Abstract
Introduction:
There is conflicting evidence for gender differences in smoking cessation, and there has been little research on gender differences in smoking cessation medication (SCM) use and effectiveness. Using longitudinal data from the International Tobacco Control Four Country Surveys (ITC-4) conducted in the United Kingdom, the United States, Canada, and Australia, we examined gender differences in the incidence of quit attempts, reasons for quitting, use of SCMs, reasons for discontinuing use of SCMs, and rates of smoking cessation.
Methods:
Data were analyzed from adult smokers participating in the ITC-4, annual waves 2006–2011 (n = 7,825), as well as a subsample of smokers (n = 1,079) who made quit attempts within 2 months of survey. Adjusted modeling utilized generalized estimating equations.
Results:
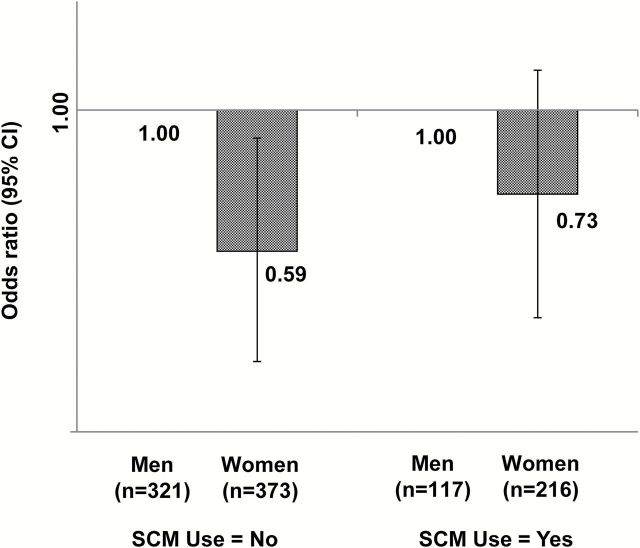
There were no gender differences in the likelihood of desire to quit, plans to quit, or quit attempts between survey waves. Among quit attempters, women had 31% lower odds of successfully quitting (OR = 0.69; 95% CI = 0.51, 0.94). Stratified by medication use, quit success was lower among women who did not use any SCMs (OR = 0.59; 95% CI = 0.39, 0.90), and it was no different from men when medications were used (OR = 0.73; 95% CI = 0.46, 1.16). In particular, self-selected use of nicotine patch and varenicline contributed to successful quitting among women.
Conclusions:
Women may have more difficulty quitting than men, and SCMs use may help attenuate this difference.
Introduction
Despite the large number of investigations examining gender differences in smoking cessation, it remains unclear whether clinically meaningful differences exist. Results from cross-sectional studies of the quit-ratio have been mixed,1–4 although more recent studies have tended to find a lack of gender differences.2,4
These cross-sectional studies, however, cannot directly assess gender differences in difficulty quitting because the denominator of the quit ratio includes both smokers who attempted to give up smoking as well as those who never attempted quitting; therefore, the quit ratio is influenced by the likelihood and frequency with which smokers make quit attempts. To more directly assess likelihood of successful smoking cessation, some studies have taken advantage of longitudinal survey data.5–8 These studies have selected for smokers who made at least one attempt to give up smoking over a follow-up period (assessed retrospectively at follow-up), and included gender differences as covariates in analyses. For example, Hymowitz et al.7 used longitudinal data from the first two waves of the National Cancer Institute’s Community Intervention Trial for Smoking Cessation (COMMIT; 1988 and 1993), selecting for smokers who had made at least one attempt to stop smoking between survey waves. They found that women were less likely to have achieved at least 6-months of abstinence than men at follow-up. Similarly, analyses from two large epidemiological studies in Copenhagen8 found that among those who attempted to stop smoking at least once since the baseline survey, women were less likely to report any smoking (either daily or non-daily) at both the 5- and 15-year follow-up. However, other longitudinal studies have found no gender differences in successful quitting.5,6,9
As noted, these longitudinal studies have an important advantage over cross-sectional studies of gender differences in cessation because they eliminate the influence of those who did not make any attempts to stop smoking over a given period of time. However, this approach still does not account for frequency of quit attempts, or factors that may differentially influence quitting by gender over time (such as pregnancy). A second potentially relevant limitation is recall bias. Previous research has shown that those who use medications during a quit attempt are more likely to recall more distal failed attempts,10 and other studies have shown that women are more likely to report use of smoking cessation medications (SCMs) than men.11 It is possible that this recall bias may have inflated gender differences in some previous investigations. The lack of consistent findings from both cross-sectional and longitudinal studies, as well as limitations of previous investigations, has led to a lack of clarity concerning gender differences in quitting.
Investigations using clinical trial data have nearly unequivocally found that women are less likely to successfully quit smoking than men.12–16 It is important to note, though, that these findings apply to a unique group of smokers (treatment seekers who typically smoke at least 10 cigarettes/day), and may or may not apply to the broader population of smokers.
Gender Differences in SCM Use and Efficacy/Effectiveness
Unlike 25 years ago, when availability of SCMs and behavioral support services were limited and rarely used by smokers, today approximately half of smokers in the general population who attempt to quit use some form of cessation aid, with proportions of medication users increasing in recent years.11,17,18 There is mixed evidence concerning gender differences in medication efficacy from clinical trial data. One meta-analysis of gender differences in nicotine patch efficacy reported equal efficacy among men and women,19 while a more recent analysis reported evidence of greater efficacy among men.20 A meta-analysis of gender differences in bupropion efficacy found no gender difference.15 While a meta-analysis of varenicline efficacy by gender does not exist, two Phase III investigations found no gender difference.21,22 Beyond clinical trial data, there is very little research on gender differences in medication effectiveness among the general population of smokers. One of the primary aims of the current investigation was to expand previous research on gender differences in smoking cessation, by testing interactions between gender and medication use in the prediction of quitting. We also examined gender differences in likelihood of medication use, reasons for stopping medication use, and effectiveness of specific medications.
