;13:809–819. [DOI] [PubMed] [Google Scholar]
- 17. Mojtabai R, Crum RM. Cigarette smoking and onset of mood and anxiety disorders. Am J Public Health. 2013;103:1656–1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Dudas RB, Hans K, Barabas K. Anxiety, depression and smoking in schoolchildren–implications for smoking prevention. J R Soc Promot Health. 2005;125:87–92. [DOI] [PubMed] [Google Scholar]
- 19. Fergusson DM, Goodwin RD, Horwood LJ. Major depression and cigarette smoking: results of a 21-year longitudinal study. Psychol Med. 2003;33:1357–1367. [DOI] [PubMed] [Google Scholar]
- 20. McKenzie M, Olsson CA, Jorm AF, Romaniuk H, Patton GC. Association of adolescent symptoms of depression and anxiety with daily smoking and nicotine dependence in young adulthood: findings from a 10-year longitudinal study. Addiction. 2010;105:1652–1659. [DOI] [PubMed] [Google Scholar]
- 21. Ramsey SE, Brown RA, Strong DR, Sales SD. Cigarette smoking among adolescent psychiatric inpatients: prevalence and correlates. Ann Clin Psychiatry. 2002;14:149–153. [DOI] [PubMed] [Google Scholar]
- 22. Schroeder SA, Morris CD. Confronting a neglected epidemic: tobacco cessation for persons with mental illnesses and substance abuse problems. Annu Rev Public Health. 2010;31:297–314. [DOI] [PubMed] [Google Scholar]
- 23. Williams JM, Steinberg ML, Griffiths KG, Cooperman N. Smokers with behavioral health comorbidity should be designated a tobacco use disparity group. Am J Public Health. 2013;103:1549–1555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Brown RA, Ramsey SE, Strong DR., et al. Effects of motivational interviewing on smoking cessation in adolescents with psychiatric disorders. Tob Control. 2003;12(suppl 4):IV3–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Leventhal AM, Waters AJ, Boyd S, Moolchan ET, Lerman C, Pickworth WB. Gender differences in acute tobacco withdrawal: effects on subjective, cognitive, and physiological measures. Exp Clin Psychopharmacol. 2007;15:21–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. McClure EA, Saladin ME, Baker NL, Carpenter MJ, Gray KM. Smoking topography and abstinence in adult female smokers. Addict Behav. 2013;38:2833–2836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Perkins KA, Scott J. Sex differences in long-term smoking cessation rates due to nicotine patch. Nicotine Tob Res. 2008;10:1245–1250. [DOI] [PubMed] [Google Scholar]
- 28. Piasecki TM, Jorenby DE, Smith SS, Fiore MC, Baker TB. Smoking withdrawal dynamics: III. Correlates of withdrawal heterogeneity. Exp Clin Psychopharmacol. 2003;11:276–285. [DOI] [PubMed] [Google Scholar]
- 29. Dickmann PJ, Mooney ME, Allen SS, Hanson K, Hatsukami DK. Nicotine withdrawal and craving in adolescents: effects of sex and hormonal contraceptive use. Addict Behav. 2009;34:620–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hall SM, Tsoh JY, Prochaska JJ, et al. Treatment for cigarette smoking among depressed mental health outpatients: a randomized clinical trial. Am J Public Health. 2006;96:1808–1814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Prochaska JJ, Hall SE, Delucchi K, Hall SM. Efficacy of initiating tobacco dependence treatment in inpatient psychiatry: a randomized controlled trial. Am J Public Health. 2014;104:1557–1565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Prochaska JJ, Fromont SC, Wa C, Matlow R, Ramo DE, Hall SM. Tobacco use and its treatment among young people in mental health settings: a qualitative analysis. Nicotine Tob Res. 2013;15:1427–1435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Grana RA, Ramo DE, Fromont SC, Hall SM, Prochaska JJ. Correlates of tobacco dependence and motivation to quit among young people receiving mental health treatment. Drug Alcohol Depend. 2012;125:127–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol. 1983;51:390–395. [DOI] [PubMed] [Google Scholar]
- 35. Hall SM, Havassy BE, Wasserman DA. Commitment to abstinence and acute stress in relapse to alcohol, opiates, and nicotine. J Consult Clin Psychol. 1990;58:175–181. [DOI] [PubMed] [Google Scholar]