Gender Differences in Quit Attempts and Quitting Motives
As secondary aims of the current investigation, we sought to examine gender differences in likelihood of attempting to stop smoking and reasons for thinking about quitting. While previous literature on gender differences in these outcomes is scant, studies examining likelihood of quit attempts have found no gender differences.5,9,23 Results from studies of quit motives have varied.24–26 Among adult smokers, McKee et al.25 found that women scored higher than men on all quitting-motive scales, including motives related to health, well-being, finances, physical appeal, and social approval. It is important to note that women also scored higher than men on several scales related to perceived risks of quitting smoking (e.g., weight gain, negative affect). In contrast, a study of former smokers in Norway found that men were more likely to report having quit smoking to improve their health and physical appearance.24 This suggests there may be a cultural component to gender differences in quitting motives, although it is difficult to draw conclusions from the few studies conducted thus far.
Study Aims and Hypotheses
In the current investigation we used data from the International Tobacco Control Four Country Survey (ITC-4), a longitudinal survey conducted in the United Kingdom, United States, Canada, and Australia to examine gender differences in several smoking cessation-related outcomes. Our two primary aims were to examine gender differences in the likelihood of achieving at least 30-days of abstinence from smoking among the overall sample and those who recently attempted to stop smoking (within the previous two months), and to determine whether gender interacted with medication use to predict likelihood of abstinence. We also examined whether sociodemographic and smoking characteristics (e.g., dependence) moderated associations between gender and achieving abstinence, and tested gender differences in the likelihood of attempting to stop smoking, quitting motives, medication use, and reasons for stopping medication use. Based on previous literature, we hypothesized that women would be less likely than men to achieve abstinence, both in the overall sample as well as among those who attempted to stop smoking. Given the lack of previous research on gender differences in cessation based on medication use, we hypothesized women would be less likely to achieve abstinence regardless of medication use. Regarding secondary aims, we hypothesized: (a) no gender differences in likelihood of attempting to stop smoking and (b) that women would report stronger quitting motives, particularly those related to health and physical appearance. We considered our investigation of reasons for stopping medication use to be exploratory and did not have a priori hypotheses.
Methods
Participants
Participants were adult smokers (i.e., aged 18+ years who smoked at least 100 cigarettes in their lifetimes and at least once in the past 30 days at baseline) recruited into the ITC-4. The ITC-4 is a cohort study which initially recruited approximately 2,000 smokers from each of four countries (i.e., United Kingdom, Canada, Australia, and United States) in 2002. Respondents are resurveyed annually, and new participants are recruited each year to replace those lost to attrition (~30% on average, ITC Waves 2–8 Technical Report27). Detailed descriptions of the study design and procedures have been published elsewhere.27–30
The analyses reported here include 7,825 respondents from any of the four countries who were interviewed between 2006 and 2011. The selection of survey waves during this 5-year period allowed us to keep our evaluation of medication use consistent over time. A subset of analyses was restricted to 1,079 participants who reported making a recent attempt to quit smoking (i.e., within two months of interview). The study protocol was approved by the institutional review boards/research ethics boards of the University of Waterloo (Canada), Roswell Park Cancer Institute (United States), University of Strathclyde (United Kingdom), University of Stirling (United Kingdom), The Open University (United Kingdom), and The Cancer Council Victoria (Australia).
Measures
Quit Attempts
During each follow-up survey, participants were asked, “Have you made any attempts to stop smoking since we last talked with you?” Those who made a quit attempt and had not relapsed were asked, “When did your most recent quit attempt start?” and those who attempted to quit but had already gone back to smoking were asked, “How long ago did your most recent quit attempt end?” and “How long were you quit for, on your most recent quit attempt?” The number of days since the start of the most recent quit attempt was determined for everyone who attempted to quit since last survey.
Reasons for Quitting
Smokers were asked whether each of the following reasons led them to consider quitting smoking during the past six months: concern for personal health; concern about the effect of cigarette smoke on non-smokers; society disapproves of smoking; the price of cigarettes; smoking restrictions at work; smoking restrictions in public places; advice from a doctor, dentist, or other health professional to quit; free, or lower cost, SCM; availability of telephone helpline/quitline/information line; advertisements or information about the health risks of smoking; warning labels on cigarette packages; setting an example for children; close friends and family disapprove of smoking (the friends/family item was included in waves 6–8 only). Response options for each item were: not at all, somewhat, or very much.
Thirty-Day Cigarette Smoking Abstinence
Respondents were classified as having quit cigarette smoking if they maintained 30-day continuous abstinence from cigarette smoking, which was determined at first follow-up among those who attempted to quit more than one month prior to the interview, and at next follow-up among those who attempted to quit within one month of first follow-up interview (since they did not yet have the chance to reach the one-month cessation endpoint at first follow-up), using the item, “How long were you quit for, on your quit attempt that had started on (quit date from Last Survey Date [LSD])?” Those whose quit attempt started less than 30 days prior to first follow-up interview and were not contacted at next follow-up were excluded from analyses even if they were known to have relapsed by first follow-up interview (n = 48; 3.8%). We also considered defining cessation as quitting use of all measured forms of tobacco (cigars, pipes, cigarillos, bidis, hookahs, chewing tobacco, moist snuff or snus, nasal snuff, Ariva, and Exalt). Prevalence of use of other forms of tobacco were low, and results did not differ based on whether cessation was defined by cigarettes only or all forms of tobacco; therefore, we only describe analyses and present findings for cigarette smoking cessation.
Use of SCMs
At each survey wave, respondents were asked, “In the last year, since LSD, have you used any stop smoking medications, such as nicotine replacement therapies like nicotine gum or the patch, or other medications that require a prescription, such as Zyban?” Those who reported that they had used medication were asked their reason(s) for using it (i.e., to stop smoking completely, to reduce the amount smoked, to cope with times when smoking is not allowed, or some other reason). Only respondents who reported using medication in an effort to stop smoking completely were considered medication users in these analyses. They were asked which product(s) they used, which were categorized as: varenicline (i.e., Chantix™/Champix™), bupropion (i.e., Zyban™/Wellbutrin™), nicotine gum, oral nicotine replacement therapy (NRT; i.e. nicotine gum, lozenges, or sublingual tablets), nicotine patch, any NRT (i.e., nicotine gum, lozenges, sublingual tablets, or patch), and any SCM (i.e., varenicline, bupropion, or any NRT). When examining gender differences in the likelihood of medication use, each medication was examined separately. We created binary variables, with those who did not use a given type of medication coded as 0, and those who did use that type of medication coded as 1. When examining medication use as a covariate/moderator in analyses evaluating cigarette smoking cessation among quit attempters, we collapsed across medications to preserve sufficient power to detect significant associations. We created a binary variable coded 0 for those who did not use any medication and 1 for those who used any medication.
Participants who had used an SCM since LSD but were not still using the medication at the time of interview were asked how long they had used it and why they discontinued use. Current users of medication were also asked how long they have been using it, but since their use is ongoing, they were not included in estimates of duration of use. Reasons for discontinuing use were categorized as: quit/it worked, didn’t work/went back to smoking, side-effects/made me feel sick, ran out, too expensive/insurance coverage ran out, stressful situation, social situation, or some other reason. Respondents could give multiple reasons for discontinuing use.
Nicotine Dependence
At each wave, current smokers were asked how many cigarettes they smoke per day and how soon after waking they have their first cigarette. Cigarettes per day were grouped into the following categories: 1–10, 11–20, and 21+ cigarettes. Time to first cigarette was grouped into the following categories: 0–10, 11–59, and 60+ min.
Socio-Environmental Variables
The following variables were evaluated as moderators of the association between gender and cessation: respondents’ country, age group (i.e., 18–29, 30–54, 55+), children (i.e., aged less than 18 years) living in the home with the respondent, other smokers living in the home with the respondent, marital status of respondent (i.e., married vs. other), smoking status of the respondent’s spouse (among those who are married), and number of the respondent’s friends who smoke (assessed with the item, “Of the five closest friends or acquaintances that you spend time with on a regular basis, how many of them are smokers?” which was used as a dichotomous variable [i.e., 0–1 vs. 2–5]).
Demographic Variables
The following control variables were included in adjusted analyses: country (i.e., United Kingdom, United States, Canada, Australia), majority/minority group (i.e., racial/ethnic group in the United Kingdom, Canada, and the United States, and English language spoken at home in Australia, per standard practice), level of education (i.e., “low” if completed high school or less in Canada, United States, and Australia, or secondary/vocational or less in the United Kingdom, “moderate” if completed community college/trade/technical school/some university (no degree) in Canada and the United States, college/university (no degree) in the United Kingdom, or technical/trade/some university (no degree) in Australia, or “high” if completed university or postgraduate in all countries), and annual household income (defined as “low” if less than US$30,000 (United States, Canada, Australia) or less than £30,000 (United Kingdom), “moderate” if between US$30,000 and US$59,999 (or £30,000 and £44,999 in the United Kingdom), or “high” if equal to or greater than US$60,000 (or £45,000 in the United Kingdom), and survey wave. The exact wording of all items used in the ITC surveys can be found at: www.ITCproject.org.
Statistical Analyses
Repeated longitudinal logistic regression analyses, via generalized estimating equations (GEEs), were used to combine data from all survey waves while accounting for multiple observations from the same individuals at different time points.31,32 Specifically, an unstructured within-person correlation matrix was specified in each GEE model and confidence intervals were calculated using a robust variance estimator. Models used to evaluate dichotomous outcomes included a specification for the binomial distribution of the dependent variable, and models used to evaluate continuous outcomes included a specification for the Gaussian distribution of the dependent variable. All analyses were conducted using Stata Version 11.
Quit Attempts, Reasons for Quitting, and Smoking Cessation
Using data from the overall sample, we examined gender differences in cigarette smoking cessation and making an attempt to quit smoking. Analyses were carried out unadjusted, and adjusted for country, age group, majority/minority group, education, income, time to first cigarette (assessed prior to the assessment of each outcome), cigarettes per day (assessed prior to the assessment of each outcome), and survey wave. We examined moderation by first stratifying the sample by the following groups: any SCM use (yes vs. no) cigarettes per day (0–10, 11–20, 21+), time to first cigarette after waking (0–10, 11–59, 60+ min), age group (i.e., 18–29, 30–54, 55+), children living in the home (yes vs. no), other smokers living in the home (yes vs. no), marital status (married vs. not married), if married—the spouse’s smoking status (yes vs. no), country, and number of friends who smoke (0–1 vs. 2–5). In each stratified analysis, estimates were again adjusted for country, majority/minority group, education, income, time to first cigarette, cigarettes per day, SCM use, and survey wave (unless stratified by one of these variables). We then used data from the overall sample to examine gender interactions with these same moderator variables, adjusting for all other variables listed above.
To examine gender differences in quit attempt success, we then selected the sample for those who had made a quit attempt within two months of the interview, and modeled smoking cessation as the outcome. We conducted analyses both unadjusted and adjusted for covariates listed above, adding SCM use as an additional adjustment variable. To test moderation, we followed the same procedures as those used for the overall sample, examining both stratified analyses and testing interactions.
To examine gender differences in medication effectiveness, we stratified the sample by gender and in separate models predicted likelihood of success (among attempters) based on the use of each individual type of medication (varenicline, bupropion, NRT patch, oral NRT). Analyses were adjusted for the same covariates as previously described models. Interactions between gender and specific medication types were not examined due to limited sample sizes of those using specific medication types.
Repeated clustered ordinal logistic regression analyses (clustered on individuals to account for repeated evaluations of the same respondents over time) were used to evaluate gender differences in the extent to which each reason led smokers to consider quitting. Analyses were unadjusted and were carried out among the overall sample and among the subset of respondents who reported making a recent quit attempt at follow-up survey.
Likelihood of Medication Use, Length of Use, and Reasons for Stopping Use
Among those who made a quit attempt since their previous interview, use of NRT gum, NRT patch, any NRT, bupropion, varenicline, and any SCM (i.e., six separate outcomes) were each evaluated as functions of gender. Analyses were carried out both unadjusted and adjusted for country, gender, age group, majority/minority group, education, income, time to first cigarette, cigarettes per day, and survey wave.
Among those who used each type of medication and ceased use by the time of interview, duration of use was evaluated as a function of gender. When calculating descriptive statistics we used the raw variables; when testing significance of associations we used natural logarithm transformation to improve normality. Associations between gender and length of use were conducted unadjusted and adjusted for country, age group, majority/minority group, education, income, time to first cigarette, cigarettes per day, and survey wave.
Reasons for discontinuing medications were evaluated as functions of gender, medication (i.e., NRT gum, NRT patch, bupropion, varenicline), among those who had ceased medication use by the time of interview. These analyses were unadjusted.
Results
Unadjusted Gender Differences in Quitting
Unadjusted gender differences in key sociodemographic and smoking cessation variables are presented in Table 1. Differences are presented for the overall sample as well as the portion of the sample that made at least one quit attempt during the two months prior to interview. Among the overall sample, there were small but significant gender differences in the likelihood of smoking cessation. Nine-percent of women quit smoking compared to 11% of men (p < .05). This gender difference was more pronounced when selecting for those who made a recent quit attempt. In this sub-sample, 17% of women quit smoking compared to 23% of men (p < .05).
Table 1.
Unadjusted Gender Differences in Key Study Variables
| Overall sample (n = 7,825) | Among quit attempters (n = 1,079; 4,959)a | |||||
|---|---|---|---|---|---|---|
| Women (n = 4,486) % | Men (n = 3,339) % | p b | Women (n = 490; 2,856)a % | Men (n = 589; 2,103)a % | p b | |
| Primary outcomes | ||||||
| ≥1 Quit attempt | 38.9 | 36.9 | .086 | – | – | – |
| Quit smoking | 9.4 | 10.9 | .004 | 16.8 | 22.2 | .009 |
| Use of smoking cessation medication (SCM): | – | – | – | |||
| NRT gum | 8.9 | 8.9 | .834 | |||
| NRT patch | 23.1 | 19.4 | <.001 | |||
| Any NRT | 34.0 | 30.2 | .002 | |||
| Bupropion | 5.0 | 4.4 | .178 | |||
| Varenicline | 11.9 | 10.0 | .005 | |||
| Any SCM | – | – | 48.2 | 42.1 | <.001 | |
| Descriptive variables and secondary outcomes | ||||||
| Time to first cigarette (min) | .139 | .575 | ||||
| 0–10 | 33.8 | 30.9 | 32.5 | 28.6 | ||
| 11–59 | 34.6 | 37.9 | 33.4 | 38.4 | ||
| 60+ | 31.5 | 31.3 | 34.1 | 33.0 | ||
| Cigarettes per day | <.001 | <.001 | ||||
| 1–10 | 31.9 | 26.5 | 40.8 | 31.1 | ||
| 11–20 | 48.1 | 45.8 | 42.1 | 43.6 | ||
| 21+ | 20.0 | 27.8 | 17.1 | 25.3 | ||
| Any children | 39.0 | 33.2 | <.001 | 34.6 | 35.9 | .485 |
| Other smokers in home | 34.9 | 29.9 | <.001 | 33.3 | 33.3 | .792 |
| Married | 51.2 | 56.7 | <.001 | 43.8 | 54.8 | <.001 |
| Spouse smokesc | 49.8 | 34.8 | <.001 | 57.5 | 46.2 | .141 |
| Friends smoke | 68.5 | 71.2 | .002 | 68.3 | 68.8 | .627 |
| Ever made a quit attempt (prior to past year) | 88.3 | 84.4 | <.001 | 95.4 | 93.4 | .132 |
| Duration of longest prior quit attempt | <.001 | .153 | ||||
| <1 week | 24.4 | 27.5 | 15.0 | 19.7 | ||
| 1 week–< 1 month | 18.8 | 19.4 | 23.3 | 21.0 | ||
| 1 month–<6 months | 25.9 | 25.4 | 25.6 | 25.7 | ||
| 6 months–<1 year | 7.6 | 5.8 | 7.6 | 6.5 | ||
| 1 year–<3 years | 13.4 | 13.0 | 15.4 | 17.0 | ||
| 3+ years | 10.0 | 8.9 | 13.3 | 10.2 | ||
| Want to quit (among those not planning) | .300 | .566 | ||||
| No | 60.2 | 62.1 | 43.4 | 48.1 | ||
| Yes | 39.8 | 38.0 | 56.6 | 51.9 | ||
| Planning to quit | .014 | – | – | – | ||
| Not planning | 29.3 | 32.2 | ||||
| Beyond 6 months | 37.1 | 35.6 | ||||
| Within 6 months | 33.6 | 32.2 | ||||
| Length of SCM use (days)d | – | – | – | |||
| NRT gum | 29.5 (40.3) | 34.2 (91.5) | .366 | |||
| NRT patch | 35.0 (42.4) | 32.7 (35.0) | .263 | |||
| Bupropion | 63.2 (115.1) | 41.2 (33.6) | .456 | |||
| Varenicline | 51.8 (50.3) | 51.0 (49.7) | .989 | |||
Analyses were unadjusted; recent quit attempters were those who recalled making a quit attempt within 2 months of the interview. Cessation was defined as self-reported 30-day abstinence from smoking at the time of the interview.
aAll variables except for SCM use and length of use were examined among those who made a quit attempt during the past 2 months at the time of their interview (the first sample size in parentheses). SCM variables were examined among those who made a quit attempt since their last interview (the second sample size in parentheses). See Methods for explanations of sample selection.
b p value based on bivariate generalized estimating equation (GEE) modeling, accounting for repeated measures design.
cAmong those who were married (wave 6 through wave 8 only). For the overall sample, n = 1,409 women, 1,166 men; for attempters, n = 80 women, 91 men.
dDuration for each medication examined among those who used that medication during a quit attempt. Sample sizes were as follows: women—NRT gum, n = 248; NRT patch, n = 683; Bupropion, n = 153; Varenicline, n = 368; Men—NRT gum, n = 169; NRT patch, n = 406; Bupropion, n = 91; Varenicline, n = 207.
Adjusted Gender Differences in Quitting
Table 2 shows adjusted associations between gender, making a quit attempt, and smoking cessation. There were significant gender differences in quit rates after accounting for relevant covariates. Among the overall sample, women had 16% lower odds of quitting smoking than men (OR = 0.84, 95% CI = 0.75, 0.94). Among those who made a quit attempt, women had 33% lower odds of successfully quitting smoking than men (OR = 0.67, 95% CI = 0.49, 0.91). There was no gender difference in the likelihood of making a quit attempt (p > .05).
Table 2.
Adjusted Gender Differences in Smoking Cessation Outcomes
| Overall sample (n = 7,825) | Among quit attempters (n = 1,079)a | |||||
|---|---|---|---|---|---|---|
| Smoking cessation | Quit attemptsa | Smoking cessationb | ||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Gender | ||||||
| Male | Ref. | Ref. | Ref. | |||
| Female | 0.84 | [0.75, 0.94] | 1.05 | [0.98, 1.13] | 0.67 | [0.49, 0.91] |
Associations examined using generalized estimating equation (GEE) modeling, adjusting for country, age group, majority/minority group, education, income, time to first cigarette after waking, cigarettes per day, and survey wave. Analyses among recent quit attempters also were adjusted for smoking cessation medication use (any use, yes vs. no).
aQuit attempters defined as those who attempted to quit within the 2 months previous to their interview.
bSmoking cessation defined as self-reported 30-day abstinence from smoking at the time of interview.
Medication Use, Gender, and Cessation
Gender differences in likelihood of using SCMs during a quit attempt are presented in Table 3. Women were more likely to have reported using nicotine patch than men (OR = 1.40, 95% CI = 1.07, 1.84). This was the only gender specific difference for use of specific medications. When predicting smoking cessation among recent attempters, the interaction between gender and medication use was nonsignificant (p value > .05). However, when recent quit attempters were stratified by medication use (Figure 1), results revealed a significant gender difference among those who did not use medications (OR = 0.59, 95% CI = 0.39, 0.90) but not among those who did use medications (OR = 0.73, 95% CI = 0.46, 1.16). Table 4 shows associations between specific types of SCM and likelihood of smoking cessation, stratified by gender. Associations between nicotine patch (vs. no medication) and cessation were significant among women (OR = 2.01, 95% CI = 1.22, 3.31) but not men (OR = 1.49, 95% CI = 0.88, 2.51). The association between varenicline and cessation also appeared to be stronger among women (OR = 3.08, 95% CI = 1.53, 6.18) than men (OR = 1.92, 95% CI = 0.92, 4.04), although the sample size was inadequate for testing interactions between gender and type of medication use.
Table 3.
Adjusted Gender Differences in Smoking Cessation Medication (SCM) Use Among Recent Quit Attempters (n = 1,079)a
| NRT gum | NRT patch | Any NRT | Bupropion | Varenicline | Any SCM | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Gender | ||||||||||||
| Male | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | ||||||
| Female | 0.94 | [0.66, 1.34] | 1.40 | [1.07, 1.84] | 1.28 | [1.01, 1.62] | 1.08 | [0.61,1.90] | 1.26 | [0.80, 2.00] | 1.26 | [1.00, 1.59] |
Associations examined using generalized estimating equation (GEE) modeling, adjusting for country, age group, majority/minority group, education, income, time to first cigarette after waking, cigarettes per day, and survey wave.
aQuit attempters defined as those who attempted to quit within the 2 months previous to their interview.
Figure 1.
Gender differences in odds for smoking cessation, stratified by smoking cessation medication use (SCM; any use, yes vs. no). Women were significantly less likely to quit smoking than men among those who did not use SCM. There was no significant difference among those who used SCM.
Table 4.
Associations Between Smoking Cessation Medication Use and Smoking Cessation Among Recent Quit Attempters, Stratified by Gender (n = 1,079)a
| Female | Male | |||||||
|---|---|---|---|---|---|---|---|---|
| n = 589 (17% quit) | n = 490 (23% quit) | |||||||
| Medication use | n | % quit | OR | 95% CI | n | % quit | OR | 95% CI |
| No medication | 373 | 13 | Ref. | 321 | 20 | Ref. | ||
| Varenicline | 44 | 32 | 4.78 | [2.21, 10.33] | 37 | 32 | 2.13 | [0.92, 4.94] |
| Bupropion | 18 | 22 | 2.45 | [0.74, 8.10] | 18 | 33 | 2.50 | [0.81, 7.75] |
| Nicotine patch | 118 | 24 | 2.34 | [1.37, 4.01] | 85 | 27 | 1.38 | [0.78, 2.43] |
| Oral NRT | 51 | 13 | 0.82 | [0.36, 1.90] | 48 | 25 | 0.99 | [0.49, 2.03] |
Associations examined using generalized estimating equation (GEE) modeling. Adjusted estimates accounted for country, age group, majority/minority group, education, income, time to first cigarette after waking, cigarettes per day, and survey wave.
aQuit attempters defined as those who attempted to quit within the 2 months before their interview. Smoking cessation defined as self-reported 30-day abstinence from smoking at the time of interview.
There were no gender differences in length of medication use among those who had ceased use of medication by the time of follow-up interview either prior to or after adjusting for covariates. Mean length of medication use tended to be longer for prescription medications (bupropion = 55 days [SD = 93], varenicline = 52 days [SD = 50]) than NRT (gum = 31 days [SD = 66], patch = 34 days [SD = 40]; Table 1). Gender differences in reasons for stopping medication use are presented in Supplementary Table S1 (online only). Differences were minor, although they followed a general pattern. Women were less likely than men to report stopping use of NRT gum and NRT patch because it worked/they quit (OR = 0.50, 0.69, respectively; p < .05), and were more likely than men to report stopping use of these same medications because of side effects (OR = 3.03, 1.85, respectively; p < .05). Women were less likely than men to report stopping varenicline use because it did not work (OR = 0.48, p < .05).
Gender Differences in Reasons for Quitting
Differences between men and women in their reasons for quitting smoking are presented in Supplementary Table S2 (online only). These results are provided for the overall sample as well as the sub-sample of recent quit attempters. In all cases where there were significant gender differences, women were more likely to endorse items than men. These included health concerns, cost of cigarettes, concern for non-smokers, societal disapproval of smoking, advice from a health professional, availability of free or lower cost SCMs, availability of helpline/quitline/information line, advertisements or information about health risks of smoking, and setting an example for children. The same pattern of results was found among recent quit attempters.
Moderators of the Association Between Gender and Cessation
We conducted several moderation analyses through both sample stratification and testing interactions. The following variables were considered as potential moderators of gender differences in quitting: country, time to first cigarette after waking (0–10, 11–69, and 60+ min), cigarettes per day (1–10, 11–20, 21+ cigarettes), whether respondents had any children, whether there were other smokers in the home, marital status, spouse’s smoking status (if married), and number of friends that smoked (0–1 vs. 2–5). When stratified by cigarettes per day, women were less likely than men to quit smoking among those consuming 11–20 cigarettes (OR = 0.48, 95% CI = 0.30, 0.76) but not among those smoking 0–10 or 21+ cigarettes (OR = 0.92, 95% CI = 0.56, 1.52; OR = 0.64, 95% CI = 0.26, 1.59, respectively). When stratified by time to first cigarette, women were less likely to quit smoking than men among those who smoked within 11–59min after waking (OR = 0.40, 95% CI = 0.23, 0.69), but not those smoking within 0–10min or after 60min (OR = 0.82, 95% CI = 0.41, 1.65; OR = 0.95, 95% CI = 0.57, 1.59, respectively). When stratified by age, women were less likely to quit smoking among those aged 30–54 (OR = 0.57, 95% CI = 0.38, 0.87), but not those aged 18–29 (OR = 0.85, 95% CI = 0.35, 2.03) or those aged 55+ (OR = 0.72, 95% CI = 0.38, 1.36). Women were also less likely than men to quit smoking among those who: lived with at least one other smoker (OR = 0.55, p < .05); were not married (OR = 0.61, p < .05); and who had 2–5 friends who smoked (OR = 0.63, p < .05). However, when sub-groups were combined none of the interactions by gender were significant (all p’s > .05). When considering cessation rates among the overall sample (without selecting for recent attempters), we found a similar pattern of results.
Discussion
There were three key findings of this study: (a) women were no more likely than men to make a quit attempt (defined as at least one attempt to stop smoking during the two months prior to interview), (b) among quit attempters, women had 31% lower odds of successfully quitting smoking (defined as 30-day abstinence at the time of interview) compared to men, and (c) successful quitting was lowest in women who did not use any SCMs (13% women vs. 20% men), and no different from men when medications were used. In particular, self-selected use of nicotine patch and varenicline contributed to successful quitting in women. Further, gender differences in quitting were only found among moderately dependent smokers (i.e., those smoking 11–20 cigarettes/day and those who smoked their first cigarette of the day within 11–59min of waking) and respondents aged 30–54. However, as in neither case was the overall interaction significant, these differences should be interpreted with caution. Despite generally higher scores on reasons for thinking about quitting among women, there were no gender differences in likelihood of wanting to quit or planning to quit (among those who did not make a quit attempt), or making a quit attempt between survey waves. Women were more likely to report stopping use of nicotine replacement therapy because of side effects.
The gender difference in quitting observed in this study is consistent with a number of previous clinical trials,12,14,15 but inconsistent with the most recent observational studies.4,6 The current investigation provides insight into this conflicting literature. It has been suggested that gender differences in clinical trial data may be due to differences between treatment seekers and non-treatment seekers.4 Our findings suggest that this is not the case: women were significantly less likely to successfully quit among those reporting they did not use any SCMs.
This study suggests multiple distinguishing factors that have resulted in conflicting evidence from previous investigations. Gender differences were most substantial and only statistically significant among those smoking 11–20 cigarettes/day (and those smoking within 11–59min of waking). Importantly, differences were least and nonsignificant among light smokers (0–10 cigarettes/day and smoking an hour after waking), who are typically not included in clinical trials but are included in population samples. The lack of gender differences among the lightest and heaviest smokers may have been due to low variability in quit rates among these groups (i.e., lightest smokers have generally higher likelihood of success; heaviest smokers have generally lower likelihood of success).
A second important differentiating factor may be recency of the attempt to quit smoking and length of time under investigation. Gender differences were more pronounced when we limited the sample to those who had made a recent quit attempt, making the sample more similar to clinical trial designs than long-term longitudinal studies or cross-sectional studies. We also limited our definition of successful quitting to one month. Results may not apply to studies that cover longer periods of time. Consensus in the literature may be reached by acknowledging that women have more difficulty quitting than men (particularly women who are moderately dependent) in a given quit attempt. Possible contributing factors may be negative affect-induced and cue-induced smoking.33–35 A woman’s menstrual phase during her quit attempt may also be an important moderator of successful quitting.36,37 Over-time these differences may be attenuated by other factors (e.g., motivation to quit, pregnancy). Pregnancy may be a particularly strong motivating factor to quit for younger women, possibly explaining the higher quit ratios among younger women compared to men in cross-sectional studies.2,4 In our study, prevalence of pregnancy among recent quit attempters was too low to have a substantial influence on quit rates, potentially explaining why we did not replicate this finding. More research is needed to evaluate these hypothesized explanations. It is also important to note that the large sample size of the current investigation may have resulted in greater power to detect small to moderate effects in comparison to some other investigations.
Another key finding from the current investigation is that gender differences in likelihood of quitting were only significant among those who did not use SCMs. This was primarily driven by low quit rates among women who did not use medications (13%, compared to 20% among men), highlighting the importance of promoting medication use among women trying to quit smoking. In analysis stratified by gender, NRT (patch) and varenicline significantly increased odds of successful cessation among women, but not men. It is important to caution that the results for specific medications were based on relatively small samples, and follow-up investigations with future waves of data will have more power to detect these effects. Still, even if results among men were significant, effect sizes were small, compared to small-moderate effect sizes among women. Previous investigations regarding differential effectiveness of nicotine replacement therapy (particularly patch) have been mixed,38,39 although placebo-controlled studies have found either no gender difference or lower efficacy among women. The findings from this observational sample do not follow this trend. However, as noted, gender differences in medication effectiveness were primarily driven by low rates of successful quitting for women who did not use any SCM. It is possible that differences in findings between this study and previous clinical trial data may be due to differences in the comparison group (non-treatment seekers vs. treatment seekers who were not given medication), or differences between those who self-select to use nicotine patch versus those who are assigned to treatment through a clinical trial.
In addition to medication use, we also found evidence for sociodemograhpic moderators of the association between gender and smoking cessation. Gender differences were significant among those with 2–5 friends who smoked (but not those with fewer friends who smoked), those who were not married, and those who lived with at least one other smoker. These findings are consistent with previous studies demonstrating women are more likely to identify with social barriers to cessation. For example, Pirie et al.40 found young adult women were more likely to agree with the following statement as a barrier to quitting: “If I quit smoking, it would be hard to go out with friends who smoke” (46.5% of women endorsed vs. 32.7% of men). McKee et al.25 similarly found that women scored higher than men on a measure indicating social ostracism as a perceived risk of quitting.
Study limitations include the relatively low survey response rates (though characteristics of responders to our survey correspond well to characteristics of responders to national benchmark surveys [ITC Wave 1 Technical Report29]), and relatively high attrition rates, which we addressed in our multivariate analyses by adjusting for characteristics known to vary with respect to retention. Our study did not include menstrual cycle phase data, and some research has associated cycle phase with likelihood of quitting.36 We were consequently unable to examine cycle as a control variable or moderator. Additionally, since our follow-up time was approximately one year, we likely underestimated the proportion of smokers who made a quit attempt. However, we attempted to control for any bias introduced by differences in quit attempt recall by restricting our analyses of smoking cessation to those who recalled making a quit attempt within two months of interview. Further, our large sample of smokers from four countries, surveyed across several years, our control for numerous potential confounders, and our analytic approach which allowed us to maximize power, are noteworthy strengths of this study.
The results of this study suggest that among general smokers making a quit attempt, women may have more difficulty successfully quitting than men, at least over the first month of an attempt, and particularly among smokers who do not use SCMs. Use of varenicline or nicotine patch during a quit attempt substantially increased the likelihood of success among women who elected to use these medications. While further investigation into gender differences in SCM efficacy/effectiveness is needed, this study suggests that the use of medications for women during a quit attempt is critical to increase rates of successful smoking cessation. Social factors, such as friends who smoke and other smokers in the household, may contribute to gender differences in difficulty quitting. This indicates a need to address social/behavioral factors when designing effective gender-sensitive smoking interventions for women.
Supplementary Material
Supplementary Tables S1 and S2 are available online at http://www.ntr.oxfordjournals.org
Funding
National Institutes of Health funding included P50 DA016511, R01 CA100362, P50 CA111236, P50 DA033945, P30 CA138313, K12DA031050, P01 CA138389, P50 DA016511 and ULTR000062; Robert Wood Johnson Foundation (045734); Canadian Institutes of Health Research (57897, 79551); National Health and Medical Research Council of Australia (265903, 540110, APP1005922).
Declaration of Interests
KMC provides expert testimony in litigation against cigarette manufacturers; he also provides consulting advice and has received grants from Pfizer, and he previously served as a co-investigator on a multi-center trial that evaluated a nicotine vaccine from Nabi Biopharmaceuticals. AH has received funding from Pfizer to purchase Varenicline for conducting a pilot study to examine the feasibility of administering Varenicline in a quitline setting. SAM has received investigator-initiated grants from Pfizer to study alcohol-varenicline interactions.
Supplementary Material
Acknowledgment
Data from this paper were presented at a Pre-Conference Workshop at the Society for Research on Nicotine and Tobacco Annual Meeting; February 25, 2015; Philadelphia, Pennsylvania, USA.
References
- 1. Centers for Disease Control and Prevention. Cigarette smoking among adults -- United States, 1991. MMWR. 1993;42:230–233 http://www.cdc.gov/mmwr/preview/mmwrhtml/00020103.htm. Accessed October 17, 2014.8450828 [Google Scholar]
- 2. Fidler J, Ferguson SG, Brown J, Stapleton J, West R. How does rate of smoking cessation vary by age, gender and social grade? Findings from a population survey in England. Addiction. 2013;108:1680–1685. [DOI] [PubMed] [Google Scholar]
- 3. Glassman AH, Helzer JE, Covey LS, et al. Smoking, smoking cessation, and major depression. JAMA. 1990;264:1546–1549. [PubMed] [Google Scholar]
- 4. Jarvis MJ, Cohen JE, Delnevo CD, Giovino GA. Dispelling myths about gender differences in smoking cessation: population data from the USA, Canada and Britain. Tob Control. 2013;22:358–362. [DOI] [PubMed] [Google Scholar]
- 5. Hyland A, Borland R, Li Q, et al. Individual-level predictors of cessation behaviours among participants in the International Tobacco Control (ITC) Four Country Survey. Tob Control. 2006;15(suppl 3):iii83–iii94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hyland A, Li Q, Bauer JE, Giovino GA, Steger C, Cummings KM. Predictors of cessation in a cohort of current and former smokers followed over 13 years. Nicotine Tob Res. 2004;6(suppl 3):S363–S369. [DOI] [PubMed] [Google Scholar]
- 7. Hymowitz N, Cummings KM, Hyland A, Lynn WR, Pechacek TF, Hartwell TD. Predictors of smoking cessation in a cohort of adult smokers followed for five years. Tob Control. 1997;6(suppl 2):S57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Osler M, Prescott E, Godtfredsen N, Hein HO, Schnohr P. Gender and determinants of smoking cessation: a longitudinal study. Prev Med. 1999;29:57–62. [DOI] [PubMed] [Google Scholar]
- 9. Rose JS, Chassin L, Presson CC, Sherman SJ. Prospective predictors of quit attempts and smoking cessation in young adults. Health Psychol. 1996;15:261–268. [DOI] [PubMed] [Google Scholar]
- 10. Borland R, Partos TR, Cummings KM. Systematic biases in cross-sectional community studies may underestimate the effectiveness of stop-smoking medications. Nicotine Tob Res. 2012;14:1483–1487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kasza KA, Hyland AJ, Borland R, et al. Effectiveness of stop-smoking medications: findings from the International Tobacco Control (ITC) Four Country Survey. Addiction. 2013;108:193–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bohadana A, Nilsson F, Rasmussen T, Martinet Y. Gender differences in quit rates following smoking cessation with combination nicotine therapy: influence of baseline smoking behavior. Nicotine Tob Res. 2003;5:111–116. [DOI] [PubMed] [Google Scholar]
- 13. Collins BN, Wileyto EP, Patterson F, et al. Gender differences in smoking cessation in a placebo-controlled trial of bupropion with behavioral counseling. Nicotine Tob Res. 2004;6:27–37. [DOI] [PubMed] [Google Scholar]
- 14. Kralikova E, Kmetova A, Stepankova L, Zvolska K, Davis R, West R. Fifty-two-week continuous abstinence rates of smokers being treated with varenicline versus nicotine replacement therapy. Addiction. 2013;108:1497–1502. [DOI] [PubMed] [Google Scholar]
- 15. Scharf D, Shiffman S. Are there gender differences in smoking cessation, with and without bupropion? Pooled-and meta-analyses of clinical trials of Bupropion SR. Addiction. 2004;99:1462–1469. [DOI] [PubMed] [Google Scholar]
- 16. Wetter DW, Kenford SL, Smith SS, Fiore MC, Jorenby DE, Baker TB. Gender differences in smoking cessation. J Consult Clin Psychol. 1999;67:555. [DOI] [PubMed] [Google Scholar]
- 17. Fiore MC. The new vital sign: assessing and documenting smoking status. JAMA. 1991;266:3183–3184. [PubMed] [Google Scholar]
- 18. U.S. Department of Health and Human Services. Reducing the Health Consequences of Smoking: 25 Years of Progress. A report of the Surgeon General, 1989. U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control, Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1989. http://profiles.nlm.nih.gov/NN/B/B/X/S/. [Google Scholar]
- 19. Munafò M, Bradburn M, Bowes L, David S. Are there sex differences in transdermal nicotine replacement therapy patch efficacy? A meta-analysis. Nicotine Tob Res. 2004;6:769–776. [DOI] [PubMed] [Google Scholar]
- 20. Perkins KA, Scott J. Sex differences in long-term smoking cessation rates due to nicotine patch. Nicotine Tob Res. 2008;10:1245–1250. [DOI] [PubMed] [Google Scholar]
- 21. Gonzales D, Jorenby DE, Brandon TH, Arteaga C, Lee TC. Immediate versus delayed quitting and rates of relapse among smokers treated successfully with varenicline, bupropion SR or placebo. Addiction. 2010;105: 2002–2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Jorenby DE, Hays JT, Rigotti NA, et al. ; Varenicline Phase 3 Study Group. Efficacy of varenicline, an alpha4beta2 nicotinic acetylcholine receptor partial agonist, vs placebo or sustained-release bupropion for smoking cessation: a randomized controlled trial. JAMA. 2006;296: 56–63. [DOI] [PubMed] [Google Scholar]
- 23. Fagan P, Augustson E, Backinger CL, et al. Quit attempts and intention to quit cigarette smoking among young adults in the United States. Am J Public Health. 2007;97:1412–1420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Grøtvedt L, Stavem K. Association between age, gender and reasons for smoking cessation. Scand J Public Health. 2005;33:72–76. [DOI] [PubMed] [Google Scholar]
- 25. McKee SA, O’Malley SS, Salovey P, Krishnan-Sarin S, Mazure CM. Perceived risks and benefits of smoking cessation: gender-specific predictors of motivation and treatment outcome. Addictive Behav. 2005;30: 423–435. [DOI] [PubMed] [Google Scholar]
- 26. Turner LR, Mermelstein R. Motivation and reasons to quit: predictive validity among adolescent smokers. Am J Health Behav. 2004;28:542–550. [DOI] [PubMed] [Google Scholar]
- 27. ITC Project. International Tobacco Control Policy Evaluation Survey (ITC Four Country Survey) Waves 2–8 technical report. Waterloo, Ontario, Canada: University of Waterloo; 2001. [Google Scholar]
- 28. Fong GT, Cummings KM, Borland R, et al. The conceptual framework of the international tobacco control (ITC) policy evaluation project. Tob Control. 2006;15(suppl 3):iii3–iii11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. ITC Project. International Tobacco Control Policy Evaluation Survey (ITC Four Country Survey) Wave 1 technical report. Waterloo, Canada: University of Waterloo; 2004. [Google Scholar]
- 30. Thompson ME, Fong GT, Hammond D, et al. Methods of the International Tobacco Control (ITC) four country survey. Tob Control. 2006;15(suppl 3);iii12–iii18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Liang K, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- 32.Hardin JW, Hilbe JM. Generalized Estimating Equations. Boca Raton, FL: Chapman & Hall; 2003.
- 33. Carpenter MJ, Saladin ME, LaRowe SD, et al. Craving, cue reactivity, and stimulus control among early-stage young smokers: effects of smoking intensity and gender. Nicotine Tob Res. 2014;16:208–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Saladin ME, Gray KM, Carpenter MJ, LaRowe SD, DeSantis SM, Upadhyaya HP. Gender Differences in Craving and Cue Reactivity to Smoking and Negative Affect/Stress Cues. Am J Addiction. 2012;21: 210–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Weinberger AH, McKee SA. Gender differences in smoking following an implicit mood induction. Nicotine Tob Res. 2012;14:621–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Franklin TR, Ehrman R, Lynch KG, et al. Menstrual cycle phase at quit date predicts smoking status in an NRT treatment trial: a retrospective analysis. J Womens Health. 2008;17:287–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Mazure CM, Toll B, McKee SA, Wu Ran, O’Malley SS. Menstrual cycle phase at quit date and smoking abstinence at 6 weeks in an open label trial of bupropion. Drug Alcohol Depend. 2011;114: 68–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Cepeda-Benito A, Reynoso JT, Erath S. Meta-analysis of the efficacy of nicotine replacement therapy for smoking cessation: differences between men and women. J consult clin psychol. 2004;72:712–722. [DOI] [PubMed] [Google Scholar]
- 39. Wetter DW, Fiore MC, Young TB, McClure JB, de Moor CA, Baker TB. Gender differences in response to nicotine replacement therapy: objective and subjective indexes of tobacco withdrawal. Exp Clin Psychopharmacol. 1999;7:135. [DOI] [PubMed] [Google Scholar]
- 40.Pirie PL, Murray DM, Luepker RV. Gender differences in cigarette smoking and quitting in a cohort of young adults. Am. J. Public Health. 1991;81:324–327. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.